Medical imaging has transformed dramatically over the last century. We moved from the simple shadows of X-rays to the detailed cross-sections of Computed Tomography. Yet, physicians faced a significant limitation for years. We could see the structure of the body, but we could not see its behavior.
Table of Contents
That changed with the advent of PET CT Scan Imaging. As a specialist in Diagnostic Nuclear Medicine, I have witnessed how this hybrid technology redefines patient care. It does not just show us a mass.
It tells us if that mass is alive, aggressive, or benign scar tissue. This distinction is the difference between life-saving surgery and unnecessary intervention.
Quick Answer: What is a PET/CT Scan?
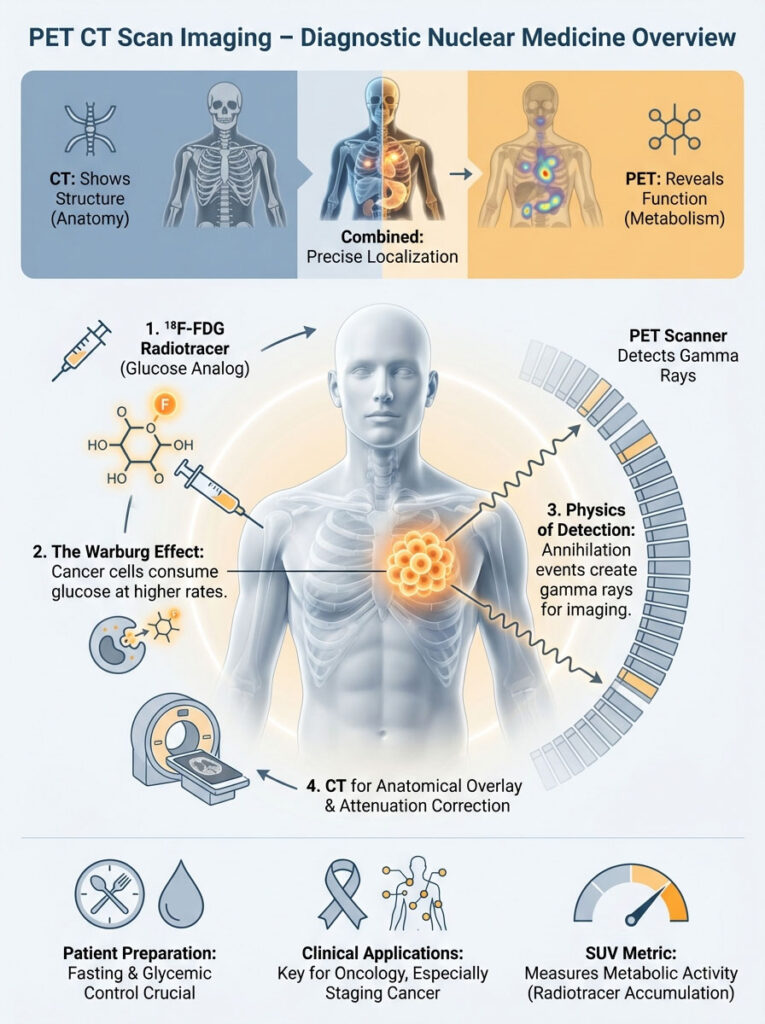
A PET/CT scan is a dual-imaging test that fuses metabolic information (PET) with anatomical structure (CT). By injecting a radioactive tracer (usually a sugar analog), the scan detects areas of high chemical activity. This highlights cancer cells, infection, or inflammation. It is primarily used to diagnose cancer, stage disease progression, and monitor treatment response.
Key Statistics in Molecular Imaging
- Management Change: PET/CT alters patient treatment plans in approximately 30% to 35% of oncologic cases (Source: National Oncology PET Registry).
- Sensitivity: For Hodgkin Lymphoma, PET/CT sensitivity exceeds 90%, significantly higher than CT alone.
- Radiation Dose: The typical effective dose ranges from 10 to 25 mSv, depending on the protocol.
