You are doing everything right. You start your morning with a green smoothie packed with spinach and pineapple. You snack on walnuts and yogurt. Dinner is a healthy filet of salmon with a side of eggplant. Yet, instead of feeling energized, you feel exhausted. Your head throbs, your skin feels itchy, and your digestion is unpredictable. This is the great health paradox facing millions of people today. The very foods celebrated as “anti-inflammatory superfoods” might actually be fueling a hidden fire in your body.
Table of Contents
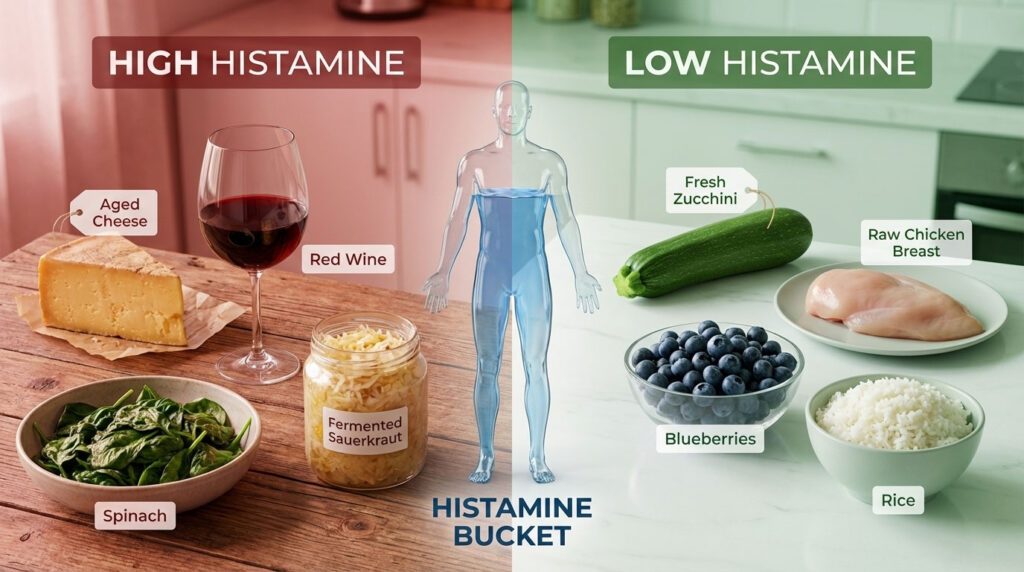
For millions dealing with unexplained headaches, hives, or digestive distress, the solution isn’t just eating healthy. It is about following a low histamine anti-inflammatory diet that respects the body’s enzymatic limitations. When your biological “bucket” is full, even a nutritious avocado can trigger a cascade of symptoms.
A low histamine anti-inflammatory diet is a therapeutic eating protocol that eliminates high-histamine foods (like aged cheeses and fermented products) and histamine-liberating ingredients (like citrus and tomatoes) while prioritizing fresh, nutrient-dense whole foods. This approach supports the reduction of mast cell activation and systemic inflammation, allowing the gut lining to heal and the immune system to stabilize.

This guide is not just another restrictive food list. It is a biochemical roadmap. We will deconstruct why your body reacts to “healthy” foods, identify the specific triggers, and provide a comprehensive strategy to calm your system using the right low histamine foods.
Understanding the Low Histamine Anti-Inflammatory Diet Protocol
To understand why a low histamine anti-inflammatory diet works, we must first look at the mechanism of histamine intolerance (HIT) and Mast Cell Activation Syndrome (MCAS). Histamine is not a villain. It is a vital biogenic amine involved in immune response, digestion, and central nervous system signaling. In a healthy body, you eat foods containing histamine, and an enzyme in your gut called diamine oxidase (DAO) breaks it down before it enters your bloodstream.

The Science of Histamine Intolerance and Chronic Inflammation
Chronic inflammation and histamine intolerance are often two sides of the same coin. Conditions like Small Intestinal Bacterial Overgrowth (SIBO), Leaky Gut, or Inflammatory Bowel Disease (IBD) damage the delicate brush border of the small intestine. This is exactly where diamine oxidase is produced. When the gut is inflamed, DAO production drops. When DAO drops, histamine levels rise. High histamine causes more inflammation. This creates a vicious cycle that a standard diet cannot break.
