Your skin acts as a massive diagnostic window into your internal metabolic health. Before blood tests ever confirm a diagnosis, you likely noticed that your reflection had changed. Perhaps your face looks swollen despite a clean diet. Maybe your legs are insatiably itchy regardless of how much high-end lotion you apply. In my practice, I frequently see patients dismissed by other providers who label these symptoms as merely cosmetic or age-related issues. They are incorrect.
Table of Contents
Thyroid Skin Problems: How to Fix Itching and Puffiness?
is not just a question of vanity; it is a critical question of endocrine physiology. When your thyroid downregulates, it disrupts the epidermal barrier function and fundamentally alters the structure of your dermis.
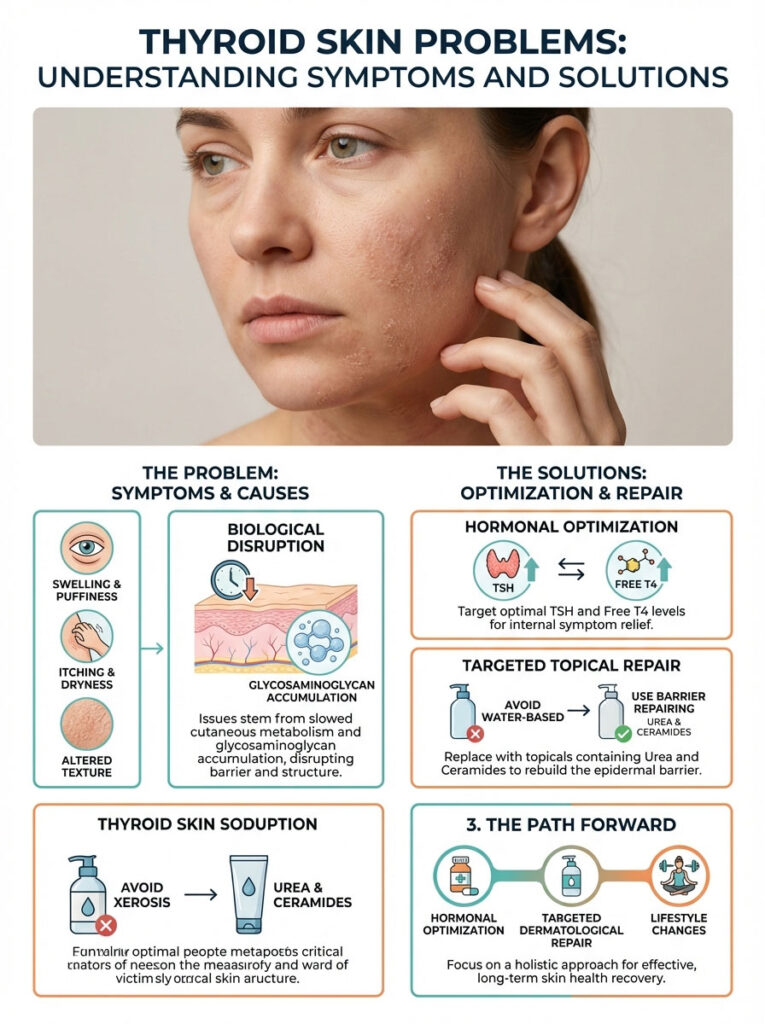
Quick Answer: Thyroid skin issues stem from a slowdown in cutaneous metabolism and the accumulation of sugar-protein chains called glycosaminoglycans. To fix itching and puffiness, you must first optimize TSH and Free T4 levels through medication. Simultaneously, replace standard water-based lotions with barrier-repairing topicals containing Urea and Ceramides to physically reconstruct the skin’s lipid layer.
I understand the deep frustration of feeling uncomfortable in your own skin. This guide provides a comprehensive medical explanation of myxedema (puffiness) and the biochemistry of xerosis (itching). We will move far beyond generic advice. We will look at how to medically manage these symptoms through hormonal optimization, targeted dermatological repair, and lifestyle changes.
Key Statistics: Thyroid & Skin Health
- 70-80% of hypothyroid patients report cutaneous changes before diagnosis.
- Sebum (oil) secretion can decrease by over 50% in hypothyroid states.
- Skin turnover slows significantly; it takes longer than the standard 28 days to renew.
- 30% of patients with autoimmune thyroid disease also suffer from chronic hives (urticaria).
- Visible reduction in myxedema typically takes 3 to 6 weeks after achieving euthyroid status.
- 40% of patients experience reduced sweating (hypohidrosis), leading to severe dryness.
The Physiology of the “Thyroid Face”: Understanding Myxedema
Many patients ask me why their face looks swollen. This is particularly noticeable in the morning. This is not simple water retention caused by a salty meal. In the world of endocrinology, we call this specific condition thyroid puffiness / Myxedema. To treat it, you must understand what is happening beneath the surface.
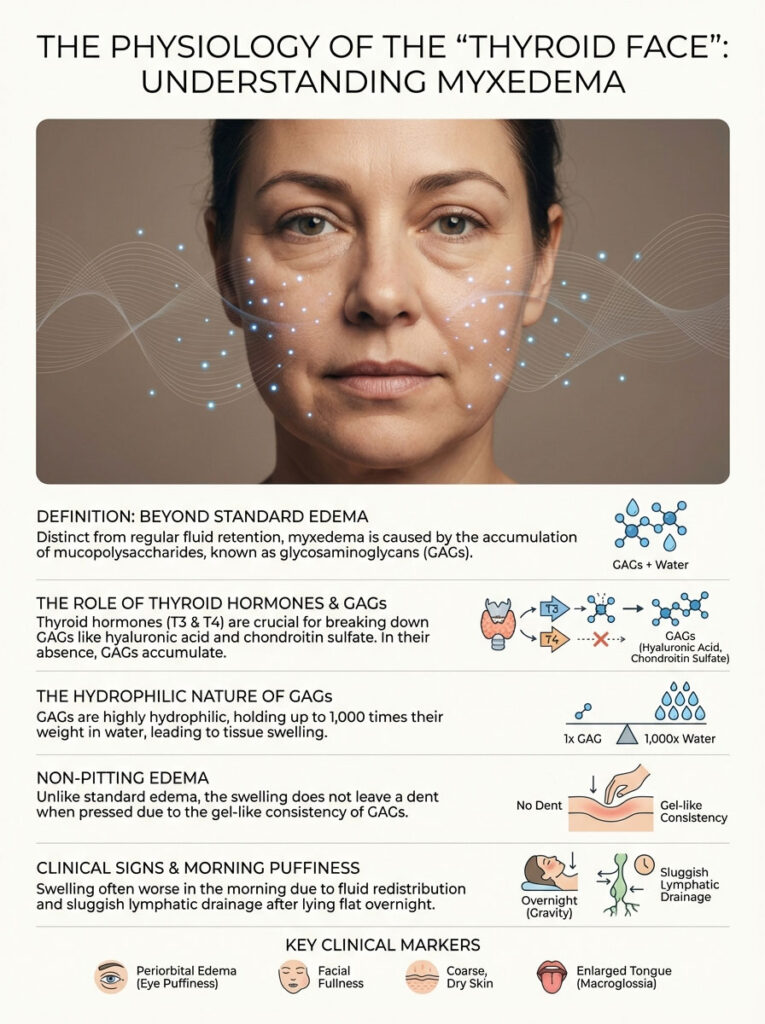
Defining Myxedema and Mucopolysaccharides
Unlike standard edema, which is usually just water, myxedema involves the accumulation of mucopolysaccharides. These are specifically glycosaminoglycans (GAGs) like hyaluronic acid and chondroitin sulfate. In a healthy body, fibroblasts constantly produce and break down these GAGs. However, thyroid hormones (T3 and T4) are required to stimulate the breakdown process. When you are hypothyroid, your body produces GAGs but cannot degrade them. They accumulate in the dermis. This is the thick layer of skin beneath the surface.
