I see the same scenario play out in my clinic almost every week. A new patient walks in battling fatigue, stubborn weight gain, and brain fog. They read online that the thyroid needs iodine to work, so they started taking high-dose kelp drops or Lugol’s solution. Instead of feeling better, they crashed. This is the classic presentation of the complex relationship between iodine and hypothyroidism. While iodine is the essential building block of thyroid hormones, flooding your system with it does not supercharge your metabolism. In fact, for many people in the United States, it does the exact opposite.
Table of Contents
Can too much iodine cause hypothyroidism?
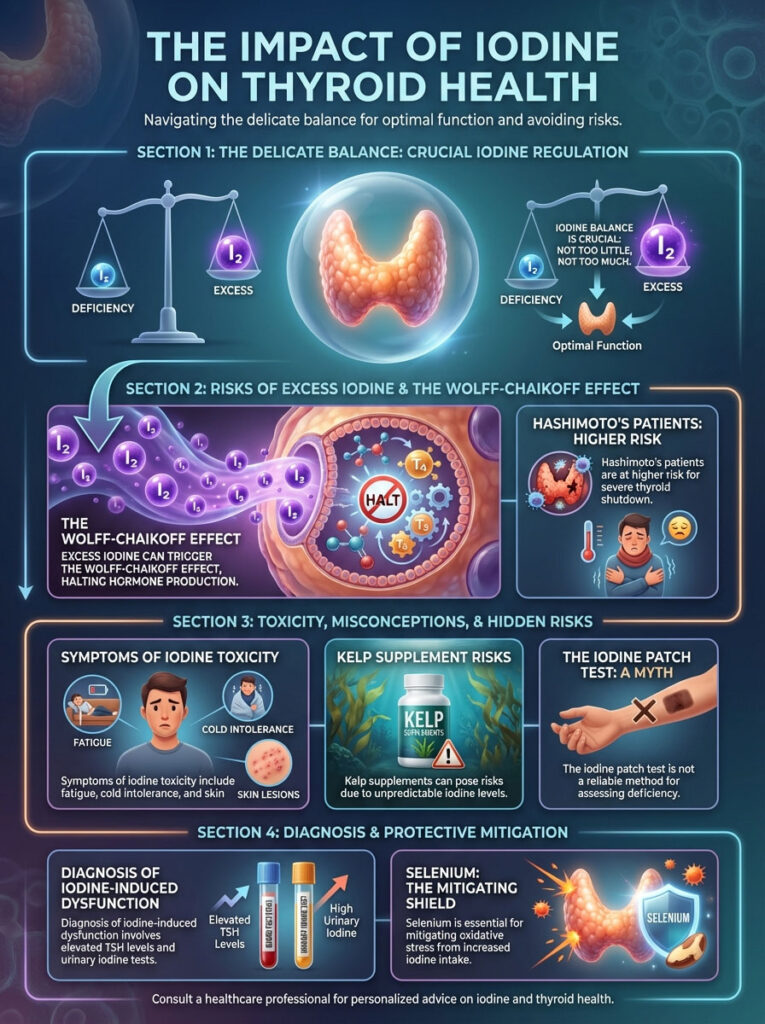
Yes. While iodine is necessary for thyroid function, excessive intake triggers a protective biological mechanism called the Wolff-Chaikoff effect. This causes the thyroid gland to temporarily shut down hormone production to prevent toxicity. In patients with Hashimoto’s thyroiditis, this shutdown can become permanent, leading to overt hypothyroidism.

There is a pervasive myth that if a little is good, a lot must be better. Biology rarely works that way. The thyroid gland operates on a strict U-shaped curve. Both severe deficiency and significant excess lead to dysfunction.
In the United States, true iodine deficiency is rare due to salt iodization. The greater risk for many of my patients is actually iodine excess. As an endocrinologist, I want to walk you through exactly what happens when you overdose on this mineral.
We will look at the biochemistry of the shutdown. We will explore why autoimmune patients are at higher risk. Finally, we will discuss how to safely navigate your intake without crashing your thyroid.
Key Statistics: Thyroid Health & Iodine
- RDA for Adults: 150 micrograms (mcg) per day.
- Tolerable Upper Limit (UL): 1,100 mcg per day.
- Hashimoto’s Prevalence: Affects approximately 5 out of every 100 people in the U.S.
- Kelp Supplement Variation: Some supplements contain up to 4,000% of the daily value per pill.
- Recovery Time: Most healthy thyroids recover from iodine shock in 2 to 4 weeks.
- Amiodarone Content: A single 200mg tablet contains roughly 75,000 mcg of iodine.
- Salt Intake: Only about 70% of table salt sold in the U.S. is iodized.
The Biochemistry of Excess: Understanding the Wolff-Chaikoff Effect
To understand why iodine and hypothyroidism are linked, we have to look at the cellular level. The thyroid has a built-in safety valve known as the Wolff-Chaikoff effect. This was discovered in 1948.
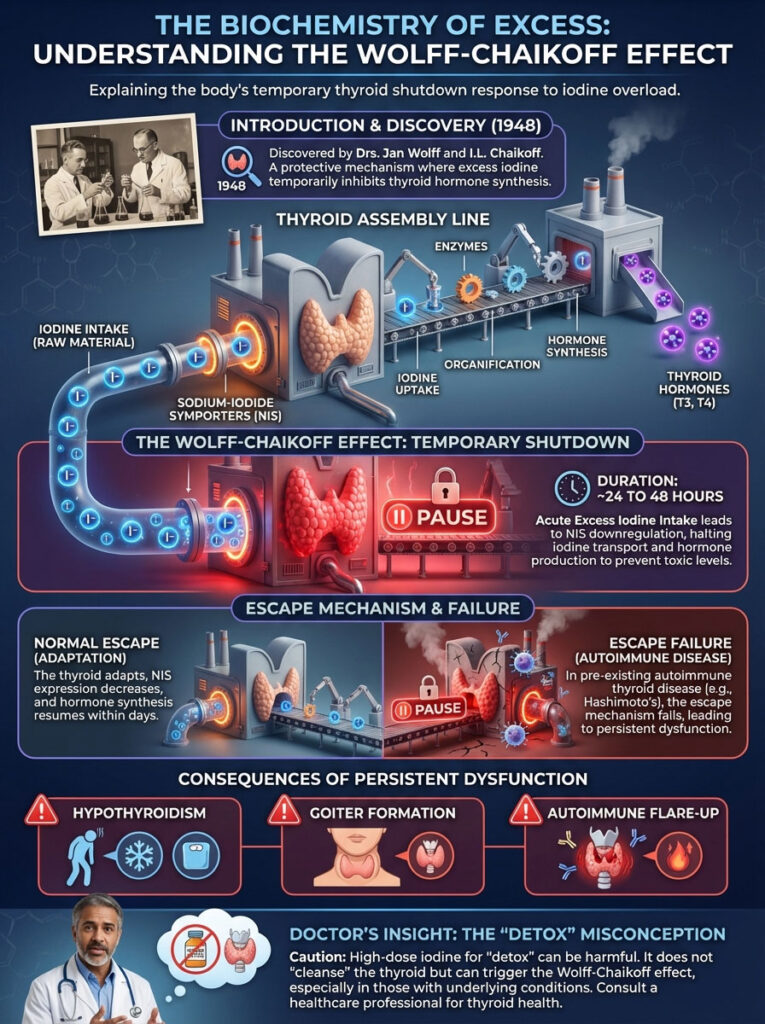
It remains one of the most important concepts in thyroid physiology. Think of your thyroid like a factory assembly line. Iodine is the raw material.
