You know that sudden, shaky feeling that hits around 3 PM. Your hands tremble slightly, your focus evaporates into a fog, and you feel an intense, almost primal need to eat something immediately. Or perhaps you wake up feeling groggy, anxious, and exhausted before the day has even started. These are not just signs of hunger or fatigue. They are biological signals that your glucose levels are swinging too wildly.
Table of Contents
Whether you are navigating a new diagnosis of Pre-diabetes, managing established Type 2 Diabetes, or dealing with the unpredictable drops of Reactive Hypoglycemia, the goal remains the same: Stability.
Blood sugar management involves balancing macronutrients—specifically carbohydrates, proteins, and fats—to maintain glucose levels within a target range (typically 70–140 mg/dL). A structured 7 day meal plan for low blood sugar focuses on low-Glycemic Index (GI) foods, high soluble fiber, and protein anchoring to prevent insulin spikes and hypoglycemic crashes.
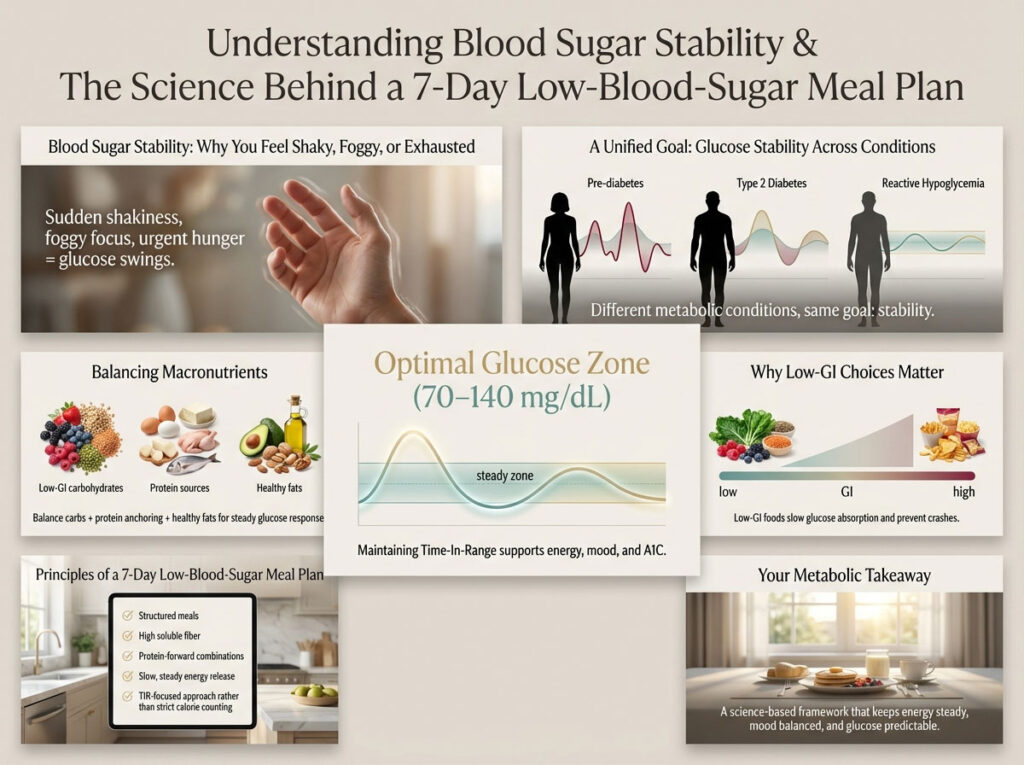
This comprehensive guide moves beyond generic “eat less sugar” advice. We will provide you with a deep-dive, scientifically grounded schedule designed to keep your energy steady, your mood balanced, and your A1C levels in check. We focus on “Time-in-Range” (TIR) rather than just calorie counting, bridging the gap between clinical endocrinology and your kitchen table.
The Biological Mechanics of Blood Sugar Instability and Insulin Resistance
To master your metabolic health, you must first understand the internal machinery operating every time you take a bite of food. It is not just about calories; it is about a hormonal cascade. When you consume simple carbohydrates, they break down rapidly into glucose. This glucose floods the bloodstream, demanding an immediate response.

In a metabolically healthy body, the pancreas releases insulin to usher that sugar into your cells for energy. However, in cases of insulin resistance, the cells’ locks are “rusty.” The pancreas must shout louder, flooding the system with excess insulin to get the job done. This overcompensation often leads to a rapid plunge in sugar levels—a crash.
This crash triggers a “counter-regulatory” response. Your body releases cortisol (the stress hormone) and adrenaline to force the liver to release stored sugar (glycogen). This is why you feel anxious, sweaty, or “hangry” during a low. You are essentially in a chemically induced fight-or-flight state.
Understanding Glycemic Load vs. Glycemic Index for Diabetic Diet Planning
Many people get confused by these terms, but distinguishing them is vital for blood sugar stability. The Glycemic Index (GI) measures how quickly a specific food raises blood sugar compared to pure glucose. However, GI implies that you eat foods in isolation, which we rarely do.
Glycemic Load (GL) is the superior metric for real-world eating because it accounts for portion size.
- The Watermelon Paradox: Watermelon has a high GI (72), suggesting it is “bad.” However, a standard slice has a very low Glycemic Load (4) because it is mostly water and fiber.
- The Bagel Trap: A white bagel has both a high GI and a massively high GL because it is dense, refined starch.