The Biochemistry of Puffiness
Here is the biochemical reality. GAGs are extremely hydrophilic. This means they love water. They can hold up to 1,000 times their weight in water. As these sugar chains build up in your skin, they trap fluid in a gel-like matrix. This creates what we call non-pitting edema. If you press your finger into a swollen ankle caused by heart failure, it leaves a dent (pit). If you press into thyroid puffiness / Myxedema, it usually does not pit. The fluid is bound within that gel matrix. This is why diuretics (water pills) often fail to fix the “thyroid face.” The problem isn’t just fluid; it is the structures holding the fluid.
Clinical Signs of Facial Myxedema
In clinical exams, I look for specific markers of this condition. You can check for these in the mirror:
- Periorbital Edema: This is distinct swelling specifically around the eyelids. The tissue here is loose. This allows GAGs to accumulate easily. It leads to a “heavy” look around the eyes.
- Broadening of Features: Patients often report their nose looks wider. Some say their lips feel thicker. This is the dermal thickening at work.
- Macroglossia: This refers to the swelling of the tongue. You might notice teeth indentations on the sides of your tongue when you wake up. This is critical. A swollen tongue can obstruct your airway during sleep. This contributes to sleep apnea. Sleep apnea further stresses the thyroid.
Why Morning Puffiness is Worse
You might notice the swelling is most severe when you wake up. During the day, gravity helps drain fluid from the face. When you lie flat at night, fluid redistributes. In a healthy person, the lymphatic system drains this. In a hypothyroid person, the lymphatic system is sluggish. The GAGs in the face grab this fluid and hold it. This results in that “doughy” morning appearance.
The Mechanism of the Itch: Thyroid-Induced Xerosis
While puffiness is distressing, hypothyroidism itching can be maddening. I have had patients scratch until they bleed. The sensation is deep and persistent. This is not just “dry skin.” It is a metabolic failure of the skin’s hydration system.
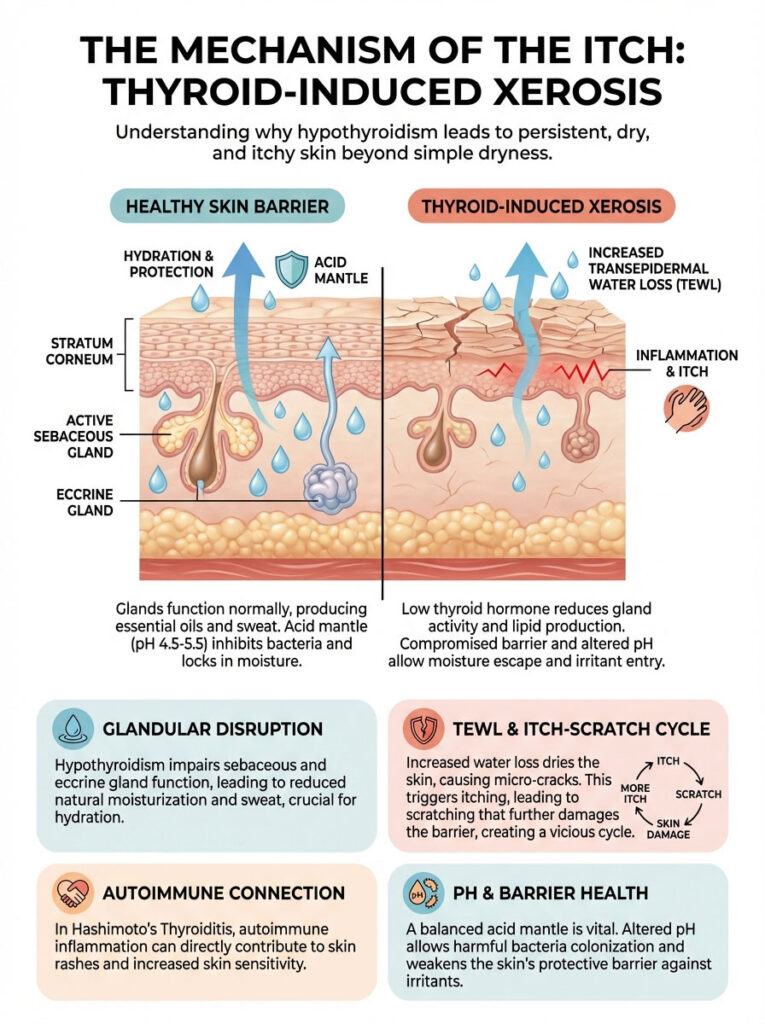
Sebaceous and Eccrine Gland Dysfunction
Your skin relies on two types of glands to stay soft. These are sebaceous glands (oil) and eccrine glands (sweat). Thyroid hormones directly regulate the secretion rates of these glands. Research indicates that in hypothyroid states, lipid secretion can drop significantly. Without this lipid layer, your skin loses its seal. Furthermore, hypohidrosis (a lack of sweating) is common. While sweating less might sound appealing, sweat contains urea and lactate. These are natural moisturizing factors that keep skin hydrated. Without them, the skin becomes brittle.
Transepidermal Water Loss (TEWL)
When the lipid barrier fails, we see a spike in Transepidermal Water Loss (TEWL). This means water from the deeper layers of your skin evaporates into the air. This happens because the surface oil barrier is missing. As the skin dries out, the stratum corneum (the outer layer) develops microscopic cracks. These micro-fissures expose nerve endings to the air. They also expose nerves to environmental irritants. This triggers the itch-scratch cycle. Standard lotions often fail here. They add moisture but do not repair the barrier that keeps the moisture in.
The Autoimmune Connection (Hashimoto’s and Hives)
If you have Hashimoto’s Thyroiditis, your itching might be more than just dryness. There is a strong link between high anti-TPO antibodies and Hashimoto’s rash. This is technically known as Chronic Spontaneous Urticaria (CSU). This is an immune response where the body releases histamine in the skin. This causes hives or welts. If your itch moves around or comes with red welts, it is likely autoimmune-driven. This is distinct from simple xerosis.
The Role of pH and the Acid Mantle
Healthy skin is slightly acidic. It has a pH around 5.5. This is called the “acid mantle.” This acidity protects against bacteria and keeps the barrier intact. Hypothyroidism can alter sweat production. This disrupts the pH balance. When the pH rises (becomes more alkaline), enzymes that control skin shedding stop working. Dead skin cells pile up. This leads to that rough, scaly texture. It also invites bacteria like Staph aureus to colonize. This makes the itching even worse.
Comparative Analysis: Is it Thyroid or Just Dry Skin?
It is vital to distinguish between environmental dryness and metabolic dryness. Environmental dryness is like winter itch. Metabolic dryness is caused by thyroid skin problems. The treatment protocols differ significantly.
