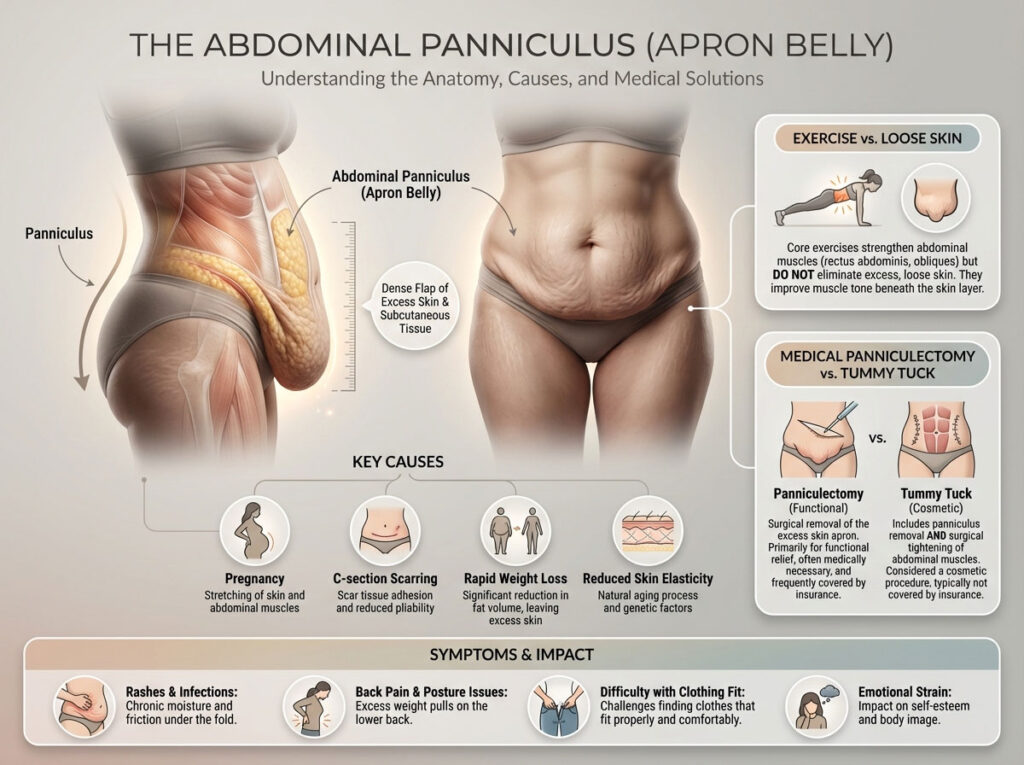
An apron belly, medically recognized as an abdominal panniculus, is a dense flap of excess skin and subcutaneous tissue that hangs from the lower abdomen. It most commonly results from pregnancy, C-section scarring, or rapid weight loss where skin elasticity fails to retract. While core exercises can strengthen the abdominal wall, they cannot eliminate the loose skin. The only permanent medical solution is a panniculectomy, a functional surgery often covered by insurance, whereas a tummy tuck is a cosmetic procedure used for muscle repair.
Table of Contents
You finally reached your goal weight or welcomed your new baby into the world. You expected to feel lighter and more confident. Yet the mirror reflects something you did not expect. Instead of the flat stomach you worked for, you see a dense fold of skin hanging low. It might cover your underwear line. In more severe cases, it might rest heavily on your thighs. This is not just stubborn fat. This is an anatomical reality for millions of people.
It can be incredibly frustrating to put in the work to lose weight only to feel like your body is hiding your progress. You might deal with rashes that never seem to heal. You might suffer from back pain that makes standing difficult. You likely feel the emotional exhaustion of trying to find clothes that fit a body shape that feels foreign to you.
Understanding what is happening under the surface is the first step to reclaiming your comfort. This is not a failure of willpower. It is not a sign that you simply need to do more crunches. It is a structural condition involving skin elasticity, connective tissue, and tissue weight. This comprehensive guide breaks down exactly what an apron belly is, why it happens, and the specific medical and non-surgical paths to fixing it.
The Core Concept: Anatomy of an Apron Belly
Many people confuse an apron belly with general obesity. While they can coexist, they are distinct medical issues. General abdominal obesity usually involves visceral fat. This is the hard, dangerous fat stored deep around the organs which pushes the stomach wall outward. An apron belly, medically known as an abdominal panniculus, is largely characterized by gravity and skin laxity.
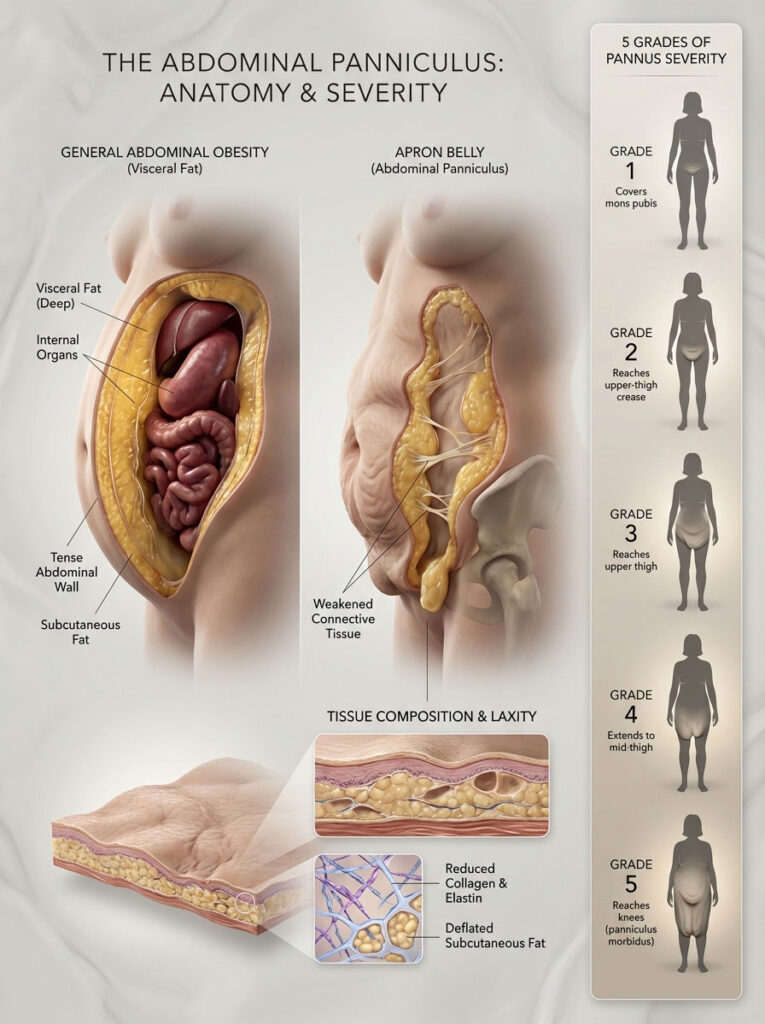
It occurs when the skin and subcutaneous fat in the lower abdomen lose their structural integrity. The connective tissues that usually hold the skin tight against the muscle wall weaken or snap. Instead of holding tight, the tissue succumbs to gravity and hangs downward. This creates an “apron” of flesh that hangs over the pubis.
