A clear liquid diet for diverticulitis is a temporary medical intervention used to induce “bowel rest” during an acute flare-up. By consuming only transparent fluids like clear broth, pulp-free juices, and electrolyte-rich beverages, patients can significantly reduce colonic pressure and inflammation. This protocol is typically prescribed for 48 to 72 hours. If abdominal pain does not improve within 24 hours of starting this diet, immediate medical attention is required to rule out complications such as perforation or abscesses.
Table of Contents
You know the specific, terrifying signal. It usually begins as a subtle, nagging discomfort that rapidly escalates into a sharp, localized cramping pain in the lower left quadrant of your abdomen. For the millions of Americans diagnosed with diverticular disease, this sensation is the herald of a flare-up. It means the small pouches in your colon, known as diverticula, have become inflamed or infected.
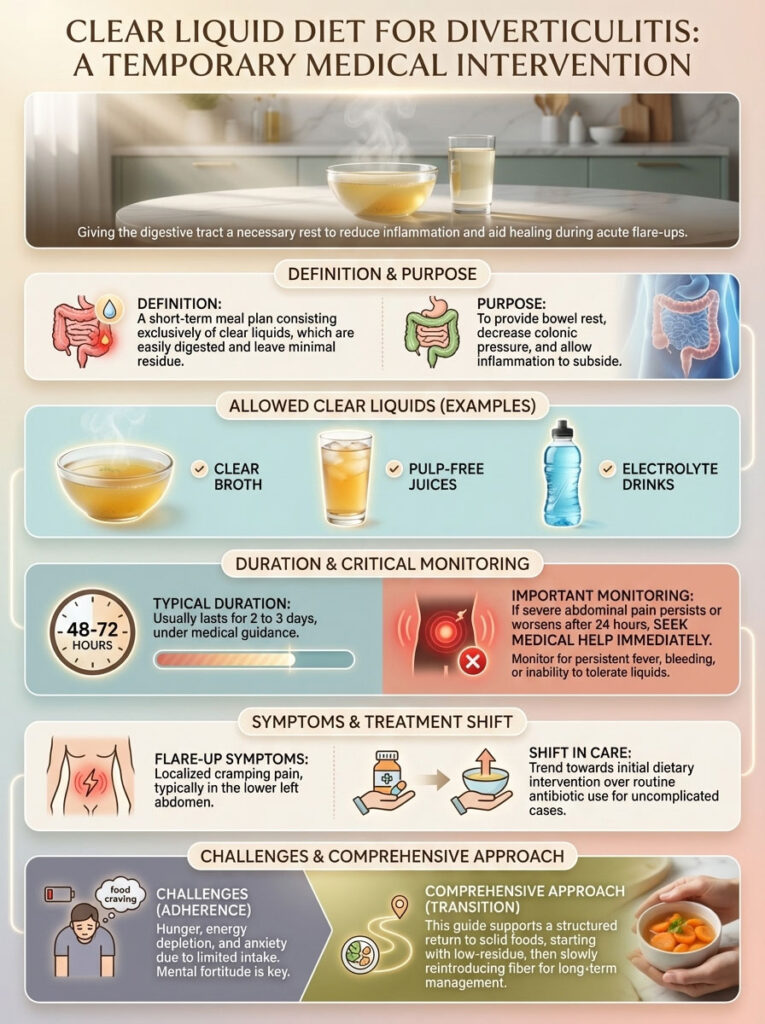
Your immediate priority shifts from daily life to crisis management. The goal is to prevent this localized infection from spiraling into a systemic emergency that requires hospitalization or surgery. While antibiotics were once the automatic first step, modern gastroenterology has shifted toward a more holistic initial approach. The primary defense mechanism is now a strategic dietary intervention known as “bowel rest.”
Navigating a clear liquid diet for diverticulitis is physically taxing and psychologically difficult. You are essentially asking your body to fight an infection while depriving it of solid fuel. The hunger can be overwhelming. The lack of energy is palpable. The anxiety about when to eat again is real.