According to Harvard Health standards, we categorize foods to build our plan:
- Low GI (55 or less): Most non-starchy vegetables, legumes, berries, nuts, and minimally processed grains like barley.
- Medium GI (56-69): Brown rice, whole wheat bread, sweet potatoes.
- High GI (70+): White bread, jasmine rice, sugary beverages, instant oats.
For optimal blood sugar management, this meal plan focuses almost exclusively on Low GI foods that also carry a low Glycemic Load.
The Critical Role of Soluble Fiber and Protein Anchoring in Glucose Control
The most effective, non-pharmaceutical tool for blood sugar management is nutrient anchoring. This concept is simple yet transformative: Never eat a “naked carb.”
If you eat an apple alone, your glucose spikes relatively quickly. If you eat that same apple with 12 almonds or a slice of sharp cheddar cheese, the fat and protein act as a metabolic anchor. They physically and chemically slow down gastric emptying. This results in a slower, gentler release of sugar into the bloodstream, flattening the curve.
Soluble fiber is particularly important. Found in oats, flaxseeds, and legumes, soluble fiber dissolves in water to form a thick, gel-like substance in your gut. This gel traps sugar molecules, preventing them from rushing into your blood. This is why our plan leans heavily on “viscous” foods like chia seed pudding and lentil soups.
Evidence-Based Dietary Guidelines for Stabilizing Blood Sugar Levels
Before we walk through the daily menu, we must establish the ground rules of engagement. These guidelines ensure that even if you deviate from the specific recipes, you can still maintain blood sugar stability in any environment.

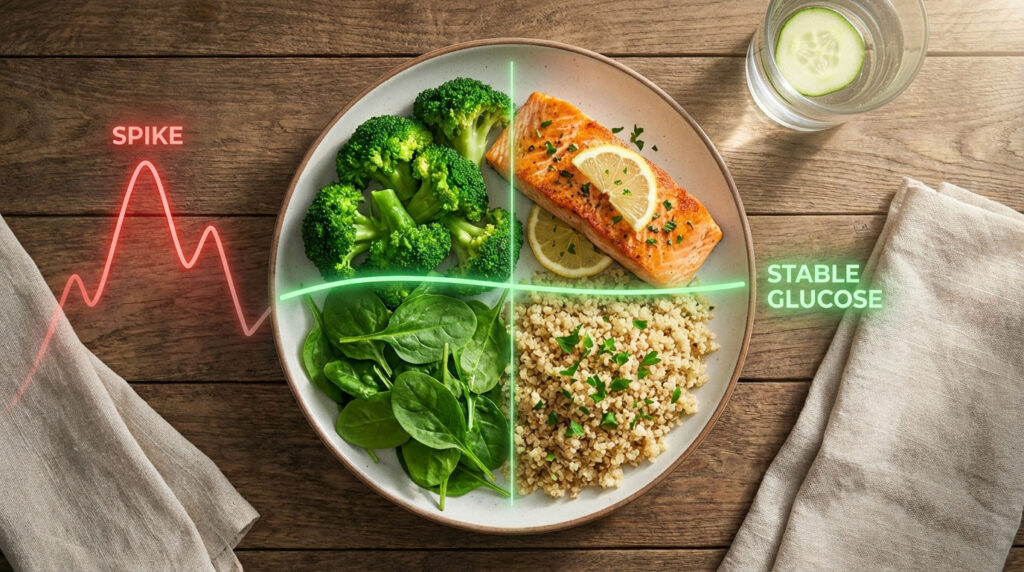
Implementing the ADA Plate Method for Balanced Macronutrients
The American Diabetes Association (ADA) recommends the Plate Method as a visual tool for meal planning. It is superior to calorie counting because it focuses on macronutrient interaction rather than energy restriction.
- 50% Non-Starchy Vegetables: Spinach, broccoli, peppers, kale, zucchini. These provide volume, hydration, and micronutrients without impacting blood sugar levels.
- 25% Lean Protein: Chicken, turkey, tofu, fish, eggs, Greek yogurt. Protein has a negligible effect on blood glucose and is essential for satiety.
- 25% Complex Carbohydrates: Quinoa, sweet potato, beans, berries, steel-cut oats. These provide the energy you need but digest slowly due to their fiber matrix.
The 15-15 Rule Protocol for Treating Acute Hypoglycemia Safety
While this plan is designed for stability and prevention, you must know how to handle an emergency drop. If you have reactive hypoglycemia or take insulin/sulfonylureas, you might experience “lows” (hypoglycemia).
The Protocol: If your glucometer reads below 70 mg/dL or you feel the tell-tale dizziness and shaking:
- Consume 15 grams of fast-acting carbohydrates. Good sources include 4 ounces of fruit juice, 1 tablespoon of honey, or 3-4 glucose tablets.
- Wait 15 minutes. Do not eat more during this time, even if you still feel hungry. It takes time for the sugar to hit the bloodstream.
- Check Again. Measure your blood sugar.
- Stabilize. Once your levels are above 70 mg/dL, eat a small snack with protein (like peanut butter crackers) to prevent it from dropping again.
Crucial Note: The meal plan below is for prevention. Do not use complex carbs (like oatmeal) to treat an acute low, as they digest too slowly to save you from a dangerous crash.
