The best medications for hepatitis B currently approved by the FDA are oral nucleos(t)ide analogues with a high barrier to resistance. These include Tenofovir alafenamide (TAF), Tenofovir disoproxil fumarate (TDF), and Entecavir. These first-line antiviral therapies effectively suppress viral replication and reduce liver inflammation.
Table of Contents
Patients should generally avoid older drugs like Lamivudine due to resistance risks, as well as hepatotoxins like high-dose acetaminophen, alcohol, and unchecked herbal supplements.
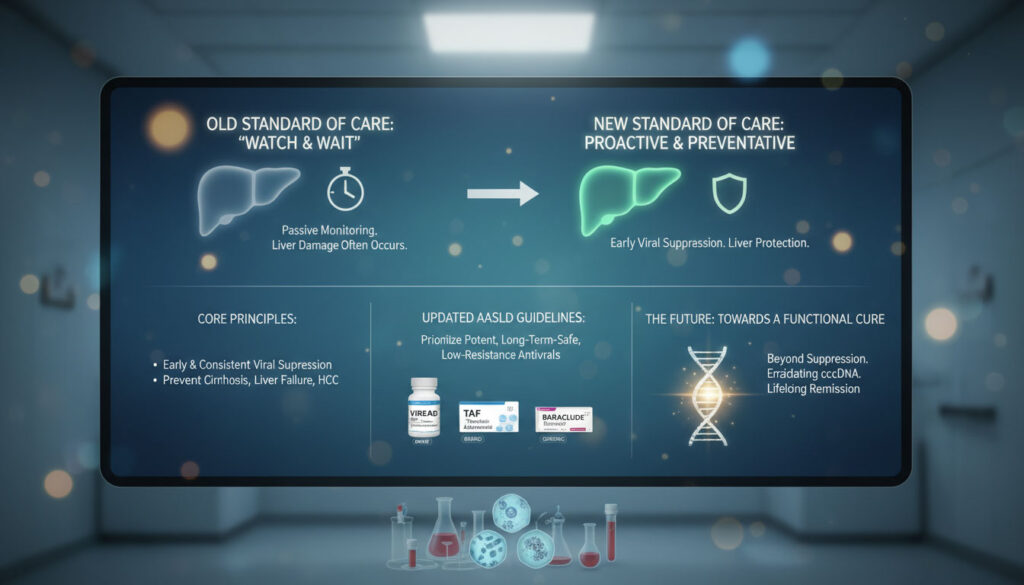
The New Standard of Care for Chronic Hepatitis B
Living with a chronic liver condition often feels like a silent negotiation with your body. You might feel perfectly healthy on the outside while your liver enzymes fluctuate internally. For years, the medical approach to chronic hepatitis B treatment was largely passive. Doctors would watch and wait. They monitored blood work and only intervened when liver damage became obvious.
That era has ended.
The current medical consensus has shifted aggressively toward preventative management. We now understand that early and consistent viral suppression is the only reliable way to alter the course of the disease. The goal is no longer just to lower the amount of virus in the blood. The objective is to halt the progression toward liver cirrhosis risks, prevent liver failure, and significantly reduce the likelihood of developing hepatocellular carcinoma (HCC).
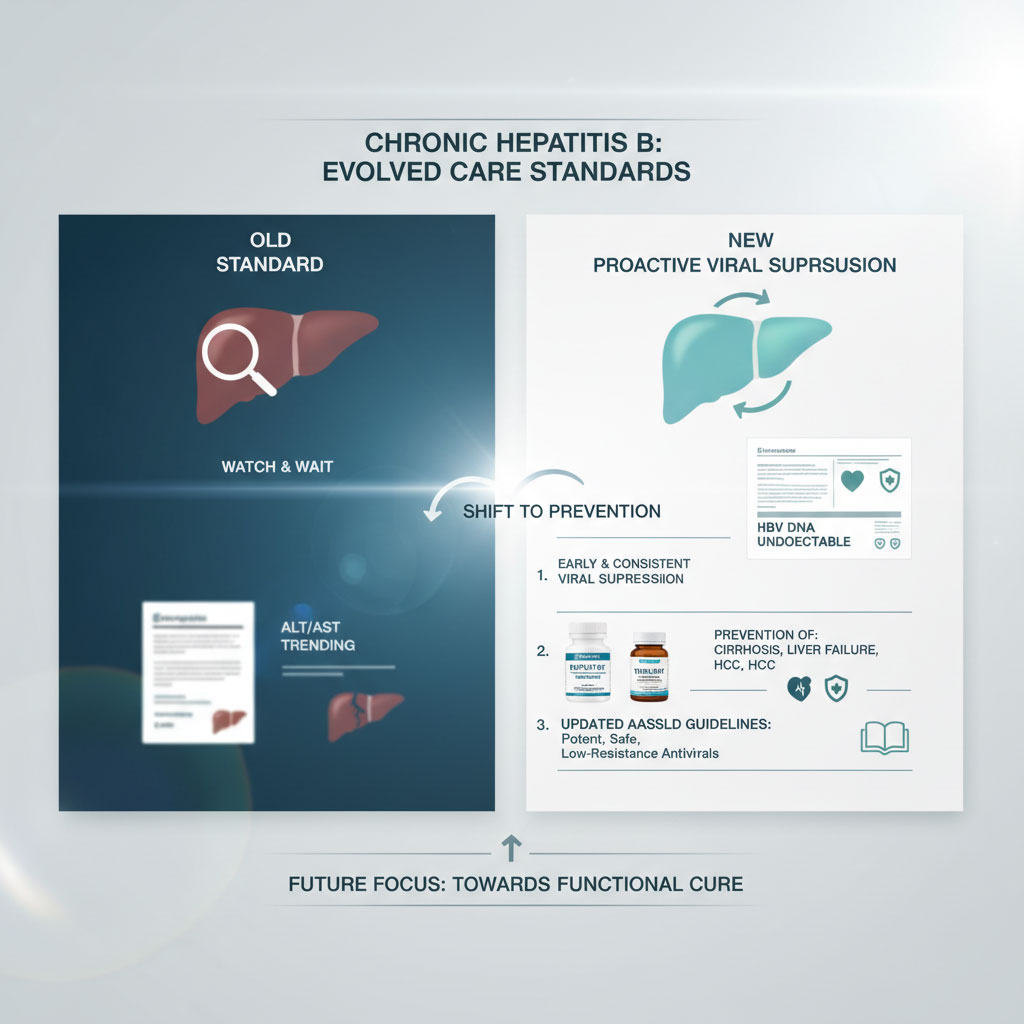
Leading organizations like the American Association for the Study of Liver Diseases (AASLD) have updated their guidelines to reflect this proactive stance. They prioritize medications that are potent, safe for long-term use, and unlikely to develop drug resistance.
Navigating these options can be overwhelming. Patients often struggle to distinguish between generic names and brand names or wonder if their current regimen is outdated. This guide breaks down the best medications for hepatitis B, explains why certain drugs must be avoided, and looks ahead to the promising future of a functional cure.
Understanding How Antivirals Work
Before diving into specific drug names, it helps to understand what these medications actually do inside your body. The Hepatitis B virus is a master of replication. It hijacks your liver cells and uses them as factories to produce copies of itself.