If you back a dump truck up to the factory door and dump tons of raw material onto the floor, the machinery gets clogged. The workers cannot move. Production stops.
Here is the step-by-step mechanism:
- Ingestion: You consume a high load of iodine (plasma inorganic iodide).
- Inhibition: The thyroid cells sense this dangerous surge. To prevent the production of toxic levels of thyroid hormone (thyrotoxicosis), the gland inhibits organification. This is the process where iodine is incorporated into thyroglobulin.
- Shutdown: The synthesis of T4 and T3 hormones stops completely. This is the “circuit breaker” tripping to save the system.
In a healthy person with no underlying thyroid disease, this shutdown is temporary. It lasts for about 24 to 48 hours. After this period, the thyroid adapts by downregulating the sodium-iodide symporters (NIS).
Think of the NIS as the doors to the factory. The thyroid effectively locks these doors so no more iodine can get in. This allows the internal machinery to clear the backlog and resume hormone production.
This adaptation is called the “escape” from the Wolff-Chaikoff effect. However, this escape mechanism is often broken in patients with autoimmune thyroid disease. Their thyroids shut down but fail to restart.
This leads to persistent iodine induced thyroid dysfunction.
Doctor’s Insight: Many patients believe they are “detoxing” when they feel bad after taking iodine. In reality, you are likely experiencing the acute suppression of your thyroid gland. Do not push through these symptoms.
Hashimoto’s Thyroiditis: Why You Are at Higher Risk
If you have Hashimoto’s thyroiditis, the rules change completely. Hashimoto’s is the most common cause of hypothyroidism in the United States. It is an autoimmune condition where the immune system attacks the thyroid gland.

Research clearly indicates that excess iodine acts like fuel on this autoimmune fire. When you introduce high levels of iodine to a gland that is already under attack, you increase the immunogenicity of thyroglobulin. Essentially, the iodine makes the thyroid proteins look “more foreign” to your immune system.
This provokes a stronger attack. We consistently see spikes in Thyroid Peroxidase (TPO) antibodies in patients who supplement with high-dose iodine. This antibody spike correlates with increased inflammation and tissue destruction.
For someone with Hashimoto’s thyroiditis, the Wolff-Chaikoff effect does not just cause a temporary pause. It often accelerates the progression from subclinical hypothyroidism to overt clinical hypothyroidism. This is the stage where you feel terrible and need medication.
Population studies support this finding. Countries that have aggressively iodized their salt supply often see a subsequent rise in the incidence of Hashimoto’s thyroiditis compared to populations with lower iodine intake. It is a delicate balance.
The Anatomy of Iodine Transport
To fully grasp the danger, we need to look at how iodine enters the cell. The thyroid cell membrane contains a specialized pump called the Sodium-Iodide Symporter (NIS). This pump is incredibly efficient.
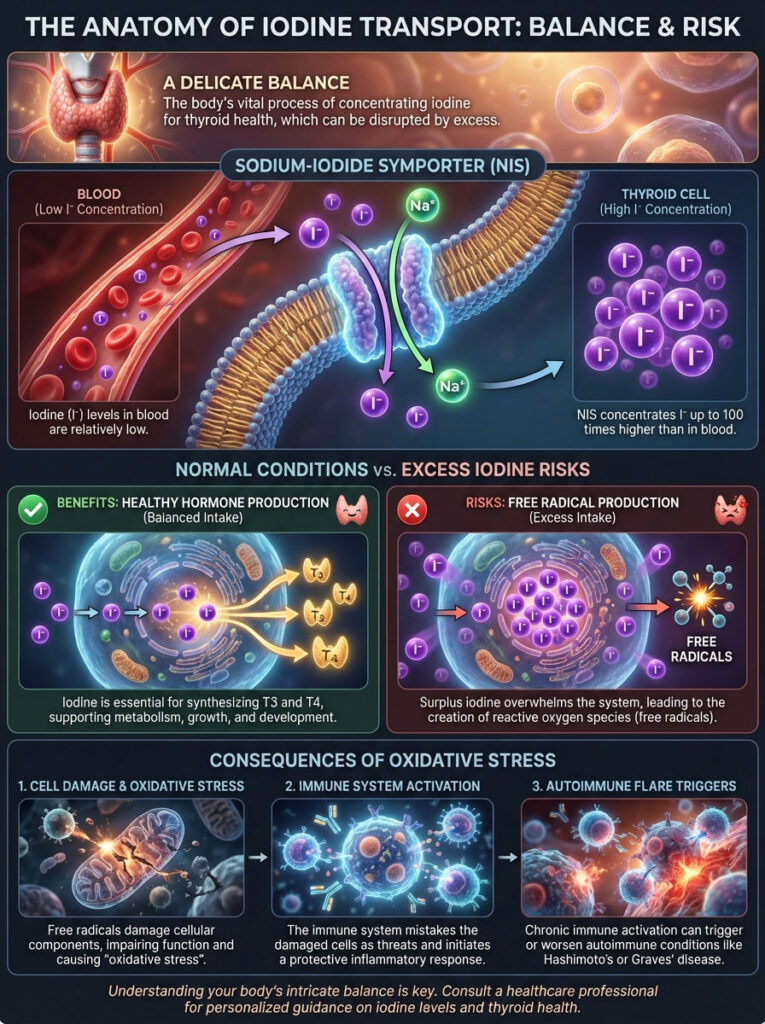
It concentrates iodine inside the thyroid cell to levels 20 to 40 times higher than in the blood. Under normal conditions, this is a miracle of biology. It ensures you can make hormones even when food is scarce.
