It starts with a sharp, breath-stealing pain under your right ribcage that radiates to your back or shoulder blade. It is not just a stomach ache; it is a visceral signal that something in your digestive engine has stalled.
Or perhaps the surgery is already behind you. The offending organ is gone, sitting in a pathology lab, but you are now staring at a hospital menu or your own refrigerator with a new kind of fear. You are wondering if eating a simple scrambled egg will send you running to the bathroom with urgency you can’t control.
Table of Contents
The anxiety surrounding food when you have gallbladder issues is paralyzing. Whether you are navigating life with active gallstones or adjusting to a no gallbladder diet after a cholecystectomy, your relationship with food has fundamentally changed. You need more than generic advice to “eat healthy.” You need to understand the mechanics of your new digestive reality.
This guide provides a comprehensive, deeply researched 7-Day Gallbladder Meal Plan. It covers the two distinct, critical phases of your journey with specific medical nutritional therapy strategies.
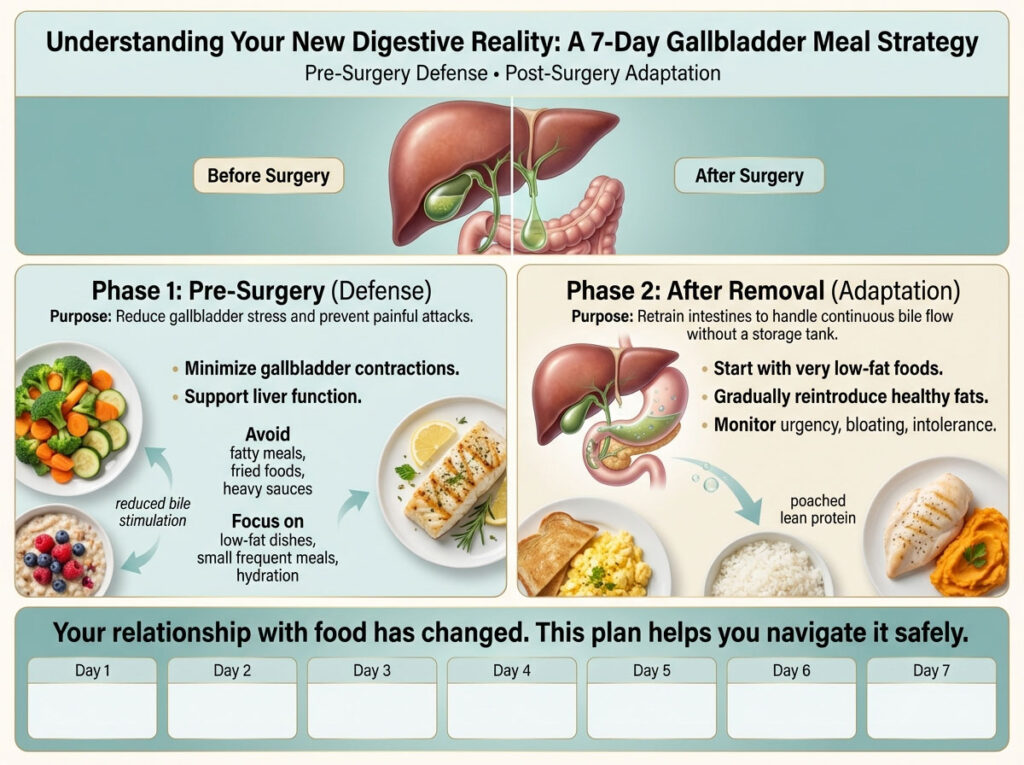
First is the “Pre-Surgery” phase, where our focus is defense: preventing painful attacks and preparing the liver.
Second is the “After Removal” phase, where we focus on adaptation: retraining your intestines to handle continuous bile flow without a storage tank.
Quick Navigation:
- Waiting for Surgery? Jump to Part 1: Pre-Surgery Gallbladder Diet Plan
- Recovering from Surgery? Jump to Part 2: Post-Cholecystectomy Recovery Diet
Understanding Digestion Anatomy: How Gallbladder Removal Changes Bile Flow
Think of your liver as a chemical factory that produces bile. Bile is a greenish-yellow fluid that acts as a detergent (emulsifier). Just as dish soap breaks down grease on a frying pan, bile breaks down the fats you eat so your body can absorb vitamins A, D, E, and K.
