During a diverticulitis flare-up, the most effective non-medical intervention is immediate dietary restriction to induce “bowel rest.” You must initially switch to a clear liquid diet for 24 to 48 hours to halt colonic contractions. Following this, you must transition to a low-residue diet and strictly avoid high-fiber foods such as whole grains, raw vegetables, nuts, seeds, and popcorn. Additionally, inflammatory triggers like red meat, fried foods, and alcohol must be eliminated until all abdominal pain and infection symptoms resolve.
Table of Contents
The sudden onset of sharp, cramping pain in the lower left quadrant of your abdomen is a distinct and frightening experience. For millions of Americans, this symptom signals a diverticulitis attack. It is a moment where the fear of hospitalization often collides with confusion about what to do next. The advice you received about eating high fiber for gut health suddenly becomes dangerous misinformation. When your sigmoid colon is inflamed, fiber is no longer a friend. It is an irritant.

Managing this condition requires a complete reversal of standard nutritional rules. The foods that usually keep you regular can now cause severe pain and complications like perforation. This guide serves as your comprehensive manual for navigating the treacherous waters of an acute flare. We will dissect the physiological reasons why specific foods trigger pain, provide a scientifically backed list of the 10 foods to avoid with diverticulitis, and outline a precise, phased recovery plan that moves you from liquid sustenance back to solid health.
Understanding the Role of Diet in Managing Acute Diverticulitis Inflammation
To effectively treat your condition at home, you must understand the mechanics of food for diverticulitis flare up. Diverticulitis occurs when small pouches called diverticula, which develop in the lining of the large intestine, become infected or inflamed. This inflammation causes the intestinal wall to swell, making the passage of waste difficult and painful.

The primary goal of your diet during this phase is to reduce fecal volume. This strategy is clinically known as a “low-residue diet.” By consuming foods that are almost entirely absorbed in the stomach and small intestine, you leave very little waste for the large intestine to process. This reduction in “residue” allows the colon to rest. It minimizes the strength of peristalsis (muscle contractions) required to move stool. Less contraction means less pressure on the inflamed pouches, which directly translates to diverticulitis pain relief.
The Critical Difference Between Soluble and Insoluble Fiber
A major source of confusion for patients is the word “fiber.” You cannot treat all carbohydrates equally during an attack. You must distinguish between the two types to avoid exacerbating your symptoms.
Insoluble Fiber is the type found in wheat bran, vegetable skins, and brown rice. It does not dissolve in water. Its function is to add bulk to the stool and scour the intestinal walls. During a flare-up, this scouring action is akin to rubbing sandpaper over a fresh wound. It can cause micro-abrasions and increase the risk of bleeding or rupture.
Soluble Fiber absorbs water to form a gel-like substance. Found in oats and the flesh of fruits, it is gentler. However, during the peak of a diverticulitis attack, even soluble fiber can cause gas and distension. Therefore, the diverticulitis diet protocol requires dropping your total fiber intake to under 10 grams per day during the acute phase.
Comprehensive List of 10 Foods to Avoid Immediately During a Diverticulitis Attack
If you are currently experiencing pain, fever, or bowel irregularity, you must purge your kitchen of specific triggers. These foods that trigger diverticulitis are categorized based on their mechanical abrasiveness, gas-producing potential, or inflammatory properties.

1. Red and Processed Meats (High Inflammation Risk)
Red meat is often the first item gastroenterologists will tell you to cut. Foods like steak, burgers, pork chops, and lamb are high in saturated fats and contain tough protein fibers that take hours to digest.
The biochemical impact of red meat is significant. The digestion of red meat releases inflammatory cytokines which can aggravate the already swollen tissue in your colon. Furthermore, studies indicate that individuals who consume high amounts of red meat have an 18% to 20% higher incidence of diverticulitis compared to those who eat lean proteins.
