Hypothyroidism & Depression are biologically linked through the availability of thyroid hormones in the brain. Low levels of Triiodothyronine (T3) slow down neuronal metabolism. This reduces the sensitivity of serotonin and dopamine receptors. It creates a state of “organic mood syndrome” where psychiatric symptoms are driven by a metabolic deficiency rather than a primary chemical imbalance. Correcting the hormonal deficit is often required before antidepressants can work effectively.
Table of Contents
You take your medication faithfully every morning. You attend therapy sessions every week. You practice sleep hygiene and force yourself to exercise. Yet, the heaviness remains. For millions of Americans, the diagnosis of Major Depressive Disorder (MDD) tells only half the story. The missing piece of the puzzle often lies in the delicate, often overlooked relationship between Hypothyroidism & Depression.
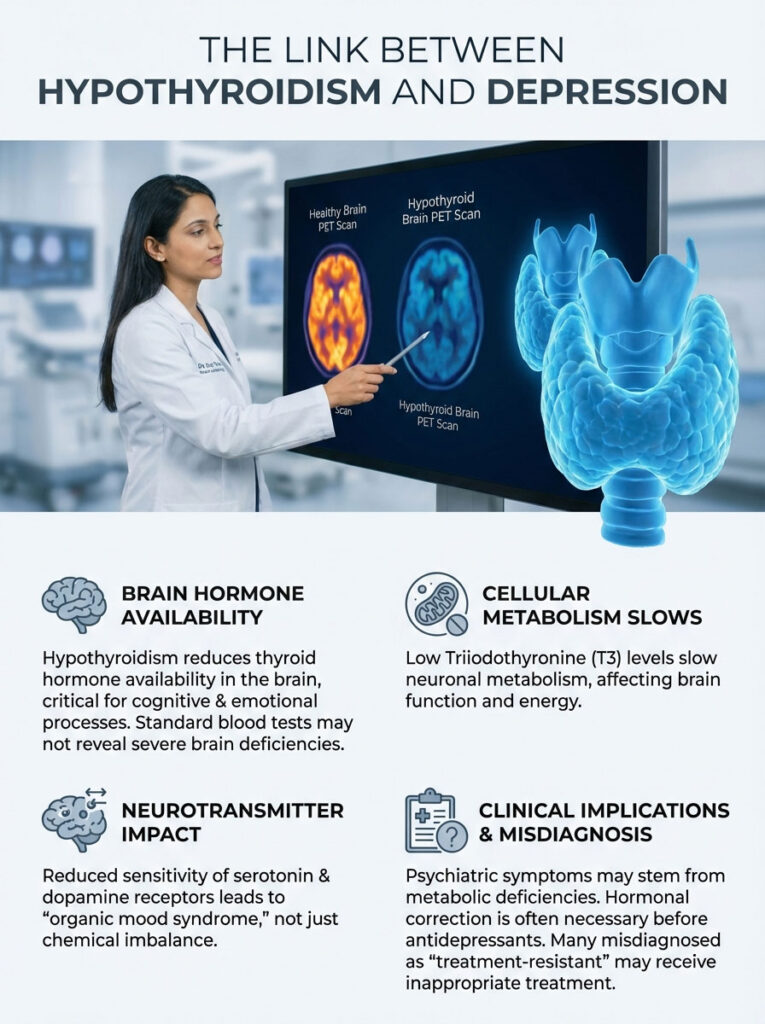
In my clinical practice as a neuro-endocrinologist, I frequently treat patients who have been labeled “treatment-resistant.” They are not resistant to treatment. They are simply receiving the wrong treatment for the wrong system. When the thyroid gland fails to produce adequate hormones, the brain suffers.
More importantly, when those hormones fail to reach the brain cells, the result is a profound slowing of cognitive and emotional processes. This article examines the biological mechanisms that link thyroid function to mental health. We will look beyond standard blood tests to understand why “normal” results might mask a severe brain-hormone deficiency.
Key Statistics: The Thyroid-Mood Link
- 60% of patients with hypothyroidism present with some degree of depression or anxiety.
- 30% of patients with “treatment-resistant” depression have subclinical hypothyroidism.
- 50% reduction in serotonin receptor sensitivity can occur in the absence of adequate T3.
- 1 in 8 women will develop a thyroid disorder during her lifetime. This often overlaps with perimenopause or postpartum periods.
- 20% of depression patients may carry the DIO2 gene mutation. This impairs T4-to-T3 conversion specifically in the brain.
The Biological Link Between Hypothyroidism & Depression
To understand thyroid mental health, we must look at the Hypothalamic-Pituitary-Thyroid (HPT) axis. This feedback loop regulates metabolism. However, its role in brain function is paramount. Most patients understand that the thyroid controls energy. Few realize it controls the speed of thought.
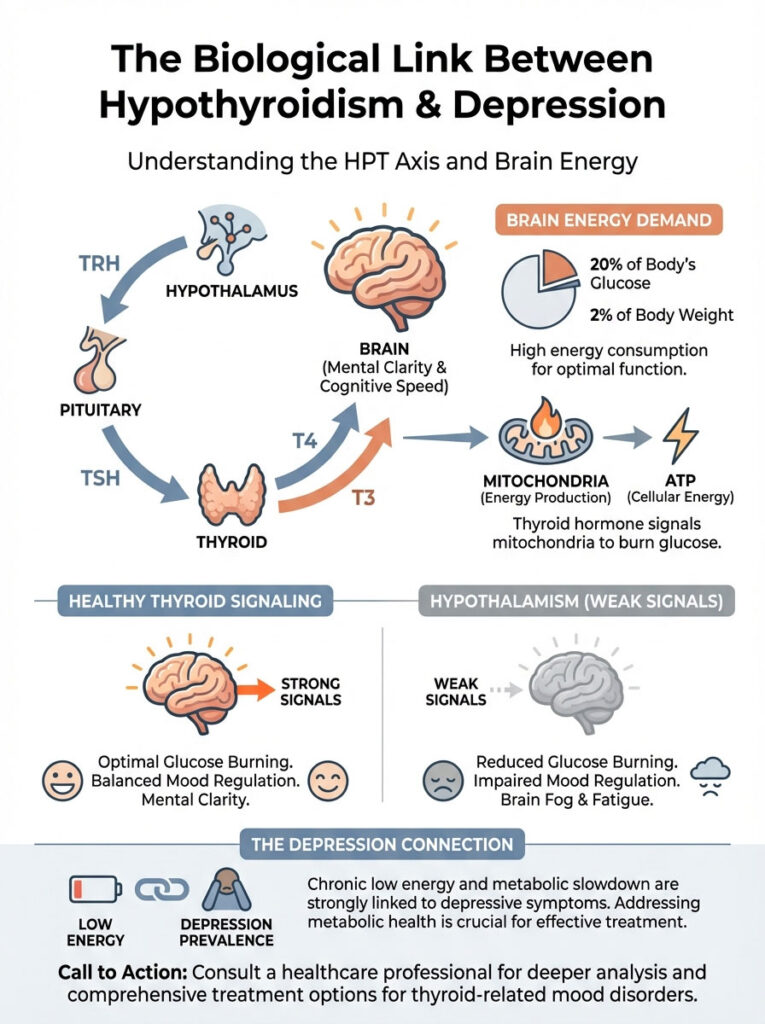
The brain is a voracious consumer of energy. It represents only 2% of body weight but consumes 20% of the body’s glucose. Thyroid hormone is the signal that tells mitochondria to burn that glucose. When the signal is weak, the lights in the brain effectively dim.
This creates a biological environment where depression thrives. It is not just about feeling sad. It is about a cellular inability to sustain the energy required for mood regulation. We must treat the metabolic root to fix the psychiatric symptom.
The Neuro-Endocrinology of the HPT Axis
The HPT axis is a complex communication network. It ensures your brain has enough fuel to function. When this network is disrupted, Hypothyroidism & Depression symptoms emerge.
