You’ve just received your latest blood test results, and your doctor mentions something that sounds both vague and concerning. They might say your thyroid is “a little sluggish,” “on the low side,” or that you have borderline hypothyroidism. The key lab finding they point to is this: your TSH is high, but your T4 is normal. But what does this actually mean for your health, your energy levels, and your future?
- Your Thyroid 101: The Brain-Gland Connection
- The Diagnosis: How Doctors Identify Subclinical Hypothyroidism
- Symptoms and Prevalence: The "Silent" Condition
- The Great Debate: When to Treat Subclinical Hypothyroidism
- The #1 Cause in the US: Hashimoto's Disease
- Take Control with Proactive Monitoring
- Special Considerations: Pregnancy and Heart Health
- Conclusion: A Diagnosis of Nuance and Partnership
- Frequently Asked Questions (FAQ)
This common but frequently misunderstood diagnosis is called subclinical hypothyroidism. It’s the earliest, mildest form of an underactive thyroid, a silent warning sign that your body is working overtime to maintain a delicate hormonal balance. While it may not require immediate action, understanding this condition is the first step toward proactive health management.
This comprehensive guide will walk you through the subclinical hypothyroidism diagnosis criteria, what your lab numbers truly mean, what symptoms you should be aware of, and—most importantly—the nuanced, modern approach to treatment and management.
Your Thyroid 101: The Brain-Gland Connection
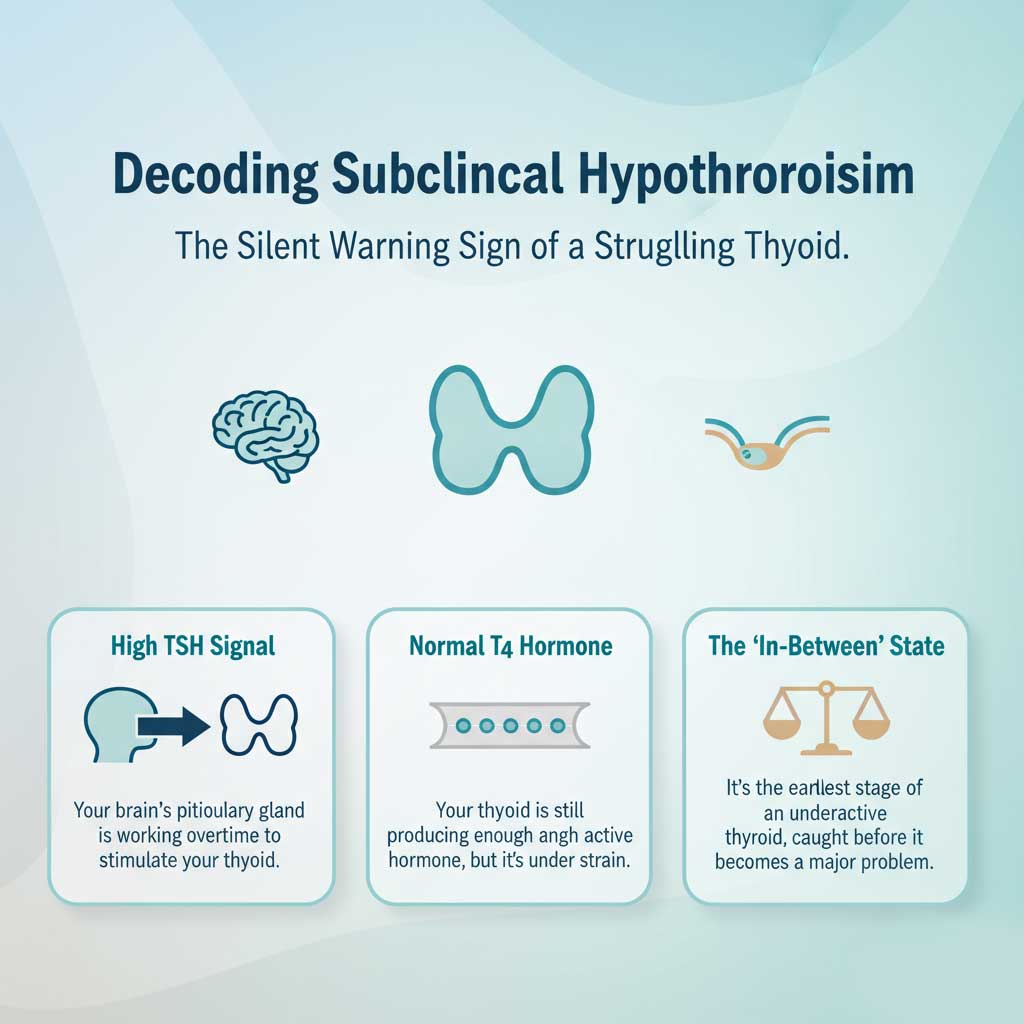
To understand subclinical hypothyroidism, you first need to understand the elegant partnership between your brain and your thyroid gland. Think of it like a smart thermostat system in your home, designed to keep your metabolism running at the perfect temperature.
