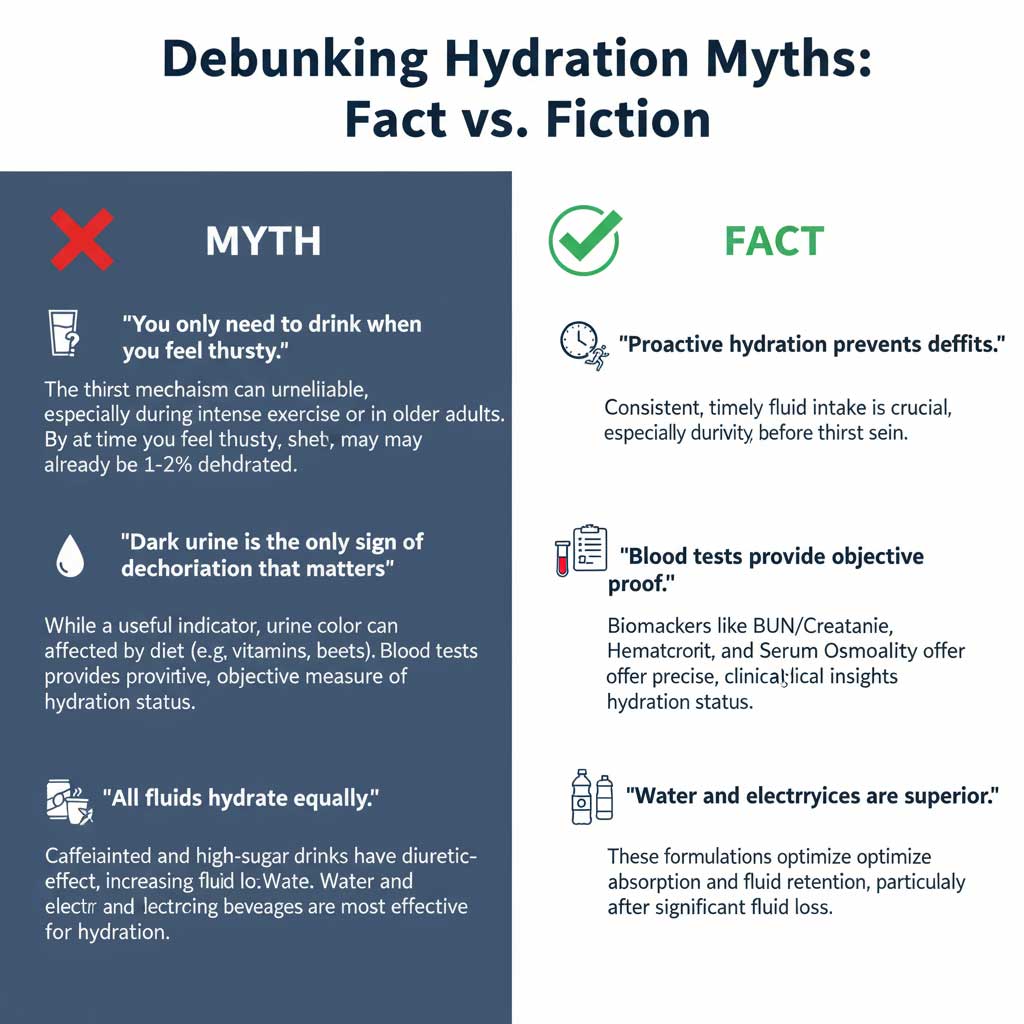
Feeling sluggish after a hot day, battling fatigue during a workout, or caring for a sick loved one? These common scenarios often have one culprit in common: dehydration. While thirst and dark urine are the body’s initial warning signals, they can be surprisingly unreliable, especially in older adults or during intense physical activity. Severe dehydration can set in long before you realize the true extent of the problem.
- Understanding Dehydration: How It Affects Your Body and Your Blood
- The 5 Key Dehydration Markers in Your Blood Test
- At-a-Glance: Your Guide to Dehydration Lab Results
- When to See a Doctor About Dehydration
- Getting Tested and Taking Control of Your Health
- Beyond the Blood Test: Prevention and Rehydration Strategies
- Conclusion: Your Blood Tells a Story
- Frequently Asked Questions (FAQ)
Fortunately, there is a definitive, scientific way to understand your body’s fluid status. The key lies within your blood, and knowing what lab values show dehydration is crucial for your health.
A simple blood test can pull back the curtain on your internal hydration levels, offering clear data that goes beyond symptoms. This article will serve as your comprehensive guide to the dehydration markers in a blood test. We will demystify the five key markers that doctors look for—Sodium, Blood Urea Nitrogen (BUN), Hematocrit, the BUN-to-Creatinine Ratio, and Serum Osmolality—to provide a complete picture of your hydration and overall well-being.
Understanding Dehydration: How It Affects Your Body and Your Blood
At its core, dehydration is a simple imbalance: your body is losing more fluid than it is taking in. This deficit prevents your organs and cells from performing their essential functions correctly. Every system in your body, from your brain to your kidneys, relies on a delicate balance of water and electrolytes to operate.
Common Causes of Dehydration
Dehydration isn’t just about not drinking enough water on a hot day. It can be triggered by a wide range of situations, including:
- Insufficient Fluid Intake: Simply not drinking enough water or other hydrating fluids throughout the day.
- Excessive Sweating: Intense exercise, high heat, or a fever can lead to significant fluid loss.
- Illness: Conditions involving vomiting, diarrhea, or fever rapidly deplete the body’s fluid and electrolyte stores.
- Increased Urination: Certain medications (like diuretics), uncontrolled diabetes, or high caffeine intake can cause you to lose more fluid.