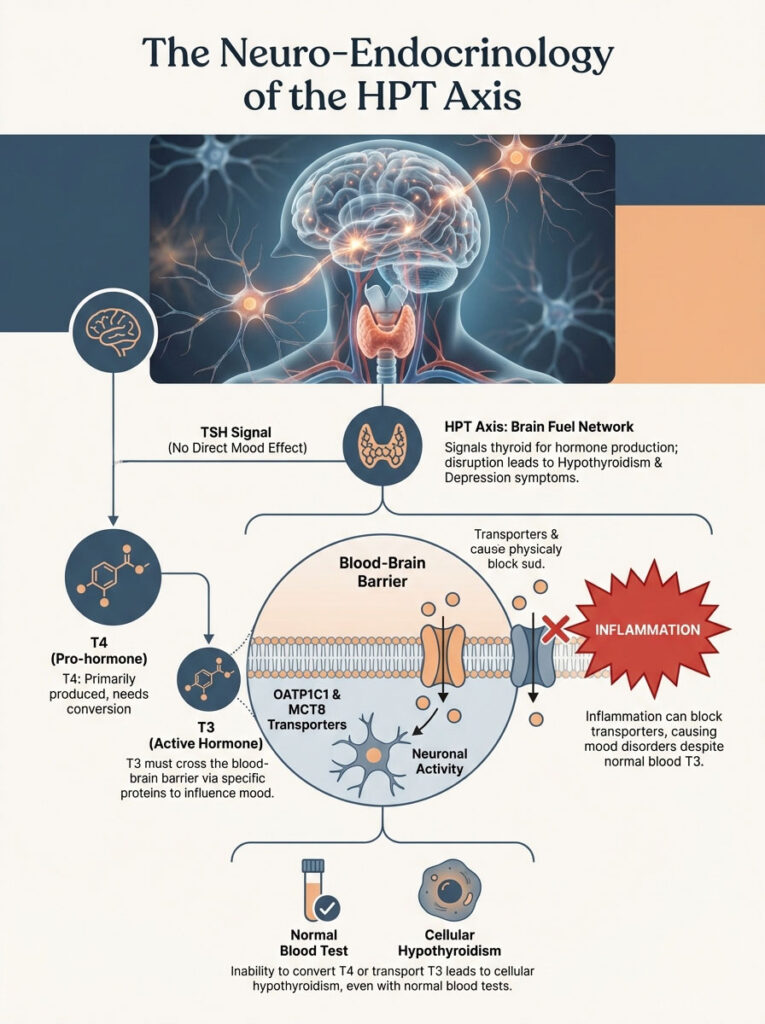
TSH is the Signal; T3 is the Fuel
Thyroid Stimulating Hormone (TSH) is a pituitary messenger. It knocks on the door of the thyroid gland. It asks for hormone production. However, TSH itself does not enter the brain to regulate mood.
The thyroid produces mostly Thyroxine (T4). This is a pro-hormone. T4 is biologically inactive until it is converted into Triiodothyronine (T3). T3 is the active molecule. It must cross the blood-brain barrier to interact with neurons.
Here is the catch. If you have plenty of T4 but cannot convert it to T3, your blood tests may look normal. Meanwhile, your brain remains in a hypothyroid state. This cellular hypothyroidism is a primary driver of mood disorders.
The Blood-Brain Barrier Challenge
Getting hormone into the blood is easy. Getting it into the brain is hard. Thyroid hormones must be transported across the blood-brain barrier by specific transporter proteins (OATP1C1 and MCT8).
Inflammation can damage these transporters. A patient might have perfect levels of T3 in their blood. But if the transporters are blocked by inflammation, the brain is starving. This is why we see patients with “normal” labs who still suffer from severe depression.
Neurotransmitters and Hormonal Interplay
Thyroid hormones do not work in isolation. They act as master regulators for the neurotransmitters that psychiatry targets. You cannot separate the endocrine system from the neurological system.
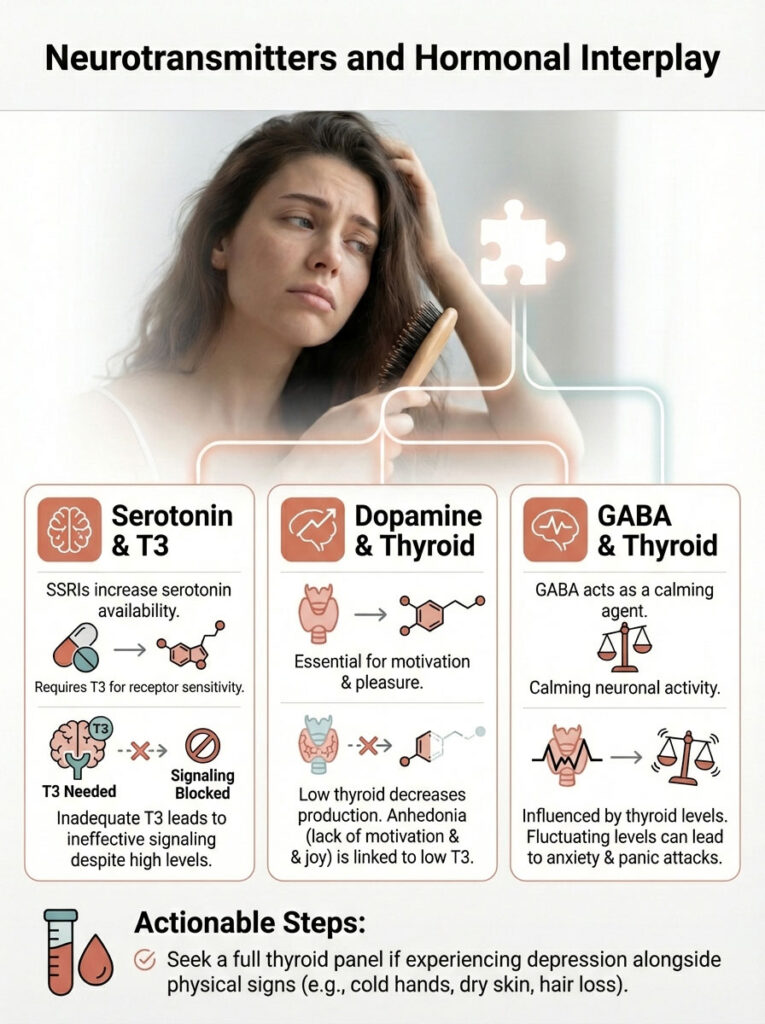
Serotonin and Receptor Sensitivity
Selective Serotonin Reuptake Inhibitors (SSRIs) work by keeping serotonin in the synaptic cleft longer. However, for serotonin to improve mood, it must bind to a receptor. Research indicates that T3 is required to maintain the sensitivity and density of these receptors.
Without adequate T3, you can flood the brain with serotonin. But the “doors” (receptors) remain locked. This explains why thyroid optimization is often the key to unlocking the efficacy of antidepressants. The drug provides the key; the thyroid provides the lock.
Dopamine and Anhedonia
Low thyroid function directly impacts dopamine signaling. Dopamine drives motivation, pleasure, and reward. When thyroid hormones are low, dopamine production slows.
This manifests not just as sadness. It manifests as anhedonia. This is the total lack of motivation or ability to feel joy. Patients often describe this as “feeling flat” rather than feeling sad. Nothing excites them. Nothing moves them. This is a dopamine deficit caused by a lack of T3.
GABA and Anxiety
Gamma-Aminobutyric Acid (GABA) is the brain’s “brake pedal.” It calms neuronal firing. Thyroid hormone modulates GABA activity. When levels fluctuate, as seen in early Hashimoto’s, the brain loses this braking mechanism.
This leads to severe anxiety or panic attacks. It seems contradictory that a “slow” metabolism causes “fast” anxiety. Yet, the loss of the GABA brake pedal creates a feeling of internal vibration and panic.
Expert Insight: “If you have been diagnosed with depression but also suffer from cold hands, dry skin, and hair loss, request a full thyroid panel immediately. Psychiatry cannot fix a metabolic problem.”
The Mitochondrial Connection: Energy for the Brain
We often talk about chemicals in the brain. We rarely talk about energy. Every neuron contains mitochondria. These are the power plants of the cell. They produce ATP, the energy currency of life.