Processed meats like bacon, sausage, hot dogs, and deli ham are even worse. They are loaded with nitrates and preservatives that disrupt the gut microbiome (the balance of good bacteria). During a flare, your microbiome is often already compromised, especially if you are taking antibiotics. Adding processed meat to the mix is fuel for the fire.
2. Whole Grains and High-Fiber Bran Products
In a healthy gut, whole grains are the gold standard. During a flare, they are a primary physical hazard. You must avoid brown rice, quinoa, barley, whole wheat bread, bran flakes, and shredded wheat.
These foods are dense with insoluble fiber. When you eat a bowl of bran cereal, the fiber passes through the stomach unchanged. When it reaches the sigmoid colon, it adds significant bulk to the stool. Your inflamed colon must then stretch to accommodate this bulk. This stretching triggers the pain receptors in the diverticula.
For the duration of your recovery, you must embrace “white” carbohydrates. Refined white bread, white rice, and plain pasta are stripped of fiber. They are digested quickly and leave minimal residue, adhering to the principles of a safe low residue diet.
3. Raw Cruciferous Vegetables (Gas and Distension)
Vegetables are usually synonymous with health, but raw cruciferous vegetables are dangerous during an attack. This category includes broccoli, cauliflower, kale, Brussels sprouts, cabbage, and bok choy.
These vegetables contain a complex carbohydrate called raffinose. Humans lack the enzyme alpha-galactosidase needed to break raffinose down in the upper digestive tract. Consequently, it travels undigested to the large intestine, where bacteria ferment it. This fermentation process produces significant amounts of methane and hydrogen gas.
When your colon is inflamed, the walls are stiff and sensitive. The rapid expansion caused by gas acts like an overinflated balloon, putting dangerous pressure on the infected diverticula. This can lead to severe cramping and, in extreme cases, contribute to micro-perforations.
4. Fried, Greasy, and Fast Foods
High-fat foods are potent triggers for colonic spasms. This includes fried chicken, french fries, onion rings, mozzarella sticks, and heavy cream sauces.
The mechanism here is hormonal. When fat enters the small intestine, the body releases hormones like cholecystokinin which stimulate the gastrocolic reflex. This reflex tells the colon to contract to make room for new food. In a healthy person, this leads to a normal bowel movement. In a person with diverticulitis, this stimulated contraction causes intense, spasmodic pain.
Greasy foods also delay gastric emptying, leaving you feeling nauseous and bloated. A strict diverticulitis diet relies on low-fat preparation methods such as poaching, steaming, or baking.
5. Nuts and Seeds (The Mechanical Irritant Debate)
The medical advice regarding nuts and seeds has evolved, but the nuance is critical. While the American Gastroenterological Association has stated that nuts and seeds do not cause diverticulitis, they are still considered foods to avoid with diverticulitis during an active flare.
The danger during a flare is mechanical. Nuts (almonds, walnuts, cashews) and seeds (sunflower, chia, sesame) are hard to chew completely. Sharp fragments often survive digestion. While they may not lodge in the pouch as previously feared, they act as physical irritants. Passing sharp, hard fragments over inflamed, swollen tissue causes unnecessary pain and potential bleeding. Avoid all trail mixes, granola bars with nuts, and seeded breads until you are fully healed.
6. Popcorn and Corn Products
Popcorn is unique because of its hull. The thin, transparent shell of the corn kernel is almost entirely insoluble cellulose. It does not break down.
Even with thorough chewing, these hulls pass through the digestive system intact. They have a tendency to slide between teeth and gums, and they can behave similarly in the folds of the intestine. For a diverticulum that is already infected, the introduction of these hulls is risky.
Whole kernel corn (like corn on the cob) presents the same issue. The outer skin of each kernel is tough and fibrous. Creamed corn (strained) might be tolerated in later stages, but whole corn and popcorn should be strictly avoided.
7. Spicy Foods and Hot Peppers
Capsaicin, the active component in chili peppers, jalapeños, and hot sauce, interacts with pain receptors known as TRPV1 receptors. These receptors are abundant in the gut lining.
