Introduction
The sudden onset of sharp, piercing pain in the lower left abdomen is a distinct and terrifying experience for millions of Americans. It marks the beginning of a diverticulitis flare-up. In that moment of discomfort. the immediate question is not about medication or surgery. but rather a desperate inquiry into what to eat with diverticulitis to stop the pain.
Table of Contents
Navigating this condition is confusing. One day you are told to eat more fiber to stay healthy. the next you are told fiber is the enemy that will worsen your infection. This contradiction leaves patients paralyzed in the grocery store aisle. afraid that a single wrong bite could lead to a hospital stay. The truth is that nutritional management for diverticular disease is not static. It is a dynamic. three-stage evolution that changes as your body heals.
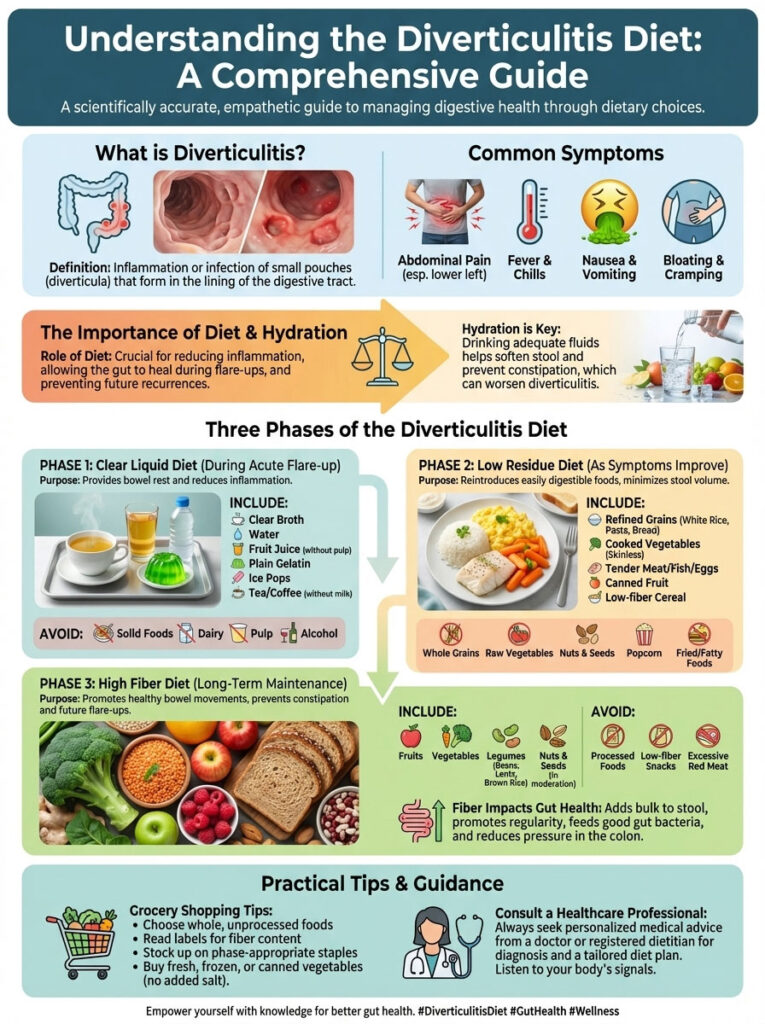
This guide serves as a comprehensive medical roadmap. We will move beyond surface-level advice and explore the deep biological mechanisms of the diverticulitis diet. You will learn exactly how to transition from the clear liquid diet phase of total bowel rest. through the low residue diet recovery phase. and finally to the high fiber diet maintenance lifestyle. By understanding the physiology of your sigmoid colon and adhering to this evidence-based protocol. you can reduce inflammation. restore your gut microbiome. and regain control over your digestive health.
Understanding the Diverticular Disease Spectrum and Colon Physiology
To truly master your diet. you must first understand the anatomy of the condition you are managing. The large intestine. specifically the sigmoid colon. is the final processing center for waste. Over decades of processing hard. processed foods. high pressure within the colon can cause weak spots in the muscular wall to bulge outward.

Differentiating Between Diverticulosis and Diverticulitis Diet Protocols
These bulging pouches are known anatomically as diverticula. The presence of these pouches without symptoms is called diverticulosis. It is incredibly common in the USA. affecting nearly half of all people over the age of 60. When you have diverticulosis. your goal is prevention.