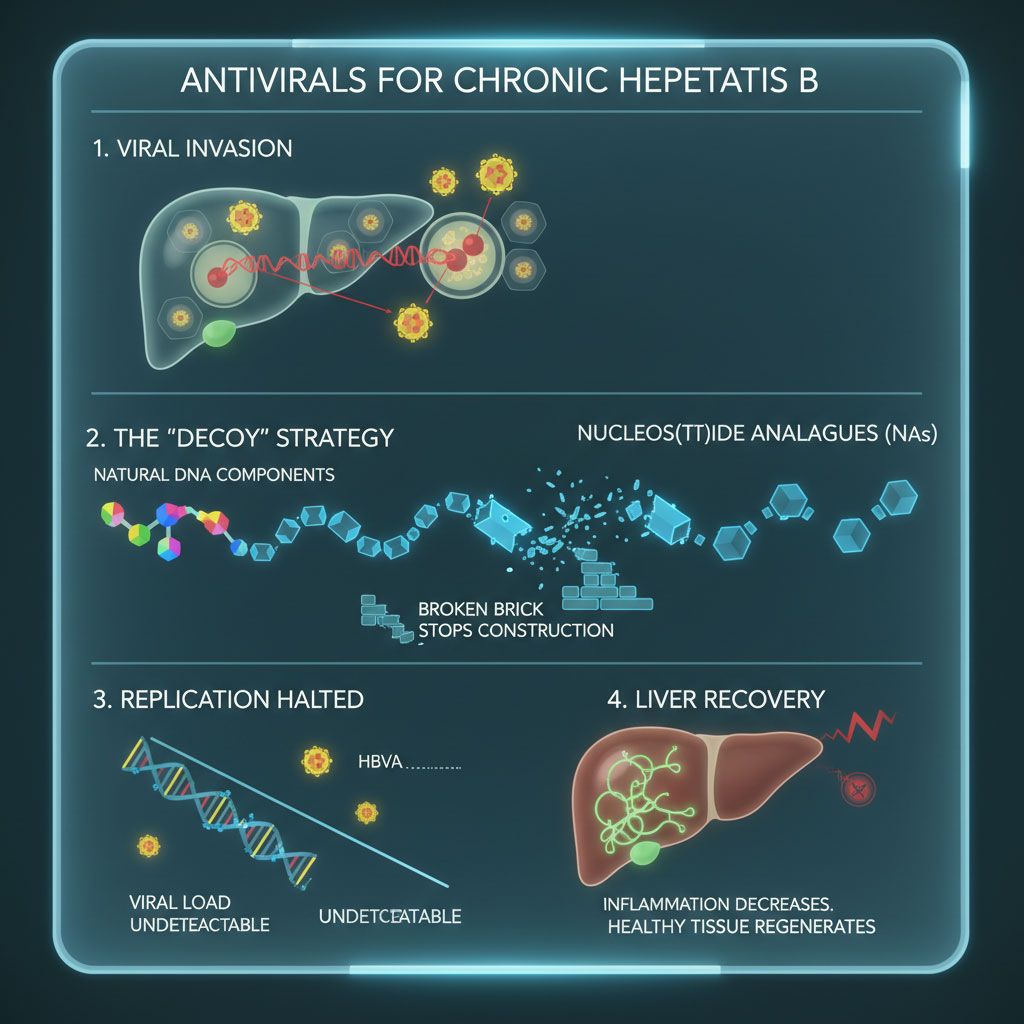
The current standard medications are classified as nucleos(t)ide analogues (NAs). You can think of them as “decoy” building blocks. When the virus tries to build new DNA to replicate, it mistakenly grabs the medication instead of the natural biological material it needs. Because the medication is chemically slightly different, it acts like a broken brick in a wall. It stops the construction process immediately.
This mechanism halts the production of new virus particles. Over time, as the old virus dies off and no new virus is created, the viral load in your blood drops to undetectable levels. This gives your liver a chance to heal from inflammation and regenerate healthy tissue.
The “Big Three”: First-Line Hepatitis B Medications Explained
When hepatologists discuss the gold standard for hepatitis B antiviral therapy, they are almost always referring to three specific drugs. These medications are preferred because they have a high barrier to resistance. This means the virus struggles to mutate in a way that allows it to survive the medication.
Tenofovir Alafenamide (TAF / Vemlidy)
Tenofovir alafenamide, commonly known as TAF or by the brand name Vemlidy, represents the latest evolution in chronic hepatitis B treatment. It was designed specifically to address the long-term safety concerns associated with older formulations of tenofovir.
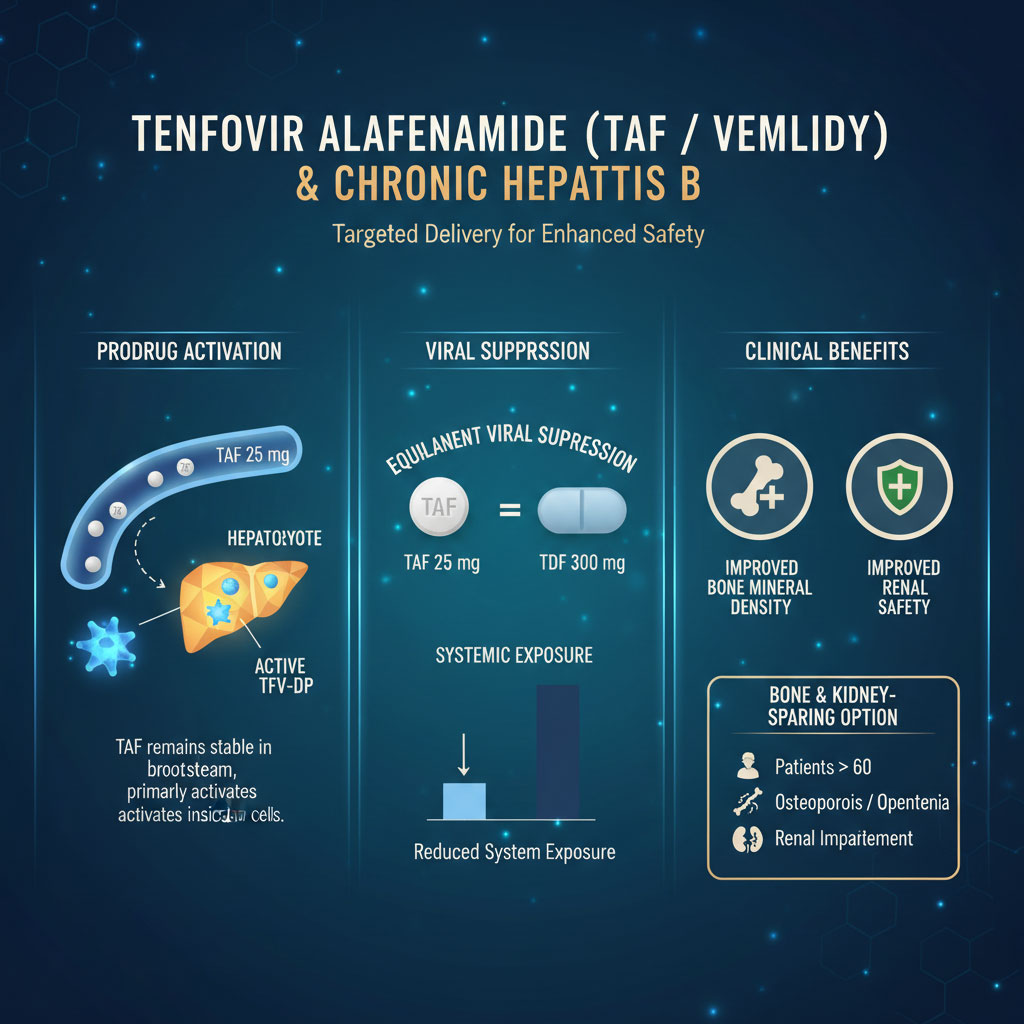
The primary advantage of TAF is its targeted delivery system. It acts as a “prodrug,” meaning it remains stable in the bloodstream and largely activates only after it has entered the liver cells. This allows for a much smaller dose to achieve the same level of hepatitis B viral load suppression as its predecessor. Specifically, 25 mg of TAF achieves similar viral suppression to 300 mg of the older TDF formulation.
Because less drug circulates in the blood, there is significantly less exposure to the kidneys and bones. Clinical trials have consistently shown that TAF offers non-inferior viral suppression compared to older drugs but with improved markers for renal safety in hepatitis B treatment and bone mineral density loss.
TAF is frequently the top choice for patients over the age of 60. It is also the preferred option for anyone with a history of osteoporosis, osteopenia, or developing renal impairment. The medical community views TAF as the “bone and kidney sparing” option, making it ideal for an aging population that requires lifelong therapy.
Entecavir (Baraclude)
Entecavir, often sold under the brand name Baraclude, is a potent guanosine analogue. It has been a cornerstone of hepatitis B antiviral therapy for many years. It remains one of the best medications for hepatitis B for specific patient populations.