During inflammation, your gut suffers from “visceral hypersensitivity.” This means your pain threshold is lowered. A level of spice that you would normally tolerate can trigger severe burning and cramping. Furthermore, spicy foods can accelerate gut transit time, leading to diarrhea. Frequent bowel movements are traumatic for an inflamed colon that needs rest.
8. Alcohol and Caffeine (Dehydration Risks)
When managing food for diverticulitis flare up, what you drink is as important as what you eat. Alcohol and caffeine are both diuretics, which means they encourage your kidneys to expel water.
Dehydration is a major enemy during recovery. If you become dehydrated, your body pulls water from the colon, resulting in hard, dry stool. Passing hard stool is excruciatingly painful during a flare and can tear healing tissues.
Caffeine is also a stimulant. Just as it stimulates your brain, it stimulates the smooth muscle of the colon. A strong cup of coffee can induce rapid, forceful contractions. During the acute phase, stick to water, herbal tea, or electrolyte solutions.
9. Beans and Legumes (Fermentation Triggers)
Beans, lentils, chickpeas, and soybeans are powerhouse sources of fiber and resistant starch. This makes them excellent for preventing diverticulitis recurrence, but terrible for treating it.
Like cruciferous vegetables, legumes are notorious for gas production due to their oligosaccharide content. The bloating caused by eating a bowl of chili or lentil soup can increase intra-abdominal pressure significantly. Until your infection has cleared and you have slowly reintroduced other foods, legumes should remain off your plate.
10. Fruits with Tough Skins and Seeds
Fruits are essential for vitamins, but their delivery method matters. You must avoid berries (strawberries, raspberries, blackberries) because of their tiny seeds which cannot be removed.
You must also avoid fruits with thick, edible skins such as apples, pears, plums, and peaches unless they are peeled. The skin is almost 100% insoluble fiber. Dried fruits like raisins, dates, and prunes are also problematic because they are concentrated sources of sugar and fiber that can draw excessive water into the gut (osmotic effect), causing cramping and diarrhea.
