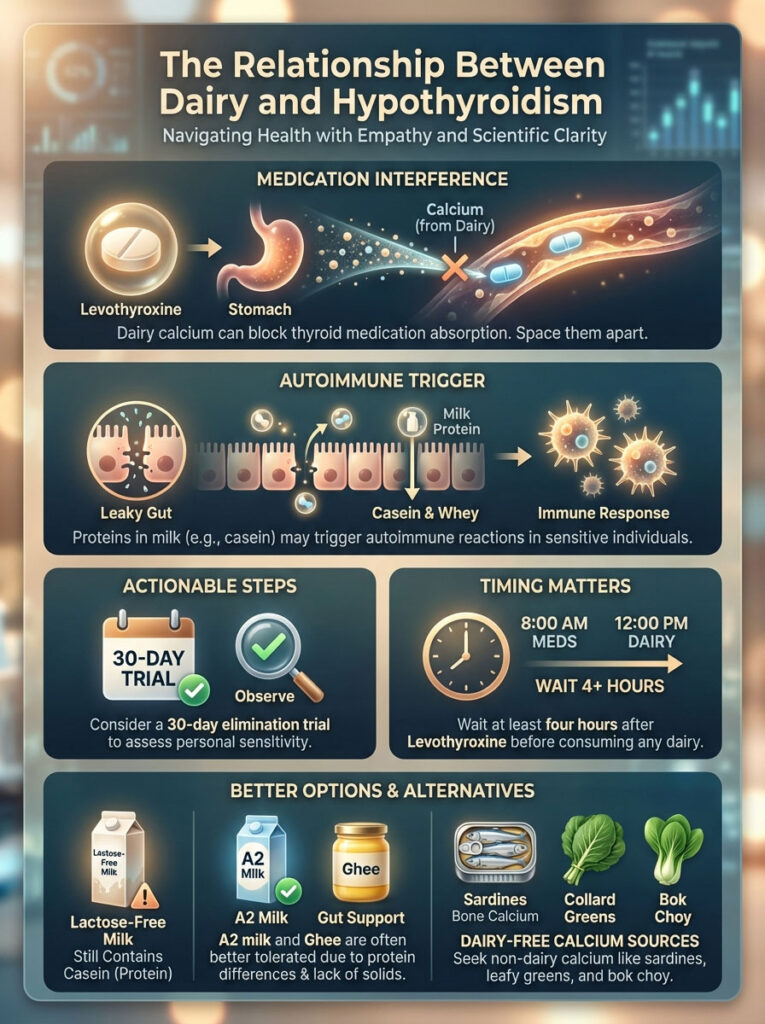
Is dairy safe for thyroid patients? Generally, no. The relationship between Dairy and Hypothyroidism presents a dual threat to the Hashimoto’s diet: calcium interferes with thyroid medication absorption, and casein proteins can trigger autoimmune attacks via molecular mimicry. While not every patient needs to be permanently dairy-free for thyroid health, a 30-day elimination trial is the clinical gold standard to determine if milk products are spiking your TSH or antibodies.
Table of Contents
Navigating the complex relationship between Dairy and Hypothyroidism is often the first major hurdle for newly diagnosed patients. You take your medication every morning at 7:00 AM sharp. You wait exactly sixty minutes before eating breakfast. You never miss a dose. Yet, when you visit your endocrinologist, your TSH levels are still fluctuating wildly, and your fatigue remains heavy.
This is what we call the “TSH Paradox” in clinical practice. When patient compliance is perfect but biochemistry is chaotic, we have to look at environmental variables. The most common silent disruptor in this equation is often the milk in your morning latte or the yogurt in your breakfast bowl.
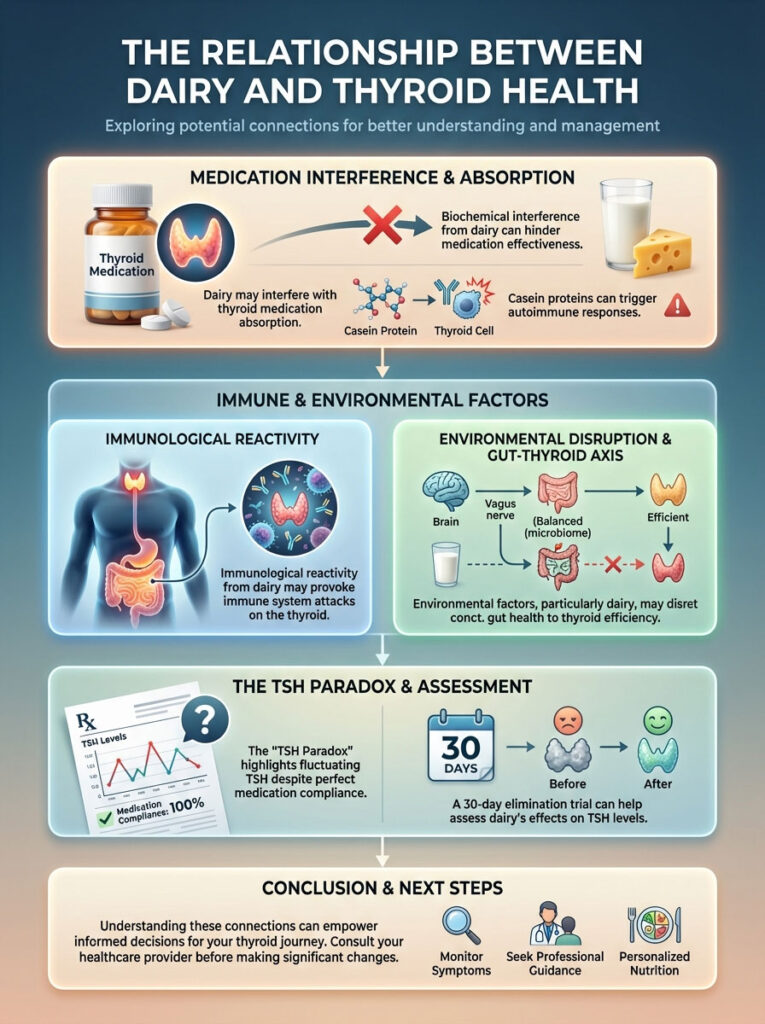
Understanding this dynamic requires us to look beyond simple lactose intolerance. We must examine the Gut-Thyroid Axis. This biological highway connects your intestinal health directly to your thyroid function. Dairy poses a unique challenge here because it attacks on two fronts. First, it causes biochemical interference which blocks your body from using medicine. Second, it causes immunological reactivity which can confuse your immune system into attacking your own gland.