However, under conditions of supplementation, this efficiency becomes a liability. The NIS pumps continue to pull iodine in until the internal concentration becomes toxic. This triggers the production of free radicals.
These free radicals cause oxidative stress. This stress damages the cellular machinery. In response, the immune system is alerted to the damage, causing an influx of white blood cells.
This is how a simple supplement can trigger an autoimmune flare. The body is trying to clean up the damage caused by the excess iodine.
The Jod-Basedow Phenomenon: The Other Side of the Coin
While the focus of this article is on iodine and hypothyroidism, I must mention the opposite risk to provide a complete picture. In some cases, excess iodine does not shut the thyroid down. Instead, it revs it up to dangerous levels.
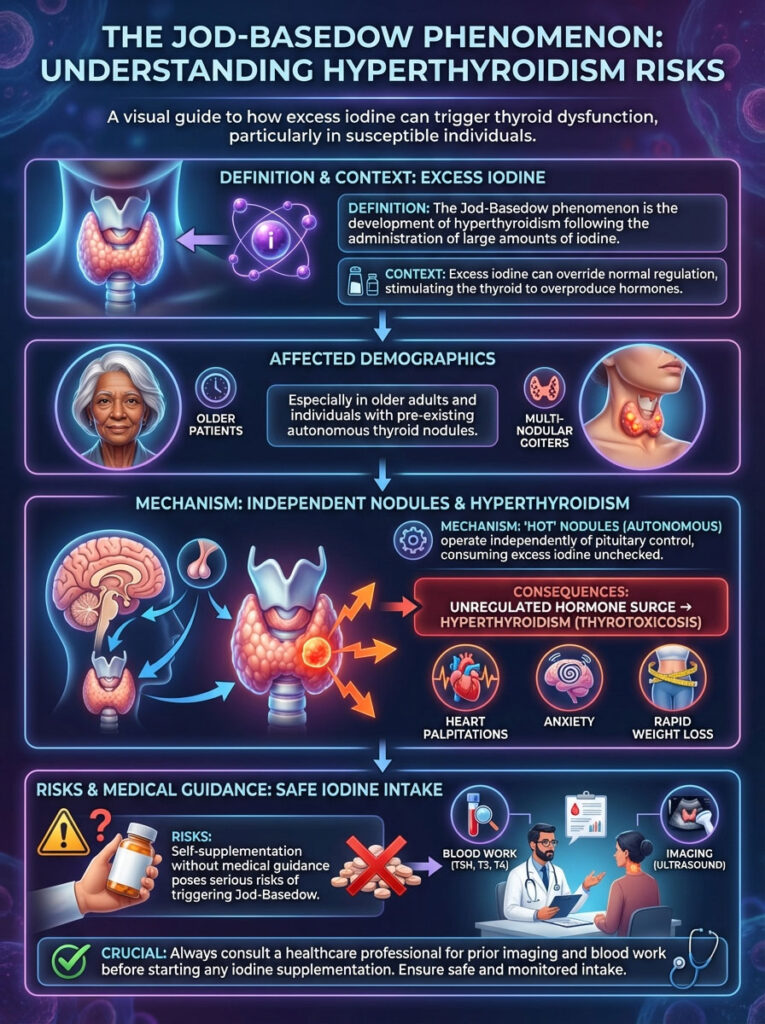
This is called the Jod-Basedow phenomenon. This typically happens in older patients or those with multi-nodular goiters. These “hot” nodules function independently of the pituitary gland’s control.
If you feed them iodine, they will produce hormone without an “off switch.” This leads to hyperthyroidism (thyrotoxicosis). The result is heart palpitations, anxiety, and rapid weight loss.
This is why self-supplementation is effectively playing Russian Roulette with your endocrine system. Without prior imaging to check for nodules and blood work to check for antibodies, you do not know how your body will react. You might face a hypothyroid crash (Wolff-Chaikoff) or a hyperthyroid storm (Jod-Basedow).
Sources of Danger: Supplements, Diet, and Medications
Where is this excess iodine coming from? In the American diet, it is rarely from table salt alone. The danger usually lurks in concentrated supplements and specific medications.
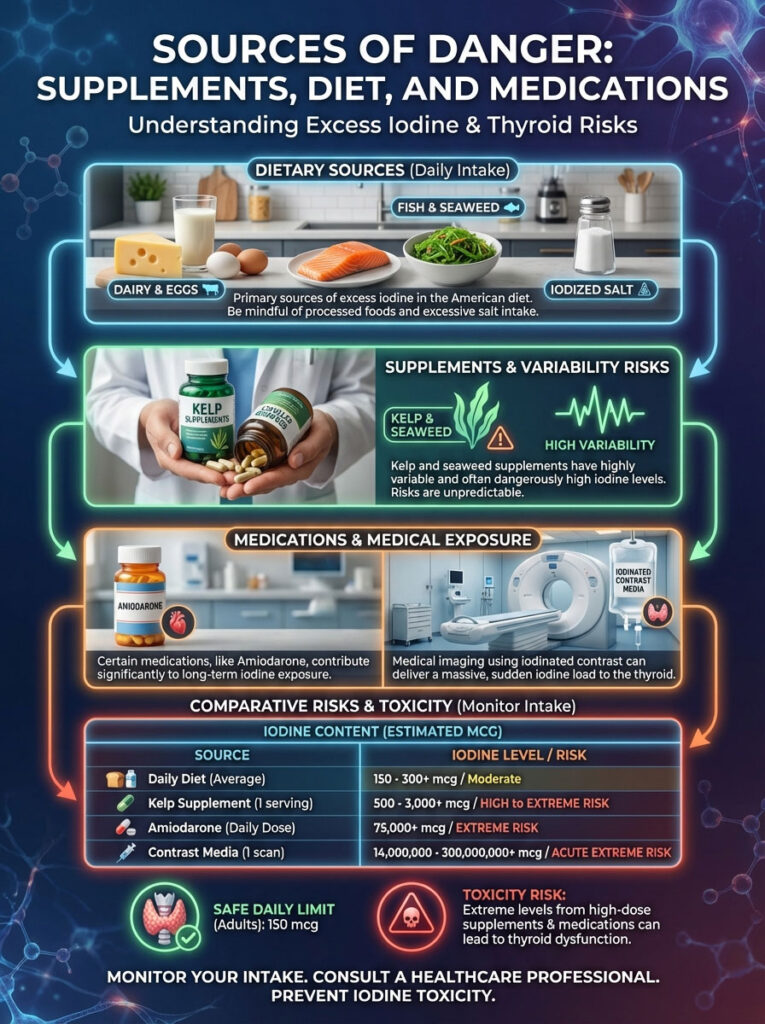
The Kelp and Seaweed Trap
Kelp supplements are the most frequent offenders I see in practice. Seaweed is incredibly efficient at soaking up iodine from seawater. The problem is the variability.