Diverticulitis occurs when one or more of these pouches become inflamed or infected. causing micro-perforations. This is the acute phase that triggers fever. nausea. and that distinct lower-left abdominal pain. The dietary strategy for a diverticulosis vs diverticulitis diet is completely opposite. While diverticulosis requires fiber to keep stool moving. active diverticulitis requires you to stop all fiber intake immediately to allow the bowel to rest. Confusing these two stages is the most common mistake patients make.
The Role of Intracolonic Pressure in Digestive Inflammation
Why do these pouches get infected? The leading medical theory involves intracolonic pressure. If your diet lacks bulk. the colon must contract violently to move small. hard stools. This pressure blows out the colon wall like a tire bubble.
During a diverticulitis flare-up diet. our primary goal is to drastically reduce this workload. We want to remove any solid waste that could irritate the inflamed pouch. Think of an inflamed colon like a sprained ankle. you would not run a marathon on it immediately. You would rest it. The same logic applies to your digestive tract. This is why “bowel rest” is the foundational concept of the first stage of recovery.
New AGA Guidelines on Antibiotics and Dietary Management
For decades. the standard treatment for any flare-up was a heavy course of antibiotics like Ciprofloxacin and Metronidazole. However. the American Gastroenterological Association (AGA) has updated its clinical guidelines. Recent data suggests that for uncomplicated diverticulitis. antibiotics may not always be necessary.
This shift places even more importance on what to eat with diverticulitis. In many mild cases. a strictly adhered-to liquid diet followed by a careful low residue diet is now the primary treatment. This approach spares your gut microbiome from the nuclear effect of antibiotics. making nutritional discipline the most powerful tool in your recovery kit.
Stage 1: The Clear Liquid Diet for Immediate Bowel Rest
When the pain is acute. severe. and accompanied by a fever or nausea. you must initiate Stage 1 immediately. The objective here is Total Bowel Rest. By removing all solids. you reduce stool volume to near zero. allowing the inflammation in the sigmoid colon to subside without mechanical irritation.
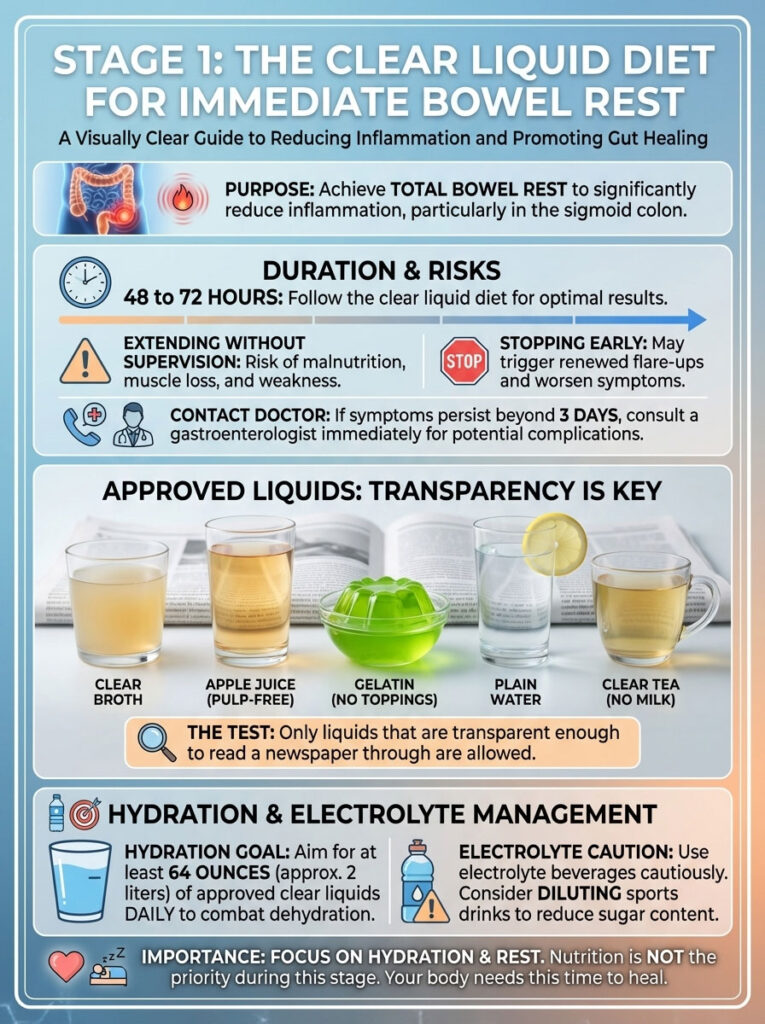
Implementing the 72-Hour Liquid Diet Protocol
The clear liquid diet should typically last between 48 to 72 hours. This is the critical window for inflammation to decrease. Extending it beyond this timeframe without medical supervision can lead to malnutrition and muscle weakness. Conversely. stopping it too soon can reignite the flare-up. If your symptoms do not improve after three days of liquids. it is vital to contact your gastroenterologist. as this may indicate a complication such as an abscess or fistula requiring hospitalization. This stage is not about nutrition. it is about hydration and rest. You are essentially putting your digestive system in “sleep mode” while maintaining electrolyte balance.
