I see it every day in my clinic. You are sitting on the paper-covered table; looking at me with a mixture of exhaustion and frustration. The lab results in your hand say “normal;” but the handful of hair you pulled from your brush this morning tells a different story. Thyroid hair loss is often the most distressing symptom for my patients because it is the one they cannot hide. It feels personal. It feels like you are losing a part of yourself.
Table of Contents
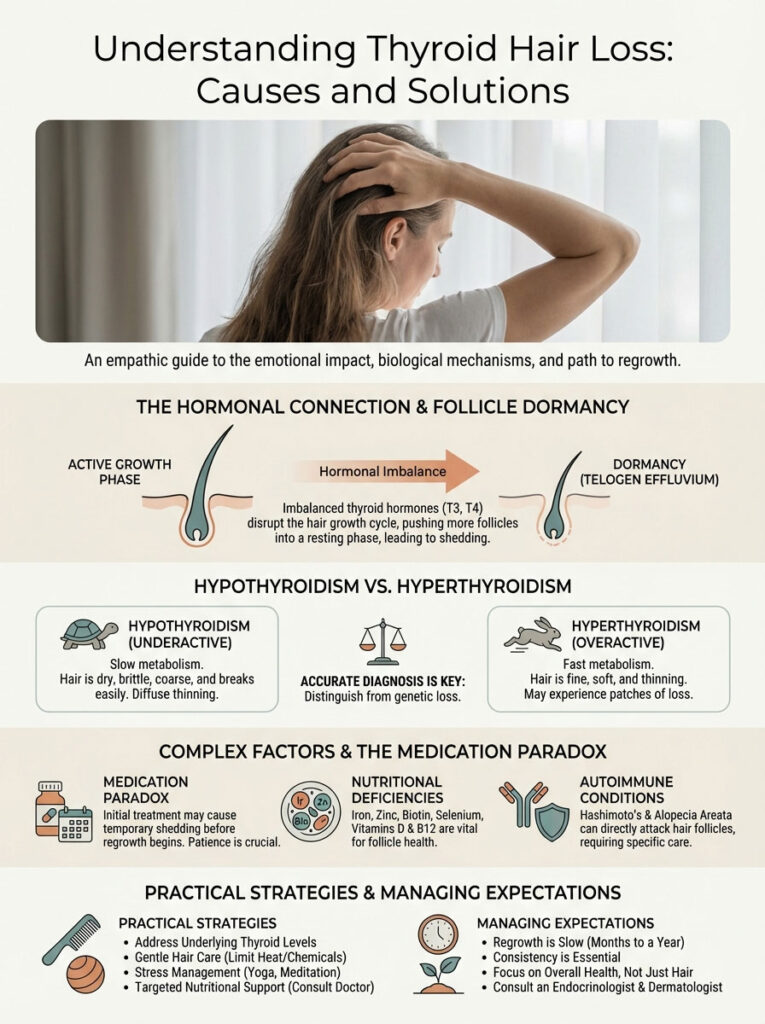
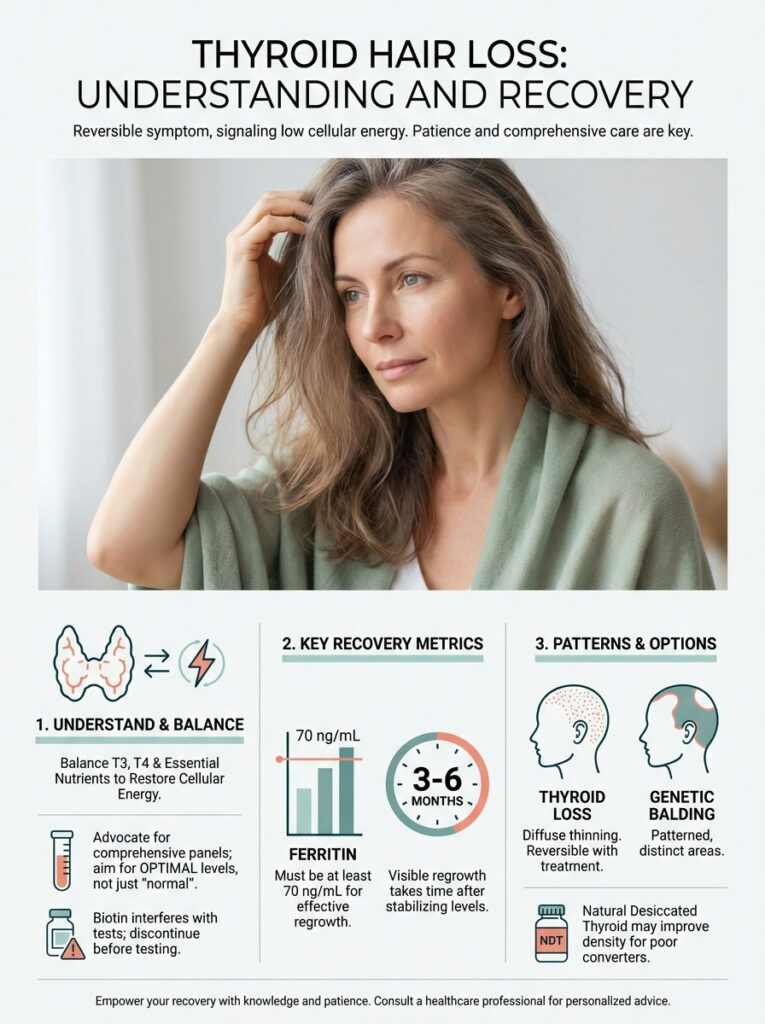
Here is the clinical reality that I share with every patient who walks through my door: this type of alopecia is almost always non-scarring. The follicle is not dead; it is simply dormant. When we correct the underlying hormonal imbalance and fix the nutritional deficits that accompany it; the hair grows back. It is a biological certainty; provided we treat the root cause correctly.
Will thyroid hair grow back?
Yes, thyroid hair loss is reversible. Once T3 and T4 hormone levels stabilize and nutritional deficiencies like ferritin are corrected, hair follicles re-enter the anagen growth phase. Visible regrowth typically occurs 3 to 6 months after treatment optimization. The follicles are not dead; they are merely in a prolonged resting state due to a lack of metabolic energy.
The journey from seeing your scalp through your hair to seeing full density returns requires patience. It involves understanding why your body has hit the “pause” button on growth; navigating the paradox of medication shedding; and optimizing your labs beyond the standard reference range. You must become the CEO of your own health.
Key Thyroid Hair Stats:
- 70%: Percentage of scalp hairs that can shift to “resting” phase during thyroid shock.