One capsule might contain 200 mcg. The next capsule from the same bottle might contain 2,000 mcg. Kelp supplements are largely unregulated, and the labels are often inaccurate.
Medications
Certain drugs carry massive iodine loads. Amiodarone, a medication used for heart rhythm problems, is 37% iodine by weight. A single dose can deliver thousands of times the daily requirement.
Iodinated contrast media is another source. This dye is used for CT scans and angiograms. It delivers a massive bolus of iodine that can trigger iodine induced thyroid dysfunction.
Table 1: The Scale of Iodine Exposure (Diet vs. Supplements)
To understand the magnitude of difference between food and supplements, look at the comparison below. Note how quickly supplements exceed the safe limits.
| Source Category | Specific Item | Iodine Content (Approx) | % of Daily RDA (150 mcg) | Risk Level |
|---|---|---|---|---|
| Dietary Standard | Iodized Table Salt (1/4 tsp) | 75 mcg | 50% | Safe / Recommended |
| Natural Food | Cod Fish (3 oz baked) | 99 mcg | 66% | Safe / Recommended |
| Supplement | Multivitamin (Standard) | 150 mcg | 100% | Safe |
| Supplement | Kelp / Bladderwrack Capsule | 500 – 3,000 mcg | 333% – 2,000% | High Risk |
| Medication | Amiodarone (1 tablet) | 75,000 mcg | 50,000% | Extreme (Requires Monitoring) |
| Supplement | Lugol’s Solution (1 drop 5%) | 6,250 mcg | 4,166% | Extreme Toxicity Risk |
The Salt Debate: Iodized vs. Sea Salt vs. Himalayan
There has been a massive culinary shift in recent years. Many households have moved away from white table salt toward pink Himalayan and Celtic sea salts. While these salts are less processed, they pose a specific problem for thyroid health.

The issue of non-iodized salt vs iodized salt is critical. Natural sea salts contain negligible amounts of iodine. This is because iodine evaporates during the drying process.
If you cook exclusively with pink salt and do not eat dairy or seafood regularly, you may drift into deficiency. This is the irony of the modern diet. We have people with iodine deficiency and people with iodine toxicity living on the same street.
However, if you are using iodized salt and taking supplements, you may drift into excess. My advice for balancing sodium and iodine is simple. Use iodized salt for your pasta water and baking.
Use the fancy finishing salts for flavor on top of the steak or salad. This strategy prevents deficiency. It also avoids the massive overdose associated with pills.
The Critical Role of Selenium
You cannot talk about iodine without talking about its partner, selenium. The relationship between iodine and selenium balance is vital for thyroid protection. Selenium is a cofactor for glutathione peroxidase.
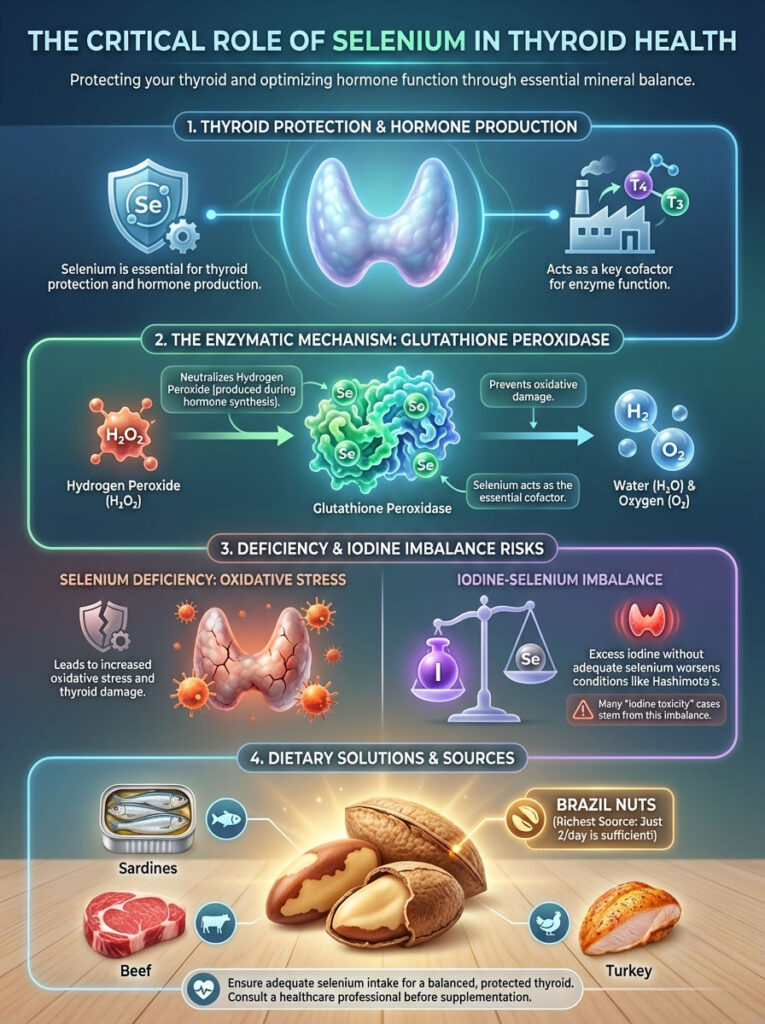
This is an enzyme that neutralizes hydrogen peroxide. When the thyroid makes hormones, it produces hydrogen peroxide as a byproduct. This is a normal part of the manufacturing process.
If you have enough selenium, your body neutralizes this oxidative stress. If you are selenium deficient and load up on iodine, the thyroid production line speeds up. Hydrogen peroxide builds up rapidly.
This acts like acid on the internal machinery. It damages the thyroid tissue directly. This damage attracts antibodies, worsening Hashimoto’s.
Many cases of “iodine toxicity” are actually cases of iodine-selenium imbalance. Before even considering iodine status, I ensure my patients have adequate selenium intake. This is best achieved through diet.