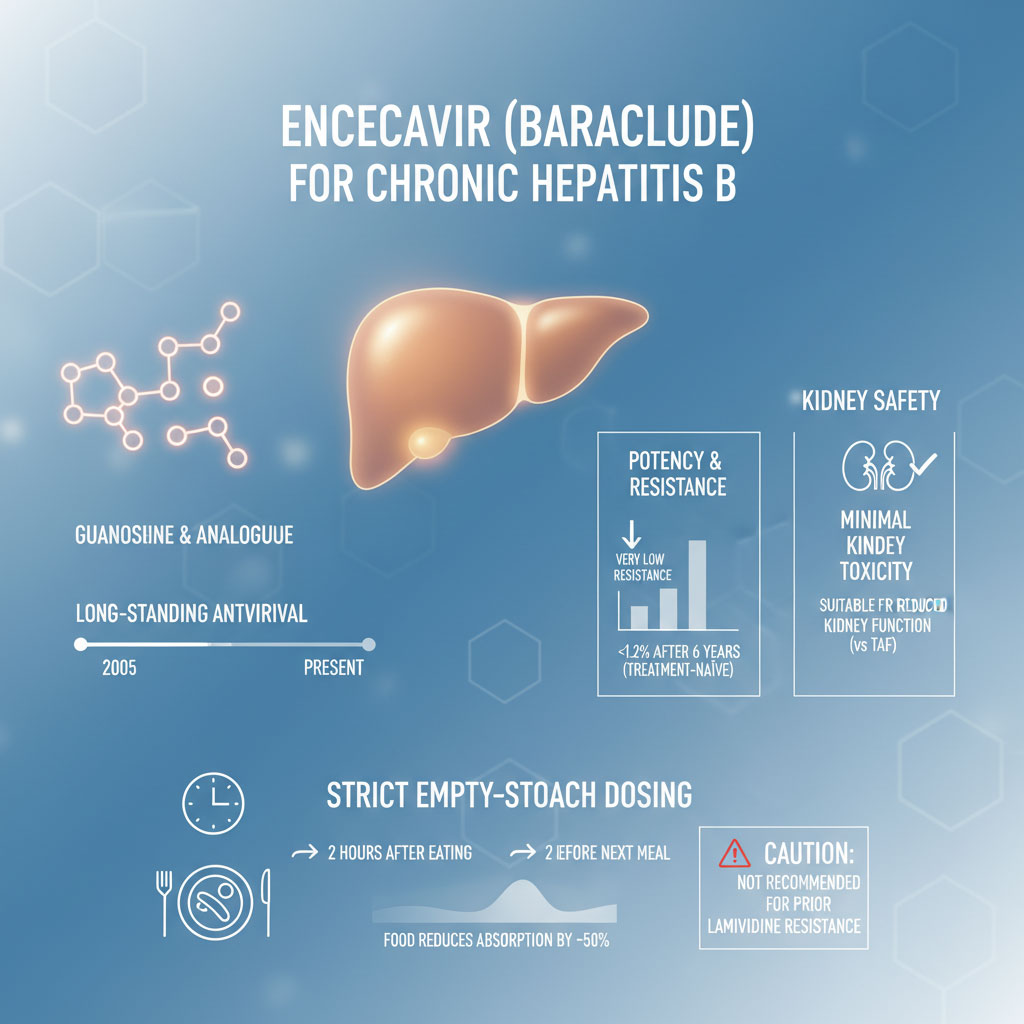
One of the key differentiators for Entecavir is that it does not carry the same potential for kidney toxicity as the older tenofovir formulations. This makes it an excellent option for patients who may already have compromised kidney function but cannot access TAF due to insurance or availability.
Studies show that in treatment-naïve patients (those who have never taken hepatitis B medication before), resistance to Entecavir is exceptionally rare. It occurs in less than 1.2% of patients after six years of continuous therapy.
However, Entecavir comes with strict dietary rules. To be effective, it must be taken on an empty stomach. This usually means taking it at least two hours after a meal or two hours before the next one. Food significantly reduces the absorption of the drug, potentially cutting its effectiveness by half.
It is also important to note that Entecavir is generally not recommended for patients who have previously developed resistance to Lamivudine. In those specific cases, the virus can quickly learn to evade Entecavir as well.
Tenofovir Disoproxil Fumarate (TDF / Viread)
Tenofovir disoproxil fumarate, or TDF, was the original game-changer in the world of chronic hepatitis B treatment. It is a nucleotide analogue that is incredibly effective at suppressing the virus.
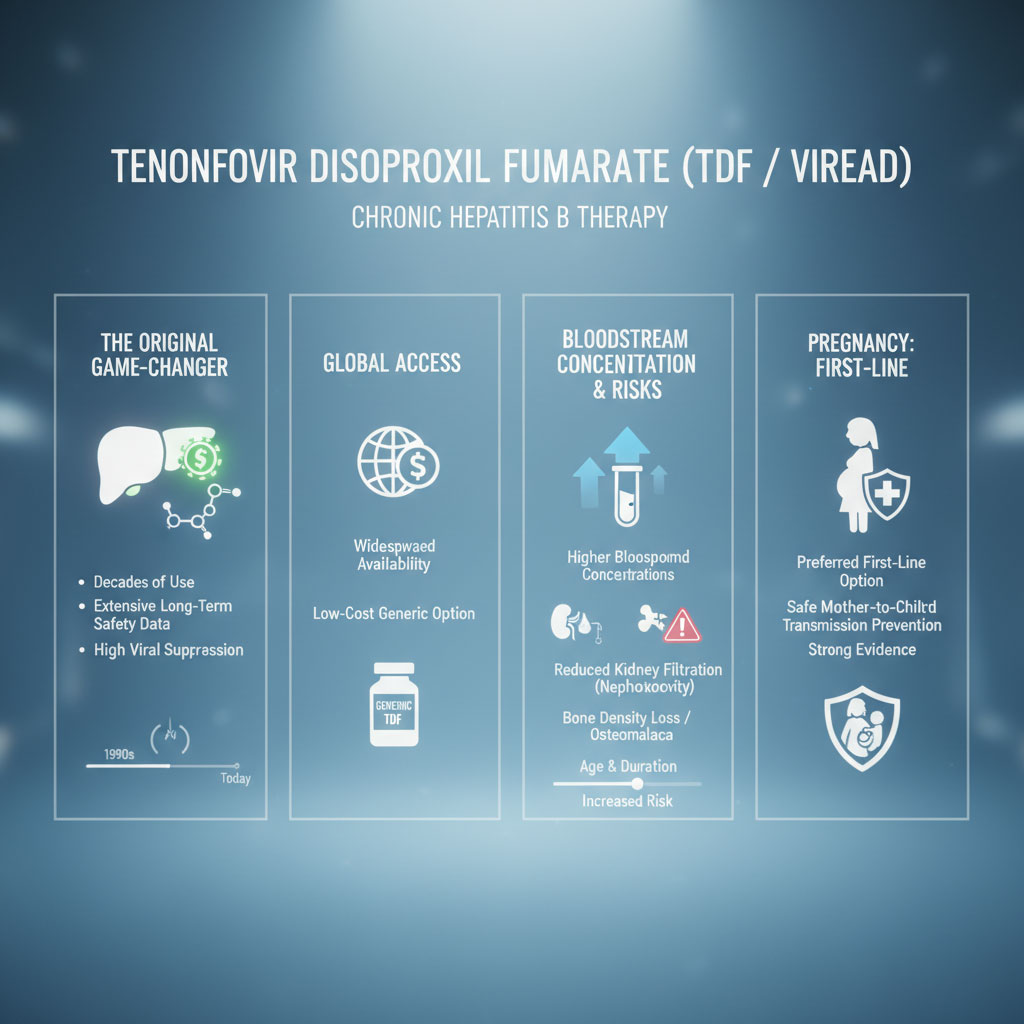
TDF has been used for decades. This provides doctors with a massive amount of long-term safety data. Because it has been on the market for so long, it is available as a generic. This makes it the most cost-effective option for many patients without comprehensive insurance coverage.
The downside of TDF is that it circulates in the blood at higher concentrations before reaching the liver. Over decades of use, this can lead to a decline in kidney filtration rates (nephrotoxicity) and a thinning of the bones (osteomalacia or density loss). While these side effects do not happen to everyone, the risk increases with age and duration of treatment.
Despite these risks, TDF remains the preferred first-line treatment for hepatitis B pregnancy treatment. The safety data for TDF in preventing mother-to-child transmission is robust. It allows pregnant women to lower their viral load safely without harming the developing fetus.
Comparative Analysis: Which Hepatitis B Drug is Right for You?
Choosing between Tenofovir (TAF or TDF) and Entecavir is a decision that relies heavily on your personal medical history. It is not simply a matter of which drug is stronger. All three are highly potent.
The decision usually comes down to your “co-morbidities.” These are the other health conditions you might have alongside hepatitis B. Your doctor will look closely at your creatinine levels and eGFR (estimated Glomerular Filtration Rate) to determine your kidney health. They will also assess your bone density history.
If your kidneys are healthy and you are looking for a cost-effective solution, TDF might be acceptable. If you have early signs of kidney disease or bone density issues, Tenofovir alafenamide or Entecavir are far superior choices.