This comprehensive guide is your survival manual. We will move beyond simple lists of allowed foods. We will explore the physiological mechanisms of gastrointestinal inflammation relief, detail the exact timeline for safety, and provide a structured plan for transitioning back to solid food without triggering a relapse. This is how you manage acute diverticulitis with the precision of a medical professional.
The Physiological Necessity of a Clear Liquid Diet for Diverticulitis
To adhere to this strict regimen, you must understand the “why” behind it. It is not simply about reducing calories or flushing the system. It is about mechanics.

How Bowel Rest Reduces Gastrointestinal Inflammation
When you consume solid food, your digestive system engages in a complex mechanical process called peristalsis. This involves the rhythmic contraction of muscles in the intestinal walls to propel waste forward. When you have acute diverticulitis, the tissues of your sigmoid colon are inflamed, swollen, and potentially micro-perforated.
Peristalsis in this state is physically traumatic to the colon. It causes excruciating pain and can aggravate the infection. Furthermore, solid food creates fecal bulk. This residue acts as an abrasive force against the raw, infected lining of the diverticula.
A clear liquid diet for diverticulitis effectively eliminates this mechanical stress. Clear liquids are absorbed almost entirely in the stomach and upper small intestine. They leave virtually no residue (undigested material) to pass through the colon. By removing the workload and the physical bulk, you minimize intraluminal pressure. This drop in pressure improves blood flow to the infected area and allows the immune system to focus on healing the tissue rather than processing waste.
Current Medical Consensus on Treating Diverticulitis at Home
The medical standard of care has evolved significantly. According to recent guidelines from the American College of Gastroenterology, not every case of uncomplicated diverticulitis requires antibiotics. The focus has shifted toward outpatient management using bowel rest and close monitoring.
Data indicates that 70–100% of uncomplicated cases can be managed successfully at home. This places a significant responsibility on the patient to adhere strictly to the diverticulitis flare up diet. Cheating on this diet—eating a piece of toast or drinking a smoothie with pulp during the acute phase—can restart the cycle of inflammation.
Comprehensive Diverticulitis Liquid Diet List for Optimal Recovery
One of the most common points of failure in managing diverticulitis at home is a misunderstanding of what constitutes a “clear liquid.” Patients often assume this means the liquid must be colorless like water. This is incorrect. A liquid is considered clear if it is transparent and leaves no residue.
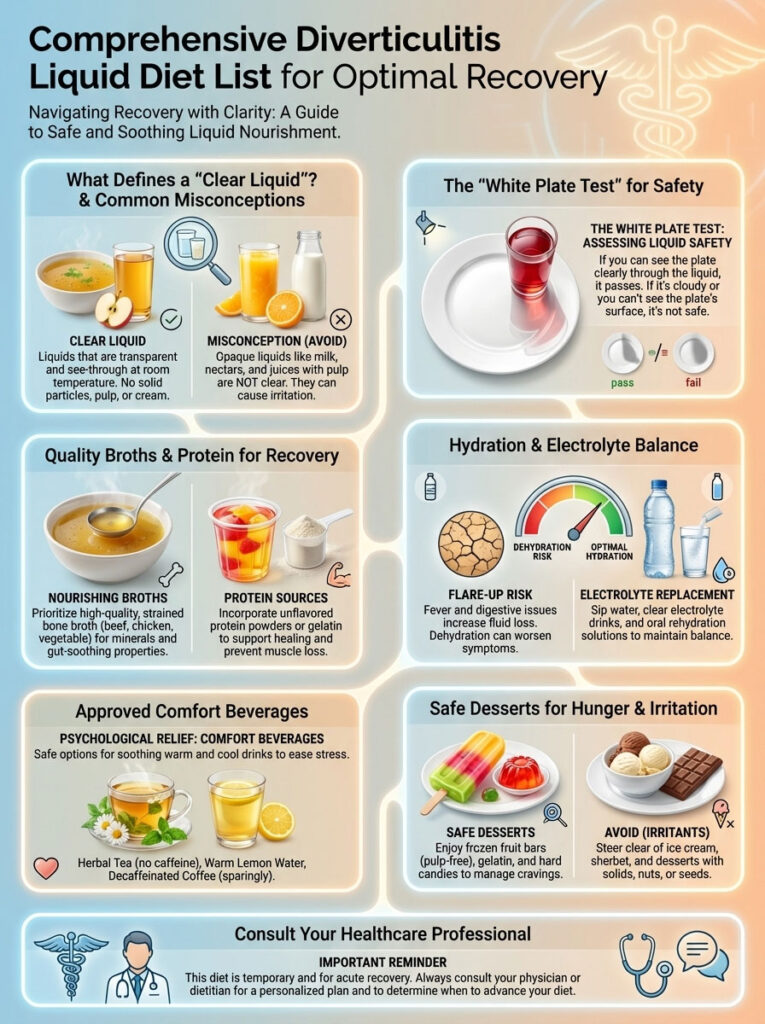
The White Plate Test for Ensuring Safety
