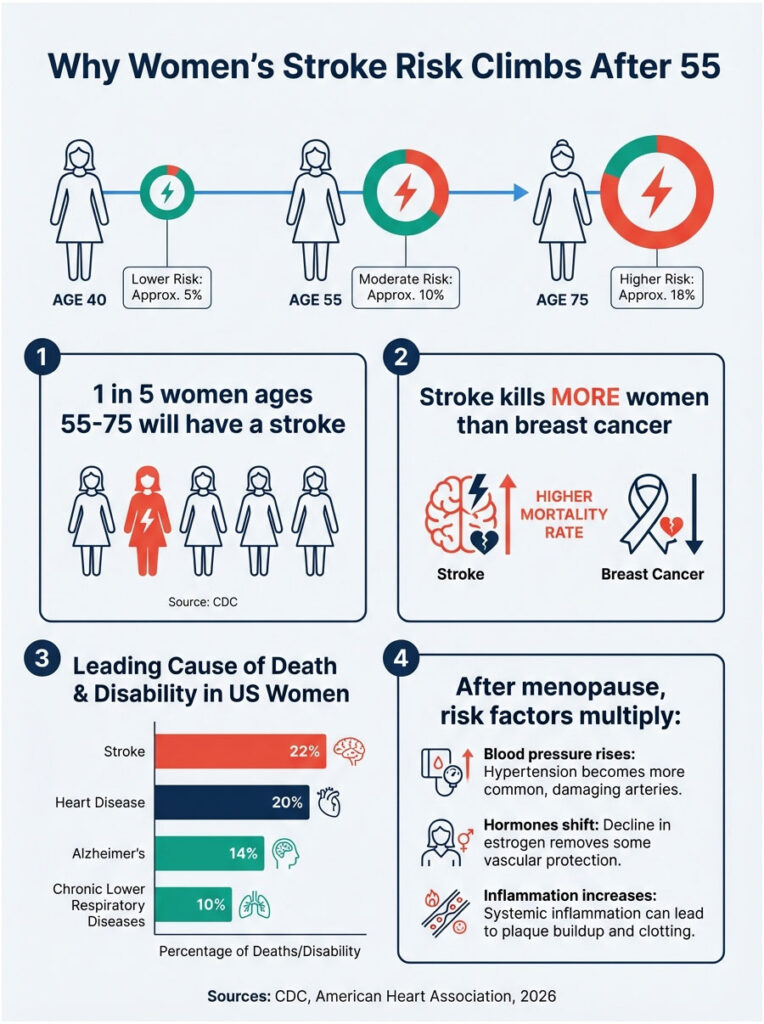
One in five American women between ages 55 and 75 will have a stroke. That’s a staggering statistic from the CDC. But here’s the thing: what you put on your lunch plate might dramatically lower those odds.
A massive new study published this month in Neurology Open Access followed over 105,000 women for more than two decades. The finding? Women who ate Mediterranean-style lunches (think chickpea salads, olive oil-drizzled vegetables, and fish) were 18% less likely to have any type of stroke compared to women who didn’t follow this eating pattern.
That’s huge. And it gets better.
The Study That’s Changing How We Think About Lunch
Researchers tracked California teachers, administrators, and retirees starting in 1995. Each woman filled out detailed questionnaires about what she ate. Then scientists waited. And watched.