- 50%: Hypothyroid patients who experience diffuse hair loss.
- 3-4 Months: Typical lag time between a thyroid event and visible shedding.
- 70 ng/mL: The minimum Ferritin level often required for regrowth.
- 0.5 – 2.5 mIU/L: The optimal TSH range where many patients see hair recovery.
The Endocrine-Follicle Connection: Why It Happens
To fix the problem; you must understand the mechanism. Your hair cells are the second fastest-dividing cells in your body; surpassed only by bone marrow. This rapid division requires an immense amount of energy in the form of ATP (Adenosine Triphosphate). Your thyroid gland is the master regulator of this metabolism. It dictates how efficiently your cells create and use energy.
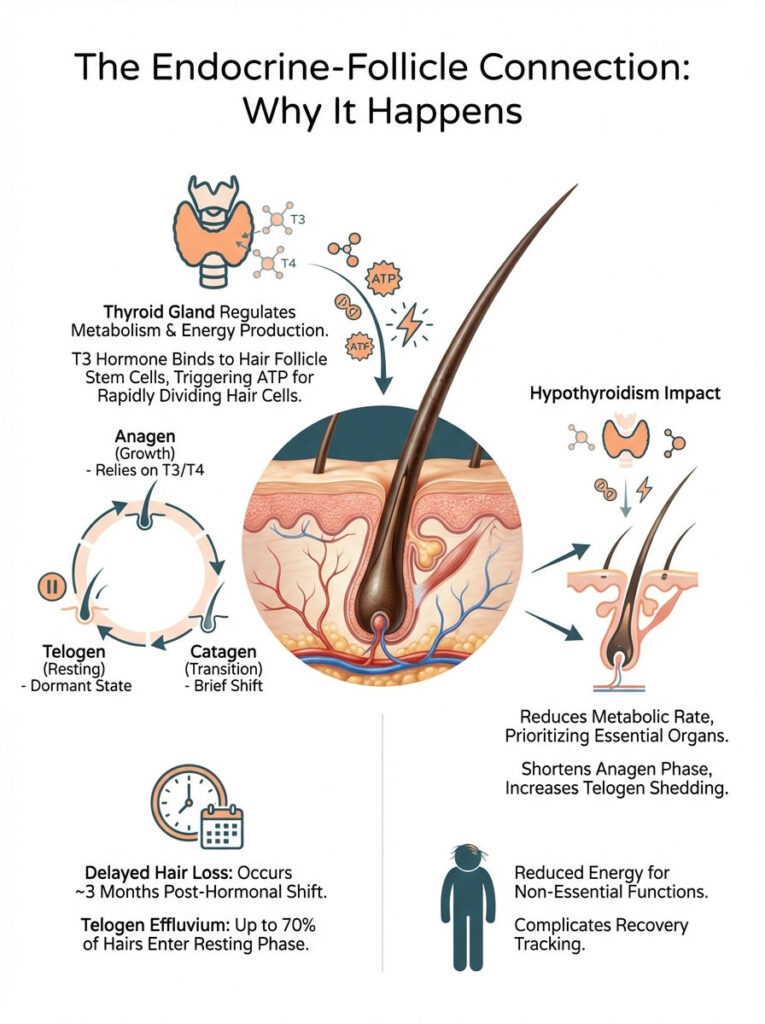
Think of your thyroid hormone as the gas pedal for your body’s cellular engine. When you have sufficient T3 (Triiodothyronine); the active thyroid hormone; it binds to receptors on the hair follicle stem cells. This binding signals the mitochondria within the cell to produce energy. This energy drives the rapid cellular division required to push a hair shaft out of the scalp.
When you have hypothyroidism (an underactive thyroid); your basal metabolic rate drops. The body enters a state of conservation. It prioritizes essential organs like the heart; lungs; and brain. Hair growth is biologically “expensive” and non-essential for survival. Therefore; the body shuts down energy supply to the hair follicles to save resources. The gas pedal is released; and the engine stalls.
Understanding the Biology of Your Hair Cycle
To understand why your hair is falling out now; we have to look at what happened three months ago. Hair growth is not a continuous process; it is cyclical. Every hair on your head is in a different phase of this cycle. Thyroid dysfunction disrupts the rhythm of this clock.
The cycle consists of three distinct phases. The first is Anagen (Growth). This phase relies heavily on T3 and T4 hormones. In a healthy scalp; 90% of your hair is in this phase for years. It is the active manufacturing of the hair shaft. Without adequate thyroid hormone; the anagen phase is cut short. The follicle cannot sustain the energy output required to lengthen the hair.
The second phase is Catagen (Transition). This is a short regression phase lasting only a few weeks. The follicle shrinks and detaches from the blood supply (the dermal papilla). This is a normal part of the process; but in thyroid disease; follicles may rush into this phase prematurely.
The final phase is Telogen (Resting). This is the shedding phase. The hair is no longer growing; it is simply sitting in the follicle waiting to be pushed out. In thyroid disease; the body forces hairs into this phase en masse to conserve energy. This is the core mechanism of your hair loss.
Telogen Effluvium Explained
The clinical term for thyroid hair loss is often Telogen Effluvium. This is not the same as going bald or genetic receding. Instead; it is a reactive process. A sudden shift in hormones shocks the system. Instead of the usual 10% of hairs being in the resting phase; up to 70% of your hairs may suddenly enter the telogen phase.
Here is the tricky part regarding timing. The resting phase lasts about three months. The hair remains anchored in the scalp during this time; even though it is dead. It only falls out when a new hair begins to grow underneath it and pushes it out. Consequently; you might not see the hair fall out until 90 days after the thyroid issue began.
This delay often confuses patients. You might be looking at what you ate last week or a shampoo you used yesterday. However; the trigger was likely a hormonal fluctuation; a stressful event; or a medication change that occurred three months prior. Understanding this lag time is crucial for tracking your recovery.
Hypothyroidism vs. Hyperthyroidism Hair Loss
While both conditions cause loss; the presentation differs clinically. As an endocrinologist; I look for specific textures and patterns to distinguish between them. Your hair tells a story about your internal metabolic state.