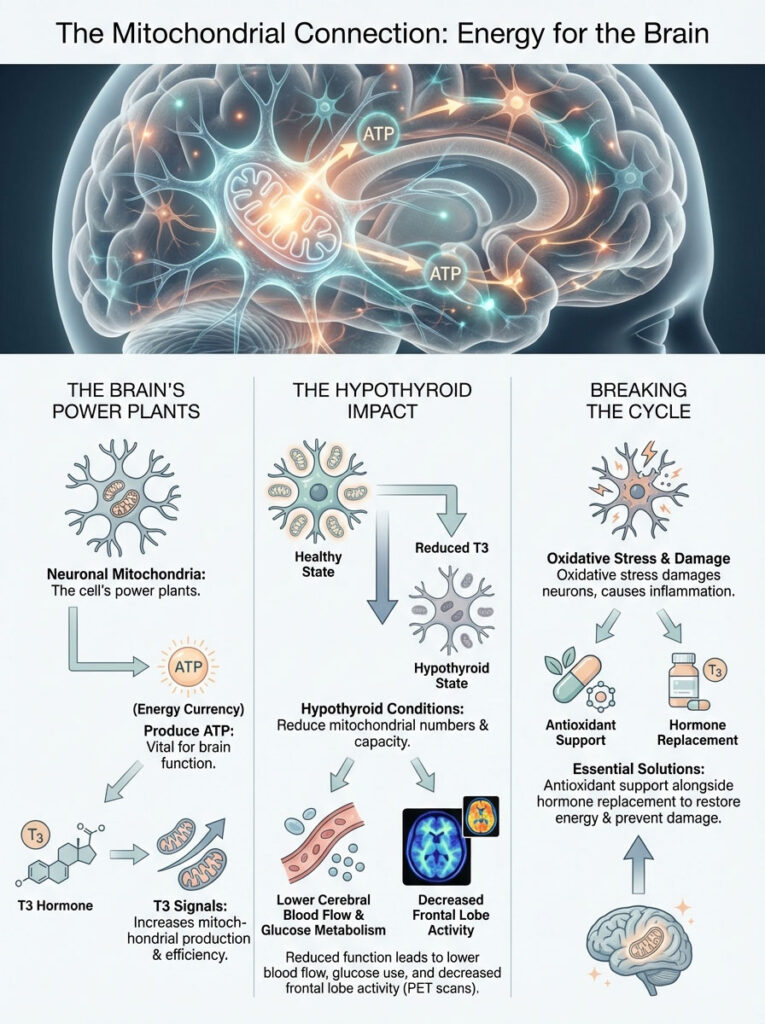
T3 Regulates Mitochondrial Biogenesis
T3 is the primary signal that tells cells to produce more mitochondria. It also tells existing mitochondria to work harder. In a hypothyroid brain, there are fewer power plants. The ones that exist are running at half capacity.
This leads to a global reduction in cerebral blood flow and glucose metabolism. PET scans of hypothyroid brains show reduced activity in the frontal lobes. These are the areas responsible for executive function and emotional regulation. The brain is literally powering down.
Oxidative Stress and Neuronal Damage
When mitochondria function poorly, they produce more waste products. These are called Reactive Oxygen Species (ROS). This leads to oxidative stress.
Oxidative stress damages neurons and causes inflammation. This inflammation further blocks thyroid transport. It is a vicious cycle. Low thyroid causes low energy. Low energy causes damage. Damage blocks thyroid hormone. Breaking this cycle requires aggressive antioxidant support alongside hormone replacement.
Differentiating Clinical Depression from Thyroid Symptoms
The term “depression” is often too broad. It fails to capture the nuance of endocrine dysfunction. Hypothyroidism & Depression presents with a specific clinical signature. It differentiates itself from classic melancholic depression.
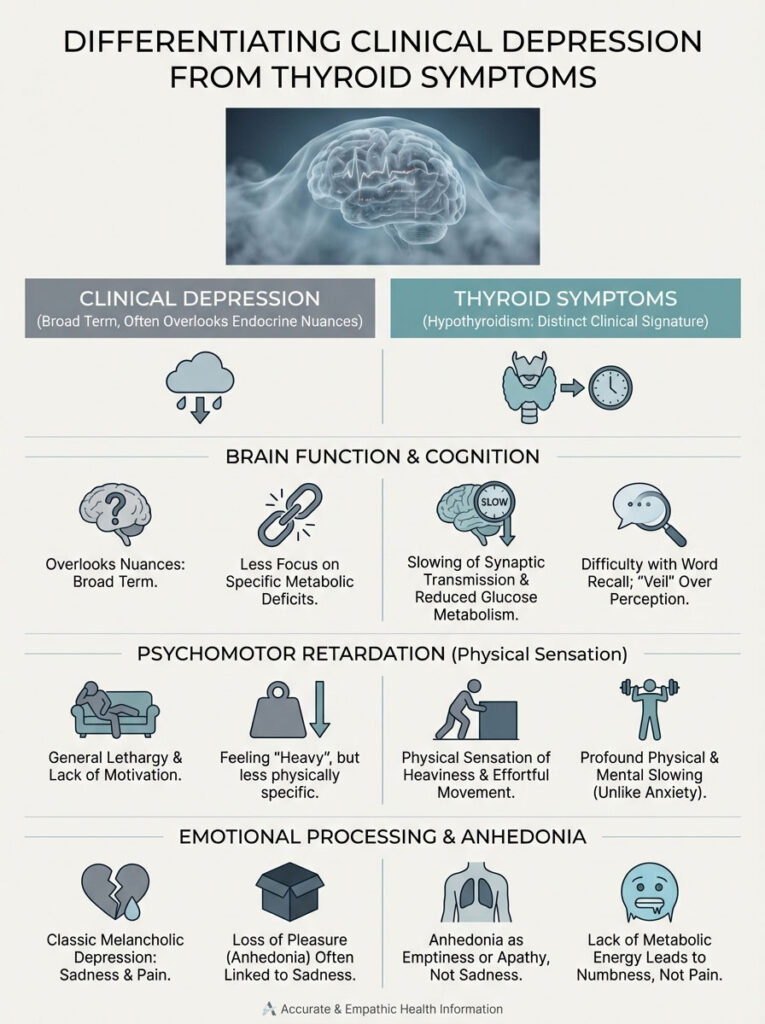
Thyroid Brain Fog
Thyroid brain fog is distinct from simple forgetfulness. It represents a measurable slowing of synaptic transmission. Glucose metabolism in the brain drops. Neurons literally have less energy to fire.
Patients report searching for words. They walk into rooms and forget why. There is a sensation of a “veil” between them and the world. This is an executive function deficit caused by low T3. It is not a lack of attention; it is a lack of fuel.
Psychomotor Retardation
A hallmark of hypothyroid depression is psychomotor retardation. This is the physical sensation of moving through mud. Speaking may feel like an effort. Limbs feel heavy.
While anxiety causes agitation, severe hypothyroidism causes a physical slowing. This parallels the mental slowing. Patients may sit for hours, staring at a wall, not because they are ruminating, but because the energy to move is absent.
Anhedonia vs. Melancholy
In classic depression, there is often intense emotional pain. There is guilt or rumination. In thyroid-mediated depression, the primary feeling is often emptiness or apathy.
The biological drive to care is dampened. The metabolic energy required to process emotion is absent. Patients often say, “I don’t feel sad, I just don’t feel anything.” This is a crucial diagnostic clue.
The Diagnostic Gap: Why Labs Fail Patients
One of the greatest frustrations in modern medicine is the patient who feels terrible but is told their labs are “perfect.” This discrepancy arises from the reference ranges used in standard care versus optimal TSH levels required for mental health.
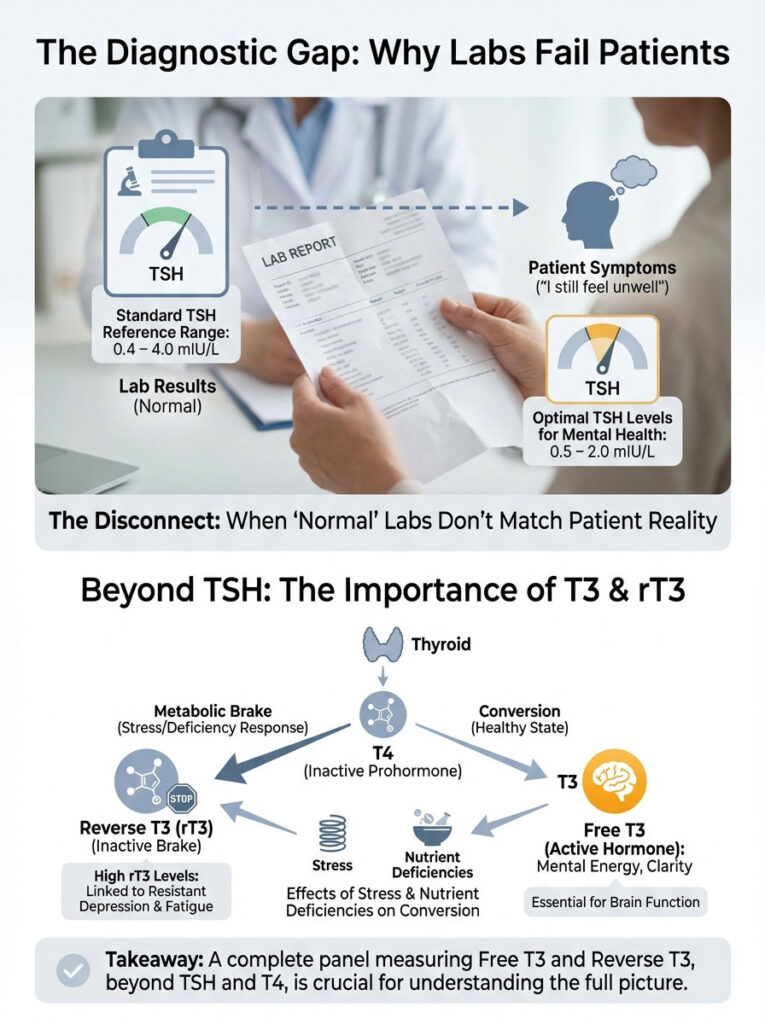
The TSH Controversy
The standard reference range for TSH is approximately 0.4 to 4.0 mIU/L. This range is based on a statistical average of the population. It is not based on optimal function.