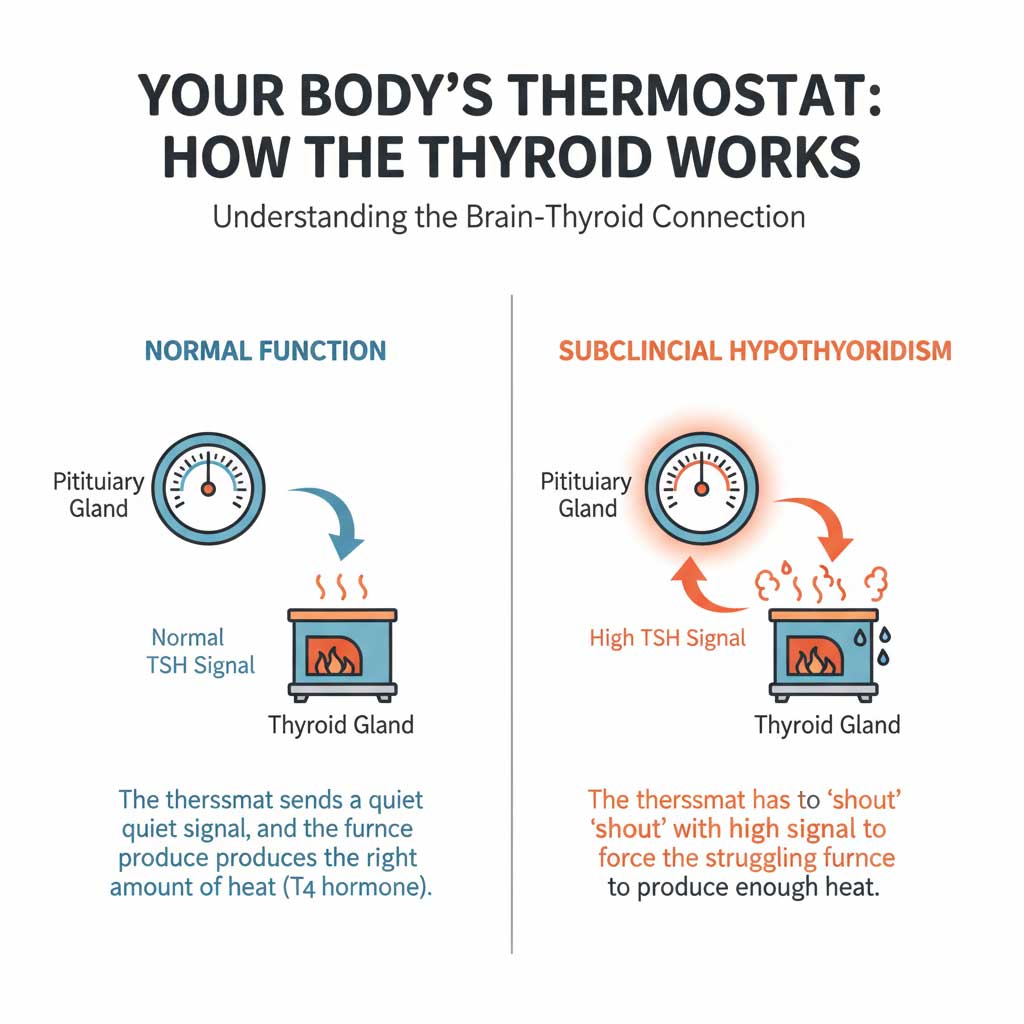
The Thermostat Analogy: A Delicate Balance
Your pituitary gland, located at the base of your brain, acts as the body’s master thermostat. Your thyroid gland, a butterfly-shaped gland in your neck, is the furnace, producing the hormones (like Thyroxine, or T4) that generate metabolic heat and energy for every cell in your body.
- Normal Function: The thermostat (pituitary) senses that the body is at the right temperature, so it sends a normal, quiet signal—called TSH (Thyroid-Stimulating Hormone)—to the furnace (thyroid). The thyroid responds by producing just the right amount of heat (T4 hormone), keeping everything in balance.
- Subclinical Hypothyroidism: The system senses the body is getting a little cold because the furnace (thyroid) is starting to struggle. To compensate, the thermostat (pituitary) has to shout, sending a loud, high TSH signal. Hearing this loud command, the struggling thyroid works extra hard and manages to produce just enough T4 to keep the body’s temperature normal—for now.
This scenario perfectly explains the core diagnostic finding of TSH high but T4 normal. It’s a clear sign that your body is successfully compensating for a failing thyroid, but it’s a state of strain that can’t last forever.
The Diagnosis: How Doctors Identify Subclinical Hypothyroidism
One of the most important things to know is that subclinical hypothyroidism is a condition defined entirely by laboratory results. It cannot and should not be diagnosed based on symptoms alone, as the symptoms are often mild, non-existent, or overlap with dozens of other conditions. The diagnosis hinges on specific patterns in your blood work.
The Gold Standard: Essential Thyroid Blood Tests
To get a clear picture of your thyroid health, your doctor will order two fundamental blood tests:
- TSH (Thyroid-Stimulating Hormone): This is the most sensitive test for detecting early thyroid issues. It measures the signal from the pituitary gland. A high TSH indicates the pituitary is working hard to stimulate a sluggish thyroid.
- Free T4 (Free Thyroxine): This test measures the amount of active thyroid hormone circulating in your blood that is available for your cells to use.
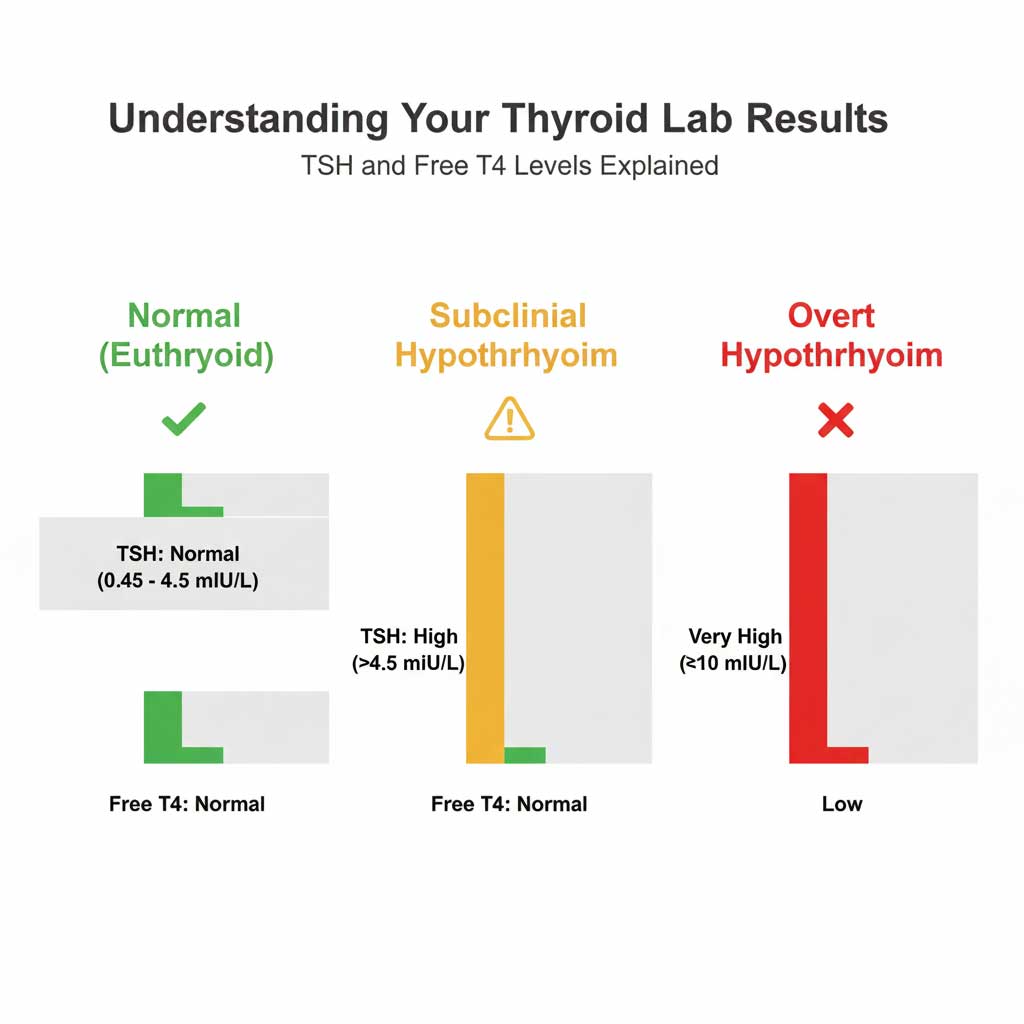
The relationship between these two values is what allows for a precise diagnosis. The subclinical hypothyroidism diagnosis criteria are met when the TSH is elevated while the Free T4 remains within the normal range.