The table below outlines the key differences to help you have an informed conversation with your specialist.
| Feature | Entecavir (Baraclude) | Tenofovir (TDF) | Tenofovir (TAF) |
| Resistance Barrier | High (in naïve patients) | Very High | Very High |
| Kidney Safety | High | Low Risk (Requires Monitoring) | High |
| Bone Safety | High | Risk of Density Loss | High |
| Pregnancy Safety | Limited Human Data | Preferred First-Line | Limited Human Data |
| Dietary Restrictions | Empty Stomach Required | With/Without Food | With Food |
| Generic Availability | Yes | Yes | No (Brand Only) |
Monitoring Your Progress: How to Know the Medication is Working
Taking the medication is step one. Knowing it is working is step two. When you are on hepatitis B antiviral therapy, your hepatologist will order blood tests every 3 to 6 months. Here are the key markers they are looking for.
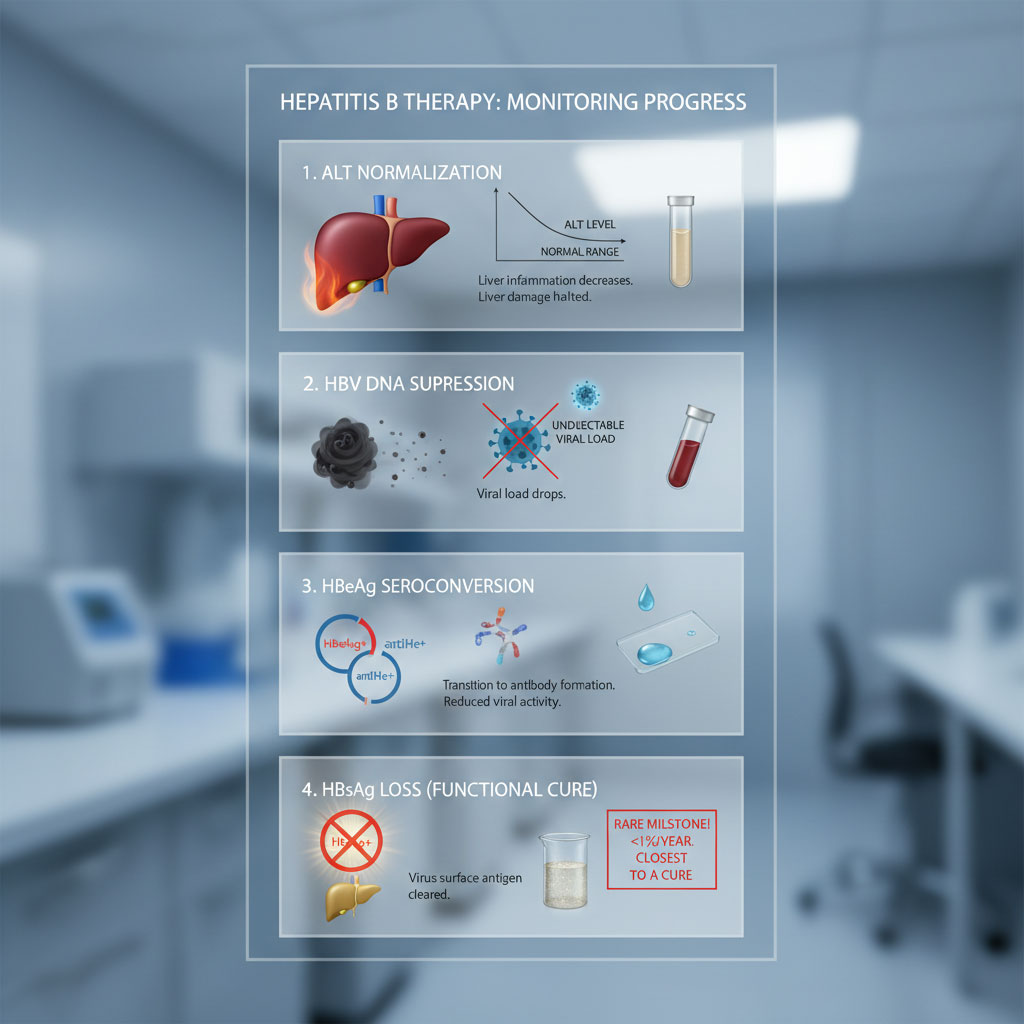
1. ALT Normalization
ALT (Alanine Aminotransferase) is an enzyme found in liver cells. When liver cells are damaged or inflamed, they leak ALT into the bloodstream. A high ALT level indicates active liver damage. The first sign that your medication is working is a drop in ALT levels to within the normal range. This means the inflammation has stopped.
2. HBV DNA Suppression
This is the most direct measure of the medication’s success. HBV DNA tests measure the amount of virus circulating in your blood. The goal is to reach an “undetectable” viral load. This does not mean the virus is gone completely from the body, but it is suppressed so heavily that standard tests cannot find it. Achieving undetectability significantly lowers the risk of cirrhosis and cancer.
3. HBeAg Seroconversion
For patients who are “HBeAg-positive” (a marker of high infectivity), a major treatment milestone is losing this antigen and developing the antibody (anti-HBe). This is called seroconversion. It represents a state of lower viral activity and better long-term outcomes.
4. HBsAg Loss (The Functional Cure)
The ultimate goal is the loss of the Hepatitis B surface antigen (HBsAg). This is rare with current oral medications, occurring in less than 1% of patients per year. However, if this happens, it is considered a functional cure, and in some cases, treatment can be stopped under strict supervision.
Medications and Substances to Avoid with Hepatitis B
Managing liver disease is as much about what you avoid as what you take. The liver is the body’s primary filtration system. When it is compromised by chronic infection, its ability to process toxins decreases.
There is a long list of drugs to avoid with hepatitis B. Some can cause direct toxicity. Others can trigger the immune system in a way that causes the virus to flare up uncontrollably.
The Painkiller Protocol: NSAIDs vs. Acetaminophen
One of the most common questions patients ask is, “Is Tylenol safe for hepatitis B?“
There is a pervasive myth that patients with liver disease must avoid acetaminophen (Tylenol) at all costs. Surprisingly, for patients with liver cirrhosis risks, acetaminophen is often safer than the alternatives if taken in limited doses.
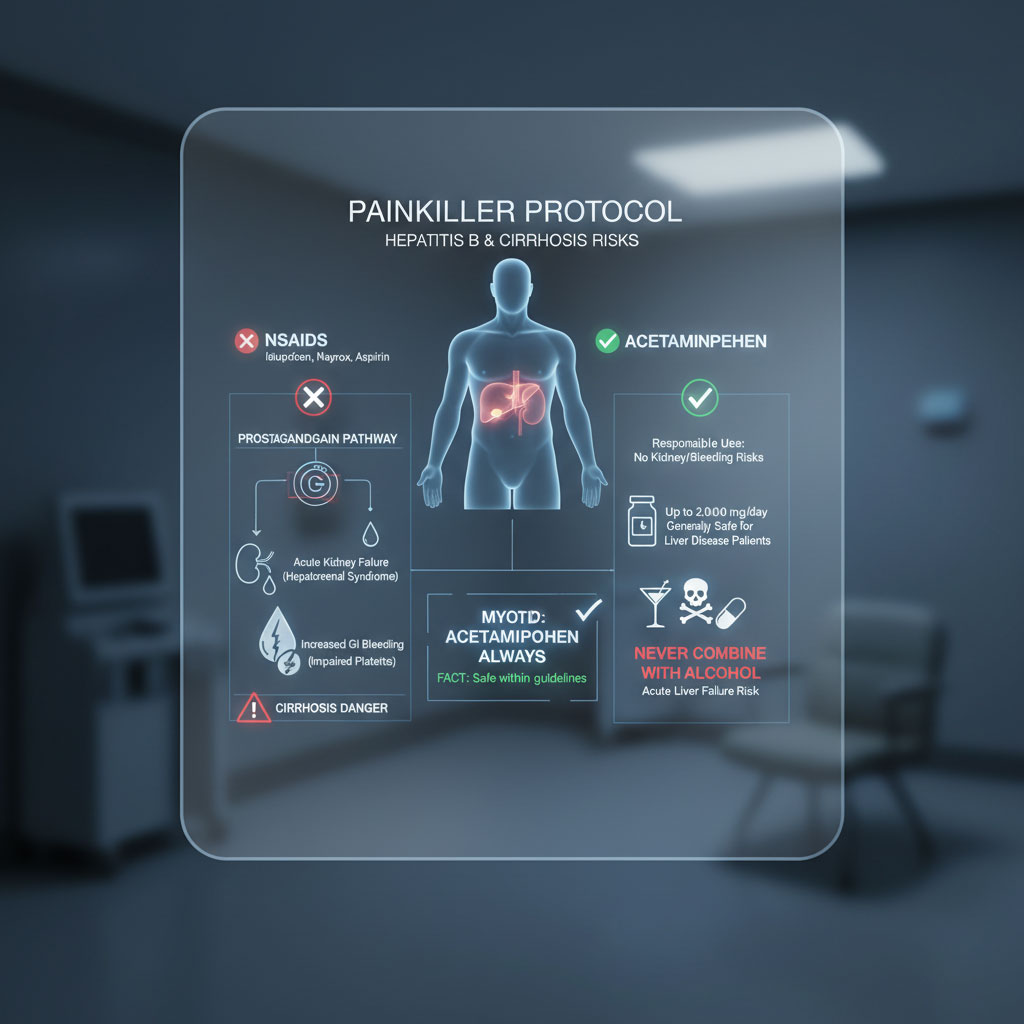
Non-steroidal anti-inflammatory drugs (NSAIDs) include common painkillers like ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin. In patients with advanced liver disease or cirrhosis, NSAIDs can be extremely dangerous.