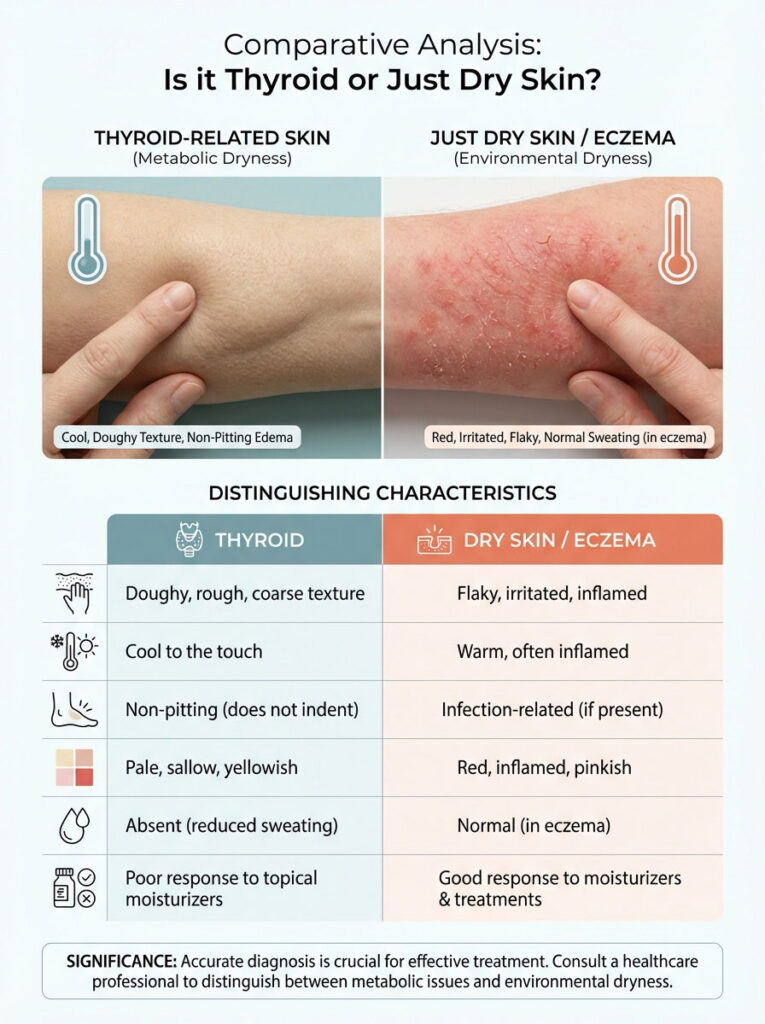
Distinguishing Clinical Features
Thyroid skin has a specific texture. I often describe it as “doughy” due to the underlying myxedema. Yet the surface feels rough and scaly. It is also typically cool to the touch. This is due to reduced blood flow (vasoconstriction). Eczema or allergic dermatitis is often warm and inflamed.
| Feature | Thyroid-Induced Skin Issues | Standard Dry Skin / Eczema |
|---|---|---|
| Primary Cause | Systemic metabolic slowdown; GAG accumulation | Environmental factors; localized inflammation |
| Texture | Doughy, cool to touch, coarse, scaly | Rough, often warm if inflamed, flaky |
| Edema (Swelling) | Non-pitting (Myxedema); facial puffiness | Usually absent unless infection is present |
| Color | Pale, sallow, or yellow-orange (Carotenemia) | Red, pink, or irritated |
| Sweating | Absent or significantly reduced (Hypohidrosis) | Normal or increased in flexural areas |
| Response to Lotion | Poor; requires barrier repair + hormone therapy | Good; responds well to standard moisturizers |
The “Pale Skin Thyroid” Phenomenon: Color Changes Explained
Beyond texture, patients often notice a change in their complexion. You might feel you look “washed out” or sickly. This is directly related to thyroid skin problems affecting blood flow and vitamin metabolism.
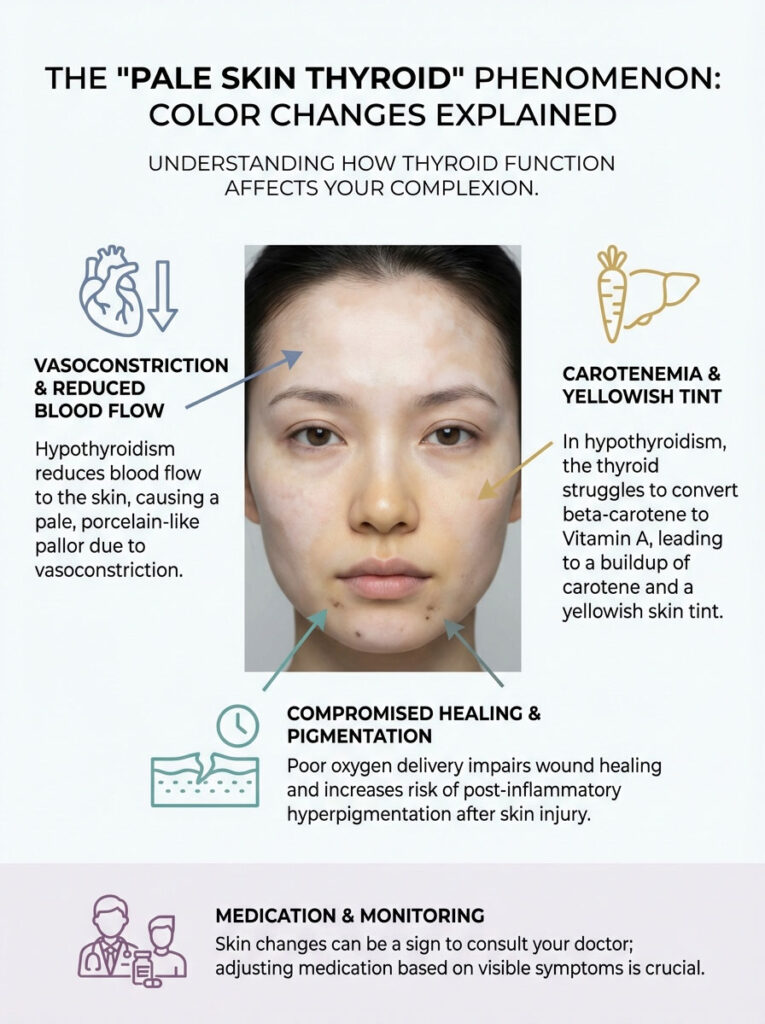
Vasoconstriction and Pallor
Thyroid hormones regulate body temperature. When you are hypothyroid, your basal metabolic rate drops. You feel cold. To conserve heat for vital organs, the body constricts the blood vessels in the skin. This is called cutaneous vasoconstriction. This diverts blood away from the surface. It leads to a ghostly, porcelain-like pallor. This is not anemia. Though anemia can coexist, this is a physiological heat-saving mechanism.
Carotenemia (The Yellow Tint)
Have you noticed a yellowish tint on your palms? Or maybe on the soles of your feet? Perhaps in the smile lines around your nose? This is called Carotenemia. The thyroid is responsible for converting dietary beta-carotene into Vitamin A. You get beta-carotene from carrots and sweet potatoes. When the thyroid is sluggish, this conversion fails. Carotene accumulates in the stratum corneum. It stains the skin yellow. It is harmless but serves as a clear visual marker. It suggests your medication dosage may need adjustment.
Poor Wound Healing
Because blood flow is reduced, oxygen delivery drops. Cell turnover is also slow. Scratches, acne lesions, or bug bites take much longer to heal. The delivery of oxygen and nutrients to the skin surface is compromised. This leaves marks that linger for weeks. We call this “post-inflammatory hyperpigmentation.” In thyroid patients, these dark spots fade much slower than in healthy individuals.
Medical Management: Fixing the Root Cause
Let me be clear. No amount of expensive cream will permanently fix thyroid puffiness / Myxedema. It will not cure hypothyroidism itching if your internal chemistry is off. Topical treatments are supportive. Hormonal correction is curative.