In many cases, specifically after rapid weight loss from bariatric surgery or the use of GLP-1 medications, the apron may feel empty or deflated. The fat volume is gone, but the excess skin remains. This loose skin lacks the collagen and elastin required to snap back into place. It effectively becomes a deflated balloon that cannot shrink on its own.
The 5 Grades of Pannus Severity
Doctors and plastic surgeons do not just look at an apron belly as “big” or “small.” They use a clinical grading system to determine the severity. This grading is critical because insurance companies often use it to decide if they will pay for a panniculectomy. Understanding where you fall on this scale is vital for your treatment plan.
- Grade 1: The pannus covers the hairline and the mons pubis but does not extend to the genitals. This is considered mild belly overhang. It is often purely cosmetic but can still cause difficulty with clothing fit.
- Grade 2: The fold extends to cover the genitals and reaches the crease of the upper thigh. This is the pivotal grade. It is often the minimum threshold for insurance coverage regarding medical necessity. At this stage, skin-on-skin friction becomes a daily issue.
- Grade 3: The apron hangs down to the upper thigh. The weight of the tissue often causes significant back pain at this stage. The physical drag on the lower spine is constant.
- Grade 4: The pannus extends to the mid-thigh. This level of severity often requires specialized clothing or support garments simply to walk comfortably.
- Grade 5: The pannus hangs to the knees or below. This severe condition is known as panniculus morbidus. It can severely impact lymphatic drainage, leading to lymphedema, and can make walking or standing for long periods nearly impossible.
Primary Causes of Apron Stomach
Understanding the root cause helps manage expectations for treatment. It is rarely just one factor but rather a combination of biological events that compromise the skin’s structure.
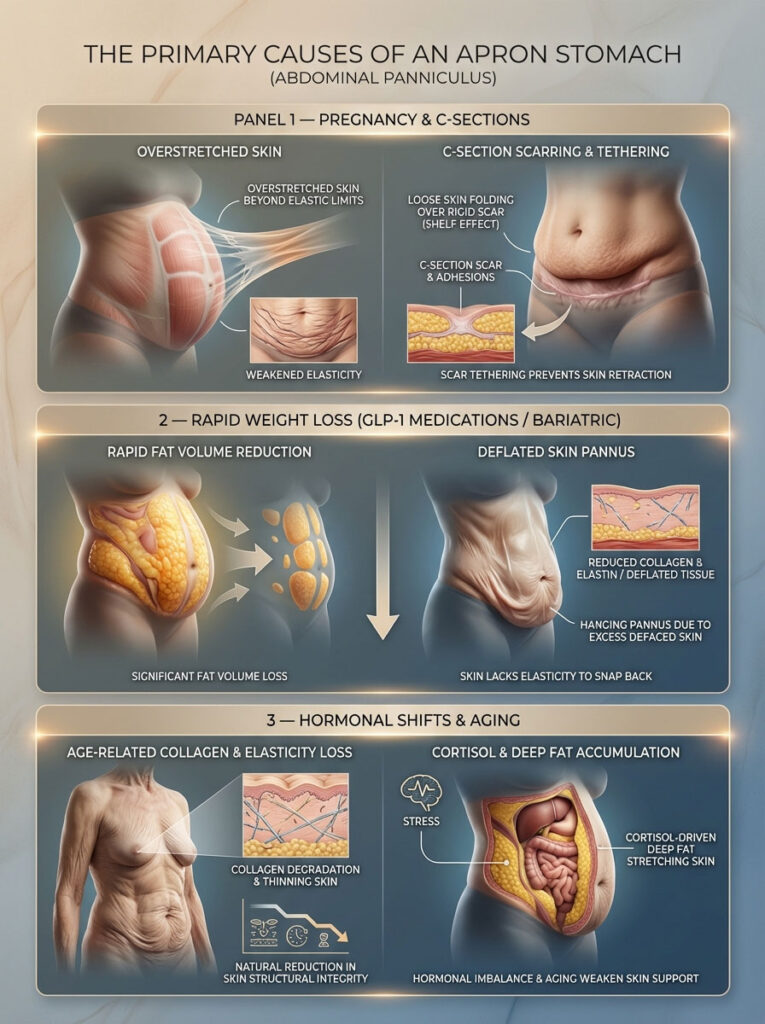
Pregnancy and C-Sections
During pregnancy, the abdominal skin stretches rapidly to accommodate the growing baby. For many women, this stretching exceeds the skin’s elastic limit. It is similar to an overstretched rubber band that does not return to its original size. After delivery, many women develop what is colloquially called a “mother’s apron.”
If you had a Cesarean section, the mechanics are even more complex. The C-section scar creates a tethering effect. The scar tissue adheres tightly to the abdominal muscle wall, but the loose skin and fat above the scar remain mobile. This creates a shelf-like overhang distinct from general belly fat. The tissue above flops over the rigid scar, accentuating the appearance of the apron even if the volume of fat is low.
