A low potassium meal plan limits daily intake to approximately 2,000 mg to manage Stage 4-5 CKD and Hyperkalemia. It prioritizes low potassium foods like apples, white rice, and cauliflower while avoiding high-risk items like bananas and potatoes to maintain safe serum potassium levels. By following a structured renal diet meal plan, patients can prevent electrolyte imbalances and protect residual kidney function.
Table of Contents
Every meal feels like a high-stakes calculation when you are living with advanced kidney disease. You are constantly told to eat healthy. Yet the very foods that the general population considers “superfoods,” such as avocados, whole grains, spinach, and bananas, can be physically dangerous for you. This contradiction creates a profound sense of “food fear.” It makes navigating the grocery store feel less like shopping and more like walking through a minefield.
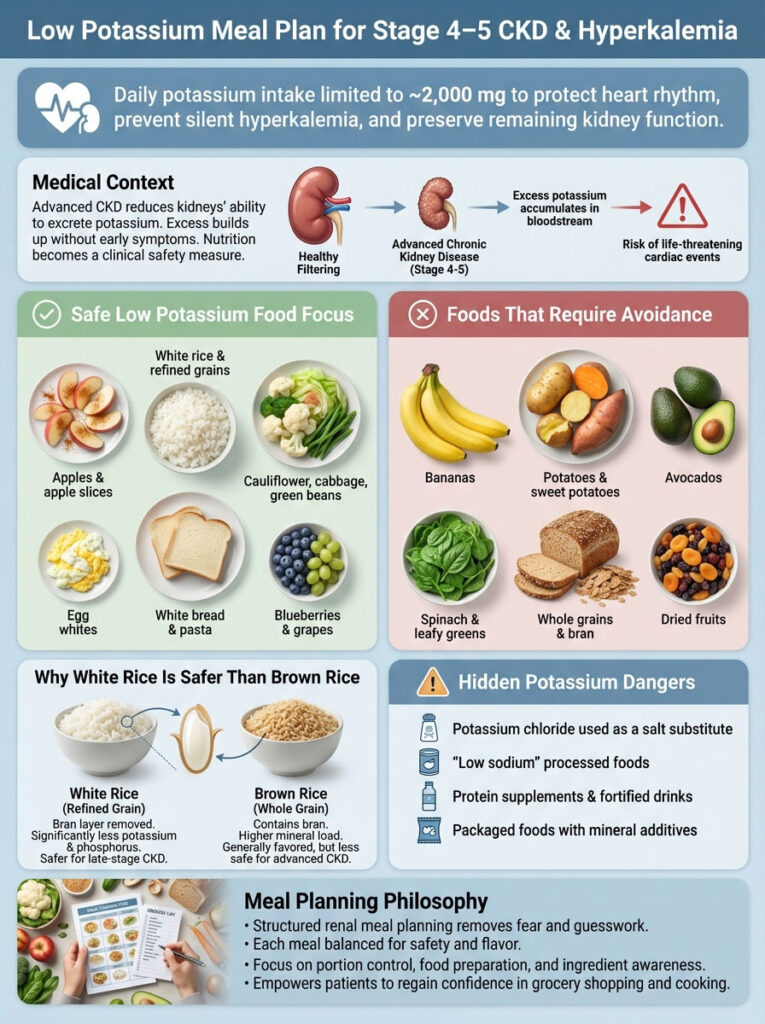
For patients diagnosed with Stage 4 or 5 Chronic Kidney Disease (CKD), managing mineral intake is not merely a lifestyle choice. It is a matter of immediate physical safety. When kidneys can no longer filter excess minerals efficiently, potassium builds up in the blood. This condition is known as Hyperkalemia. It is silent. It is often symptomless. It can be deadly if left unmanaged.
This guide is designed to eliminate the guesswork and the fear. We have constructed a comprehensive, deeply researched 7-day low potassium meal plan grounded in medical nutrition therapy. This plan adheres to the strict 2,000 mg potassium diet limit recommended by the National Kidney Foundation guidelines.
In this extensive guide, you will learn exactly which low potassium foods are safe to eat. We will explain the science behind why white rice is safer than brown rice for your specific condition. You will discover how to identify hidden dangers like potassium chloride in food labels which is a common additive that can spike your levels. Most importantly, you will regain control over your kitchen with delicious kidney friendly recipes that protect your health without sacrificing flavor.