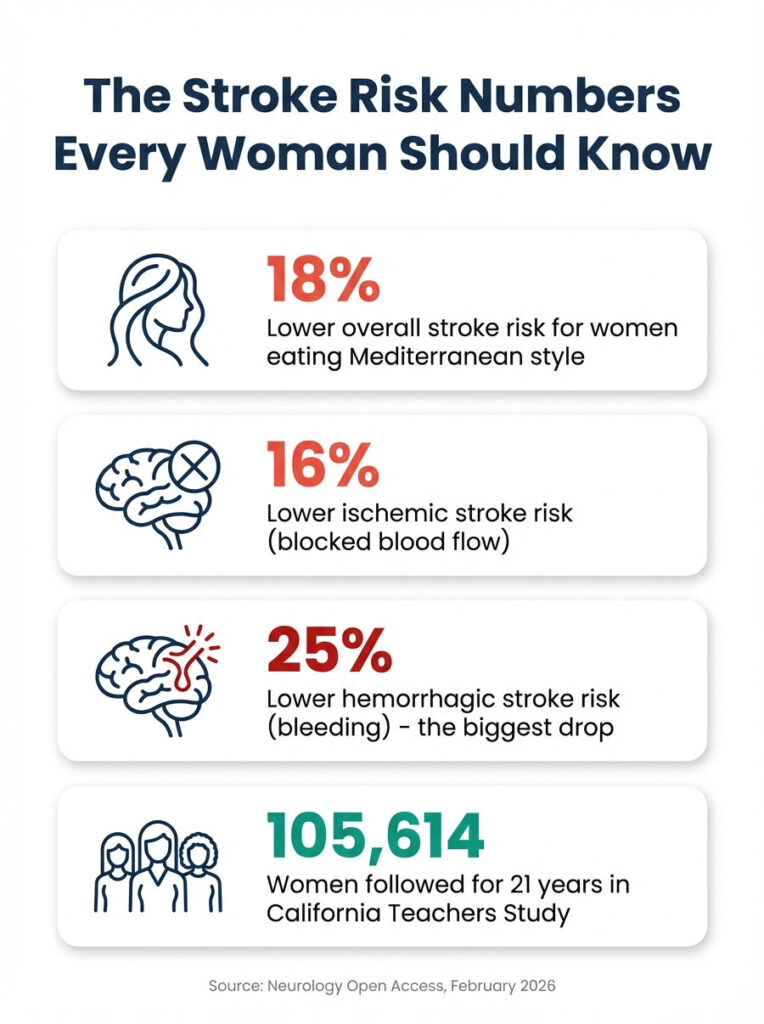
After 21 years, the results were clear. Women who scored highest on Mediterranean diet adherence (meaning they ate more vegetables, fruits, fish, olive oil, and whole grains while limiting red meat and dairy) showed an 18% drop in overall stroke risk. Their risk of ischemic stroke (caused by blocked blood flow to the brain) fell 16%. Most striking? Hemorrhagic stroke (bleeding in the brain) dropped by 25%.
Dr. Sophia Wang, a professor in the Division of Health Analytics at City of Hope Comprehensive Cancer Center in California and one of the study’s authors, put it simply. The findings support growing evidence that a healthy diet is critical to stroke prevention.
But here’s what makes this study different from the dozens of others touting Mediterranean eating. It wasn’t about fancy restaurant meals or Instagram-worthy dinner spreads. It was about what these women ate consistently, day after day. Lunch included.
Why This Hits Different for Women
Stroke kills more women than breast cancer every year. Let that sink in.
After menopause, women’s stroke risk climbs sharply. Hormonal changes, blood pressure shifts, and other factors stack up. By age 55, the danger becomes real and present.
Dr. Andrew Freeman, a preventive cardiologist and director of cardiovascular prevention and wellness at National Jewish Health in Denver (he wasn’t involved in the study), told CNN that we’ve known for a long time this is a healthier type of diet. The consistency of the evidence is what matters.
Study after study shows the same thing. A predominantly plant-based eating pattern improves all sorts of health outcomes. This isn’t a fad. It’s a pattern backed by decades of research and over 100,000 real women’s lived experiences.
The Mediterranean diet has already been linked to lower risks of dementia, depression, type 2 diabetes, and breast cancer. Now stroke joins that list with hard numbers behind it.
What This Actually Means for Your Lunch
So what did these women eat? Let’s get specific. Because “eat healthier” is useless advice. You need to know what to buy at Whole Foods or Kroger on Sunday and what to pack in your lunch bag on Tuesday.
The Mediterranean diet centers on vegetables, fruits, beans, fish, olive oil, nuts, and whole grains. It limits meat and dairy. Moderate wine consumption is fine (but optional).