Rapid Weight Loss (The “Ozempic Body”)
We are seeing a massive surge in apron belly cases due to the popularity of GLP-1 agonists like Ozempic, Wegovy, and Mounjaro. These medications cause rapid and significant weight reduction. When you undergo rapid weight loss, fat cells shrink much faster than the skin can tighten.
Skin elasticity depends on proteins called collagen and elastin. If you lose 50 or 100 pounds in a few months, your skin cannot produce enough elastin to shrink around your new, smaller frame. You are left with the surface area of your previous weight. This results in a deflated, hanging pannus that can be psychologically distressing for patients who thought weight loss would solve their body image issues.
Hormonal Shifts and Aging
As we age, our bodies produce less collagen. This accelerates during menopause when estrogen levels drop. Estrogen plays a key role in maintaining skin thickness and moisture. When it declines, the skin on the abdomen becomes thinner, crepey, and less able to fight gravity.
Simultaneously, high levels of cortisol, the stress hormone, can lead to fat redistribution. Cortisol receptors are dense in the abdominal area. High stress encourages fat storage in the deep abdomen, which stretches the skin further. Combined with age-related elasticity loss, this creates the perfect storm for a sagging lower belly.
Health Risks: More Than Just Cosmetic
While many people want to remove an apron stomach for aesthetic reasons, the medical implications are serious. An untreated pannus can lead to a cycle of physical, dermatological, and psychological complications.
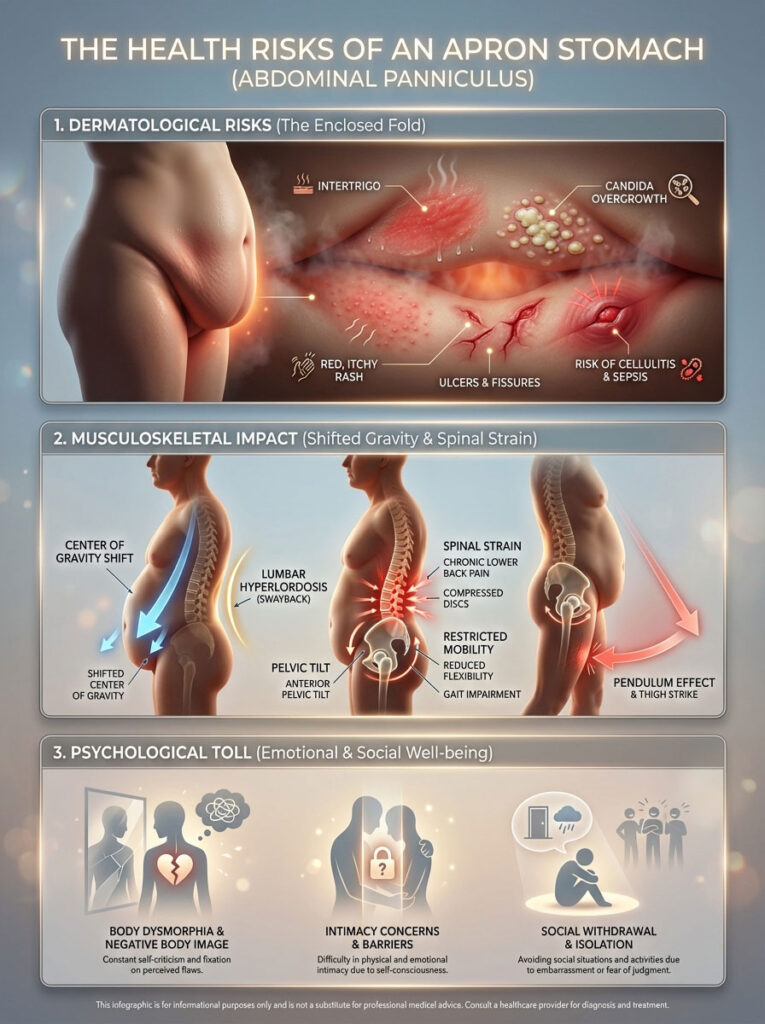
Dermatological Issues and Rashes
The most common complaint from patients with an abdominal panniculus is intertrigo. This is a chronic inflammatory rash that develops in skin folds. The area under the apron is a dark, warm, and moist environment. It lacks airflow, creating the perfect breeding ground for bacteria and yeast, specifically Candida.
If you constantly notice a red, raw, or itchy rash under your belly, you are likely dealing with a fungal infection. These rashes can smell unpleasant and be painful to the touch. In severe cases, the skin can break down into open ulcers or fissures. This allows bacteria to enter the bloodstream, leading to a risk of cellulitis, a serious skin infection that requires antibiotics, or even sepsis in extreme cases of neglect.
Musculoskeletal Impact
The weight of the excess tissue alters your center of gravity. A large pannus acts as a dead weight pulling the front of your pelvis down. To compensate, you unconsciously arch your lower back. This pulls the lumbar spine forward, leading to a condition called hyperlordosis or swayback.
This constant strain causes chronic lower back pain that no amount of stretching can fix because the mechanical trigger remains. Furthermore, the physical bulk of the hanging belly can restrict movement. It creates a pendulum effect when you walk or run. The swinging weight strikes the thighs, making exercise uncomfortable or even painful. This creates a vicious cycle where the inability to move makes maintaining weight loss even harder.
Psychological and Emotional Toll
The mental health impact of an apron belly is profound. Many patients report feelings of body dysmorphia. They may feel a disconnect between their healthy habits and their physical appearance. The condition can impact intimacy, as patients may feel self-conscious unclothed. The difficulty in finding clothes that fit can lead to social withdrawal. Recognizing that this is a medical condition, not a vanity issue, is crucial for mental well being.
Surgical Solutions: The Only Permanent Fix
It is important to be direct about treatment. While lifestyle changes improve overall health, surgery is the only method to physically remove significant amounts of excess skin. There are two primary procedures, and confusing them could cost you thousands of dollars or lead to unsatisfactory results.