Understanding Hyperkalemia and the Importance of a Low Potassium Diet for Stage 4 and 5 CKD
How Chronic Kidney Disease Affects Potassium Filtration and Serum Levels
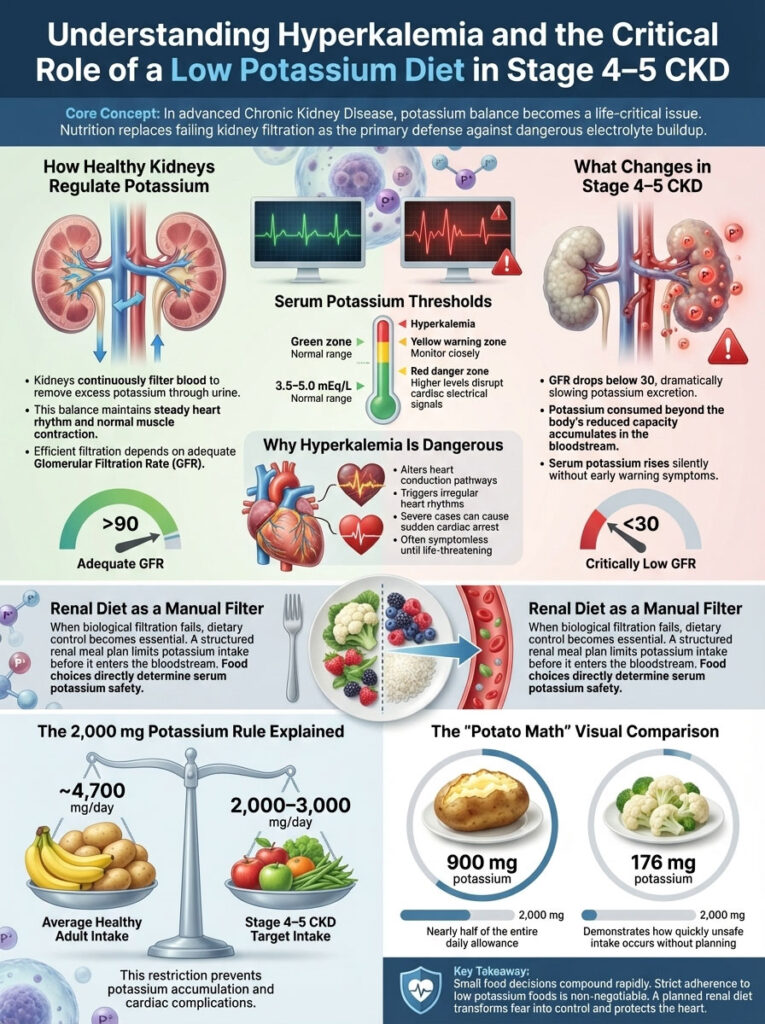
Your kidneys act as the body’s master chemists. They balance fluids and electrolytes with incredible precision. In a healthy body, the kidneys filter out excess potassium through urine to maintain a steady heartbeat and proper muscle function. However, as Stage 4 kidney disease diet protocols emphasize, this filtration system slows down significantly as the Glomerular Filtration Rate (GFR) drops.
When the GFR falls below 30, the kidneys struggle to excrete potassium efficiently. If you consume more than your body can handle, the excess remains in your bloodstream. This elevates your serum potassium levels. Normal levels range between 3.5 and 5.0 mEq/L. Levels above 5.5 mEq/L are considered Hyperkalemia.
The danger of Hyperkalemia is that it directly affects the electrical signals of the heart. Severe cases can lead to dangerous arrhythmia or sudden cardiac arrest. This is why a renal diet meal plan is the first line of defense. It acts as a manual filter when your biological filter is compromised.
The 2000 mg Potassium Restriction Rule for Renal Patients Explained
To understand the restriction, we must look at the numbers. The average American consumes about 4,700 mg of potassium per day. This is the recommendation for someone with healthy kidneys. For a patient on a low potassium diet, the limit is drastically different.
The “2,000 mg Rule” is the standard benchmark for most patients with Stage 4-5 CKD or those on a dialysis diet plan. Limiting intake to 2,000 mg to 3,000 mg per day prevents dangerous buildup in the blood.
Consider the “Potato Math” to see why this is difficult to achieve without a plan. A single medium baked potato contains roughly 900 mg of potassium. That is nearly 50% of your entire daily allowance in one side dish. In contrast, a serving of steamed cauliflower contains only about 176 mg. This is why strict adherence to a list of low potassium foods is non-negotiable. Small dietary choices accumulate rapidly to determine your safety.