Approved Clear Liquids for the Diverticulitis Flare-Up Diet
Strict adherence is required here. “Clear” is the operative word. you should be able to read a newspaper through the liquid.
- Bone Broth and Consommé: This is superior to standard water. High-quality bone broth provides essential amino acids. collagen. and electrolytes that support the gut lining during stress.
- Clear Fruit Juices: Apple. cranberry. and white grape juice are excellent choices. You must avoid orange juice. grapefruit juice. or any nectar that contains pulp. as the fiber in the pulp activates digestion.
- Gelatin (Jell-O): A staple of the hospital diet for a reason. It provides small amounts of sugar for energy. Note: Avoid red or purple dyes if you are scheduled for a colonoscopy or imaging. as these can mimic blood in the intestinal tract.
- Ice Pops and Fruit Ices: Choose fruit-flavored ice pops without real fruit chunks. seeds. or dairy cream.
- Tea and Coffee: You can consume these. but they must be black. No milk. cream. soy milk. or non-dairy creamers are allowed yet. Caffeine can stimulate the bowel. so decaffeinated versions are often safer if you are sensitive.
Electrolyte Management and Hydration Strategy
Diarrhea and fever often accompany a flare-up. leading to rapid systemic dehydration. You should aim for at least 64 ounces of liquid daily. Electrolyte beverages can be helpful. but be wary of high sugar content which can sometimes worsen diarrhea by drawing water into the gut. Diluting sports drinks with water is often a smart strategy.
Stage 2: Low-Residue Diet for Safe Recovery and Healing
Once your pain decreases significantly. your appetite returns. and you have no fever. you can transition to Stage 2. This is often the most confusing phase for patients. You might feel hungry. but your colon is still fragile and healing. We use a low residue diet here to reintroduce solids gently.
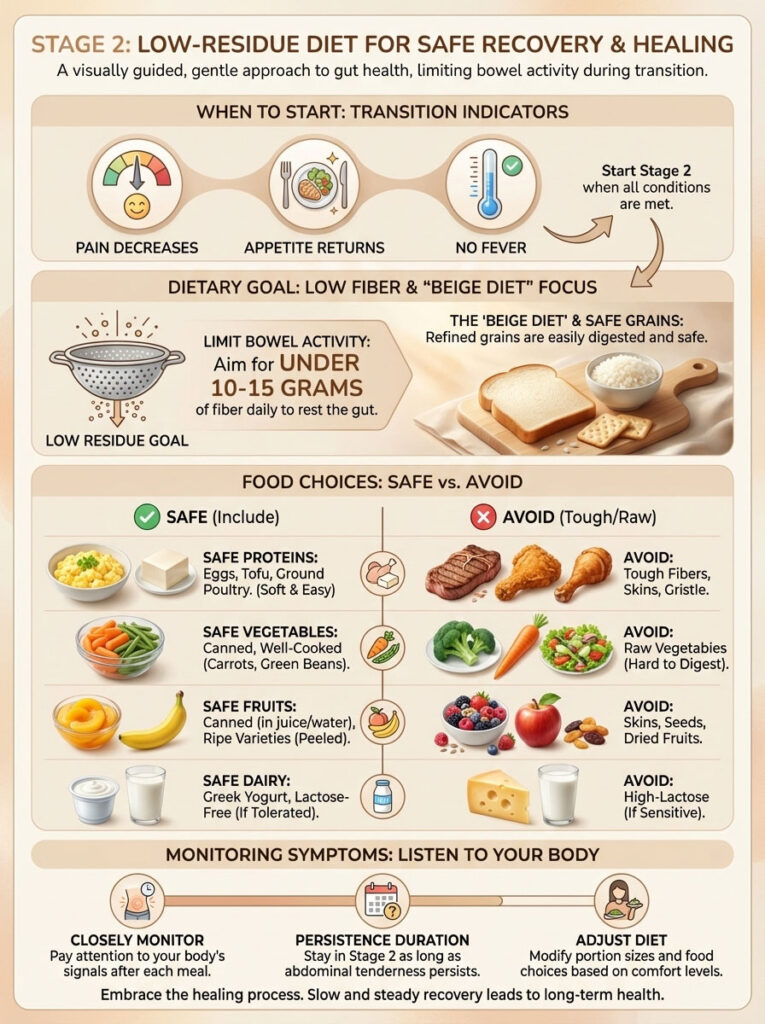
Defining Low-Residue vs Low Fiber Guidelines
A low residue diet is a specific medical subset of a low-fiber diet that also limits foods that increase bowel activity. such as dairy (for some) and prune juice. The goal is to keep daily fiber intake under 10 to 15 grams. This ensures that the stool remains small. soft. and passes easily without scraping the healing diverticula.