In this comprehensive guide, we will break down the science of Levothyroxine interactions. We will explain why protein structures matter more than sugar content. Finally, we will provide a clear framework for testing your tolerance safely without compromising your bone health.
Key Statistics for Thyroid Patients:
- 30% Reduction: Consuming calcium-rich foods like milk simultaneously with Levothyroxine can reduce drug absorption by up to 30% (American Thyroid Association).
- 75.9% Correlation: A 2014 study found that nearly 76% of Hashimoto’s patients also suffer from lactose intolerance.
- 4 Hours: The minimum time required to separate thyroid medication from calcium supplements or dairy to prevent chelation.
- 50% Cross-Reactivity: Roughly half of patients sensitive to gluten also react to casein due to similar protein structures.
- 23 Days: The approximate half-life of IgG antibodies, meaning you need at least this long to clear inflammation from a dairy exposure.
The Bioavailability Barrier: How Dairy Affects Thyroid Medication
To understand why milk is problematic, you first need to understand the pharmacokinetics of your medication. Levothyroxine interactions are notoriously sensitive. Synthetic T4 (found in Synthroid, Levoxyl, Tirosint) is a finicky molecule. It requires a highly acidic stomach environment and a complete absence of “chelating agents” to pass through the intestinal wall and enter your bloodstream.
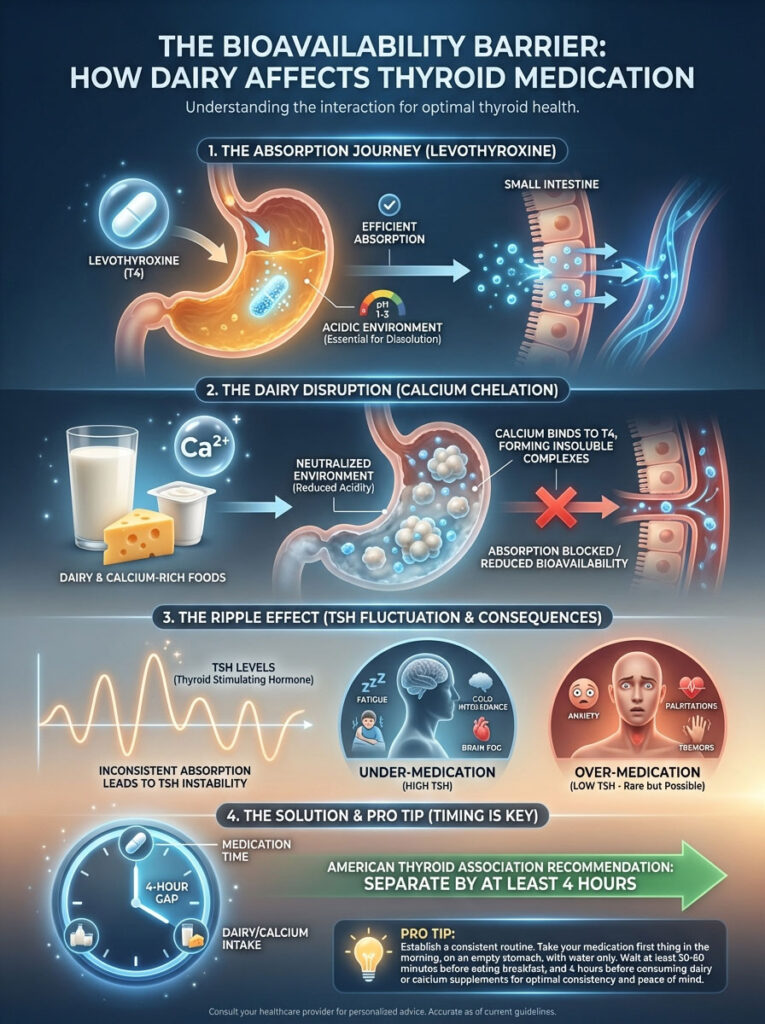
This is where the “Calcium Connection” becomes critical. Dairy is celebrated for its high calcium content, but for a thyroid patient, this is a double-edged sword. Calcium carbonate and calcium citrate are potent chelators. When you consume calcium alongside your medication, the calcium molecules bind to the hormone molecules in the stomach.