- Scan Time: Total time on the table is typically 20 to 30 minutes, though the uptake phase takes 60 minutes prior.
- Glucose Usage: The brain consumes nearly 20% of the body’s glucose, making it naturally bright on scans.
The Convergence of Anatomy and Physiology
To understand the power of PET CT Scan Imaging, you must understand the difference between form and function. A standard CT scan is like a photograph of a building. It shows you the walls, the windows, and the roof.
However, it cannot tell you if there are people working inside. It cannot tell you if the electricity is on. The PET component provides that functional data.
In my twenty years of interpreting nuclear medicine studies, I have reviewed countless cases. I recall a specific patient with a lymph node that looked normal by size criteria on a CT scan. It measured less than one centimeter.
Yet, that same node lit up intensely on the PET scan. Without the metabolic insight provided by PET CT Scan Imaging, that cancer would have been missed. The patient would have been staged incorrectly.
Conversely, I have seen large masses that looked terrifying on a CT scan. They showed zero metabolic activity on PET. This confirmed they were merely old scar tissue.
This ability to distinguish active disease from benign remnants is the cornerstone of modern diagnostic accuracy. It prevents patients from undergoing toxic treatments they do not need.
The Science of Molecular Imaging: How It Works
The magic of this technology lies in the radiotracer. The most common tracer used in the USA is 18F-FDG / Radiotracer (Fluorodeoxyglucose). This is essentially a glucose (sugar) molecule attached to a radioactive isotope, Fluorine-18.
The Warburg Effect
Why do we use sugar? In the 1920s, Otto Warburg discovered that cancer cells have a unique metabolic signature. They consume glucose at a rate 20 to 30 times higher than normal cells.
They do this to fuel their rapid division. We call this the “Warburg Effect.” When we inject a patient with 18F-FDG / Radiotracer, the cancer cells greedily devour it.
They mistake it for normal sugar. However, once inside the cell, the FDG becomes trapped. It cannot be metabolized further, so it accumulates within the tumor.
Physics of Detection
The physics behind this is fascinating. As the 18F-FDG / Radiotracer decays, it emits a positron. A positron is essentially an antimatter electron.
This positron travels a tiny distance before colliding with a nearby electron in the patient’s body. This collision is called an “annihilation event.” It converts the mass of both particles into pure energy.
This energy takes the form of two gamma rays traveling in exactly opposite directions. They shoot out 180 degrees apart. The PET scanner is a ring of crystals waiting for these strikes.
This is known as “coincidence detection.” The scanner only records a signal if two detectors opposite each other are hit at the exact same time. By calculating where these lines intersect, the computer builds a 3D image of sugar concentration.
The Role of the CT Component
The CT scanner performs two jobs. First, it provides the anatomical overlay. We need to know exactly where the glowing hot spot is located.
Second, it performs “attenuation correction.” Dense body parts (like the spine or pelvis) block some radiation. Without correction, deep structures would look falsely faint.
The CT map helps the computer correct for this density. It ensures that a tumor deep in the abdomen appears with the correct intensity. This quantitative accuracy is vital for monitoring treatment.
Patient Preparation: The Critical Role of Glycemic Control
The quality of PET CT Scan Imaging is entirely dependent on patient preparation. As a physician, I cannot overstate this. If the prep is wrong, the scan is non-diagnostic.
We are taking a picture of sugar metabolism. If your body’s sugar handling is altered, the picture will be blurry. Compliance is key.
The Fasting Rule
Patients must fast for at least 6 hours before the appointment. We prefer 6 to 8 hours. This is not just to prevent nausea.
When you eat, your body releases insulin. Insulin’s job is to drive sugar into your muscles and fat cells. This is a problem for us.
If insulin levels are high when we inject the 18F-FDG / Radiotracer, the tracer will go straight into your muscles. It will bypass the tumor. We call this “biodistribution alteration.”