| Thyroid Status | TSH (Thyroid-Stimulating Hormone) Level | Free T4 (Thyroxine) Level | What It Means |
| Normal (Euthyroid) | Typically 0.45 – 4.5 mIU/L | Within the lab’s normal range | The pituitary gland and thyroid gland are communicating perfectly. The body has the right amount of thyroid hormone. |
| Subclinical Hypothyroidism | Elevated (e.g., >4.5 mIU/L but <10 mIU/L) | Normal | The pituitary gland is overworking to stimulate the thyroid, which is still managing to produce enough T4. This is an early warning sign of thyroid failure. |
| Overt (Clinical) Hypothyroidism | Highly Elevated (e.g., >10 mIU/L) | Low | The thyroid gland can no longer produce enough T4, even with high levels of TSH stimulation from the pituitary. Medication is required. |
Understanding Your TSH Levels
So, what is a normal TSH range? For most labs in the U.S., the reference range is approximately 0.45 to 4.5 mIU/L. However, this range can vary slightly, and some experts argue for a narrower range, particularly for younger adults.
The specific subclinical hypothyroidism TSH levels are identified when a person’s TSH is persistently above this upper limit (e.g., 5.0, 7.0, or 9.0 mIU/L) across at least two tests, spaced a few weeks or months apart, while their Free T4 level remains normal.
The Next Diagnostic Step: Testing for TPO Antibodies
If your lab results show TSH high but T4 normal, a good clinician will often recommend a third test: Thyroid Peroxidase (TPO) Antibodies. This test doesn’t measure thyroid function itself, but rather looks for the cause of the dysfunction. A positive result is the hallmark of an autoimmune condition called Hashimoto’s disease, which is the leading cause of hypothyroidism in the United States.
Symptoms and Prevalence: The “Silent” Condition
One of the biggest challenges with identifying and managing subclinical hypothyroidism is its often-subtle presentation. Many people with the condition feel perfectly fine and have no idea their thyroid is struggling. When symptoms are present, they are often vague, easy to dismiss, or attribute to stress, aging, or a busy lifestyle.
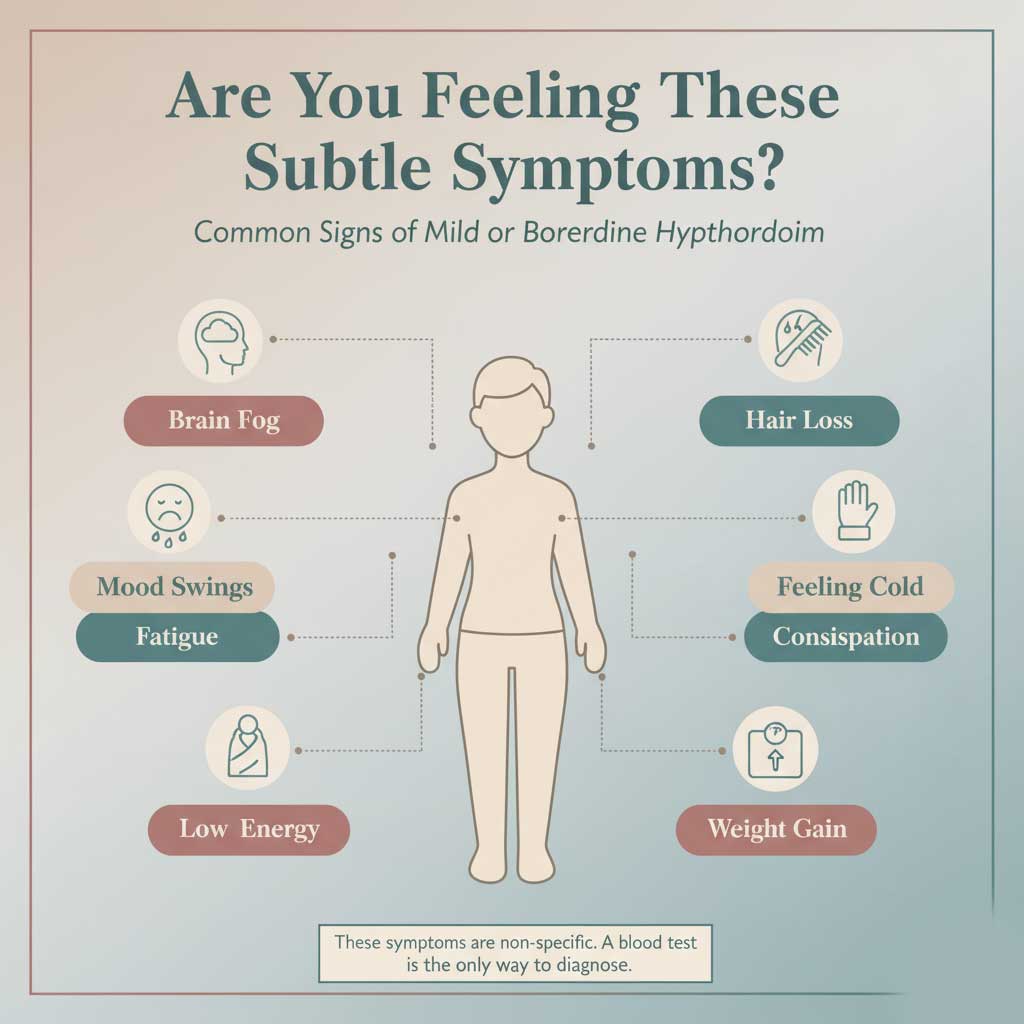
Are You Feeling It? The Vague Nature of Mild Thyroid Symptoms
If you do experience symptoms, they are typically milder versions of those seen in overt hypothyroidism. The most common mild hypothyroidism symptoms include:
- Persistent Fatigue: A feeling of being tired or sluggish that isn’t relieved by a good night’s sleep.