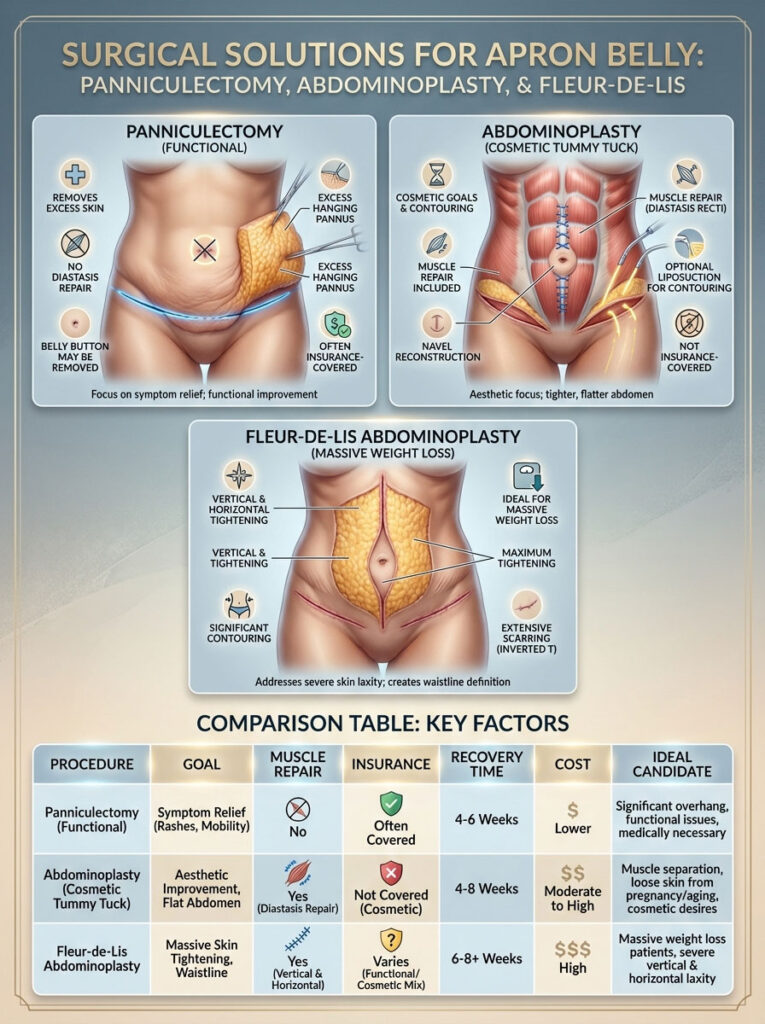
Procedure 1: Panniculectomy (The Functional Fix)
A panniculectomy is strictly a functional procedure. It is designed to cure the medical symptoms associated with the apron.
How it is performed:
The surgeon makes a horizontal incision across the lower abdomen, typically from hip bone to hip bone. They then excise, or cut away, the hanging apron of skin and fat. The remaining skin is pulled down and sutured closed.
The Goal:
The goal here is not to give you a sculpted, hourglass waistline. The goal is to relieve the physical burden of the pannus. During a panniculectomy, the surgeon does not tighten the abdominal muscles. They typically do not reposition or reconstruct the belly button; in some cases, the belly button may be removed entirely if it sits on the skin being excised. Because it treats medical issues like rashes and back pain, this procedure is frequently covered by health insurance.
Procedure 2: Abdominoplasty (The Cosmetic Tummy Tuck)
An abdominoplasty, or tummy tuck, is a comprehensive cosmetic surgery. It addresses the aesthetic appearance of the entire abdomen, not just the lower hang.
How it is performed:
Like a panniculectomy, it involves an incision and skin removal. However, the surgeon also repairs the abdominal wall. They use permanent sutures to stitch the rectus abdominis muscles back together, fixing diastasis recti. This acts like an internal corset to flatten the stomach profile. The surgeon also creates a new opening for the belly button, positioning it naturally on the tightened abdomen. Liposuction is often used to contour the waist and flanks.
The Goal:
This surgery creates a flat, contoured stomach and a narrowed waist. However, because muscle repair is considered aesthetic rather than medically necessary, insurance rarely covers it. Patients usually pay for a tummy tuck entirely out of pocket.
Procedure 3: Fleur-de-Lis Abdominoplasty
For patients who have experienced massive weight loss, such as losing 100 pounds or more, a standard horizontal incision might not be enough. These patients often have excess skin that wraps horizontally around the torso as well as hanging vertically.
A Fleur-de-Lis tummy tuck involves both a horizontal incision (like a standard tummy tuck) and a vertical incision running up the center of the abdomen. This allows the surgeon to pull the skin in from the sides, tightening the waistline significantly. The resulting scar looks like an inverted “T.” This procedure provides the most dramatic transformation for post-bariatric patients but leaves a more visible scar.
Comparison: Panniculectomy vs. Tummy Tuck
| Feature | Panniculectomy | Abdominoplasty (Tummy Tuck) |
| Primary Goal | Functional (Relieve pain, rashes, mobility issues) | Cosmetic (Aesthetics, sculpting, waist definition) |
| Muscle Repair | No (Does not fix Diastasis Recti) | Yes (Tightens abdominal wall separation) |
| Insurance Coverage | Yes (If medical necessity criteria are met) | No (Considered elective/cosmetic) |
| Recovery Time | 4–6 Weeks | 6–8 Weeks (More intense due to muscle repair) |
| Average Cost (USA) | 8,000–8,000–15,000 (Often covered by insurance) | 6,000–6,000–12,000 (100% Out of pocket) |
| Belly Button | Often removed or preserved without sculpting | Reconstructed and sculpted for natural look |
| Liposuction | Rarely included | Often included for contouring |
| Ideal Candidate | Patients with Grade 2+ pannus and chronic health issues | Moms or weight loss patients wanting a flat stomach |
The Recovery Timeline: What to Expect
Recovery from abdominal surgery is a significant journey. Understanding the timeline helps you prepare your home and your mind.