According to data referenced in the American Journal of Clinical Nutrition, approximately 1% of the population is diagnosed with histamine intolerance, though experts in gastroenterology estimate the number is significantly higher among patients with IBS and chronic functional digestive disorders.
The Histamine Bucket Theory and Symptom Thresholds
Imagine your body has a bucket. Every day, you pour histamine into it through food, stress, and environmental allergies. At the bottom of the bucket, there is a drain controlled by the DAO enzyme and Histamine N-Methyltransferase (HNMT). If the drain is clogged because of gut inflammation or genetic variants, or if you pour in too much histamine at once, the bucket overflows. This overflow manifests as symptoms that mimic an allergic reaction.
The goal of the low histamine diet is not to eliminate histamine entirely, which is impossible, but to lower the level in the bucket so that it remains below your symptom threshold. This is why some people can tolerate small amounts of “forbidden” foods occasionally, while others react immediately.
The Role of DAO Enzyme and HNMT in Metabolic Health
The DAO enzyme is your primary defense against dietary histamine. It functions primarily in the gut. However, once histamine passes the gut barrier and enters the bloodstream or the central nervous system, another enzyme called HNMT takes over.
If your gut is leaky, histamine bypasses DAO and floods the system, overwhelming HNMT. This is why digestive issues often present with non-digestive symptoms like migraines, anxiety, or insomnia. A low histamine anti-inflammatory diet supports both enzymes by reducing the incoming workload, giving your metabolic machinery a chance to catch up and repair.
Distinguishing High Histamine Foods from Histamine Liberators
A common mistake when starting a low histamine diet is focusing only on foods that contain histamine. However, you must also consider foods that trigger your body to release its own histamine. Understanding this distinction is vital for mastering the low histamine food list.
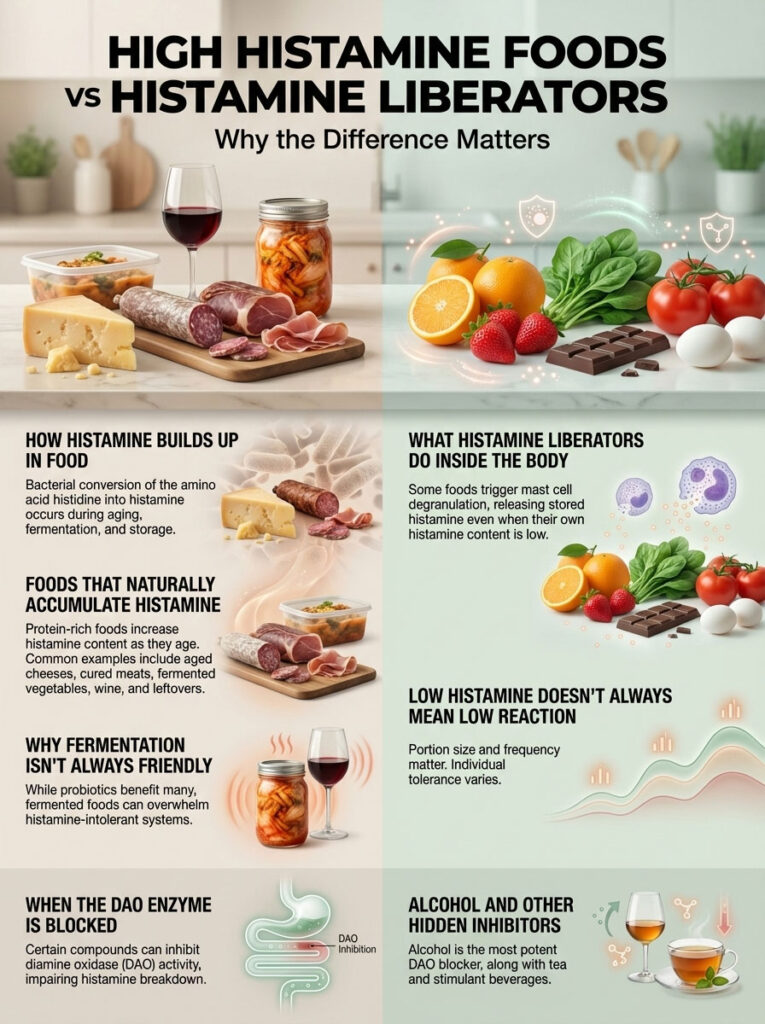
Identifying High Histamine Foods and Bacterial Growth
These are foods where bacteria have converted the amino acid histidine into histamine during aging, fermenting, or spoiling. The older the food, the higher the histamine content. This is a biological process that occurs in all protein-rich foods over time.