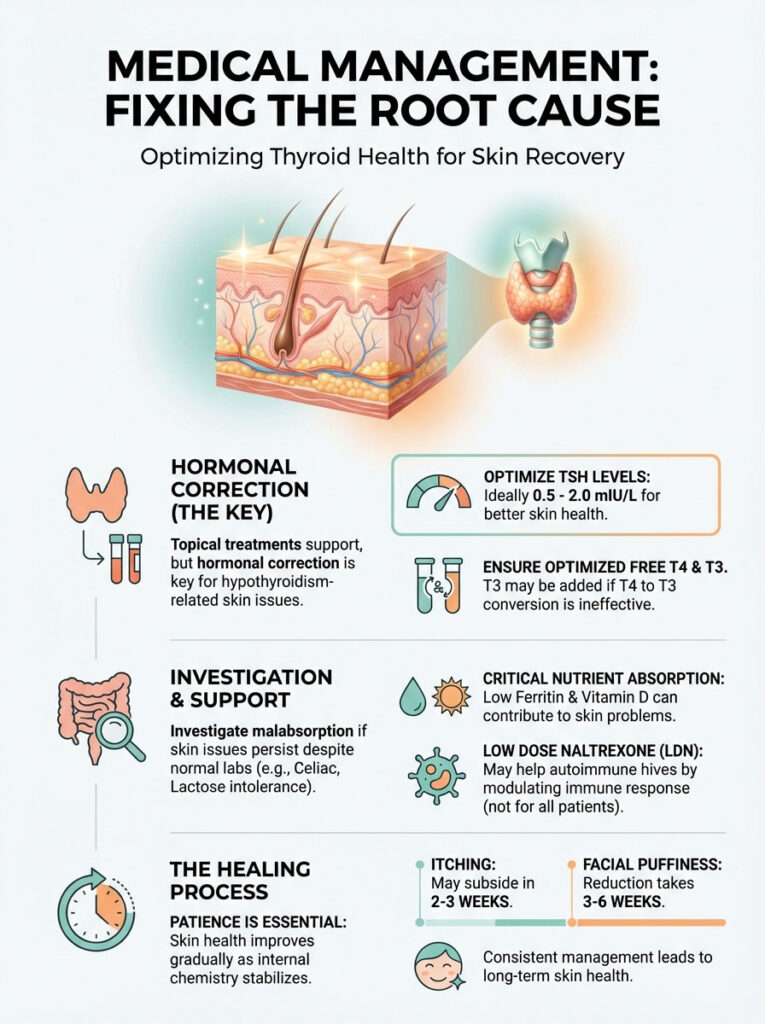
Optimizing TSH and Free T4
The standard of care typically involves Levothyroxine (T4). However, simply being in the “normal” range for TSH is often insufficient for skin health. Many patients report persistent skin issues until their TSH is in the lower half of the reference range. This is often 0.5 to 2.0 mIU/L. Their Free T4 must also be optimized. In some cases, the body cannot convert T4 to the active T3 hormone effectively. The addition of Liothyronine (T3) can significantly accelerate the reduction of thyroid puffiness / Myxedema. T3 directly stimulates fibroblast activity to break down GAGs.
The Timeline of Recovery
Patience is required. In a healthy adult, the epidermis replaces itself every 28 days. In a hypothyroid patient, this cycle is delayed. Once we achieve a euthyroid state, you should expect the hypothyroidism itching to subside first. This usually happens within 2 to 3 weeks. Structural changes take longer. The reduction of facial puffiness typically takes 3 to 6 weeks or more. The body slowly metabolizes the accumulated mucopolysaccharides.
When to Suspect Malabsorption
If your labs look perfect but your skin is still a disaster, we must investigate malabsorption. Conditions like Celiac disease are common comorbidities with Hashimoto’s. Lactose intolerance is also frequent. If you aren’t absorbing nutrients, your skin is starving. This happens regardless of your thyroid medication. We often check ferritin and Vitamin D levels to confirm this.
Low Dose Naltrexone (LDN)
For patients with autoimmune hives or severe inflammation, we sometimes consider Low Dose Naltrexone. LDN modulates the immune system. It can reduce the inflammatory cytokines that drive the itch response. It is not a standard treatment for everyone. However, for those with high antibodies and skin involvement, it can be a game-changer.
Advanced Topical Strategies: Repairing the Barrier
While we wait for the hormones to work, we need a dry skin thyroid remedy that actually functions. Standard water-based lotions evaporate too quickly on thyroid skin. There is no oil barrier to hold them in.
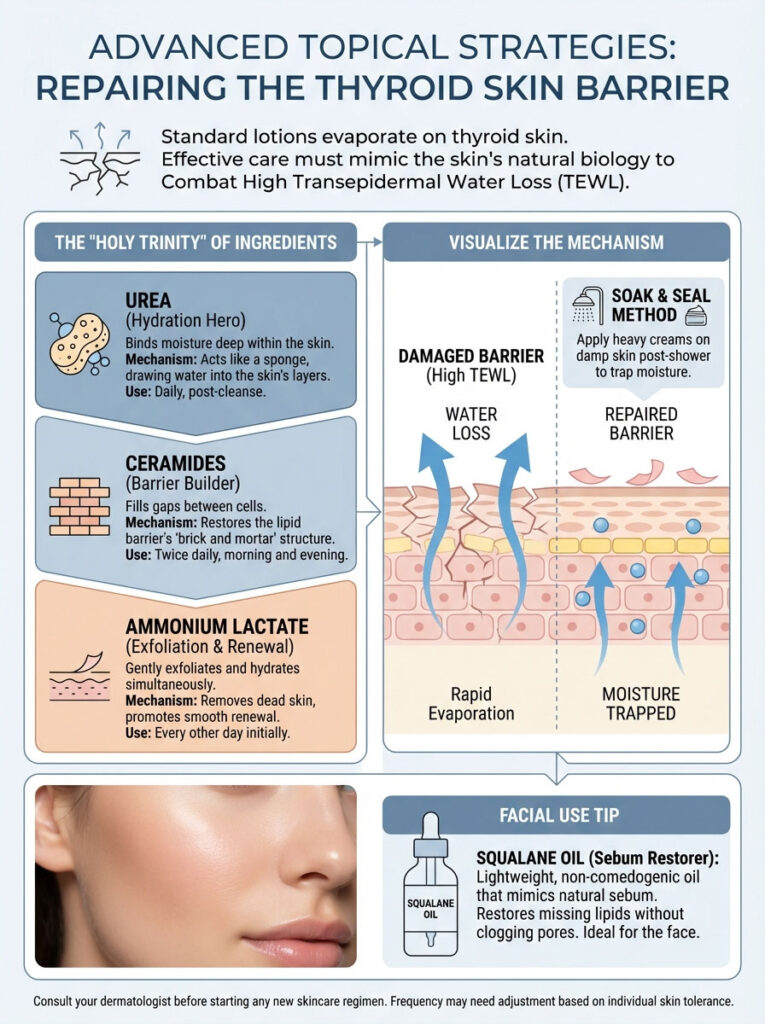
Why Standard Lotions Fail
Most commercial lotions are mostly water. When you apply them to skin with high TEWL, the water evaporates. Sometimes it draws even more moisture out of the skin with it. You need ingredients that mimic the skin’s natural biology. You need to replace the missing oils.
The “Holy Trinity” of Hypothyroid Skincare
To combat the specific pathology of thyroid skin, I recommend three key ingredients:
- Urea (10-20%): Urea is a keratolytic. This means it dissolves the glue holding dead skin cells together. It fixes that scaly texture. More importantly, it is a humectant. It binds water deep in the skin. It can penetrate the thick, doughy layer of thyroid skin better than almost anything else.
- Ceramides: Think of your skin cells as bricks. Think of lipids as the mortar. Hypothyroidism destroys the mortar. Ceramides replace it. They physically rebuild the barrier. Look for products that list ceramides NP, AP, and EOP.