Think of it like a magnet. The calcium snaps onto the thyroid hormone, creating a large, insoluble complex. Your gut lining cannot absorb this complex. Instead of entering your blood to regulate your metabolism, the medication is simply excreted through your bowel movements. You aren’t absorbing the dose your doctor prescribed; you are absorbing a fraction of it.
The Chemistry of Chelation
The chemical reaction happening in your stomach is immediate. Thyroid hormones are negatively charged molecules in certain pH environments, while calcium ions are positively charged. They attract one another with significant force. Once they bond, the resulting molecule is too large to pass through the tight junctions of the intestinal villi.
This leads to fluctuating TSH levels. One day you might have coffee without milk and absorb 80% of your medication. The next day you have a latte and absorb only 50%. Your doctor sees the TSH spike and increases your dose. Then, you stop drinking lattes, and suddenly you are over-medicated and hyperthyroid. The dairy is driving the rollercoaster.
The 4-Hour Clinical Rule
Many patients believe that waiting 30 minutes or even an hour is sufficient. It is not. The American Thyroid Association guidelines are clear regarding calcium and thyroid medication: you must separate them by at least four hours.
Why four hours? It takes the stomach roughly that long to fully clear a calcium-rich meal and return to a baseline pH where absorption is optimized. If you take your meds at 7:00 AM and have a latte at 8:00 AM, you are likely under-medicating yourself daily, regardless of the dosage on the bottle.
Pro Tip: The Split Schedule
If you cannot function without your morning milky coffee or yogurt, you must change your medication timing, not just your diet.
- Option A (Night Dosing): Take your Levothyroxine at bedtime, at least 4 hours after your last meal. This leaves your morning free for dairy.
- Option B (The Early Riser): Set an alarm for 4:00 AM, take your medication, and go back to sleep. By 8:00 AM, you are in the clear for calcium consumption.
The Hashimoto’s-Lactose Connection: Inflammation and TSH
Beyond the chemistry of absorption, we must look at the biology of the gut. There is a staggering overlap between autoimmune thyroid disease and lactose intolerance and thyroid dysfunction. Research published in the journal Endocrine demonstrated that lactose restriction alone was enough to normalize TSH levels in patients who were previously resistant to treatment.
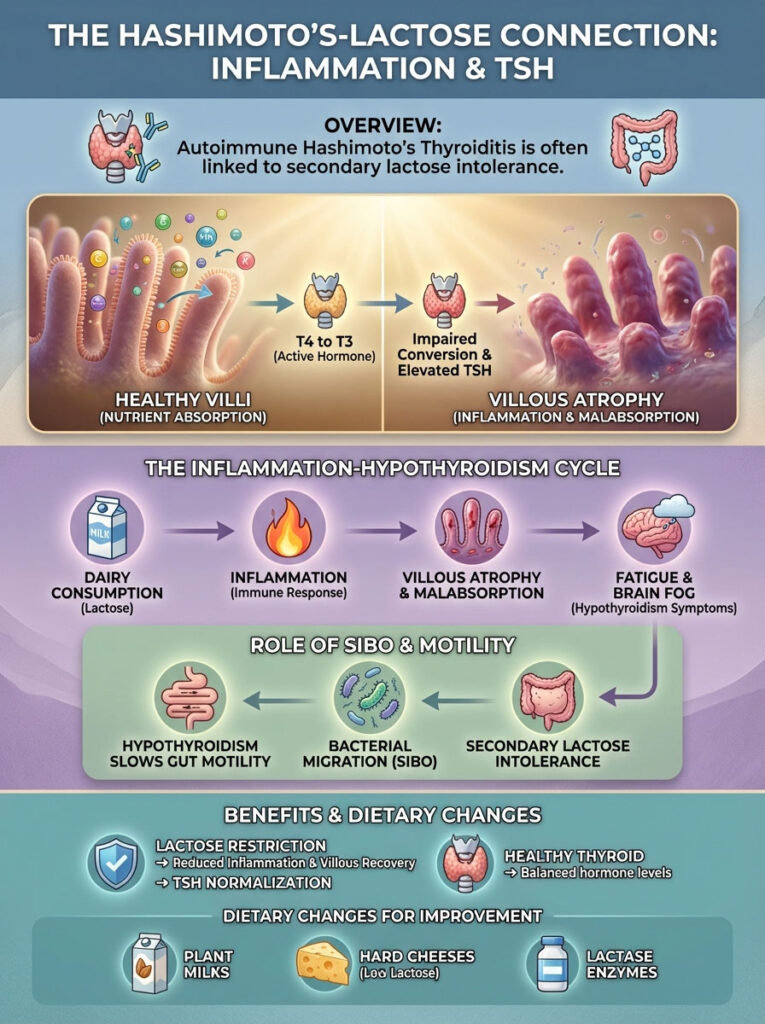
The mechanism here is “villous atrophy.” Your small intestine is lined with tiny, finger-like projections called villi. These villi are responsible for absorbing nutrients like Selenium and Zinc, which are vital for converting T4 (inactive hormone) into T3 (active hormone). When a person with lactose intolerance consumes dairy, the resulting inflammation blunts and damages these villi.
This damage leads to malabsorption. You might be eating a nutrient-dense diet, but if your villi are atrophied from chronic dairy exposure, you are effectively starving your thyroid of the minerals it needs to function. This creates a cycle where Dairy and Hypothyroidism feed into each other, worsening fatigue and brain fog.