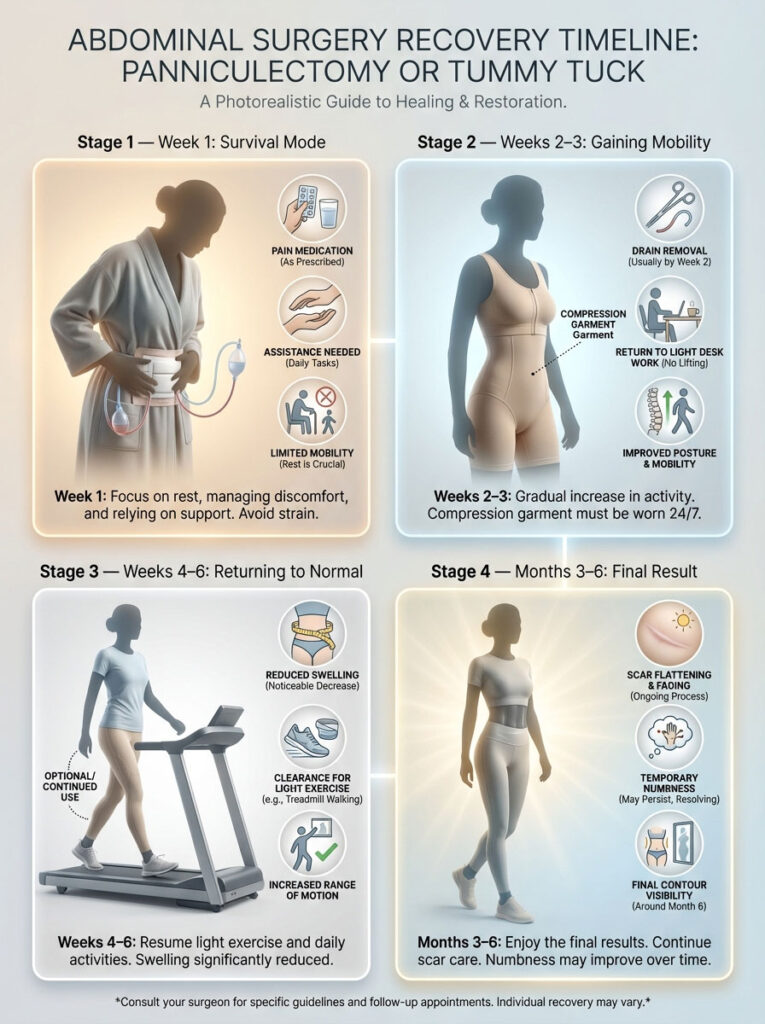
Week 1: Survival Mode
The first few days are the hardest. You will likely have surgical drains—small tubes that remove fluid from the incision site to prevent swelling. You will need to walk hunched over to protect the incision. You will need help getting out of bed and managing basic tasks. Pain medication is usually required.
Weeks 2–3: Gaining Mobility
The drains are usually removed during this window. You can stand a bit straighter but must still wear a compression garment 24/7. This garment helps minimize swelling and supports the healing tissues. Most patients can return to a desk job by the end of week 2 or 3, provided they do not have to lift anything heavy.
Weeks 4–6: returning to Normal
Swelling begins to subside significantly. You may be cleared for light exercise, such as walking on a treadmill. You can stop wearing the compression garment around the clock, though many patients prefer to keep wearing it for comfort.
Months 3–6: The Final Result
It takes several months for the residual swelling to completely resolve and for the scar to flatten. Numbness around the incision line is common and may take up to a year to improve. By month 6, you are typically seeing your final contour.
Financials: Insurance, Costs, and Requirements (USA Context)
Navigating insurance coverage for apron belly removal can be one of the most confusing aspects of the journey. In the United States, carriers like Blue Cross Blue Shield, Aetna, UnitedHealthcare, and Medicare have strict, specific definitions for “medical necessity.”
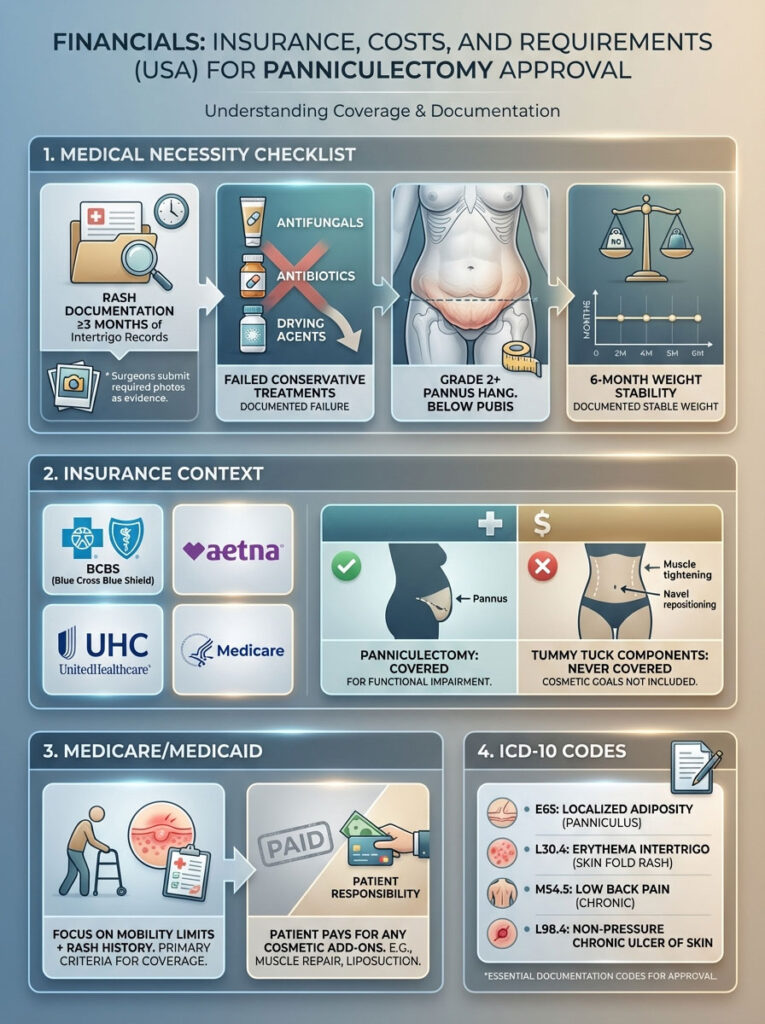
The “Medical Necessity” Checklist
To get approved for a panniculectomy, you cannot simply show up and ask for surgery. You need to build a case file. Insurance companies want proof that this is a health issue, not a cosmetic desire. Most 2025 policy guidelines require the following documentation:
- Documentation of Rashes: You must have medical records showing recurrent cases of intertrigo or skin breakdown. Crucially, these records must usually span at least 3 months. This means you need to visit your primary care doctor or dermatologist multiple times to have the rash formally diagnosed and treated.