The “Beige Diet” Strategy for Gut Healing
We often call this the “Beige Diet” because safe foods tend to be white or light-colored refined grains. While nutritionists usually demonize processed grains. they are medicinal in this specific context.
- White Rice: Well-cooked white rice is easily digested and helps bind loose stool.
- White Bread: Sourdough. French bread. or standard white bread are safe options. You must strictly avoid whole wheat. multigrain. rye. or any bread with visible seeds or nuts.
- Refined Pasta: Standard white pasta cooked until soft is an excellent energy source.
- Crackers: Saltines. soda crackers. or oyster crackers can help settle nausea and provide calories without bulk.
Safe Proteins and Canned Vegetable Options
Protein is essential for tissue repair and immune function. However. you must avoid gristle. skin. and tough muscle fibers.
- Eggs: Scrambled or poached eggs are arguably the perfect Stage 2 food. They provide a complete amino acid profile with zero fiber.
- Poultry: Baked or poached chicken breast and turkey are safe. Ensure they are skinless and not fried.
- Fish: White fish like cod. tilapia. or halibut is gentle on the stomach.
- Canned Tuna: Packed in water (not oil). this provides easy protein.
- Vegetables: You can reintroduce vegetables. but they must be canned or cooked to a mushy consistency. Canned green beans. carrots without skin. and skinless baked potatoes are standard. The cooking process breaks down the cellular walls of the vegetables. doing the work your stomach would usually do.
Analysis of Foods to Avoid with Diverticulitis in Stage 2
It is critical to know foods to avoid with diverticulitis during this delicate transition. Eating the wrong thing here causes a “rebound” flare-up.
| Food Category | Safe for Stage 2 (Recovery) | Unsafe / Avoid in Stage 2 | Reason for Avoidance |
| Grains | White rice, white pasta, sourdough, cream of wheat | Brown rice, quinoa, oatmeal, bran cereal | Insoluble fiber irritates healing tissue. |
| Vegetables | Canned carrots, green beans, peeled potatoes | Raw salads, corn, broccoli, cauliflower, skins | Raw fiber is hard to digest and causes gas. |
| Proteins | Eggs, tofu, ground poultry, white fish | Steak, sausage, lentils, kidney beans | Tough fibers and skins increase stool bulk. |
| Fruits | Canned peaches, applesauce, ripe bananas | Berries, raw apples, pineapple, dried fruit | Seeds and skins are high residue. |
| Dairy | Greek yogurt, cottage cheese, hard cheese | High-lactose milk (if sensitive), ice cream with nuts | Lactose can cause bloating in inflamed guts. |
Monitoring Symptoms During the Transition Phase
You should remain in Stage 2 for as long as you have any tenderness. For some patients. this is a few days. for others. it is a few weeks. Listen to your body. If you eat a piece of toast and feel cramping. step back to liquids for 12 hours. There is no rush. Healing the mucosal lining of the colon takes time.
Stage 3: High-Fiber Maintenance Diet for Long-Term Prevention
You should only move to Stage 3 when you are completely symptom-free. This usually happens a few weeks after the initial attack. The diverticulitis diet strategy now flips 180 degrees. Long-term studies show that a high fiber diet is the gold standard for preventing recurrence.