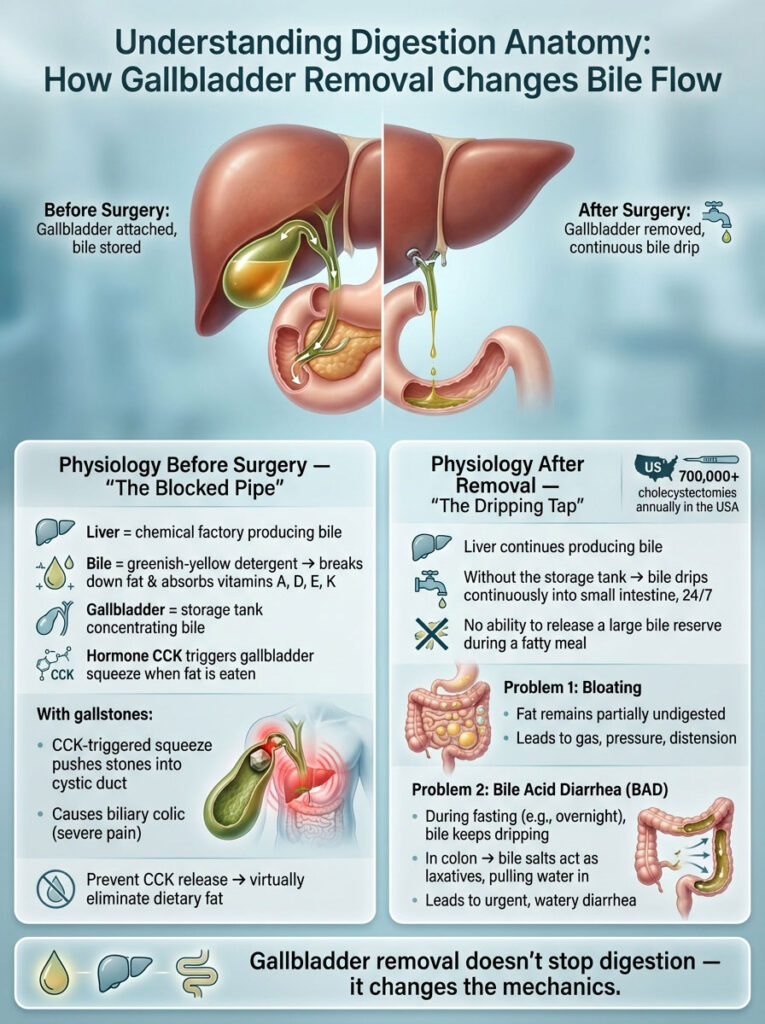
The Physiology Before Surgery: The Blocked Pipe
In a healthy system, the gallbladder acts as a storage tank. When you are fasting (between meals), the liver trickles bile into this tank, where it is concentrated and stored. When you eat fat, a hormone called Cholecystokinin (CCK) signals the gallbladder to squeeze.
If you have gallstones, this squeeze is the enemy. The gallbladder contracts, pushing a stone against the sensitive cystic duct. This causes biliary colic—the agonizing pain you know too well. Your dietary goal in this phase is to stop the CCK hormone from triggering that squeeze. The only way to do that is to virtually eliminate dietary fat.
The Physiology After Removal: The Dripping Tap
Surgeons perform approximately 700,000 cholecystectomies annually in the USA alone. Once the “storage tank” is removed, your liver does not stop making bile. However, instead of being stored and concentrated, the bile now drips continuously into your small intestine, 24 hours a day.
This creates two distinct problems:
- Bloating: When you eat a large fatty meal, you no longer have a “reserve” of concentrated bile to release all at once. The fat remains undigested, leading to gas and bloating.
- Bile Acid Diarrhea (BAD): When you are fasting (like while sleeping), bile keeps dripping into an empty intestine. Bile salts act as a laxative in the colon, drawing water in and causing urgent, watery diarrhea.
The following 7-day gallbladder meal plan is engineered to solve both specific physiological problems.
Part 1: Pre-Surgery Gallbladder Diet Strategies to Prevent Attacks
If you are waiting for surgery, you are likely in survival mode. You are not trying to “heal” the gallbladder—gallstones do not dissolve with diet alone—you are trying to keep the organ dormant.
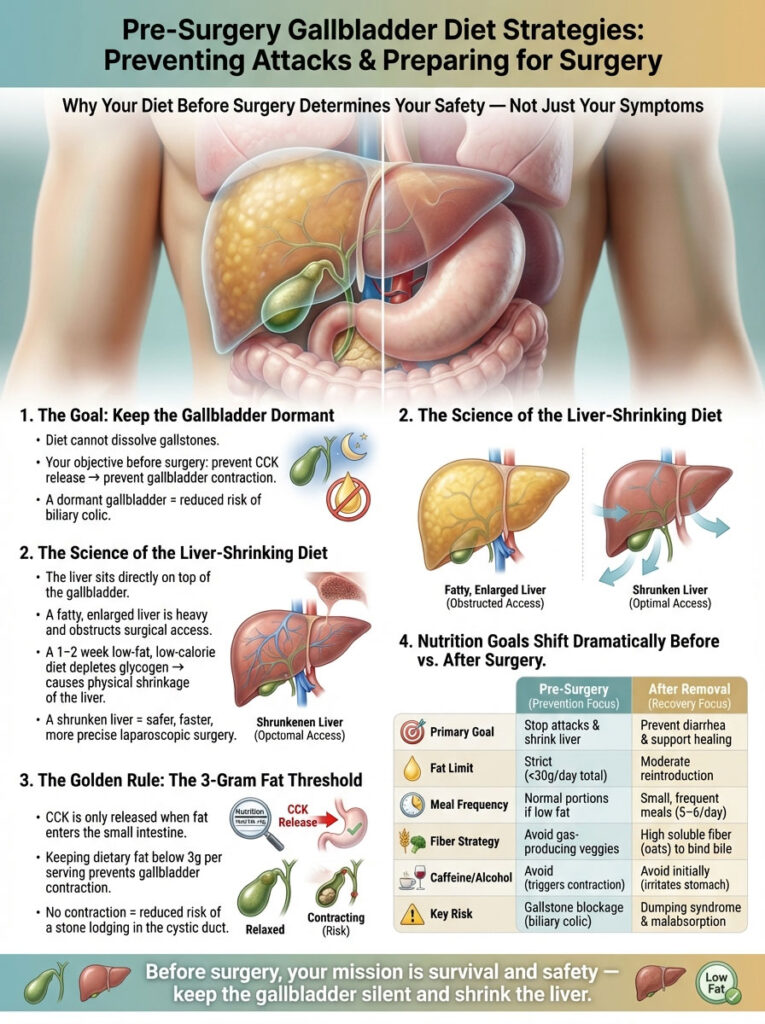
The Science of the “Liver Shrinking Diet”
Your surgeon may have explicitly placed you on a “Liver Shrinking Diet” prior to your operation. This is critical for safety, not just weight loss. The liver sits directly on top of the gallbladder. If the liver is fatty and enlarged, it is heavy and difficult for the surgeon to lift up to access the gallbladder during laparoscopic surgery.