Comparative Analysis: Carbohydrates and Glycemic Impact
To achieve blood sugar stability, you must learn to swap “Spikers” for “Stabilizers.” The following table illustrates the difference in glycemic impact of common foods.
| Food Category | “The Spiker” (Avoid) | “The Stabilizer” (Eat) | Glycemic Impact Explanation |
| Breakfast Grains | Instant Oatmeal | Steel-cut Oats | Steel-cut oats retain the hull and fiber, taking twice as long to digest as processed instant oats, leading to a gentle rise in blood sugar levels. |
| Rice & Sides | White Jasmine Rice | Quinoa or Cauliflower Rice | Quinoa is a complete protein and complex carb. Cauliflower rice has near-zero impact on glucose. |
| Fruit Choices | Dried Fruits / Fruit Juice | Whole Berries / Green Apples | Juice lacks fiber and hits the blood instantly. Whole berries are packed with antioxidants and soluble fiber that blunt glucose spikes. |
| Breads | White Sandwich Bread | Sprouted Grain (Ezekiel) Bread | Sprouted grains have a lower glycemic index and higher protein content (enzymatically active) than refined flour breads. |
| Potatoes | Mashed White Potato | Roasted Sweet Potato | Sweet potatoes have more fiber and beta-carotene. Cooling them after cooking also increases “resistant starch,” which acts like fiber. |
| Snack Foods | Rice Cakes | Handful of Walnuts | Rice cakes are pure starch with a high GI (82+). Nuts provide healthy fats and protein to stabilize energy and hormones. |
Comprehensive 7 Day Low Glycemic Index Meal Plan for Glucose Management
This meal plan averages 30-45g of net carbs per main meal and includes high-satiety ingredients. It is specifically architected to prevent both the “Dawn Phenomenon” (morning spikes driven by cortisol) and the “Somogyi Effect” (rebound highs after night lows).
Monday: The Metabolic Reset and Detox
We start the week by eliminating processed sugars and focusing on whole, unprocessed foods to reset your insulin sensitivity and reduce systemic inflammation.
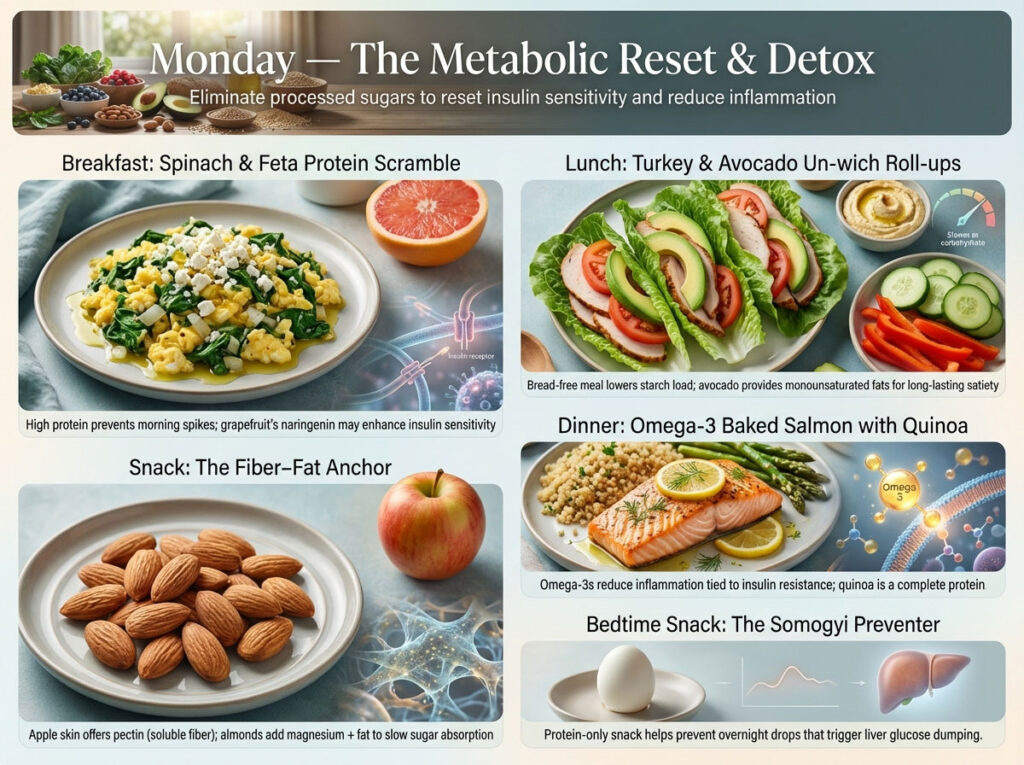
- Breakfast: Spinach & Feta Protein Scramble
- The Meal: Whisk 2 large eggs with a splash of water. Sauté 1 cup of fresh spinach and 1/4 cup diced onions in olive oil until soft. Pour in eggs and scramble. Top with 1 tbsp crumbled feta.
- The Pair: Serve with ½ a grapefruit. Grapefruit contains naringenin, a flavonoid that may improve insulin sensitivity.
- Why it works: High protein prevents the morning spike, while the acidity of the grapefruit lowers the glycemic response.
- Lunch: Turkey & Avocado “Un-wich” Roll-ups
- The Meal: Take 3 large romaine lettuce leaves. Layer 4oz of low-sodium deli turkey breast (or roasted turkey), 2 tomato slices, and ¼ avocado inside each leaf. Roll them up tight.
- The Side: ¼ cup hummus with cucumber rounds and red pepper strips.
- Why it works: Removing the bread eliminates the heavy starch load, while the avocado provides monounsaturated fats to keep you full for 4 hours.
- Snack: The Fiber-Fat Anchor
- The Meal: 12 raw almonds paired with 1 small apple (skin on).