Secondary Lactose Intolerance & SIBO
Here is a nuance many general practitioners miss: Small Intestinal Bacterial Overgrowth (SIBO). Hypothyroidism slows down gut motility (the speed at which food moves through you). This stagnation allows bacteria to migrate from the colon up into the small intestine.
These bacteria eat the enzyme lactase, which resides on the tips of your villi. As a result, even if you weren’t born lactose intolerant, having hypothyroidism can make you secondarily intolerant. This is why dairy-free for thyroid protocols often yield such rapid improvements in bloating and digestion.
Casein, Gluten, and Molecular Mimicry: The Autoimmune Trigger
We need to make a critical distinction: Lactose is a sugar; Casein is a protein. While lactose intolerance causes digestive distress, casein sensitivity drives autoimmune destruction. This is the most dangerous aspect for Hashimoto’s patients.
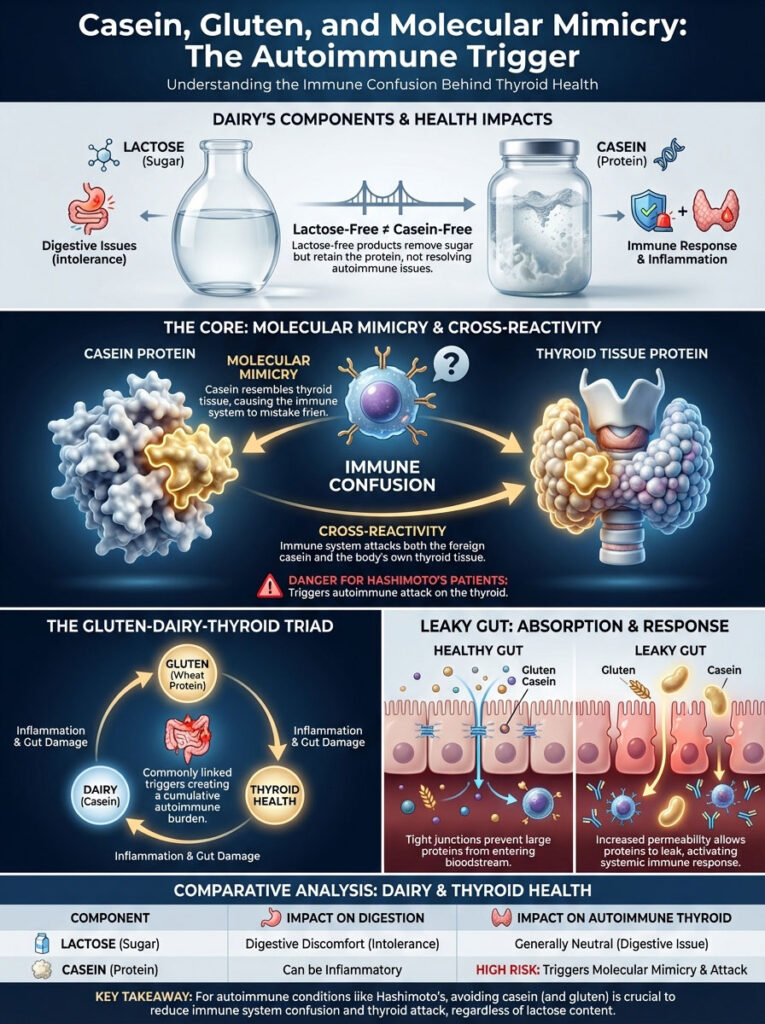
The theory of molecular mimicry suggests that the protein structure of casein (specifically alpha-casein and beta-casein) looks remarkably similar to the protein structure of your own thyroid tissue. In a body with a hyper-vigilant immune system, like one with Hashimoto’s, the immune cells tag the casein protein as an invader.
However, because the thyroid gland looks so similar to the casein, the immune system gets confused. It launches an attack on the dairy protein you ate, but in the crossfire, it also attacks your thyroid gland. This is cross-reactivity. Every time you consume casein, you may be stimulating the production of Thyroid Peroxidase (TPO) antibodies, effectively throwing gas on the fire of your autoimmune condition.
This is why lactose-free milk is often not the solution. Lactose-free milk still contains casein. If your issue is immune-based rather than digestive, lactose-free products will continue to spike your inflammation markers.
The Gluten-Dairy-Thyroid Triad
It is rare to see a patient who reacts to casein but tolerates gluten perfectly. The proteins in wheat (gliadin) and milk (casein) share similar amino acid sequences. This is often referred to as the “Gluten-Dairy-Thyroid Triad.”
When the gut barrier is compromised (Leaky Gut), these undigested proteins slip into the bloodstream. The immune system creates antibodies against them. Because the proteins are so similar, the antibodies created to fight gluten often latch onto casein, and vice versa. This is why many functional medicine practitioners recommend eliminating both simultaneously for at least 90 days to see a true drop in antibody levels.
Comparative Analysis: Dairy Components and Thyroid Impact
| Dairy Component | What Is It? | Mechanism of Thyroid Interference | Clinical Recommendation |
|---|---|---|---|
| Calcium | Mineral | Chelates (binds) Levothyroxine in the gut, reducing absorption. | Separate from meds by 4 hours. |
| Lactose | Sugar (Disaccharide) | Causes villous atrophy in intolerant patients; leads to malabsorption. | Use lactase enzymes or avoid if intolerant. |
| Casein | Protein | Triggers molecular mimicry; increases TPO antibodies in sensitive patients. | Strict elimination for 30 days to test. |
| Whey | Protein | Spikes insulin; generally less inflammatory than casein but can be reactive. | Monitor blood sugar response. |
| Growth Hormones | Additive (rBGH) | Endocrine disruptors found in non-organic dairy. | Consistently choose organic/grass-fed. |
The A1 vs. A2 Beta-Casein Distinction: Is All Milk the Same?