Brazil nuts are the most potent source. Eating just two Brazil nuts a day provides sufficient selenium. Sardines, beef, and turkey are also excellent sources.
Why the “Patch Test” is a Myth
You may have seen a popular home test on social media. The test involves painting a square of iodine on your skin. The claim is that if the patch disappears quickly, you are deficient.
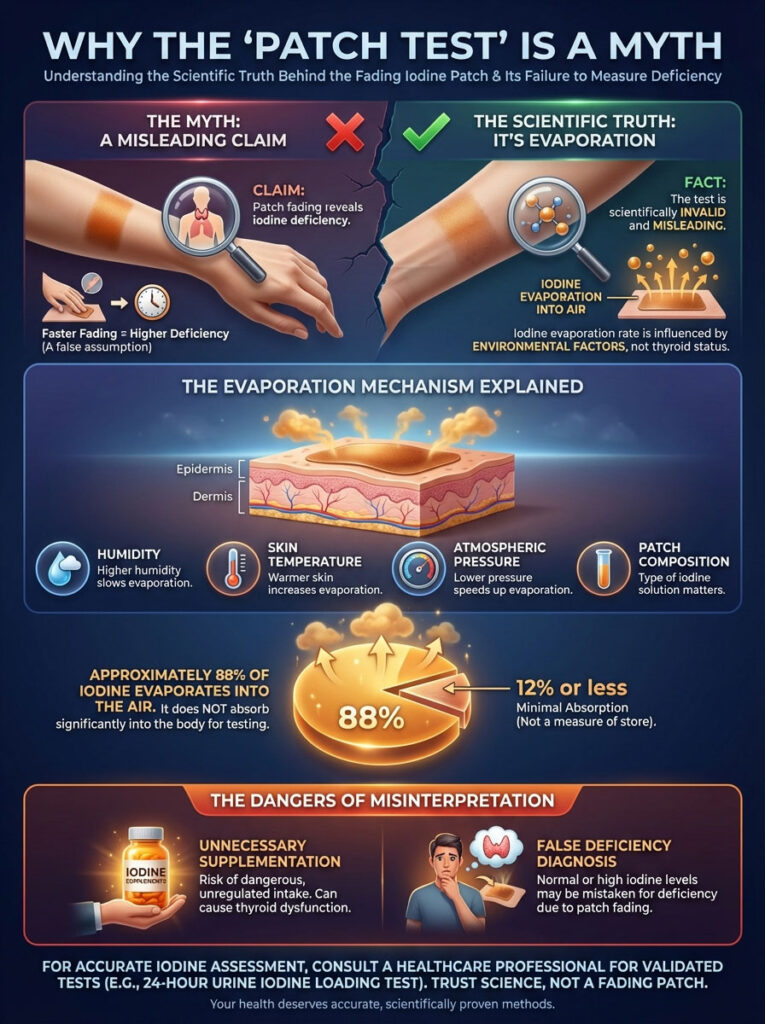
Here is the truth: The iodine patch test is scientifically invalid. The rate at which iodine disappears from your skin has nothing to do with your thyroid status. It is determined by evaporation and ambient humidity.
It is also determined by skin temperature and atmospheric pressure. About 88% of the iodine evaporates into the air. It does not absorb into your body.
Relying on this test can lead to dangerous supplementation. You might think you are deficient because the patch faded. In reality, you could have normal or even high iodine levels.
Interpreting Thyroid Labs: Identifying Iodine Issues
How do we know if iodine is the culprit behind your symptoms? We look at the data. Can too much iodine cause hypothyroidism visible on a lab test? Absolutely.
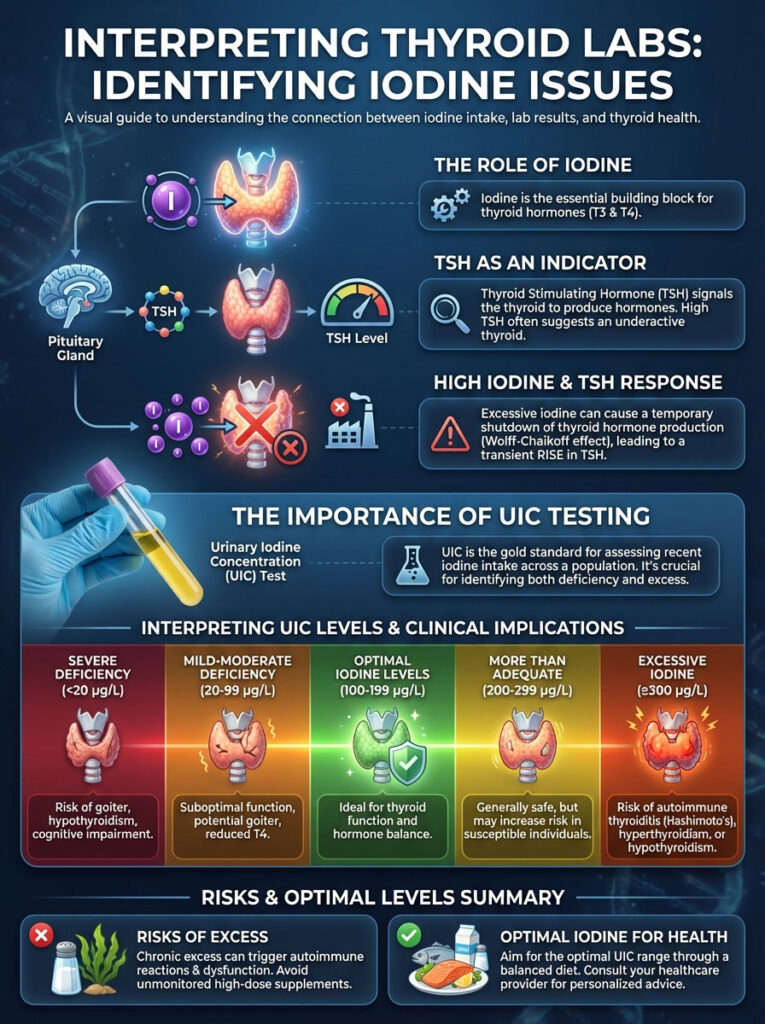
TSH (Thyroid Stimulating Hormone)
When the Wolff-Chaikoff effect hits, the thyroid stops making hormones. The pituitary gland senses low T4 levels. It screams at the thyroid to work harder.
This results in a rapid spike in TSH levels. I have seen TSH jump from 2.0 to 15.0 in a matter of weeks following high-dose supplementation. This mimics the lab results of severe thyroid failure.