- Unexplained Weight Gain: Difficulty losing weight despite a healthy diet and exercise, or gaining a few pounds for no apparent reason. This is a very common concern related to subclinical hypothyroidism and weight gain.
- Increased Sensitivity to Cold: Feeling chilly when others are comfortable.
- Brain Fog: Difficulty with concentration, memory, or mental clarity.
- Constipation: A noticeable slowing of the digestive system.
- Physical Changes: Dry skin, brittle nails, and increased hair shedding or hair loss.
- Mood Changes: Mild depression, low mood, or a general lack of motivation.
It’s crucial to remember that having these symptoms does not mean you have a thyroid problem, but their presence in combination with elevated TSH levels strengthens the clinical picture.
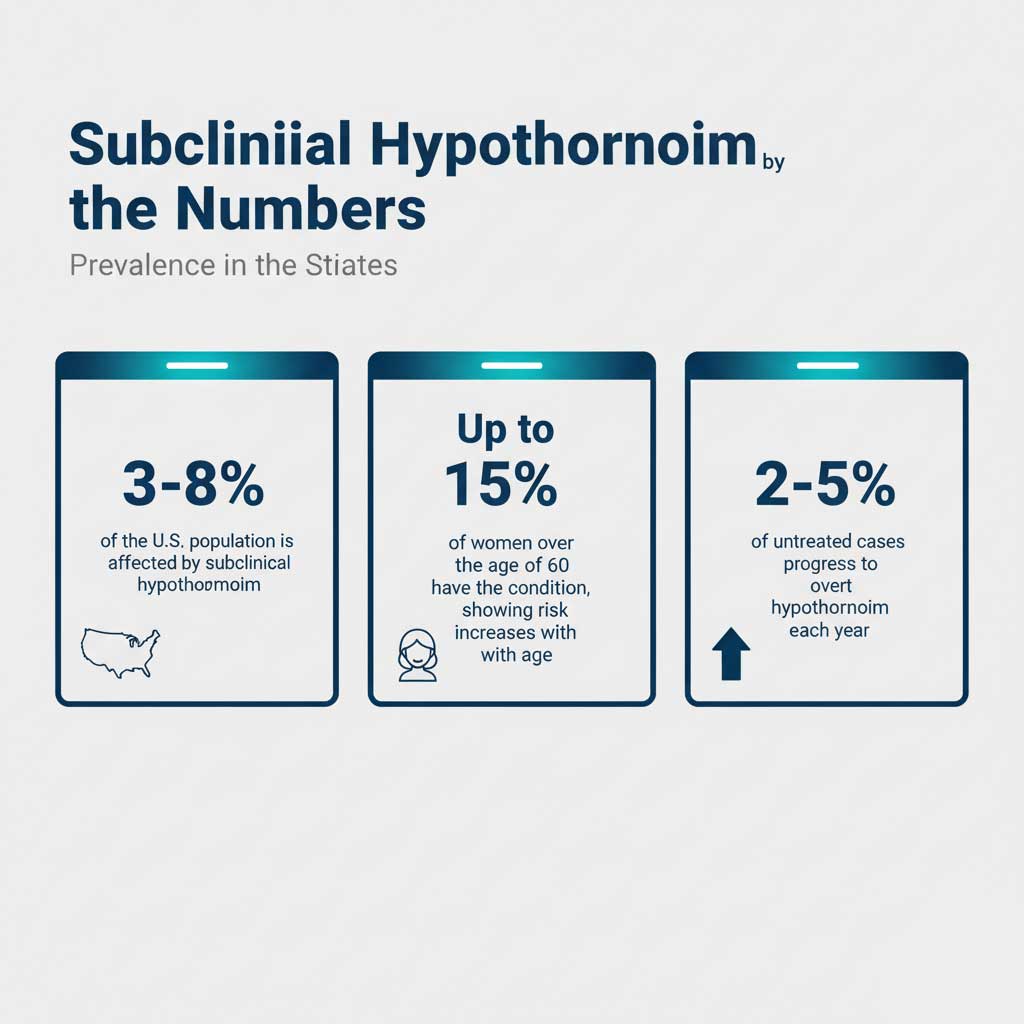
How Common Is Subclinical Hypothyroidism?
This isn’t a rare condition. In fact, it’s quite common, particularly as we age and among women.
- Real Data: Subclinical hypothyroidism affects an estimated 3-8% of the U.S. population. Its prevalence increases significantly with age, impacting up to 15% of women over the age of 60.
Because it is often asymptomatic, it’s frequently discovered incidentally during routine annual blood work—a strong case for proactive health screening.