Comparative Analysis of Safe vs. Unsafe Foods for Diverticulitis Patients
Navigating the grocery store aisles can be confusing when you are trying to avoid so many common staples. The following comparison clarifies exactly what you should reach for and what you should leave on the shelf. This table distinguishes between high-residue triggers and low-residue safe zones.
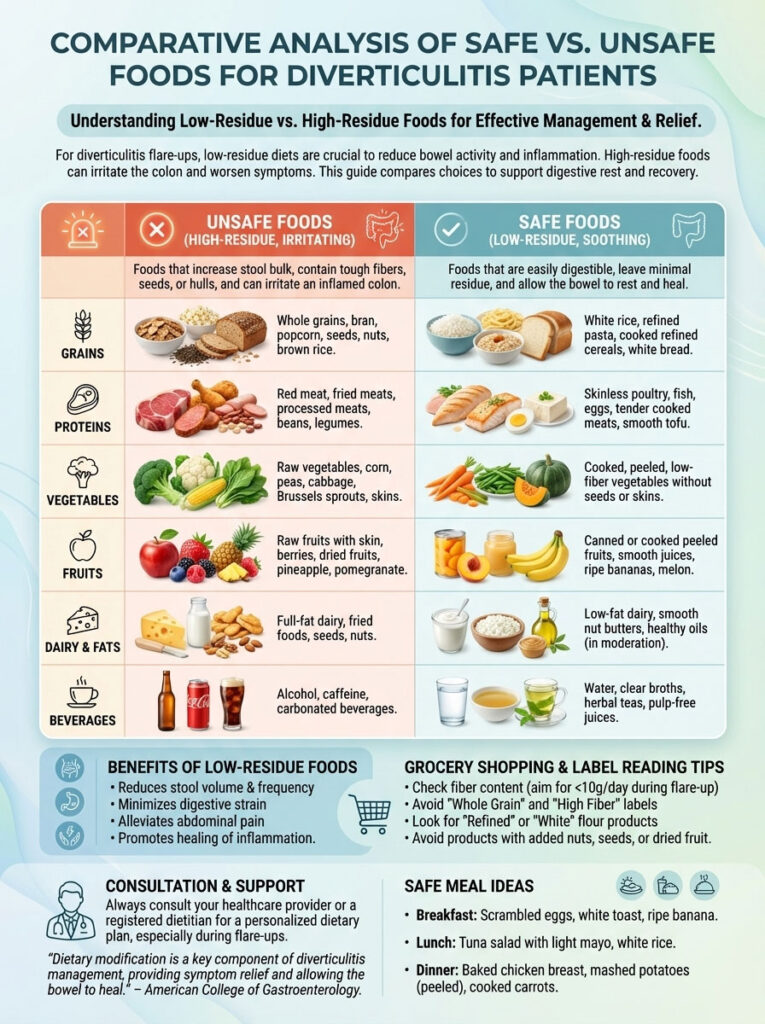
| Food Category | ❌ AVOID Immediately (High Residue/Irritant) | ✅ SAFE to Consume (Low Residue/Bland) |
| Grains & Starches | Brown rice, quinoa, wild rice, whole wheat bread, bran cereal, granola, barley, buckwheat | White rice, white bread (refined), plain pasta, saltines, cream of rice, white bagel (no seeds), couscous |
| Animal Proteins | Ribeye steak, bacon, sausage, fried chicken, pepperoni, salami, tough pork chops | Poached eggs, baked white fish (tilapia/cod), grilled chicken breast, tender turkey, tofu |
| Vegetables | Raw salad greens, spinach, broccoli, cauliflower, corn, onions, peppers, potato skins | Canned green beans, cooked carrots (peeled), mashed potatoes (no skin), pureed pumpkin, asparagus tips |
| Fruits | Raspberries, strawberries, blackberries, raw apples with skin, dried apricots, figs, raisins | Canned peaches (in water), canned pears, applesauce, ripe bananas, honeydew melon, cantaloupe |
| Dairy & Fats | Whole milk, heavy cream, high-fat cheese, yogurt with fruit pieces, crunchy peanut butter | Lactose-free milk, mild cheddar, cottage cheese, smooth yogurt, smooth peanut butter, butter (sparingly) |
| Beverages & Soups | Alcohol, espresso, energy drinks, soda, prune juice, bean soup, chowder | Water, chamomile tea, pulp-free apple juice, chicken bone broth, electrolyte drinks, clear consommé |
Step-by-Step Low Residue Diet Plan for Diverticulitis Recovery
Recovery is not a switch you flip; it is a ladder you climb. Moving from acute pain to normal eating takes time and discipline. Rushing this process is the most common reason for relapse and hospital readmission. The following three phases outline the clinical standard for recovery.