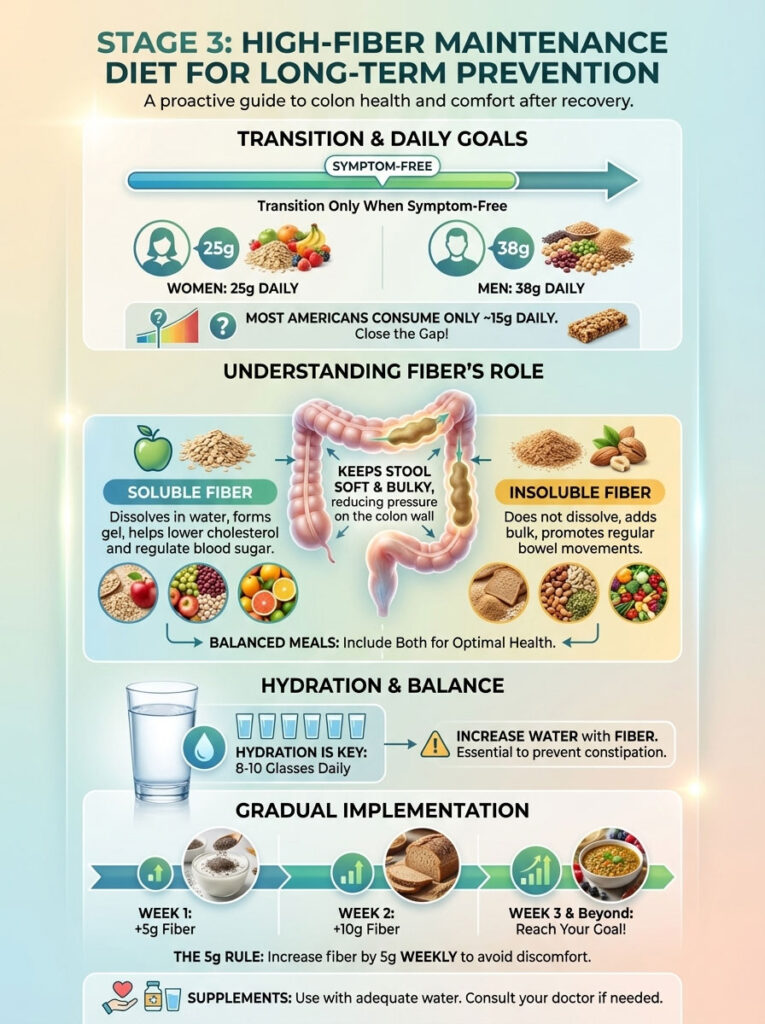
Establishing Daily Fiber Intake Goals
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recommends a daily fiber intake of 25 grams for women and 38 grams for men. Most Americans only consume about 15 grams per day. This chronic deficit is a primary driver of diverticular disease. By keeping the stool soft and bulky. fiber reduces the pressure required to move waste. preventing new pouches from forming and old ones from tearing.
Soluble vs Insoluble Fiber Mechanisms
Understanding fiber types helps you build a balanced plate that promotes colon health.
- Soluble Fiber: This dissolves in water to form a gel-like substance. It helps with soft. formed stools and feeds beneficial gut bacteria. Primary sources include oats. apples (without skin). flaxseed. and psyllium husk.
- Insoluble Fiber: This does not dissolve. It adds bulk and speeds up the passage of food through the digestive tract. reducing the time waste sits in your colon. Sources include whole wheat bran. vegetables. and fruit skins.
A healthy diverticulitis diet includes a mix of both. but starting with higher soluble fiber is often more comfortable.
The Hydration Equation and Fiber Supplements
There is a catch to the high fiber diet. Fiber works by absorbing water. If you increase your fiber intake without increasing your water intake. the fiber effectively turns into cement in your colon. This leads to constipation and increased pressure. the exact opposite of our goal.
Rule of Thumb: For every significant increase in fiber. add another glass of water. Aim for 8 to 10 glasses (80 oz) of clear fluids daily. If you use supplements like psyllium husk or methylcellulose. you must drink a full glass of water with the dose and another immediately after.
The “5g Rule” for Safe Dietary Transitioning
Do not jump from 10g of fiber to 35g overnight. This will cause severe bloating. cramping. and gas. Follow the “5g Rule”. increase your daily fiber intake by only 5 grams each week. This slow ramp-up allows your gut bacteria to adjust to the new fuel source without producing excessive gas.
Debunking Dietary Myths: Nuts, Seeds, and Red Meat
For decades. doctors told patients to avoid nuts. seeds. corn. and popcorn. fearing these small particles would physically get stuck in the pouches and cause infection. We now know this advice is scientifically incorrect.