The result is a scan that looks like a muscle anatomy chart. The cancer is hidden behind the noise. The scan becomes unreadable.
Hydration and Exercise
We encourage drinking plain water. Hydration helps flush unbound radiation out of the kidneys and bladder. This reduces background noise in the abdomen.
It also lowers the radiation dose to the bladder wall. However, exercise is strictly prohibited for 24 hours prior. This includes heavy lifting or long runs.
Even a heavy workout the day before can cause your muscles to repair themselves. Repair requires glucose. This results in “muscle uptake” that can hide disease.
Expert Insight: Instructions for Diabetics
Diabetic management is the biggest challenge in PET CT Scan Imaging. Ideally, blood glucose should be under 200 mg/dL at the time of injection.
- Type 2 Diabetics: Usually, we ask you to hold oral medications like Metformin on the morning of the scan.
- Insulin-Dependent: We typically schedule you for early morning. You should not take short-acting insulin within 4 hours of the scan, as it will force the tracer into muscles.
Always consult the imaging center for their specific protocol.
The Patient Experience: Step-by-Step
Understanding the process alleviates anxiety. Here is what happens when you arrive for a PET CT Scan Imaging appointment. The total time in the center is usually around two hours.
Arrival and Screening
You will check in and complete a safety questionnaire. A technologist will review your medical history. They will check your blood sugar via a finger stick.
If your glucose is too high (usually above 200 mg/dL), we may have to reschedule. High sugar competes with the radiotracer. It prevents the scanner from seeing the cancer.
The Injection and Uptake Phase
Once cleared, an IV is placed in your arm. The 18F-FDG / Radiotracer is injected. It is a small amount of liquid and you will feel no difference.
You then move to a “quiet room.” This is a crucial 60-minute period. You must sit or lie perfectly still.
You cannot read, look at your phone, or chew gum. Why? Because brain activity uses sugar.
Eye movement uses sugar. Chewing uses jaw muscles. Any activity will cause the tracer to accumulate in those areas, potentially obscuring tumors in the head and neck.
The Scan
After an hour, you move to the scanner. You will lie on a narrow table. The table moves through the doughnut-shaped gantry.
The CT scan happens first. It is fast and quiet. It takes less than a minute.
Then, the PET scan begins. The table moves in small steps. This part takes 20 to 30 minutes.
It is silent. You must breathe normally and stay still. Motion is the enemy of image sharpness.
Clinical Applications: Oncology Staging and Diagnosis
Oncology is the primary driver for Positron Emission Tomography utilization. The ability to stage cancer accurately determines the entire care path. It decides whether a patient receives surgery, chemotherapy, or radiation.
Lung Cancer Assessment
Lung cancer is one of the most common indications. A patient might appear to have a localized lung tumor on a standard X-ray. It looks operable.
However, a whole-body PET CT Scan Imaging study might reveal a distant metastasis. We often find spread in the adrenal gland or bone. This “upstaging” occurs in roughly 30% of cases.
This finding saves the patient from undergoing a futile surgery. Instead of removing a lung lobe, the patient is referred for systemic therapy. This preserves quality of life.
Lymphoma Evaluation
For Hodgkin and Non-Hodgkin Lymphoma, this scan is the gold standard. Lymphoma involves the immune system. It can appear anywhere in the body.
We use the “Deauville Score” to grade response. This is a 5-point scale based on visual intensity. A score of 1 or 2 is complete metabolic response.
A score of 4 or 5 indicates active disease. This score dictates if chemotherapy should be shortened or intensified. It allows for personalized medicine.
Breast Cancer Staging
While mammography finds the primary tumor, PET is used for advanced staging. It is excellent at detecting spread to the axillary lymph nodes. It also finds metastases in the internal mammary chain.
Furthermore, it is highly sensitive for bone metastases. Lytic bone lesions light up brightly. This often precedes the structural damage seen on CT.