Identifying High Potassium Foods and Hidden Dangers in the Grocery Store
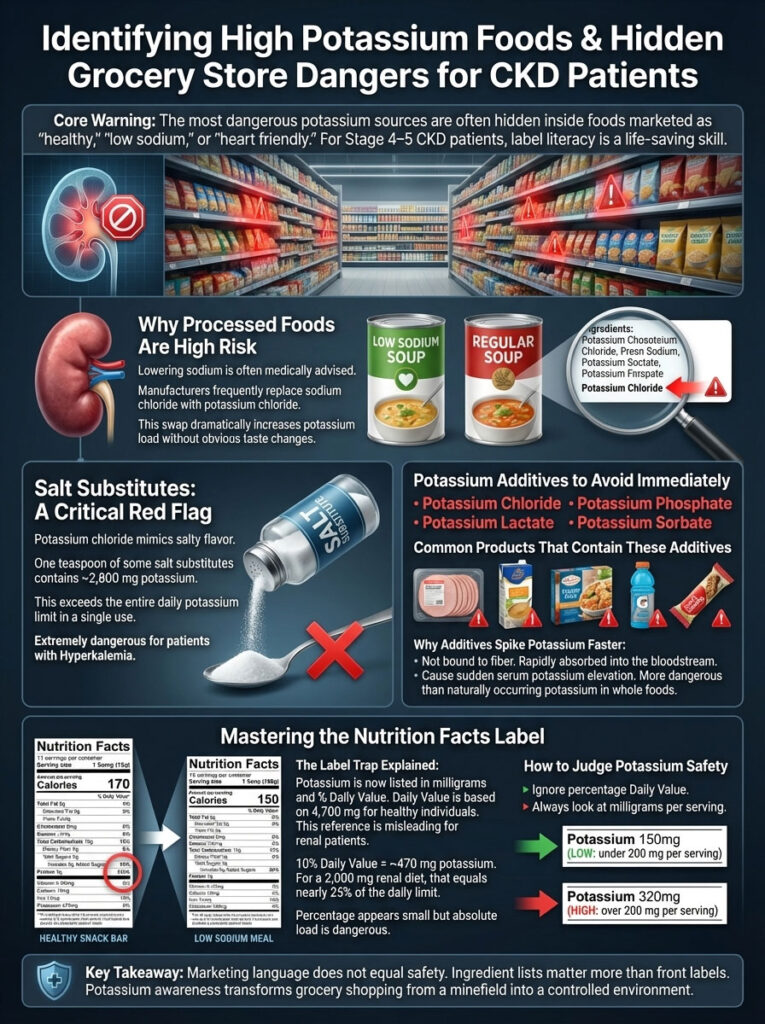
The Hidden Dangers of Potassium Chloride and Phosphate Additives in Processed Foods
The most dangerous item in the grocery store for a kidney patient often looks like a healthy choice. It is the “Salt Substitute.” Many patients are told to lower their sodium intake to control blood pressure. They reach for products labeled “No Salt,” “Low Sodium,” or “Heart Healthy.”
You must be extremely vigilant. Manufacturers often replace sodium chloride (table salt) with potassium chloride.
Potassium chloride tastes salty but is lethal for someone with Hyperkalemia. A single teaspoon of some salt substitutes can contain nearly 2,800 mg of potassium. That exceeds your entire daily limit in one seasoning.
Always scan the ingredient list for these additives:
- Potassium Chloride
- Potassium Lactate
- Potassium Phosphate
- Potassium Sorbate
If you see these words, put the product back immediately. These additives are often found in processed meats, low-sodium soups, and sports drinks. They are absorbed rapidly by the body and spike serum potassium levels faster than whole foods because they are not bound to fiber.
Mastering the Nutrition Facts Label to Calculate Daily Potassium Intake
Historically, potassium was not required on US nutrition labels. This changed with recent FDA updates. Now, most nutrition facts labels list potassium content in milligrams and as a percentage of the Daily Value (DV).
However, there is a catch. The “Daily Value” on the label is based on a healthy diet of 4,700 mg. If a label says a food provides “10% DV,” that means it contains 470 mg. For a healthy person, that is low. For you, on a 2,000 mg potassium diet, that is nearly 25% of your daily limit.
Do not look at the percentage. Look at the specific milligram count. A food is generally considered one of the low potassium foods if it has less than 200 mg per serving. A food is high potassium if it has more than 200 mg per serving.
The Definitive Low Potassium Food List and Safe Substitutions for Renal Diets

Green Light Foods: What Fruits and Vegetables Are Safe for Kidney Disease?
To simplify your life, visualize your low potassium diet as a traffic light. Green means go, but portion control still applies.
Green Foods (Go): These are low potassium foods with less than 200 mg per serving.
- Fruits: Apples, blackberries, blueberries, grapes, lemon, lime, pineapple, strawberries, cranberries.
- Vegetables: Alfalfa sprouts, cauliflower, celery, cucumber, eggplant, green beans, lettuce (Iceberg or Romaine), onions, peppers (green or red), radishes, summer squash.
- Starches: White rice, white bread, white pasta, couscous, cream of wheat.