Not all cows are created equal, and neither is their milk. In the United States, the vast majority of dairy comes from Holstein cows. These cows produce a specific protein variant known as A1 vs A2 beta-casein. The A1 protein, found in standard grocery store milk, breaks down in the human gut into a peptide called Beta-casomorphin-7 (BCM-7).
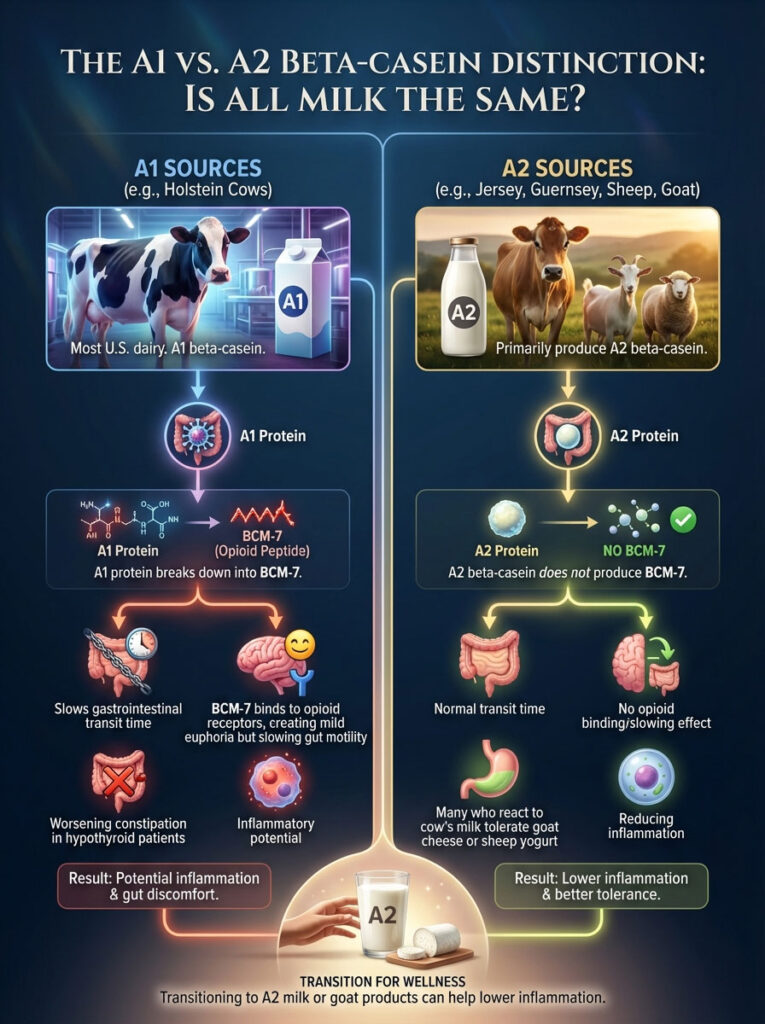
BCM-7 is an opioid peptide with significant inflammatory potential. It has been shown to slow down gastrointestinal transit time. For a hypothyroid patient who already struggles with constipation, consuming A1 milk is like putting the brakes on a car that is already moving too slowly. This stagnation promotes the reabsorption of toxins and estrogen from the gut back into the bloodstream.
However, cows like Jerseys and Guernseys, as well as sheep and goats, produce primarily A2 beta-casein. This protein does not break down into the inflammatory BCM-7 peptide. This is why many patients who react poorly to cow’s milk find they can tolerate goat cheese or sheep yogurt without issue. If you are reluctant to go fully dairy-free for thyroid reasons, switching to A2 milk or goat products can be a viable “step-down” strategy to lower inflammation.
The Opioid Effect of Casomorphins
Why is cheese so addictive? It is not just the fat and salt. The BCM-7 peptide attaches to opioid receptors in the brain. This can create a mild sensation of euphoria or relief, similar to a very weak dose of morphine. For patients with autoimmune fatigue, this temporary boost can feel like energy.
However, this comes at a cost. The binding of BCM-7 to receptors in the gut slows down peristalsis (the wave-like muscle contractions that move food). In Hashimoto’s patients, gut motility is already compromised by low thyroid hormone. Adding an opioid peptide to the mix exacerbates constipation, leading to bacterial overgrowth and toxin recirculation.
Hidden Dairy in Pharmaceuticals
Here is a shocking fact for many patients: your thyroid medication itself might contain dairy. Lactose is a common filler (excipient) used in the pharmaceutical industry to add bulk to pills. While the amount is small, it can be problematic for those with severe sensitivity or Celiac disease.

Brand name Synthroid contains lactose monohydrate. Many generic versions of Levothyroxine also contain it. For the average person, this milligram amount is negligible. But for a “super-responder” with autoimmune reactivity, even this daily micro-dose can keep inflammation simmering.
If you have eliminated dietary dairy but still feel symptoms, check your medication. Cleaner formulations like Tirosint (liquid gel caps) or compounded medications are often free of lactose fillers. Discussing a switch with your doctor could be the missing link in your treatment plan.