- Failure of Conservative Treatment: Your records must show that you tried lower-cost treatments and they failed. This includes prescription antifungal creams (like Nystatin), oral antibiotics, or drying agents. If the rash keeps coming back despite these treatments, surgery becomes the next logical step.
- The “Hang” Severity: The pannus must hang below the pubis (Grade 2 or higher). Photos are often required for authorization. The surgeon will take these photos during your consultation.
- Weight Stability: You must have maintained a stable weight for at least 6 months. Fluctuating weight increases the risk of surgical complications. If you had bariatric surgery, many insurers require you to be 18 months post-op to ensure your weight loss has plateaued and your nutrition levels are stable.
Medicare and Medicaid Specifics
Medicare coverage for panniculectomy is possible but very strict. They focus heavily on functional impairment. If the apron stomach prevents you from walking, working, or performing daily activities, and you have the rash documentation, coverage is likely. However, Medicare will never pay for the “add-on” cost of muscle tightening found in a tummy tuck. That portion of the bill would be entirely your responsibility.
Medical Codes for Your Doctor
When visiting your dermatologist or primary care physician to document your condition, ask them to ensure the correct ICD-10 codes are in your chart. This signals to the insurance company that this is a medical issue, not a vanity visit.
- E65: Localized adiposity.
- L30.4: Erythema intertrigo.
- M54.5: Low back pain (if the weight is affecting your spine).
- L98.4: Non-pressure ulcer of skin (if you have open sores).
Non-Surgical Management: Treating the Symptoms
Surgery is a major decision involving anesthesia, recovery time, and risk. It is not accessible to everyone immediately. If you are not ready for a panniculectomy, or if you are currently pregnant or planning more children, you need effective management strategies to live comfortably.
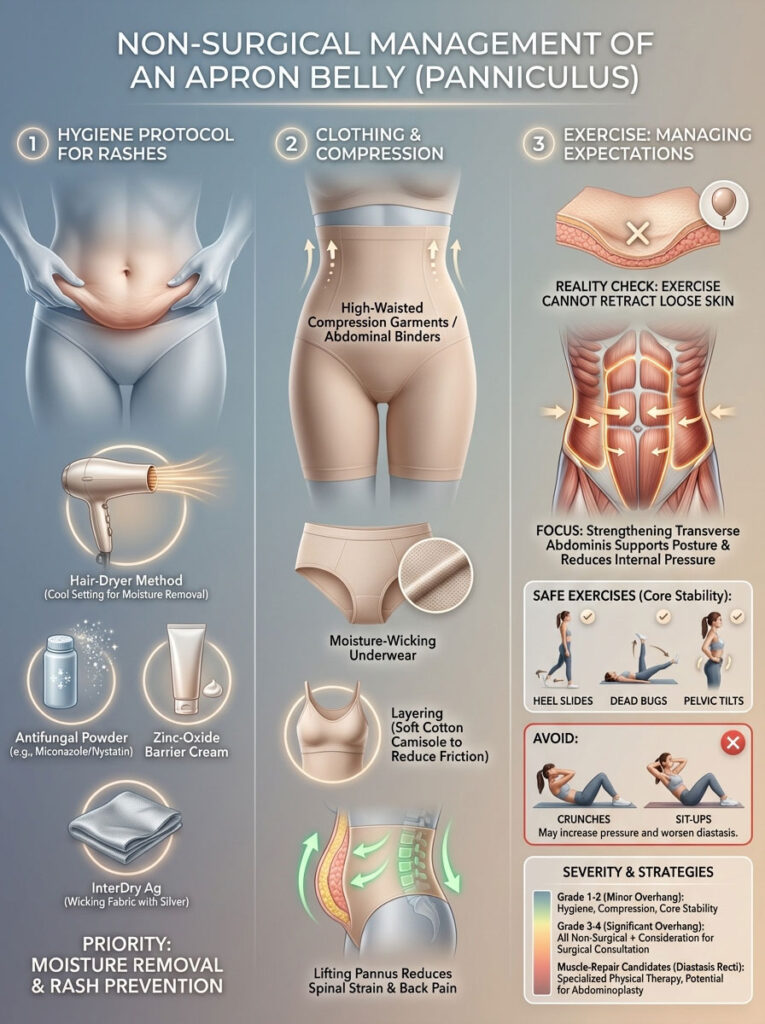
Hygiene Protocol for Rashes
The goal of hygiene management is to eliminate moisture. Fungal infections thrive on damp skin.
- The Hair Dryer Method: After showering, do not just towel dry. Towels can be abrasive and might not reach deep into the crease. Lift the apron belly and use a hair dryer on a cool or warm setting to ensure the skin fold is completely dry before getting dressed.
- Antifungal Powders: Apply a powder containing miconazole or Nystatin. Avoid cornstarch, as it can sometimes feed bacteria or clump up, causing more irritation.
- Barrier Creams: Use a cream containing zinc oxide (commonly found in diaper rash creams). This creates a waterproof barrier that protects the skin from sweat and friction.
- InterDry Fabric: Ask your doctor about antimicrobial fabric strips containing silver. These are placed between the skin folds to wick away moisture and kill bacteria.
Clothing and Compression
The right clothing makes a massive difference in daily comfort and confidence.
- Support Garments: High-waisted compression garments or abdominal binders can provide lift. By physically lifting the pannus, you relieve the downward strain on your lower back.
- Fabric Choice: For daily wear, choose moisture-wicking underwear (like bamboo or performance cotton) that sits high on the waist. Avoid low-rise jeans or underwear with thin elastic bands that cut into the midsection, as they can cause irritation or bleeding where the skin hangs.
- Layering: Wear a soft cotton camisole tucked inside your underwear to create a buffer layer between the skin of the belly and the skin of the pubic area.