Examples include aged cheddar, salami, sauerkraut, kimchi, kombucha, red wine, and leftovers stored for more than 24 hours. The bacteria responsible for fermentation are effectively histamine factories. While probiotics are generally good for health, for a histamine-intolerant individual, they can be like pouring gasoline on a fire.
Understanding Histamine Liberators and Mast Cell Triggers
These foods may be low in histamine themselves, but they act as chemical keys that unlock your mast cells. When you eat them, your mast cells degranulate, flooding your system with inflammatory mediators.
Examples include citrus fruits, strawberries, egg whites (for some individuals), spinach, chocolate, and tomatoes. Even though a fresh strawberry has very little histamine, eating a bowl of them can trigger a massive reaction because it forces your body to dump its stored histamine reserves.
The Impact of DAO Blockers on Digestion
Certain compounds inhibit the DAO enzyme from functioning, effectively clogging the drain of your histamine bucket. Alcohol is the most potent DAO blocker. It attacks the enzyme directly while simultaneously increasing gut permeability. Other blockers include black tea, green tea, and energy drinks. Reducing these blockers is just as important as avoiding high histamine foods.
Comprehensive Low Histamine Anti-Inflammatory Food List
Navigating a low histamine anti-inflammatory diet requires precision. Below is a comprehensive categorization of safe foods and triggers. This list prioritizes nutrient density to ensure you are fighting inflammation while keeping histamine levels low.

Low Histamine Protein Sources and the Freshness Rule
Protein is the most critical category. Bacteria begin producing histamine in meat immediately after slaughter. Therefore, the “Freshness Rule” is non-negotiable. Meat must be cooked immediately after purchase or flash-frozen.
- Safe Proteins to Prioritize:
- Fresh Poultry: Freshly butchered chicken and turkey. Skinless cuts are often better tolerated as the skin can harbor more bacteria.
- White Fish: Freshly caught cod, hake, trout, and flounder. If buying frozen, look for “frozen at sea” labels.
- Eggs: Egg yolks are generally safe and nutrient-dense. Whites can be liberators for some, so test tolerance.
- Fresh Red Meat: Lamb and beef are acceptable only if they are fresh and not aged or hung for flavor.
- High Histamine Proteins to Avoid:
- Canned Fish: Tuna, sardines, and mackerel are very high in histamine due to the canning process.
- Smoked and Cured Meats: Bacon, sausage, pepperoni, salami, and smoked salmon.
- Aged Beef: Steaks that have been dry-aged for tenderness.
- Leftovers: Any cooked meat sitting in the fridge for more than 24 hours.
Anti-Inflammatory Vegetables for Histamine Intolerance
Vegetables form the base of the anti-inflammatory diet food list, but you must choose carefully. Many “healthy” veggies are problematic for this specific condition.
- Safe Vegetables (Low Histamine):
- Cruciferous Options: Broccoli, cauliflower, bok choy, and Brussels sprouts. These are excellent for liver detoxification.
- Root Vegetables: Carrots, parsnips, sweet potatoes, and beets. These provide sustained energy and fiber.
- Greens: Arugula, butter lettuce, and kale (in moderation) are better than spinach.
- Others: Zucchini, yellow squash, cucumbers, asparagus, green beans, onions, and garlic.