By following a strict low-fat, low-calorie diet for 1-2 weeks pre-op, you deplete the liver’s glycogen stores, physically shrinking the organ and making your surgery safer and faster.
The Golden Rule: The 3-Gram Fat Threshold
Medical nutritional guidelines suggest keeping fat intake strictly below 3 grams per serving during the acute pre-op phase. This is the threshold usually required to prevent the release of Cholecystokinin. If the gallbladder does not sense significant fat, it will not contract, and the stone will hopefully remain settled away from the duct neck.
Below is a detailed comparison of how your nutritional goals shift during this journey. It is vital to understand that “Healthy Eating” means two different things depending on whether you still have the organ or not.
| Feature | Pre-Surgery (Prevention Focus) | After Removal (Recovery Focus) |
| Primary Goal | Stop attacks (pain) & shrink liver size. | Prevent diarrhea (urgency) & aid incision healing. |
| Fat Limit | Strict Limit (<30g/day total). | Moderate Reintroduction (<30% of total calories). |
| Meal Frequency | Normal portions permitted if low fat. | Small, Frequent Meals (5–6/day) are mandatory. |
| Fiber Strategy | Avoid gas-producing veggies (bloating). | High Soluble Fiber (Oats) to bind excess bile. |
| Caffeine/Alcohol | Avoid (Triggers contraction). | Avoid initially (Irritates empty stomach lining). |
| Key Risk | Gallstone blockage (Biliary Colic). | Dumping syndrome & Malabsorption. |
7-Day Pre-Surgery Meal Plan: The “Keep it Calm” Menu for Pain Prevention
This specific menu is designed for patients waiting for surgery. It is ultra-low-fat to keep the gallbladder dormant.
Dietary Preparation Note: Do not use oil, butter, or margarine in these recipes. Use water, vegetable broth, or non-stick cooking spray to sauté vegetables. Even “healthy” fats like olive oil or avocado can trigger an attack right now.
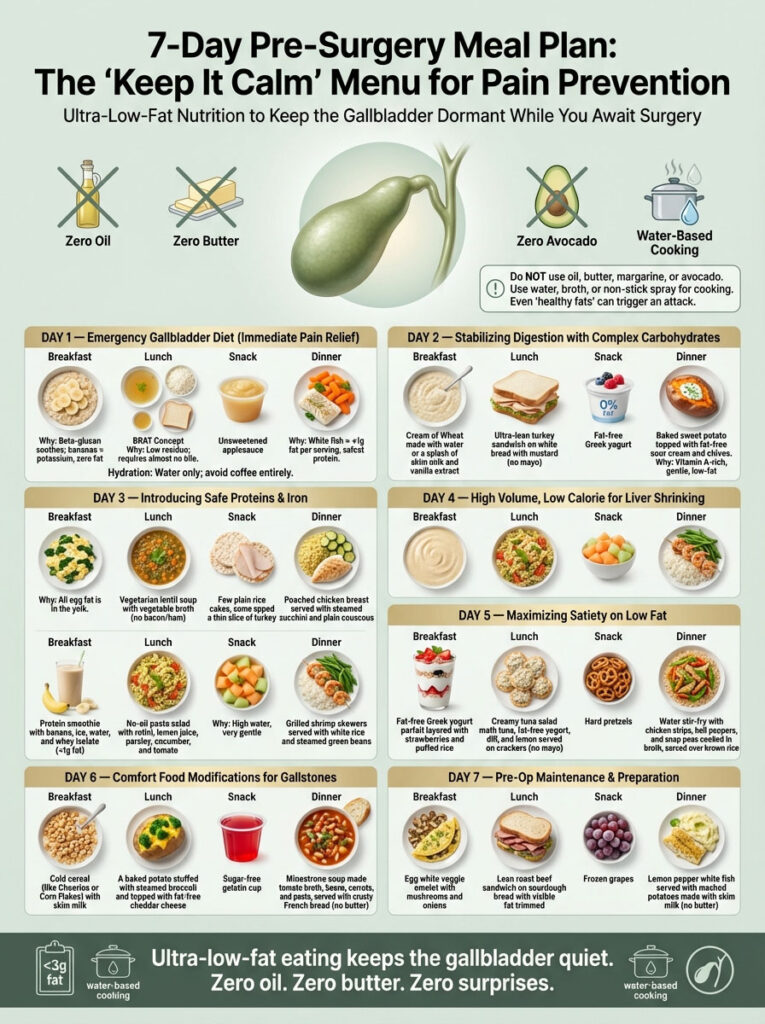
Day 1 Menu: Emergency Gallbladder Diet for Immediate Pain Relief
If you recently had an attack, your system is inflamed. This day focuses on liquids and gentle solids to reduce inflammation.