The Great Debate: When to Treat Subclinical Hypothyroidism
This is where the conversation becomes nuanced and where a partnership with a knowledgeable healthcare provider is essential. The decision of when to treat subclinical hypothyroidism is not black and white. Unlike overt hypothyroidism, where medication is always required, the approach to this mild form is highly individualized.
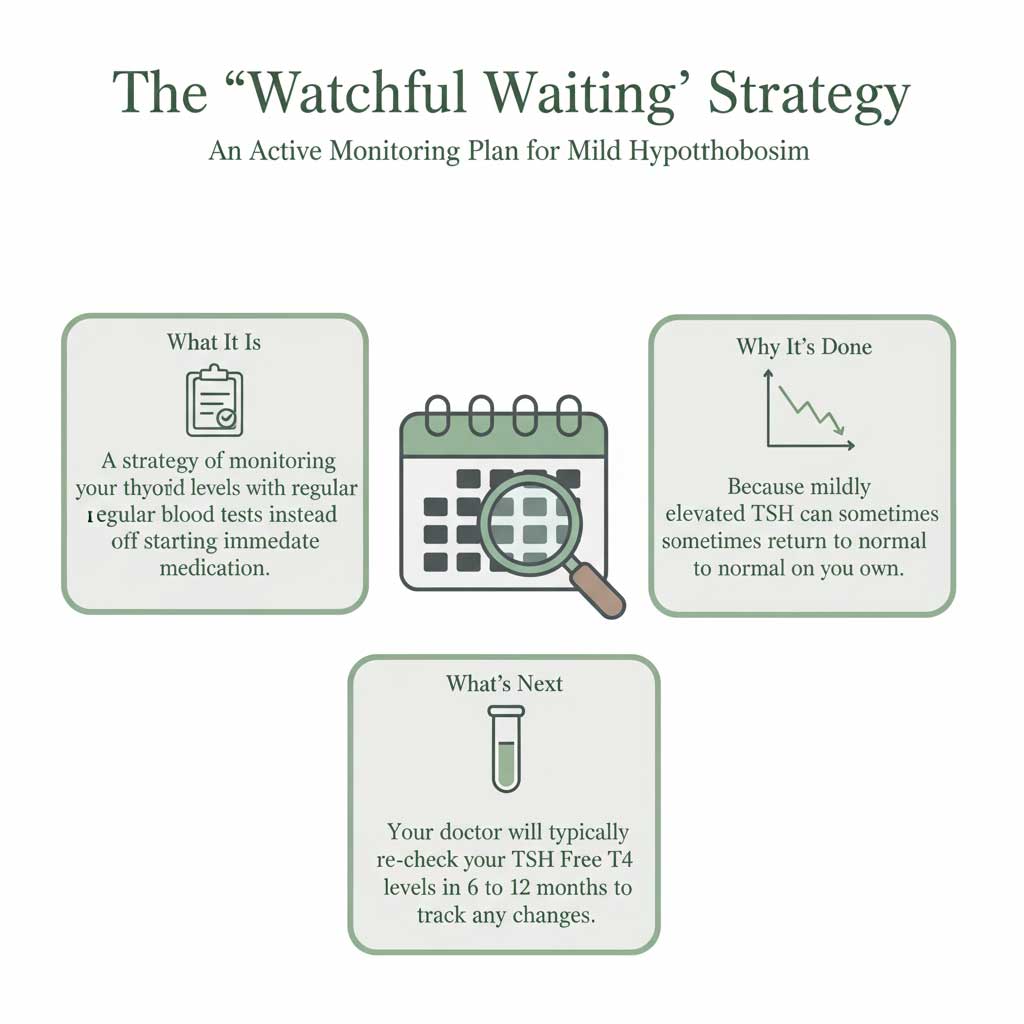
Approach 1: The “Watchful Waiting” Strategy
For many individuals, particularly older adults with a TSH level below 10 mIU/L and no symptoms, the recommended approach is often watchful waiting for hypothyroidism.
What does “watchful waiting” involve?
This strategy means you won’t be prescribed medication immediately. Instead, your doctor will recommend monitoring your thyroid function with repeat blood tests every 6 to 12 months.
Why is this approach used?
- Potential for Normalization: In a significant number of cases, a mildly elevated TSH can be transient and may return to the normal range on its own without any intervention.
- Lack of Symptom Improvement: Large-scale clinical trials have shown that for patients with a TSH below 10, the treatment for subclinical hypothyroidism with medication often does not lead to a noticeable improvement in non-specific symptoms like fatigue or weight management. The risks and costs of lifelong medication may outweigh the potential benefits.
Approach 2: Starting Medication (Levothyroxine)
The standard medication used for thyroid hormone replacement is levothyroxine for subclinical hypothyroidism (common brand names include Synthroid, Levoxyl, and Tirosint). It is a synthetic version of the T4 hormone that your own thyroid produces.
The Deciding Factors: A Personalized Treatment Plan
So, who is a candidate for medication? The decision to begin treatment for subclinical hypothyroidism is based on a careful evaluation of your entire clinical picture.