- Vegetable Triggers to Avoid:
- Spinach: High in histamine and oxalates.
- Tomatoes: A major histamine liberator found in sauces and salads.
- Eggplant: High in natural histamine.
- Avocado: Controversial. It is high in amines and often restricted in the strict elimination phase.
- Fermented Vegetables: Sauerkraut, pickles, and kimchi.
Low Histamine Fruits Rich in Antioxidants
Fruit provides quercetin and Vitamin C, which stabilize mast cells. However, citrus is a major offender.
- Safe Fruits:
- Pome Fruits: Apples and pears (peeled if sensitive to salicylates).
- Berries: Blueberries and blackberries are packed with polyphenols and are generally safe.
- Tropical: Mango, watermelon, cantaloupe, and honeydew melon.
- Stone Fruit: Cherries, apricots, and peaches.
- Fruit Liberators to Avoid:
- Citrus: Lemon, lime, orange, and grapefruit trigger histamine release.
- Berries: Strawberries are a known liberator.
- Others: Kiwi, pineapple, papaya, and overly ripe bananas.
Grains and Starches for Gut Health and Energy
Whole grains are generally safe, but gluten can be inflammatory for those with Leaky Gut.
- Safe Starches:
- Rice: White, brown, basmati, and jasmine rice are staples.
- Quinoa: A complete protein, but rinse it well to remove saponins.
- Oats: Ensure they are certified gluten-free to avoid cross-contamination.
- Millet and Buckwheat: Nutrient-dense ancient grains.
- Potatoes: White, red, and Yukon gold potatoes are excellent anti-inflammatory carbs.
- Inflammatory Starches to Avoid:
- Bleached Flours: Highly processed wheat products.
- Yeast Breads: Commercial breads use yeast fermentation, which raises histamine.
- Wheat Germ: Can be inflammatory for sensitive guts.
Healthy Fats to Reduce Systemic Inflammation
Healthy fats are essential for repairing cell membranes.
- Safe Fats:
- Extra Virgin Olive Oil: High polyphenol content fights inflammation.
- Coconut Oil and Milk: Additive-free versions are great for cooking and curries.
- Ghee and Butter: Fresh butter and clarified butter (ghee) are usually well tolerated.
- Fresh Animal Fats: Lard and tallow from grass-fed animals.
- Inflammatory Fats to Avoid:
- Walnut Oil: Walnuts are high in histamine.
- Seed Oils: Soybean, canola, and sunflower oils are often highly processed and pro-inflammatory.
The Traffic Light System for Histamine Foods
| Category | Green Light (Eat Freely) | Yellow Light (Eat with Caution) | Red Light (Strictly Avoid) |
| Vegetables | Zucchini, Carrots, Asparagus | Avocado, Mushrooms | Spinach, Tomatoes, Eggplant |
| Proteins | Fresh Chicken, Cod, Egg Yolk | Fresh Beef (minced), Pork | Salami, Canned Tuna, Bacon |
| Fruits | Apples, Blueberries, Pears | Bananas (not overripe) | Citrus, Strawberries, Pineapple |
| Dairy/Alt | Coconut Milk, Mozzarella (fresh) | Fresh Milk, Cream | Aged Cheddar, Parmesan, Yogurt |
| Grains | Rice, Quinoa, Potatoes | Corn, Gluten-free Bread | Wheat Germ, Yeast Bread |
| Condiments | Olive Oil, Fresh Herbs, Salt | Apple Cider Vinegar | Soy Sauce, Ketchup, Miso |
A quick reference guide to navigating the Low Histamine Anti-Inflammatory Diet.
Health Benefits of a Low Histamine Anti-Inflammatory Diet
Adopting this way of eating is not just about symptom management. It is about systemic repair. The low histamine anti-inflammatory diet benefits extend across multiple body systems, offering relief where traditional medicine often hits a wall.

Managing SIBO and Restoring Gut Health
By removing fermented and irritating foods, you reduce the inflammatory burden on the gut lining. This allows the brush border to heal and naturally regenerate the DAO enzyme. For those with histamine intolerance driven by SIBO, this diet provides immediate symptom relief. Less bloating and cramping occur because you are stopping the intake of bacterial fuel. While the diet manages symptoms, it creates a calm environment for antimicrobial treatments to effectively address the bacterial overgrowth.