- Breakfast:Water-Based Oatmeal. Cook ½ cup of rolled oats with water. Top with a sliced banana.
- Why this works: Oats contain beta-glucan, a soluble fiber that is soothing, while bananas provide potassium without any fat.
- Lunch:The BRAT Concept. A bowl of clear chicken broth with white rice and a slice of white toast.
- Why this works: White rice is low-residue and very easy to digest, requiring almost no bile to process.
- Snack: ½ cup of unsweetened applesauce.
- Dinner:Steamed White Fish. 4oz of Cod, Tilapia, or Flounder. Season with lemon juice and dill. Serve with boiled carrots.
- Why this works: White fish is the leanest protein source available (less than 1g fat per serving).
- Hydration: Sip water throughout the day. Avoid coffee entirely today.
Day 2 Menu: Stabilizing Digestion with Complex Carbohydrates
- Breakfast: Cream of Wheat. Prepared with water or a splash of skim milk. Add a drop of vanilla extract for flavor.
- Lunch: Turkey Mustard Sandwich. 3 slices of ultra-lean deli turkey breast on white bread with yellow mustard. Strictly no mayonnaise.
- Snack: Fat-Free Yogurt. Check the label to ensure it is truly 0% fat. Greek yogurt is preferred for the higher protein content.
- Dinner:Loaded Sweet Potato. Baked sweet potato topped with fat-free sour cream and chives.
- Why this works: Sweet potatoes are nutrient-dense and high in Vitamin A, which supports mucous membrane health without taxing the gallbladder.
Day 3 Menu: Introducing Safe Proteins and Iron
- Breakfast:Egg White Scramble. Use 3 egg whites and a handful of spinach. Cook in a non-stick pan with zero-calorie cooking spray.
- Why this works: The fat in eggs is entirely in the yolk. The white is pure protein and safe.
- Lunch: Vegetarian Lentil Soup. Ensure it is made with vegetable broth and no ham hocks or bacon fat.
- Snack: Rice Cakes. Top with a thin slice of turkey breast or eat plain.
- Dinner: Poached Chicken Breast. Poach chicken in water with herbs. Serve with steamed zucchini and a side of plain couscous.
Day 4 Menu: High Volume and Low Calorie for Liver Shrinking
- Breakfast:Protein Smoothie. Blend ice, water, a banana, and a scoop of vanilla protein powder isolate.
- Check the label: Ensure the protein powder has <1g of fat per scoop. Whey Isolate is usually safer than Concentrate.
- Lunch: No-Oil Pasta Salad. Rotini pasta tossed with fresh lemon juice, fresh parsley, diced cucumbers, and cherry tomatoes. Season with salt and pepper.
- Snack:Melon Bowl. Cantaloupe or Honeydew melon.
- Why this works: Melons are high water content and gentle on the digestive tract.
- Dinner: Grilled Shrimp Skewers. Shrimp is naturally low in fat. Serve with plain white rice and steamed green beans.
Day 5 Menu: Maximizing Satiety on a Low Fat Diet
- Breakfast: Berry Yogurt Parfait. Fat-free Greek yogurt layered with sliced strawberries and ¼ cup of puffed rice cereal for crunch.
- Lunch: Creamy Tuna Salad (No Mayo). Mix one can of tuna (packed in water, drained) with 2 tablespoons of fat-free Greek yogurt, dill, and lemon. Serve on saltine crackers.
- Snack: Pretzels. A handful of hard pretzels (check label for fat content, usually very low).
- Dinner: Water Stir-Fry. Sauté chicken breast strips, bell peppers, and snap peas using vegetable broth instead of oil. Serve over brown rice.
Day 6 Menu: Comfort Food Modifications for Gallstones
- Breakfast: Cold Cereal. A bowl of Cheerios or Corn Flakes with skim milk.
- Lunch: Stuffed Baked Potato. Large baked potato topped with steamed broccoli and a sprinkle of fat-free cheddar cheese.
- Snack: Sugar-Free Jello Cup.
- Dinner: Minestrone Soup. A clear tomato-based broth with kidney beans, pasta shells, and carrots. Serve with crusty French bread (no butter).
Day 7 Menu: Pre-Op Maintenance and Preparation
- Breakfast: Veggie Omelet. Egg whites folded over sautéed mushrooms and onions.
- Lunch: Roast Beef Sandwich. Use very lean roast beef, trim all visible white fat, and serve on sourdough bread with tomato slices.