- Proteins: Egg whites, fresh chicken, fresh pork, fresh fish (cod, tilapia, salmon).
Yellow Foods (Caution): These have moderate levels (200-300 mg). Eat them occasionally or in small portions.
- Fruits: Peaches, pears, cherries, watermelon.
- Vegetables: Corn, peas, asparagus, broccoli (raw is lower than cooked volume-wise), carrots.
- Dairy: Limit to 4 ounces of milk or yogurt daily (high in phosphorus too).
- Beverages: Coffee (limit to 1 cup).
Red Light Foods: Which High Potassium Items Must Be Avoided Completely?
Red Foods (Stop): These are foods to avoid with kidney disease. They typically have over 300-400 mg per serving or are very dense in minerals.
- Fruits: Bananas, oranges, avocados, cantaloupe, dried fruits (raisins, prunes, dates), kiwi, mango, papaya.
- Vegetables: Potatoes (unless leached), sweet potatoes, tomatoes (sauce and paste are very high), spinach, beet greens, pumpkin, winter squash, artichokes.
- Starches: Brown rice, whole wheat bread, bran cereal, granola.
- Additives: Molasses, chocolate, nuts and seeds (unless in very small amounts), salt substitutes.
Comparison Table: High vs. Low Potassium Food Swaps
Preventing “diet depression” is key to sticking to a renal diet meal plan. Use these swaps to enjoy similar textures and flavors without the risk.
| High Potassium Food (Avoid) | Low Potassium Alternative (Safe Swap) | Why It Works for Kidney Patients |
| Banana (422 mg) | Apple (195 mg) | Apples provide crunch and fiber without the massive potassium load found in tropical fruits. |
| Potato (Baked, 900 mg) | Cauliflower (Steamed, 176 mg) | Mashed cauliflower with garlic and butter mimics the texture of mashed potatoes safely. |
| Tomato Sauce | Red Pepper Puree | Roasted red peppers offer the vibrant red color and zest without the concentration of K found in tomatoes. |
| Orange Juice | Cranberry or Apple Juice | Citrus is generally high in K. Orchard fruits like apples and grapes are safer choices for juice. |
| Brown Rice | White Rice | White rice has significantly lower phosphorus and potassium because the bran layer is removed. |
| Spinach (Cooked) | Green Beans | Spinach shrinks when cooked, concentrating the minerals. Green beans maintain volume and are lower in K. |
| Chocolate | Lemon or Vanilla Cake | Chocolate is high in both potassium and phosphorus. Fruity desserts are usually kidney-friendly. |
| Whole Wheat Bread | Sourdough White Bread | Sourdough is lower in additives and the fermentation process makes it gut-friendly without the bran. |
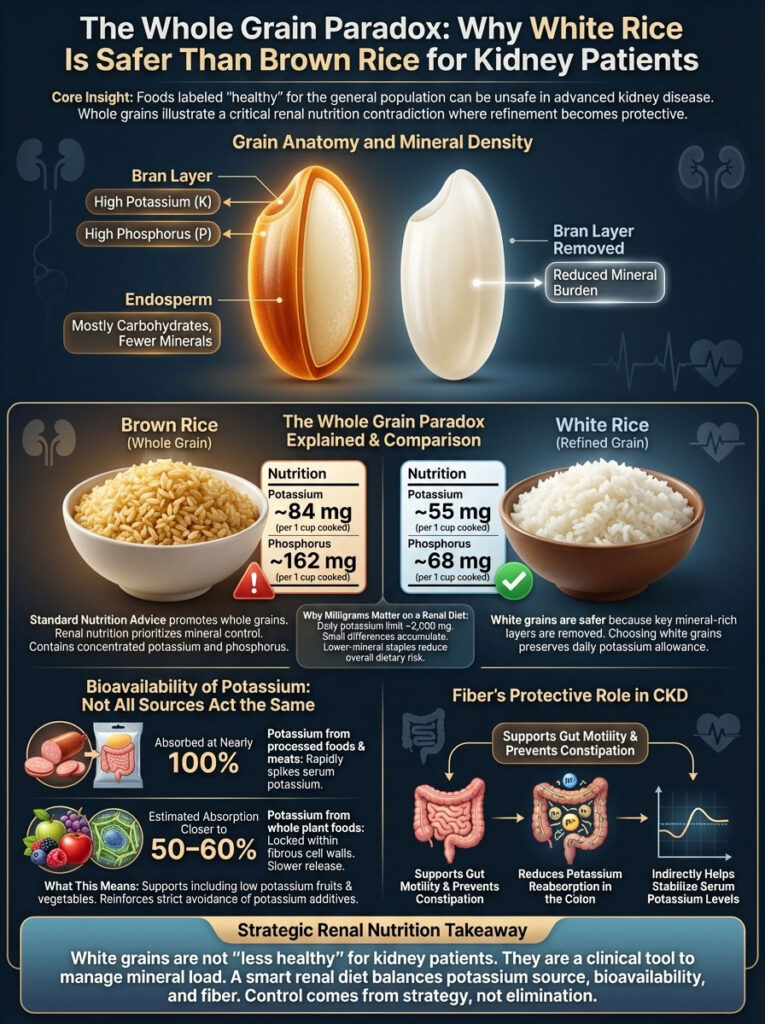
The Whole Grain Paradox: Why White Rice Is Safer Than Brown Rice for Kidney Patients
Bioavailability of Phosphorus and Potassium in Plant-Based vs Animal Sources
One of the most confusing aspects of a renal diet meal plan is the carbohydrate rule. General nutrition advice champions whole grains like brown rice and whole wheat bread. However, for a low potassium diet, these “healthy” grains are often on the “avoid” list. This is what we call the Whole Grain Paradox.