In my experience, a TSH above 2.5 mIU/L can already signal insufficient thyroid activity for the brain. The heart and metabolism might be technically surviving. But the brain is highly sensitive. For a patient with a history of depression, we aim for a tighter TSH window. We often target between 0.5 and 2.0 mIU/L.
The Importance of Free T3
Most screenings measure only TSH and T4. This assumes the body is converting T4 to T3 perfectly. This is a dangerous assumption. Stress, inflammation, and nutrient deficiencies inhibit the deiodinase enzymes (D1, D2) responsible for this conversion.
We must measure Free T3. This tells us how much active hormone is actually available to the brain. A patient can have high T4 and low T3. This condition is called “Low T3 Syndrome.” It is heavily correlated with resistant depression.
Reverse T3: The Metabolic Brake
There is another player in this game. It is called Reverse T3 (rT3). Under stress, the body converts T4 into rT3 instead of T3. rT3 is inactive. It binds to thyroid receptors but does not activate them.
Think of it as a key that fits in the lock but won’t turn. It blocks the real key (T3) from getting in. High levels of rT3 indicate a body in “hibernation mode.” This is often seen in chronic stress or trauma. It mimics depression perfectly.
The Autoimmune Factor: Hashimoto’s and the Brain
Most cases of hypothyroidism in the US are caused by Hashimoto’s Thyroiditis. This is an autoimmune disease. The link between Hashimoto’s and anxiety is profound and often misdiagnosed.
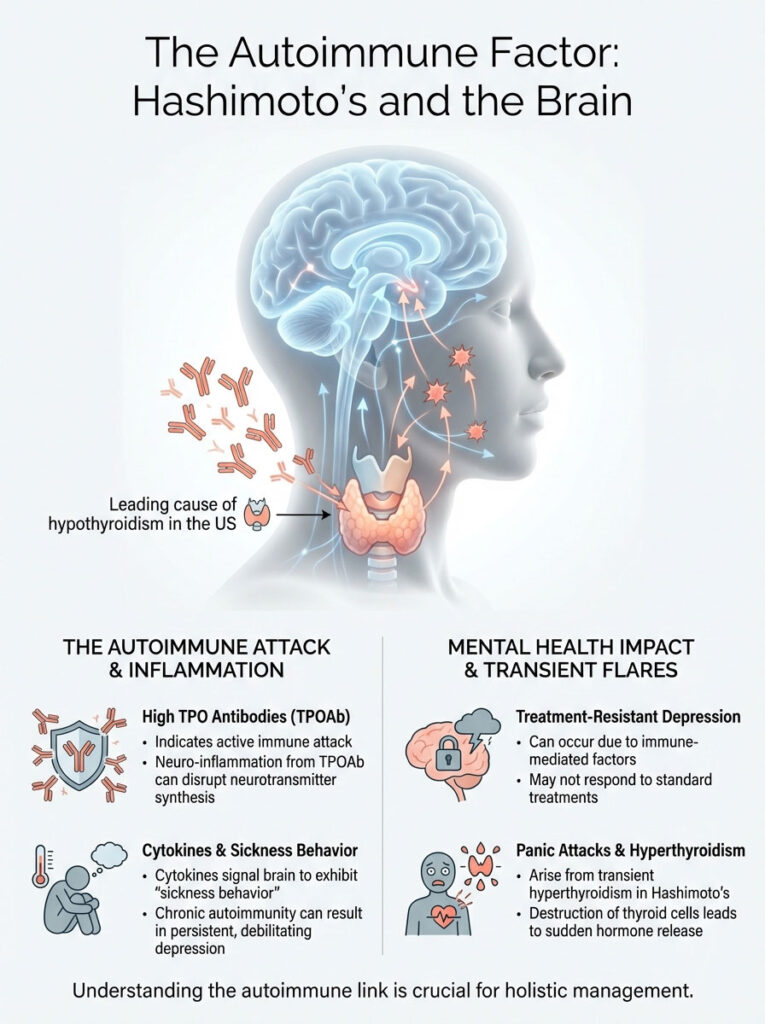
Hashimoto’s Encephalopathy: Brain on Fire
Even if thyroid hormone levels are normal, high antibodies matter. The presence of high Thyroid Peroxidase Antibodies (TPOAb) indicates an active immune attack. These antibodies and associated inflammatory cytokines can cross the blood-brain barrier.
This creates neuro-inflammation. We sometimes refer to this as “brain on fire.” This inflammation disrupts neurotransmitter synthesis. It leads to treatment-resistant depression that is immune-mediated. It is not just hormonal.
Can Low Thyroid Cause Panic Attacks?
Yes, but the mechanism is specific. In Hashimoto’s, the thyroid gland is slowly destroyed. As thyroid cells die, they can dump their stored hormone into the bloodstream all at once.
This causes transient hyperthyroidism (excess hormone). The patient experiences heart palpitations. They have racing thoughts and severe anxiety. A doctor might diagnose Generalized Anxiety Disorder (GAD). They miss the fact that this is a physical “thyroid storm” in miniature.
Cytokines and Mood
The immune system releases cytokines during autoimmune flares. These proteins signal the brain to enter “sickness behavior.” This state is characterized by withdrawal, fatigue, and low mood.
This is an evolutionary mechanism. It is meant to conserve energy for healing. But in chronic autoimmunity, the signal never stops. It manifests as persistent, debilitating depression.
The Gut-Brain-Thyroid Connection
You cannot heal the brain without healing the gut. The gut, thyroid, and brain form a triad of health. Disruption in one affects the others.
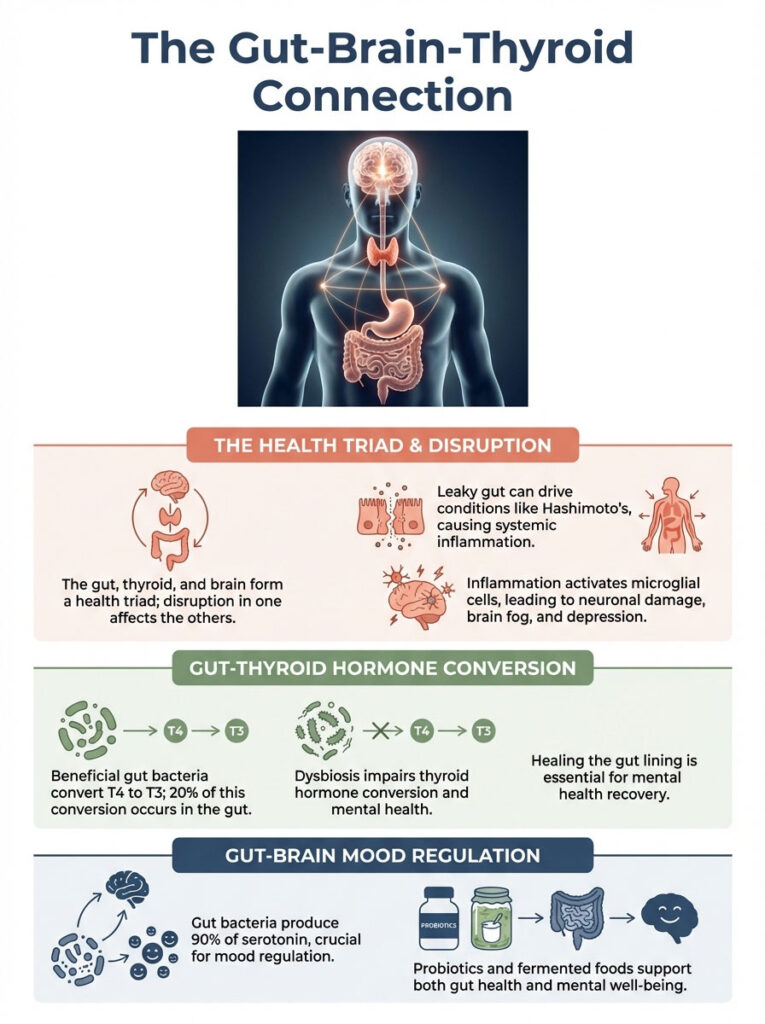
Intestinal Permeability (Leaky Gut)
Hashimoto’s is often driven by intestinal permeability. When the gut lining is compromised, food particles and bacteria enter the bloodstream. The immune system attacks them. This creates systemic inflammation.