If you are standing in the grocery store aisle and are unsure if a beverage is safe, use the “White Plate Test.” Pour a small amount of the liquid into a clear glass. Hold a white piece of paper or a plate behind the glass. If you can see the white object clearly through the liquid, even if the liquid has a color (like yellow or green), it passes the test. If the liquid is cloudy, milky, or opaque, it fails. It is not safe for colon health recovery.
High-Quality Broths and Protein Sources
You cannot survive on water alone. Your body needs protein to repair tissue.
- Bone Broth for Diverticulitis: This is the gold standard for recovery. Unlike standard stock, bone broth is simmered for long periods, extracting collagen and amino acids like glutamine. Glutamine is the primary fuel source for enterocytes (the cells lining your gut). Drinking warm, strained bone broth provides a direct healing mechanism for the colon wall.
- Strained Vegetable or Meat Broth: If bone broth is unavailable, standard chicken, beef, or vegetable broth is acceptable. You must ensure it is strained. If there are bits of parsley, peppercorns, or fat floating on top, skim them off before consumption.
Hydration and Electrolyte Replacement for GI Issues
Dehydration is a major risk during a flare-up, especially if you have a low-grade fever.
- Pedialyte and Medical-Grade Electrolytes: These are superior to sports drinks because they contain higher sodium and potassium levels with less sugar. Proper electrolyte balance prevents the “brain fog” and fatigue associated with fasting.
- Isotonic Sports Drinks: Gatorade or Powerade can be used for caloric energy. If you are diabetic or sensitive to sugar, opt for “Zero” versions, but be aware that artificial sweeteners can sometimes cause gas in sensitive individuals.
- Clear Fruit Juices: Apple juice, white grape juice, and cranberry cocktail are excellent energy sources. They provide the glucose your brain needs to function. You must ensure they are “pulp-free.” Unfiltered apple cider or orange juice is strictly forbidden due to fiber content.
Approved Comfort Beverages and Desserts
Psychological comfort is crucial when you are in pain and hungry.
- Tea and Coffee: You can drink coffee, but it must be black. You cannot add dairy, almond milk, or powder creamers, as these contain fats and proteins that trigger digestion. Herbal teas like chamomile or peppermint are excellent for soothing gastrointestinal inflammation.
- Gelatin (Jell-O): Gelatin is a protein that is liquid at body temperature. It counts as a clear liquid. Eating Jell-O provides the sensation of chewing, which can help satisfy hunger pangs.
- Fruit-Flavored Ice Pops: Popsicles are excellent for hydration and cooling a feverish body. You must choose varieties without fruit chunks, seeds, or yogurt swirls.
Forbidden Foods on a Diverticulitis Flare Up Diet
Certain items may look like clear liquids but are dangerous during an acute attack. Knowing what to avoid is just as important as knowing what to consume.