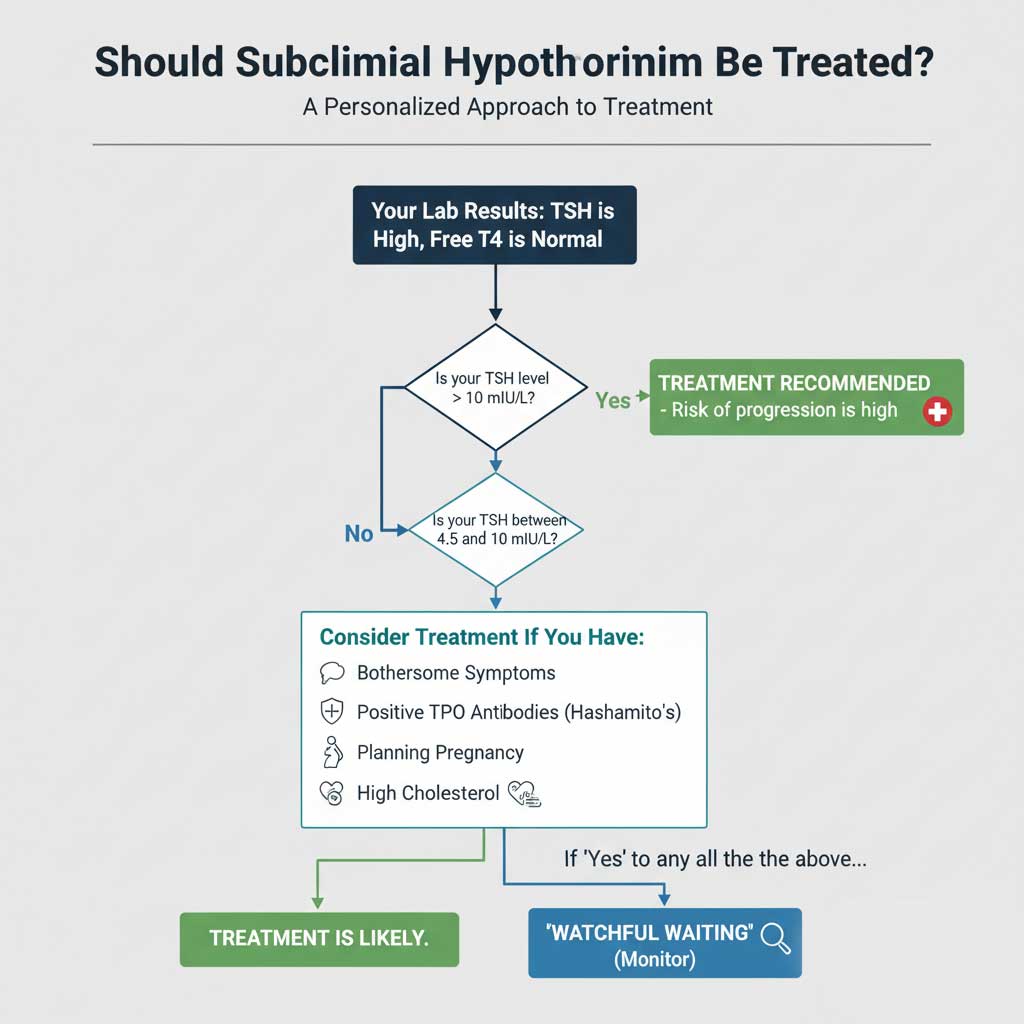
TSH Level > 10 mIU/L
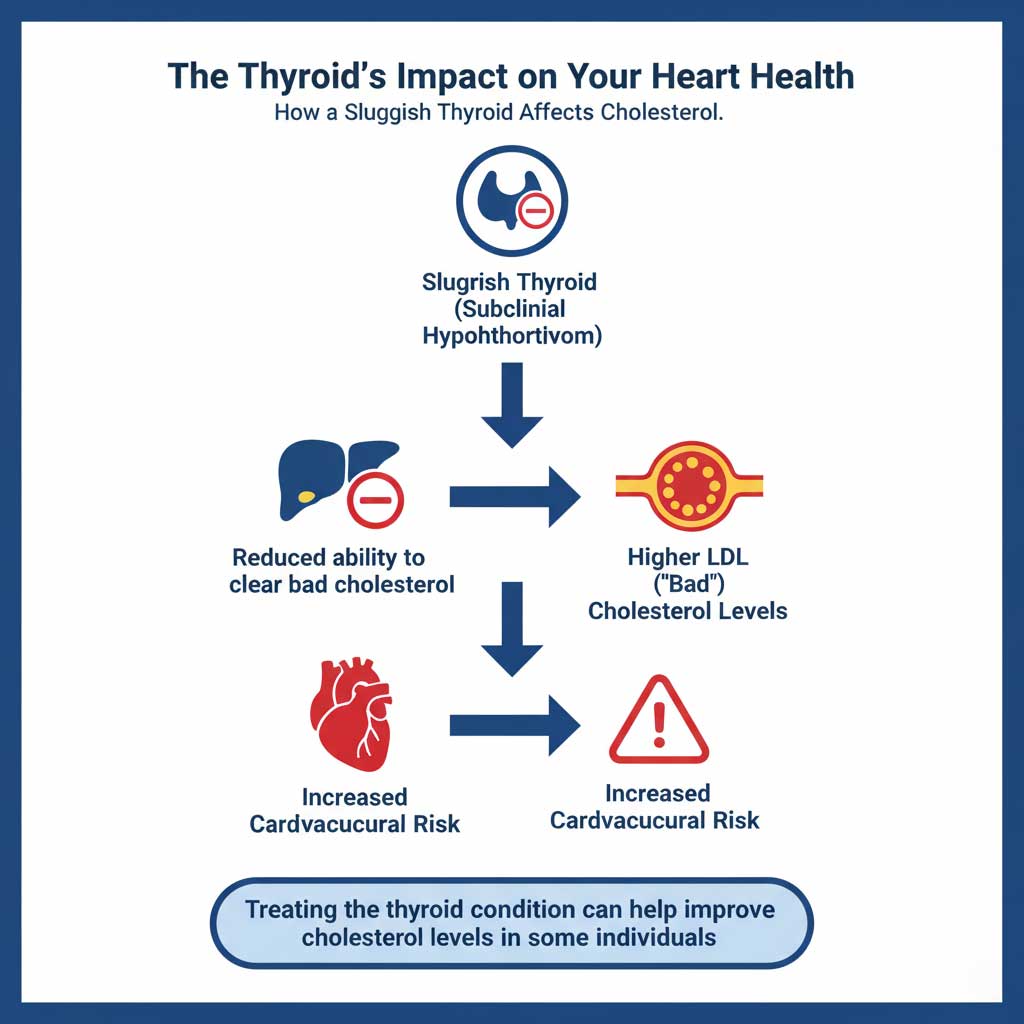
If your TSH is persistently above 10 mIU/L, even if your T4 is still normal, most medical guidelines recommend starting treatment. At this level, the risk of progressing to overt hypothyroidism is very high, and there is a greater chance of developing associated health issues like high cholesterol.
TSH Level Between 4.5 – 10 mIU/L
This is the “gray area” where personalization is key. Your doctor will strongly consider treatment if you have subclinical hypothyroidism TSH levels in this range AND one or more of the following factors:
- You Have Clear Symptoms: If you are experiencing bothersome mild hypothyroidism symptoms like significant fatigue or brain fog, a trial of medication may be offered to see if your symptoms improve.