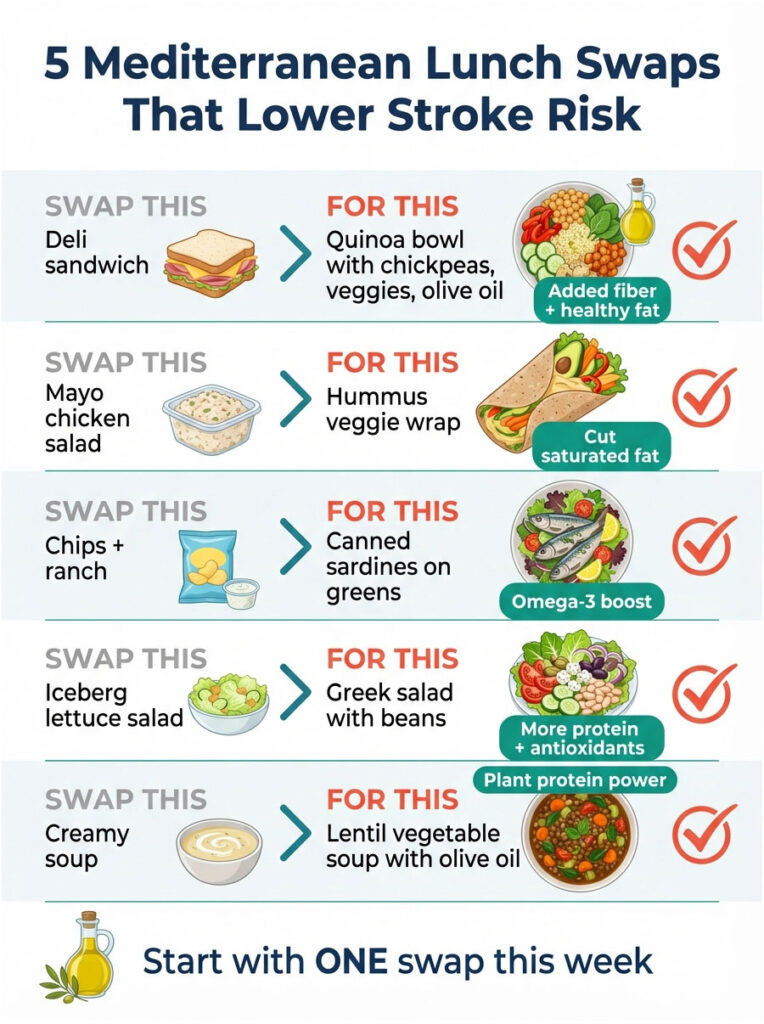
Here are five Mediterranean lunch strategies you can start this week.
Swap your deli sandwich for a loaded grain bowl. Cook a big batch of quinoa or farro on Sunday. For lunch, top it with canned chickpeas (rinse and drain them), chopped cucumber, cherry tomatoes, kalamata olives, and a handful of baby spinach. Drizzle with two tablespoons of extra virgin olive oil and a squeeze of lemon. Add a sprinkle of feta if you want. This bowl has fiber, plant protein, healthy fat, and tons of antioxidants.
Make hummus your new best friend. Swap mayo-based chicken salad for a whole-wheat pita stuffed with store-bought (or homemade) hummus, shredded carrots, sliced bell peppers, and arugula. Drizzle the inside of the pita with olive oil before adding the fillings. The fat from the olive oil and hummus keeps you full until dinner. The vegetables give you vitamins and fiber without the saturated fat bomb of a typical sandwich.
Stock your pantry with canned fish. Sardines, anchovies, and canned salmon are Mediterranean staples. They’re cheap, shelf-stable, and loaded with omega-3 fatty acids (the kind that protect your brain and heart). Try this: flake canned salmon into a bowl with cooked white beans, diced tomatoes, fresh parsley, a drizzle of olive oil, and lemon juice. Eat it cold over mixed greens or stuff it into a whole-grain wrap. Twenty grams of protein. Zero cooking required.
Think of salad as a main dish, not a side. A Greek-style salad can absolutely be lunch. Chop romaine, cucumbers, tomatoes, red onion, and bell peppers. Add a handful of chickpeas or white beans for protein. Toss with olive oil, red wine vinegar, oregano, and a little crumbled feta. Serve with a slice of whole-grain bread for dipping. This isn’t rabbit food. It’s a full, satisfying meal that takes 10 minutes to throw together.
