Lisa sat in my office. She looked visibly exhausted. Her hands clutched a lab report that her previous doctor had labeled “normal.” She had been battling debilitating fatigue for years. She was soaking through super-plus tampons every two hours. She was told her heavy flow was just “part of being a woman.” Others suggested it was early perimenopause. But Lisa didn’t have a gynecological problem in isolation. She had an endocrine crisis.
Table of Contents
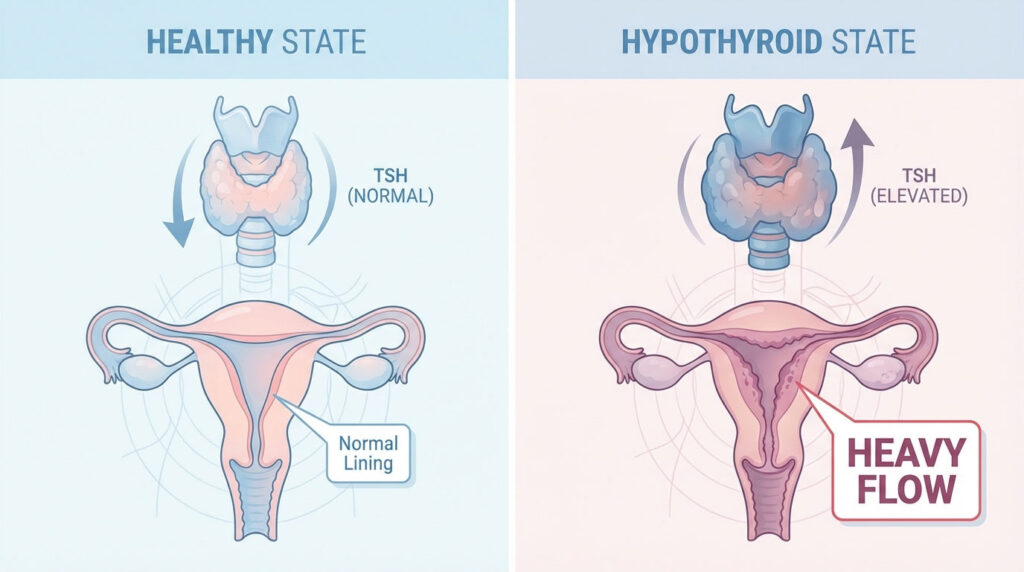
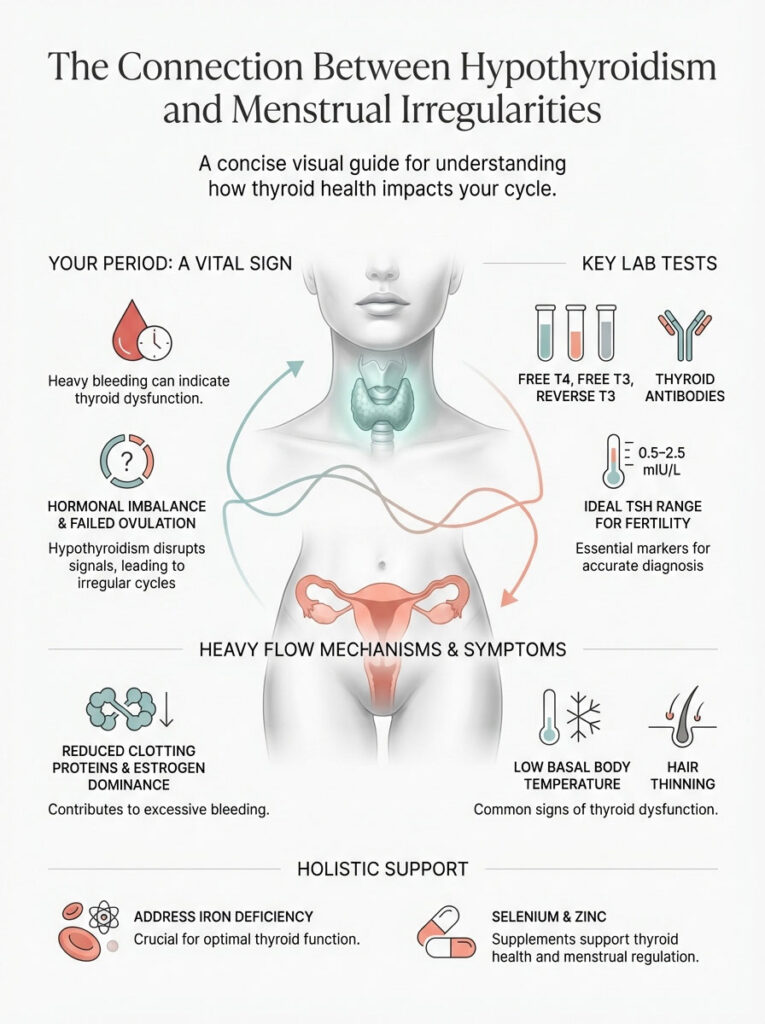
Her story is not unique. In my practice as a reproductive endocrinologist, I see this scenario daily. Women treat the symptom while the root cause goes undetected. Hypothyroidism and periods are intrinsically linked. Yet this connection is frequently overlooked in primary care. When your thyroid slows down, it doesn’t just lower your energy. It dismantles the delicate communication network known as the Hypothalamic-Pituitary-Ovarian (HPO) axis.