- Snack: Frozen Grapes. A refreshing, zero-fat sweet treat.
- Dinner: Lemon Pepper Fish. Grilled white fish with a squeeze of fresh lemon. Side of mashed potatoes made with skim milk (no butter).
Part 2: Diet After Gallbladder Removal and the Recovery Timeline
Congratulations, the surgery is over. The immediate threat of stone blockage is gone.
However, your anatomy has changed. Your liver is now connected directly to your small intestine. This diet after gallbladder removal is designed to slowly retrain your intestines to handle bile.
The New Rule: Frequency is Key
You must eat 5 to 6 times a day. You can never let your stomach stay empty for too long, or bile will pool and irritate the lining. Conversely, you cannot eat a huge meal, or you will overwhelm the available bile.
7-Day After Removal Meal Plan: The “Re-Training” Menu
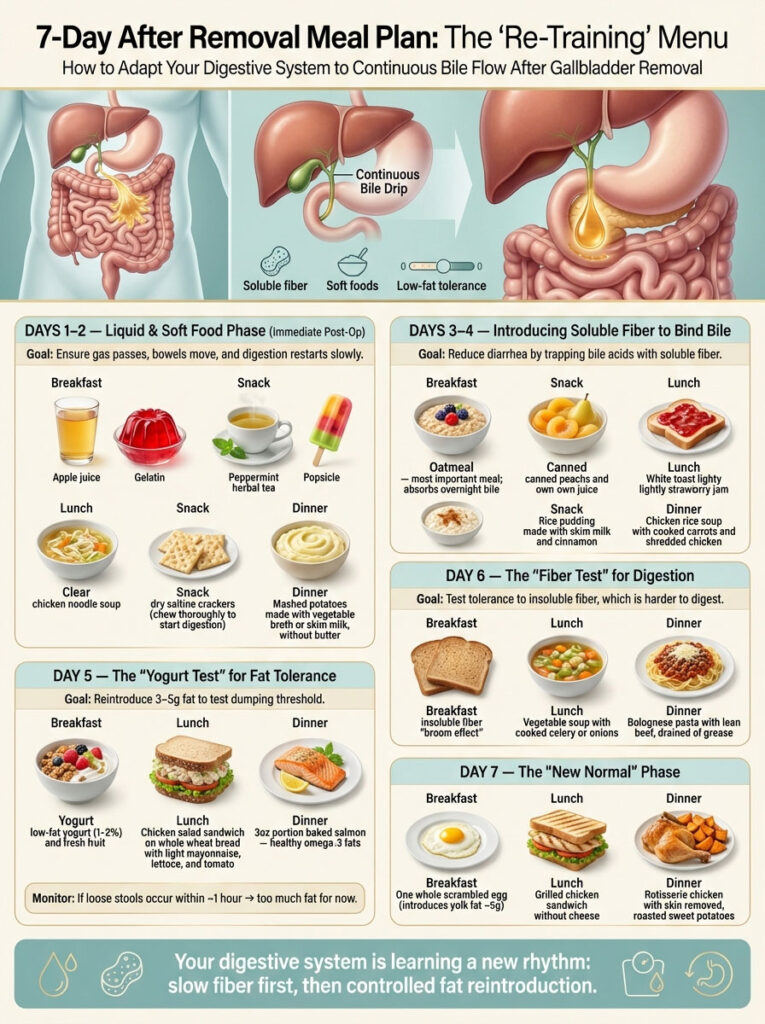
Day 1 & 2 Menu: The Liquid and Soft Food Phase (Immediate Post-Op)
Your body is healing from the anesthesia and the abdominal trauma of surgery. Digestion will be slow.
- Breakfast: Clear Fluids. Apple juice and gelatin (Jello).
- Snack: Herbal Tea. Peppermint tea (helps with gas pain from the surgery) and a popsicle.
- Lunch: Broth. Chicken noodle soup, eating mostly the broth and soft noodles.
- Snack: Saltines. Dry saltine crackers. Chew them thoroughly to start the digestive enzymes in your mouth.
- Dinner:Mashed Potatoes. Made with vegetable broth or skim milk. No butter yet.
- Goal: To ensure bowels are moving and gas is passing before introducing solids.
Day 3 & 4 Menu: Introducing Soluble Fiber to Bind Bile
Now we start managing digestion specifically to prevent diarrhea. Soluble fiber turns into a gel in your gut, trapping bile acids.
- Breakfast: Warm Oatmeal. This is the most important meal. The fiber acts as a sponge for the bile that accumulated overnight.
- Snack: Canned Fruit. Peaches or pears in juice (peeled). Raw fruit skins are too hard to digest right now.
- Lunch: Jam Toast. White toast with a very thin layer of strawberry jam.
- Snack: Rice Pudding. Made with skim milk and a dash of cinnamon.
- Dinner: Chicken Rice Soup. With cooked carrots. You can start eating the shredded chicken now.
Day 5 Menu: The “Yogurt Test” for Fat Tolerance
We begin to reintroduce fats in tiny increments (3g to 5g) to test your dumping threshold.