Batch-cook a big pot of lentil or white bean soup. Lentils and beans are Mediterranean diet MVPs. They’re high in fiber and plant-based protein, and they cost basically nothing. On Sunday, simmer a pot of lentils with diced carrots, celery, onion, garlic, canned tomatoes, and vegetable broth. Season with oregano and a bay leaf. Portion it into containers. Reheat for lunch all week. Drizzle each bowl with olive oil before eating (yes, even on soup). That extra tablespoon of olive oil adds richness and those heart-protective fats the study linked to lower stroke risk.
Notice a pattern? Olive oil shows up everywhere. That’s not an accident.
The Olive Oil Question
Extra virgin olive oil is the cornerstone of Mediterranean eating. The women in this study who ate above-average amounts of olive oil scored higher on the Mediterranean diet scale. And those high scorers had the biggest drop in stroke risk.
But not all olive oil is created equal. You want extra virgin. That means it’s minimally processed and packed with antioxidants that reduce inflammation in your blood vessels. Regular olive oil doesn’t have the same benefits. Check the label. If it says “extra virgin,” you’re good.
Two tablespoons a day is the sweet spot. That might sound like a lot if you’re used to fat-free dressing and Pam spray. But remember: this isn’t about cutting fat. It’s about choosing the right fat. Olive oil is unsaturated fat. It protects your heart and brain. Butter, cream, and the fat marbling a steak? Saturated fat. That’s the stuff to limit.
Use olive oil to sauté vegetables. Drizzle it over salads. Mix it into soups. Pour it over roasted veggies. It adds flavor and keeps you full between meals. Women who follow Mediterranean eating patterns don’t skimp on olive oil. And the data shows it works.
What the Study Didn’t Prove (And Why That’s Okay)
Let’s be clear about what this research actually shows. It’s an observational study. That means researchers watched what women ate and tracked who had strokes. They didn’t assign women to specific diets and run a controlled experiment. So this study shows an association between Mediterranean eating and lower stroke risk. It doesn’t prove that the diet directly prevents strokes.
The dietary information was also self-reported. Women filled out questionnaires about what they remembered eating. People aren’t perfect at recalling every meal. Some women might have underestimated their junk food intake or overestimated their vegetable consumption.
Researchers also didn’t track changes in diet over the 21-year study period. Maybe some women started eating more Mediterranean foods after the study began. Maybe others fell off the wagon. We don’t know because diet was only measured at the start.
But here’s why the study still matters. This limitation exists in almost all long-term nutrition research. You can’t lock people in a lab and control their meals for two decades. So researchers do the next best thing: they follow huge groups of people, track their habits, and look for patterns. When you see the same pattern across multiple large studies (and we do with Mediterranean eating), the evidence becomes pretty convincing.
Dr. Freeman acknowledged these limitations but emphasized that the findings add to a long line of well-done research. The consistency is what counts. Study after study shows that a predominantly plant-based diet reduces cardiovascular and cerebrovascular disease.
Plus, there’s virtually no downside. Eating more vegetables, fish, and olive oil while cutting back on red meat and processed foods won’t hurt you. The worst-case scenario? You eat healthier and nothing happens. Best case? You slash your stroke risk by nearly 20%.
The Bottom Line
Stroke is a leading cause of death and disability for women in the United States. After menopause, the risk climbs. But this 21-year study of over 105,000 women shows that what you eat can make a real difference.