For many of my patients, heavy menstrual bleeding (menorrhagia) is the very first clinical sign. It indicates that their thyroid function is compromised. It is not a coincidence. It is a biological signal. We need to decode that signal to restore your health.
Quick Answer: Why is your period heavy?
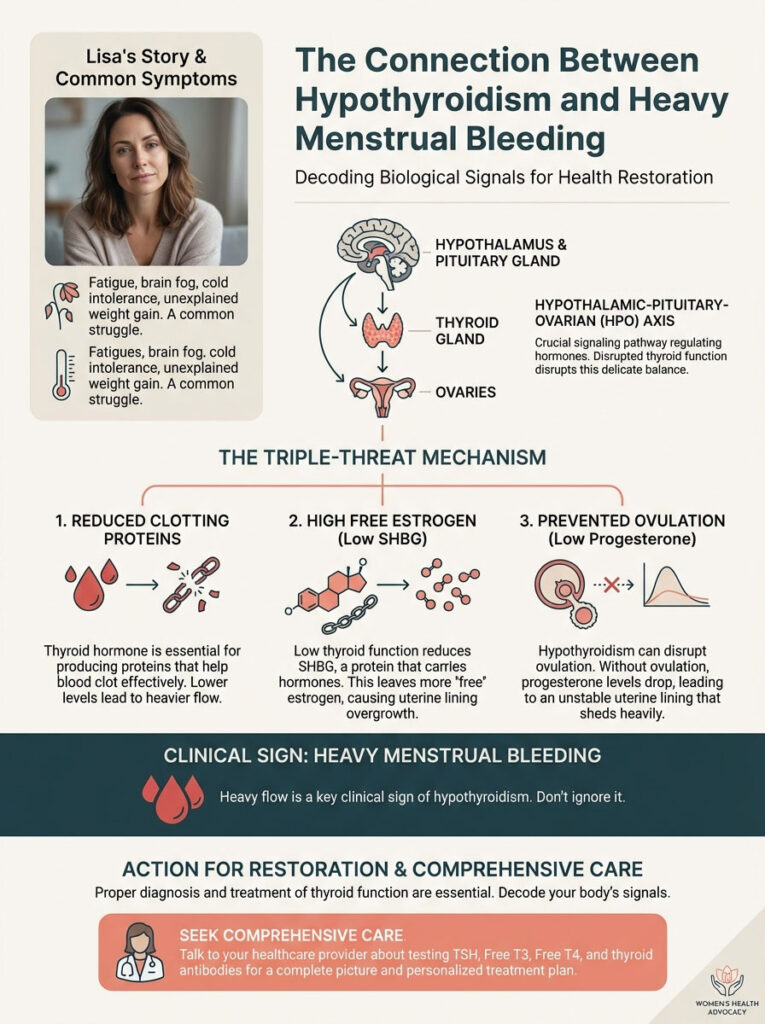
Hypothyroidism causes heavy periods through a “triple-threat” mechanism. First, it reduces the production of blood-clotting proteins (Factor VII and VIII). This makes it harder for bleeding to stop. Second, it lowers SHBG levels. This leads to high free estrogen which thickens the uterine lining. Third, it often prevents ovulation. This results in low progesterone and a chaotic, heavy shed.
The Physiology of the HPO Axis: How the Thyroid “Talks” to the Ovaries
To understand why you are bleeding heavily, we must look beyond the uterus. The thyroid gland acts as the metabolic throttle for every cell in your body. This includes your reproductive organs. The relationship between hypothyroidism and periods begins deep in the brain.