Reducing Migraines and Neurological Inflammation
Histamine is a vasodilator. It widens blood vessels. In the brain, this sudden expansion can press on nerves, triggering migraines and cluster headaches. By adhering to low histamine foods for headaches and migraines, many sufferers report a drastic reduction in the frequency and intensity of their attacks. Additionally, histamine acts as an excitatory neurotransmitter. Lowering the load can reduce anxiety, insomnia, and “brain fog” caused by neuroinflammation.
Alleviating Skin Rashes Hives and Eczema
Your skin is packed with mast cells. When these cells are triggered by food, they release histamine, causing hives (urticaria), eczema flares, flushing, and relentless itching. Following a diet rich in low histamine foods for skin rashes stops the internal itch. It turns down the dial on the immune response, allowing the skin barrier to repair itself without the constant interference of inflammatory cytokines.
Supporting Recovery from Long COVID and MCAS
Recent research has established a link between Long COVID and Mast Cell Activation Syndrome (MCAS). Viral reservoirs or persistent immune activation can leave mast cells hyper-sensitive. A low histamine diet is increasingly used as a foundational therapy for “long haulers” to calm the cytokine storm and restore energy levels. By reducing the external histamine load, the body can focus its resources on fighting the viral remnants rather than fighting lunch.
Comprehensive 7-Day Low Histamine Anti-Inflammatory Meal Plan
A low histamine meal plan does not have to be boring. By using fresh herbs and safe fats, you can create delicious meals that heal. The key is simplicity and freshness.

Low Histamine Breakfast Ideas for Energy
- Monday: Oatmeal cooked with water or coconut milk, topped with fresh blueberries, chia seeds, and a drizzle of maple syrup.
- Tuesday: Savory Hash made with sautéed sweet potatoes, zucchini, and fresh onion. Serve with two soft-boiled egg yolks.
- Wednesday: Apple Stack featuring sliced crisp apples topped with macadamia nut butter and hemp hearts.
- Thursday: Rice Porridge (Congee) made with chicken broth and ginger.
- Friday: Smoothie with coconut milk, frozen mango, protein powder (pea or rice), and a handful of basil.
- Saturday: Gluten-free pancakes made with oat flour, served with fresh pear slices.
- Sunday: Fresh mozzarella cheese with melon slices and a side of rice cakes.
Low Histamine Lunch Ideas for Busy Workdays
- Monday: Quinoa Power Salad with roasted carrots, diced cucumber, fresh parsley, and grilled chicken breast. Dress with extra virgin olive oil.
- Tuesday: Creamy Carrot Soup made by blending roasted carrots and ginger with coconut milk.
- Wednesday: Turkey Wrap using large lettuce leaves filled with fresh roasted turkey slices, shredded carrots, and a spread of mashed plain chickpeas.
- Thursday: Leftover Chicken (frozen immediately after cooking and reheated) with a side of steamed broccoli.
- Friday: Cold Pasta Salad using gluten-free pasta, zucchini ribbons, olive oil, and fresh mozzarella.
- Saturday: Freshly grilled white fish tacos using corn tortillas (if tolerated) and cabbage slaw (no mayo, use olive oil).
- Sunday: Lamb Meatballs (fresh ground lamb) with a cucumber and dill salad.
Low Histamine Dinner Ideas for Family Meals
- Monday: Herb-Crusted Cod topped with chopped basil and parsley, baked until flaky. Serve with steamed asparagus and white rice.
- Tuesday: Lamb Patties made with fresh ground lamb, garlic, and rosemary. Serve with roasted sweet potato wedges.
- Wednesday: Chicken Stir-Fry with cubed fresh chicken breast, bok choy, carrots, and onions. Season with garlic, ginger, and sea salt.
- Thursday: Baked Potato Bar with toppings like ghee, chives, broccoli, and fresh chicken.