- Breakfast: Low-Fat Yogurt. Switch from fat-free to low-fat (1% or 2%) with granola.
- Lunch: Chicken Salad. Made with light mayonnaise. This tests your tolerance for oil-based fats.
- Dinner:Baked Salmon. Salmon is fatty, but it is healthy Omega-3 fat. Eat a small portion (3oz) to start.
- Monitor: Watch for loose stools within an hour of eating. If it happens, you are not ready for this fat level yet.
Day 6 Menu: The “Fiber Test” for Digestion
- Breakfast: Whole Wheat Toast. Insoluble fiber (the roughage in whole wheat) acts as a broom. It can be harder to digest, so we test it now.
- Lunch: Vegetable Soup. Containing cooked celery and onions.
- Dinner: Bolognese Pasta. Lean ground beef pasta sauce over white pasta. Ensure the beef is drained of all grease before adding the sauce.
Day 7 Menu: The “New Normal”
- Breakfast: Whole Egg. Scramble one whole egg. This introduces the fat from the yolk (approx 5g fat).
- Lunch: Grilled Chicken Sandwich. On a bun with lettuce and tomato. Avoid cheese for now.
- Dinner: Rotisserie Chicken. Remove the skin before eating. Serve with roasted sweet potatoes.
Comprehensive List of Foods to Eat With Gallstones or After Surgery
Navigating the grocery store is the hardest part of the recovery. Use this detailed breakdown to make quick, safe decisions.

1. Proteins: The Building Blocks of Healing
Proteins are generally safe if the fat is removed.
- Best Choices: Egg whites, Cod, Flounder, Tilapia, Haddock, Skinless chicken breast, Turkey breast, Tofu, Seitan.
- Use with Caution: Lean ground beef (90% lean or higher), Pork loin (trim fat), Whole eggs.
- Avoid Completely: Bacon, Sausage, Bratwurst, Ribeye steak, Duck, Dark meat chicken with skin.
2. Carbohydrates: Energy for Recovery
Carbs are your friend on a gallbladder diet because they rarely contain fat.
- Best Choices: White rice, Oatmeal, Barley, Quinoa, Couscous, White pasta, Potatoes (without skin at first), Sweet potatoes.
- Use with Caution: Whole grain breads (seeds can be irritating), Brown rice (higher fiber load).
- Avoid Completely: Croissants, Donuts, Biscuits, Pie crusts, Granola with added nuts/oils.
3. Fruits and Vegetables: Vitamins and Soluble Fiber
- Best Choices: Bananas, Applesauce, Canned fruits, Cooked carrots, Green beans, Zucchini, Spinach, Beets.
- Use with Caution: Raw salads (hard to digest), Citrus fruits (acidic).
- Avoid Completely: Creamed corn, Fried okra, Avocado (only in Phase 1; safe in moderation Phase 2), Coconut.
4. Dairy: The Common Trigger
Dairy fat is very dense and causes strong gallbladder contractions.
- Best Choices: Skim milk, Fat-free cheese, Fat-free Greek yogurt, Almond milk, Rice milk.
- Use with Caution: 2% Milk, Low-fat cottage cheese, Part-skim mozzarella.
- Avoid Completely: Ice cream, Heavy whipping cream, Butter, Brie, Cheddar cheese, Whole milk.
Comparison Table: The Gallbladder Diet Traffic Light System
| Category | 🟢 Green Light (Safe & Healing) | 🟡 Yellow Light (Test Tolerance) | 🔴 Red Light (Danger Zone) |
| Proteins | Egg whites, White fish, Tofu, Skinless Chicken. | Whole eggs, Lean steak (Sirloin), Pork Loin. | Bacon, Sausage, Ribeye, Fried Chicken. |
| Dairy | Skim milk, Fat-free yogurt/cheese. | 2% Milk, Low-fat cottage cheese. | Heavy Cream, Butter, Full-fat cheese. |
| Carbs | White rice, Oats, Potatoes (no skin). | Brown rice, Whole wheat bread. | Croissants, Donuts, Pastries, Biscuits. |
| Veggies | Cooked carrots, Green beans, Beets. | Raw salad, Broccoli (Gas), Avocado. | Creamed corn, Fried onions, Cauliflower. |
| Condiments | Mustard, Ketchup, Lemon juice, Herbs. | Light Mayo, Hummus (small amount). | Butter, Lard, Ranch Dressing, Creamy dips. |
Managing Post-Cholecystectomy Syndrome and Complications
Statistics show that up to 40% of people experience changes in digestion after surgery, ranging from mild bloating to chronic diarrhea. This collection of symptoms is often called Post-Cholecystectomy Syndrome (PCS). Understanding the specific causes can help you treat them.