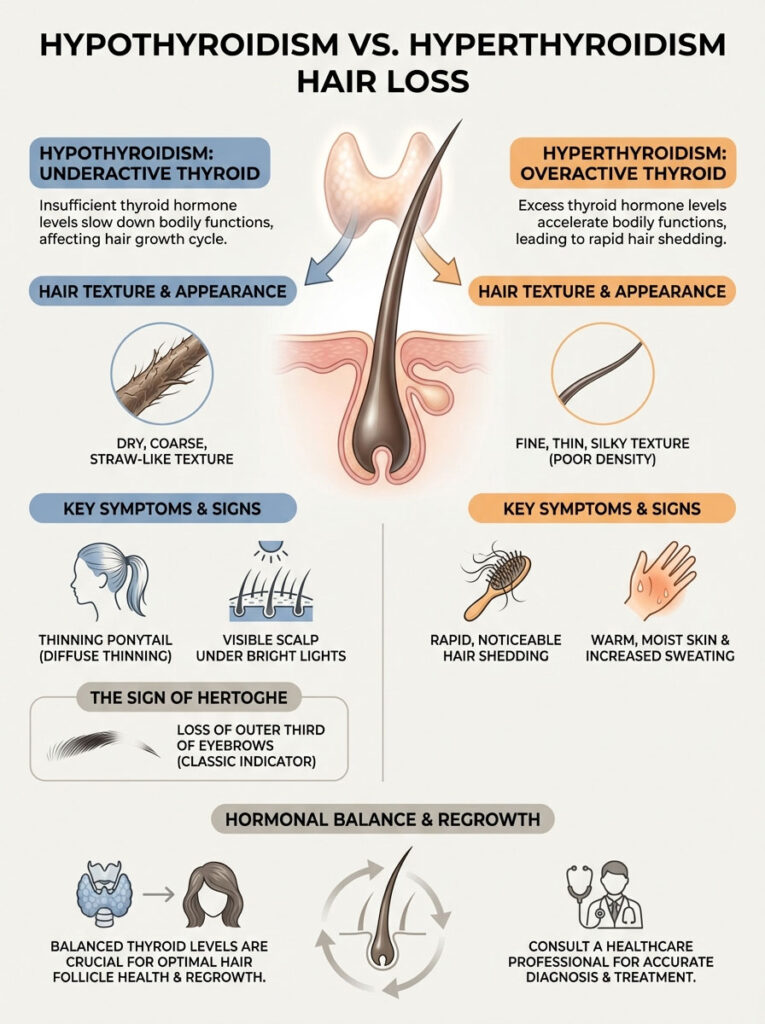
Hypothyroidism (Underactive): The metabolism is too slow. The hair becomes dry; coarse; and straw-like. It lacks moisture because the sebaceous glands (oil glands) are also down-regulated by low thyroid hormone. The hair breaks easily. The loss is diffuse; meaning it thins evenly all over the scalp rather than in a specific spot. Patients often report their ponytail feels thinner or they see more scalp showing through under bright lights.
Hyperthyroidism (Overactive/Graves’ Disease): The mechanism here is different. The metabolism is too fast. The hair cycle accelerates so rapidly that the hair falls out before it can fully thicken or grow long. The hair texture is often fine; thin; and silky; but the density is poor. It can feel baby-soft but lacks the structural integrity to grow length. Patients may also notice their skin is warm and moist due to increased blood flow and sweating.
The Sign of Hertoghe
One of the most telling physical signs I look for during a physical exam is the Sign of Hertoghe. This refers to the thinning or complete loss of the outer third of the eyebrows. It is a classic sign of hypothyroidism that has been recognized for over a century. It is named after Queen Anne of Denmark; who was famously depicted with this sign.
If you look in the mirror and see your eyebrows stopping abruptly before the arch ends; this is a strong indicator. It suggests that your thyroid medication dose is not yet optimal; regardless of what the TSH lab report says. Eyebrow hairs are particularly sensitive to thyroid hormone levels. Their loss is often the first sign of an issue and their regrowth is a reliable marker of recovery.
Diagnosis: Is It Your Thyroid or Genetics?
A common fear is that the hair loss is genetic and therefore permanent. Distinguishing between hormonal loss and genetic balding is vital for the treatment plan. We use a “Pull Test” in the office. I gently grasp a cluster of about 40 hairs and apply light traction. In genetic hair loss; I might get one or two hairs. In active Telogen Effluvium; I might easily pull out six to ten hairs with white bulbs at the end.
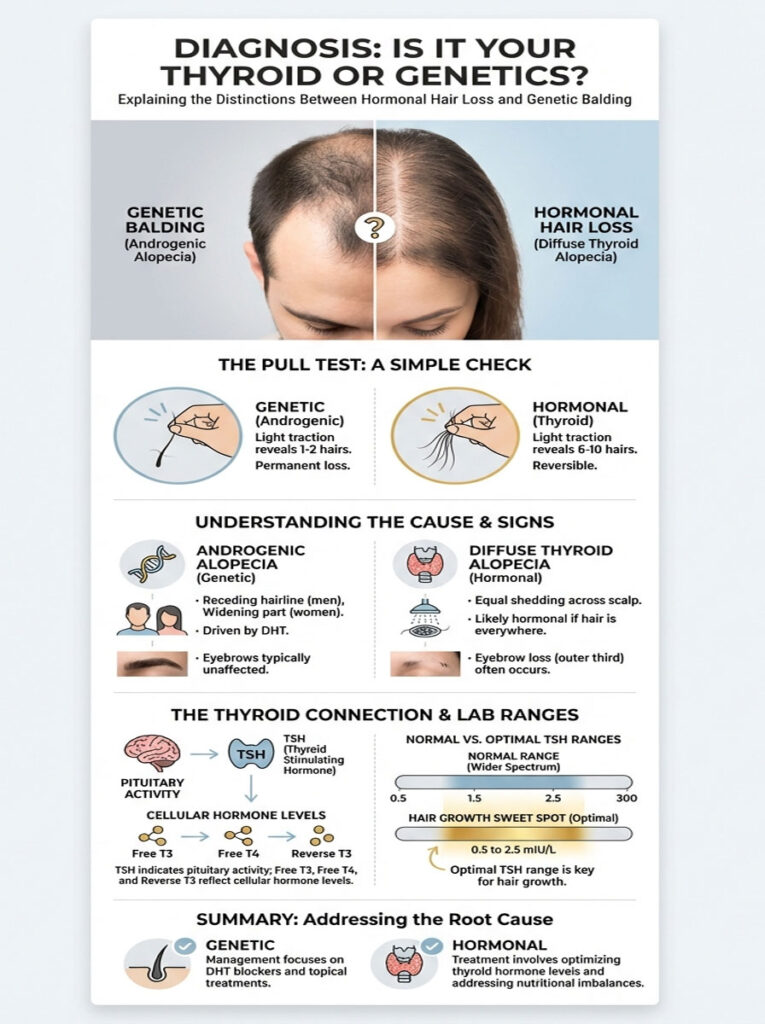
Distinguishing Hormonal Loss from Genetic Balding
Androgenic Alopecia (genetic pattern baldness) presents differently. In men; the hairline recedes at the temples. In women; the part widens significantly; often resembling a Christmas tree pattern; but the frontal hairline is usually preserved. This is driven by DHT (dihydrotestosterone); not a lack of energy.