- Friday: Fresh Salmon (ensure it is fresh) with roasted cauliflower and a side of quinoa.
- Saturday: Roast Chicken Dinner with parsnips and green beans.
- Sunday: Shepherd’s Pie made with fresh ground beef, carrots, and topped with mashed white potatoes (freeze leftovers immediately).
Comparing Standard Anti-Inflammatory Diets vs Low Histamine Protocols
Many patients are confused because they switch from a “Standard American Diet” to a “Mediterranean Diet” and feel worse. This comparison highlights why the nuances matter.
| Feature | Standard Anti-Inflammatory (Mediterranean) | Low Histamine Anti-Inflammatory Diet |
| Primary Protein | Canned fish, Legumes, Aged Cheese | Fresh Meat, Fresh Fish, Eggs |
| Vegetable Base | Spinach, Tomatoes, Eggplant | Zucchini, Carrots, Asparagus |
| Fermented Foods | Highly Encouraged (Yogurt, Kimchi, Wine) | Strictly Avoided (Triggers inflammation) |
| Fruits | Citrus, Berries, Grapes | Apples, Pears, Blueberries, Mango |
| Bone Broth | Recommended (Long cook times) | Avoided (High histamine due to cook time) |
| Focus | Heart Health & General Longevity | Immune Calm, Symptom Management, Gut Repair |
| Leftovers | Encouraged for meal prep | Discouraged unless frozen immediately |
Table 2: Understanding the key differences between a standard anti-inflammatory approach and a low histamine protocol.
Practical Strategies for Success on a Low Histamine Diet
Transitioning to a low histamine diet can feel overwhelming initially. However, with the right strategies, it becomes a manageable lifestyle.

The Cook and Freeze Method for Meal Prep
This is the single most effective strategy for success. Bacteria multiply rapidly on cooked food in the refrigerator, converting histidine to histamine. A chicken breast cooked on Sunday is a histamine bomb by Tuesday.
- The Strategy: Cook your dinner. Immediately portion the leftovers into individual glass containers. Place them directly in the freezer. When you need a quick lunch, thaw the meal rapidly in a microwave or on the stove. Do not let it thaw slowly on the counter. This stops bacterial growth in its tracks.
Navigating Grocery Shopping and Reading Labels
When shopping for low histamine anti-inflammatory foods, your goal is to avoid additives that trigger inflammation.
- Meat Counter Strategy: Ask the butcher which day the delivery arrived. Buy meat on the day it comes in. Avoid “seasoned” or “marinated” meats, as these often contain high-histamine preservatives.
- Label Reading: Watch out for hidden names for MSG (yeast extract, hydrolyzed protein) and preservatives like sulfites and benzoates. These are known histamine liberators that can ruin an otherwise safe meal.
Dining Out Safely with Histamine Intolerance
You can still enjoy restaurants by communicating clearly.
- The Script: “I have a sensitivity to aged and fermented foods. Could I have the fish/chicken grilled plain with just olive oil and salt? I also need to avoid citrus and tomatoes.”
- Safe Bets: Steakhouses (fresh steak and baked potato), Sushi bars (sashimi, avoiding soy sauce and spicy mayo), and Farm-to-table restaurants (roast chicken and seasonal veg).
Supplements and Lifestyle Levers for Mast Cell Stabilization
Diet is the foundation, but supplements can be the scaffolding that supports your healing.

Using DAO Enzyme Supplements Effectively
For many, the natural production of diamine oxidase is compromised. Taking an exogenous DAO supplement 15 minutes before meals can effectively break down dietary histamine in the gut. These are typically derived from porcine kidney, though vegan options made from legumes (sprouted peas) are emerging. This acts as a safety net, especially when dining out or when you cannot verify the freshness of your food.
Natural Antihistamines and Quercetin Benefits
- Quercetin: A flavonoid found in apples and onions. It helps stabilize mast cells, preventing them from releasing histamine.
- Stinging Nettle: Often used as a tea or tincture (ensure it is not fermented) to reduce allergy symptoms.
- Vitamin C: Acts as a natural antihistamine and helps degrade the histamine molecule. However, ensure the source is not fermented corn or citrus-based if you are sensitive.