Clinical Framework: How to Conduct a Dairy Elimination Trial
So, should you quit dairy forever? Not necessarily. In functional nutrition, we follow a simple rule: Why guess when you can test? The only way to know if Dairy and Hypothyroidism are linked in your specific biology is to conduct a structured elimination and provocation trial.
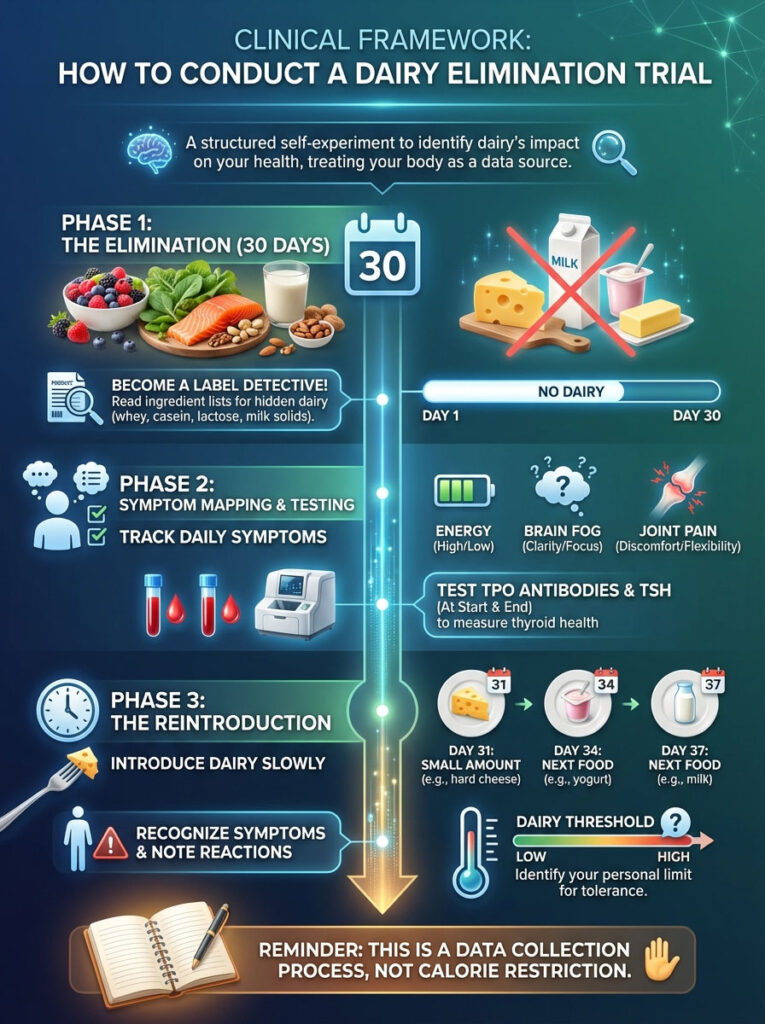
This is not about calorie restriction; it is about data collection. Here is the Gold Standard protocol we use in clinic:
Phase 1: The Elimination (30 Days)
For four weeks, you must consume zero dairy. This means no milk, cheese, yogurt, butter, or cream. You must also become a label detective, looking for hidden ingredients like “caseinate,” “whey powder,” and “milk solids” in processed foods. It takes roughly 23 days for antibodies to reduce significantly, so cheating on day 15 resets the clock.
Phase 2: Symptom Mapping
During these 30 days, track your data. Rate your energy, brain fog, joint pain, and bowel movements on a scale of 1-10 daily. Ideally, you should test your Thyroid Peroxidase (TPO) antibodies and TSH at the start and end of this period. Look for changes in “soft signs” like sinus congestion, acne, or post-nasal drip, which are often linked to dairy sensitivity.
Phase 3: The Reintroduction
On day 31, do not eat a pizza. You will overwhelm your system. Introduce dairy in a hierarchy of safety:
- Level 1: Ghee (Clarified butter, almost pure fat).
- Level 2: Butter (Trace amounts of protein).
- Level 3: Hard, aged cheese (Low lactose, concentrated casein).
- Level 4: Whole Milk (High lactose, high casein).
Introduce one new food every 3 days. If you experience a return of symptoms—bloating, fatigue, headache, or a rash—you have found your “Dairy Threshold.”
Nutrient Density vs. Restriction: Protecting Bone Health
A valid concern when adopting a Hashimoto’s diet that excludes dairy is the loss of calcium. Dairy is a primary source of calcium and Vitamin D for many Americans. Since hypothyroidism itself is a risk factor for lower bone density, we cannot simply remove dairy without replacing its nutrients.

However, dairy is not the only, nor necessarily the best, source of calcium. Bioavailability matters. The calcium in cow’s milk is not always absorbed efficiently if gut health is compromised. There are excellent non-dairy sources that support an anti-inflammatory diet.
Canned sardines and salmon (with the bones left in) are superior sources because they provide calcium alongside Omega-3 fatty acids, which reduce inflammation. Leafy greens like Collard greens and Bok choy are also excellent. A word of caution: while spinach is healthy, it is high in oxalates, which can block calcium absorption, so it should not be your primary calcium source.
Furthermore, calcium does not work alone. For calcium to actually enter your bone matrix rather than calcifying your arteries, it requires co-factors: specifically Vitamin D3, Vitamin K2, and Magnesium. A dairy-free for thyroid plan must ensure these co-factors are present.