- Lactic Acid/Alpha Hydroxy Acids: Since your cell turnover is sluggish, these gentle acids help. They stimulate the skin to shed dead cells. They encourage the production of new ones. Lactic acid is also a humectant, so it hydrates while it exfoliates.
Expert Insight: Do not apply moisturizer to dry skin. Apply your heavy cream or ointment within 3 minutes of getting out of the shower. Do this while your skin is still damp. This traps the water on your body before it evaporates. We call this the “Soak and Seal” method.
| Ingredient | Mechanism of Action | Best For | Frequency of Use |
|---|---|---|---|
| Urea (10-20%) | Dissolves keratin bonds; binds water | Thick, alligator-like skin; heels and elbows | Daily (Evening) |
| Ceramides | Replenishes lipid bilayer | General itching; facial dryness | Twice Daily |
| Ammonium Lactate | Exfoliates dead surface cells | “Muddy” complexion; scaly legs | Every other day |
| Hyaluronic Acid | Draws moisture to epidermis | Facial dehydration (use with occlusive) | Morning (under sunscreen) |
| Petrolatum | Occlusive seal | Locking in moisture after bathing | Immediately post-shower |
The Role of Squalane
I also frequently recommend Squalane oil. Note the “a” in the spelling. Squalene is a natural oil produced by our skin. Squalane is the shelf-stable version. Because thyroid patients produce less sebum, applying Squalane is like giving the skin back exactly what it is missing. It is lightweight, non-comedogenic (won’t clog pores), and mimics human sebum perfectly. It is excellent for facial use where heavier creams might cause breakouts.
Step-by-Step Daily Skincare Routine
Implementing a structured routine is key. You cannot treat thyroid skin sporadically. Here is a protocol I often suggest to patients dealing with thyroid skin problems.

Morning Routine: Protection and Hydration
- Gentle Cleanse: Do not use foaming cleansers. They strip oil. Use a creamy, non-foaming hydrating cleanser.
- Vitamin C Serum: This helps with the dullness and pigmentation. It provides antioxidant protection against environmental stress.
- Hyaluronic Acid: Apply to damp skin to pull moisture in.
- Ceramide Moisturizer: Seal the hydration in with a lipid-rich cream.
- Sunscreen: Thyroid skin heals slowly. UV damage makes it worse. Use a mineral SPF 30 or higher.
Evening Routine: Repair and Exfoliate
- Oil Cleanse: If you wear makeup, start with an oil balm. This removes dirt without harsh scrubbing.
- Treatment (Alternate Nights):
- Night A: Use a chemical exfoliant like Lactic Acid (5-10%). This helps shed the dead skin cells that make you look dull.
- Night B: Use a Retinol product. Retinol is Vitamin A. Since your body lacks it, topical application helps speed up cell turnover. Start slowly to avoid irritation.
- Heavy Moisturizer: Use a thicker cream at night. Look for ingredients like Shea Butter or Colloidal Oatmeal.
- Occlusive Layer (Slugging): If you are very dry, apply a thin layer of petrolatum (Vaseline) over your face. This creates a greenhouse effect. It forces moisture into the skin while you sleep.
Lifestyle and Dietary Interventions
Managing thyroid skin problems requires a holistic approach. We must support the body’s ability to maintain fluid balance and skin integrity from the inside out.
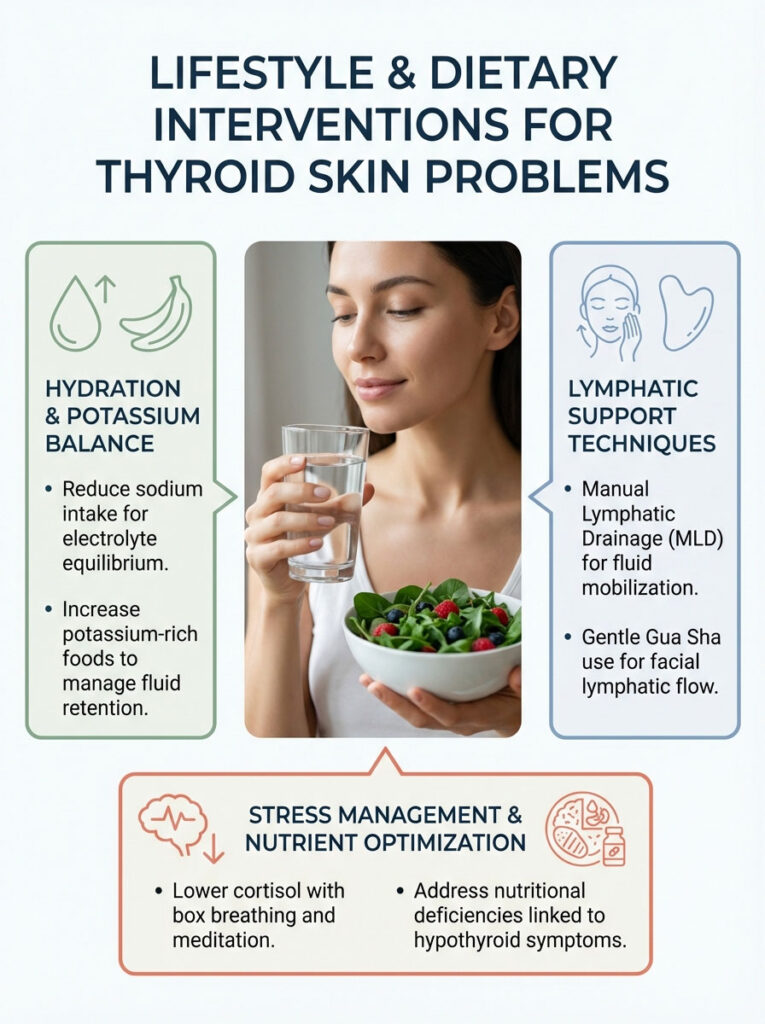
Hydration Strategies for Myxedema
There is a common myth that drinking gallons of water will flush out puffiness. In the context of thyroid puffiness / Myxedema, this is not entirely true. Because the GAGs are holding onto water, simply adding more water can sometimes increase the feeling of bloating. This happens if electrolyte balance is off. The strategy here is hydration with electrolyte management. Reducing sodium intake is critical. Sodium binds to the GAGs. This worsens fluid retention. Focus on potassium-rich foods like avocados and sweet potatoes. Potassium helps balance sodium levels and encourages fluid excretion.
Critical Nutrients for Skin Health
Nutritional deficiencies often mimic or exacerbate hypothyroid symptoms. We need to address these specifically.
- Zinc: This mineral is essential for skin integrity and wound healing. It is also required for the conversion of T4 to T3. A deficiency here hits you twice. You get poor skin repair and lower active thyroid hormone. I often recommend 30mg of Zinc Picolinate daily with food.
- Vitamin A (Retinol): As mentioned, your body struggles to convert carrots into Vitamin A. Therefore, consuming preformed Vitamin A is necessary. You find this in liver, eggs, and dairy. You can also use Cod Liver Oil. This prevents thyroid skin problems like follicular hyperkeratosis (bumpy skin).
- Selenium: Research suggests selenium supplementation can reduce anti-TPO antibodies. This may alleviate the severity of Hashimoto’s rash. Brazil nuts are a famous source, but a standardized supplement of 200mcg is often more reliable.
- Omega-3 Fatty Acids: These combat systemic inflammation. They help improve the lipid composition of the skin barrier. High-dose fish oil (2-3 grams daily) can help lubricate the skin from within.