The Impact on Your Blood
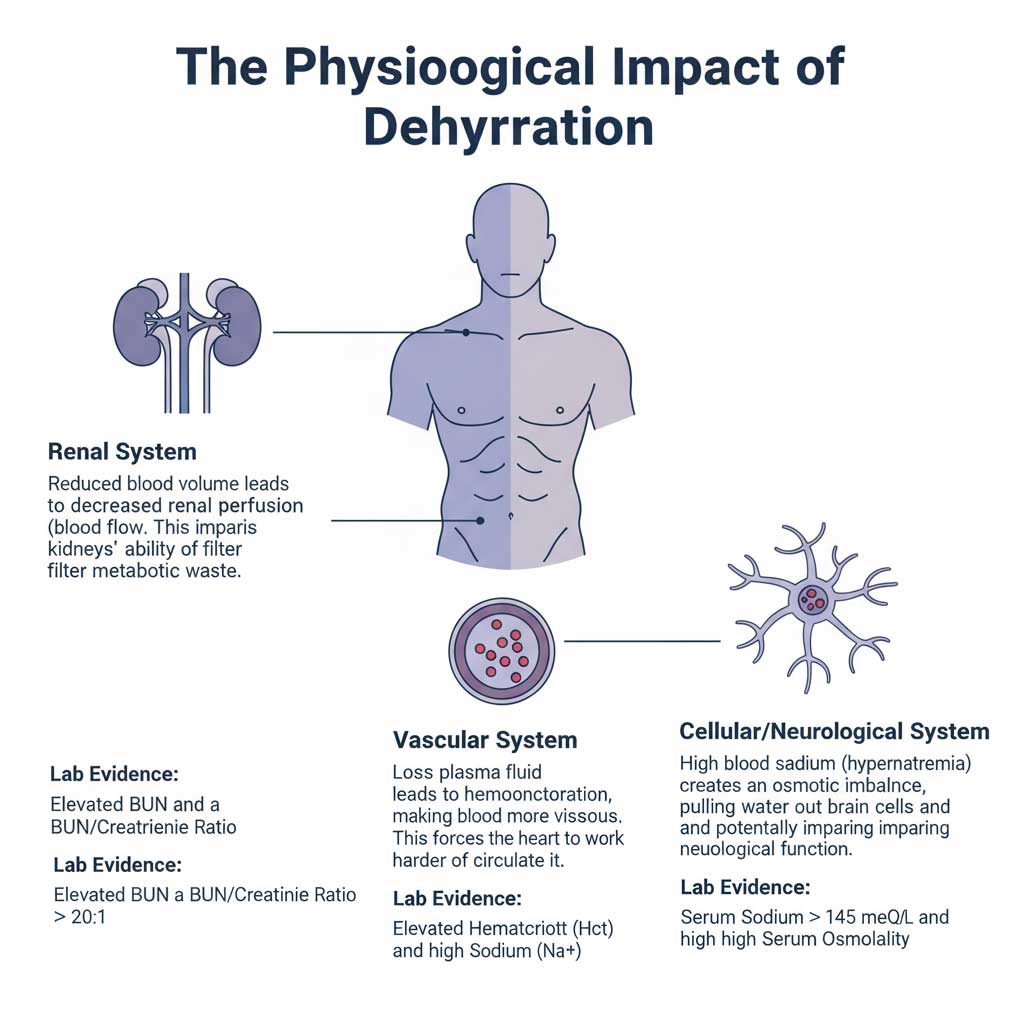
So, how does this fluid loss show up in your blood? Think of your bloodstream as a river. When the water level (plasma) drops, everything else in the river—the boats, the fish, the sediment (your blood cells, electrolytes, and waste products)—becomes more concentrated. This principle is precisely why a blood test is so effective at diagnosing dehydration. The signs of dehydration in a blood test are essentially signs of this increased concentration.
What Blood Test Indicates Dehydration?
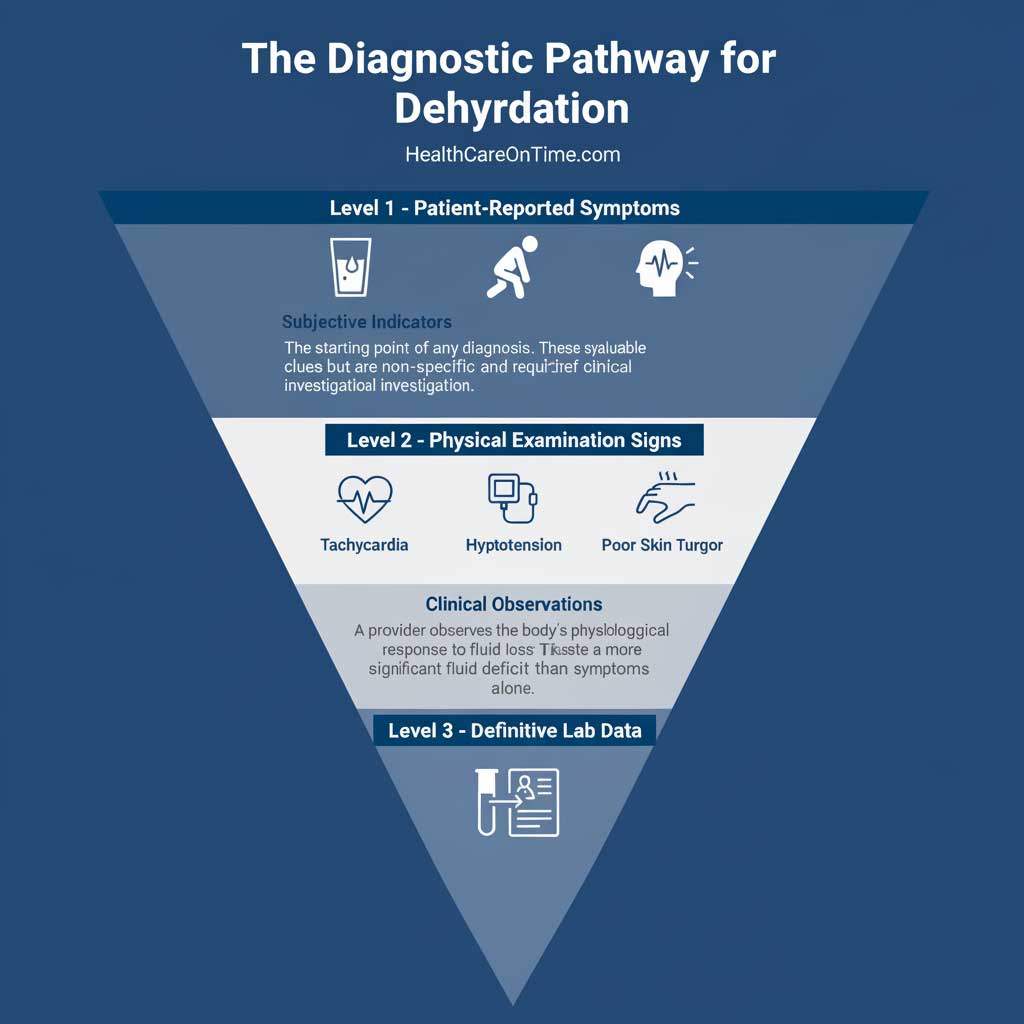
Doctors don’t use a single, specific “dehydration test.” Instead, they look for clues within two standard blood panels that provide a wealth of information about your health. Understanding what blood test indicates dehydration involves looking at these two key reports:
- Comprehensive Metabolic Panel (CMP): This broad test is a cornerstone for assessing your body’s overall function. For dehydration, it’s invaluable because it measures your electrolyte levels (like sodium and potassium), kidney function (BUN and creatinine), and blood sugar, all of which are affected by your hydration status.