Diffuse Thyroid Alopecia ignores these boundaries. It affects the sides; the back; and the top equally. If you are finding hair everywhere—on your pillow; in the shower; on your clothes; and on the floor—it is likely hormonal. You are shedding from the entire surface area of the scalp. This distinction is important because treatments for genetic loss (like DHT blockers) will not fix thyroid loss.
The “Normal” vs. “Optimal” Lab Range Debate
This is where many patients get stuck. You might be told your TSH levels are “normal” because they fall under 4.5 or 5.0 mIU/L. However; “normal” is a statistical average including many sick people; not a definition of health. The reference range is a bell curve of the population visiting the lab; many of whom have thyroid dysfunction.
For hair follicle recovery; we aim for “optimal.” The Hair Growth “Sweet Spot” for TSH is typically between 0.5 and 2.5 mIU/L. If your TSH is 3.5; you might not have clinical fatigue; but it may be high enough to inhibit hair growth. The follicle is the canary in the coal mine; it is the first thing to suffer when levels drift.
Furthermore; TSH tells us what the pituitary gland is doing; not how much hormone is reaching the cells. We must look at Free T3; Free T4; and Reverse T3 to get the full picture. Free T3 is the active gas. If your TSH is normal but your Free T3 is in the bottom 20% of the range; your hair will likely continue to shed.
| Feature | Thyroid Hair Loss (Telogen Effluvium) | Genetic Hair Loss (Androgenic Alopecia) |
|---|---|---|
| Pattern | Diffuse thinning all over the scalp; including sides and back. | Distinct pattern (receding hairline or widening part). |
| Texture | Hair becomes dry; straw-like; brittle; and tangles easily. | Hair texture remains normal; strands just become finer (miniaturization). |
| Onset | Can be sudden (months) after a hormonal shift or medication change. | Gradual onset over several years; slow progression. |
| Eyebrows | Often affects the outer third (Sign of Hertoghe). | Usually does not affect eyebrows. |
| Reversibility | Highly reversible with treatment optimization. | Difficult to reverse; treatment aims to slow progression. |
The Medication Paradox: “I Started Meds and Lost More Hair”
There is a specific moment of panic that occurs about two months after a patient starts treatment. They call the office; upset; saying; “The medication is making my hair fall out!” This is the Levothyroxine hair loss paradox. It is counterintuitive; but this shedding is actually a sign that the treatment is working.
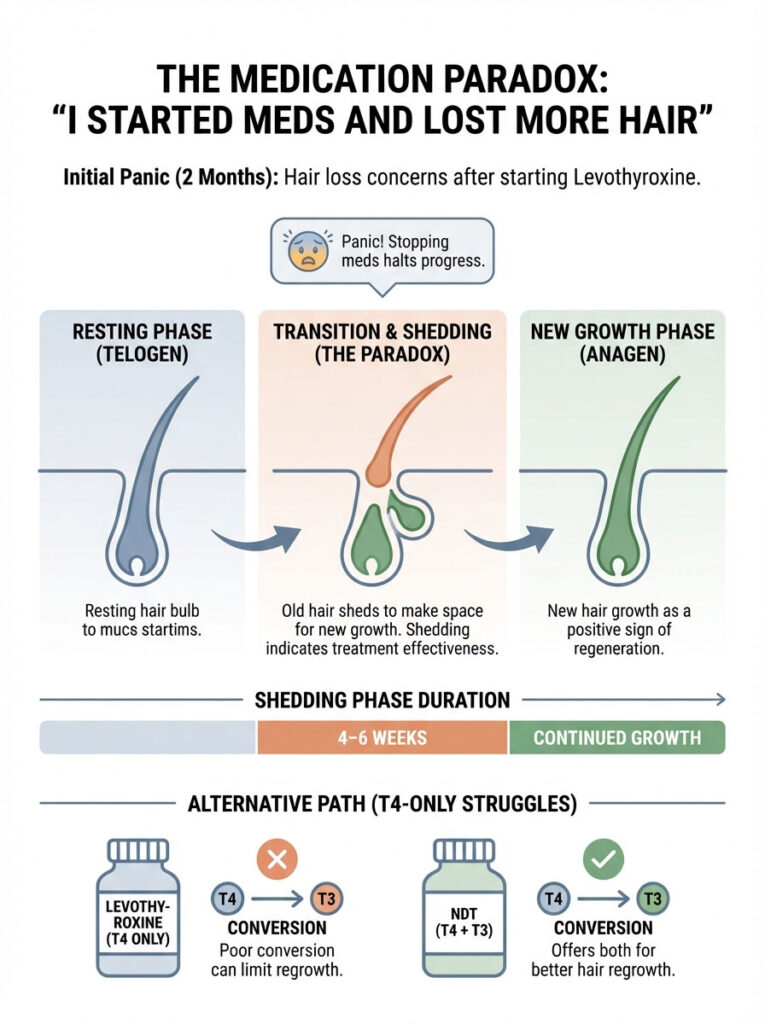
This phenomenon terrifies patients. It leads many to stop their medication; thinking they are having an allergic reaction. Understanding the physiology behind this shed is the only way to stay the course. It is a necessary evil on the road to regrowth.
The Levothyroxine Shedding Phase
When you introduce thyroid hormone (Levothyroxine/Synthroid) to a body that has been starved of it; the metabolic rate accelerates. This sudden surge of energy “wakes up” the hair follicles. The follicles that have been stuck in the resting phase are pushed into the growth phase.
Here is the catch: a follicle cannot hold two hairs at once. To grow a new hair; the follicle must first eject the old; dead hair shaft that was sitting in the pore. Consequently; you see a mass exodus of hair. This is not new hair loss; it is the shedding of hair that effectively died three months ago. The medication is simply flushing out the debris to make room for the new growth.
This phase is temporary; usually lasting 4 to 6 weeks. If you stop the medication now; you stop the new growth. You must ride the wave. Visualizing the new hairs pushing out the old ones can help reframe this frightening experience as a positive sign of regeneration.