The mechanism involves prostaglandins. These are chemicals that help keep the blood vessels in the kidneys open. NSAIDs block prostaglandins. In a healthy person, this is fine. In a person with cirrhosis, the kidneys rely heavily on prostaglandins to maintain blood flow. Taking NSAIDs can constrict these vessels, precipitating acute kidney failure (hepatorenal syndrome). Furthermore, NSAIDs impair platelet function, which increases the risk of bleeding in the gastrointestinal tract, a catastrophic event for cirrhosis patients.
Acetaminophen does not carry these same bleeding or kidney risks. The American College of Gastroenterology generally suggests that up to 2,000mg (2 grams) of acetaminophen per day is safe for most patients with liver disease. This is about half the maximum dose recommended for a healthy person.
However, you must never combine acetaminophen with alcohol. That combination is a direct pathway to acute liver failure.
Hepatotoxic Drugs and Supplements
The wellness industry promotes many products that claim to “detox” or support the liver. Unfortunately, many herbal supplements harmful for liver health are sold without strict FDA regulation.
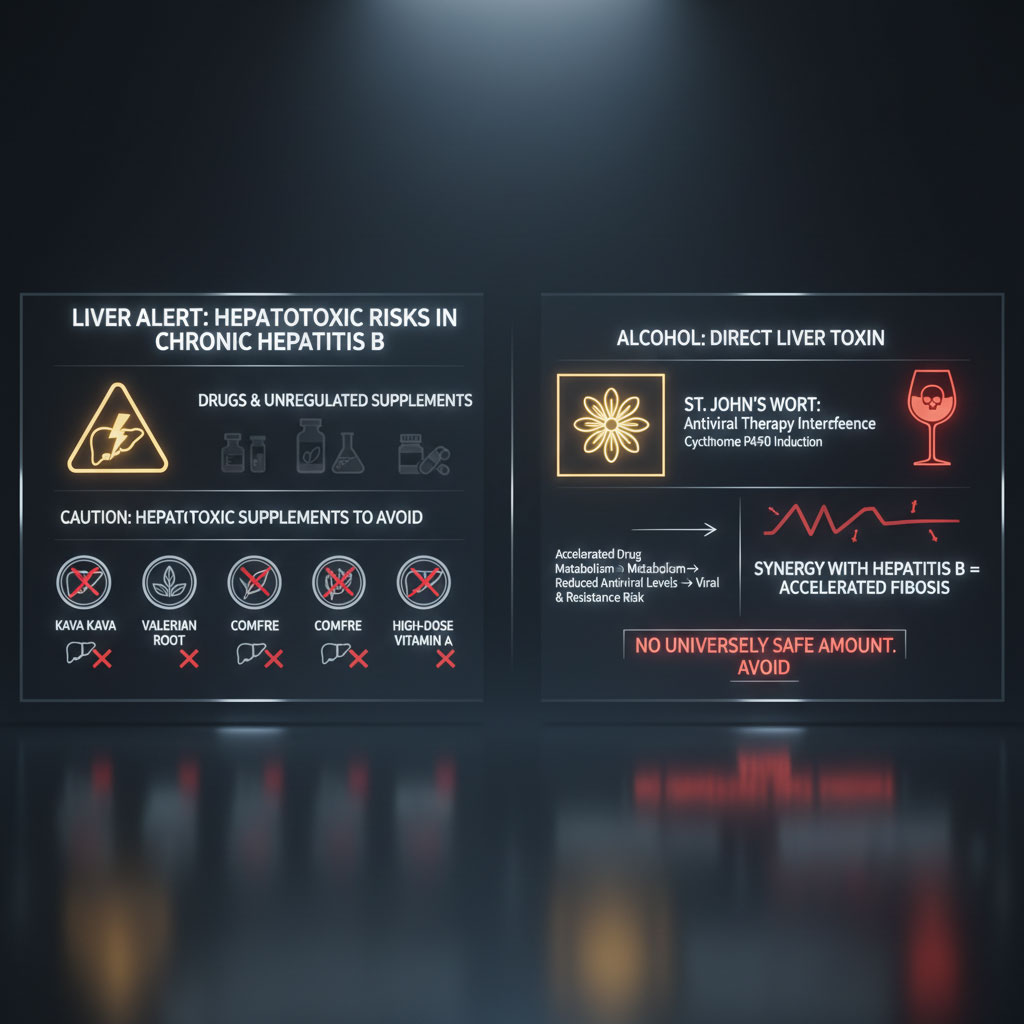
Patients with chronic hepatitis B treatment plans should be extremely wary of supplements containing Kava Kava, Valerian, Comfrey, or very high doses of Vitamin A. These substances have known hepatotoxic profiles.
St. John’s Wort is another herbal supplement to avoid. It acts as an inducer of the Cytochrome P450 enzyme system in the liver. This means it speeds up the way your liver processes drugs. If you take St. John’s Wort, it can cause your hepatitis B antiviral therapy to be metabolized and excreted too quickly. This effectively lowers the therapeutic dose in your body and gives the virus a chance to replicate and develop resistance.
Alcohol acts as a direct toxin to liver cells. Studies consistently show that combining alcohol with chronic hepatitis B dramatically accelerates the fibrosis process. There is no universally “safe” amount of alcohol for someone with active hepatitis B. The synergy between the virus and the alcohol creates a much faster path to cirrhosis than either factor alone.
Obsolete Antivirals (Second-Line Options)
Decades ago, the landscape of best medications for hepatitis B looked very different. Drugs like Lamivudine (Epivir-HBV) and Adefovir were the only options available.
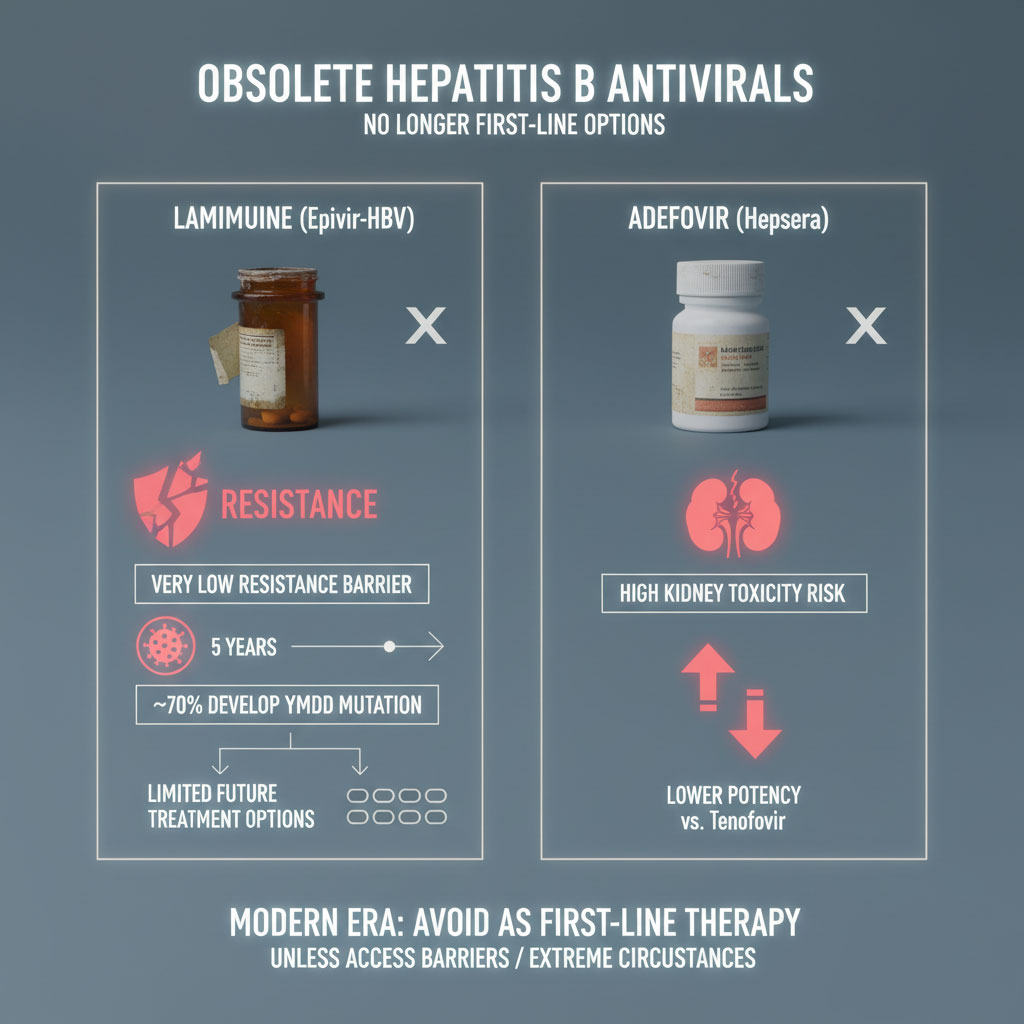
Today, these drugs are considered obsolete for new patients. Lamivudine has a very low barrier to resistance. Within five years of treatment, nearly 70% of patients will develop a drug-resistant strain of the virus known as the YMDD mutation.