The reason lies in the anatomy of the grain. The bran, which is the outer layer of the grain, contains the highest concentration of phosphorus and potassium. White rice and white bread are processed to remove the bran. This processing significantly lowers the mineral content.
For example, a cup of cooked brown rice has about 84 mg of potassium and 162 mg of phosphorus. A cup of white rice has only 55 mg of potassium and 68 mg of phosphorus. When you are counting every milligram on a 2,000 mg potassium diet, choosing white products helps you save your allowance for nutrient-dense fruits and vegetables.
However, emerging research in nephrology is shifting how we view plant-based potassium. Studies suggest that the bioavailability of potassium from plant sources is different from animal sources. Potassium in processed foods and meats is absorbed at a rate of nearly 100%. However, potassium found in whole fruits and vegetables is locked within fibrous cell walls. Some research indicates that the body may only absorb 50% to 60% of the potassium from these fiber-rich sources.
This does not mean you can eat unlimited bananas. It does mean that a low potassium diet should not eliminate all fruits and vegetables. Instead, it should focus on low potassium foods like berries and apples while strictly limiting processed additives. High-fiber plant foods also help prevent constipation. This is crucial because constipation can actually cause potassium levels to rise as the gut reabsorbs waste.
Comprehensive 7-Day Renal Diet Menu and Daily Low Potassium Meal Plan
This renal diet meal plan is designed to keep you under the 2,000 mg limit while ensuring adequate protein and calories. Always consult your dietitian as protein needs vary depending on whether you are on dialysis. All “cups” refer to standard measuring cups. Do not use salt substitutes.

Day 1: The Foundation of Safe Eating
- Breakfast: 2 poached eggs on 1 slice of sourdough toast (white) with 1 tablespoon of unsalted butter. Served with a side of ½ cup fresh blueberries.
- Why this works: Eggs are a high-quality protein with low phosphorus compared to dairy. Blueberries are an antioxidant powerhouse with very low potassium.
- Lunch: Chicken salad made with ½ cup chopped boiled chicken breast, 1 tablespoon mayonnaise, and chopped celery on a white tortilla wrap. Serve with ½ cup of red grapes.
- Tip: Boil your own chicken breast rather than buying deli meat to avoid phosphate additives.
- Dinner: Lemon-garlic Tilapia (3 oz) baked with fresh dill and lemon slices. Served with ¾ cup steamed white rice and ½ cup green beans.
- Why this works: White fish is lower in phosphorus than red meat. Lemon adds flavor without sodium.
- Snack: 1 cup of plain popcorn (air-popped) with a drizzle of olive oil.
Day 2: Comfort Food Adjusted for Kidneys
- Breakfast: ¾ cup Cream of Wheat (made with water or rice milk) topped with 1 teaspoon of honey and ¼ cup sliced strawberries.
- Tip: Cream of Wheat is fortified with iron but much lower in potassium than oatmeal.
- Lunch: Turkey sandwich: 2 oz fresh roasted turkey (not deli slices) on white bread with lettuce, cucumber slices, and yellow mustard.
- Dinner: Herb-roasted chicken breast (3 oz) with ½ cup steamed carrots and ¾ cup couscous.
- Why this works: Couscous is a pasta alternative that cooks quickly and is kidney-friendly.
- Snack: ½ cup of unsweetened applesauce.
Day 3: The “Leached” Potato Day
- Breakfast: Scrambled egg whites (from 3 eggs) with 2 tablespoons of diced bell peppers and onions.
- Tip: Using egg whites eliminates the phosphorus found in the yolk.