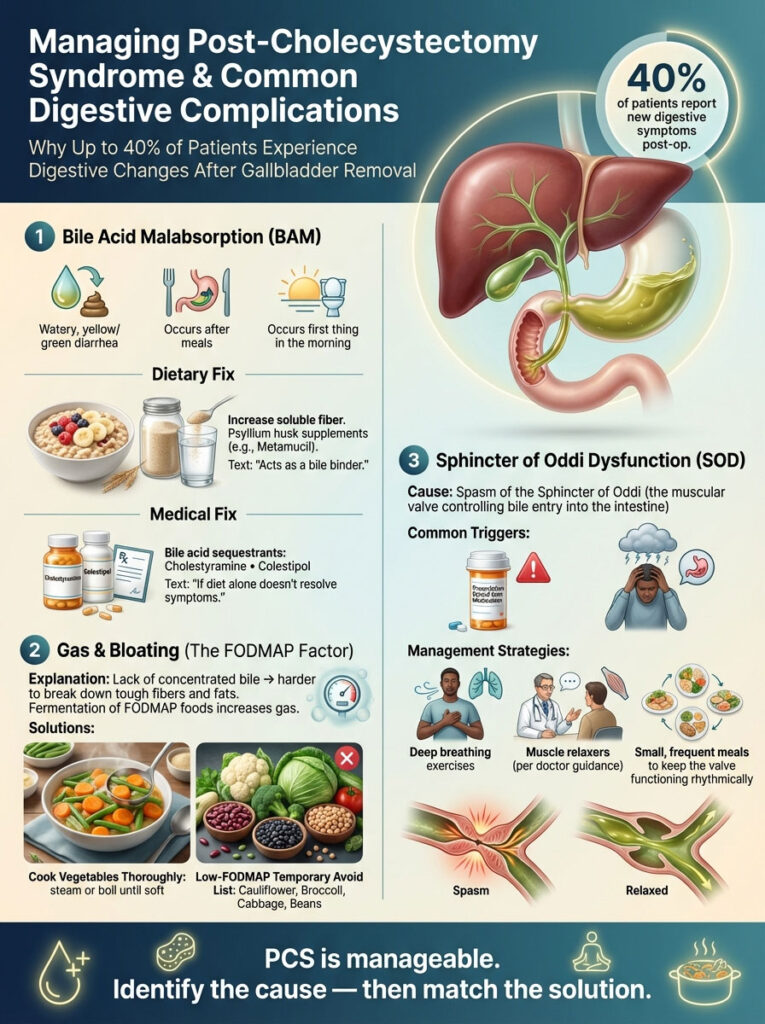
Dealing with Bile Acid Malabsorption (BAM)
This is the most common complaint. It happens because bile flows too fast into the colon.
- Symptoms: Watery, yellow/green diarrhea, often immediately after eating or first thing in the morning.
- Dietary Fix: Increase soluble fiber immediately. Psyllium husk supplements (like Metamucil) can act as a binder.
- Medical Fix: If diet doesn’t work, doctors can prescribe bile acid sequestrants (binders) like Cholestyramine or Colestipol.
Reducing Gas and Bloating (The FODMAP Factor)
You might notice that vegetables you used to love now cause painful bloating. This is because you lack the concentrated bile needed to break down tough plant fibers and fats effectively.
- The Solution: Cook your veggies thoroughly. Steam or boil them until soft.
- Low-FODMAP: Temporarily avoid gas-producing foods like cauliflower, broccoli, cabbage, and beans. These generate gas in the lower intestine, which can mimic gallbladder pain.
Sphincter of Oddi Dysfunction
Sometimes, people still feel “gallbladder pain” even after the organ is removed. This can be due to a spasm in the Sphincter of Oddi, the muscle valve that controls bile flow into the small intestine.
- Trigger: Opioid pain medications and stress can trigger this spasm.
- Management: Deep breathing, muscle relaxers, and eating small, frequent meals to keep the valve functioning rhythmically.
Actionable Lifestyle Tips for Long-Term Gallbladder Health
Following a 7-day gallbladder meal plan is a great start, but you need long-term habits to live comfortably without this organ.
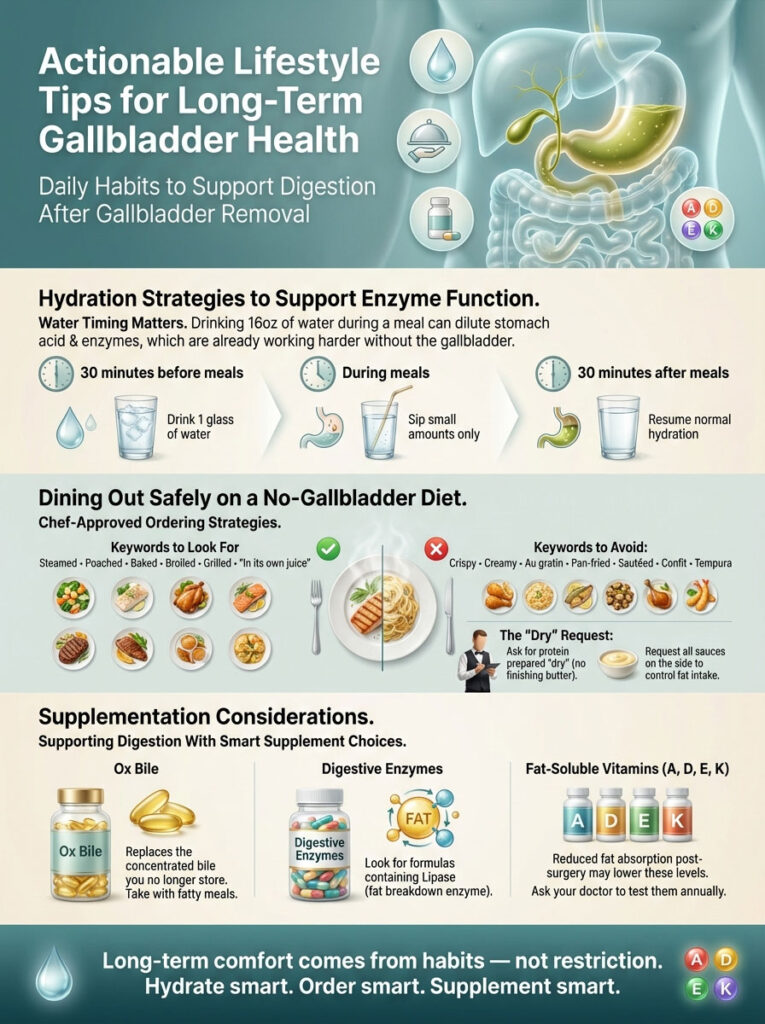
Hydration Strategies to Support Enzyme Function
Water is essential for digestion, but timing matters. Drinking 16oz of water during a meal can dilute the stomach acid and enzymes that are already struggling to work without a gallbladder.