The Danger of Red and Purple Dyes
You must strictly avoid any gelatin, sports drink, or popsicle that is red, purple, or blue. The dyes used in these products (such as Red 40) can stain your stool. If your symptoms worsen and you need to go to the Emergency Room, a doctor may ask for a stool sample or perform a digital rectal exam. Red-stained stool looks identical to bloody stool. This can lead to a misdiagnosis of gastrointestinal bleeding, resulting in unnecessary invasive testing. Stick to lemon, lime, orange, or clear flavors.
Why Dairy and Opaque Liquids are Prohibited
Milk, soy milk, almond milk, and cream soups are fluids, but they are not clear liquids. They contain fats, proteins, and residues that require active digestion. Consuming dairy triggers the release of digestive enzymes and bile, stimulating the very organ you are trying to rest. Even a splash of milk in your coffee can disrupt the bowel rest process.
Alcohol and Carbonation Warnings
Alcohol acts as a gut irritant and causes dehydration. It must be avoided entirely until you are fully recovered. Carbonated beverages like ginger ale or seltzer can be helpful for nausea, but the gas bubbles can cause bloating and distension in the colon. If you choose to drink soda, pour it into a glass and let it sit for 20 minutes to allow the carbonation to dissipate before drinking.
Comparison of Clear Liquid Diet vs Low Residue Diet Stages
There is often confusion between “Stage 1” (Clear Liquid) and “Stage 2” (Low Residue). Patients frequently transition too early or mix the rules, leading to prolonged pain.

| Feature | Stage 1: Clear Liquid Diet | Stage 2: Low Residue Diet |
| Medical Objective | Complete Bowel Rest (Halt Inflammation) | Gradual Reactivation of Digestion |
| Duration | 1 to 3 Days (Maximum) | 2 to 4 Weeks (Until Symptom-Free) |
| Consistency | Transparent Fluids Only | Soft Solids, Low Fiber (<10g/day) |
| Protein Sources | Bone Broth, Gelatin | Eggs, Tofu, White Poultry, White Fish |
| Dairy Allowed? | None (or clear whey isolate) | Yogurt (no seeds), Cheese, Milk |
| Fiber Allowance | 0 Grams (Strict) | Very Low (Refined grains only) |
| Survival Strategy | Focus on Electrolytes & Hydration | Chew thoroughly; Small, frequent meals |
| Typical Menu | Broth, Tea, Apple Juice, Jell-O | White Rice, White Toast, Canned Pears |
Managing Acute Diverticulitis at Home: Duration and Safety
The most common question patients ask is: “How long do I have to do this?” The answer requires a balance between healing the gut and starving the body.

The Standard 72-Hour Protocol
Most gastroenterologists recommend adhering to the clear liquid diet for 48 to 72 hours. This timeframe is usually sufficient for the acute inflammation to subside. Extending the diet beyond three days is generally not recommended without medical supervision. Clear liquids provide almost no nutritional value. Prolonged adherence can lead to muscle wasting, severe fatigue, and a weakened immune system—the exact opposite of what you need to fight an infection.
The 24-Hour Red Flag Rule
While the diet lasts three days, the first 24 hours are the most critical for diagnostic purposes.
If your abdominal pain does not decrease after 24 hours of strict bowel rest, this is a red flag.
Bowel rest should provide noticeable relief relatively quickly. If the pain persists or worsens despite the diet, it suggests that the diverticulitis flare up is complicated. You may have an abscess (a pocket of pus), a fistula, or a perforation. In this scenario, diet alone will not work. You must contact your healthcare provider immediately.
Survival Strategies for Managing Diverticulitis Hunger
Surviving on liquids requires mental fortitude. The hunger pangs on Day 2 can be intense. Here are practical strategies to manage the discomfort while staying compliant.

Flavor Rotation Techniques
Palate fatigue is real. If you drink only sweet apple juice and lemon Jell-O, you will quickly become nauseated by the sugar.