Urinary Iodine Concentration (UIC)
Blood tests for iodine are notoriously unreliable. Iodine clears the blood very quickly. The gold standard is the urinary iodine concentration test.
Ideally, this is a 24-hour collection. However, spot tests are more common clinically. They give us a snapshot of how much iodine your body is excreting.
Table 2: Urinary Iodine Concentration (UIC) & Thyroid Health Status
This table outlines how we interpret urinary iodine levels in the context of thyroid health.
| Iodine Status | Urinary Iodine (mcg/L) | Clinical Implication | Impact on Thyroid |
|---|---|---|---|
| Severe Deficiency | < 20 mcg/L | Insufficient Hormone Production | Goiter, Hypothyroidism |
| Mild Deficiency | 20 – 49 mcg/L | Suboptimal Function | Risk of nodules |
| Optimal | 100 – 199 mcg/L | Ideal Thyroid Health | Normal T4/T3 production |
| Excessive | > 300 mcg/L | Risk of Dysfunction | Wolff-Chaikoff effect, Autoimmune flare-ups |
Signs You Have Overdosed on Iodine
Your body usually gives you warning signs before the thyroid completely crashes. Iodine toxicity symptoms can be physical and quite distinct from general hypothyroid symptoms. You need to know what to look for.
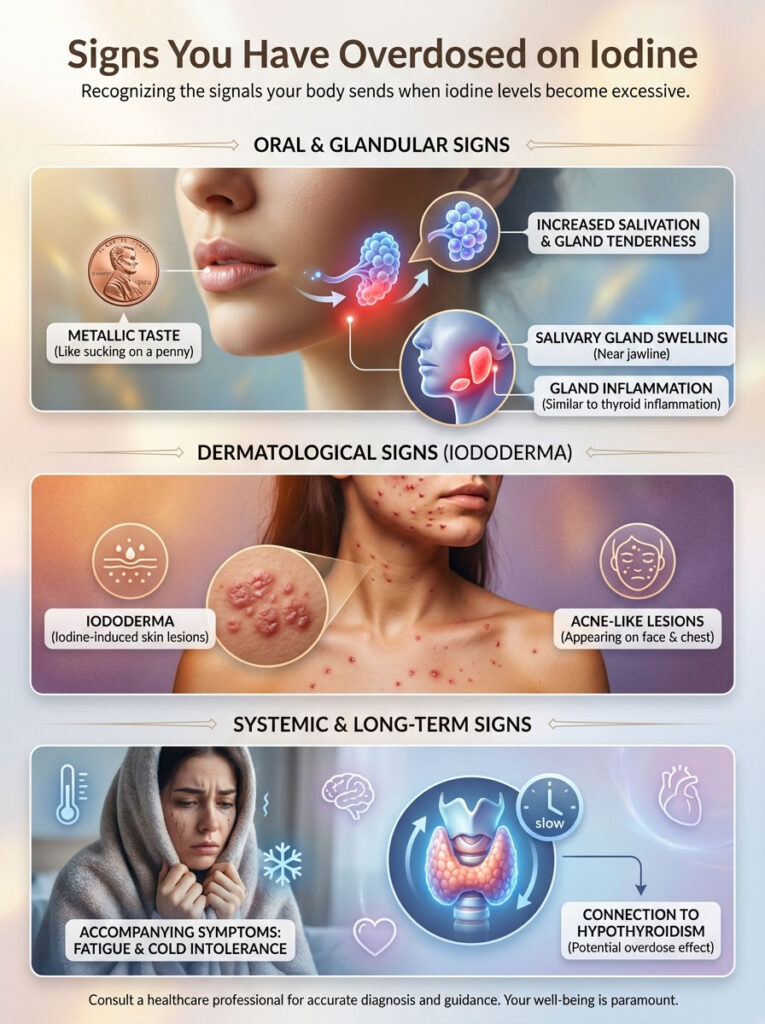
The most specific sign is a metallic taste in the mouth. Patients often describe it as sucking on a penny. This is due to iodine being secreted into the saliva.
Another common sign is increased salivation. You might also notice swelling of the salivary glands. These glands sit near the jawline and can become tender.
Because the salivary glands also concentrate iodine, they become inflamed just like the thyroid. You may also experience “iododerma.” This presents as acne-like skin lesions.
These lesions typically appear on the face and chest. If you develop these physical signs alongside fatigue and cold intolerance, pay attention. It is highly likely that iodine and hypothyroidism are linked in your case.
Special Populations: Pregnancy and Vegans
While excess is the main topic, we must address two specific groups. Pregnant women and vegans face unique challenges regarding iodine. The stakes are higher for these groups.
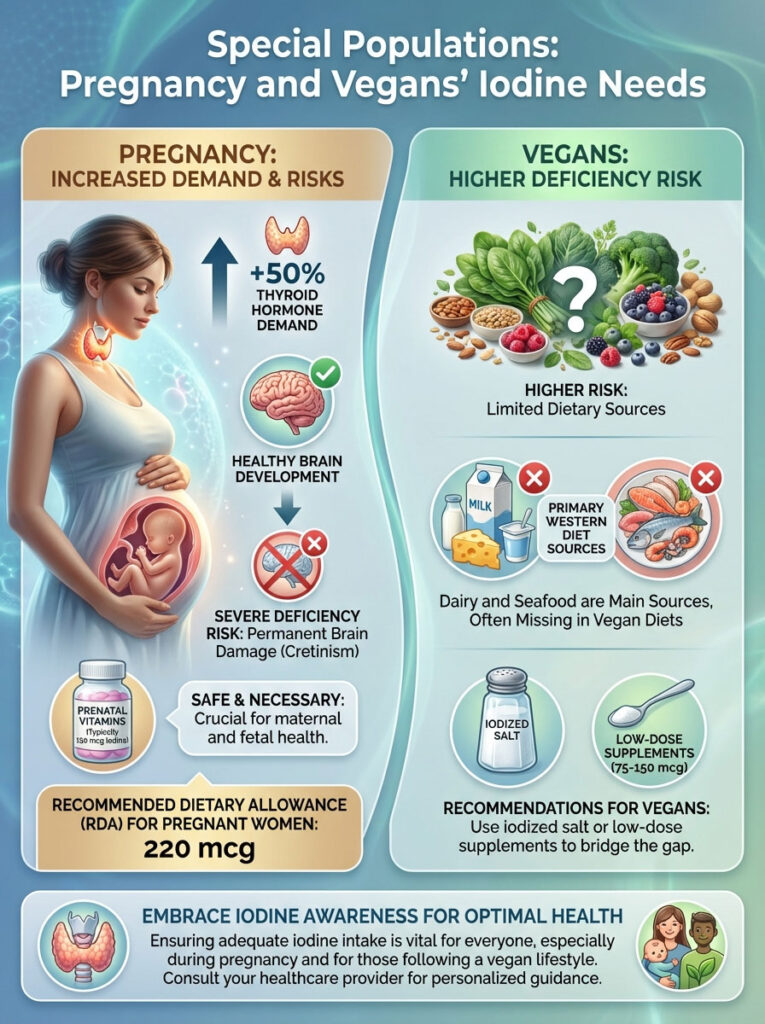
Pregnancy
During pregnancy, the demand for thyroid hormone increases by 50%. The mother must produce enough for herself and the developing baby. Severe iodine deficiency during pregnancy can lead to permanent brain damage in the infant.