- The Strategy: Drink a glass of water 30 minutes before your meal to hydrate the body. Sip small amounts during the meal. Wait 30 minutes after the meal to resume heavy drinking.
Dining Out Safely on a No Gallbladder Diet
Socializing can be scary. Use these chef secrets to order safely:
- Keywords to look for: Steamed, Poached, Baked, Broiled, Grilled, “In its own juice.”
- Keywords to avoid: Crispy, Creamy, Au Gratin, Pan-fried, Sautéed, Confit, Tempura.
- The “Dry” Request: Ask your server to have the chef prepare your protein “dry” (without finishing butter) and put all sauces on the side. This gives you control over the fat content.
Supplementation Considerations
- Ox Bile: Some functional medicine practitioners recommend Ox Bile supplements. These replace the concentrated bile you are missing. Take them with fatty meals.
- Digestive Enzymes: Look for enzymes containing Lipase, which specifically breaks down fat.
- Vitamin D, A, E, K: Since you digest fat less efficiently, you may absorb fewer fat-soluble vitamins. Ask your doctor to check your levels during your annual physical.
Frequently Asked Questions (FAQ)
Can I ever eat pizza again after gallbladder removal?
Yes, you likely can, but not immediately. You should wait at least 2 to 3 months to allow your system to heal. When you do eat it, choose thin crust (less doughy carbs), ask for “light cheese” or half cheese, and use a napkin to blot any pools of grease on top. Avoid processed meat toppings like pepperoni initially; stick to veggie toppings.
Does gallbladder removal cause weight gain?
It is a common phenomenon. Many patients lose weight before surgery because eating causes pain. After surgery, they can eat freely again without pain. This increased caloric intake, combined with a temporary slower metabolism during recovery and potential insulin resistance changes, can lead to weight gain. Focusing on high-fiber, low-calorie density foods helps prevent this.
Is coffee safe for gallbladder pain?
Generally, no. Caffeine is a stimulant that causes the gallbladder to contract. If you have stones, this strong contraction can trigger an attack. After surgery, the acidity of coffee combined with the laxative effect of caffeine can severely irritate the empty stomach and worsen diarrhea. Switch to herbal tea (chamomile or peppermint) or decaf initially
How long should I stay on a low-fat diet plan?
Most surgeons recommend a strict low-fat diet for 4 to 6 weeks post-op. This allows the liver and bile ducts time to adapt to the new flow. After that, you can slowly reintroduce fats. Listen to your body; if a certain food causes diarrhea, wait two weeks and try it again.
Can I drink alcohol without a gallbladder?
You should avoid alcohol for at least 2 weeks post-op, preferably a month. Your liver is working hard to adapt to the changes in bile flow and heal from the anesthesia. Alcohol adds unnecessary stress to the liver and can irritate the stomach lining, leading to gastritis.
Why do I have diarrhea after eating salad?
Raw vegetables contain insoluble fiber (cellulose). Without stored, concentrated bile to help break this down efficiently, it can pass through your system too quickly. This is often called “dumping.” Stick to cooked vegetables for the first month until your gut bacteria adapt.
What if I have constant yellow diarrhea that won’t stop?
If you are 6+ weeks post-op and still having daily urgent diarrhea, you may have Bile Acid Malabsorption (BAM). Diet alone might not fix this. Consult your gastroenterologist about a trial of a bile acid binder medication.
Disclaimer
This article is for informational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. Every individual’s recovery is unique. Always consult with your surgeon, gastroenterologist, or a registered dietitian before making significant changes to your diet or starting new supplements.
References
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Dieting & Gallstones.”
- Mayo Clinic. “Cholecystectomy (gallbladder removal): Diet.”
- American College of Surgeons. “Cholecystectomy: Surgical Patient Education.”
- Harvard Health Publishing. “What to do about gallstones.”
- British Society of Gastroenterology. “Guidelines on the management of bile acid malabsorption.”