- The Savory-Sweet Cycle: Alternate your intake. Start with a warm mug of salty beef bone broth (savory). Follow it two hours later with a cold glass of cranberry juice (tart/sweet). Follow that with herbal tea (neutral). This rotation keeps your taste buds engaged and prevents the diet from feeling monotonous.
Temperature Variance Strategy
Varying the temperature of your liquids can mimic the sensation of a “meal.”
- “Breakfast”: Hot coffee or tea.
- “Lunch”: Warm chicken broth served in a bowl (use a spoon to trick your brain into thinking you are eating soup).
- “Snack”: Ice-cold popsicles or frozen electrolyte slushies.
- “Dinner”: Warm savory broth.
The sensation of warmth in the stomach can be soothing and satiating, while ice-cold items can wake up the senses.
The Ice Chip Trick
Chewing is a physiological need. The act of mastication releases tension. Since you cannot chew food, chew ice chips. You can also freeze Gatorade or Pedialyte in ice cube trays and chew on those. This provides hydration, electrolytes, and the satisfaction of “crunching” something without breaking the diverticulitis liquid diet list rules.
Transitioning from Liquid Diet to Low Fiber Foods for Colon Health
The transition phase is the most dangerous period for relapse. When the pain stops, patients often make the mistake of celebrating with a large, fibrous meal. This shocks the dormant colon and can cause immediate spasms.
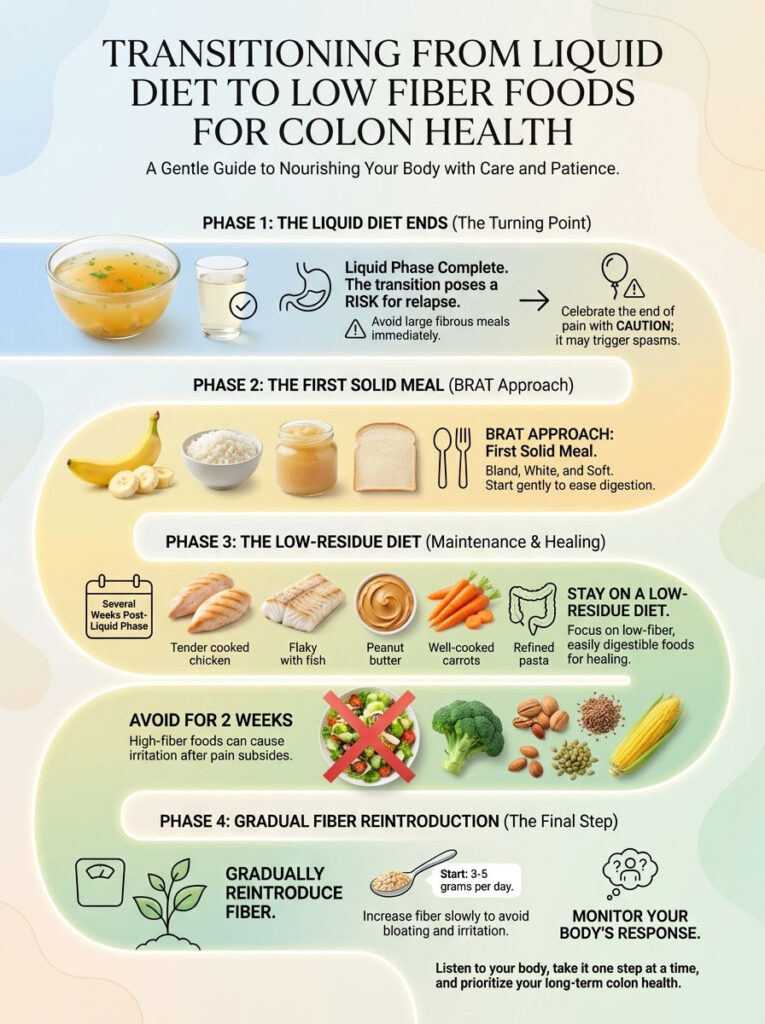
The First Solid Meal: The BRAT Approach
Your first meal after the liquid phase should be bland, white, and soft. Think of it as baby food for adults.