Once resistance develops, it makes treating the virus much more difficult. It can also limit which drugs will work for you in the future. Adefovir, another older drug, is associated with a high risk of kidney toxicity and is less potent than Tenofovir. Unless there are extreme circumstances or lack of access, no patient should start their therapy with Lamivudine or Adefovir in the modern era.
Special Populations: Tailoring Treatment
Hepatitis B does not affect every patient in the same way. Treatment plans must be tailored to life stages and other medical conditions.
Pregnancy and Hepatitis B
For women of childbearing age, the management of hepatitis B pregnancy treatment is critical. The virus can be passed from mother to child during birth. This is the most common way the infection becomes chronic globally.
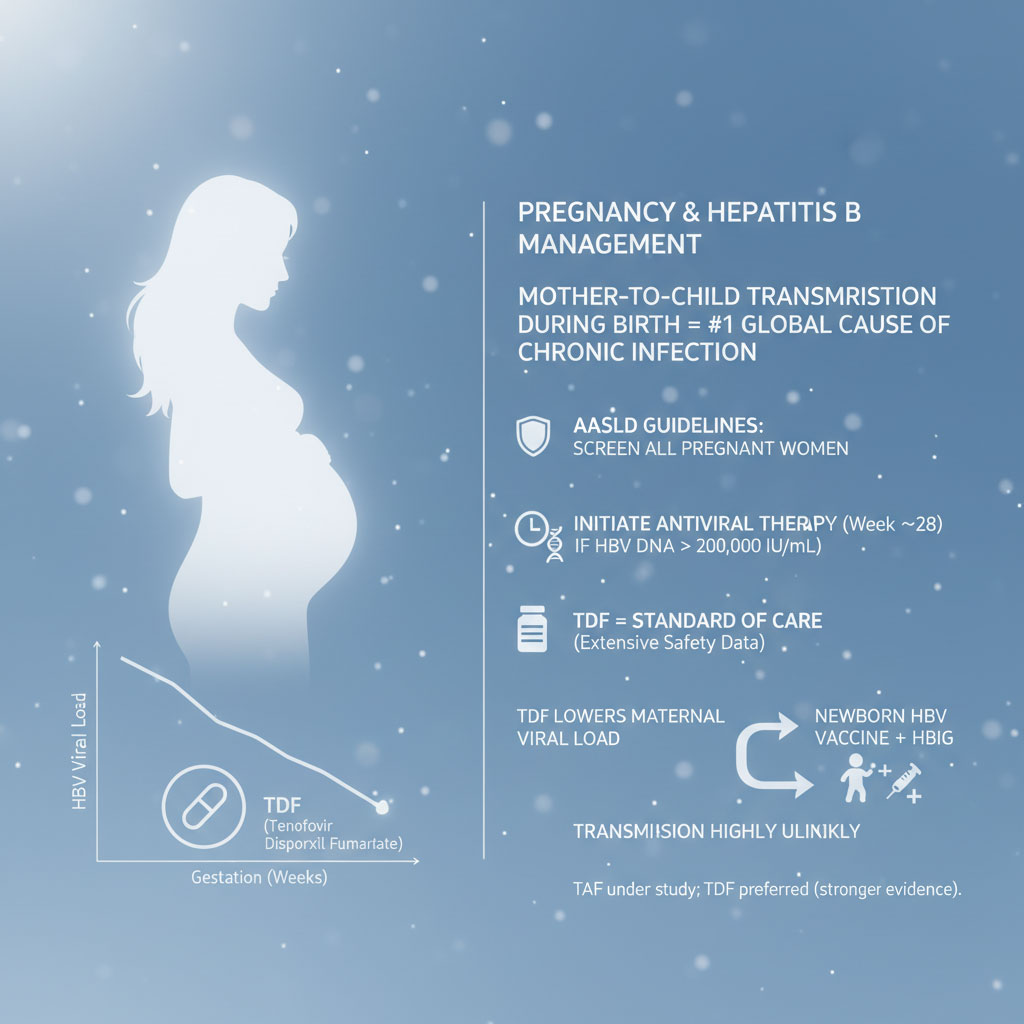
The AASLD guidelines hepatitis B section recommends screening all pregnant women. If the viral load is high (usually greater than 200,000 IU/mL), antiviral therapy is recommended starting in the third trimester (around week 28).
Tenofovir disoproxil fumarate (TDF) is the standard of care here. It has an extensive safety record for use during pregnancy. It lowers the viral load enough to make transmission to the baby highly unlikely. This is especially effective when combined with the hepatitis B vaccine and immunoglobulin (HBIG) given to the newborn immediately after birth. TAF is currently being studied in pregnancy, but TDF retains the most safety data.
Co-Infection (HIV or Hepatitis C)
Patients co-infected with HIV and Hepatitis B face a unique challenge. Both viruses require treatment. Fortunately, some HIV medications are also effective against Hepatitis B.

Regimens containing Tenofovir (either TDF or TAF) combined with emtricitabine (such as Truvada or Descovy) are often used to treat both infections simultaneously.
It is vital that patients do not stop these medications abruptly. Doing so can cause a severe flare-up of hepatitis B. Additionally, patients undergoing treatment for Hepatitis C must ensure their Hepatitis B is covered. The new Direct Acting Antivirals (DAAs) for Hepatitis C are extremely effective, but curing Hepatitis C can sometimes cause the Hepatitis B virus to “wake up” or reactivate if it is not being suppressed with hepatitis B antiviral therapy. This is because the Hepatitis C virus often suppresses the Hepatitis B virus when both are present. Removing the Hepatitis C virus removes this suppression.
Immunosuppression and Chemotherapy
A critical, often overlooked group includes patients undergoing chemotherapy or taking immunosuppressive drugs for conditions like rheumatoid arthritis or inflammatory bowel disease. Drugs like Rituximab (used for lymphoma and autoimmune diseases) or high-dose steroids can cause a catastrophic reactivation of Hepatitis B.