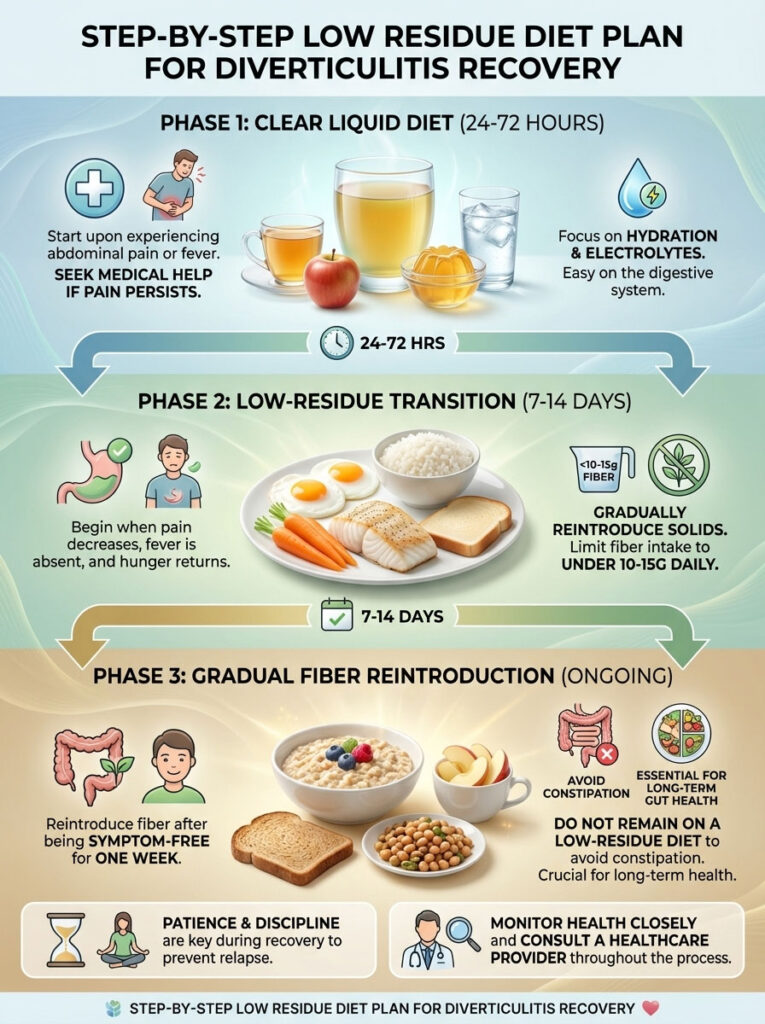
Phase 1: The Clear Liquid Diet (The “Gut Rest” Phase)
Duration: 24 to 72 hours maximum.
When to start: Immediately upon feeling specific lower abdominal pain or fever.
The objective of this phase is to provide hydration and essential electrolytes while requiring near-zero digestive effort from the colon.
- Breakfast: A glass of pulp-free apple juice and a bowl of lime gelatin.
- Lunch: Warm chicken or beef bone broth. The gelatin in bone broth is soothing and provides trace proteins.
- Snack: A fruit-flavored ice pop (ensure it contains no fruit chunks or milk).
- Dinner: Clear vegetable broth and a cup of herbal tea.
- Hydration: Sip water constantly. Electrolyte drinks (like Gatorade or Pedialyte) are recommended to maintain sodium and potassium levels.
Critical Note: If you are diabetic, monitor your blood sugar closely, as the juices and gelatin are high in simple sugars. If pain does not subside after 3 days of liquids, seek medical attention immediately.
Phase 2: The Low-Residue Transition (The Healing Phase)
Duration: 7 to 14 days.
When to start: When abdominal pain has significantly decreased, you have no fever, and you start to feel hungry again.
This is the most misunderstood phase. You are eating solids, but you are strictly limiting fiber to under 10-15g per day. The goal is nutrition without bulk.
- Breakfast: Two scrambled eggs, one slice of white toast with a thin layer of smooth jelly (no seeds).
- Lunch: A sandwich made with white bread and lean turkey breast (no lettuce or tomato), plus a cup of canned peaches.
- Snack: A ripe banana or a small container of smooth vanilla yogurt.
- Dinner: Baked white fish or a poached chicken breast, a side of white rice, and well-cooked green beans.
- Key Strategy: Chew everything thoroughly. Your mouth should do the work so your stomach and colon do not have to. Eat small portions every 3-4 hours rather than large meals.
Phase 3: Gradual Fiber Reintroduction (The Prevention Phase)
Duration: Ongoing (Starts after you are symptom-free).
When to start: When you have had normal bowel movements and zero pain for at least one week.
You cannot stay on a low-residue diet forever, or you risk constipation and long-term colonic health issues. You must re-train your gut to handle fiber.