- Scrambled Eggs: These are the perfect transition food. They are high in protein, soft, and digested easily in the small intestine.
- White Toast or Rice: Use refined white bread or white rice. Avoid whole grains, brown rice, or quinoa. You want easily digestible carbohydrates.
- Canned Fruit: Peaches or pears packed in juice (not syrup) are soft and low in fiber.
Reintroducing Fiber Slowly to Prevent Relapse
You must stay on a low-residue diet for several weeks. Do not reintroduce high-fiber foods like salads, raw vegetables, nuts, seeds, or corn until you have been completely pain-free for at least two weeks. When you do start eating fiber again, add only 3 to 5 grams per day. Suddenly jumping from 2 grams of fiber to 30 grams will cause massive bloating and could irritate the healed diverticula.
Identifying Complications: When Home Care Fails
While this guide focuses on home management, you must remain vigilant for signs that the flare-up is becoming life-threatening.
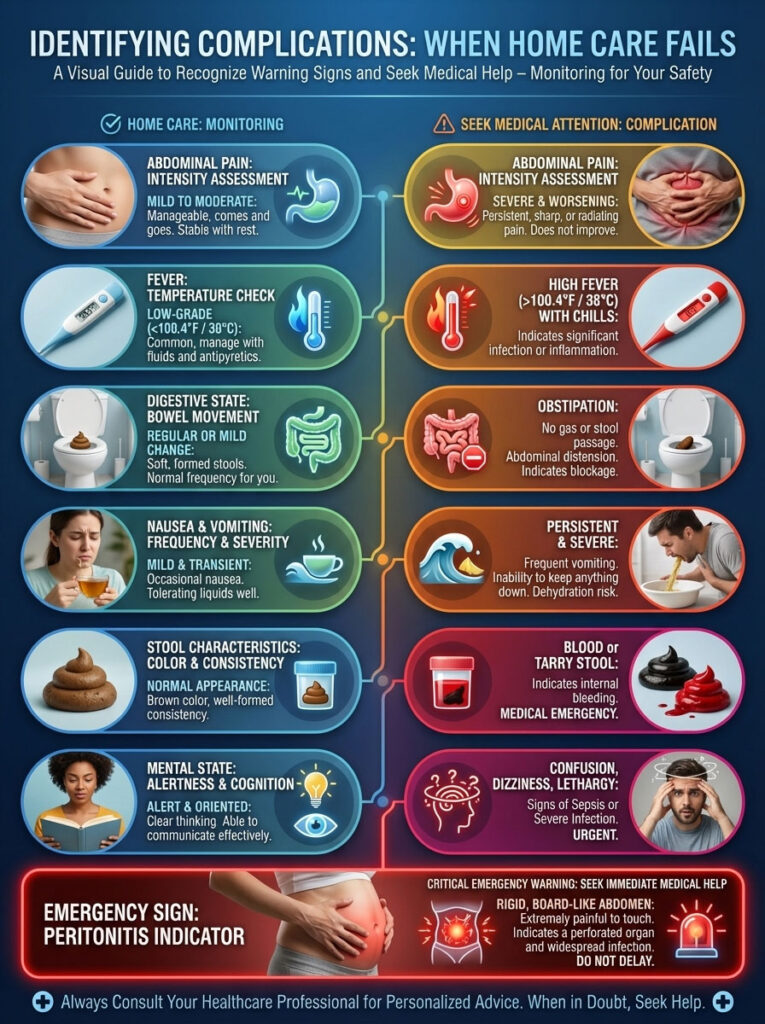
| Symptom | Home Management (Safe) | Emergency (Hospital Required) |
| Abdominal Pain | Mild to Moderate (Improving with rest) | Severe, Sharp, or Rigid “Board-like” Abdomen |
| Fever | None or Low Grade (<100.4°F) | High Fever (>100.4°F) with Chills/Shaking |
| Digestive State | Passing gas; some bowel movement | Obstipation (Cannot pass gas or stool at all) |
| Nausea | Mild | Persistent Vomiting (Dehydration risk) |
| Stool Characteristics | Loose (due to liquid diet) | Blood in Stool (Maroon, Black, or Bright Red) |
| Mental State | Alert, perhaps tired | Confused, dizzy, or fainting (Signs of Sepsis) |
If you experience a rigid abdomen—where your stomach feels hard to the touch and you reflexively flinch when touching it—this is a sign of peritonitis. This is a surgical emergency.