Synthetic vs. Natural Desiccated Thyroid (NDT)
Some patients do not respond well to T4-only medications like Synthroid or Levothyroxine. T4 is a storage hormone; it is inactive until the body converts it into T3. This conversion happens primarily in the liver and gut. If your liver is sluggish or your gut is inflamed; you may not convert T4 efficiently.
Since the hair follicle receptors specifically rely on T3; these patients may continue to experience thinning hair despite normal TSH. Their blood has plenty of storage hormone (T4); but their cells are starving for active hormone (T3). This is called “cellular hypothyroidism.”
In these cases; switching to Natural Desiccated Thyroid (like Armour or NP Thyroid) or adding a synthetic T3 (Cytomel) can be a game-changer for thyroid hair regrowth. NDT contains both T4 and T3. The direct availability of T3 stimulates the anagen phase more effectively in poor converters. It bypasses the conversion bottleneck.
The Nutritional Pillars of Regrowth (Beyond Hormones)
You cannot build a house without bricks; and you cannot grow hair with just hormones. You need raw materials. In my practice; I rarely see a thyroid patient who does not also have nutritional deficiencies. The most significant of these is iron.
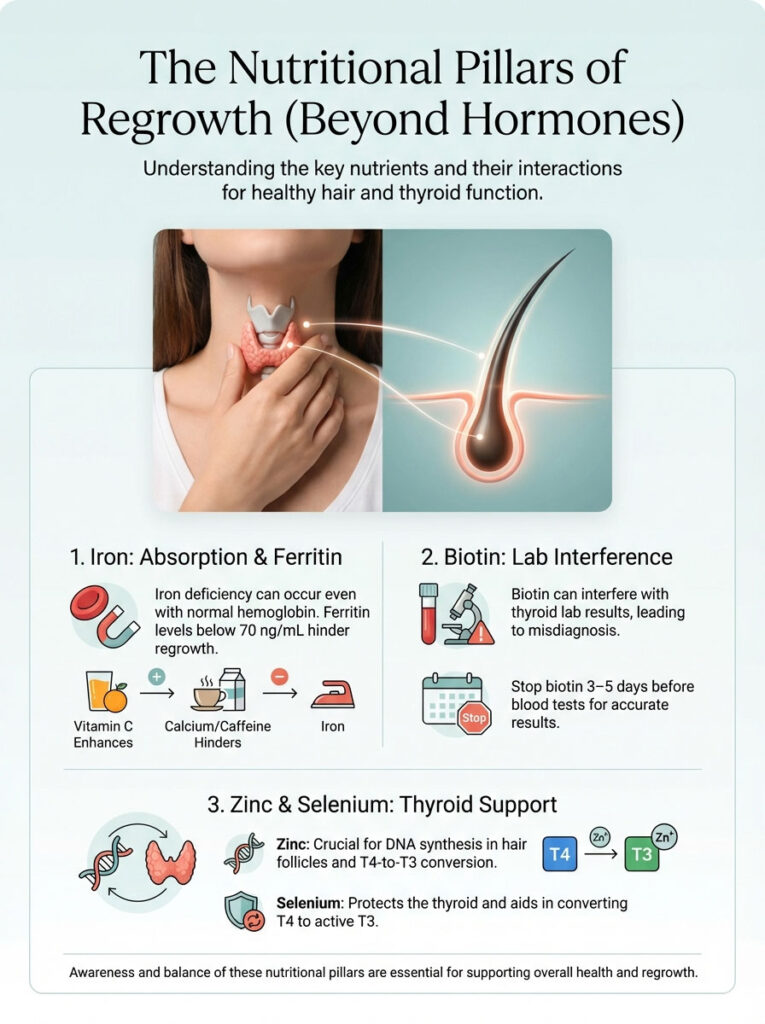
The thyroid gland and the hair follicle compete for resources. If nutrients are scarce; the thyroid gland (being an endocrine organ) usually wins; or the body pulls from the “luxury” items like hair to support the blood. We must flood the body with enough nutrients to satisfy the essential organs and have plenty left over for the hair.
The Critical Role of Ferritin (Iron Storage)
Ferritin is a protein that stores iron. You can have normal hemoglobin (meaning you are not anemic) but still have dangerously low ferritin. This is “Iron Deficiency without Anemia.” The body views hair as non-essential. If your ferritin drops below a certain threshold; the body pulls stored iron from the hair follicles to support red blood cell production.
Research and clinical observation suggest that while a ferritin level of 15-20 ng/mL is considered “normal” by labs; a level of at least 70 ng/mL is required for hair regrowth. If your ferritin is 30; your doctor might say you are fine; but your hair will continue to shed. The follicle suffocates without iron.
Raising ferritin is a slow process. It can take 6 months of supplementation to move from 30 to 70. Iron should always be taken with Vitamin C (like a glass of orange juice) to increase absorption. It should be taken away from thyroid medication; coffee; and dairy; as calcium and caffeine block iron absorption.
The Biotin Warning (Patient Safety)
We must discuss biotin and thyroid labs. Biotin (Vitamin B7) is famous for hair growth; and many patients take high doses (5,000 to 10,000 mcg). While biotin is great for strengthening the keratin infrastructure of the hair; it poses a diagnostic danger.
Biotin interferes with the immunoassay technology used to measure TSH; T3; and T4. It does not change your actual thyroid levels; but it changes what the lab machine reads. It can make your TSH look falsely low and your T4 look falsely high. This pattern mimics Graves’ disease (hyperthyroidism).
Crucial Medical Advice: You do not need to stop taking biotin permanently; but you MUST stop taking it 3 to 5 days before any thyroid blood draw. Failing to do so can lead to a misdiagnosis and an incorrect change in your medication dose.
Zinc and Selenium: The Conversion Catalysts
These two minerals are the catalysts for your thyroid function. Zinc is vital for DNA synthesis within the hair follicle. It is also a key player in the enzyme that converts T4 to T3. A zinc deficiency can lead to hair shedding that looks exactly like thyroid hair loss.