- Why it works: The skin of the apple provides pectin (soluble fiber), while the almonds provide magnesium and fat to blunt the sugar absorption.
- Dinner: Omega-3 Baked Salmon with Quinoa
- The Meal: Bake a 5oz salmon fillet with lemon slices and dill at 400°F for 12-15 minutes.
- The Side: ½ cup cooked quinoa and 1 cup roasted asparagus.
- Why it works: Salmon is rich in Omega-3 fatty acids, which reduce inflammation associated with insulin resistance. Quinoa is a complete protein, unlike rice.
- Bedtime Snack: The Somogyi Preventer
- The Meal: 1 Hard-boiled egg.
- Why it works: A pure protein snack before bed prevents blood sugar from dropping overnight, stopping the liver from panic-dumping glucose at 3 AM.
Tuesday: High Soluble Fiber Loading
Today we focus on increasing fiber intake to slow digestion and improve gut microbiome health, which is linked to better glucose control.

- Breakfast: Overnight Chia Seed Pudding
- The Meal: Mix 3 tbsp chia seeds with 1 cup unsweetened almond milk, 1 scoop of vanilla protein powder, and a drop of stevia. Let it sit in the fridge overnight. Top with ¼ cup fresh blueberries.
- Why it works: Chia seeds expand 10x in your stomach, creating a high-viscosity gel that drastically slows sugar absorption.
- Lunch: High-Fiber Lentil Soup
- The Meal: A bowl of hearty lentil soup (lentils, carrots, celery, broth).
- The Side: A green salad with olive oil and vinegar dressing.
- Why it works: Lentils have a very low GI (around 32). The vinegar in the salad dressing contains acetic acid, which further reduces the glycemic impact of the lentils.
- Snack: The Crunchy Protein Fix
- The Meal: 2 stalks of celery filled with 2 tbsp natural peanut butter (no added sugar).
- Why it works: The “crunch” satisfies cravings, while the fat in peanut butter provides long-lasting fuel without a glucose spike.
- Dinner: Chicken & Vegetable Stir-Fry with Cauliflower Rice
- The Meal: Sauté diced chicken breast with broccoli florets, snap peas, and bell peppers in sesame oil. Add soy sauce (or tamari) and ginger.
- The Base: Serve over 1 cup of steamed cauliflower rice.
- Why it works: Using cauliflower instead of white rice saves you roughly 40g of carbohydrates, making this a “flat-line” glucose meal.
- Bedtime Snack: Walnut Brain Fuel
- The Meal: A small handful (approx. 1 oz) of walnuts.
- Why it works: Walnuts are unique for their high ALA (Alpha-Linolenic Acid) content, supporting vascular health in diabetics.
Wednesday: Plant-Based Insulin Sensitivity
Plant-based fats and proteins can improve insulin resistance by reducing the load of saturated fats.
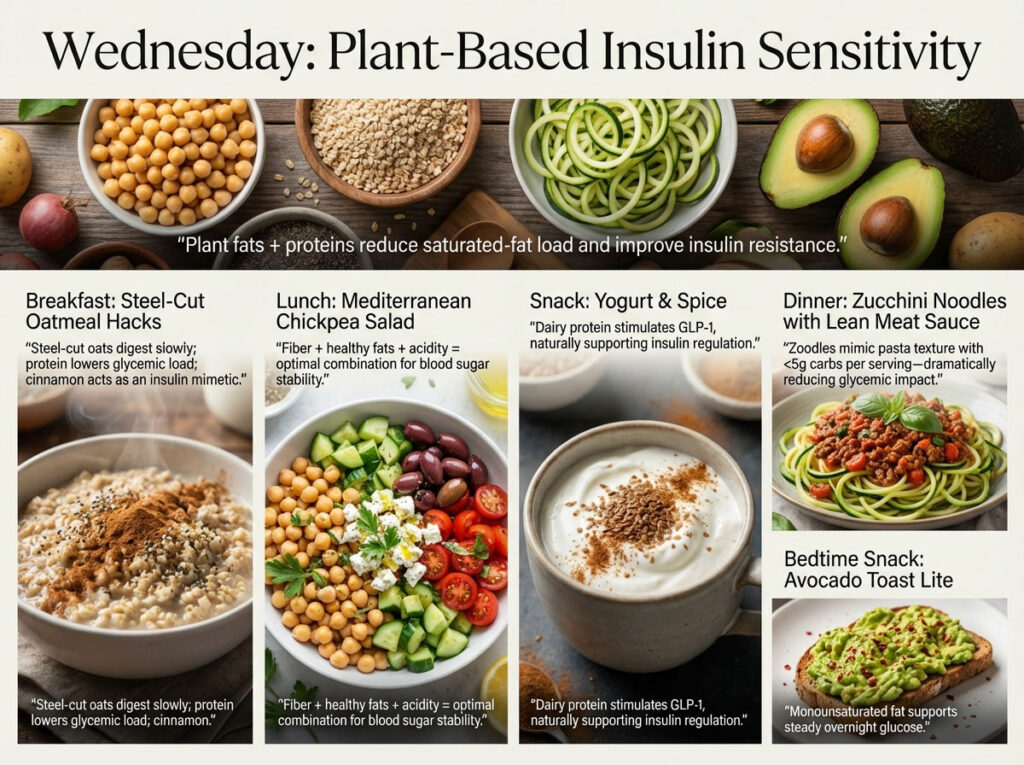
- Breakfast: Steel-Cut Oatmeal Hacks
- The Meal: ½ cup cooked steel-cut oats (not instant).