- Complete Blood Count (CBC): This test analyzes the different components of your blood, including red blood cells, white blood cells, and platelets. When it comes to dehydration, the most important value on a CBC is your hematocrit, which measures the concentration of red blood cells.
By examining the dehydration lab results from these two panels, a healthcare provider can accurately diagnose dehydration and determine its severity.
The 5 Key Dehydration Markers in Your Blood Test
When your doctor reviews your blood work, they are looking for specific values that have shifted outside the normal range. These shifts are the lab results indicating dehydration. Let’s explore each of the five critical markers in detail to understand the story they tell about your body’s hydration.
1. Sodium (Na+): The Electrolyte Red Flag
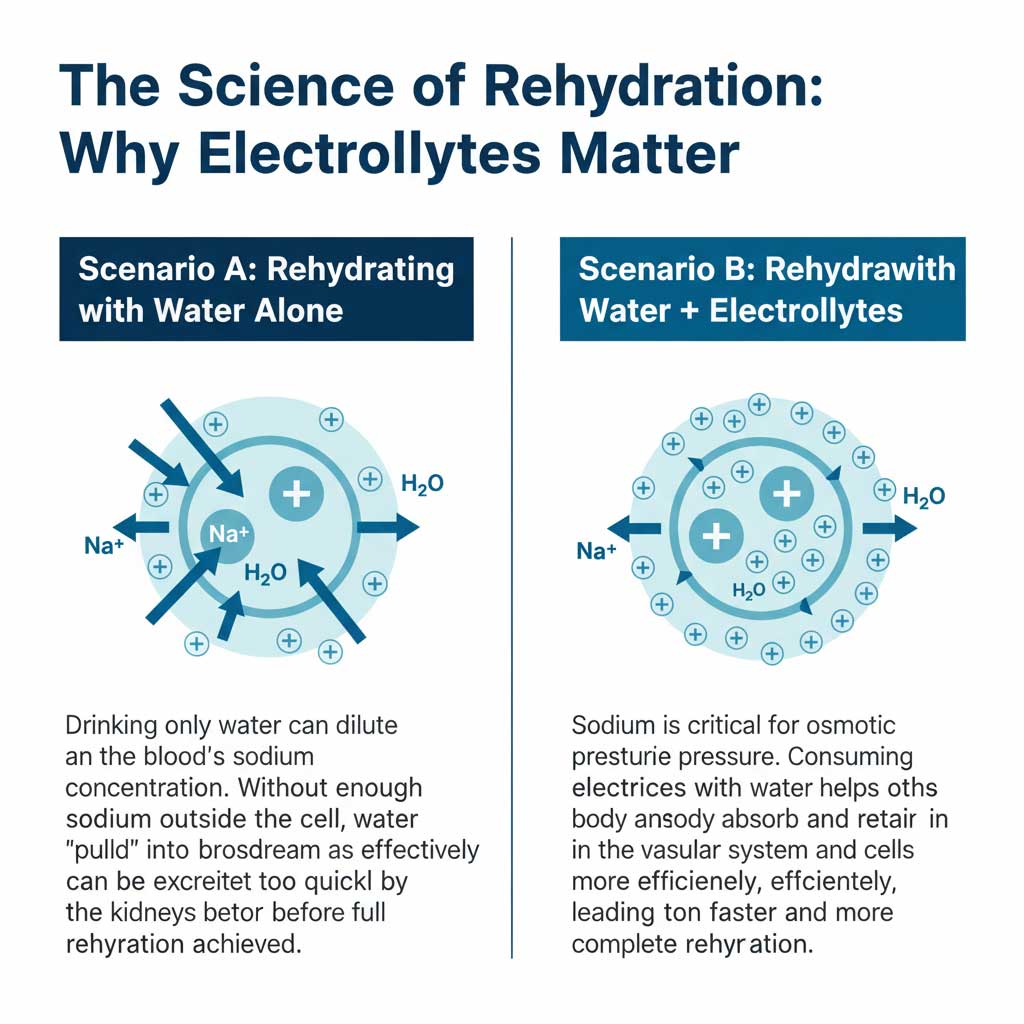
Sodium is far more than just a component of table salt; it’s a critical electrolyte that acts like a magnet for water, helping to maintain the right amount of fluid both inside and outside your body’s cells. Your body works tirelessly to keep sodium levels in a very narrow, stable range.