This inflammation travels to the brain. It activates microglial cells. These are the brain’s immune cells. When activated chronically, they eat away at healthy neuronal connections. This leads to brain fog and depression. Healing the gut lining is a prerequisite for healing the mind.
The Microbiome Influence
Beneficial gut bacteria assist in converting T4 to T3. Approximately 20% of this conversion happens in the gut. If you have dysbiosis (imbalance of bacteria), your conversion suffers.
Furthermore, gut bacteria produce 90% of the body’s serotonin. A healthy microbiome supports both thyroid conversion and neurotransmitter production. Probiotics and fermented foods are not just good for digestion. They are essential for mental health.
Genetic Influences on Mental Health
Why do some people respond to T4 medication while others remain depressed? The answer often lies in their genes. Personalized medicine is the future of psychiatry.
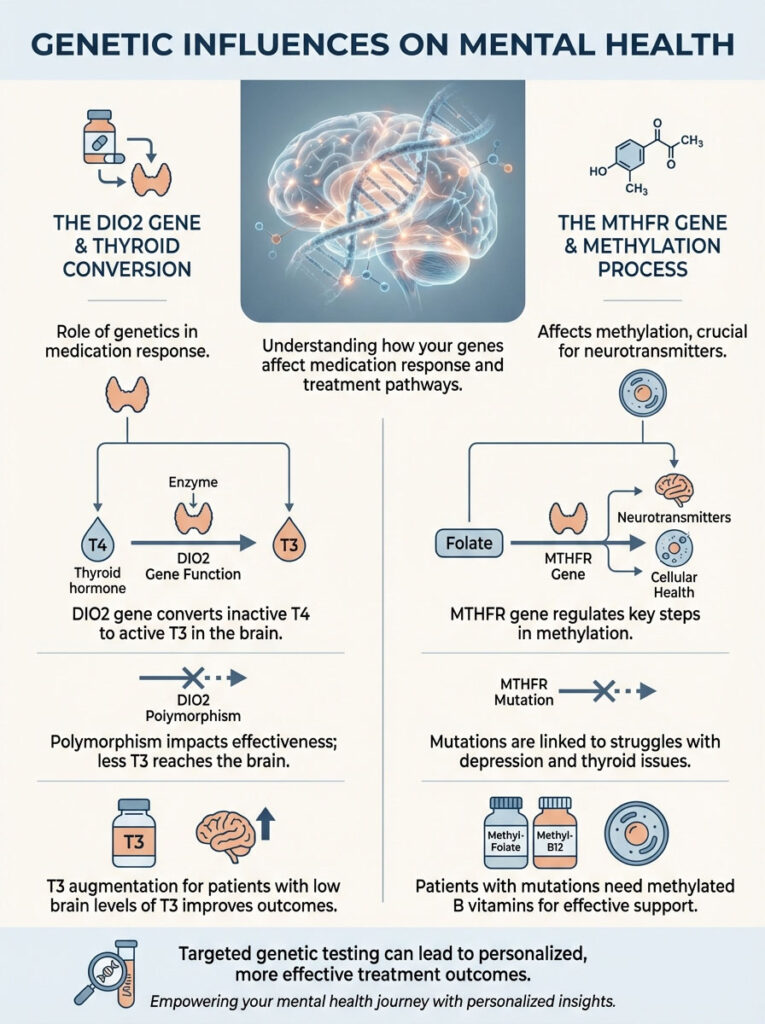
The DIO2 Polymorphism
Recent research highlights the DIO2 gene. This gene controls the enzyme that converts T4 to T3 specifically within the brain. A polymorphism (mutation) in this gene creates a problem.
A patient can have normal blood levels of T3 but low brain levels of T3. These patients often feel no relief on Levothyroxine (T4 only). However, they respond dramatically to T3 augmentation. Testing for this gene can change the entire treatment trajectory.
MTHFR and Methylation
The MTHFR gene mutation affects methylation. This process is vital for producing neurotransmitters and detoxifying hormones. Patients with MTHFR mutations often struggle with both depression and thyroid issues.
They require methylated B vitamins (Methyl-Folate and Methyl-B12) to bypass the genetic block. Addressing methylation can improve the efficiency of thyroid medication and antidepressant therapy.
Advanced Treatment Protocols for Thyroid Depression
Standard care often involves prescribing Levothyroxine (T4) and an antidepressant. For many, this is insufficient. Treatment-resistant depression thyroid protocols require a more nuanced approach.

Standard of Care vs. Neuro-Optimization
Levothyroxine monotherapy works well for restoring TSH levels. But it may fail to restore brain T3 levels. If a patient remains depressed despite normal TSH, we must pivot. We must consider that they are poor converters of T4 to T3.
T3 Augmentation Strategy
T3 augmentation involves adding Liothyronine (Cytomel) to the patient’s regimen. The STAR*D trial was a landmark study in psychiatry. It demonstrated that adding T3 to an antidepressant was one of the most effective strategies for achieving remission in resistant depression.
By directly providing the active hormone, we bypass the conversion bottleneck. We directly activate neuronal receptors. Patients often report “waking up” within days of starting T3.
Natural Desiccated Thyroid (NDT)
Some patients respond better to Natural Desiccated Thyroid (e.g., Armour Thyroid, NP Thyroid). These medications are derived from porcine glands. They contain T4, T3, and trace amounts of T2 and T1.
Many patients report better mental clarity on NDT. This is likely due to the presence of T3 and other co-factors not found in synthetic T4. It mimics the body’s natural output more closely.
Low Dose Naltrexone (LDN)
For patients with high antibodies, Low Dose Naltrexone (LDN) is a game changer. It modulates the immune system. It raises endorphins. It reduces neuro-inflammation.
By calming the autoimmune attack, LDN allows the thyroid to function better. It also directly improves mood by increasing natural “feel good” chemicals in the brain.
Comparison of Therapeutic Interventions
Choosing the right intervention requires understanding the mechanism of action. The table below compares common treatments regarding their mental health impact.