- The Anchor: Stir in 1 scoop of unflavored protein powder or 2 tbsp of hemp seeds. Top with cinnamon.
- Why it works: Steel-cut oats are complex carbs. By adding protein powder, we lower the overall glycemic load. Cinnamon acts as an insulin mimetic.
- Lunch: Mediterranean Chickpea Salad
- The Meal: Combine ½ cup rinsed chickpeas, diced cucumber, cherry tomatoes, 5 kalamata olives, and 1 oz crumbled feta cheese. Dress generously with extra virgin olive oil and lemon juice.
- Why it works: The combination of fat (olive oil), fiber (chickpeas), and acid (lemon) creates the perfect trifecta for blood sugar stability.
- Snack: Yogurt & Spice
- The Meal: ½ cup plain Greek Yogurt (unsweetened) mixed with 1 tsp flaxseeds and a dash of cinnamon.
- Why it works: Dairy protein stimulates GLP-1 (a gut hormone) which helps regulate insulin secretion naturally.
- Dinner: Zucchini Noodles with Lean Meat Sauce
- The Meal: Spiralized zucchini noodles sautéed briefly. Top with a meat sauce made from lean ground beef (93/7) and marinara sauce (check label for no added sugar).
- Why it works: Traditional pasta is a major spiker. Zucchini mimics the texture but has less than 5g of carbs per serving.
- Bedtime Snack: Avocado Toast Lite
- The Meal: 1 slice of whole-wheat or high-fiber crispbread with ¼ avocado smashed on top.
- Why it works: The monounsaturated fat stabilizes sugars through the night.
Thursday: Anti-Inflammatory and Gut Health Focus
Chronic inflammation can worsen insulin resistance. Today’s menu helps calm the immune system.

- Breakfast: The Green Stability Smoothie
- The Meal: Blend 1 cup spinach, ½ green banana (rich in resistant starch), 1 tbsp almond butter, 1 scoop whey or pea protein powder, and water/ice.
- Why it works: Green bananas have not yet converted their starch to sugar, acting as a prebiotic fiber. The almond butter prevents the liquid meal from spiking sugar.
- Lunch: Leftover Chicken Stir-Fry Repurpose
- The Meal: Reheat the leftovers from Tuesday.
- Why it works: “Leftover Effect”: When starches like cauliflower or veggies are cooled and reheated, their structure changes slightly, often becoming more resistant to digestion.
- Snack: Savory Cottage Cheese
- The Meal: ½ cup Cottage Cheese topped with 1 tbsp roasted sunflower seeds.
- Why it works: Cottage cheese is rich in casein protein, which digests very slowly, providing a steady stream of amino acids and glucose control.
- Dinner: Grilled Shrimp Tacos (Low Carb)
- The Meal: Grill 6oz shrimp with chili lime seasoning. Serve in large cabbage leaves or low-carb almond flour tortillas. Top with fresh salsa and black beans.
- Why it works: Shrimp is pure protein with zero carbs. Black beans add anthocyanins (antioxidants) and fiber.
- Bedtime Snack: String Cheese
- The Meal: 1 stick of mozzarella string cheese.
- Why it works: Portable, perfectly portioned protein that requires no preparation.
Friday: Omega-3 Loading for Cellular Health
Healthy fats are essential for protecting the brain and nerves from the damaging effects of fluctuating sugar levels.
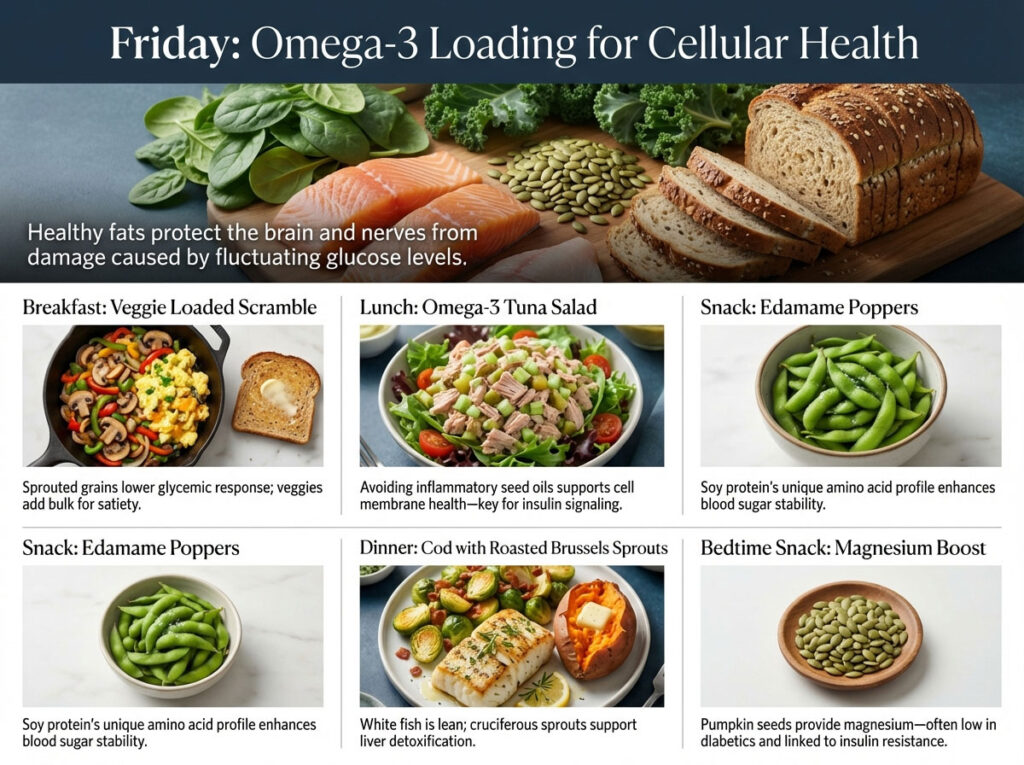
- Breakfast: Veggie Loaded Scramble
- The Meal: Sauté mushrooms, bell peppers, and onions. Scramble with 2 eggs.