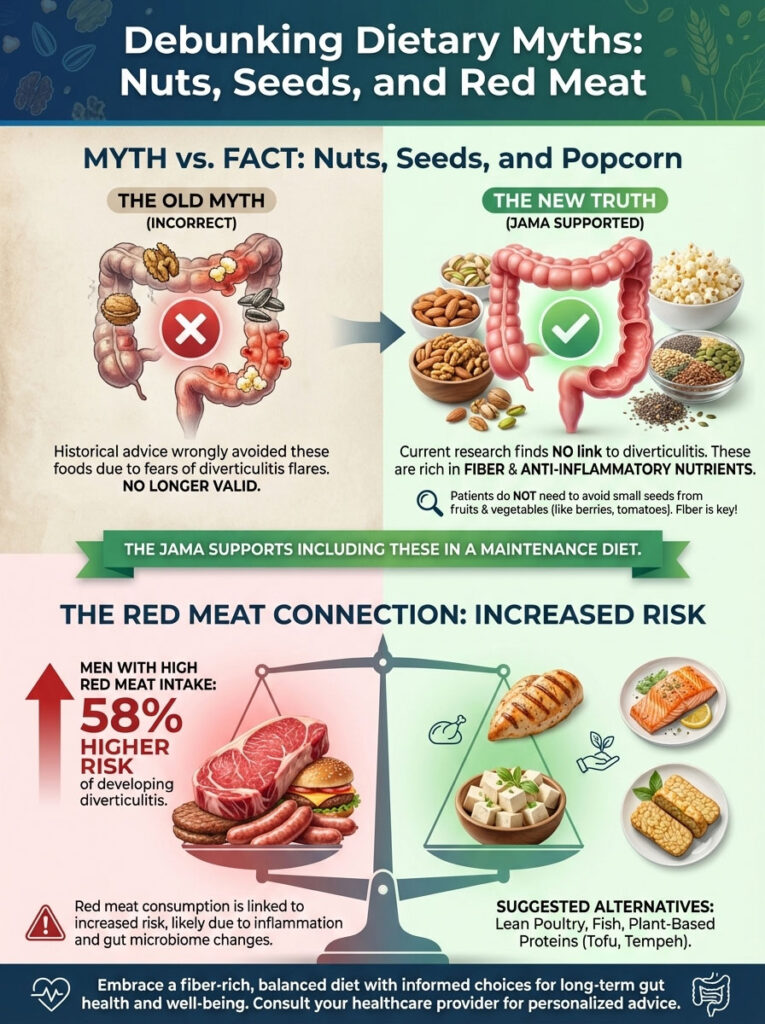
The Truth About Popcorn and Seeds Consumption
Current research. including massive datasets from the Health Professionals Follow-up Study. has proven there is no correlation between nut. corn. or popcorn consumption and diverticulitis. In fact. these foods are high in fiber and anti-inflammatory nutrients. The JAMA (Journal of the American Medical Association) has published findings supporting the inclusion of these foods in a diverticulitis maintenance diet. You do not need to spend your life avoiding strawberry seeds. tomatoes. or sesame buns.
The Real Villain: Unprocessed Red Meat Risks
While seeds are innocent. red meat appears to be guilty. Research indicates that high consumption of red meat. particularly unprocessed beef. lamb. and pork. is associated with an increased risk of diverticulitis. Studies show that men who consume the most red meat have a 58% higher risk of developing the condition compared to those who eat the least.
To optimize your diverticulitis diet. replace steaks and burgers with lean poultry. fish. or plant-based proteins like tofu and tempeh.
Optimizing Gut Health: Probiotics and Lifestyle Factors
Beyond the macronutrients of fiber and protein. your microscopic gut environment plays a huge role in recovery and prevention.
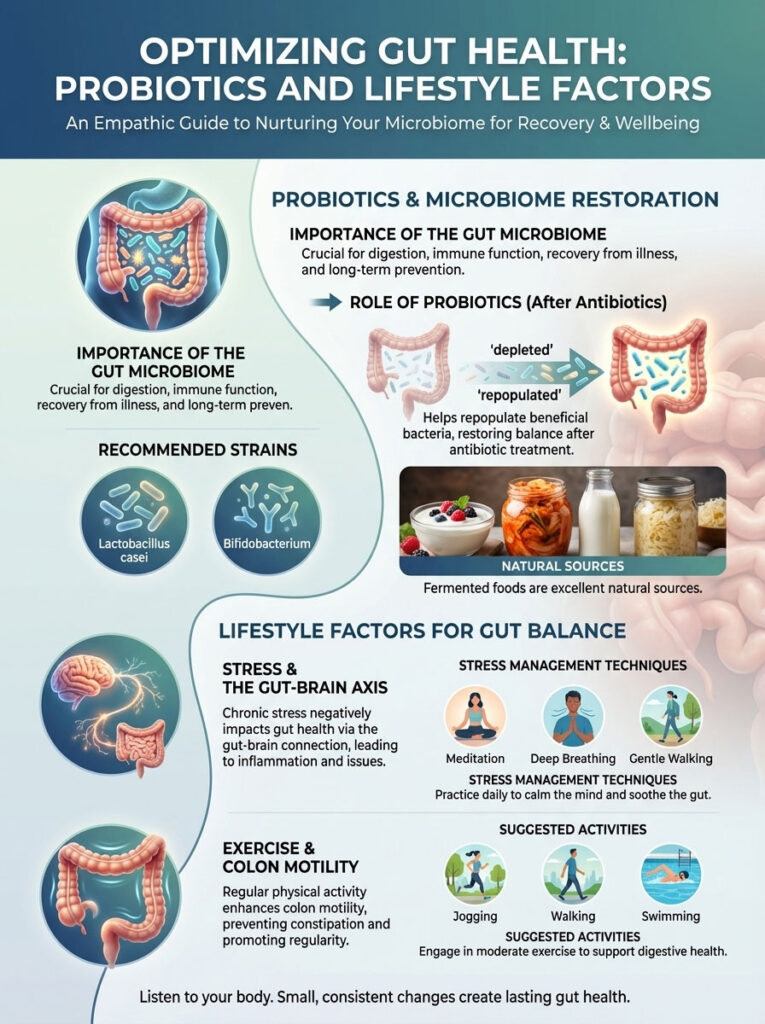
Restoring the Microbiome with Probiotics
If your treatment involved antibiotics. your gut microbiome has been depleted. Repopulating the gut with beneficial bacteria is crucial. Probiotics for diverticulitis show promise in reducing bloating and recurrence.