The Calcium Paradox
Many cultures with low dairy consumption actually have lower rates of osteoporosis than Western nations with high dairy consumption. This is known as the Calcium Paradox. Bone health is not just about calcium intake; it is about calcium retention.
High-protein, acidic diets (common in the West) can force the body to leach calcium from bones to buffer blood pH. Furthermore, without adequate Vitamin K2 (found in natto, egg yolks, and organ meats), calcium tends to deposit in soft tissues like arteries rather than in the skeletal system. When going dairy-free, focus on a whole-foods diet rich in these co-factors to ensure your bones stay strong.
Comparison of Dairy Alternatives for Thyroid Health
| Milk Alternative | Pros for Thyroid | Cons for Thyroid | Best For |
|---|---|---|---|
| Coconut Milk | Contains MCTs for metabolism; low allergen risk; AIP compliant. | Low in protein and calcium (unless fortified). | Cooking, coffee, AIP diets. |
| Almond Milk | Low calorie; widely available. | High in oxalates; often contains gums/fillers. | Smoothies (if not sensitive to nuts). |
| Soy Milk | High protein. | Avoid: Contains goitrogens and isoflavones that inhibit TPO enzyme. | Not Recommended for Hypothyroidism. |
| Cashew Milk | Creamy texture; mineral dense. | High FODMAP (may irritate SIBO). | Cream-based sauces. |
| Oat Milk | Creamy; popular. | High glycemic index (blood sugar spike); cross-contamination with gluten. | Occasional treats only. |
| Hemp Milk | Complete protein; Omega-3s. | Earthy taste can be polarizing. | Protein shakes and baking. |
The Role of Fermentation and Ghee
In the world of Dairy and Hypothyroidism, there are two notable exceptions that many patients tolerate well: Ghee and long-fermented dairy.

Ghee is clarified butter. The process involves simmering butter until the water evaporates and the milk solids (where the lactose and casein live) separate and are skimmed off. What remains is pure butterfat. This fat is rich in Butyrate, a short-chain fatty acid that actually fuels the cells of the gut lining and helps repair leaky gut. For patients who react to the protein in dairy but need the healthy fats, Ghee is often a safe “superfood.”
Fermentation is another tool. Products like Kefir and yogurt contain live bacterial cultures (probiotics). During the fermentation process, these bacteria consume the lactose sugar, effectively “pre-digesting” it for you. This significantly lowers the lactose content. Additionally, fermentation can partially break down casein proteins.
However, a warning on Greek Yogurt: While it is high in protein and lower in lactose, it is actually concentrated dairy. It requires more milk to make a cup of Greek yogurt than regular yogurt. Consequently, it has a very high density of casein. If you have casein sensitivity or elevated antibodies, Greek yogurt might be one of the most inflammatory foods you can eat, despite its reputation as a health food.
Histamine Intolerance Considerations
Another layer of complexity is histamine. Many Hashimoto’s patients suffer from Mast Cell Activation Syndrome (MCAS) or histamine intolerance. Fermented foods like yogurt, kefir, and aged cheeses are naturally high in histamine.
If you switch to fermented dairy and find yourself suffering from headaches, hives, or a racing heart, the issue might not be the dairy protein itself, but the histamine produced during fermentation. In these cases, a low-histamine diet that excludes all fermented products, dairy or otherwise, may be necessary.
Practical Lifestyle Tips for Going Dairy-Free
Transitioning to a dairy-free lifestyle can feel overwhelming, especially when dining out or traveling. However, with a few strategic adjustments, it becomes second nature. Here are practical ways to navigate the world without dairy.

Navigating Restaurants
Most restaurants cook with butter. It is the secret ingredient that makes restaurant food taste better than home cooking. When ordering, you must be explicit. Ask for your vegetables to be steamed or sautéed in olive oil. Be wary of steaks, which are often finished with a pat of butter before serving.
The “Creamy” Texture Hack
The biggest thing patients miss is the creamy texture of dairy in soups and sauces. You can replicate this easily using cashews or cauliflower. Soaking raw cashews and blending them creates a neutral, rich cream that thickens sauces perfectly. Alternatively, steaming cauliflower and blending it into soups adds body and creaminess without the inflammatory proteins.
Reading Labels for Hidden Sources
Dairy hides in unexpected places. Processed meats like sausages often use milk solids as binders. Potato chips can have whey powder for flavoring. Even some breath mints contain casein. Always look for the bold “Contains Milk” warning on the allergen statement, but also scan the ingredients list for “lactalbumin,” “recaldent,” and “tagatose,” which are all dairy derivatives.
Summary & Key Takeaways
The relationship between Dairy and Hypothyroidism is complex, but the path forward is clear. Dairy is not universally “evil,” but it is chemically incompatible with the timing of your medication and biologically risky for those with autoimmune antibodies. The calcium in milk blocks thyroid medication absorption, and the proteins in milk can mimic thyroid tissue, confusing your immune system.
If you are struggling to stabilize your TSH or lower your antibodies, you owe it to yourself to investigate this link. Do not rely on internet trends; rely on your own data. A 30-day elimination trial is a safe, free, and highly effective clinical tool. It allows you to listen to what your body is telling you without the noise of inflammation.
Ultimately, managing Hashimoto’s is about reducing the burden on your immune system. If removing dairy calms the fire, it is a small price to pay for reclaiming your energy and your health.