Colorectal Cancer and CEA Levels
Colorectal cancer often spreads to the liver. Sometimes, a patient has a rising tumor marker (CEA) in their blood. Yet, their CT scan looks normal.
A PET scan can identify the recurrence. It might find a small implant in the peritoneum or a liver lesion. Early detection here allows for curative resection.
Comparison Table: Imaging Modalities Explained
Patients often ask why they need a PET scan if they just had a CT or MRI. The following table outlines the distinct differences between these modalities.
| Feature | Standard CT Scan | MRI | PET/CT Scan |
|---|---|---|---|
| Primary Focus | Anatomy & Structure (Bones, Organs) | Soft Tissue Contrast & Fluid | Cellular Metabolism & Function |
| Contrast Agent | Iodine-based (Intravenous/Oral) | Gadolinium | Radiotracers (e.g., 18F-FDG) |
| Radiation Exposure | Moderate | None | Moderate to High (Dual modality) |
| Scan Duration | 5–10 Minutes | 30–60 Minutes | 20–30 Minutes (plus 60 min uptake) |
| Best For | Trauma, Bleeding, Appendicitis, Fractures | Brain, Spine, Joints, Liver | Cancer Staging, Dementia, Cardiac Viability |
Treatment Monitoring: The Power of Response
How do we know if chemotherapy is working? Traditionally, we waited for the tumor to shrink. We used criteria known as RECIST (anatomical size).
However, tumors often die from the inside out. They might stop growing but remain the same size. This is where PET CT Scan Imaging excels.
Metabolic Shutdown
A tumor will often stop consuming sugar long before it shrinks. We call this metabolic shutdown. PET CT Scan Imaging can show this response weeks or months earlier than a CT alone.
We use PERCIST criteria for this. If the metabolic activity drops significantly after two cycles of chemo, we know the treatment is effective. We continue the course.
Pivot or Proceed
Conversely, if the metabolic activity remains high, the drug is failing. The oncologist can switch drugs immediately. This spares the patient from the side effects of an ineffective drug.
It also saves valuable time. In aggressive cancers, time is the most precious commodity. This real-time feedback loop is revolutionary.
Beyond Oncology: Neurology and Cardiology
While cancer is the dominant application, PET CT Scan Imaging plays a vital role in other specialties. It answers questions that MRI and CT cannot.
Differentiating Dementia
In neurology, we use it to differentiate types of dementia. Alzheimer’s disease presents with a very specific pattern. We see “hypometabolism” (low activity) in the temporal and parietal lobes.
This looks distinct from Frontotemporal Dementia. In that disease, the frontal lobes go dark. Lewy Body Dementia affects the occipital lobes (visual processing).
Identifying these patterns early helps neurologists. They can prescribe the correct medications. It also helps families plan for the future.
Myocardial Viability
In cardiology, we perform “Myocardial Viability” studies. Consider a patient with severe heart failure. Surgeons need to know if the heart muscle is dead (scar tissue) or just “hibernating.”
Hibernating muscle is alive but starving for blood. It stops beating to save energy. Positron Emission Tomography with 18F-FDG is the gold standard here.
If the heart muscle takes up the sugar, it is still alive. It will likely recover after bypass surgery. If it does not take up sugar, it is scar tissue.
In that case, surgery would be high-risk with low reward. The patient might be better served by a transplant or medical management.
Interpreting the Results: The SUV Metric
When you receive a report, you will likely see a number called the Standardized Uptake Value (SUV). This is a mathematical calculation. It measures how bright a spot is relative to the dose injected and the patient’s body weight.
What is a “High” SUV?
The Standardized Uptake Value (SUV) is not a simple pass/fail grade. It requires context. An SUV of 2.5 in a lung nodule is suspicious for malignancy.
However, an SUV of 2.5 in the liver is considered normal background activity. Generally, aggressive tumors have high SUVs (often >10). Low-grade tumors have lower values.
We look at SUVmax (the hottest pixel) and SUVmean (the average). We compare these to the background “blood pool” activity. If the nodule is hotter than the blood pool, it warrants investigation.