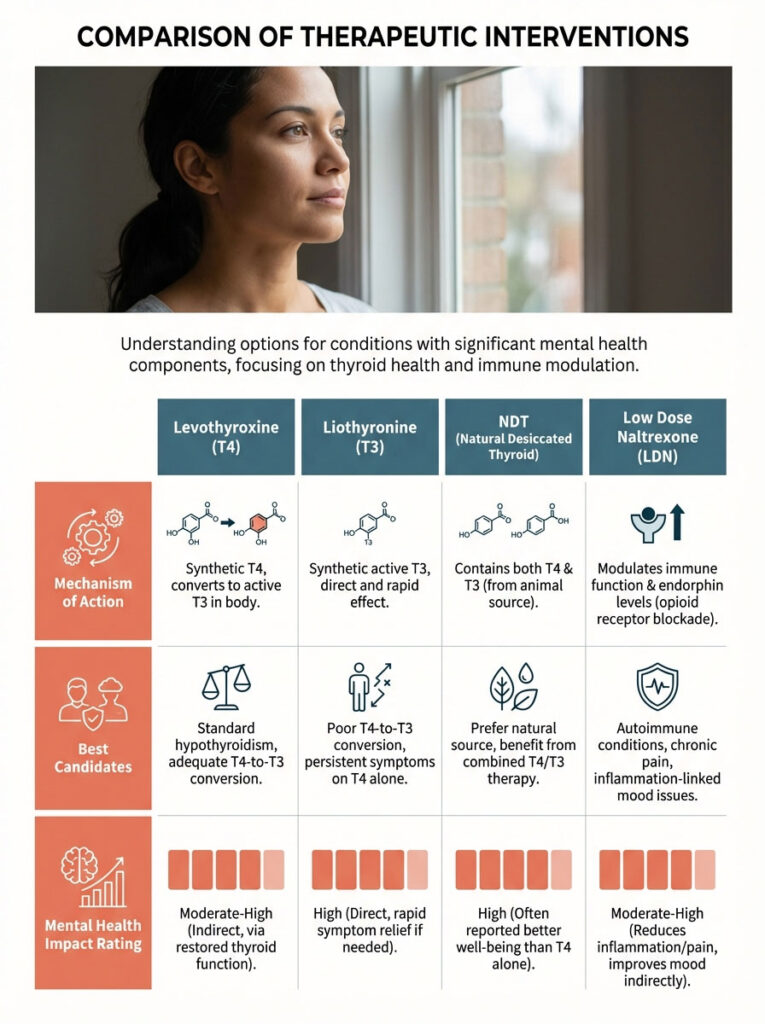
| Intervention | Mechanism of Action | Best Candidates | Mental Health Impact |
|---|---|---|---|
| Levothyroxine (T4 Only) | Replaces storage hormone | Patients with good conversion | Moderate; often leaves residual brain fog |
| Liothyronine (T3) | Direct active hormone | Poor converters; DIO2 gene mutation | High; rapid improvement in mood/cognition |
| NDT (Armour/NP Thyroid) | Contains T4, T3, T2, T1 | Patients preferring natural options | High; provides broad spectrum hormones |
| Low Dose Naltrexone (LDN) | Immune modulator | High TPO Antibodies (Hashimoto’s) | Reduces neuro-inflammation and anxiety |
Nutritional Psychiatry for Thyroid Optimization
Medication is a pillar of recovery. However, it is not the entire structure. We must support the biology that allows the medication to work. Nutritional deficiencies are rampant in depression and hypothyroidism.
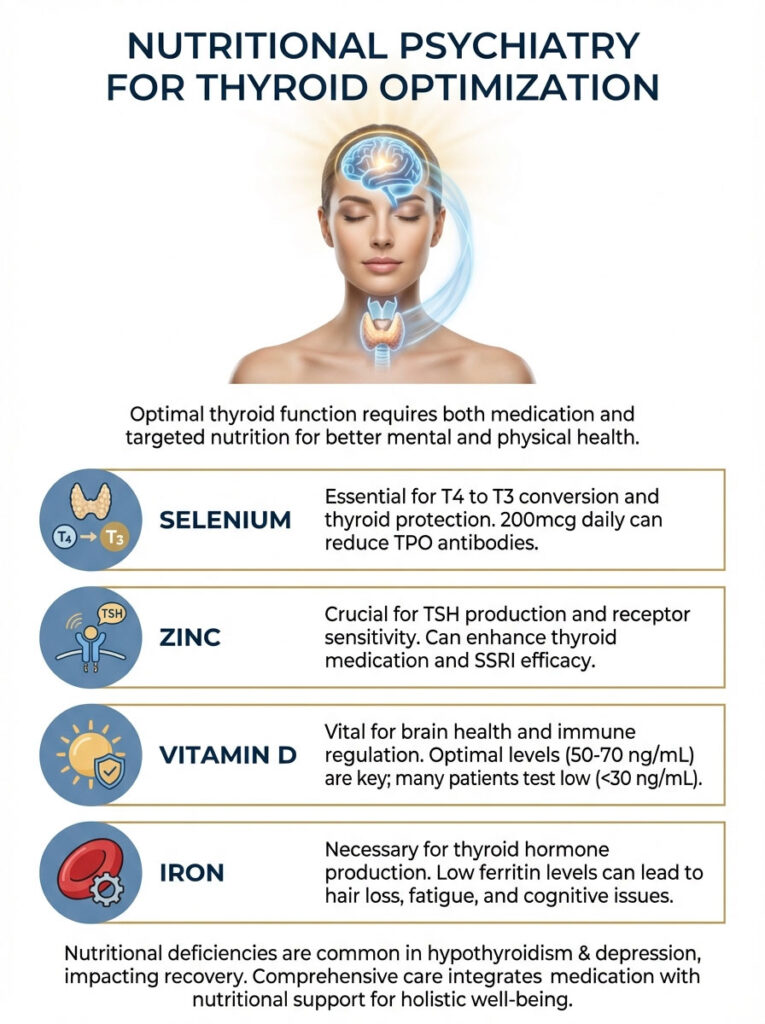
Selenium: The Converter
Selenium is non-negotiable. It is required for the deiodinase enzymes that convert T4 to T3. Without selenium, conversion stops.
It also acts as an antioxidant within the thyroid gland. It protects the gland from damage during hormone production. Studies show that 200mcg of selenium daily can reduce TPO antibodies significantly. This lowers inflammation and improves mood.
Zinc: The Receptor Sensitizer
Zinc is essential for TSH production. It is also vital for the receptor sensitivity of both thyroid hormone and neurotransmitters. You need zinc to smell, taste, and make serotonin.
Antidepressants often deplete zinc. This creates a paradoxical effect where the treatment worsens the deficiency. Supplementing with zinc picolinate or glycinate can improve the efficacy of both thyroid meds and SSRIs.
Vitamin D: The Immune Modulator
There is a strong correlation between low Vitamin D, autoimmunity, and depression. Vitamin D is actually a steroid hormone. It regulates the immune system.
Optimal levels are vital for preventing the immune system from attacking the brain. We often aim for levels between 50 and 70 ng/mL. Most patients with depression test below 30 ng/mL.
Iron and Ferritin
Iron is required for the thyroid peroxidase enzyme. This enzyme makes thyroid hormone. Low iron equals low thyroid output.
Ferritin is the storage form of iron. If ferritin drops below 50, many patients experience hair loss and fatigue. If it drops below 30, brain function is compromised. Iron deficiency is a common, reversible cause of brain fog.
Lifestyle Factors: Sleep, Stress, and Movement
You cannot out-medicate a bad lifestyle. The HPT axis is intimately connected to your daily habits. Small changes here yield massive dividends for mental health.
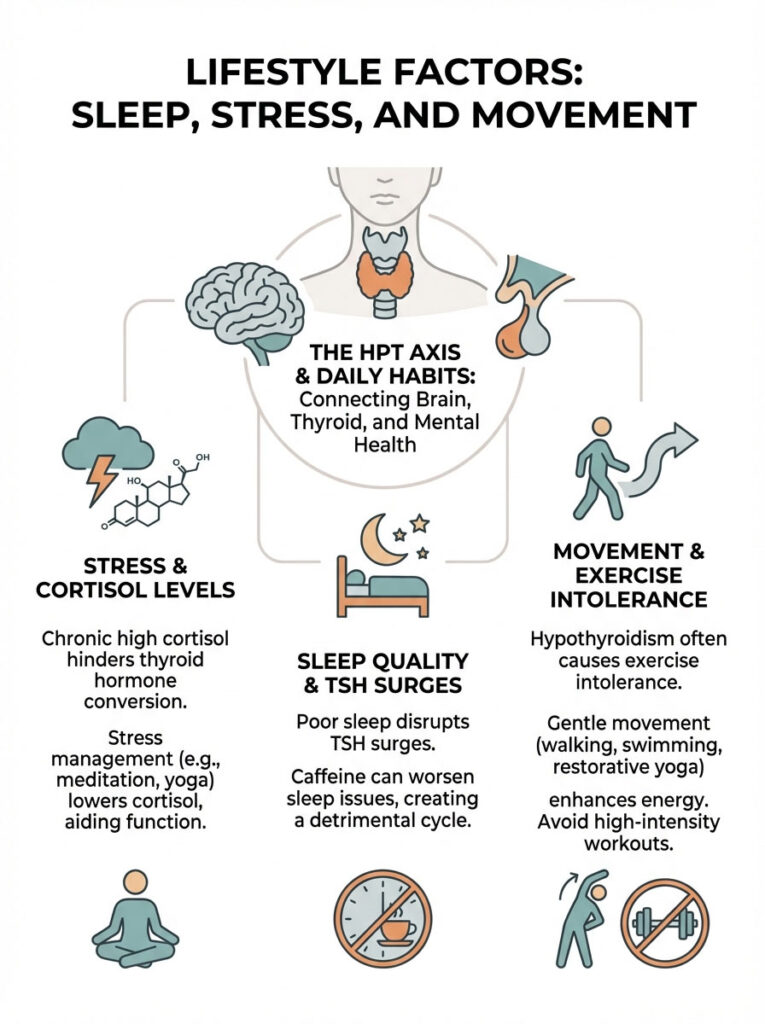
Stress Management and Cortisol
High cortisol is the enemy of the thyroid. Cortisol is the stress hormone. When it is chronically high, it blocks the conversion of T4 to T3. It also increases Reverse T3.