Frequently Asked Questions
How long should I wait to eat dairy after taking Levothyroxine?
Clinical guidelines from the American Thyroid Association recommend waiting at least four hours after taking your thyroid medication before consuming dairy or calcium-rich foods. This window is necessary to prevent the chemical process of chelation, where calcium ions bind to the synthetic T4 molecule and render it unabsorbable by the intestinal villi.
Is lactose-free milk safe for patients with Hashimoto’s disease?
While lactose-free milk addresses digestive issues like bloating, it still contains casein, the primary protein linked to autoimmune cross-reactivity. If your Hashimoto’s is triggered by molecular mimicry, your immune system will continue to attack your thyroid gland in response to the casein proteins regardless of whether the lactose sugar has been removed.
Why does dairy cause TSH levels to fluctuate so much?
Dairy creates a “TSH Paradox” by interfering with medication bioavailability on an inconsistent basis. If you consume varying amounts of milk or yogurt with your medication, your body absorbs a different percentage of the hormone each day, leading to chaotic lab results and a frustrating cycle of dosage adjustments by your endocrinologist.
Can I use A2 milk if I have hypothyroidism and constipation?
A2 milk is often a better choice because it lacks the A1 beta-casein protein that breaks down into BCM-7, an opioid peptide known to slow gastrointestinal motility. For hypothyroid patients already struggling with a slow metabolism, switching to A2 or goat’s milk can help prevent the “opioid effect” that exacerbates chronic constipation.
Does thyroid medication like Synthroid contain hidden dairy ingredients?
Yes, many common thyroid formulations, including brand-name Synthroid and various generic Levothyroxine tablets, use lactose monohydrate as a pharmaceutical filler or excipient. For highly sensitive “super-responders” with severe autoimmune reactivity, switching to a lactose-free alternative like Tirosint liquid gel caps may be necessary to fully resolve symptoms.
How does dairy consumption affect the gut-thyroid axis?
Dairy can cause inflammatory damage to the intestinal lining, leading to villous atrophy in sensitive patients. This damage hinders the absorption of critical micronutrients like selenium and zinc, which are essential co-factors for converting inactive T4 hormone into the metabolically active T3 hormone your cells need.
Is ghee allowed on a dairy-free thyroid elimination diet?
Ghee, or clarified butter, is typically tolerated well because the inflammatory milk solids—lactose and casein—are removed during the clarification process. Ghee is actually considered a “superfood” in the functional medicine community because it is rich in butyrate, a short-chain fatty acid that helps heal the gut barrier and reduce systemic inflammation.
What are the best dairy-free calcium sources to protect bone health?
To maintain bone density without dairy, prioritize calcium-dense whole foods like canned sardines with bones, collard greens, and bok choy. It is also vital to ensure adequate intake of Vitamin K2 and Magnesium, which act as biological traffic controllers to ensure calcium is deposited into the bone matrix rather than the arteries.
Why should soy milk be avoided as a dairy alternative for hypothyroidism?
Soy milk contains high concentrations of goitrogens and isoflavones that can interfere with the thyroid peroxidase (TPO) enzyme. Since this enzyme is responsible for the synthesis of thyroid hormones, regular consumption of soy can further suppress thyroid function and potentially increase the dosage requirements for your medication.
Can taking thyroid medication at night help if I want to consume dairy?
Taking your Levothyroxine at bedtime, at least four hours after your last meal, is an excellent clinical strategy for dairy lovers. This “night dosing” protocol allows the medication to absorb undisturbed while you sleep, freeing up your morning hours for calcium-rich foods without risking a drug-nutrient interaction.
What is the connection between gluten sensitivity and dairy in thyroid disease?
This is frequently called the “Gluten-Dairy-Thyroid Triad” due to the structural similarities between the proteins gliadin (wheat) and casein (dairy). Because of molecular mimicry, the immune system often cross-reacts, meaning that if you are sensitive to gluten, your body is highly likely to treat dairy proteins as a similar threat, maintaining high antibody levels.
How long does it take to see results after going dairy-free for thyroid health?
You should commit to a strict 30-day elimination trial to see a measurable difference. This timeframe allows the 23-day half-life of IgG antibodies to clear from your system, providing enough time for gut inflammation to subside and for you to accurately track improvements in energy, brain fog, and joint pain.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The relationship between Dairy and Hypothyroidism is complex and varies by individual. Always consult with a qualified endocrinologist or healthcare professional before making significant changes to your diet, supplements, or thyroid medication schedule.
References
- American Thyroid Association – thyroid.org – Clinical guidelines on the interference of calcium carbonate with Levothyroxine absorption.
- Endocrine Journal – “Lactose intolerance in thyroid disease” – Peer-reviewed study demonstrating TSH normalization following lactose restriction in Hashimoto’s patients.
- Journal of Clinical Endocrinology & Metabolism – academic.oup.com/jcem – Research regarding the pharmacokinetics of T4 and the impact of gastric pH and chelating agents.
- National Center for Biotechnology Information (NCBI) – “The Gut-Thyroid Axis” – Comprehensive review of how intestinal dysbiosis and food sensitivities affect thyroid function.
- British Journal of Nutrition – “A1 vs A2 Beta-Casein” – Study on the inflammatory potential of BCM-7 peptides and gastrointestinal transit time.
- Journal of Autoimmunity – “Molecular Mimicry in Autoimmune Disease” – Foundational paper on how food proteins can trigger cross-reactivity with human tissue.