- Lunch: Low-sodium tuna salad served with 6 unsalted saltine crackers and slices of cucumber.
- Warning: Check the tuna can label for “vegetable broth” or “soy” which often indicates added phosphates.
- Dinner: 3 oz Pork chop (grilled) served with ½ cup of leached mashed potatoes (see technique below) and ½ cup of boiled cabbage.
- Why this works: Leaching the potatoes makes a small portion safe for most patients.
- Snack: ½ cup of fresh pineapple chunks.
Day 4: Pasta Night and Italian Flavors
- Breakfast: Apple cinnamon oatmeal. Use old-fashioned oats (½ cup dry) cooked with water, diced apples (¼ cup), and cinnamon.
- Warning: Avoid instant oatmeal packets which are high in sodium and additives.
- Lunch: Pasta salad made with 1 cup cooked white pasta, diced red peppers, onions, and an oil-and-vinegar dressing. No tomatoes.
- Dinner: Shrimp stir-fry: 3 oz shrimp sautéed with garlic, 1 cup of mixed low-potassium vegetables (broccoli florets, peppers, onions) served over white rice.
- Tip: Use fresh shrimp. Frozen shrimp is often treated with sodium tripolyphosphate.
- Snack: Rice cakes (2) with unsalted butter or jam.
Day 5: Vegetarian Focus and Plant Proteins
- Breakfast: Renal-friendly smoothie: ½ cup rice milk, ½ cup mixed berries, and a scoop of protein powder (must be approved by dietitian).
- Lunch: Egg salad sandwich on white bread with a side of coleslaw (vinegar-based dressing, not creamy).
- Dinner: “Cauliflower Steaks”: Thick slices of cauliflower brushed with olive oil and herbs, roasted until tender. Serve with a white dinner roll and grilled chicken (optional).
- Why this works: Cauliflower takes on a meaty texture when roasted and is very low in potassium.
- Snack: Gelatin cup (check that it is not potassium-fortified) with whipped topping.
Day 6: The Weekend Brunch
- Breakfast: French Toast: 2 slices of white bread dipped in egg whites and a splash of vanilla extract. Fried in a pan and topped with syrup.
- Lunch: Leftover chicken wrap from Day 1 or a simple grilled chicken breast.
- Dinner: The “No-Tomato” Burger: 3 oz ground beef patty (lean) on a white bun with lettuce, onion, and mayonnaise. Side of raw carrot sticks.
- Tip: Ketchup is high in sugar and sodium. Try a little mustard or mayonnaise instead.
- Snack: 1 small apple.
Day 7: Sunday Roast
- Breakfast: Omelet made with 2 eggs, mushrooms, and onions. Slice of white toast.
- Lunch: Grilled cheese sandwich on sourdough bread using 1 slice of mild cheddar cheese. Side of canned pears (drained of syrup).
- Dinner: 3 oz Roast Beef with Yorkshire pudding (or white roll) and ½ cup glazed carrots.
- Tip: Avoid using the beef drippings for gravy as they contain concentrated potassium.
- Snack: Shortbread cookies (3 small cookies).
Advanced Cooking Techniques to Lower Potassium Content in High Risk Vegetables
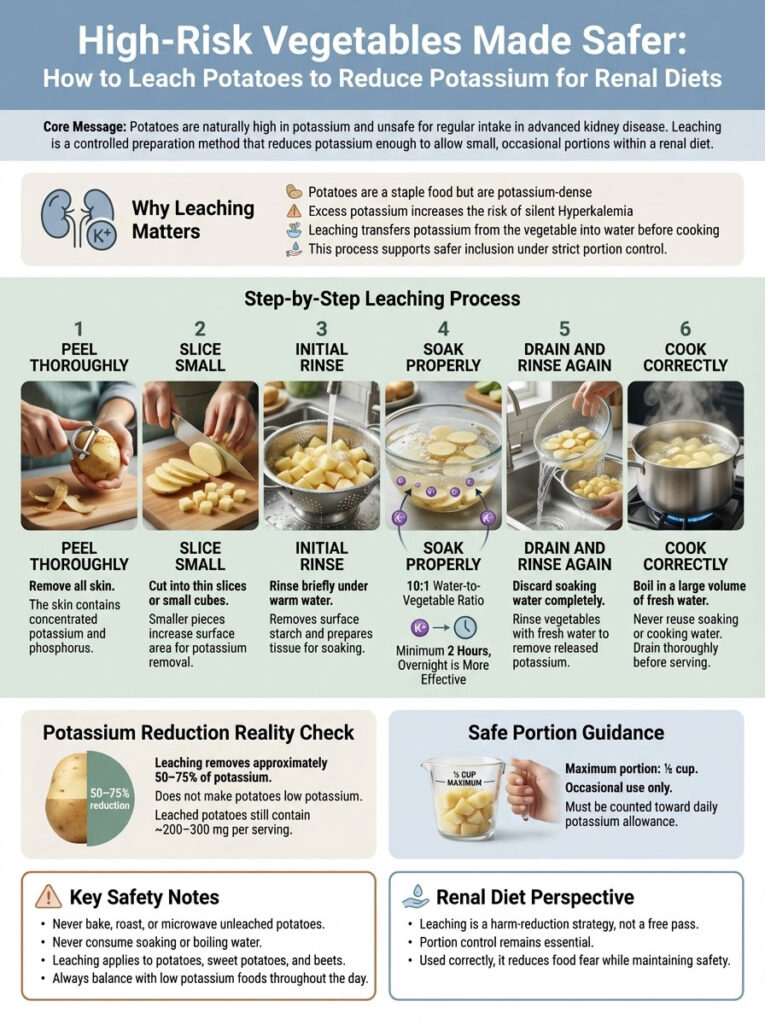
Step-by-Step Guide on How to Leach Potatoes to Reduce Potassium Levels
You may miss potatoes. They are a staple of the American diet. While they are on the list of foods to avoid with kidney disease, you can make them safer through a process called leaching. This technique pulls some of the potassium out of the vegetable and into the water.