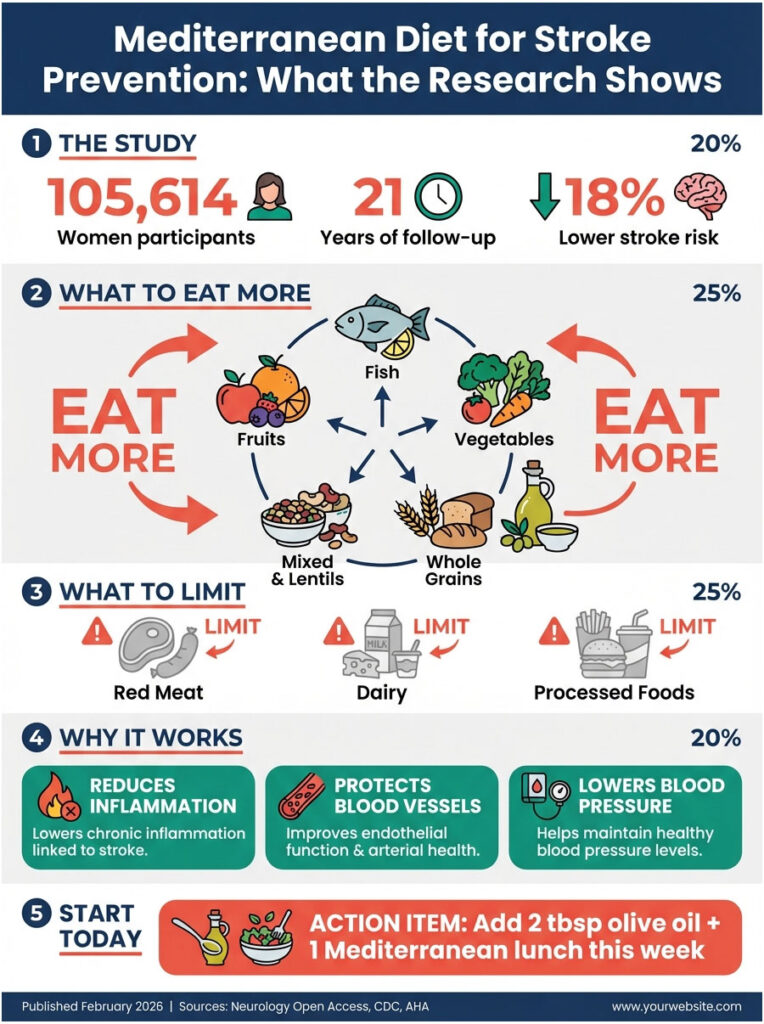
Women who followed a Mediterranean eating pattern (lots of vegetables, fruits, fish, olive oil, whole grains, and beans) had an 18% lower risk of stroke. That protection extended across all stroke types, including the rarer and deadlier hemorrhagic strokes.
The takeaway isn’t that you need to overhaul your entire life by Thursday. Start with lunch. Swap one or two meals this week for a Mediterranean-style option. Pack a grain bowl instead of a turkey sandwich. Make a big batch of lentil soup. Try hummus and veggies in a whole-wheat wrap.
Small, consistent changes add up. That’s what the California teachers taught us over 21 years. Your lunch plate is more powerful than you think.
MEDICAL DISCLAIMER
This article is here to share the latest research and give you practical ideas, not to replace advice from your doctor. Before making any changes to your diet, especially if you have existing health conditions or take medication, talk with a healthcare provider who knows your medical history. Everyone’s body responds differently, and what works for one person might not be the right fit for another. If you experience sudden symptoms like numbness, confusion, trouble speaking, or severe headache, seek emergency medical help immediately. Those could be signs of a stroke.
REFERENCES
[1] Wang SS, et al. “Association of the Mediterranean Diet With Stroke Incidence Among Middle-Aged and Older Women: Findings From the California Teachers Study.” Neurology Open Access, February 4, 2026. DOI: 10.1212/NXG.0000000000200185
[2] Centers for Disease Control and Prevention. “Stroke Facts.” CDC.gov. https://www.cdc.gov/stroke/facts.htm
[3] American Heart Association. “Mediterranean Diet.” Heart.org. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/mediterranean-diet
[4] Estruch R, et al. “Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts (PREDIMED Study).” New England Journal of Medicine, 2018. DOI: 10.1056/NEJMoa1800389
[5] City of Hope Comprehensive Cancer Center. “Dr. Sophia S. Wang, Faculty Profile.” https://www.cityofhope.org/sophia-wang
[6] National Jewish Health. “Dr. Andrew Freeman, Preventive Cardiologist.” https://www.nationaljewish.org/doctors-departments/providers/cardiologists/andrew-freeman