This condition is known as cretinism. Because of this, the RDA for pregnant women is higher (220 mcg). Most prenatal vitamins contain 150 mcg of iodine.
This is safe and necessary. Do not avoid iodine in your prenatal vitamin out of fear of toxicity. The dose in prenatals is physiological, not pharmacological.
Vegans
Vegans are at higher risk for deficiency. The primary sources of iodine in the Western diet are dairy and seafood. Plant-based milks (almond, oat, soy) typically contain no iodine unless fortified.
If you are vegan, you should use iodized salt. Alternatively, you can take a low-dose supplement (75-150 mcg). Avoid high-dose kelp products, as they are too unpredictable.
Treatment and Recovery: Reversing Iodine-Induced Hypothyroidism
The good news is that iodine induced thyroid dysfunction is often reversible. The treatment protocol is primarily about removal and patience. We have to let the system clear.

Step 1: Elimination. You must stop the source of excess iodine immediately. This means cessation of kelp supplements and seaweed snacks.
Check your multivitamins and hair/nail supplements. If the source was a medication like Amiodarone, do not stop it abruptly. Consult your cardiologist, but alert them to the thyroid changes.
Step 2: The Waiting Game. For many patients, the Wolff-Chaikoff effect reverses spontaneously. This usually happens within 2 to 4 weeks of lowering iodine intake.
We monitor TSH levels every 4 to 6 weeks. We want to watch them normalize without jumping the gun on medication. The body is resilient.
Step 3: Levothyroxine Support. Sometimes the TSH remains dangerously high or symptoms are debilitating. In these cases, we may use a short course of Levothyroxine.
This takes the pressure off the thyroid gland. It allows the gland to rest while the excess iodine clears the system. For patients with Hashimoto’s thyroiditis, this support might need to be longer-term.
Expert Guidelines for Safe Intake
So, how do you get enough without getting too much? The Recommended Dietary Allowance (RDA) for adult men and women is 150 mcg per day. During pregnancy, this increases to 220 mcg.
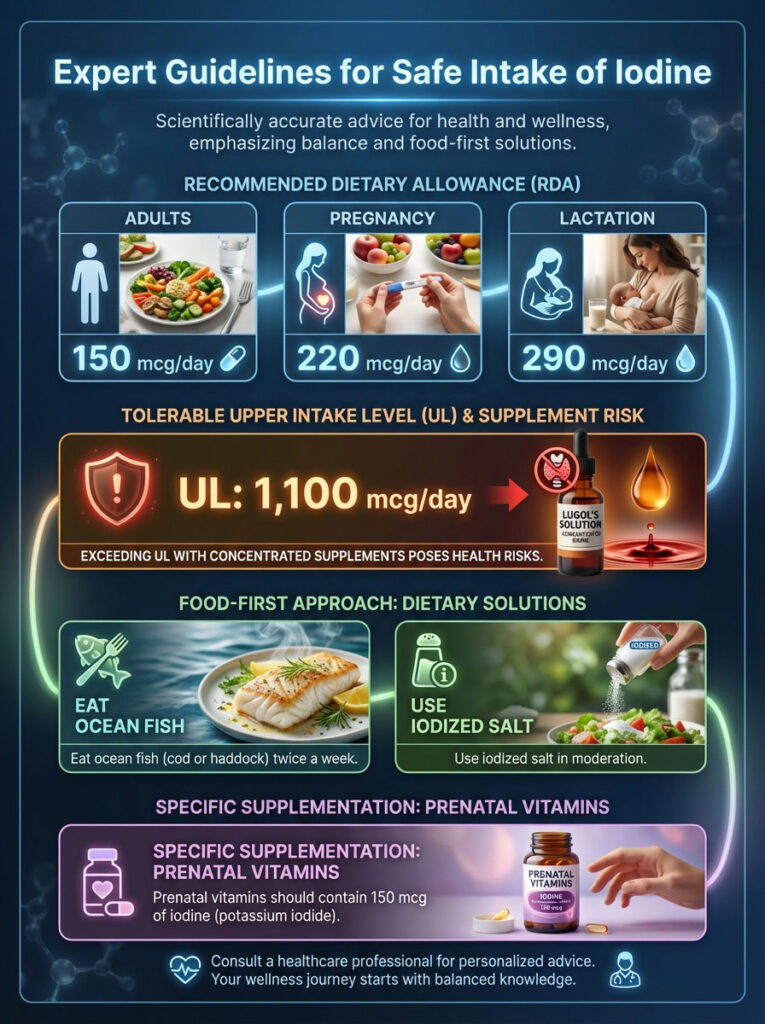
During lactation, it increases further to 290 mcg. These numbers are well-researched and safe. They provide enough fuel for the factory without clogging the machines.
The Tolerable Upper Intake Level (UL) is 1,100 mcg. While this seems like a large buffer, remember the concentration of supplements. One drop of Lugol’s solution can contain over 6,000 mcg.
It is incredibly easy to blow past the safety limit with concentrated products. My protocol for patients is food-first. Eat ocean fish (like cod or haddock) twice a week.
Use iodized salt in moderation. If you are pregnant, ensure your prenatal vitamin contains 150 mcg of iodine. This is usually in the form of potassium iodide.
Avoid high-dose kelp supplements unless prescribed for a very specific reason. An example would be radioactive protection protocols. For general health, they are unnecessary risks.
The Dangers of Online “Iodine Protocols”
There are numerous online communities promoting “high-dose iodine protocols.” These groups often recommend taking 12,000 mcg to 50,000 mcg daily. They claim this cures everything from breast cysts to fatigue.