Step-by-Step Leaching Guide:
- Peel: Peel the potatoes, sweet potatoes, or beets thoroughly. The skin holds nutrients that you need to avoid.
- Slice: Cut the vegetable into thin slices or small dice. The smaller the piece, the more surface area is exposed to the water which aids extraction.
- Rinse: Rinse the vegetables in warm water for a few seconds to remove surface starch.
- Soak: Place the vegetables in a large pot of warm water. Use a ratio of at least 10 parts water to 1 part vegetable. Let them soak for at least 2 hours. If you can soak them overnight, that is even better.
- Rinse Again: Drain the soaking water. Rinse the vegetables one more time with fresh water.
- Cook: Boil the vegetables in a large amount of fresh water. Drain well before eating.
Does this remove all potassium?
No. Leaching potatoes removes about 50% to 75% of the potassium. A serving of leached potatoes still contains significant potassium (around 200-300 mg), so you must still limit your portion to ½ cup. However, it makes an occasional treat possible within a renal diet meal plan.
Strategies for Eating Out and Managing Social Meals on a Kidney Friendly Diet

Navigating Fast Food Menus to Find Low Potassium and Low Sodium Options
Socializing is important for mental health, but restaurants are difficult for a low potassium diet. Fast food is typically high in sodium and phosphorus. However, you can navigate the menu with these specific strategies.
Strategy 1: Avoid the Potato.
The biggest offender in fast food is the French fry. A medium fry is loaded with potassium. Swap fries for a side salad (no tomatoes) or apple slices if available. If no side is safe, simply order the sandwich alone.
Strategy 2: The “Plain” Burger.
Order a hamburger or grilled chicken sandwich plain. Ketchup and tomatoes add potassium. Ask for mustard, mayonnaise, lettuce, and onion. Pickles add sodium, so ask for them on the side or omit them.
Strategy 3: Grilled over Fried.
Fried foods often contain phosphate additives in the breading to keep it crispy. Choose grilled chicken or broiled fish whenever possible.
Strategy 4: Asian Cuisine Caution.
Soy sauce is extremely high in sodium, but Asian food can be managed. Order steamed white rice (not fried rice, which is higher in sodium/potassium). Choose stir-fried dishes with vegetables like broccoli and peppers. Ask for the sauce on the side or “light sauce.”
Best Fast Food Bets:
- Grilled chicken sandwich on a white bun (no tomato).
- Single hamburger (no cheese, no tomato).
- Egg McMuffin style sandwich (no meat, or limit meat).
- Steamed rice and vegetable bowls.
Worst Offenders:
- Pizza (tomato sauce + cheese + processed meat = triple threat).
- Loaded baked potatoes.
- French fries and onion rings.
- Milkshakes (extremely high in potassium and phosphorus).
Clinical Impact of Dietary Compliance on Serum Potassium and GFR Stability
Does a strictly managed renal diet meal plan actually work? Clinical observations suggest it significantly impacts patient stability and can delay the need for dialysis.

Consider a hypothetical patient scenario involving “Michael,” a patient with Stage 4 CKD. His GFR was 22, and his serum potassium levels were consistently hovering around 5.8 mEq/L (Hyperkalemia). He was consuming a “healthy” diet rich in avocados, bran cereal, and orange juice.