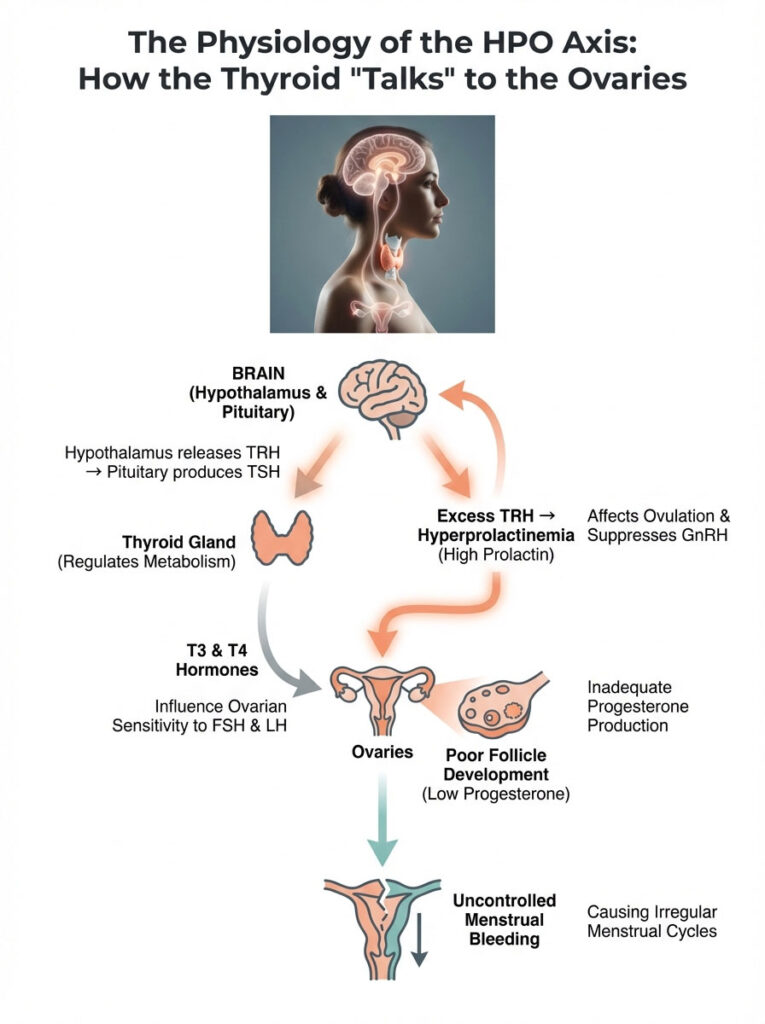
Your reproductive system relies on a precise rhythm. Hormones must pulse at specific times. The thyroid hormone provides the energy for this rhythm. When thyroid levels drop, the rhythm breaks. The communication lines between the brain and the ovaries become filled with static.
Key Statistics: Thyroid & Reproductive Health
- 1 in 8 women will develop a thyroid disorder during her lifetime (American Thyroid Association).
- 44% of women with hypothyroidism experience menstrual irregularities. This compares to only 20% of euthyroid women.
- Menorrhagia (heavy bleeding) occurs in approximately 60% of severe hypothyroid cases.
- Undiagnosed thyroid dysfunction is a contributing factor in 2.3% to 4.6% of infertility cases.
- Women with heavy periods are 4 times more likely to have subclinical hypothyroidism than those with normal flow.
The Feedback Loop Disruption
The hypothalamus releases Thyrotropin-Releasing Hormone (TRH). This signals the pituitary gland to make TSH. When thyroid hormone levels are low, the hypothalamus screams for more production. It does this by pumping out excess TRH. This is where the cross-wiring happens.
The cells in the pituitary that produce Prolactin are situated right next to the TSH-producing cells. They share a blood supply. They share receptor sensitivity. When the alarm bell rings for TSH, the Prolactin cells wake up too.
The Prolactin Connection
High levels of TRH inadvertently stimulate the pituitary to overproduce Prolactin. This condition is known as hyperprolactinemia. It is a common side effect of hypothyroidism. High prolactin suppresses Gonadotropin-Releasing Hormone (GnRH).