- You Have Positive TPO Antibodies: A positive TPO test indicates an active autoimmune process (Hashimoto’s and subclinical hypothyroidism). These individuals are far more likely to progress to overt hypothyroidism, and many clinicians will treat them earlier to prevent this.
- You Are Pregnant or Trying to Conceive: This is a non-negotiable reason for treatment. Subclinical hypothyroidism and pregnancy requires immediate attention, as normal maternal thyroid levels are absolutely critical for the baby’s brain development.
- You Have High Cholesterol: There is a well-established link between subclinical hypothyroidism and cholesterol. Even mild thyroid failure can impair the body’s ability to clear LDL (“bad”) cholesterol. Treating the thyroid can help improve lipid levels.
- You Are Younger: Clinicians are more likely to treat a younger person (e.g., under 65) with a persistently elevated TSH, as they have a longer lifetime risk of progression and developing complications.
The #1 Cause in the US: Hashimoto’s Disease
To fully understand your diagnosis, it’s essential to understand its most common cause. In the United States and other parts of the world with sufficient iodine intake, the overwhelming cause of subclinical hypothyroidism is Hashimoto’s disease.
Unmasking the Culprit Behind Your High TSH
Hashimoto’s disease is not a problem with your thyroid gland itself; it’s a problem with your immune system. It is an autoimmune condition where the immune system mistakenly identifies the thyroid gland as a foreign invader and creates antibodies—specifically TPO antibodies—to attack and gradually destroy it.
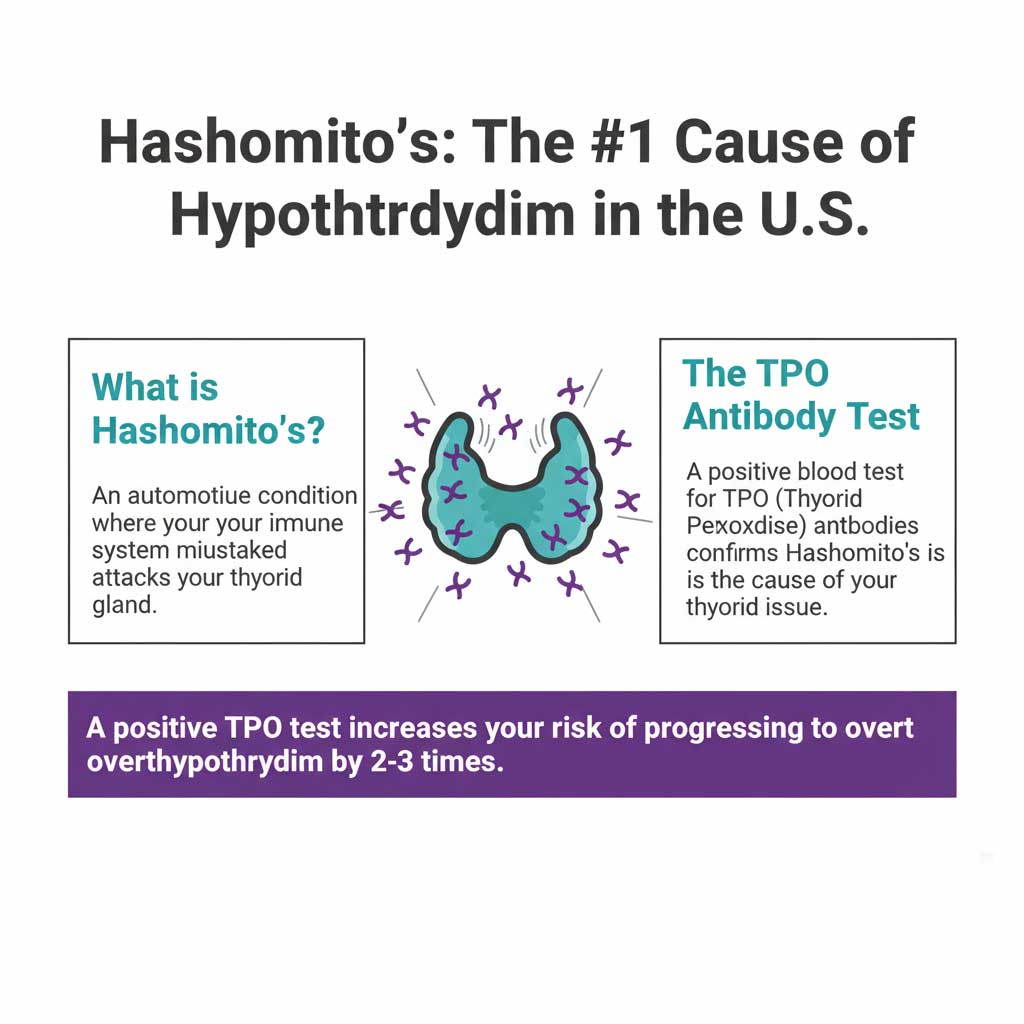
This slow, progressive destruction is why thyroid function declines over time. The TSH high but T4 normal lab result often represents a snapshot in time where the gland is damaged but not yet completely failed. A positive TPO antibody test essentially confirms a diagnosis of Hashimoto’s and subclinical hypothyroidism.
Understanding Your Progression Risk
Knowing your TPO antibody status is critical because it helps predict the future of your thyroid health.
- Real Data: The presence of TPO antibodies significantly increases the chance of progressing from subclinical hypothyroidism to overt hypothyroidism. Studies show the annual progression rate is around 4-5% in TPO-positive individuals, compared to just 2% in those who are TPO-negative.
Take Control with Proactive Monitoring
Whether you and your doctor decide on a watchful waiting for hypothyroidism plan or begin treatment, one thing is certain: regular, reliable blood testing is the cornerstone of managing your thyroid health. This is where you can take an active role.
Your Partner in Thyroid Health Management
At HealthCareOnTime.com, we believe that managing your health should be simple, accessible, and convenient. We remove the barriers to essential diagnostic testing, putting you in control.