Selenium protects the thyroid gland from oxidative damage. The production of thyroid hormone generates hydrogen peroxide as a byproduct. Selenium acts as an antioxidant to neutralize this; preventing damage to the gland. More importantly; it is the “key” that unlocks the enzyme for T4 to T3 conversion. Without selenium; your medication may build up in your blood as T4 without ever becoming the active T3 your hair needs.
| Nutrient | Role in Hair/Thyroid Health | Target Level (Consult Doctor) | Food Sources |
|---|---|---|---|
| Ferritin | Stores iron; essential for hair cell protein production. | > 70 ng/mL | Red meat; liver; spinach; lentils. |
| Zinc | Vital for DNA synthesis and T4-to-T3 conversion. | Top half of reference range. | Oysters; pumpkin seeds; beef. |
| Selenium | Protects thyroid from oxidative damage; aids conversion. | Mid-range (toxicity is possible). | Brazil nuts (1-2 per day); sardines. |
| Vitamin D | Regulates hair follicle cycling. | 50–80 ng/mL | Sunlight; fatty fish; fortified dairy. |
| Biotin | Strengthens keratin infrastructure. | Adequate intake (Caution with labs). | Eggs; almonds; cauliflower. |
Autoimmunity: Hashimoto’s and Alopecia Areata
For 90% of hypothyroid patients in the USA; the cause is Hashimoto’s Thyroiditis. This is an autoimmune disease. Your immune system is attacking your thyroid gland. Unfortunately; autoimmune diseases tend to travel in packs. There is a documented link between Hashimoto’s thyroiditis hair loss and Alopecia Areata.
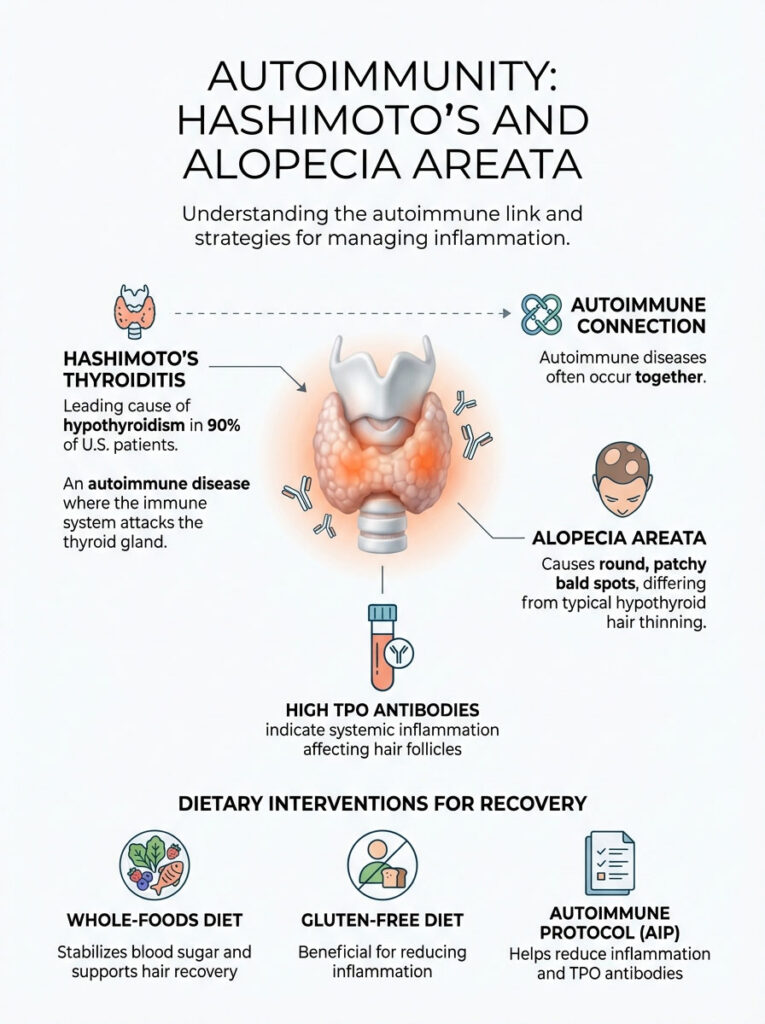
Alopecia Areata causes round; coin-sized patchy bald spots. It is different from the diffuse thinning of standard hypothyroidism. In this condition; the immune system mistakenly attacks the hair follicle directly. If you have Hashimoto’s; you are at a statistically higher risk for this secondary autoimmune condition.
Reducing Inflammation through Diet
If you have high TPO antibodies (Thyroid Peroxidase Antibodies); you have systemic inflammation. This inflammation can attack the hair follicles directly via cytokines. To stop the shedding; we must calm the immune system. This often involves dietary interventions.
The Autoimmune Protocol (AIP) or a strict Gluten-Free diet has shown promise in reducing TPO antibodies. The molecular structure of gliadin (the protein in gluten) mimics the structure of thyroid tissue. When you eat gluten; your body creates antibodies to attack it. Due to molecular mimicry; these antibodies also attack your thyroid. By removing the trigger; inflammation subsides; and the hair follicle environment improves.
Sugar and processed foods also drive inflammation. Insulin resistance is common in hypothyroid patients. High insulin levels can increase androgens (male hormones); which can further miniaturize hair follicles. Adopting a whole-foods diet that stabilizes blood sugar is a foundational step for hair recovery.
Practical Regrowth Strategies (The “What To Do” Guide)
While we wait for your hormones and ferritin levels to optimize; we need a strategy to protect the hair you have and stimulate the follicles manually. We cannot just sit and wait for the blood work to improve. We need proactive measures.
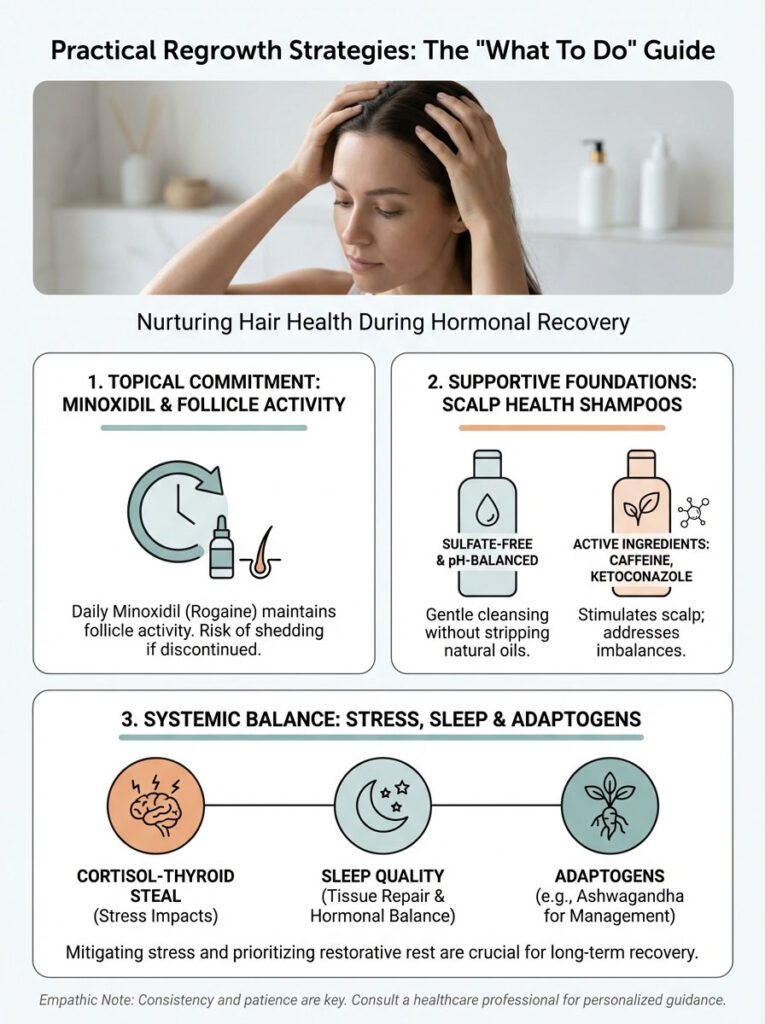
Topical Treatments and Scalp Care
Patients often ask if they can use Minoxidil (Rogaine). The answer is yes. It acts as a bridge. Minoxidil is a vasodilator; it widens blood vessels around the follicle; forcing more oxygen and nutrients to the hair root. It does not fix the thyroid issue; but it keeps the follicle active while we fix the internal chemistry.