Without the rhythmic pulsing of GnRH, your pituitary cannot signal your ovaries to ovulate properly. This leads to anovulation (lack of ovulation). It can also cause irregular periods. This sets the stage for the heavy bleeding that follows later in the cycle.
Impact on FSH and LH Sensitivity
Thyroid hormones (T3 and T4) directly modulate ovarian sensitivity. They determine how your ovaries respond to Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH). Without adequate T3, the granulosa cells in the ovary cannot develop a healthy follicle.
A poor follicle leads to a weak corpus luteum. A weak corpus luteum means your body cannot produce enough progesterone. As we will discuss, progesterone is the “brake” on menstrual bleeding. Without it, the flow becomes uncontrollable.
Why You Bleed Heavily: The Three Distinct Mechanisms
Patients often ask me a logical question. “Why does a slow metabolism make me bleed more?” It seems counterintuitive. You might expect everything to slow down or stop. However, the link between hypothyroidism and periods is driven by three specific biological failures. Understanding these helps you advocate for the right testing.
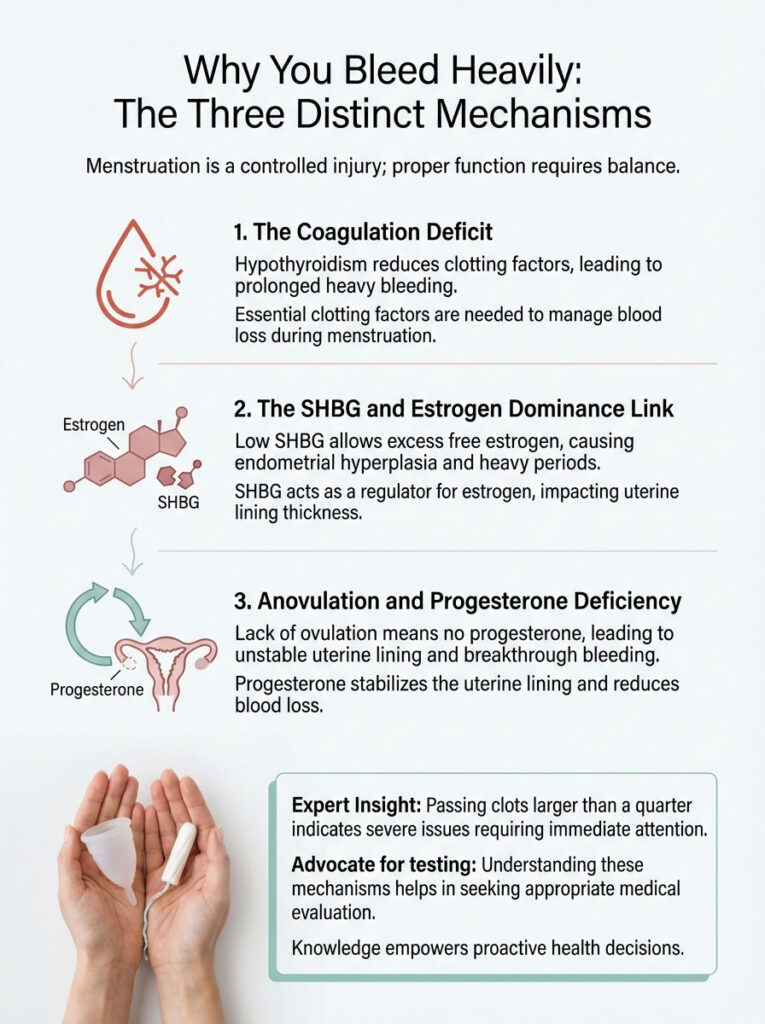
A. The Coagulation Deficit (Hematological Pathway)
This is the most critical factor. It is also the least discussed factor in general practice. Hypothyroidism is not just hormonal. It is hematological. It affects your blood’s ability to clot. Thyroid hormone regulates the synthesis of coagulation factors in the liver.
When you are hypothyroid, your body produces significantly less of these essential proteins:
- Factor VII (Proconvertin)
- Factor VIII (Antihemophilic factor)
- von Willebrand factor
Think of menstruation as a controlled injury. During menstruation, your body relies on these “chemical tools.” They plug the blood vessels in the uterine lining as it sheds. If you lack these clotting factors, the vessels remain open longer than necessary.
Consequently, you experience heavy menstrual bleeding. This often lasts longer than 7 days. It happens simply because your body cannot form the clots needed to stem the flow. You are essentially dealing with a temporary, thyroid-induced bleeding disorder.