- Week 1: Add one serving of fiber every two days. Start with a baked potato with the skin or a peeled apple.
- Week 2: Introduce oatmeal or whole wheat toast at breakfast.
- Week 3: Reintroduce cooked broccoli or beans in small amounts.
- Monitoring: If you feel twinges of pain or bloating, scale back to Phase 2 for 24 hours.
Detailed Nutritional Management and Supplementation Strategies
When you restrict your diet to white rice and broth, you are significantly reducing your intake of vitamins, minerals, and macronutrients. Prolonged restriction can lead to fatigue and muscle loss. It is vital to manage your nutrition intelligently during the diverticulitis diet phases.

The table below outlines the key nutrients at risk during a flare-up and how to source them safely without triggering symptoms.
| Nutrient Category | Physiological Role in Recovery | Safe Dietary Sources During Flare |
| High-Quality Protein | Essential for repairing damaged tissue and maintaining muscle mass during bed rest. | Eggs, lactose-free whey protein isolate, smooth Greek yogurt, silken tofu, bone broth (collagen). |
| Potassium & Sodium | Critical for maintaining fluid balance and preventing dehydration-related cramping. | Coconut water (strained), pulp-free orange juice, salted crackers, broth. |
| Probiotics | Helps repopulate the gut microbiome which may be damaged by antibiotics or inflammation. | Kefir, cultured yogurt (smooth), physician-recommended probiotic supplements (Lactobacillus strains). |
| Vitamin C & Zinc | Vital for immune function and wound healing (closing micro-perforations). | Vitamin supplements (liquid or chewable form is best for absorption), cantaloupe. |
The Role of Liquid Nutrition Supplements
During Phase 1 and early Phase 2, it may be difficult to meet your calorie needs. High-calorie nutritional shakes (like Ensure or Boost) can be helpful, but you must read the label. Choose “Plus” or “High Protein” versions, but avoid “High Fiber” versions during the acute phase. Ensure they do not contain high amounts of high-fructose corn syrup if that is a trigger for you.
Lifestyle Adjustments for Diverticulitis Pain Relief
Food is the primary lever, but how you live during a flare-up also dictates the speed of your recovery.

Strategic Hydration Protocols
Constipation is a common side effect of the low-residue diet because there is no fiber to bulk the stool. To prevent this, you must hyper-hydrate.
- The Rule: Drink at least 80 to 100 ounces of fluid daily.
- The Method: Do not chug water. Taking large gulps swallows air, which adds gas pressure to the colon. Sip consistently throughout the day using a straw or a small glass.
The Science of “Mechanical Digestion”
Your stomach does not have teeth. The more you chew your food, the less acid and churning are required by your stomach, and the more liquid the chyme (digested food) is when it enters the intestines.
- Actionable Tip: Chew every bite of food 20 to 30 times until it reaches the consistency of applesauce. This is one of the most effective ways to reduce post-meal cramping.
Meal Timing and Volume
A large meal causes rapid distension of the stomach. Through the gastrocolic reflex, this triggers strong contractions in the colon.
- Strategy: Adopt a “grazing” schedule. Eat 5 to 6 mini-meals per day. A meal might consist of just half a cup of rice and one egg. This keeps the digestive system moving gently without overwhelming it.
Stress and the Gut-Brain Axis
The connection between the brain and the gut is physical. The enteric nervous system lining your gut is sensitive to stress hormones like cortisol. Stress can induce spasms and heighten pain sensitivity.
- Technique: Practice diaphragmatic breathing (belly breathing) for 5 minutes before eating. This activates the parasympathetic nervous system (the “rest and digest” state), which relaxes the smooth muscles of the colon.
Essential Medical Context and Warning Signs
While diet is powerful, diverticulitis is a medical condition that can become life-threatening if complications like abscesses, fistulas, or perforations occur.