False Positives and Pitfalls
A high Standardized Uptake Value (SUV) does not always mean cancer. Infection and inflammation also consume glucose avidly. A patient with active pneumonia will light up on a PET scan.
A healing surgical wound will also glow. This is where the “CT” part of PET CT Scan Imaging is essential. Seeing the morphology (shape) of the lesion helps us decide.
Is it a spiky, irregular tumor? Or is it a wedge-shaped consolidation typical of pneumonia? The Nuclear Medicine Physician synthesizes this data to render a diagnosis.
Advanced Tracers and Theranostics
While 18F-FDG / Radiotracer is the workhorse, it is not perfect. Some cancers do not consume sugar efficiently. Prostate cancer and neuroendocrine tumors are prime examples.
For these, we use specialized molecules. This represents the cutting edge of the field.
PSMA PET for Prostate Cancer
Prostate cancer cells overexpress a protein called Prostate-Specific Membrane Antigen (PSMA). New tracers like Pylarify (18F-pL) bind specifically to this protein.
PSMA PET for prostate imaging has revolutionized urology. We can now see microscopic recurrence at PSA levels as low as 0.2 ng/mL. This was impossible with older technology.
We can pinpoint a single lymph node in the pelvis. This allows for targeted radiation rather than blind systemic therapy.
Theranostics: See It, Treat It
This leads to the exciting field of Theranostics. If we can see the tumor with a diagnostic isotope, we can replace that isotope. We switch it for a therapeutic one.
For example, we use Gallium-68 PSMA to find the cancer. Then, we inject Lutetium-177 PSMA to treat it. The therapeutic isotope travels to the exact same location.
It delivers a lethal dose of beta radiation directly to the cancer cell. This spares the surrounding healthy tissue. This “search and destroy” method is the future of Diagnostic Nuclear Medicine.
Comparison Table: Common Radiotracers
Different diseases require different keys to unlock the diagnosis. Here is a breakdown of the tracers we use beyond standard glucose.
| Radiotracer | Target Mechanism | Primary Clinical Use | Typical Half-Life |
|---|---|---|---|
| 18F-FDG | Glucose Metabolism | Lung, Lymphoma, Melanoma, Breast Cancer | ~110 Minutes |
| 18F-Sodium Fluoride | Bone Remodeling | Skeletal Metastases (Bone Scan replacement) | ~110 Minutes |
| 68Ga-Dotatate | Somatostatin Receptors | Neuroendocrine Tumors (Carcinoid) | ~68 Minutes |
| 18F-PSMA (Pylarify) | PSMA Protein Expression | Prostate Cancer Recurrence & Staging | ~110 Minutes |
| 13N-Ammonia | Myocardial Perfusion | Cardiac Blood Flow (Stress Test) | ~10 Minutes |
Safety, Radiation, and Risks (ALARA)
Safety is a valid concern for any patient undergoing PET CT Scan Imaging. Because it is a dual modality, patients are exposed to radiation from both sources. This includes the CT X-rays and the 18F-FDG / Radiotracer.
The typical effective dose is between 10 and 25 millisieverts (mSv). To put this in perspective, the average American receives about 3 mSv of background radiation per year. This comes from the sun and soil.
The Risk-Benefit Analysis
We adhere strictly to the ALARA principle. This stands for “As Low As Reasonably Achievable.” We adjust the CT dose based on the patient’s body mass index (BMI).
This ensures we use the minimum amount of radiation necessary to get a diagnostic image. The risk of not detecting a spreading cancer almost always outweighs the theoretical risk of the radiation dose. In oncology, information is survival.
Contraindications
However, strict contraindications exist. Pregnant women should avoid Positron Emission Tomography unless it is a medical emergency. The fetus is highly sensitive to radiation.
Breastfeeding mothers are typically advised to “pump and dump” their milk. This is usually required for a specific period after the injection. This prevents passing the tracer to the infant.