They often state that negative side effects are just “bromine detox symptoms.” As a medical professional, I must warn you against this. There is no scientific evidence supporting “bromine detox” as a cause of these symptoms.
The symptoms described—headaches, fatigue, brain fog—are classic signs of induced hypothyroidism. Following these protocols can cause permanent damage to the thyroid. It can turn a temporary problem into a lifelong disease.
Summary & Key Takeaways
The relationship between iodine and hypothyroidism is a classic example of the Goldilocks principle: not too little, not too much. While the internet is full of advice suggesting that high doses of iodine will cure your fatigue and weight gain, the biological reality of the Wolff-Chaikoff effect proves otherwise.
Excess iodine triggers a protective shutdown of the thyroid gland. For those with Hashimoto’s thyroiditis, this shutdown can be severe and persistent. By understanding the risks of iodine toxicity symptoms and prioritizing a balanced intake through whole foods and safe salt practices, you can protect your thyroid function.
If you suspect you have induced thyroid dysfunction through supplementation, do not panic. Stop the supplements immediately. See an endocrinologist for a full panel.
Ensure this panel includes a urinary iodine concentration test and thyroid antibodies. Your thyroid is resilient, but it needs the right environment to thrive. Treat it with respect, not with massive doses of raw materials it cannot handle.
Frequently Asked Questions
Can too much iodine cause hypothyroidism?
Yes, excessive iodine can trigger a protective biological mechanism known as the Wolff-Chaikoff effect, which causes the thyroid to temporarily stop producing hormones. While intended to prevent toxicity, this shutdown can lead to persistent hypothyroidism, particularly in individuals with pre-existing autoimmune conditions like Hashimoto’s.
What is the Wolff-Chaikoff effect in thyroid physiology?
The Wolff-Chaikoff effect is an auto-regulatory phenomenon where the thyroid gland inhibits the organification of iodide in response to high plasma inorganic iodide levels. Essentially, the gland shuts down the synthesis of T4 and T3 to prevent a dangerous surge of thyroid hormones, acting as a metabolic circuit breaker.
Is iodine supplementation safe for patients with Hashimoto’s thyroiditis?
I generally advise against high-dose iodine for Hashimoto’s patients because it can increase the immunogenicity of thyroglobulin, effectively fueling the autoimmune attack. In these cases, the thyroid often fails to “escape” the Wolff-Chaikoff shutdown, accelerating the progression from subclinical to overt clinical hypothyroidism.
How does excess iodine impact TPO antibody levels?
Clinical research shows that a sudden influx of iodine can cause a significant spike in Thyroid Peroxidase (TPO) antibodies. This increase in antibodies correlates with heightened inflammation and oxidative stress within the thyroid tissue, often worsening the underlying autoimmune disease.
What are the primary symptoms of iodine toxicity or overdose?
Specific signs of iodine toxicity include a metallic taste in the mouth, increased salivation, and swelling of the salivary glands near the jawline. You may also notice “iododerma,” which are acne-like skin lesions, alongside systemic symptoms like profound fatigue and cold intolerance as hormone production drops.
Is the iodine skin patch test an accurate way to check for deficiency?
The iodine patch test is scientifically invalid and I do not recommend it for clinical assessment. The rate at which the iodine stain disappears from your skin is determined by atmospheric pressure, ambient humidity, and skin temperature, rather than your internal thyroid status.
Why do kelp supplements pose a risk to thyroid health?
Kelp and other seaweed-based supplements are notoriously unregulated and exhibit extreme variability in their iodine content. A single capsule can contain thousands of micrograms, far exceeding the tolerable upper limit of 1,100 mcg, which can easily trigger a thyroid crash or a hyperthyroid storm.
What is the difference between the Wolff-Chaikoff effect and the Jod-Basedow phenomenon?
The Wolff-Chaikoff effect leads to hypothyroidism by shutting down hormone production, while the Jod-Basedow phenomenon leads to hyperthyroidism by causing the gland to overproduce hormones. Jod-Basedow typically occurs in older patients or those with multi-nodular goiters who lack the normal regulatory “off switch.”
How long does it take for the thyroid to recover from iodine-induced dysfunction?
In most patients with healthy thyroid glands, hormone production resumes within two to four weeks after stopping the excess iodine intake. However, those with autoimmune markers may require a longer recovery period or a temporary course of levothyroxine to support the gland while it clears the excess mineral.
Do I need iodine supplements if I use pink Himalayan or Celtic sea salt?
Because natural specialty salts contain negligible amounts of iodine, you may drift into deficiency if you do not consume other sources like dairy or seafood. I recommend using iodized table salt for standard cooking and saving the specialty salts for finishing to ensure a consistent, safe daily intake.
Why is selenium important when considering iodine intake?
Selenium is a vital cofactor for enzymes that neutralize hydrogen peroxide produced during thyroid hormone synthesis. If you increase iodine without adequate selenium, the resulting oxidative stress can damage thyroid cells, potentially triggering or worsening autoimmune thyroiditis.
How is iodine-induced thyroid dysfunction diagnosed in a clinical setting?
We typically identify this through a combination of blood work showing elevated TSH levels and a comprehensive urinary iodine concentration (UIC) test. A UIC reading above 300 mcg/L, paired with a history of recent supplementation, strongly suggests iodine-induced dysfunction.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The relationship between iodine and thyroid function is complex; always consult a qualified endocrinologist or healthcare professional before starting or stopping any supplement regimen, especially if you have a pre-existing autoimmune condition.
References
- American Thyroid Association – thyroid.org – Professional guidelines on iodine supplementation and thyroid function in the U.S. population.
- The Journal of Clinical Endocrinology & Metabolism – “The Wolff-Chaikoff Effect” – Peer-reviewed research detailing the biochemical inhibition of thyroid hormone synthesis by excess iodide.
- National Institutes of Health (NIH) – Office of Dietary Supplements – Official data on RDA, Upper Limits, and iodine content in various foods and medications.
- Endocrine Reviews – “Iodine-Induced Thyroid Dysfunction” – Comprehensive clinical review of the Jod-Basedow phenomenon and Wolff-Chaikoff effect.
- World Health Organization (WHO) – “Urinary Iodine Concentrations for Determining Thyroid Status” – Global standards for assessing iodine sufficiency and excess in populations.
- Thyroid Journal – “Autoimmunity and Iodine Intake” – Research study linking aggressive salt iodization to increased prevalence of Hashimoto’s thyroiditis.