Look for strains like Lactobacillus casei and Bifidobacterium. Fermented foods are excellent natural sources:
- Kefir: A fermented milk drink that is often 99% lactose-free and packed with cultures.
- Yogurt: Choose plain Greek yogurt with “live active cultures” listed on the label.
- Miso: Fermented soybean paste used in soup.
- Sauerkraut: Ensure it is raw/refrigerated. as heat-treated shelf-stable versions lack live bacteria.
Stress Management and the Gut-Brain Axis
The connection between your brain and your gut is powerful. High stress levels can increase gut sensitivity and inflammation via the vagus nerve. While stress does not cause the pouches to form. it can certainly trigger a flare-up or make the pain perception worse. Incorporating gentle walking. deep breathing. or meditation can be a functional part of your diverticulitis recovery timeline.
Exercise and Colon Motility Improvement
Physical activity stimulates normal bowel contractions. known as peristalsis. A sedentary lifestyle is a major risk factor for constipation. Regular jogging. walking. or swimming helps keep the digestive system “awake” and moving. complementing your high fiber diet.
Comprehensive 3-Stage Food Guide Comparison
To simplify your planning. the following table breaks down food choices across the entire recovery spectrum. giving you a quick reference for any stage of your journey.
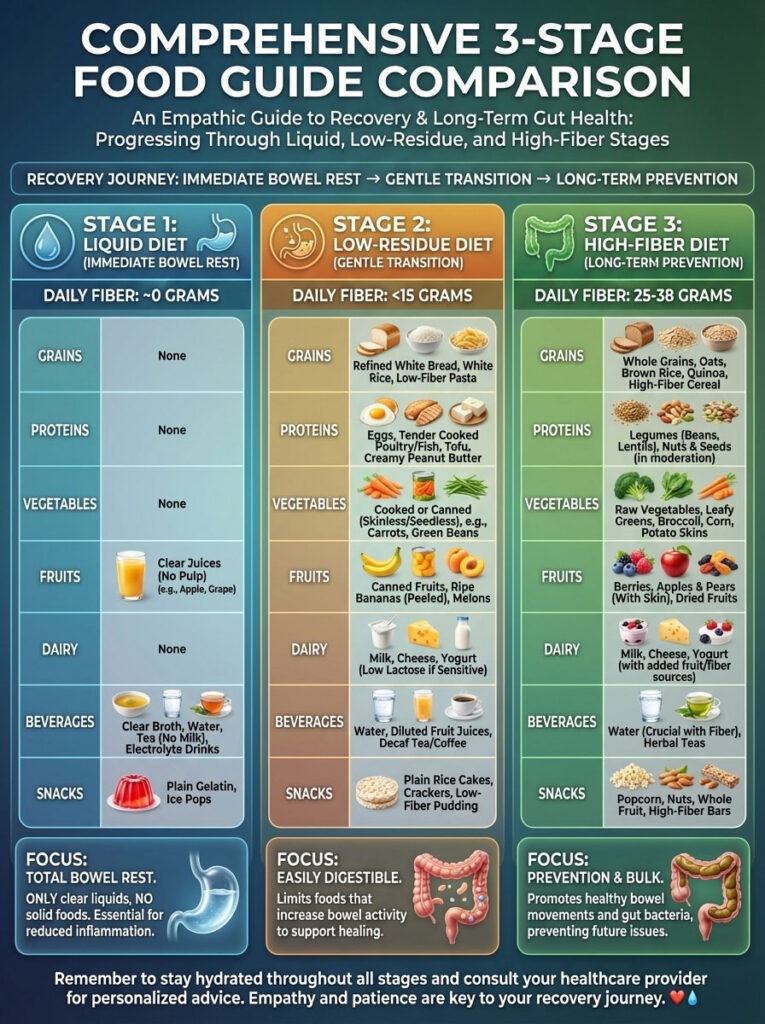
| Food Category | Stage 1: Liquid (Acute Pain) | Stage 2: Low-Residue (Recovery) | Stage 3: High-Fiber (Prevention) |
| Fiber Goal | ~ 0 grams | < 15 grams per day | 25 – 38 grams per day |
| Grains | None (Liquids only) | White rice, white pasta, sourdough | Brown rice, quinoa, bran, oats |
| Proteins | Bone broth, gelatin | Eggs, tofu, tender chicken | Black beans, lentils, nuts |
| Vegetables | None | Canned green beans, peeled potatoes | Broccoli, kale, raw carrots, salads |
| Fruits | Clear juice (Apple/Grape) | Canned peaches, ripe bananas | Apples with skin, berries, pears |
| Dairy | None | Greek yogurt, cottage cheese | Kefir, milk (if tolerant) |
| Beverages | Water, tea, clear juice | Water, herbal tea | Water, smoothies with seeds |
| Snacks | Ice pops | Saltines, applesauce | Popcorn, trail mix, almonds |
Frequently Asked Questions (FAQ)
Can I eat eggs with diverticulitis?
Yes. Eggs are one of the best foods for the Stage 2 low residue diet. They provide high-quality protein without fiber. making them easy to digest. Scrambled or poached eggs are gentle on an inflamed colon and provide essential nutrients for healing.
How long does a diverticulitis flare-up last?
Most uncomplicated flare-ups begin to subside within 2 to 4 days of starting antibiotics or the clear liquid diet. However. complete healing of the colon wall can take several weeks. You should remain on the low-residue plan until you are completely pain-free to avoid a relapse.
Is peanut butter safe during a flare-up?