Can Exercise Help? (Managing Expectations)
This is the most common and hopeful question: “What core exercises get rid of an apron belly?”
You need to know the medical truth to avoid disappointment. Exercise cannot retract loose skin. No amount of planks, sit-ups, or cardio will make a Grade 2 pannus disappear. Skin does not have muscle fibers that can be “flexed” back into tightness.
However, exercise is still vital for your quality of life. Strengthening the deep core muscles, specifically the Transverse Abdominis, acts like an internal corset. This muscle wraps around your spine and abdomen. When it is strong, it pulls the abdominal wall inward, reducing the protrusion of visceral fat. This might make the apron appear slightly smaller or hang less aggressively because the internal pressure is reduced.
Effective Exercises:
- Heel Slides: Lie on your back and slowly slide one heel out and back while keeping your core engaged. This activates the deep core without bulging the stomach.
- Dead Bugs: This is a safe way to work the core and coordination without flexing the spine or putting pressure on the neck.
- Pelvic Tilts: These help correct the swayback posture caused by the belly’s weight, relieving lower back pain.
Exercises to Avoid:
- Crunches and Sit-ups: If you have diastasis recti (muscle separation) from pregnancy, these exercises can cause your belly to “cone” or bulge outward. This can potentially worsen the appearance of the lower abdomen and widen the muscle gap.
Treatment Options by Severity Table
| Condition Severity | Recommended Strategy | Expected Outcome |
| Grade 1 (Minor Hang) | Diet, Core Exercise, Shapewear | Visceral fat reduction may retract the profile slightly; shapewear smooths the silhouette. |
| Grade 2 (Genital Coverage) | Hygiene regimen, Compression garments | Symptom relief for rashes and back pain; skin will not retract naturally. |
| Grade 2+ (With Rashes) | Panniculectomy (Insurance) | Complete removal of the overhang; permanent resolution of rashes and hygiene issues. |
| Muscle Separation (Bulge) | Tummy Tuck (Cosmetic) | Flat, sculpted stomach; narrowed waistline; core strength restored via muscle repair. |
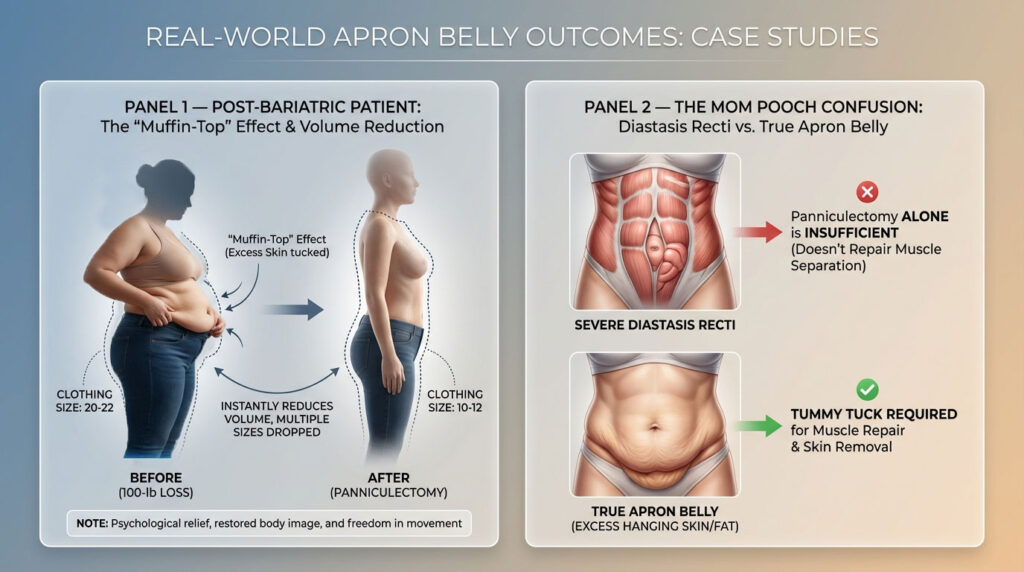
Case Studies and Real-World Context
To understand the impact of treatment, it helps to look at real-world scenarios.
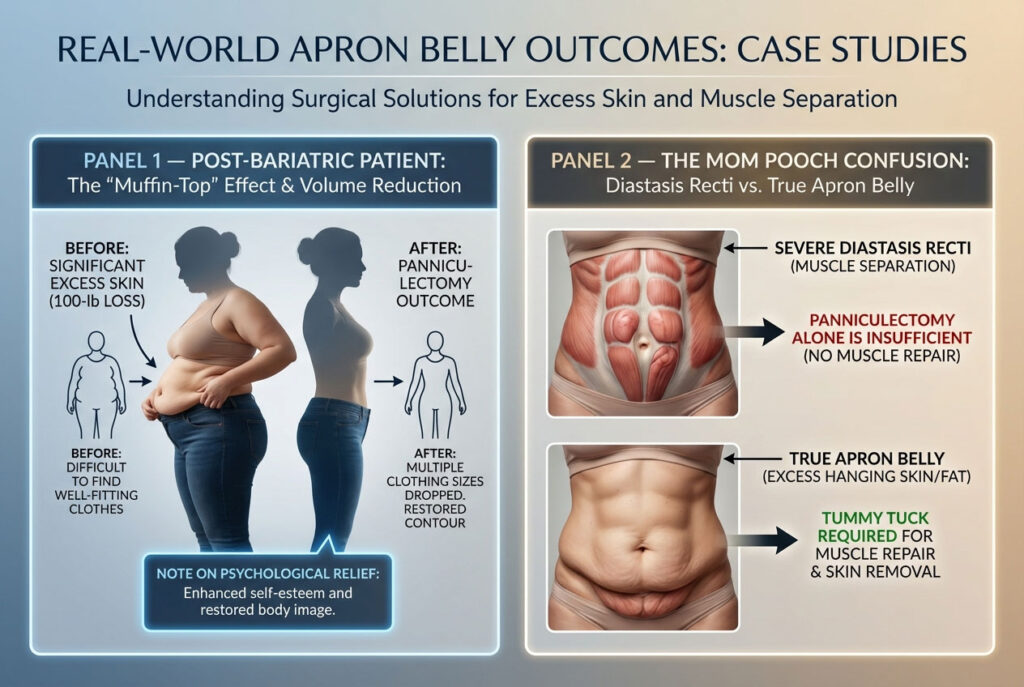
The Post-Bariatric Patient
Consider a patient who has lost 100 pounds through gastric bypass. They feel lighter and healthier, yet they still wear the same size pants. Why? Because they have to fold and tuck the excess skin inside the waistband. This creates a “muffin top” effect that isn’t fat, but skin. For these patients, a panniculectomy changes their clothing size instantly. They might drop three sizes in one day, not by weight loss, but by volume removal. The psychological relief of finally seeing the body they worked for is immeasurable.