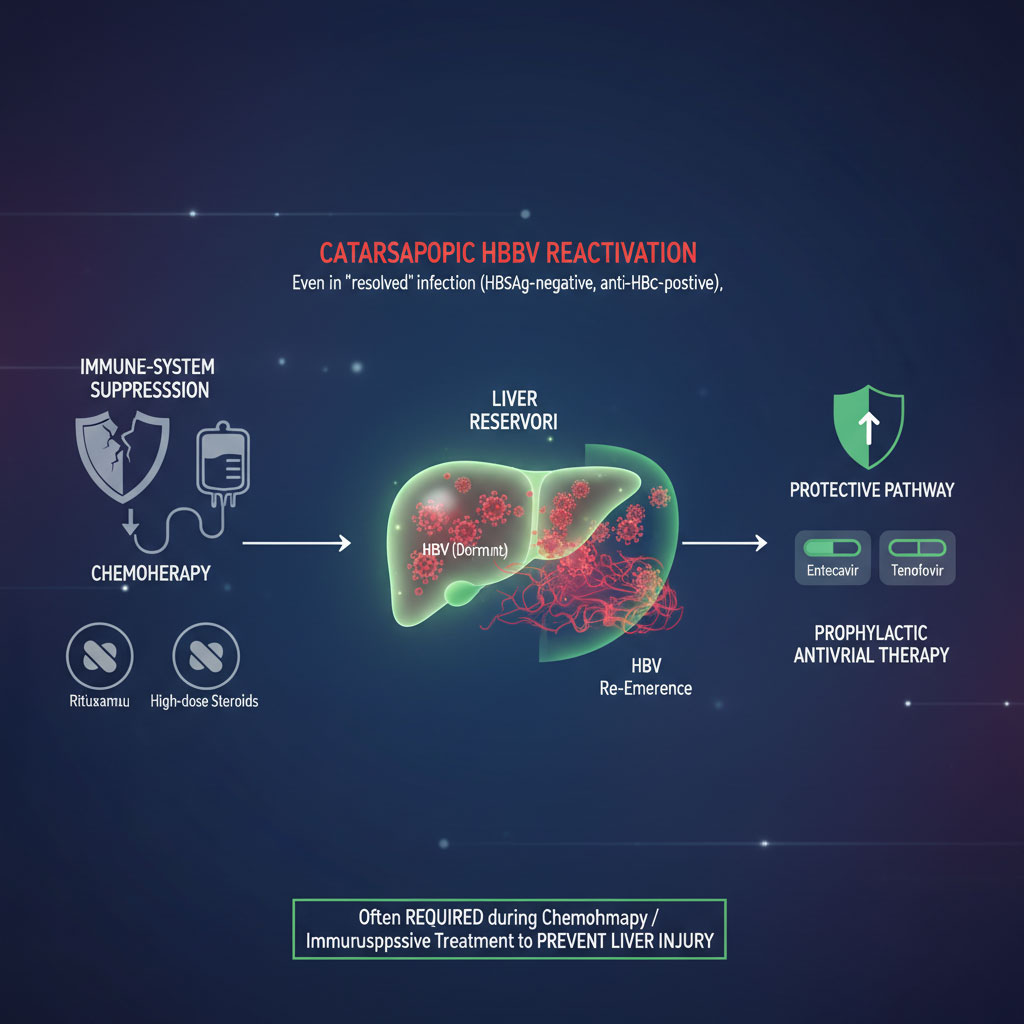
Even if a patient has a “resolved” infection (HBsAg negative but anti-HBc positive), strong immunosuppression can allow the virus to re-emerge from the liver reservoir. In these cases, prophylactic antiviral therapy with Entecavir or Tenofovir is often required to protect the liver during the course of chemotherapy.
The Future of Treatment: Functional Cure and Innovation
While current therapies are effective at suppression, they are rarely curative. Patients usually must stay on medication for years or for life. This has driven researchers to find a hepatitis B functional cure.
The challenge lies in the biology of the virus. Hepatitis B forms a “mini-chromosome” called cccDNA (covalently closed circular DNA) inside the nucleus of infected liver cells. Current oral drugs stop the virus from replicating, but they do not destroy this cccDNA reservoir. As long as the cccDNA exists, the virus can return if medication is stopped.
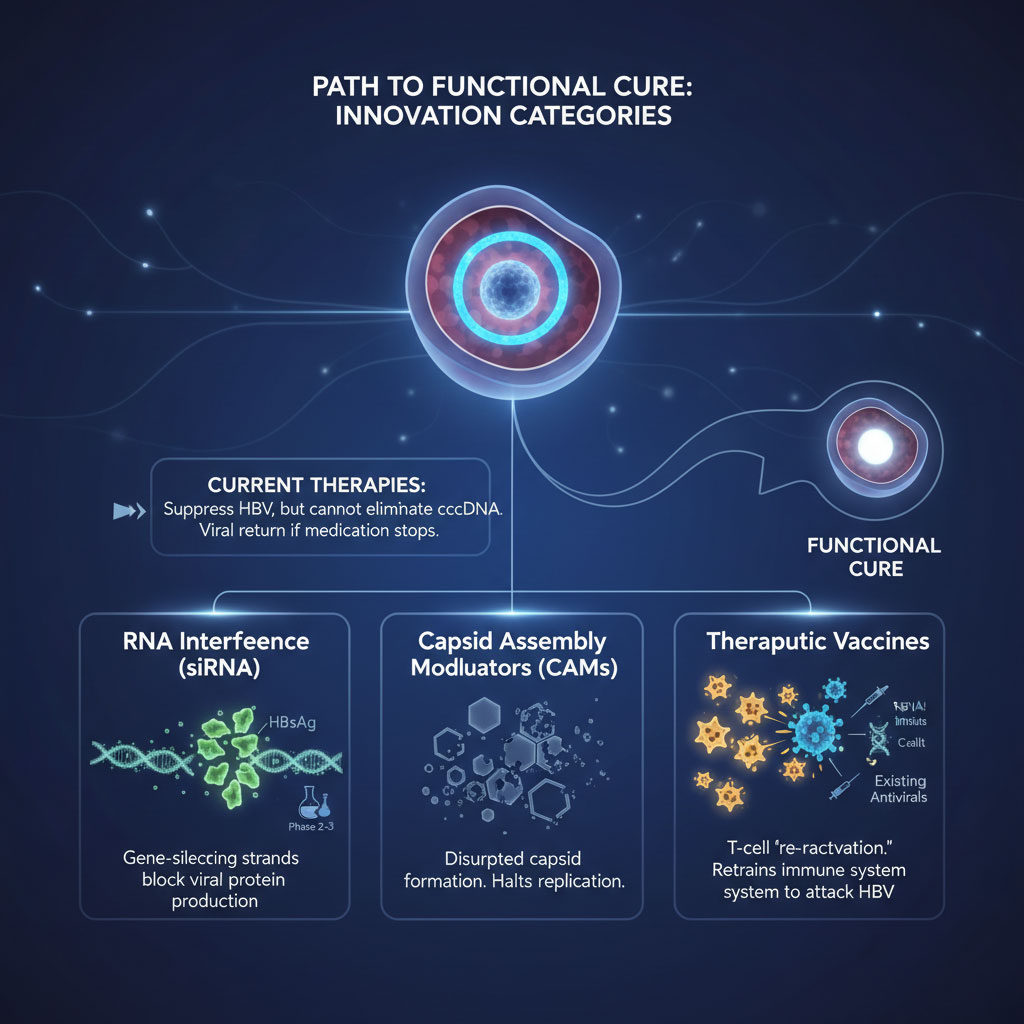
RNA Interference (siRNA)
One of the most exciting areas of research involves RNA interference. These drugs are designed to silence the specific genes the virus uses to produce proteins. By cutting off the production of viral proteins, particularly the Surface Antigen (HBsAg), these therapies hope to overwhelm the virus and allow the immune system to regain the upper hand. Several major pharmaceutical companies have siRNA candidates in Phase 2 and Phase 3 clinical trials.
Capsid Assembly Modulators (CAMs)
The virus needs a protective shell, called a capsid, to transport its genetic material. Capsid Assembly Modulators are a new class of drugs that trick the virus into building defective shells. Some CAMs cause the capsid to form too early, trapping the genetic material uselessly. Others prevent the capsid from forming at all. This disrupts the replication cycle at a fundamental level distinct from how current NAs work.
Therapeutic Vaccines
Unlike preventative vaccines, therapeutic vaccines are designed for people who are already infected. Patients with chronic hepatitis B often have an “exhausted” immune system that ignores the virus. Therapeutic vaccines aim to wake up or retrain the T-cells to recognize the virus as a threat and attack infected cells. These are often tested in combination with siRNA and current antivirals to attack the virus from multiple angles simultaneously.
Safety & Interactions Cheat Sheet
Navigating daily life with chronic hepatitis B treatment requires vigilance regarding drug interactions. This reference table simplifies the risk levels of common substances.
| Drug/Substance Class | Risk Level for HBV Patients | Recommendation |
| Alcohol | 🔴 Critical Risk | Avoid completely; accelerates cirrhosis. |
| NSAIDs (Ibuprofen/Advil) | 🟡 Moderate/High Risk | Avoid if you have cirrhosis; use sparingly otherwise. |
| Acetaminophen (Tylenol) | 🟢 Safe (with limits) | Safe under 2g/day; avoid with alcohol. |
| Corticosteroids | 🔴 High Risk | Can trigger severe viral flares; requires antiviral prophylaxis. |
| Statins | 🟢 Generally Safe | Usually safe; monitor liver enzymes. May reduce cancer risk. |
| Herbal “Detox” Teas | 🔴 High Risk | Avoid; unregulated and potential for direct toxicity. |
| Antibiotics (some classes) | 🟡 Low/Moderate Risk | Generally safe, but confirm liver metabolism with doctor. |
Summary & Key Takeaways
The management of hepatitis B has entered a new era of safety and efficacy. The best medications for hepatitis B available today offer patients the ability to live normal, healthy lives with minimal side effects.