However; there is a caveat. Minoxidil requires commitment. Once you start; you must use it daily. If you stop; any hair that was preserved by the medication will shed. It is a tool to buy time and maintain density during the recovery phase. It is particularly useful if the hair loss has been going on for years.
Your shampoo choice matters significantly. Thyroid hair is fragile and brittle. Sulfates found in cheap shampoos strip natural oils; leading to breakage. You need to switch to a sulfate-free; pH-balanced shampoo. Ingredients like caffeine and ketoconazole can also support scalp health by reducing local inflammation and stimulating blood flow.
Stress Management: The Cortisol Steal
This is not just “relax.” It is biochemistry. Cortisol (the stress hormone) and thyroid hormones compete. High cortisol inhibits the conversion of T4 to T3. It also increases the production of Reverse T3; an inactive hormone that blocks thyroid receptors. This is known as the “Cortisol-Thyroid Steal.”
When you are chronically stressed; your body diverts raw materials away from thyroid production to make more cortisol. This perpetuates the hair loss cycle. Prioritizing sleep is non-negotiable. Sleep is when the body repairs tissues and balances hormones. Adaptogens like Ashwagandha can help lower cortisol; but always check with your doctor; as Ashwagandha can stimulate thyroid hormone production and may interact with medication.
The Timeline: Managing Expectations
Hair growth is a lesson in delayed gratification. The hair you see on your head is dead tissue; the living action happens below the surface. We operate on the 6-Month Rule. You must mentally prepare for a marathon; not a sprint.
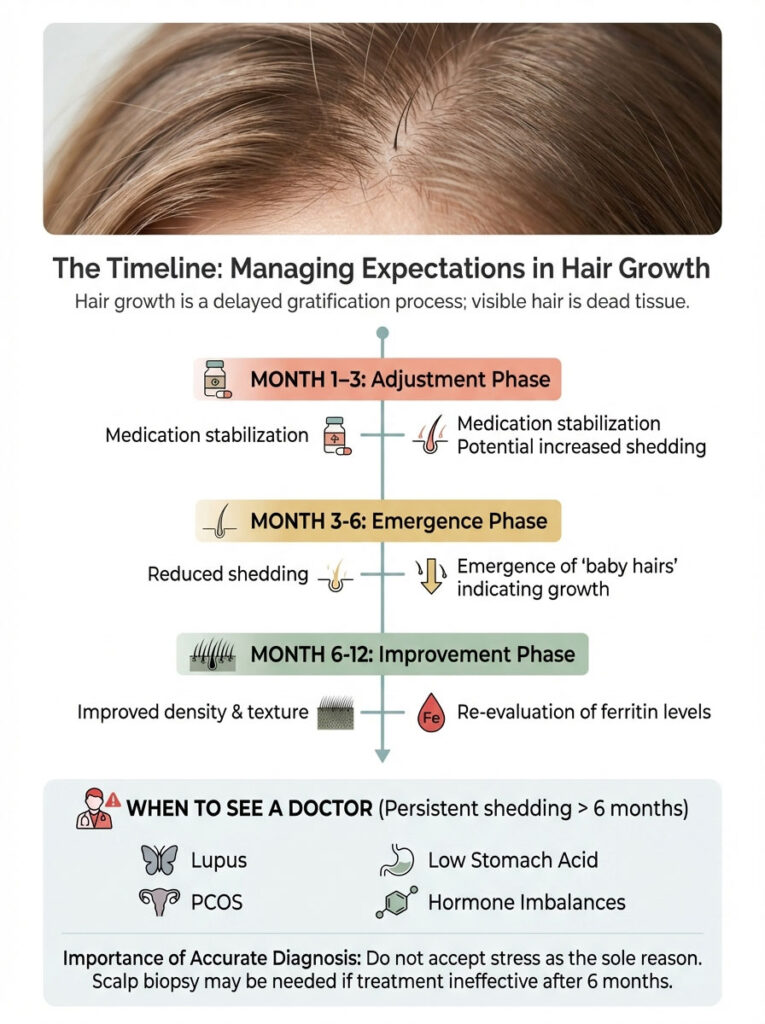
Month 1-3: This is the adjustment phase. We adjust medication and supplements. TSH stabilizes. Shedding may continue or even peak due to the “medication paradox” mentioned earlier. This is the hardest phase psychologically. You are doing everything right; but the mirror says otherwise. Trust the process.
Month 3-6: Shedding slows down significantly. You will notice less hair in the shower drain and on your brush. If you look closely at your hairline; you may see “baby hairs” that stick up uncontrollably. These are often lighter in color and finer than your other hair. Celebrate them.
Month 6-12: Density improves. The texture begins to return to normal; becoming softer and less brittle. The ponytail starts to feel thicker. The outer third of the eyebrows begins to fill in. At this stage; we re-evaluate ferritin levels to ensure they are holding steady above 70 ng/mL.
When to See the Doctor Again
If shedding persists after 6 months of optimal TSH levels (0.5-2.5 mIU/L) and optimal ferritin (>70 ng/mL); we must investigate further. Other culprits could be at play. Lupus; PCOS (Polycystic Ovary Syndrome); low stomach acid (hypochlorhydria); or sex hormone imbalances (estrogen dominance) are common comorbidities.