- Collagen Peptides: While not a cure, hydrolyzed collagen provides the amino acids glycine and proline. These are the building blocks of skin. Since your fibroblast activity is low, giving them easy-to-use building blocks can support dermal thickness.
Lymphatic Drainage and Massage
Since the fluid in myxedema is trapped in a gel matrix, mechanical stimulation can help. Manual lymphatic drainage (MLD) is very effective. Using a gua sha tool on the face can also help. The goal is to mobilize stagnant fluid toward the lymph nodes. While it doesn’t remove the GAGs, it can temporarily reduce the severity of the morning puffiness. Do this gently. The skin is fragile. Use an oil to prevent dragging the skin.
The Impact of Stress on Skin
Stress raises cortisol. High cortisol suppresses thyroid function further. It also degrades collagen. This creates a vicious cycle. We call this the “Brain-Skin Axis.” Techniques like box breathing or meditation are not just for mental health. They are physiological tools to lower cortisol. This allows the thyroid to function better and the skin to repair itself.
The Connection Between Gut Health and Skin
You cannot talk about thyroid skin without talking about the gut. The “Gut-Skin Axis” is well documented. In autoimmune thyroid disease, the gut barrier is often compromised. This is sometimes called “leaky gut.”
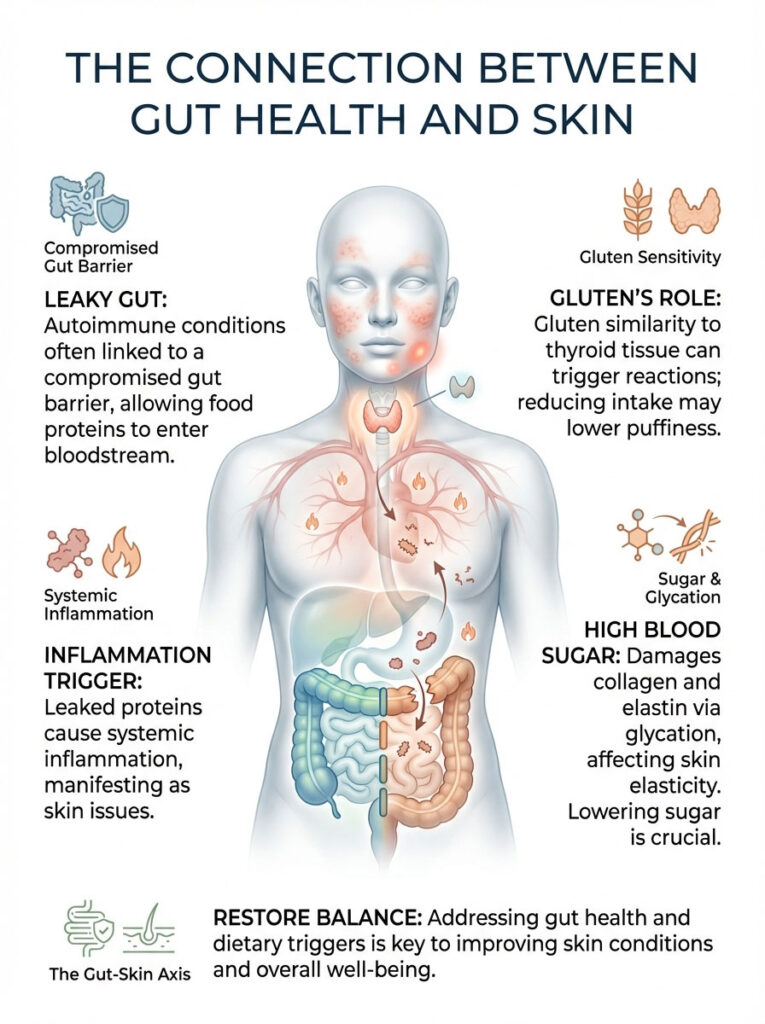
Food Sensitivities and Inflammation
When the gut is permeable, food proteins escape into the bloodstream. The immune system attacks them. This creates systemic inflammation. This inflammation often manifests in the skin as eczema, hives, or general puffiness. Gluten is the most common culprit. The protein structure of gluten (gliadin) resembles thyroid tissue. This leads to molecular mimicry. Many of my patients see a dramatic reduction in thyroid puffiness / Myxedema within 30 days of going strictly gluten-free.
The Role of Sugar and Glycation
High blood sugar is damaging to the skin. It leads to a process called glycation. Sugar binds to proteins in the skin (collagen and elastin). It forms Advanced Glycation End-products (AGEs). These AGEs make the skin stiff and prone to cracking. Hypothyroidism slows down glucose metabolism. This makes you more susceptible to blood sugar spikes. Reducing refined sugar is essential for restoring skin elasticity.
Case Studies and Clinical Data
To illustrate how these treatments work in the real world, let’s look at two typical cases from my experience. These stories highlight the timeline and the multi-modal approach required.
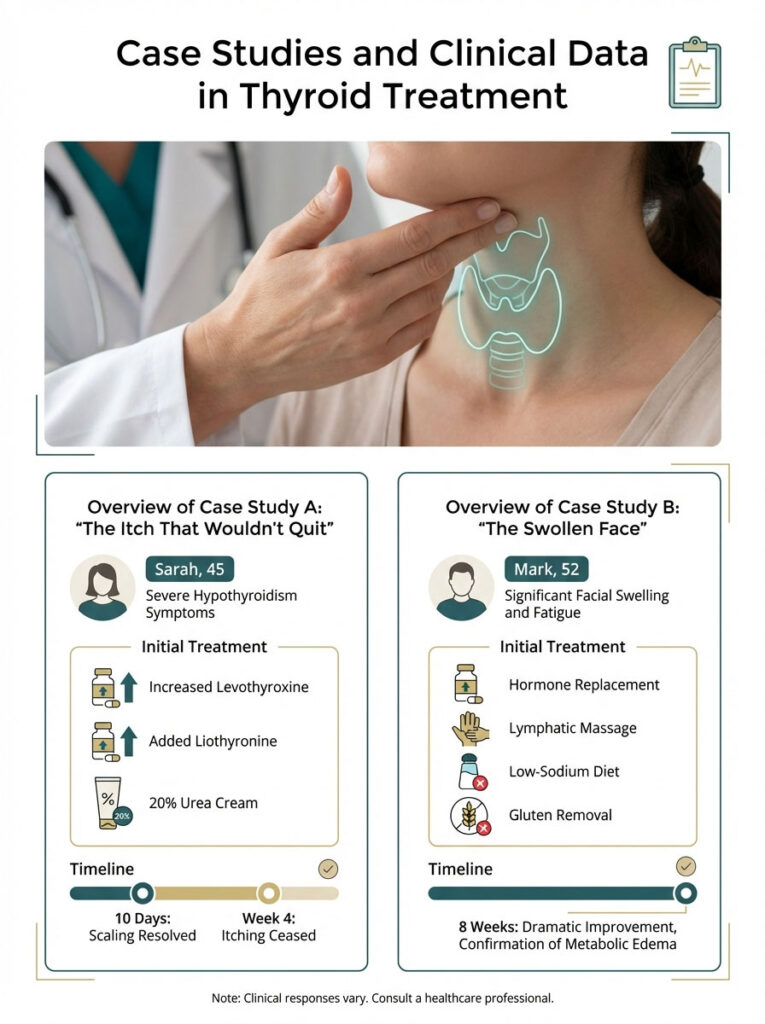
Case Study A: “The Itch That Wouldn’t Quit”
Sarah, a 45-year-old female, presented with severe hypothyroidism itching on her shins and forearms. She had been using standard drugstore lotions with no relief. Her legs were covered in excoriations (scratch marks). Her TSH was 3.5 mIU/L. This is technically “normal” but not optimal for someone with symptoms. Her Free T3 was at the very bottom of the range.