B. The SHBG and Estrogen Dominance Link
Your liver produces a protein called Sex Hormone-Binding Globulin (SHBG). Think of SHBG as a sponge. It soaks up excess hormones in the bloodstream. It keeps them inactive until they are needed. Thyroid hormone stimulates the liver to create this protein. Therefore, low thyroid function equals low SHBG.
When SHBG is low, it cannot bind to estrogen effectively. This leads to a spike in “Free Estrogen.” Estrogen is a proliferative hormone. Its job is to thicken the endometrium (uterine lining). With unchecked free estrogen, the lining becomes excessively thick. We call this Endometrial Hyperplasia.
When this overgrown lining finally sheds, the result is dramatic. You experience a massive, clot-filled, and painful period. This state is often referred to as “Estrogen Dominance.” But in this context, it is secondary to the thyroid dysfunction. The ovaries aren’t necessarily making too much estrogen. The liver just isn’t clearing it.
C. Anovulation and Progesterone Deficiency
In a healthy cycle, ovulation triggers the production of progesterone. Progesterone changes the endometrium. It shifts it from a growing state to a stable state. It acts like glue for the uterine lining. It also promotes the production of vasoconstrictors (substances that constrict blood vessels) when the period begins. This limits blood loss.
Because hypothyroidism disrupts the HPO axis, anovulation is common. If you do not ovulate, you make zero progesterone. The lining continues to build under the influence of estrogen. It builds until it becomes unstable. Eventually, it collapses under its own weight.
This results in “breakthrough bleeding.” This flow is heavy. It is prolonged. It is unpredictable. This is a classic presentation of hypothyroidism and periods. You miss the “brake” pedal (progesterone), so the car (your period) crashes through the garage door.
Expert Insight: If you are passing clots larger than a quarter, this is a strong indicator of a coagulation defect or severe estrogen dominance. Do not ignore this sign. It requires immediate evaluation.
The Vicious Cycle: The Iron-Thyroid Feedback Loop
One of the most frustrating aspects of treating heavy menstrual bleeding is the feedback loop. It creates a self-perpetuating cycle with the thyroid. Heavy periods lead to iron loss. Iron loss leads to worse thyroid function. Worse thyroid function leads to heavier periods.
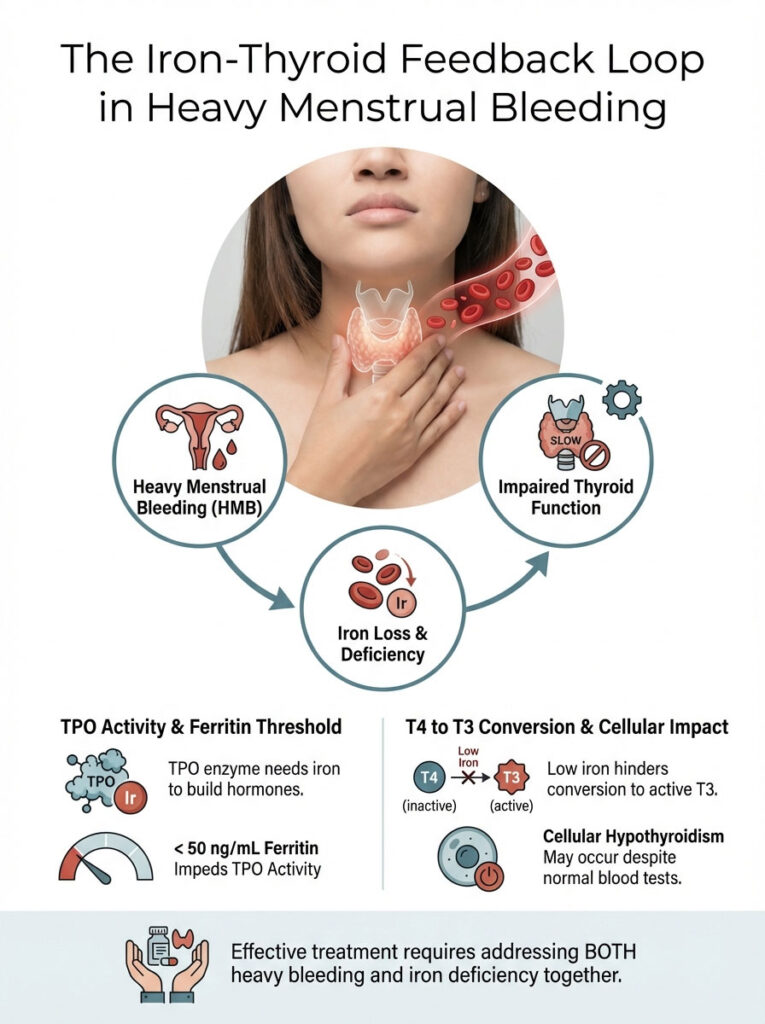
Here is why this matters biologically. The enzyme responsible for manufacturing thyroid hormones is called Thyroid Peroxidase (TPO). This enzyme is heme-dependent. This means it requires iron to function. If your ferritin (stored iron) drops below 50 ng/mL due to chronic blood loss, your TPO enzyme slows down. You produce less thyroid hormone.