Chronic stress literally steals thyroid hormone from the brain. Practices like meditation, deep breathing, or gentle yoga are not just “relaxing.” They are metabolic interventions. They lower cortisol and allow T3 to reach the brain.
Circadian Rhythm and Sleep
Sleep regulates the HPT axis. TSH surges at night while you sleep. If you have poor sleep quality or sleep apnea, you disrupt this surge.
This creates a vicious cycle. You are tired, so you drink caffeine. Caffeine disrupts sleep. The thyroid suffers. Prioritizing sleep hygiene is critical. This includes dark rooms, cool temperatures, and no screens before bed.
Exercise Intolerance
Patients with hypothyroidism often have exercise intolerance. They feel exhausted for days after a workout. This is because their mitochondria cannot recover.
We recommend starting low and slow. Walking, swimming, or restorative yoga are best. High Intensity Interval Training (HIIT) can spike cortisol and worsen the condition. Listen to your body. Movement should energize you, not deplete you.
Special Considerations for Women
The intersection of reproductive hormones and thyroid function creates a “perfect storm” for women’s mental health. Estrogen and progesterone fluctuations directly influence thyroid binding globulins and receptor sensitivity.
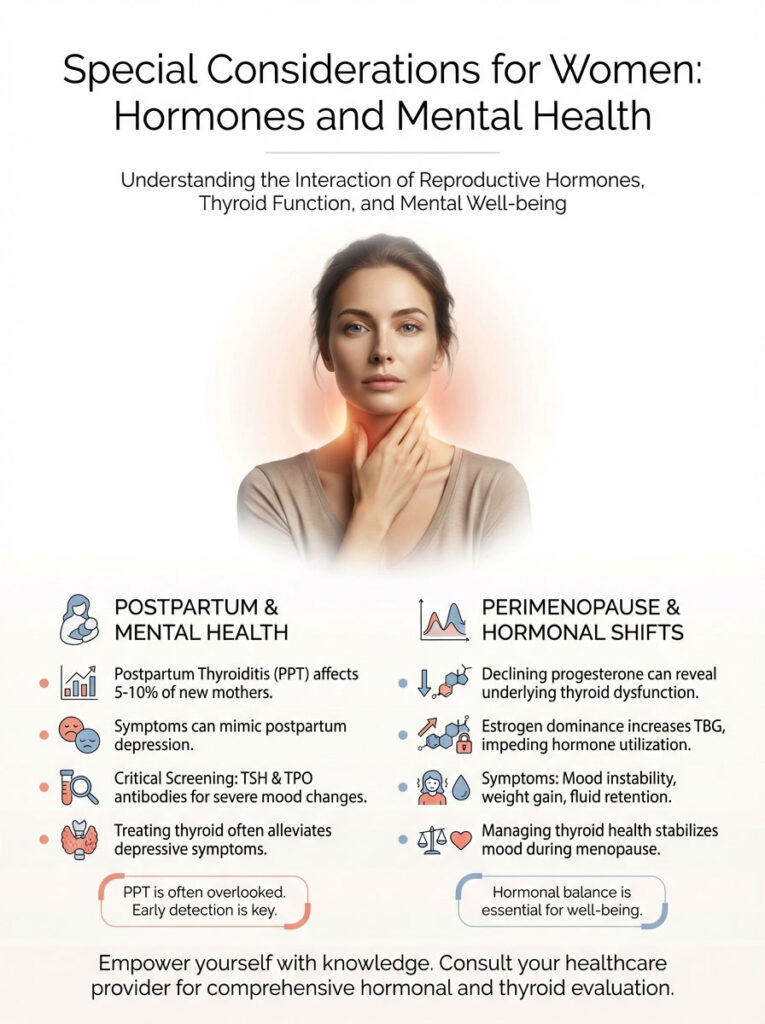
Postpartum Thyroiditis
Postpartum depression (PPD) is a serious concern. Roughly 5-10% of women experience Postpartum Thyroiditis. The immune system rebounds after pregnancy. It attacks the thyroid.
This can look exactly like PPD. Symptoms include fatigue, weeping, and an inability to cope. Screening for TSH and TPO antibodies should be standard for any woman experiencing severe mood changes after delivery. Treating the thyroid often resolves the “depression.”
Perimenopause and Estrogen Dominance
As progesterone drops during perimenopause, the body’s ability to tolerate stress decreases. This often unmasks underlying thyroid issues. Estrogen dominance increases Thyroid Binding Globulin (TBG).
TBG binds up thyroid hormone so it cannot be used. You might have plenty of hormone, but it is all tied up. The combination leads to severe mood instability, weight gain, and fluid retention. Treating the thyroid is often necessary to stabilize the menopausal transition.
When to See a Neuro-Endocrinologist
If you are battling Hypothyroidism & Depression, you need a provider who looks at the whole picture. Standard primary care may not have the time or specialized training. They often cannot interpret the nuances of the HPT axis.
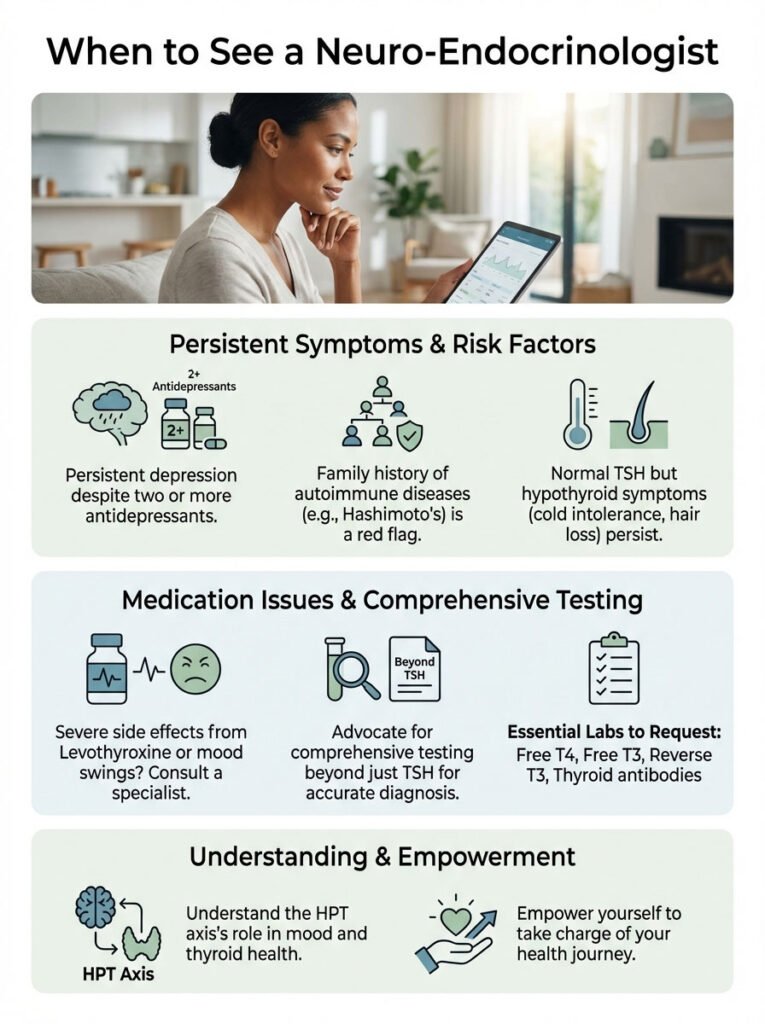
Red Flags
You should seek a specialist if you meet certain criteria. Do you have depression resistant to two or more antidepressants? Do you have a family history of autoimmune disease?
Perhaps you have “normal” TSH but classic hypothyroid symptoms like cold intolerance and hair loss. Maybe you experience severe Levothyroxine and mood swings. These are signs that standard protocols are failing you.
The Full Panel Request
Do not settle for just TSH. You must advocate for yourself. Request the following labs to get a clear picture of your neuro-endocrinology of mood:
- TSH: The pituitary signal.
- Free T4: The storage hormone.
- Free T3: The driver of mental health.
- Reverse T3: The brake pedal.