Frequently Asked Questions About Diverticulitis Recovery
Can I have coffee on a clear liquid diet for diverticulitis?
Yes, but with strict limitations. It must be black coffee. You cannot use dairy, almond milk, or powdered creamers, as these contain fats and proteins that trigger digestive enzymes. If caffeine stimulates your bowels too much or causes jitteriness, switch to decaf black coffee.
Is bone broth better than regular broth for diverticulitis recovery?
Yes, bone broth for diverticulitis is superior. It is naturally rich in collagen and glutamine, an amino acid that helps repair the intestinal lining (mucosa). Regular stock is mostly flavored water, while bone broth offers genuine therapeutic value for gut healing.
How long to stay on a clear liquid diet for diverticulitis?
The general medical consensus is 48 to 72 hours. Extending the diet beyond three days can lead to malnutrition and weakness. If symptoms persist beyond three days, you need medical re-evaluation rather than continued dieting.
Can I drink protein shakes on a clear liquid diet?
Standard milky protein shakes are forbidden. However, there are “clear whey isolate” protein drinks available on the market that are transparent and fruit-flavored. These are generally acceptable and can help maintain muscle mass, but check the label to ensure they are fiber-free.
Is ginger ale good for diverticulitis flare ups?
Yes, ginger ale is acceptable and can soothe nausea. However, the carbonation can cause gas and bloating, which might increase abdominal pain. It is best to pour the soda into a glass and let it go flat before drinking it.
What are the signs of diverticulitis flare up getting worse?
Escalating pain, a fever that spikes despite Tylenol, vomiting that prevents you from keeping liquids down, and the cessation of passing gas are all signs that the condition is deteriorating and requires urgent care.
Can I eat eggs on a clear liquid diet?
No. Eggs are soft solids, not liquids. They are excellent for Stage 2 (Low Residue Diet) but are not permitted during the clear liquid bowel rest phase.
Why can’t I have red or purple Jell-O?
Red and purple dyes can stain the stool, mimicking the appearance of blood. This can complicate medical diagnosis if a stool sample or colonoscopy is required during your flare-up.
Can I take probiotics during a flare-up?
It is generally best to pause probiotics during the acute liquid phase unless directed otherwise by a doctor. Introducing bacteria into an actively inflamed gut can sometimes cause increased bloating. Wait until you are in the recovery phase.
Does a liquid diet cure diverticulitis?
The diet does not “cure” the underlying disease (the diverticula will remain), but it resolves the acute inflammation of the flare-up by allowing the colon to rest. It is a management tool, not a cure for diverticulosis itself.
Can stress cause a diverticulitis flare-up?
While diet is the primary driver, stress affects the gut-brain axis and can increase colonic motility and inflammation. High stress can exacerbate symptoms or make a flare-up more painful.
When can I start eating salad again?
Raw vegetables like lettuce are high in insoluble fiber and are difficult to digest. You should wait until you have been completely symptom-free for at least 4 to 6 weeks before reintroducing raw salads.
Disclaimer: This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
References:
- American College of Gastroenterology (ACG) Clinical Guidelines.
- Mayo Clinic: Diverticulitis Diet & Management.
- Cleveland Clinic: Gastrointestinal Soft Diet Protocols.