Infection and Inflammation: The Hidden Utility
Beyond cancer and heart disease, we use this tool for diagnostic dilemmas. One common scenario is “Fever of Unknown Origin” (FUO). A patient has had a fever for weeks, but all blood tests are normal.
A PET scan can find the source. It might reveal an infected heart valve (endocarditis). It could show a pocket of infection in the spine (discitis).
It can also detect large vessel vasculitis. This is an inflammation of the aorta. Diagnosing this early prevents catastrophic aneurysms.
The Role of the Nuclear Medicine Physician
It is important to understand who is reading your scan. A Nuclear Medicine Physician or a dual-boarded Radiologist interprets these images. This requires years of specialized training.
We do not just look at the pictures. We correlate them with your history, pathology reports, and prior scans. We look for artifacts that mimic disease.
For example, “brown fat” in the neck can light up when a patient is cold. An inexperienced reader might call this cancer. An expert knows it is just a physiological response to temperature.
Summary & Key Takeaways
PET CT Scan Imaging stands at the forefront of personalized medicine. By fusing anatomical precision with metabolic data, it provides the “whole picture.” Modern oncology requires this level of detail.
Whether it is for initial staging, assessing chemotherapy response, or detecting a subtle recurrence, this technology changes the course of treatment. It saves lives by directing the right therapy to the right patient.
The quality of the scan depends heavily on patient compliance. Fasting, hydration, and proper glucose control are the variables that patients can control. These factors ensure your Nuclear Medicine Physician gets clear images.
If you are facing a cancer diagnosis, discuss this with your oncologist. Ask whether molecular imaging is appropriate for your specific condition. It could be the key to a more accurate diagnosis and a better outcome.
Frequently Asked Questions
What is the main difference between a PET scan and a standard CT scan?
A standard CT scan focuses on anatomical structures like bones and organs, while a PET scan evaluates cellular metabolism and function. By fusing these modalities, PET CT provides a dual-layer map that shows both where a lesion is located and whether it is biologically active. This allows us to distinguish between active disease and benign scar tissue that might look identical on a regular CT.
Why do I need to fast for six hours before my PET CT imaging?
Fasting is essential to lower your blood insulin levels, ensuring the 18F-FDG radiotracer is absorbed by glucose-hungry cancer cells rather than your muscles. If you eat before the scan, insulin will drive the tracer into your skeletal muscles, creating “background noise” that can hide tumors. Maintaining a fasting state for at least 6 hours ensures the highest diagnostic sensitivity.
What does a high Standardized Uptake Value (SUV) mean on a PET report?
The Standardized Uptake Value (SUV) is a semi-quantitative metric used to measure the intensity of radiotracer accumulation in a specific area. While a higher SUV often correlates with more aggressive metabolic activity, it must be interpreted in context, as inflammation or infection can also cause elevated values. We compare these numbers against background activity in the liver or blood pool to determine the clinical significance of a “hot spot.”
How does the Warburg Effect explain why cancer shows up on a PET scan?
The Warburg Effect refers to the phenomenon where cancer cells consume glucose at a significantly higher rate than normal cells to fuel rapid division. Since our primary radiotracer, 18F-FDG, is a sugar analog, these hypermetabolic cells “greedily” take up the radioactive tracer. This allows the PET scanner to detect biochemical changes in the body long before structural changes appear on an X-ray or CT.
Can I exercise the day before my PET CT scan?
Physical activity must be avoided for 24 hours prior to your scan because muscle repair requires significant glucose consumption. Strenuous exercise can cause “muscle uptake,” where the radiotracer accumulates in the legs, arms, or torso instead of the areas we need to evaluate. This metabolic distraction can obscure small tumors and lead to a non-diagnostic or misinterpreted study.
How should diabetic patients prepare for a PET CT scan?