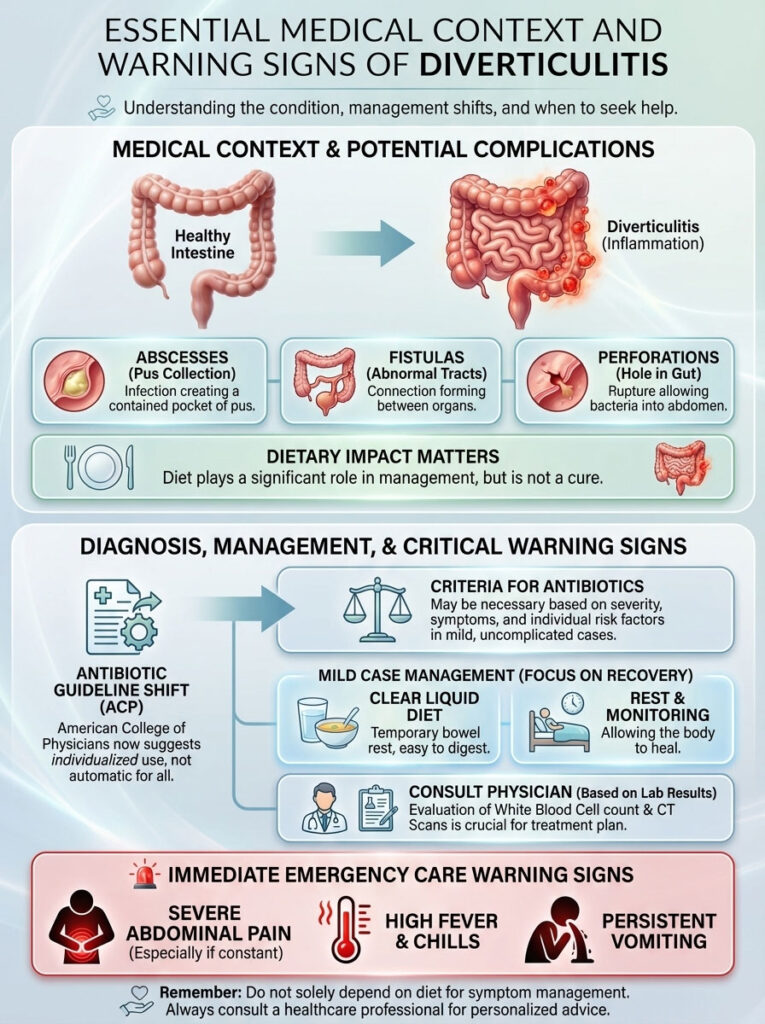
Current Perspectives on Antibiotics
It is important to note a shift in medical guidelines. Historically, antibiotics were prescribed for every diagnosis. Recent guidance from the American College of Physicians suggests that for mild, uncomplicated diverticulitis in otherwise healthy patients, antibiotics may not always be necessary. The clear liquid diet and rest may be sufficient for the body to heal itself. However, this is a decision strictly for your doctor, based on blood work (white blood cell count) and CT scan results.
When to Seek Emergency Care
Do not rely solely on diet if your symptoms escalate. Go to the Emergency Room if you experience:
- A fever rising above 100.4°F (38°C) accompanied by chills.
- Nausea that prevents you from keeping down liquids.
- Bright red blood in your stool or black, tarry stools.
- A rigid, board-like abdomen that is painful to the touch.
- Pain that radiates to your back or groin.
Frequently Asked Questions (FAQ)
Can I eat eggs during a diverticulitis flare up?
Yes, eggs are one of the safest and most nutritious foods you can eat during a flare-up. They provide high-quality protein and are easily digested with almost zero residue. Scrambled, poached, or soft-boiled eggs are ideal for Phase 2 of your recovery. Avoid frying them in heavy grease or adding cheese with added peppers or spices.
How long does a diverticulitis flare up last with diet change?