Why Sodium Rises in Dehydration
When you lose water but not an equivalent amount of sodium—a common scenario with sweating or inadequate water intake—the sodium left behind in your bloodstream becomes more concentrated. This condition is known as hypernatremia. It’s one of the most direct signs of dehydration in a blood test. Your brain detects this high concentration and triggers the sensation of thirst, compelling you to drink and restore balance.
Interpreting Your Sodium Levels
- Real Data: A normal sodium level in the blood is typically between 135 and 145 milliequivalents per liter (mEq/L).
- Dehydration Indicator: Sodium levels and dehydration are closely linked. A result above 145 mEq/L is a clear indicator of hypernatremia and often points directly to dehydration. Levels rising above 155 mEq/L can become medically serious, potentially leading to confusion, seizures, or worse if left untreated.
2. Blood Urea Nitrogen (BUN): A Sign of Stressed Kidneys
Your kidneys are your body’s master filtration system. Blood Urea Nitrogen, or BUN, is a waste product that forms when your liver breaks down proteins. In a well-hydrated state, your kidneys efficiently filter this waste from your blood and excrete it through urine.
Why BUN Rises in Dehydration
When you’re dehydrated, your overall blood volume decreases. This means less blood flows to your kidneys per minute, a condition known as “prerenal azotemia.” This reduced blood flow makes the kidneys’ job much harder. They can’t filter waste as effectively, causing urea to accumulate in the bloodstream instead of being flushed out. This is why high BUN and dehydration are so strongly connected.
Interpreting Your BUN Levels
- Real Data: A normal BUN range is generally between 7 and 20 milligrams per deciliter (mg/dL).
- Dehydration Indicator: In cases of dehydration, it’s common to see BUN levels climb above 20 mg/dL. While high BUN and dehydration are a classic pairing, it’s important to note that other conditions, like kidney disease, a very high-protein diet, or certain medications, can also elevate BUN. This is why doctors look at it in conjunction with other markers.
3. Hematocrit (Hct): Measuring Blood Concentration
A Complete Blood Count (CBC) provides many insights, but for hydration, the key value is hematocrit. Hematocrit measures the percentage of your blood volume that is composed of red blood cells.
Why Hematocrit Rises in Dehydration
The easiest way to understand this is with an analogy. Imagine a glass filled with water and marbles. The marbles are your red blood cells, and the water is your plasma. If you pour out half the water, the total volume in the glass decreases, but the number of marbles stays the same. As a result, the percentage of the glass’s volume taken up by marbles becomes much higher.
This is exactly what happens in your bloodstream during dehydration. The liquid portion of your blood (plasma) decreases, making the red blood cells more concentrated. This is why elevated hematocrit and dehydration are frequently seen together in dehydration lab results.
Interpreting Your Hematocrit Levels
- Real Data: Normal hematocrit ranges vary by sex. For men, it’s typically 38.3% to 48.6%. For women, it’s 35.5% to 44.9%.
- Dehydration Indicator: A value that is elevated above your normal baseline can be one of the key lab results indicating dehydration. One of the telling signs is that this value will typically return to its normal range once you are properly rehydrated. It’s crucial to differentiate this temporary elevation from chronic conditions like polycythemia vera, where the body genuinely overproduces red blood cells.
4. The BUN-to-Creatinine Ratio: The Most Revealing Indicator
While looking at BUN alone is helpful, comparing it to another kidney waste product, creatinine, provides an even clearer picture. Creatinine is a waste product from muscle metabolism that is filtered by the kidneys at a relatively steady rate. The BUN-to-creatinine ratio in dehydration is one of the most powerful diagnostic tools a doctor has.