- TPO Antibodies & Tg Antibodies: To rule out Hashimoto’s.
- Vitamin D & Ferritin: Essential co-factors.
Summary & Key Takeaways
The connection between Hypothyroidism & Depression is undeniable. It is deeply rooted in our biology. The brain is the most thyroid-sensitive organ in the body. When fuel is low, the brain conserves energy. It shuts down “expensive” processes like mood regulation, motivation, and complex cognition.
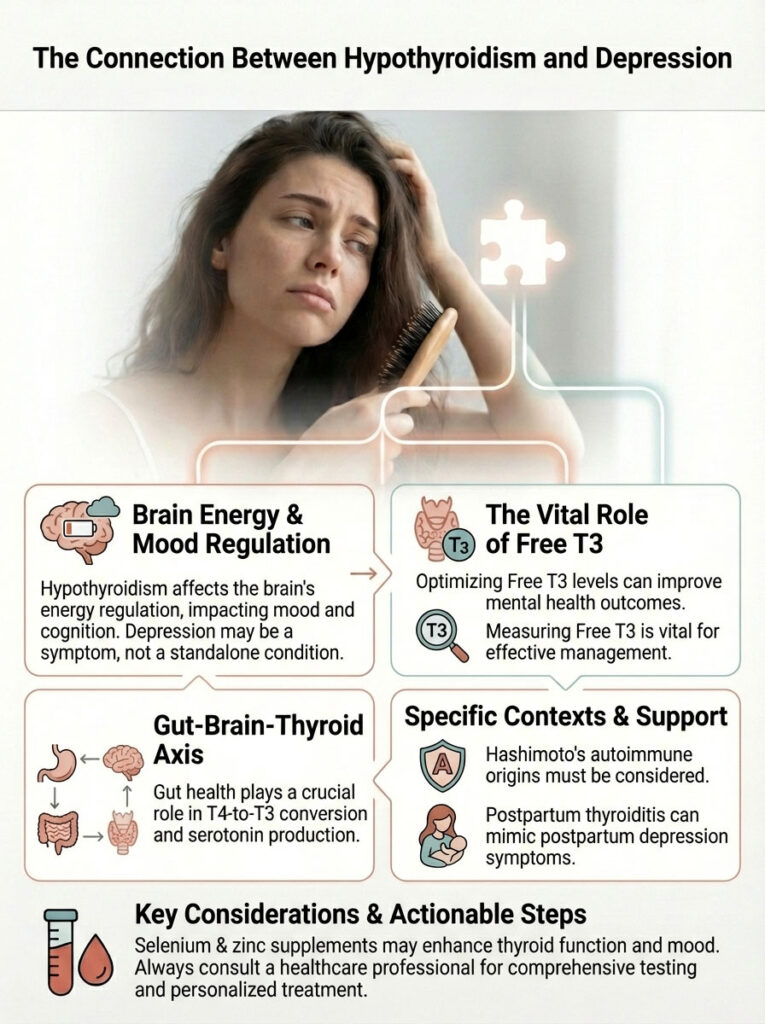
Depression in the presence of thyroid dysfunction is often a symptom. It is not always a separate disease. It is a biological signal that the brain is starving for T3. By optimizing thyroid levels—specifically Free T3—we can change the outcome.
We must also address the autoimmune roots of Hashimoto’s. We must fix the gut and replenish nutrients. This comprehensive approach can often lift the veil of depression that antidepressants alone cannot touch. Advocate for full testing. Look beyond the “normal” range. Your mental health depends on it.
Frequently Asked Questions
Why does hypothyroidism cause symptoms of depression?
Low levels of Triiodothyronine (T3) reduce the sensitivity and density of serotonin and dopamine receptors in the brain. This creates a metabolic deficiency where neurons lack the energy to regulate mood effectively, often resulting in a state known as organic mood syndrome.
Why do I still feel depressed if my TSH levels are in the normal range?
Standard reference ranges for TSH are often too broad; for optimal mental health, many patients require a tighter TSH window between 0.5 and 2.0 mIU/L. Furthermore, a normal TSH does not account for poor T4-to-T3 conversion or issues with thyroid hormone transport across the blood-brain barrier.
Can Hashimoto’s disease cause anxiety and panic attacks?
Yes, Hashimoto’s can cause transient hyperthyroidism where dying thyroid cells dump excess hormone into the bloodstream, triggering heart palpitations and racing thoughts. Additionally, high TPO antibodies create neuro-inflammation that disrupts GABA activity, the brain’s natural calming mechanism.
What is the DIO2 gene mutation and how does it affect mood?
The DIO2 polymorphism impairs the enzyme responsible for converting T4 into active T3 specifically within the brain’s tissues. Patients with this mutation may have perfect blood work but suffer from severe brain hypothyroidism, often requiring T3 medication to see any improvement in depressive symptoms.
Is T3 augmentation an effective treatment for treatment-resistant depression?
Clinical trials like STAR*D demonstrate that adding Liothyronine (T3) to an antidepressant regimen is one of the most effective strategies for achieving remission. T3 provides the metabolic lock that allows the antidepressant’s serotonin key to function properly within the neuronal synapse.
How do I distinguish between clinical depression and thyroid-related brain fog?
Thyroid-mediated depression typically presents with psychomotor retardation—a physical feeling of moving through mud—and a profound sense of apathy or anhedonia. Unlike classic melancholia, patients often report a cognitive veil and a lack of metabolic energy to process any emotion at all.
Why is measuring Free T3 more important for mental health than TSH alone?
Free T3 is the active hormone that actually enters brain cells to regulate mitochondrial function and neurotransmitter signaling. TSH is merely a pituitary signal; if your body cannot convert T4 to T3 due to stress or inflammation, your brain will remain in a hypothyroid state regardless of your TSH level.
What role does Reverse T3 play in mood and energy levels?
Reverse T3 (rT3) acts as a metabolic brake by binding to thyroid receptors and blocking active T3 from entering the cell. High rT3 levels, often triggered by chronic stress or trauma, put the body into a hibernation mode that mimics the symptoms of severe clinical depression.
How does gut health influence the connection between the thyroid and depression?
Approximately 20% of T4-to-T3 conversion occurs in the gut, and a healthy microbiome is essential for producing the serotonin that thyroid hormones regulate. Intestinal permeability can also trigger the systemic inflammation that drives Hashimoto’s and subsequent neuro-inflammation.
Can selenium and zinc supplements improve thyroid-related mood disorders?
Selenium is a critical co-factor for the deiodinase enzymes that convert T4 to T3, while zinc is necessary for TSH production and receptor sensitivity. Correcting these deficiencies can lower TPO antibodies and improve the efficacy of both thyroid replacement therapy and SSRIs.
Why is postpartum depression often linked to thyroid dysfunction?
Postpartum thyroiditis affects up to 10% of women when the immune system rebounds after pregnancy and attacks the thyroid gland. This causes a shift in hormone levels that can look identical to postpartum depression, making thyroid screening essential for any new mother experiencing mood instability.
What are the benefits of Natural Desiccated Thyroid (NDT) for mental clarity?
NDT medications like Armour or NP Thyroid provide a full spectrum of hormones, including T4, T3, T2, and T1, which more closely mimics human thyroid output. Many patients report superior cognitive function and mood stability on NDT compared to synthetic T4-only treatments like Levothyroxine.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The connection between Hypothyroidism & Depression is complex and requires individualized care. Always consult with a qualified neuro-endocrinologist, psychiatrist, or healthcare professional before making changes to your medication, supplement regimen, or lifestyle. Do not disregard professional medical advice or delay seeking it because of something you have read in this article.
References
- American Thyroid Association (ATA) – thyroid.org – Clinical guidelines on the diagnosis and management of hypothyroidism and its psychiatric manifestations.
- The STAR*D Trial – American Journal of Psychiatry – A landmark study demonstrating the efficacy of T3 augmentation in patients with treatment-resistant depression.
- Journal of Thyroid Research – hindawi.com/journals/jtr/ – Research regarding the DIO2 gene polymorphism and its impact on brain-specific T3 levels.
- National Institute of Mental Health (NIMH) – nimh.nih.gov – Statistics on Major Depressive Disorder and the prevalence of co-occurring endocrine disorders.
- Endocrine Society – endocrine.org – Comprehensive resources on the HPT axis and the metabolic requirements of neuronal function.
- Frontiers in Endocrinology – frontiersin.org – Studies on the role of inflammatory cytokines and thyroid antibodies in neuro-inflammation and mood.