- The Carb: 1 slice of toasted Ezekiel (sprouted grain) bread with a thin layer of butter.
- Why it works: Sprouted grain bread has a lower glycemic response than whole wheat. The veggies add bulk to keep you full.
- Lunch: Omega-3 Tuna Salad
- The Meal: Mix 1 can of tuna with mayonnaise made with avocado oil or olive oil (avoid soybean oil). Add diced celery and pickles. Serve on a bed of mixed greens.
- Why it works: Avoiding inflammatory seed oils helps improve cell membrane health, which is crucial for insulin reception.
- Snack: Edamame Poppers
- The Meal: ½ cup steamed Edamame (shelled).
- Why it works: Soy protein is unique in its amino acid profile and supports blood sugar stability better than many other plant proteins.
- Dinner: Cod with Roasted Brussels Sprouts
- The Meal: Pan-sear a cod fillet. Roast Brussels sprouts with olive oil and bacon bits until crispy. Serve with a small (fist-sized) baked sweet potato.
- Why it works: White fish is lean and light. Brussels sprouts are cruciferous veggies that aid liver detoxification.
- Bedtime Snack: Magnesium Boost
- The Meal: 2 tbsp pumpkin seeds (pepitas).
- Why it works: Pumpkin seeds are high in magnesium. Magnesium deficiency is common in diabetics and is linked to insulin resistance.
Saturday: The “Weekend Warrior” Flexibility Plan
Managing social eating and cravings without ruining your progress is a skill you must develop.

- Breakfast: Almond Flour Pancakes
- The Meal: Mix almond flour, eggs, almond milk, and baking powder. Cook like regular pancakes. Top with sugar-free maple syrup or fresh strawberries.
- Why it works: Almond flour is low carb and high fat, making these pancakes a “stabilizer” meal rather than a “spiker” like traditional flour pancakes.
- Lunch: The Bun-less Burger Bowl
- The Meal: Order or make a lean beef patty. Place it over a large salad bowl with tomato, onion, pickles, and mustard. Add cheese if desired.
- Why it works: You get all the flavor of a burger without the 40g of carbs from the bun.
- Snack: Sweet & Savory Pairing
- The Meal: 1 pear sliced + 1 oz cheddar cheese cubes.
- Why it works: The savory cheese cuts the sweetness of the pear and slows down the fructose absorption.
- Dinner: Steakhouse at Home
- The Meal: 4oz lean steak (sirloin or filet). Steam a large portion of broccoli.
- The Hack: Eat the broccoli first (see “Glucose Hacks” section).
- Why it works: Red meat provides iron and satiety. Broccoli acts as the fiber preload.
- Bedtime Snack: Golden Milk
- The Meal: Warm unsweetened almond milk with turmeric, ginger, and a pinch of black pepper.
- Why it works: Turmeric is a potent anti-inflammatory. The warm liquid is soothing for better sleep hygiene, which impacts cortisol.
Sunday: Meal Prep and Glycogen Replenishment
Preparing for the week ahead helps you stick to your 7 day meal plan for low blood sugar.

- Breakfast: Poached Egg Avocado Toast
- The Meal: 1 slice sprouted grain bread, toasted. Top with ½ smashed avocado, red pepper flakes, and a soft-poached egg.
- Why it works: This is the gold standard for a balanced breakfast—complex carb + healthy fat + high quality protein.
- Lunch: The Ultimate Cobb Salad
- The Meal: A massive bowl of greens topped with hard-boiled eggs, chopped bacon, grilled chicken strips, avocado, and blue cheese. Vinaigrette dressing.
- Why it works: High volume, high protein, high fat, near-zero carbs. This meal will keep your blood sugar a flat line for hours.
- Snack: Guacamole Dippers
- The Meal: Carrot sticks and bell pepper strips dipped in guacamole.
- Why it works: Replaces chips (high carb) with veggies (fiber/water) while keeping the healthy fats of the dip.
- Dinner: Slow Cooker Turkey Chili
- The Meal: Lean ground turkey, kidney beans, black beans, onions, peppers, and chili spices. Go light on the tomatoes.
- Why it works: Beans are high in resistant starch and fiber. This meal reheats well for Monday’s lunch.
- Bedtime Snack: Greek Yogurt
- The Meal: ½ cup Greek Yogurt.
- Why it works: Casein protein for the overnight fast.
Advanced Glucose Hacks and Behavioral Strategies for Reducing Spikes
Diet is not just about what you eat, but how you eat. Modern metabolic research has uncovered specific behaviors that can flatten glucose spikes significantly, even without changing the food on your plate.

The Science of Food Sequencing: Why Vegetables Must Come First
The order in which you eat your macronutrients matters immensely. A landmark study from Weill Cornell Medical College found that eating vegetables and protein before carbohydrates can reduce post-meal glucose and insulin levels by up to 73%.