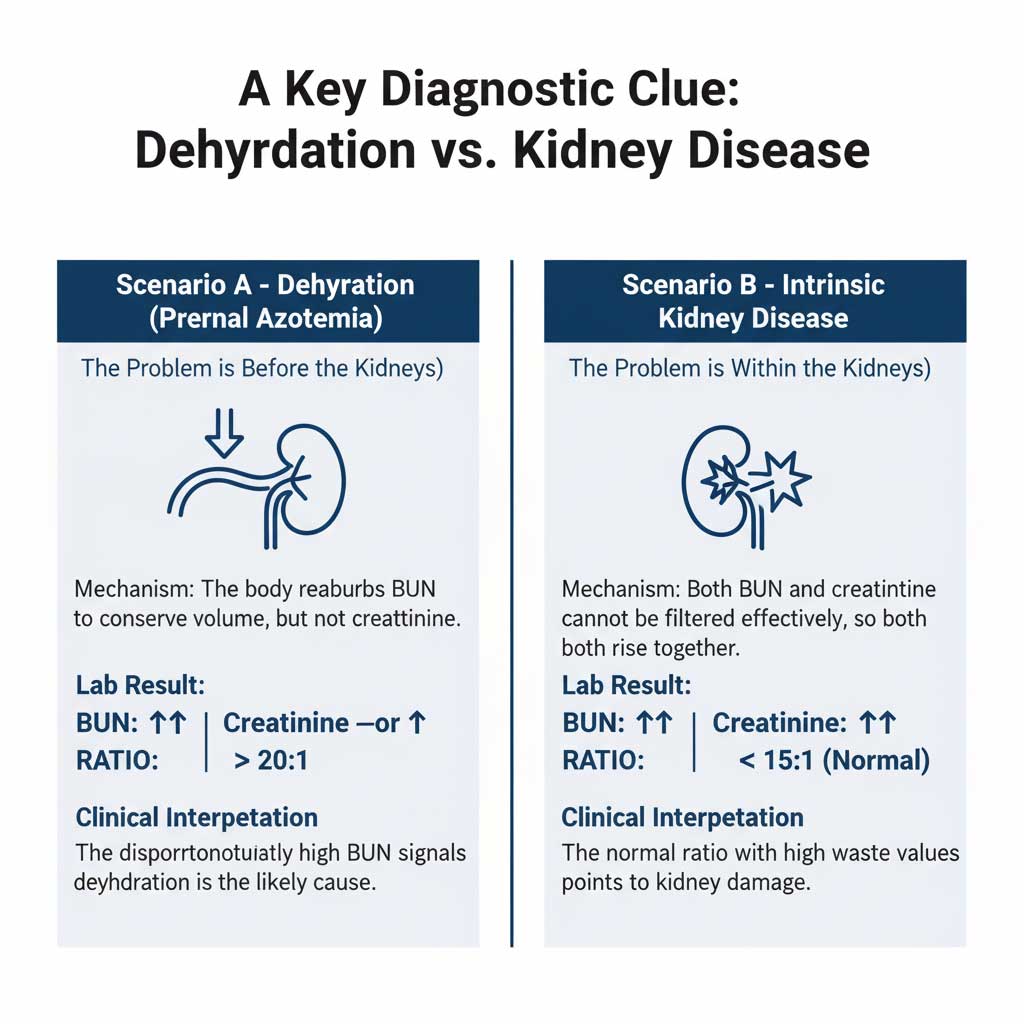
Why the Ratio is So Significant
Here’s the key difference: When your body senses dehydration, it goes into water-conservation mode. Your kidneys start reabsorbing water and urea (BUN) back into the bloodstream to maintain blood pressure. However, they do not reabsorb creatinine.
This leads to a situation where BUN levels in the blood rise significantly, while creatinine levels may only rise slightly or stay the same. The result is a skewed, or high, BUN-to-creatinine ratio. This specific pattern is a hallmark of dehydration-related kidney stress.
Interpreting Your BUN-to-Creatinine Ratio
- Real Data: A normal ratio is typically between 10:1 and 20:1.
- Dehydration Indicator: A ratio greater than 20:1 is a strong sign that the cause of the high BUN is “prerenal” (meaning, “before the kidney”), pointing directly to issues like dehydration rather than intrinsic kidney disease. Understanding the BUN to creatinine ratio in dehydration is vital for accurate diagnosis.
5. Serum Osmolality: The Gold Standard for Diagnosis
While the other four markers are excellent clues, serum osmolality is considered by many clinicians to be the gold standard for assessing hydration status. This test provides the most direct measurement of your blood’s concentration. It measures the total number of all dissolved particles (solutes like sodium, glucose, and urea) per kilogram of your blood’s fluid component.
Why Serum Osmolality is So Accurate
Unlike other markers that can be influenced by diet or other conditions, serum osmolality offers a direct, unambiguous look at the water-to-solute balance in your blood. When you lose water, the concentration of these solutes naturally increases, and this test captures that change with high precision. The link between serum osmolality and dehydration is direct and scientifically robust.
Interpreting Your Serum Osmolality Levels
- Real Data: A normal serum osmolality range is 275 to 295 milliosmoles per kilogram (mOsm/kg).
- Dehydration Indicator: A value greater than 300 mOsm/kg is a definitive diagnostic marker of dehydration. This result provides conclusive evidence that confirms the story told by the other dehydration markers in a blood test.