With strict adherence to a clear liquid diet followed by a low-residue diet, acute pain often begins to subside within 2 to 4 days. However, the inflammation in the colon can take 10 to 14 days or longer to fully resolve. You should not return to a normal high-fiber diet until you have been completely symptom-free for at least one week to prevent a relapse.
Is yogurt good for diverticulitis inflammation?
Yes, yogurt is beneficial, specifically because of its probiotic content which helps restore healthy gut bacteria. However, you must choose the right type. During the recovery phase, stick to smooth, low-fat yogurt. You must strictly avoid yogurts that contain fruit chunks, berries with seeds, or granola mix-ins. Greek yogurt is an excellent choice for extra protein.
Is coffee bad for diverticulitis?
Coffee should be avoided during an acute attack for two reasons. First, caffeine is a stimulant that increases bowel motility, which can cause painful spasms in an inflamed colon. Second, it is a diuretic that can lead to dehydration and harder stools. Decaffeinated coffee is a better option, but herbal tea or warm water is best during the first few days.
What is the fastest way to calm a diverticulitis flare up?
The fastest way to reduce pain is immediate “bowel rest.” Stop eating solid foods the moment you feel the characteristic pain and switch to clear liquids. Combine this with physical rest (bed rest) and a heating pad applied to the abdomen to relax cramping muscles. If prescribed antibiotics, take them exactly as directed.
Can I eat bananas during a flare?
Yes, bananas are a staple of the “BRAT” diet (Bananas, Rice, Applesauce, Toast) and are safe for diverticulitis recovery. They are soft, easy to digest, and low in insoluble fiber. Ensure the bananas are ripe; green bananas contain resistant starch that can be harder to digest and may cause gas.
Is peanut butter safe for diverticulitis?
The texture of the peanut butter is the deciding factor. Smooth, creamy peanut butter is generally safe and a good source of calories and fats during the low-residue phase. Crunchy peanut butter is strictly forbidden because the nut fragments can irritate the sensitive colon lining.
What soups are safe to eat?
During Phase 1 (Clear Liquids), you can only eat clear broths—chicken, beef, or vegetable—that have been strained of all solids. During Phase 2, you can introduce thicker, pureed soups like butternut squash or tomato soup, provided they are smooth and do not contain chunks of vegetables, cream, or milk (if you are sensitive to dairy).
Does stress cause diverticulitis flare ups?
Stress is not a direct cause of the formation of diverticula, but it is a significant trigger for flare-ups. Stress releases cortisol and adrenaline, which affect gut motility and increase inflammation and pain sensitivity. Managing stress through rest and breathing exercises is a valid component of treatment.
When can I start eating salad again?
Raw leafy greens are among the hardest foods to digest. You should only reintroduce salads after you have fully recovered, successfully reintroduced cooked vegetables, and have been pain-free for several weeks. When you do start, choose soft lettuces like butter lettuce over tough greens like kale, and chew thoroughly.
Are potatoes safe?
White potatoes are safe and soothing if they are peeled and cooked until soft (boiled, baked, or mashed). The skin of the potato is very high in insoluble fiber and must be removed during the acute and recovery phases. Sweet potatoes are also acceptable if peeled and mashed.
Should I take fiber supplements during a flare?
No. You should discontinue fiber supplements like psyllium husk, methylcellulose, or wheat dextrin during an active flare-up. Adding bulk to an inflamed colon will worsen the obstruction and pain. Reintroduce them very slowly only after you are fully healed to help prevent future constipation.
Disclaimer: The information provided in this article is for educational purposes only and does not constitute medical advice, diagnosis, or treatment. Diverticulitis can lead to serious, life-threatening complications. Always consult with a qualified gastroenterologist or healthcare provider for a personalized treatment plan.
References:
- American Gastroenterological Association (AGA) Guidelines on Management of Acute Diverticulitis.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Diet for Diverticulitis.
- Mayo Clinic: Diverticulitis Symptoms and Causes.
- Harvard Health Publishing: Diverticulitis Management Strategies.