Tenofovir alafenamide (TAF), Tenofovir disoproxil fumarate (TDF), and Entecavir are the pillars of modern treatment. TAF and Entecavir are generally preferred for their safety profiles regarding kidneys and bones, making them the superior choice for aging populations. TDF remains a vital tool for pregnancy and cost-conscious care.
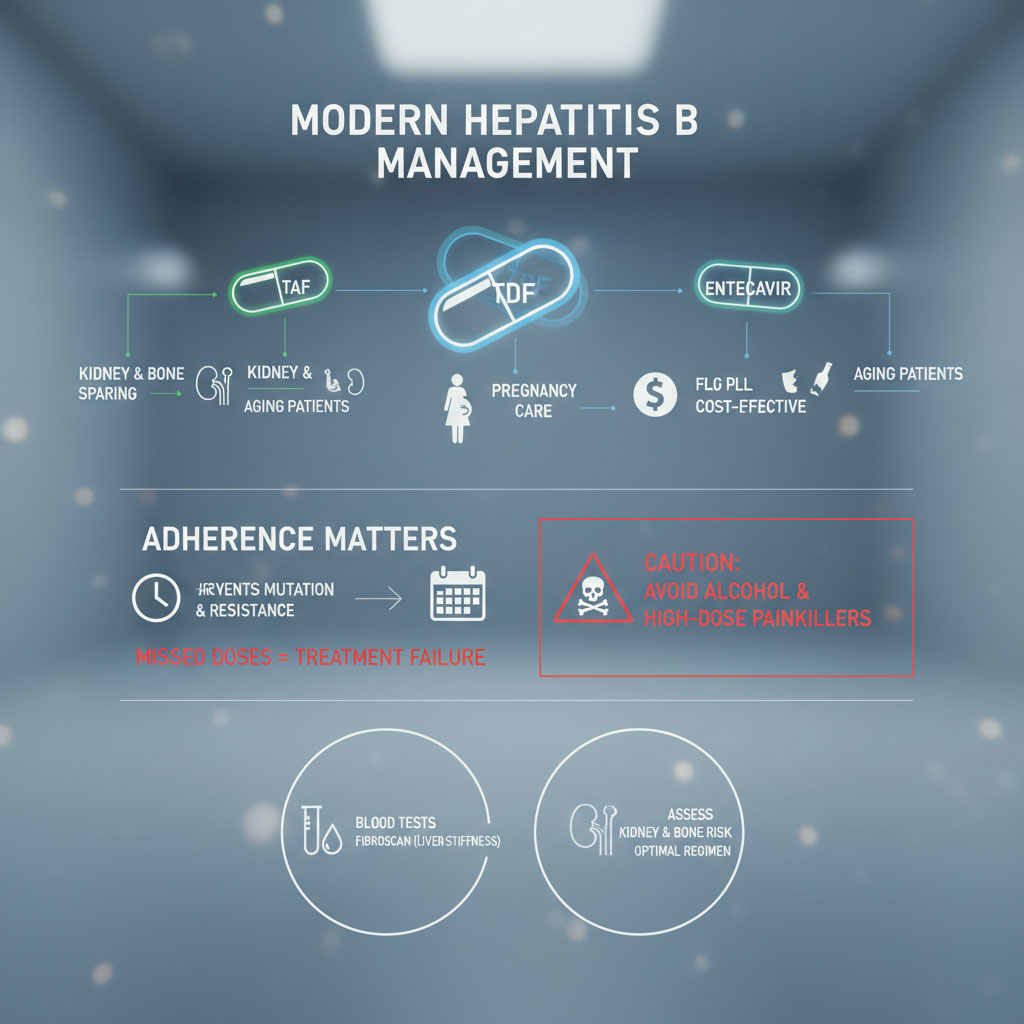
The most critical action you can take is to maintain adherence. Taking your medication every day prevents the virus from mutating. Missing doses is the number one cause of treatment failure and viral resistance. Furthermore, avoiding drugs to avoid with hepatitis B like alcohol and high-dose painkillers protects your remaining liver function.
If you have not done so recently, ask your hepatologist for updated blood work and a FibroScan to assess liver stiffness. Discuss your specific risk factors for bone and kidney health to ensure you are on the optimal antiviral regimen. Treatment is a marathon. With the right strategy, your liver can remain healthy for the long haul.
Frequently Asked Questions (FAQs)
What is the number one best medication for Hepatitis B?
There is no single best drug for everyone, but Tenofovir alafenamide (TAF) is currently considered the most versatile first-line treatment. It offers the high potency of Tenofovir with a better safety profile for kidneys and bones compared to older drugs. Entecavir is an equally strong contender, particularly for those with kidney issues, provided they are not resistant to Lamivudine.
Which drugs should be strictly avoided in Hepatitis B patients?
Patients should strictly avoid alcohol, as it accelerates liver damage. You should also avoid herbal supplements like Kava, Comfrey, and Valerian due to toxicity risks. Older antivirals like Lamivudine are no longer recommended. High doses of acetaminophen and long-term use of NSAIDs (like ibuprofen) should be avoided, especially in those with liver cirrhosis risks.
Is Tenofovir better than Entecavir?
Tenofovir (both TAF and TDF) is often preferred for women of childbearing age and patients with prior exposure to other antivirals because it has a slightly higher barrier to resistance. However, Entecavir is excellent for patients with renal impairment. The “better” drug depends on your kidneys, bone density, and pregnancy plans.
Can Hepatitis B be cured?
Currently, we have a “viral suppression” treatment rather than a sterilizing cure. This means we can suppress the virus to undetectable levels, preventing damage. A true hepatitis B functional cure, where the surface antigen is permanently lost, is rare with current oral drugs but is the goal of new therapies like RNAi currently in clinical trials.
What are the side effects of Tenofovir Disoproxil Fumarate (TDF)?
The two primary long-term concerns with TDF are nephrotoxicity (kidney damage) and a decrease in bone mineral density loss. Patients on TDF need regular monitoring of their creatinine and phosphate levels. If these markers worsen, doctors often switch the patient to TAF or Entecavir.
Is it safe to stop taking Hepatitis B medication?
It is generally dangerous to stop hepatitis B antiviral therapy without close medical supervision. Stopping the medication can lead to a severe hepatitis flare. The virus can rebound rapidly, causing a spike in liver enzymes that can lead to acute liver failure or death in severe cases.
Can I take painkillers like Ibuprofen with Hepatitis B?
If you have early-stage hepatitis B with no scarring, occasional ibuprofen is usually safe. However, if you have advanced fibrosis or cirrhosis, you should avoid NSAIDs like ibuprofen entirely. They can cause kidney failure and bleeding. In these cases, low-dose acetaminophen is surprisingly the safer choice.
How long does Hepatitis B treatment last?
For the vast majority of patients with chronic hepatitis B treatment, therapy is indefinite (long-term or lifelong). The goal is to keep the virus suppressed to prevent liver cirrhosis risks. Stopping treatment is only considered in very specific immunological circumstances and carries a risk of relapse.
Are there new treatments coming for Hepatitis B?
Yes. The pipeline for hepatitis B functional cure drugs is robust. Several pharmaceutical companies are testing gene-silencing drugs (siRNA), capsid assembly modulators, and therapeutic vaccines. These aim to allow patients to eventually stop taking medication safely.
Does insurance cover Vemlidy (TAF)?
Coverage for Vemlidy (TAF) varies by insurance provider in the USA. Because there is no generic version yet, it can be expensive. Many insurers require patients to try and fail generic Tenofovir (TDF) or Entecavir before they will approve TAF. Savings cards and patient assistance programs are often available from the manufacturer.
What is the difference between TDF and TAF?
Both are forms of Tenofovir. TDF is the older version that circulates in the blood at high levels, impacting kidneys and bones. TAF is the newer “prodrug” that delivers the active medication directly into liver cells. This allows for a much smaller dose and significantly reduced toxicity risks while maintaining the same viral suppression.
Can herbal supplements cure Hepatitis B?
No. There is no scientific evidence that any herbal supplement can cure Hepatitis B. In fact, many herbal supplements harmful for liver function can make the condition worse or interfere with your prescribed antivirals. Always consult your hepatologist before adding any supplements to your routine.