Diabetic patients require careful management because high blood glucose levels compete with the 18F-FDG tracer for entry into cells. Generally, we aim for a blood sugar level below 200 mg/dL and advise against taking short-acting insulin within four hours of the injection. We typically schedule these appointments for early morning to better manage fasting requirements and medication timing.
What is the purpose of the 60-minute uptake phase after the radiotracer injection?
The 60-minute uptake phase allows the 18F-FDG radiotracer to circulate through your bloodstream and be fully absorbed by tissues with high metabolic activity. During this hour, you must remain perfectly still and quiet to prevent the tracer from accumulating in active muscles or brain regions used for talking or reading. This resting period is critical for ensuring that the final images are sharp and free of physiological artifacts.
How is PET CT used to determine if chemotherapy is actually working?
PET CT imaging is superior to standard CT for monitoring treatment because it detects “metabolic shutdown” before a tumor actually shrinks in size. Using PERCIST criteria, we can see if a tumor has stopped consuming sugar after just a few cycles of chemotherapy. This real-time feedback allows oncologists to either proceed with effective treatment or pivot to a different drug if the cancer remains metabolically active.
What are the specific benefits of PSMA PET scans for prostate cancer patients?
PSMA PET imaging uses specialized tracers that bind to the Prostate-Specific Membrane Antigen protein found on the surface of prostate cancer cells. This technology is far more sensitive than traditional bone scans or CTs, allowing us to detect microscopic recurrences at very low PSA levels. It is a game-changer for staging and localized treatment planning in patients with biochemical recurrence.
Is the radiation exposure from a PET CT scan dangerous?
The effective radiation dose from a PET CT scan typically ranges from 10 to 25 mSv, which combines the exposure from the radiotracer and the CT component. While this is higher than a standard X-ray, we follow the ALARA (As Low As Reasonably Achievable) principle to minimize exposure while ensuring diagnostic quality. In most oncologic cases, the life-saving information gained from accurate staging far outweighs the theoretical risks of the radiation dose.
How does PET imaging help differentiate between types of dementia like Alzheimer’s?
In neurology, PET scans identify specific patterns of “hypometabolism,” or reduced sugar usage, in different regions of the brain. Alzheimer’s disease typically shows low activity in the temporal and parietal lobes, whereas Frontotemporal Dementia affects the frontal lobes. These metabolic signatures help clinicians provide an accurate diagnosis when clinical symptoms and MRI findings are inconclusive.
What is Theranostics and how does it relate to nuclear medicine imaging?
Theranostics is an emerging field that combines “therapy” and “diagnostics” by using the same molecular target for both imaging and treatment. We first use a diagnostic radiotracer to “see” the tumor, and if it lights up, we switch the isotope to a therapeutic one that delivers targeted radiation directly to the cancer cells. This “search and destroy” approach represents the pinnacle of personalized nuclear medicine.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The field of Diagnostic Nuclear Medicine is complex and constantly evolving. Always consult a qualified healthcare professional, oncologist, or Nuclear Medicine Physician before making health decisions or interpreting imaging results.
References
- National Oncology PET Registry (NOPR) – https://www.cancerpetregistry.org – Source for statistics on how PET/CT alters patient treatment plans in 30-35% of oncologic cases.
- Society of Nuclear Medicine and Molecular Imaging (SNMMI) – https://www.snmmi.org – Authoritative guidelines on the use of 18F-FDG / Radiotracer and Positron Emission Tomography protocols.
- Journal of Clinical Oncology – https://ascopubs.org/journal/jco – Research supporting the efficacy of PET CT Scan Imaging in lung cancer and lymphoma staging.
- American College of Radiology (ACR) – https://www.acr.org – Official practice parameters for the performance of fused PET/CT imaging and SUV calculations.
- National Cancer Institute (NCI) – https://www.cancer.gov – Detailed scientific background on the Warburg Effect and the role of glucose metabolism in cancer detection.
- Prostate Cancer Foundation – https://www.pcf.org – Information regarding the impact of PSMA PET for prostate imaging on modern urological care.