Do not accept “it’s just stress” if the data suggests otherwise. If the treatment isn’t working after half a year; the diagnosis may be incomplete. You may need a scalp biopsy to rule out scarring alopecia; although this is rare in thyroid cases.
Summary & Key Takeaways
Thyroid hair loss is a symptom; not a permanent state. It is your body’s way of waving a red flag; telling you that cellular energy is low and resources are scarce. The good news is that the body is forgiving. Once we restore the balance of T3; T4; and essential nutrients; the biological imperative to grow hair returns.
- It is Reversible: The follicle is dormant; not dead. Regrowth is the expected outcome of proper treatment.
- Check Your Ferritin: Normal is not optimal. Aim for ferritin levels above 70 ng/mL to support hair growth.
- Optimize TSH: Don’t settle for “in range.” Aim for a TSH between 0.5 and 2.5 mIU/L.
- Expect the Shed: Starting medication may cause temporary shedding. This is a sign of metabolic acceleration and future growth.
- Be Patient: The hair cycle is slow. Give your treatment plan at least 6 months before judging the results.
Don’t settle for “normal” lab results if you still feel symptoms. Advocate for full thyroid panels; check your iron storage; and be patient with your body as it heals. Aim for “optimal,” and you will see your hair and your vitality return.
Frequently Asked Questions
Will my hair grow back after thyroid treatment?
Yes, thyroid-related alopecia is typically non-scarring, meaning the follicles remain viable but have simply entered a dormant state. Once we stabilize your T3 and T4 levels and address underlying nutrient gaps like iron deficiency, the follicles re-enter the anagen phase, leading to a restoration of density.
How long does it take to see visible hair regrowth after stabilizing thyroid levels?
Because of the natural hair growth cycle, there is a significant lag time of about 3 to 6 months before you see visible results. You may first notice a decrease in daily shedding and the appearance of fine “baby hairs” at the hairline before the overall volume of your ponytail feels restored.
Why is my hair falling out more after starting Levothyroxine or Synthroid?
This medication paradox occurs because the sudden surge in metabolic energy wakes up follicles that were stuck in the resting phase. The new growth pushes out old, dead hair shafts simultaneously; this is a temporary but positive sign that your cellular metabolism is accelerating and the treatment is working.
What TSH level is considered optimal for hair growth?
While standard lab ranges are broad, I typically aim for an optimal TSH range between 0.5 and 2.5 mIU/L for patients struggling with hair loss. The hair follicle is highly sensitive to metabolic shifts, and many patients find regrowth only occurs when levels are tightly regulated within this narrow window rather than just being “in range.”
How does ferritin impact thyroid-related hair thinning?
Ferritin is your body’s iron storage, and hair follicles require significant iron to maintain the rapid cellular division of the growth phase. Clinical data suggests that while “normal” labs start at 15 ng/mL, you generally need a ferritin level of at least 70 ng/mL to stop shedding and trigger robust regrowth in thyroid patients.
Why do I need to stop taking biotin before my thyroid blood work?
Biotin interferes with the lab’s testing technology, often causing a falsely low TSH and falsely high T4 reading that mimics hyperthyroidism. To ensure your medication dose is adjusted based on accurate data, you must discontinue biotin supplements at least 3 to 5 days before any thyroid panel.
Can switching to Natural Desiccated Thyroid (NDT) improve hair density?
For patients who are “poor converters”—those whose bodies struggle to turn T4 into active T3—switching to NDT or adding Cytomel can be a game-changer. Since hair follicles rely specifically on T3 for energy, providing this active hormone directly often succeeds where T4-only medications like Levothyroxine fail.
What is the Sign of Hertoghe and how does it relate to hypothyroidism?
The Sign of Hertoghe is the thinning or complete loss of the outer third of the eyebrows, a classic clinical marker of an underactive thyroid. If you notice this sign, it often indicates that your cellular thyroid levels are not yet optimized, even if your TSH appears within the standard reference range on your lab report.
How can I distinguish between thyroid hair loss and genetic balding?
Thyroid hair loss, or Telogen Effluvium, is diffuse, meaning you will notice thinning evenly across the entire scalp, including the sides and back. In contrast, genetic balding follows specific patterns like a receding hairline or a widening part, and usually leaves the eyebrows and the density of the back of the head unaffected.
Does Hashimoto’s disease cause different hair loss patterns than standard hypothyroidism?
While Hashimoto’s causes diffuse thinning due to low hormones, it is also an autoimmune condition that increases your risk for Alopecia Areata. This can result in distinct, coin-sized bald patches where the immune system directly attacks the follicle, requiring an anti-inflammatory approach to treatment alongside hormone replacement.
Which specific nutrients are required to support thyroid hair follicle recovery?
Beyond iron, your follicles require zinc and selenium to catalyze the conversion of T4 to active T3 and protect the gland from oxidative stress. Vitamin D is also critical, as it regulates the cycling of the hair follicle; I recommend aiming for levels between 50 and 80 ng/mL for the best results.
Is it safe to use topical treatments like Minoxidil for thyroid-related thinning?
Yes, Minoxidil can serve as a helpful bridge by increasing blood flow and nutrient delivery to the follicles while we work on balancing your internal hormones. It doesn’t treat the root cause, but it can help maintain hair density and stimulate growth during the several months it takes for thyroid medication to take full effect.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Thyroid conditions and hair loss can be complex and may be linked to various underlying health issues. Always consult a qualified healthcare professional or endocrinologist before starting new medications, changing your dosage, or beginning a supplement regimen.
References
- American Thyroid Association (ATA) – https://www.thyroid.org – Provides clinical guidelines on the systemic effects of hypothyroidism and hyperthyroidism on integumentary health.
- Journal of Clinical Endocrinology & Metabolism – Oxford Academic – Research regarding the impact of T3 and T4 hormones on human hair follicle stem cell activation.
- National Institutes of Health (NIH) – https://ods.od.nih.gov/factsheets/Iron-HealthProfessional/ – Authoritative data on ferritin levels and their role in non-scarring alopecia.
- British Journal of Dermatology – https://onlinelibrary.wiley.com/journal/13652133 – Clinical studies defining the relationship between telogen effluvium and endocrine dysfunction.
- Mayo Clinic – https://www.mayoclinic.org – Comprehensive overview of Hashimoto’s thyroiditis and its autoimmune comorbidities including alopecia.
- U.S. Food and Drug Administration (FDA) – Safety communication regarding biotin interference with thyroid-stimulating hormone (TSH) immunoassays.