Think of fiber as a physical net. When you eat vegetables (fiber) first, they deploy this net across the lining of your small intestine. When you eventually eat the starch (like rice or potato), the glucose molecules get caught in that fiber net and absorb much slower.
- The Strategy: Always eat your green vegetable starter before you touch the bread basket or the rice on your plate.
Utilizing Apple Cider Vinegar to Improve Insulin Sensitivity
Vinegar is an ancient remedy backed by modern science. It contains acetic acid, which temporarily inactivates alpha-amylase, the enzyme in your saliva and gut that breaks down starch into sugar.
Research Insight: Consuming 1 tablespoon of apple cider vinegar (ACV) diluted in a tall glass of water 10 minutes before a high-carb meal can improve insulin sensitivity by 19-34% (Source: Diabetes Care).
- The Protocol: Mix 1 tbsp ACV in 8oz water. Drink it through a straw (to protect tooth enamel) right before dinner. This acts as a pharmacological blocker for sugar spikes.
Post-Prandial Walking to Activate GLUT4 Transporters Naturally
Your muscles are the largest glucose “sinks” in your body. When you sit sedentary after eating, your pancreas has to do all the heavy lifting to clear sugar from your blood.
However, when you walk, your muscles contract. This contraction stimulates GLUT4 transporters to rise to the surface of the muscle cells. These transporters open the “doors” to let sugar in without needing as much insulin.
- The Hack: Commit to a 10-minute walk within 30 minutes of finishing a meal. This can reduce the peak glucose spike by significant margins and prevent the subsequent crash.
Navigating Restaurants and Social Events while Maintaining Stability
One of the biggest challenges to blood sugar management is dining out. Restaurants often use hidden sugars in sauces and dressings. Here is your survival guide for different cuisines.

Smart Ordering Tactics for Italian, Mexican, and Fast Food Chains
Italian Restaurants:
- The Trap: Unlimited breadsticks and pasta.
- The Fix: Order “Carpaccio” or a Caprese salad as an appetizer (Protein/Fat). For the main, choose Chicken Piccata or Grilled Salmon with a side of steamed spinach instead of pasta. If you must have pasta, limit it to an appetizer size and eat your protein first.
Mexican Restaurants:
- The Trap: Chips, salsa, and margaritas (liquid sugar).
- The Fix: Fajitas are your best friend. They arrive sizzling with peppers, onions, and meat. Skip the flour tortillas and rice. Mash the guacamole into the beans and eat the meat with a fork. It is high satiety and low glycemic impact.
Fast Food Burgers:
- The Trap: The bun and the fries (a double starch bomb).
- The Fix: Nearly every major chain will do a “lettuce wrap” or “low carb bowl” if requested. Double the meat, add bacon and cheese, but skip the ketchup (which is 20% sugar). Drink water or unsweetened iced tea.
Asian Cuisine:
- The Trap: Sweet and Sour sauce, Hoisin sauce, and white rice.
- The Fix: Steamed dishes are best. “Chicken with Broccoli” or “Beef with Mixed Vegetables.” Ask for the sauce on the side, or ask for it “steamed with sauce on the side.” Avoid breaded meats (like General Tso’s).
Long-Term Management: Comparing Popular Diets for Metabolic Health
There is no single “perfect” diet, but there are approaches that are statistically better for blood sugar stability. How does the Plate Method used in this article stack up against other popular trends?
| Diet Approach | Pros for Blood Sugar Control | Cons and Risks | Best Candidate For |
| Keto (Ketogenic) | Extremely effective at lowering blood sugar levels and A1C quickly due to near-zero carb intake (<20g/day). | Can be hard to sustain socially. Risk of hypoglycemia for those on insulin if not monitored closely. “Keto Flu” during adaptation. | Those needing rapid weight loss or reversal of severe insulin resistance. |
| Mediterranean Diet | High in healthy fats (olive oil, nuts) and fiber. Proven to reduce cardiovascular risk, which is high in diabetics. | Includes grains and fruits which may still spike some individuals if portions aren’t watched. Slower weight loss than Keto. | Those looking for a sustainable, lifelong lifestyle change for heart & metabolic health. |
| Vegan (Whole Food) | High fiber intake improves insulin sensitivity naturally. Low saturated fat improves cardiovascular profile. | Can be heavy on carbs (grains/legumes). Requires careful planning to ensure protein pairing and B12 sufficiency. | Those who prefer plant-based eating for ethical or health reasons. |
| The Plate Method | Balanced, flexible, and visually intuitive. No food groups are strictly banned. Easy to use in restaurants. | Weight loss may be slower than Keto. Requires portion discipline (it’s easy to overestimate “half a plate”). | Blood sugar management for the average person wanting balance without extremes. |
Ketogenic Diet vs. Mediterranean Diet for Diabetes Management
The Ketogenic Diet is a “metabolic hammer.” By removing carbs almost entirely, you remove the need for large amounts of insulin. This is incredibly effective for Type 2 Diabetics. However, it requires strict adherence. One “cheat meal” can knock you out of ketosis.

The Mediterranean Diet, on the other hand, is a “metabolic physiotherapist.” It heals the metabolism slowly through anti-inflammatory foods. While it might not drop your A1C as fast as Keto, it is often easier to stick to for 10 or 20 years. The meal plan provided in this article is a hybrid: it uses the structure of the Mediterranean diet but with the lower-carb consciousness of a controlled diabetic protocol.
Frequently Asked Questions
What is the absolute best breakfast for low blood sugar prevention?