Creamy peanut butter is safe during Stage 2 because it is low in fiber and high in protein. You must avoid chunky peanut butter until you reach Stage 3. as the nut pieces can be irritating to a sensitive gut.
Do tomato seeds cause diverticulitis?
No. This is an outdated myth. There is no scientific evidence that tomato seeds. cucumber seeds. or strawberry seeds cause inflammation in the diverticula. They are safe to eat in the maintenance phase.
Can I drink alcohol while recovering?
It is best to avoid alcohol during a flare-up. Alcohol irritates the lining of the stomach and colon and can interact negatively with antibiotics. causing nausea. Once you are fully recovered. moderate consumption is generally acceptable.
What is the best fiber supplement?
Psyllium husk (often found in Metamucil) is widely considered the gold standard for diverticulitis diet maintenance. It is a soluble fiber that regulates bowel movements without being as harsh as insoluble bran.
Is coffee bad for diverticulitis?
During an acute attack (Stage 1). coffee can stimulate the bowel too aggressively and cause dehydration. It is better to avoid it or limit it strictly. In recovery and maintenance. moderate coffee consumption is safe for most people.
Can stress cause a flare-up?
While stress does not create the diverticula pouches. it affects gut motility and inflammation. Many patients report flare-ups during periods of high emotional stress. Managing stress is part of a holistic diverticulitis recovery timeline.
Why is my pain on the left side?
The sigmoid colon. where high pressure is most common due to its narrow diameter. is located in the lower left quadrant of the abdomen. This is why left-sided pain is the classic symptom of diverticulitis.
Are bananas good for diverticulitis?
Yes. Ripe bananas are an excellent Stage 2 food. They are soft. low in fiber (compared to other fruits). and high in potassium. which helps restore electrolytes lost during diarrhea.
Should I eat yogurt?
Yes. Yogurt. specifically varieties with live active cultures. is beneficial. It provides protein and probiotics that help restore gut health. Avoid yogurts with high sugar or fruit chunks during the early recovery phase.
When can I start eating salad again?
You should wait until you are completely pain-free and have successfully tolerated cooked vegetables and fruits for several weeks. Salad represents raw. insoluble fiber. which is the hardest texture for your colon to process.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a gastroenterologist or medical professional for diagnosis and treatment of diverticulitis.
References:
- American Gastroenterological Association (AGA) Clinical Guidelines.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
- Journal of the American Medical Association (JAMA) – Nut, Corn, and Popcorn Consumption and the Incidence of Diverticular Disease.
- Health Professionals Follow-up Study (Harvard T.H. Chan School of Public Health).