At-a-Glance: Your Guide to Dehydration Lab Results
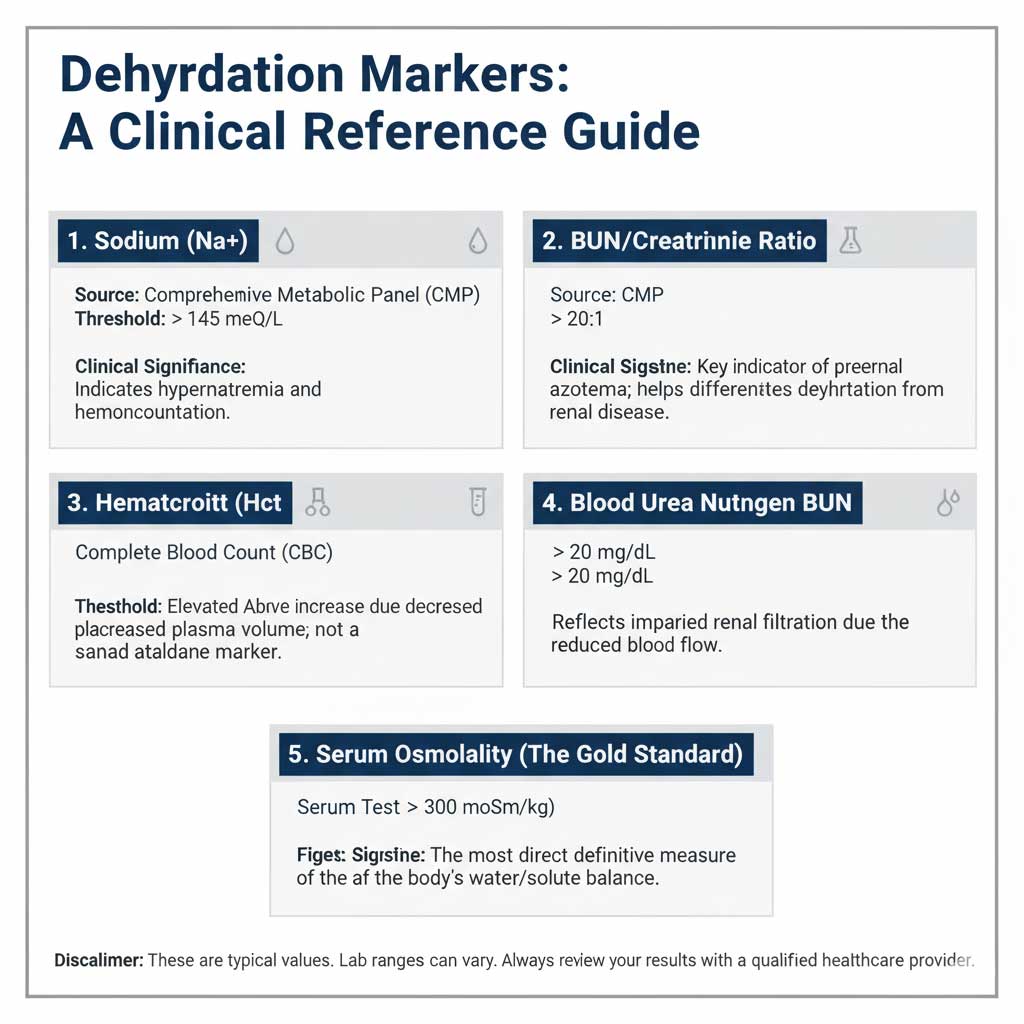
To help you quickly reference and understand these markers, here is a summary of what lab values show dehydration. This table breaks down each marker, its normal range, and what its value means for your hydration.
| Blood Test Marker | What It Measures | Normal Range (Typical) | Lab Value Indicating Dehydration | Why It Changes with Dehydration |
| Sodium (Na+) | Concentration of sodium in the blood. | 135-145 mEq/L | > 145 mEq/L (Hypernatremia) | Water is lost, but sodium is left behind, increasing its concentration in the remaining blood volume. |
| Blood Urea Nitrogen (BUN) | Waste product from protein metabolism, cleared by kidneys. | 7-20 mg/dL | > 20 mg/dL | Reduced blood flow to the kidneys (due to low fluid volume) impairs their ability to filter and excrete BUN. |
| Hematocrit (Hct) | The percentage of red blood cells in total blood volume. | Men: 38.3-48.6%<br>Women: 35.5-44.9% | Elevated above normal range | The volume of blood plasma (the liquid part) decreases, making the proportion of red blood cells appear higher. |
| BUN-to-Creatinine Ratio | The ratio of two kidney waste products. | 10:1 to 20:1 | > 20:1 | The body reabsorbs urea (BUN) to conserve water, but not creatinine. This causes BUN to rise disproportionately. |
| Serum Osmolality | Total concentration of all solutes in the blood. | 275-295 mOsm/kg | > 300 mOsm/kg | This is the most direct measurement of blood concentration. Higher osmolality means less water relative to solutes. |
When to See a Doctor About Dehydration
While mild dehydration can often be managed at home, moderate to severe dehydration is a medical emergency that requires immediate attention. It’s crucial to recognize the symptoms that signal it’s time to seek professional help.
Contact a doctor or go to an urgent care center if you or someone else experiences:
- Cognitive Changes: Dizziness, confusion, fainting, or extreme lethargy.
- Inability to Rehydrate: Persistent vomiting or being unable to keep any fluids down.
- Kidney Distress: A lack of urination for more than eight hours, or very dark, concentrated urine.
- Cardiovascular Symptoms: A rapid or weak pulse, or a racing heartbeat.
- Physical Signs: Sunken eyes or skin that doesn’t bounce back when lightly pinched (known as poor skin turgor).