The Protocol: We increased her Levothyroxine slightly to suppress TSH below 2.0. We added a small dose of Liothyronine (T3). Simultaneously, I started her on a 20% Urea cream regime. I instructed her to apply it to damp skin every evening.
The Result: Within 10 days, the scaling resolved. The urea dissolved the thick dead skin. By week 4, the itching had ceased completely. Her barrier function was restored. She no longer felt the need to scratch.
Case Study B: “The Swollen Face”
Mark, 52, came in with significant facial swelling and fatigue. He was undiagnosed. His face showed classic thyroid puffiness / Myxedema signs. He had periorbital edema and a thickened nose. He looked different than he did in photos from two years prior. We initiated hormone replacement therapy immediately.
The Protocol: I advised him that the “swelling” was structural. It would take time to move. We utilized lymphatic massage and a low-sodium diet as adjunct therapies. We also focused on gut health, removing gluten to lower systemic inflammation.
The Result: Photos taken 8 weeks later showed a dramatic sharpening of his jawline. There was a significant reduction in eyelid swelling. This confirmed that the edema was indeed metabolic. It took nearly two months, but the “mask” was lifted.
Common Pitfalls in Treatment
Even with good intentions, many patients make mistakes that delay healing. Here are the most common errors I see.
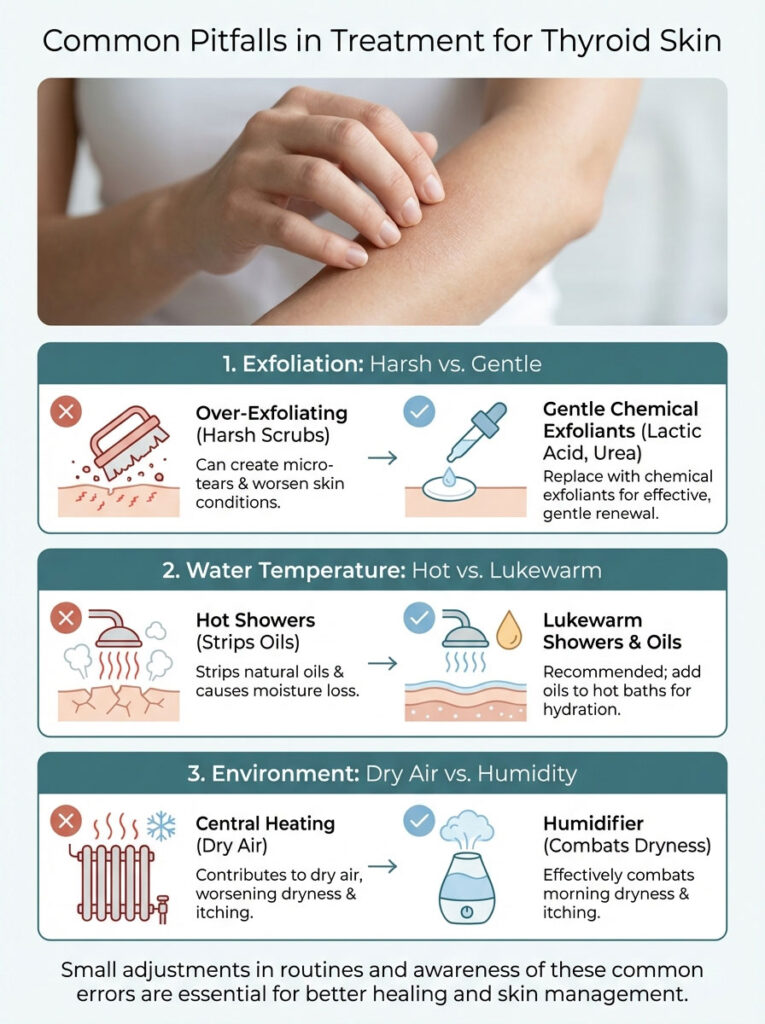
Over-Exfoliating
When skin feels rough, the instinct is to scrub it. Patients use harsh physical scrubs (like apricot scrubs). This is a mistake. Thyroid skin is thin and fragile. Scrubbing creates micro-tears. It increases water loss. It worsens the itch. Stick to chemical exfoliants like lactic acid or urea. They are much gentler and more effective.
Hot Showers
Hypothyroid patients are often cold. They love long, scalding hot showers. Unfortunately, hot water strips the natural oils from the skin. It causes immediate vasodilation followed by rapid moisture loss. You must shower in lukewarm water. If you must take a hot bath, add oil to the water. Limit the time to 10 minutes.
Ignoring Humidity
Central heating in the winter destroys thyroid skin. If the air in your home is dry, your skin will lose water to the air. Sleeping with a humidifier next to your bed is one of the simplest, most effective interventions for morning dryness and itching.
When to See a Dermatologist
While most thyroid skin problems can be managed with the strategies above, some symptoms require a specialist. You should seek a referral if:

- Nodules or Lumps: Pretibial myxedema (thickening on the shins) can sometimes look like distinct lumps. This requires evaluation to rule out other conditions.
- Persistent Hives: If hives last more than 6 weeks, it is considered chronic. You may need prescription antihistamines or biologics like Xolair.
- Hair Loss with Scarring: If you notice smooth, shiny patches on your scalp where hair has fallen out, this could be scarring alopecia. This is another autoimmune condition that needs immediate steroid treatment to prevent permanent loss.
- Yellowing of the Eyes: As discussed, yellow skin is likely Carotenemia. However, if the whites of your eyes turn yellow, that is jaundice. That indicates liver issues and is a medical emergency.
Questions to Ask Your Doctor
Advocating for yourself is crucial. When you visit your endocrinologist or primary care provider, bring specific questions regarding your skin symptoms.

- “My skin is not improving despite normal TSH. Can we check my Free T3 and Reverse T3 to see if I am converting hormones properly?”
- “Could I have a nutrient deficiency like Zinc or Vitamin A that is hindering my skin repair?”
- “Is my facial puffiness related to my sodium intake, or is it a sign that my medication dosage is too low?”
- “Should we screen for Celiac disease given my persistent skin inflammation?”
Summary & Key Takeaways
Dealing with thyroid skin problems can be emotionally draining. It affects how you look and how you feel. But it is important to remember that these symptoms are reversible. The itching and puffiness you experience are biochemical consequences. They result from low thyroid hormone, the accumulation of glycosaminoglycans, and the reduction of sebum.