The best breakfast for blood sugar stability is one that is high in protein and healthy fats, with minimal carbohydrates. Examples include a 3-egg omelet with spinach and avocado, or full-fat Greek yogurt with chia seeds. This composition counteracts the “Dawn Phenomenon,” a natural morning spike in cortisol and growth hormone that raises blood sugar. Avoiding sugary cereals, pastries, and fruit juices is critical, as these set you up for a day of roller-coaster energy.
How quickly does food affect blood sugar levels after eating?
It depends on the macronutrient profile. Simple carbohydrates (juice, candy, white bread) can spike blood sugar levels in as little as 15 minutes, peaking around 30-45 minutes. Complex carbohydrates (oats, beans, quinoa) take longer to digest, raising levels gradually over 1-2 hours. Protein and fat have a minimal direct impact on glucose but serve to slow down the absorption of any accompanying carbs.
Can I eat fruit on a low blood sugar diet?
Yes, but selection is key. You should choose low glycemic index fruits. Berries (strawberries, raspberries, blueberries, blackberries), cherries, green apples, and pears are excellent choices because they are high in fiber and lower in sugar. Tropical fruits like pineapple, mango, and ripe bananas are higher in sugar and should be limited. Always pair fruit with a protein or fat source, like nuts or cheese, to prevent a rapid glucose spike.
What is the Somogyi Effect and how do I stop it?
The Somogyi effect is a rebound high blood sugar that occurs in the morning. It happens when your blood sugar drops too low during the night (hypoglycemia), causing your body to panic and release stress hormones (glucagon, cortisol, epinephrine). These hormones force your liver to dump stored sugar, spiking your levels by the time you wake up. A protein-rich bedtime snack (like a hard-boiled egg or a few nuts) can help prevent the initial drop, thus preventing the rebound.
Is intermittent fasting safe for blood sugar control?
Intermittent fasting can improve insulin resistance for many people by giving the pancreas a “break.” However, if you suffer from reactive hypoglycemia or take insulin/medication that lowers blood sugar, fasting can be dangerous and cause severe lows. It is not recommended for everyone. Always consult your doctor before starting a fasting regimen if you have blood sugar regulation issues.
How much fiber do I really need daily for stability?
The USDA recommends 25-30 grams of fiber daily, but for blood sugar management, more is often better. High fiber intake, particularly soluble fiber (found in beans, oats, flax), is crucial because it forms a gel in the gut that slows down the absorption of sugar into the bloodstream. Most Americans only get 15g per day, which contributes to metabolic instability.
Can stress cause high blood sugar even if I eat well?
Yes, absolutely. Stress triggers the release of cortisol. Cortisol’s job is to ensure you have energy to fight or flee, so it tells your body to become insulin resistant and releases stored glucose into the bloodstream. Chronic stress can keep blood sugar levels elevated even if your diet is perfect (Zero Carb). Stress management is a pillar of blood sugar control.
What are the best snacks for dropping blood sugar?
If you are dropping but not yet in the danger zone (e.g., 75-80 mg/dL), choose a snack with complex carbs and protein to stabilize you gently, like whole-wheat crackers with peanut butter or an apple with cheese. If you are acutely low (<70 mg/dL), use the 15-15 rule with fast-acting carbs first (juice/glucose tabs) to get out of the danger zone, then follow up with protein.
Does drinking water help lower blood sugar?
Yes. When blood sugar levels are high, your body tries to flush excess glucose out through urine. This requires water. If you are dehydrated, the glucose concentration in your blood remains high. Drinking water helps your kidneys filter out the excess sugar and rehydrates the blood, effectively diluting the concentration of glucose.
What is A1C and how does diet affect it?
Hemoglobin A1C is a blood test that measures your average blood sugar levels over the past 3 months. It measures how much sugar is attached to your red blood cells. By following a stable diet like this 7 day meal plan for low blood sugar, you reduce the frequency and height of daily spikes. Over 90 days, this results in a lower A1C percentage, indicating better disease management and lower risk of complications.
Why do I get shaky if I miss a meal?
This is a classic sign of reactive hypoglycemia or poor metabolic flexibility. It means your body is struggling to switch from burning sugar (glycolysis) to burning fat (ketosis) for energy. Your body has released too much insulin for the previous meal, or your glycogen stores are depleting. Eating small, frequent meals every 3-4 hours helps prevent these shakes until your metabolism heals.
Is the Keto diet better than the Plate Method for diabetes?
Keto can be very effective for lowering A1C quickly because it removes the variable of carbohydrates almost entirely. However, it is restrictive and hard to maintain for some. The Plate Method is generally more sustainable for long-term blood sugar stability, social flexibility, and ensures a broader intake of micronutrients from fruits and vegetables.
Disclaimer: The content provided in this article is for educational purposes only and does not constitute medical advice. Blood sugar management is highly individual. Always consult with your physician or a registered dietitian before making significant changes to your diet or medication regimen, especially if you are taking insulin or sulfonylureas, as dietary changes can rapidly alter medication needs.
References:
- American Diabetes Association (ADA) – Standards of Medical Care in Diabetes (2024 Guidelines).
- Harvard T.H. Chan School of Public Health – Glycemic Index and Glycemic Load research.
- Diabetes Care Journal – “Vinegar Ingestion at Bedtime Moderates Waking Glucose Concentrations.”
- Weill Cornell Medical College – “Food Order Has Significant Impact on Postprandial Glucose and Insulin Levels.”
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Hypoglycemia treatment protocols.