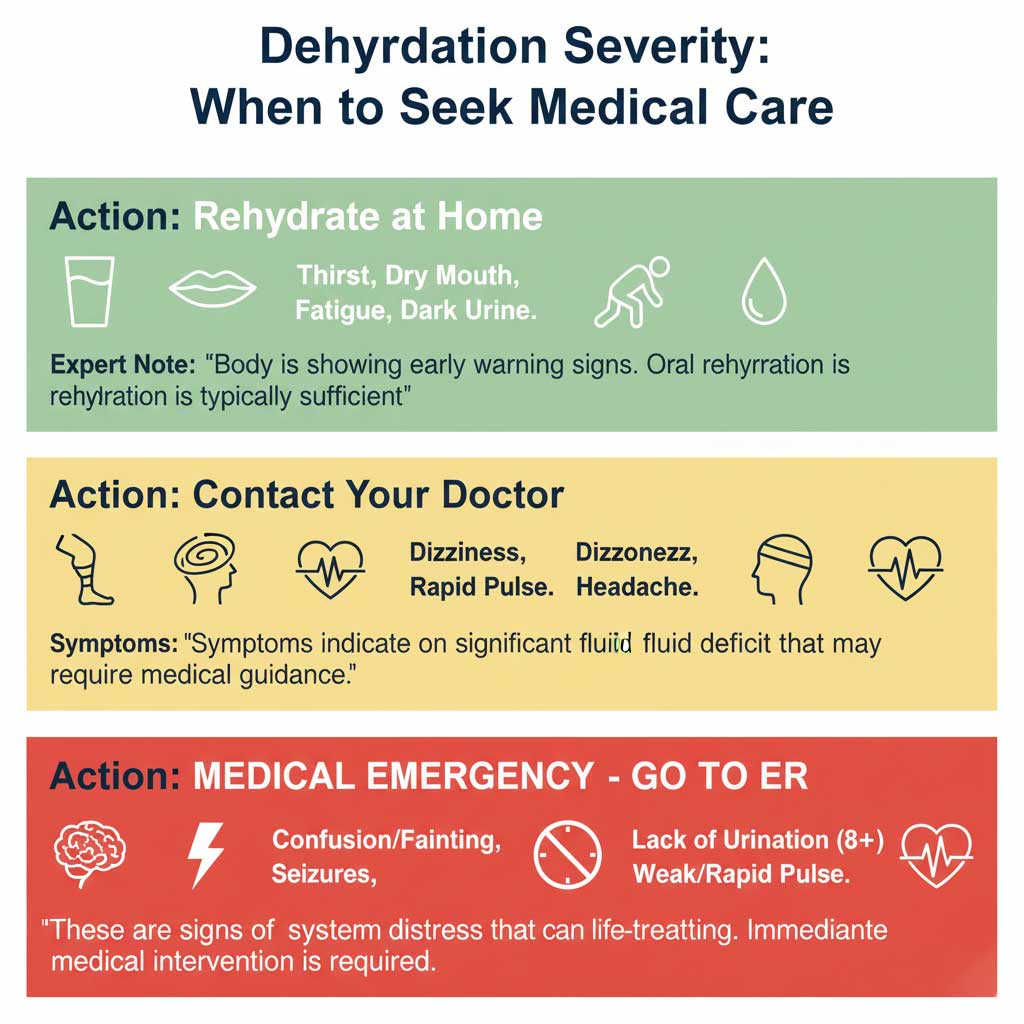
These symptoms, especially when you suspect dehydration is the cause, should not be ignored. A medical professional can confirm the diagnosis with blood work and administer the necessary treatment, such as intravenous (IV) fluids, to restore balance quickly.
Getting Tested and Taking Control of Your Health
Understanding your body’s hydration status begins with getting the right tests. Typically, a doctor will start with a physical exam and then order blood work, specifically a Comprehensive Metabolic Panel (CMP) and a Complete Blood Count (CBC), to get a full picture. These tests will provide the data needed to evaluate the five key markers we’ve discussed.
For those who want to be proactive about their health or need convenient testing solutions, services like HealthCareOnTime.com provide easy access to these essential blood panels. With health packages from HealthCareOnTime.com, you can monitor these key dehydration markers in a blood test and share your dehydration lab results with your healthcare provider. This empowers you to make informed, data-driven decisions about your diet, fluid intake, and overall hydration strategy.
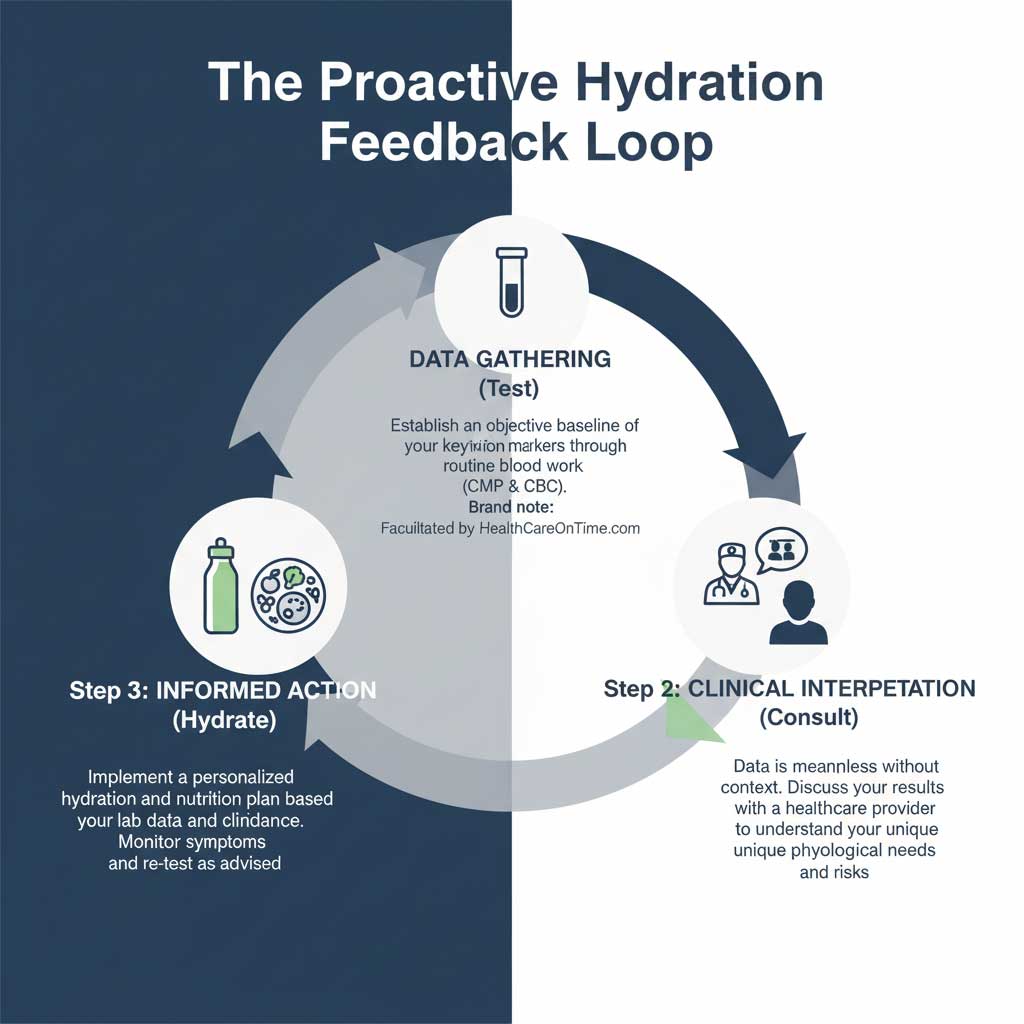
Remember, your lab results are a critical piece of the puzzle, but they should always be interpreted by a qualified healthcare professional who can consider them in the context of your symptoms, medical history, and lifestyle.