The “Mom Pooch” Confusion
Many mothers believe they have an apron stomach when they actually have severe diastasis recti. Their muscles are so separated that the internal organs push forward, looking like a hang. In this specific instance, a panniculectomy alone might yield disappointing results because the belly will still bulge forward. A tummy tuck is the correct fix here because the issue is muscular integrity, not just skin depth.
Summary and Key Takeaways
Living with an apron belly is physically and emotionally taxing, but it is a treatable medical condition. It is not a sign that you failed your diet. It is often a matter of biomechanics and skin elasticity that are out of your control.
Your Action Plan:
- Assess the Grade: Determine if your pannus is Grade 1 or Grade 2 to understand your insurance eligibility. Use a mirror to see if the hang covers the pubic area.
- Document Everything: If you want insurance to cover a panniculectomy, start visiting your doctor for rash treatments now. Do not self-treat at home without a record. Build that paper trail of medical necessity.
- Manage the Symptoms: Use the hair dryer trick, antifungal powders, and compression garments to prevent infection and pain while you wait for a permanent solution.
- Consult an Expert: Speak to a board-certified plastic surgeon. Ask them specifically if you are a candidate for a functional removal or if you require a cosmetic tummy tuck to achieve your goals.
Frequently Asked Questions
Is apron belly just fat or loose skin?
It is usually a combination of both. The “hang” is primarily caused by loose skin losing its elasticity and succumbing to gravity. However, the volume inside the apron may consist of subcutaneous fat, or visceral fat pushing the abdominal wall forward. In post-weight loss patients, it is often mostly empty skin.
How can I hide my apron belly in jeans?
Look for high-rise jeans with a rigid front panel, often labeled as “tummy control” or “sculpting.” Avoid low-rise cuts. Pair these with high-waisted compression underwear or a smoothing bodysuit. This prevents the “shelf” effect where the belly hangs over the waistband.
Will Medicare pay for apron belly removal?
Yes, Medicare may cover a panniculectomy if strict criteria are met. The pannus must hang below the pubic bone (Grade 2), and you must provide medical records showing chronic skin infections (intertrigo) that have not healed after 3 months of prescribed treatment.
Can I get a panniculectomy and a tummy tuck at the same time?
Yes, this is very common. However, insurance will typically only pay for the panniculectomy portion of the surgery (the skin removal). You will likely have to pay an “upgrade fee” out of pocket to cover the muscle repair, belly button reconstruction, and liposuction involved in the tummy tuck.
Does losing weight make apron belly go away?
Losing weight reduces the fat inside the apron, but it often makes the skin hang lower because it becomes “deflated.” The skin itself rarely shrinks back significantly, especially if the hanging is due to pregnancy stretch marks or massive weight loss.
What is the best exercise for apron belly?
Low-impact core stability exercises like Dead Bugs, Bird-Dogs, and Heel Slides are best. They strengthen the deep Transverse Abdominis muscle without straining the back. Avoid standard sit-ups, as they can worsen muscle separation and increase intra-abdominal pressure.
How painful is apron belly surgery?
A panniculectomy (skin removal only) is generally less painful than a tummy tuck (muscle repair). The skin incision burns and feels tight, but muscle repair feels like a deep, intense internal bruise. Most panniculectomy patients can return to light desk work within 2 to 3 weeks, whereas muscle repair recovery can take 6 to 8 weeks.
What causes the “C-section shelf”?
The scar from a Cesarean section creates a tight band of rigid, non-elastic tissue that adheres to the abdominal wall. The looser, softer skin and fat above the scar flop over this tight band, creating a distinct shelf-like appearance that mimics an apron stomach.
Are there creams to tighten apron belly skin?
No topical cream can retract significant amounts of hanging skin. While creams containing retinol, caffeine, or hyaluronic acid may slightly improve skin texture and hydration, they cannot lift a heavy pannus. They do not penetrate deeply enough to repair the torn dermis.
What is the difference between FUPA and apron belly?
“FUPA” is a slang term referring to fat accumulation specifically over the pubic bone area (mons pubis). Apron belly refers to the abdominal skin and fat from the stomach hanging down to cover the pubic area. They are anatomically different areas, though an apron belly often hides the pubic area.
How do I prevent rashes under my apron belly?
The key is keeping the area dry. After washing, lift the fold and dry the skin thoroughly using a towel or a hair dryer on a cool setting. Apply an antifungal powder (like Zeasorb) or place a cotton liner or “InterDry” fabric between the skin folds to absorb moisture and prevent skin-on-skin friction.
Can Ozempic cause an apron belly?
Indirectly, yes. Rapid weight loss from GLP-1 drugs like Ozempic, Wegovy, or Mounjaro can leave you with significant excess skin. If you carry weight in your midsection, losing that volume quickly often results in an apron belly because the skin does not have time to retract naturally.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Insurance policies vary by provider and state. Always consult with a board-certified plastic surgeon and your insurance representative to verify coverage and eligibility for surgical procedures.
References:
- American Society of Plastic Surgeons. (2024). Panniculectomy vs. Abdominoplasty: Understanding the Differences.
- Journal of Plastic, Reconstructive & Aesthetic Surgery. (2023). Functional outcomes of abdominal panniculectomy in post-bariatric patients.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2024). Health Risks of Overweight & Obesity: Understanding Skin Manifestations.
- Dermatology Times. (2024). Management of Intertrigo in Obese Patients.