Additionally, the body needs iron for conversion. You must convert the inactive T4 hormone (Levothyroxine) into the active T3 hormone. Low iron impairs this conversion. The result is cellular hypothyroidism. Your blood tests might look okay, but your cells are starving.
The result? Your heavy periods make you more hypothyroid. This in turn makes your periods heavier. We cannot fix the heavy menstrual bleeding without simultaneously aggressively treating the iron deficiency. I often have to use intravenous iron infusions for these patients. Oral iron is often insufficient to break the cycle.
Differential Diagnosis: Is it Thyroid, PCOS, or Perimenopause?
It is vital to distinguish thyroid issues from other common conditions. Conditions like PCOS or Perimenopause can look similar. However, the treatments are vastly different. Misdiagnosis leads to months of lost time.
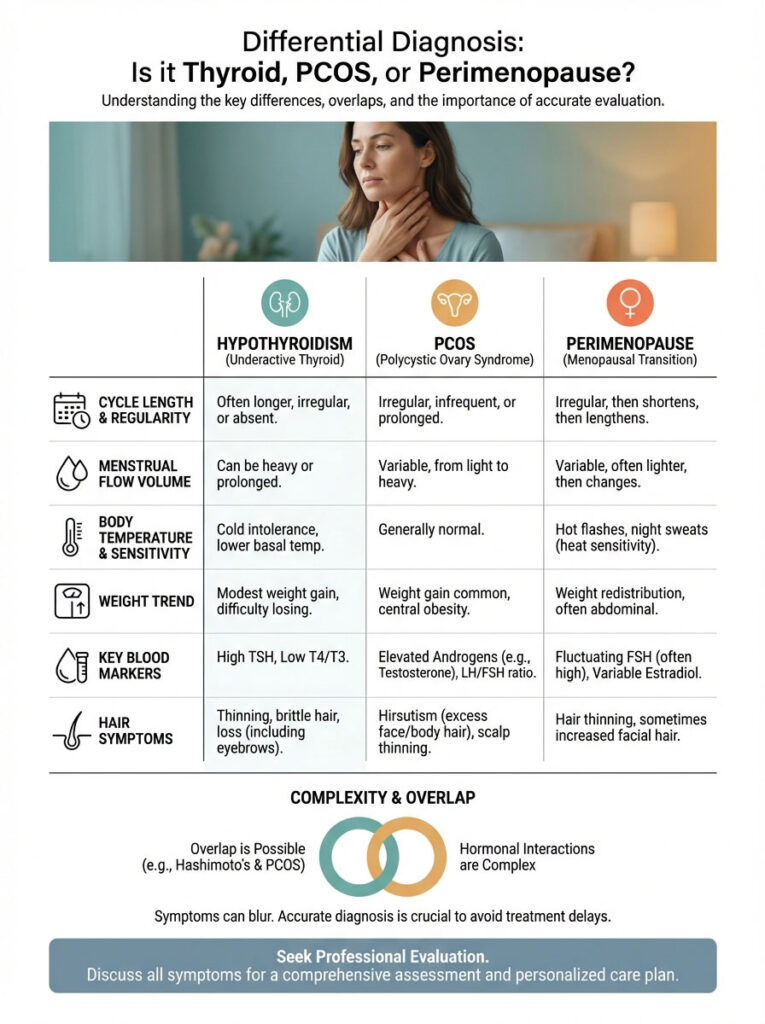
We need to look at the clinical features side-by-side. The nuance lies in the combination of symptoms. It is rarely just one thing.