Beyond the Blood Test: Prevention and Rehydration Strategies
Knowing the signs is only half the battle. The best approach is to prevent dehydration before it starts.
- Consistent Hydration: Don’t wait until you’re thirsty. Sip water and other hydrating fluids steadily throughout the day.
- Monitor Your Urine: Aim for a light, pale yellow color. Dark yellow or amber is a sign you need to drink more.
- Eat Your Water: Incorporate water-rich foods like cucumbers, watermelon, oranges, and strawberries into your diet.
- Electrolyte Balance: If you’re sweating heavily from exercise or heat, replenish with an electrolyte drink or a balanced snack to replace lost sodium and potassium.
If you find yourself mildly dehydrated, focus on rehydrating slowly and steadily with water. For more significant fluid loss due to illness or intense activity, a beverage containing electrolytes can be more effective.
Conclusion: Your Blood Tells a Story
Your body is constantly communicating its needs, and your blood work tells a vital part of that story. The five key markers—high sodium, elevated BUN, an increased BUN-to-creatinine ratio, elevated hematocrit, and high serum osmolality—are the primary lab results indicating dehydration. They offer a clear, data-driven window into your hydration status that symptoms alone cannot provide.
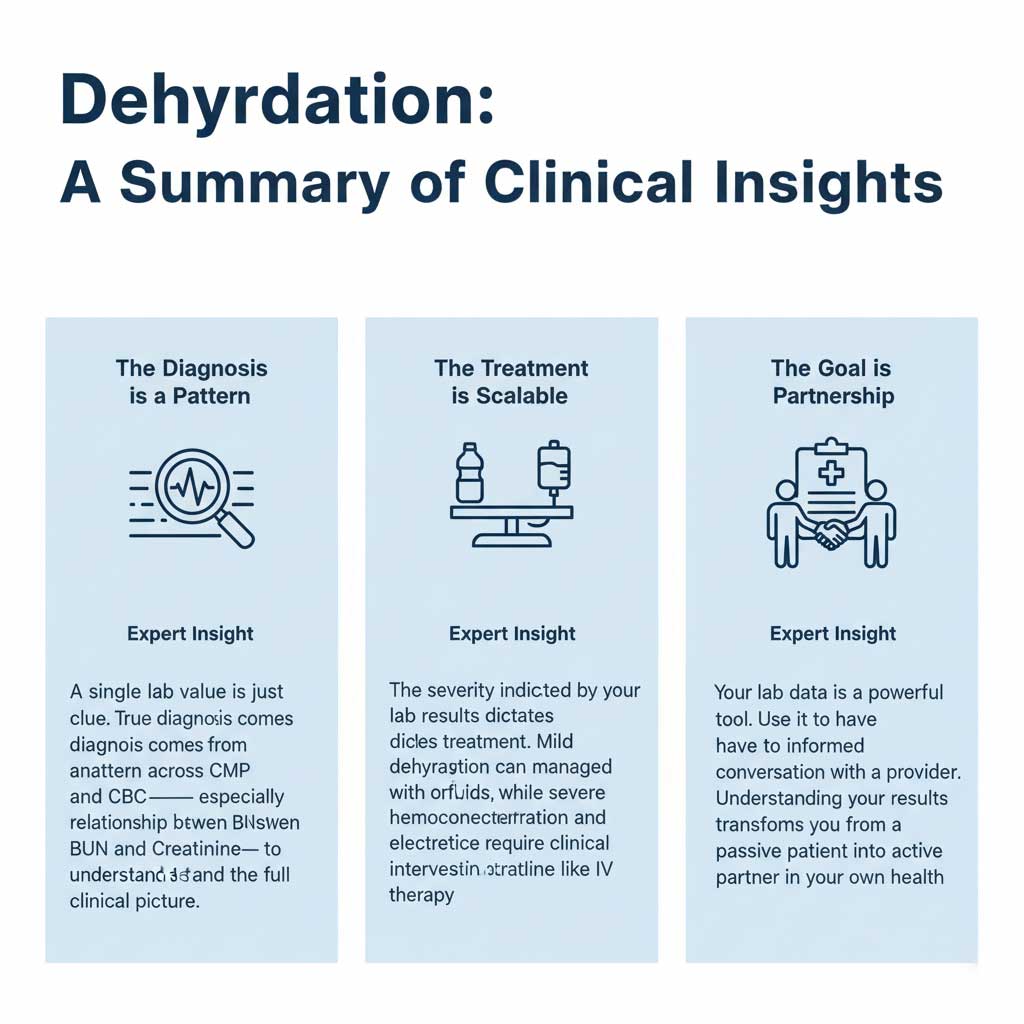
By understanding what lab values show dehydration, you are better equipped to have informed conversations with your doctor and take control of your health. Listening to your body, staying proactive with hydration, and seeking medical advice when needed are the cornerstones of maintaining the delicate fluid balance that is essential for a healthy, energetic life.