The Thyroid Monitoring Panel
Our comprehensive Thyroid Monitoring Panel is the perfect tool for managing your condition. It includes all three key tests: TSH, Free T4, and TPO Antibodies. This panel gives you and your doctor the complete picture needed for the “watchful waiting” approach or for ensuring your medication dosage is perfectly optimized. You can book your test today with no doctor’s visit required.
Annual Wellness Test
Our Annual Wellness Test includes a baseline thyroid screen (TSH), making it an excellent way to catch potential issues like borderline hypothyroidism before they become more serious. Early detection is key.
Consult an Expert
Navigating a new diagnosis can be overwhelming. If you have questions about your results or want a second opinion on your treatment plan, we can help connect you with an endocrinologist for thyroid issues to discuss your next steps with confidence.
Special Considerations: Pregnancy and Heart Health
While subclinical hypothyroidism can affect anyone, there are certain situations where it requires more immediate and aggressive attention due to its potential impact on other aspects of health.
Subclinical Hypothyroidism and Pregnancy
During pregnancy, the baby is completely dependent on the mother’s thyroid hormone for the first trimester for its own brain and nervous system development. For this reason, the standards for thyroid health are much stricter. Medical guidelines from the American Thyroid Association strongly recommend treating subclinical hypothyroidism and pregnancy to reduce the risks of miscarriage, pre-term birth, and potential long-term neurodevelopmental issues in the child.
The Link to High Cholesterol and Heart Health
Your thyroid hormones play a vital role in regulating your metabolism, including how your body processes and clears fats from the blood. The connection between subclinical hypothyroidism and cholesterol is well-documented. Even this mild form of thyroid dysfunction can lead to elevated levels of LDL (“bad”) cholesterol and triglycerides, which are known risk factors for heart disease. For some patients, starting levothyroxine for subclinical hypothyroidism can be an effective tool for improving their lipid profile and protecting their cardiovascular health.
Conclusion: A Diagnosis of Nuance and Partnership
Receiving a diagnosis of subclinical hypothyroidism can feel confusing, but it doesn’t have to be frightening. Think of it not as an illness, but as a crucial health signal—an early warning that allows you to be proactive.
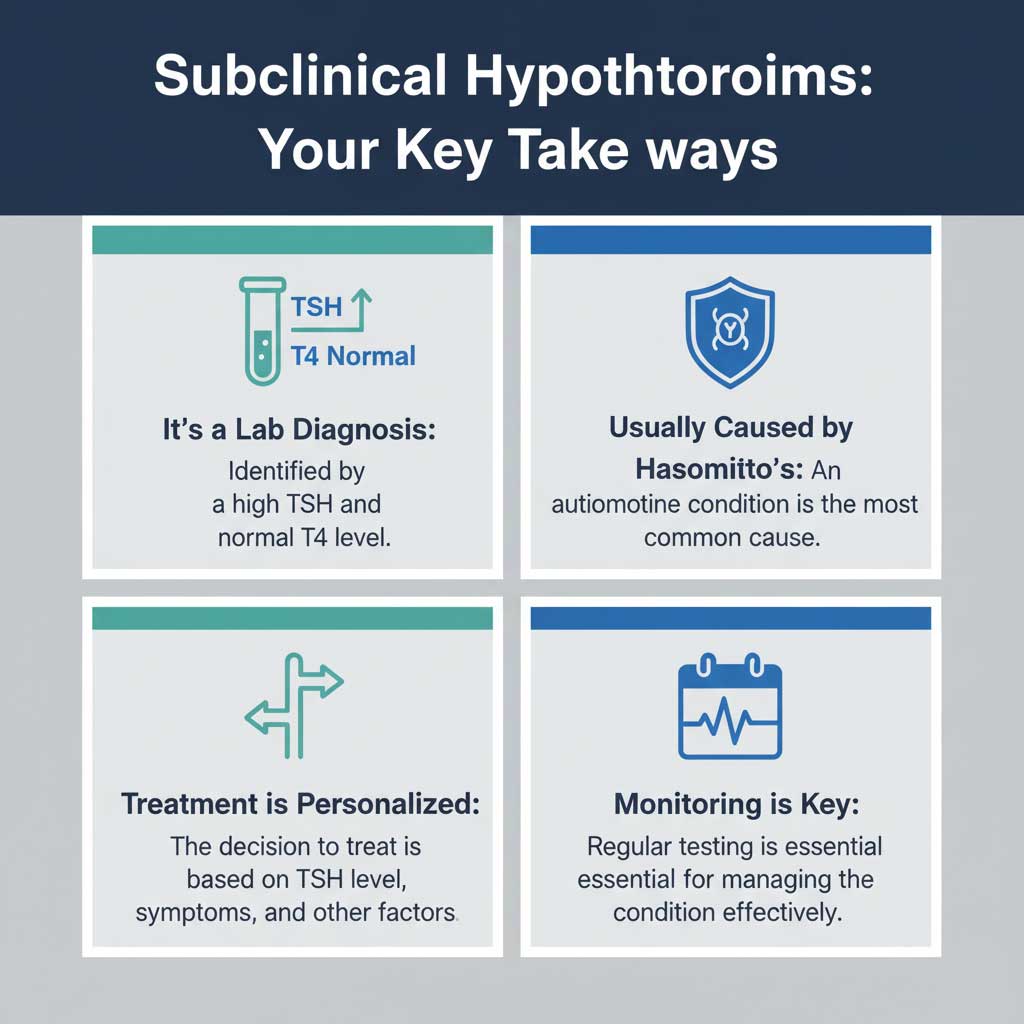
The key takeaways are clear: this is a laboratory diagnosis defined by the pattern of TSH high but T4 normal, and it’s most often caused by the autoimmune condition Hashimoto’s disease. The decision to treat is not automatic; it is a highly individualized choice based on your specific subclinical hypothyroidism TSH levels, symptoms, antibody status, and overall health goals.
This is a diagnosis of nuance, one that requires careful monitoring and, most importantly, a collaborative partnership with your healthcare provider. By understanding your lab results and playing an active role in your health, you can make informed decisions that will protect your well-being for years to come.