Frequently Asked Questions About Low Histamine Eating
What is the fastest way to flush histamine out of your body?
While you cannot instantly “flush” it, you can speed up clearance by hydrating well, taking Vitamin C (which helps degrade histamine), and using Vitamin B6, a cofactor for the DAO enzyme. Sweating through gentle exercise or a sauna can also help eliminate toxins, provided heat does not trigger your hives.
Is coffee allowed on a low histamine diet?
Coffee is controversial. It does not contain high histamine, but caffeine can block the DAO enzyme and trigger adrenaline, which destabilizes mast cells. Many people tolerate fresh, organic decaf or low-acid coffee better than regular. Instant coffee should be avoided.
Why does spinach trigger histamine symptoms?
Spinach is a potent histamine liberator. Even though it is considered a superfood, it contains high levels of oxalates and triggers mast cells to degranulate, releasing your body’s stored histamine. This makes it unsuitable for the elimination phase of this diet.
Can I eat sourdough bread on this diet?
Generally, no. Sourdough relies on fermentation, which produces histamine. While some people tolerate it better than yeast bread due to the digestion of gluten, it is usually excluded during the strict phase of a low histamine diet.
How long does it take to see results on a low histamine diet?
Most people notice a reduction in acute symptoms like headaches, flushing, and bloating within 2 to 4 weeks. Deeper issues like chronic eczema or gut dysbiosis may take 4 to 8 weeks of consistency to show significant improvement.
Are potatoes anti-inflammatory and low histamine?
Yes, fresh white, red, and sweet potatoes are low in histamine and generally anti-inflammatory. However, left-over potatoes can develop higher resistant starch and potential bacteria if not stored correctly, so cook and eat them fresh. Fried potatoes are inflammatory due to the oil.
Is apple cider vinegar safe for histamine intolerance?
No. Apple cider vinegar is a fermented product. Despite its health halo, it is high in histamine and can trigger immediate reflux or flushing in sensitive individuals.
What is the best protein powder for histamine intolerance?
Whey protein isolate (not concentrate) is often tolerated, but many prefer Rice Protein or Pea Protein. Ensure the product has no artificial sweeteners or additives. Avoid soy protein and casein, as they can be inflammatory triggers.
Can stress cause high histamine levels?
Absolutely. Stress causes the release of CRH (Corticotropin-Releasing Hormone), which activates mast cells to release histamine. This is why you might flare up during stressful times even if your diet is perfect.
Is the low histamine diet safe for pregnancy?
During pregnancy, the placenta produces massive amounts of DAO, often putting histamine intolerance into remission. However, if you need to follow this diet, consult a doctor to ensure you are getting enough folate and nutrients, as the diet restricts many common sources.
How do I reintroduce foods after an elimination diet?
Use the “ladder method.” Introduce one food at a time in a small quantity (e.g., a slice of avocado). Wait three days to watch for delayed reactions. If no symptoms occur, that food is safe. If you react, remove it and wait until symptoms subside before trying a different food.
Are probiotics safe for histamine intolerance?
Many standard probiotics contain Lactobacillus casei or Lactobacillus bulgaricus, which produce histamine. You must select specific “low histamine” strains like Bifidobacterium infantis or Lactobacillus rhamnosus that do not raise histamine levels.
Disclaimer: The information provided in this article is for educational purposes only and does not constitute medical advice. Histamine intolerance and MCAS are complex medical conditions. Always consult with a healthcare provider or a registered dietitian before making significant changes to your diet or supplement regimen.
References:
- Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American Journal of Clinical Nutrition.
- Schnedl, W. J., & Enko, D. (2021). Histamine Intolerance—The More We Know the Less We Know. A Review. Nutrients.
- Tuck, C. J., et al. (2019). Fermentable oligosaccharides, disaccharides, monosaccharides and polyols: role in irritable bowel syndrome. Expert Review of Gastroenterology & Hepatology.
- Comas-Basté, O., et al. (2020). Histamine Intolerance: The Current State of the Art. Biomolecules.