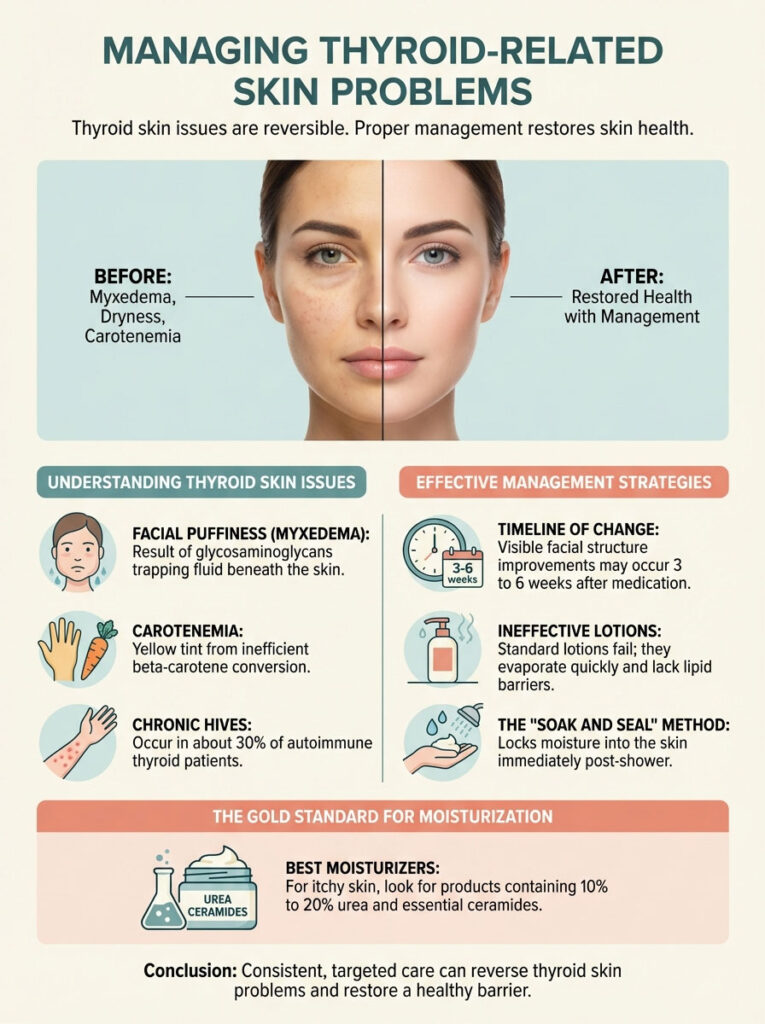
- Root Cause: It is not just dry skin. It is a metabolic breakdown of the skin barrier and a buildup of mucopolysaccharides.
- Primary Fix: Medication adjustment (Levothyroxine/Liothyronine) is non-negotiable. You must achieve a true euthyroid state, not just a “normal” TSH.
- Topical Fix: Stop using watery lotions. Switch to products with Urea and Ceramides. These artificially repair the barrier while meds kick in.
- Dietary Support: Focus on Zinc, Vitamin A, and Omega-3s. Consider removing gluten to lower autoimmune inflammation.
- Patience: Give your body 3 to 6 weeks to remodel the skin structure. The itch will go away before the puffiness does.
With proper management, the “thyroid face” and the relentless itch can be resolved. You do not have to live with uncomfortable skin. By treating the internal metabolism and supporting the external barrier, you can restore your skin’s health and your confidence.
Frequently Asked Questions
Why does my face look swollen in the morning with hypothyroidism?
Morning facial puffiness, or myxedema, occurs because glycosaminoglycans (GAGs) like hyaluronic acid accumulate in the dermis and trap fluid in a gel-like matrix. Because your lymphatic system is more sluggish overnight and gravity is not assisting drainage while you lie flat, this “doughy” swelling is most prominent upon waking.
What is the best moisturizer for thyroid-related itchy skin?
For hypothyroid xerosis, you need a barrier-repairing formula containing at least 10% to 20% urea and essential ceramides. Urea acts as a keratolytic to smooth scaly texture and bind water deep in the skin, while ceramides replace the missing “mortar” in your skin\’s lipid barrier to prevent transepidermal water loss.
How long does it take for thyroid puffiness to go away after starting medication?
Once you achieve a euthyroid state—ideally with an optimized TSH between 0.5 and 2.0 mIU/L—you can expect visible changes in facial structure within 3 to 6 weeks. While itching often subsides within the first 14 days of hormonal optimization, structural remodeling of the dermis to clear accumulated mucopolysaccharides takes longer.
Can hypothyroidism cause a yellow tint on the palms and face?
Yes, this is a condition called carotenemia, which happens when a sluggish thyroid cannot efficiently convert dietary beta-carotene into Vitamin A. This results in a harmless yellowish-orange tint in the stratum corneum, particularly visible on the palms, soles, and the smile lines around the nose.
Why do standard lotions fail to stop hypothyroidism itching?
Most commercial lotions are water-based and evaporate quickly, often drawing more moisture out of the skin in the process. Because hypothyroidism significantly reduces sebum (oil) and sweat secretion, your skin lacks the natural lipid barrier necessary to lock in moisture, requiring medical-grade humectants and occlusives instead.
What is the difference between thyroid myxedema and regular water retention?
Regular edema is typically “pitting,” meaning it leaves a temporary indentation when pressed, and is often caused by salt intake or circulation issues. Thyroid myxedema is “non-pitting” because the fluid is bound within a thick matrix of sugar-protein chains, making it resistant to diuretics and standard water-reduction strategies.
Does Hashimoto’s cause chronic hives or skin rashes?
Approximately 30% of patients with autoimmune thyroid disease suffer from Chronic Spontaneous Urticaria, often referred to as a Hashimoto’s rash. This occurs when high anti-TPO antibodies trigger a systemic immune response, leading to the release of histamine and the formation of itchy red welts that move around the body.
How does Low Dose Naltrexone help with thyroid-related skin inflammation?
Low Dose Naltrexone (LDN) works by modulating the immune system and reducing the production of inflammatory cytokines that drive the itch-scratch cycle. For patients with autoimmune-driven skin issues, LDN can help stabilize the immune response and alleviate chronic hives when traditional antihistamines and topical steroids fail.
Should I go gluten-free to help with thyroid skin problems?
Many patients see a significant reduction in systemic inflammation and facial puffiness by adopting a strictly gluten-free diet. This is due to molecular mimicry, where the body confuses gluten proteins with thyroid tissue, potentially exacerbating the autoimmune attacks that lead to skin manifestations like eczema and myxedema.
What are the most important vitamins for repairing the thyroid skin barrier?
Zinc is critical for dermal wound healing and T4 to T3 conversion, while preformed Vitamin A is necessary since hypothyroid patients struggle to convert beta-carotene. Additionally, high-dose Omega-3 fatty acids help lubricate the skin from within by improving the lipid composition of the epidermal barrier and reducing inflammation.
What is the “soak and seal” method for hypothyroid skin?
The “soak and seal” method involves applying a heavy, lipid-rich cream or ointment within three minutes of exiting a lukewarm shower while the skin is still damp. This technique physically traps moisture into the stratum corneum before it can evaporate, which is essential for patients with high transepidermal water loss (TEWL).
Can a swollen tongue be a sign of a thyroid disorder?
Yes, macroglossia, or a swollen tongue, is a clinical sign of severe hypothyroidism and myxedema. If you notice teeth indentations on the sides of your tongue (scalloping), it indicates that the same glycosaminoglycan buildup affecting your skin is also impacting your internal tissues, which can contribute to sleep apnea.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Thyroid skin problems are often symptoms of complex endocrine imbalances. Always consult with a qualified healthcare professional or endocrinologist before changing your medication, starting new supplements, or implementing intensive skincare regimens, especially if you have underlying health conditions.
References
- American Thyroid Association – https://www.thyroid.org – Comprehensive clinical guidelines on the systemic effects of hypothyroidism on integumentary health.
- Journal of Clinical Endocrinology & Metabolism – “Cutaneous Manifestations of Thyroid Disease” – A peer-reviewed study detailing the accumulation of glycosaminoglycans in dermal tissue.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – https://www.niddk.nih.gov – Official data regarding the metabolic slowdown associated with low T3 and T4 levels.
- DermNet NZ – “Thyroid Disease and the Skin” – An authoritative dermatological resource explaining the mechanisms of xerosis and myxedema.
- British Journal of Dermatology – “The role of thyroid hormones in skin physiology” – Research findings on how thyroid hormones regulate sebum production and epidermal turnover.
- Thyroid Federation International – Statistical data on patient-reported cutaneous symptoms prior to clinical diagnosis of hypothyroidism.