After switching to a low potassium diet of 2,000 mg/day, eliminating potassium chloride additives, and swapping brown rice for white, his potassium levels dropped to 4.6 mEq/L within three weeks. This allowed him to avoid emergency dialysis and stabilized his heart rhythm.
Below is a breakdown of how the nutrient profile changes when switching from a standard diet to the 7-day plan outlined above.
| Nutrient | Standard American Diet (Avg) | This 7-Day Renal Plan | Recommended Limit (Stage 4) |
| Potassium | 3,500 mg – 4,700 mg | ~1,800 mg – 2,000 mg | < 2,000 mg |
| Sodium | 3,400 mg+ | ~1,500 mg | < 2,000 mg |
| Phosphorus | 1,400 mg+ | ~800 mg – 1,000 mg | ~800 mg – 1,000 mg |
| Protein | Excessive (>1.2g/kg) | Moderate (0.6-0.8g/kg) | Varies by patient/dialysis |
This data illustrates that a calculated renal diet meal plan brings all major markers into the safety zone. This reduction in dietary load reduces the workload on the kidneys, potentially preserving residual function for longer.
Frequently Asked Questions About Low Potassium Diets and Renal Nutrition
What breakfast foods are low in potassium?
Good options include Cream of Wheat, grits, white toast, bagels, and eggs. Fruits like apples, berries, and grapes are safe sides. Avoid bran cereals, granola, and orange juice as they are very high in potassium.
Can I eat eggs on a renal diet?
Yes, eggs are an excellent protein source for kidney patients. They are naturally low in potassium. However, the yolk contains phosphorus. If you need to limit phosphorus, use egg whites, which are pure protein and very kidney-friendly.
How do I lower my potassium levels quickly?
Dietary changes take time to reflect in blood work. To lower intake immediately, eliminate the “Big Four”: Potatoes, Tomatoes, Bananas, and Avocados. Also, stop using any salt substitutes containing potassium chloride. If your levels are critically high, go to the emergency room.
Is drinking water helpful for flushing out potassium?
For healthy kidneys, water helps. For Stage 4-5 CKD, drinking more water does not flush out potassium because your kidneys cannot filter it efficiently. In fact, many kidney patients have a fluid restriction. Follow your doctor’s fluid guidelines strictly.
Are sweet potatoes safer than white potatoes for kidney disease?
No. Sweet potatoes are actually higher in potassium than white potatoes. Both are among the foods to avoid with kidney disease unless they are leached and eaten in very small portions.
What is the best bread for kidney patients?
Sourdough, white bread, and French bread are the best choices. They generally contain less potassium and phosphorus than whole wheat or multigrain breads. Always check labels for additives.
Is oatmeal high in potassium?
Oatmeal is moderate to high. Instant oatmeal often has added salts and phosphates. Old-fashioned oats are better but still contain more potassium than Cream of Wheat. If you eat oatmeal, limit it to a small serving.
Can I drink coffee if I have high potassium?
Yes, but in moderation. A standard cup of black coffee has about 116 mg of potassium. The danger is often the milk or creamer added to it. Limit intake to 1-2 cups per day and use non-dairy, low-potassium creamers if possible.
What are the symptoms of hyperkalemia?
High potassium is often symptomless. When symptoms do occur, they include nausea, muscle weakness, numbness or tingling, and an irregular heartbeat. Sudden cardiac arrest can happen without warning, which is why diet is crucial.
Which fruits are safe for Stage 4 kidney disease?
The safest fruits are apples, grapes, strawberries, blueberries, raspberries, pineapple, and cranberries. These are all considered low potassium foods.
Is salad safe for a low potassium diet?
Yes, if you choose the right greens. Iceberg lettuce, romaine lettuce, and cabbage are safe. Spinach, Swiss chard, and beet greens are very high in potassium and should be avoided. Watch your dressing choice as well.
What fast food can I eat with kidney disease?
The safest fast food is a grilled chicken sandwich (no tomato) or a plain hamburger with a side salad. Avoid french fries, milkshakes, and anything with heavy tomato sauce (like pizza).
Disclaimer
This article is for educational purposes only and does not constitute medical advice. Chronic Kidney Disease (CKD) is a complex condition, and individual dietary needs vary based on labs, dialysis status, and other comorbidities (like diabetes). Always consult a Board Certified Nephrologist or a Registered Renal Dietitian before making significant changes to your diet.
References
- National Kidney Foundation (NKF): Potassium and Your CKD Diet Guidelines.
- KDOQI (Kidney Disease Outcomes Quality Initiative): Clinical Practice Guidelines for Nutrition in CKD.
- USDA FoodData Central: Nutrient content data for potassium and phosphorus in common foods.
- American Kidney Fund: Hyperkalemia management and low-potassium food lists.