COMPARISON TABLE 1: Differential Diagnosis of Menstrual Irregularities
| Clinical Feature | Hypothyroidism-Induced | PCOS (Polycystic Ovary Syndrome) | Perimenopause |
|---|---|---|---|
| Cycle Length | Often prolonged (>35 days) or irregular | Often absent (Amenorrhea) or very long cycles | Shortening cycles initially, then skipped |
| Flow Volume | Heavy (Menorrhagia) | Variable, often heavy when it arrives | Variable to heavy |
| Body Temperature | Consistently low (< 97.6°F) | Normal or slightly elevated | Fluctuating (Hot flashes) |
| Weight Trend | Generalized gain, fluid retention | Central/Abdominal weight gain | Weight gain around midsection |
| Key Blood Marker | High TSH, Low Free T4 | High Androgens (Testosterone), High LH:FSH ratio | High FSH, Low Estrogen |
| Hair Symptoms | Diffuse thinning, loss of outer eyebrow | Male-pattern hair growth (Hirsutism) | General thinning |
As you can see, the overlap is significant. It is also possible to have two conditions at once. I frequently see patients with both Hashimoto’s and PCOS. This creates a complex hormonal storm that requires a dual-pronged approach.
Hashimoto’s Thyroiditis: The Autoimmune Factor
In the United States, the majority of hypothyroidism cases are caused by Hashimoto’s Thyroiditis. This is an autoimmune disease. This adds a layer of complexity to the hypothyroidism and periods equation. Hashimoto’s involves systemic inflammation.
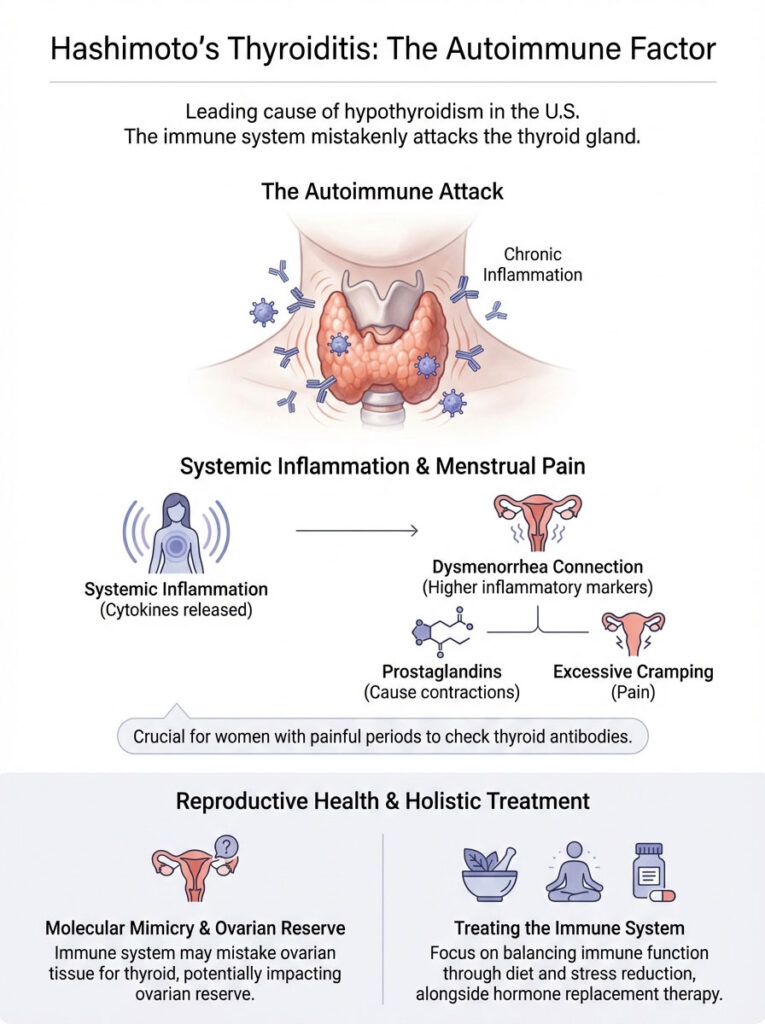
When your immune system attacks the thyroid, it releases inflammatory cytokines. These are chemical messengers of war. They circulate throughout the body. They eventually reach the uterus.
The Pain Connection (Dysmenorrhea)
These inflammatory markers stimulate the production of prostaglandins in the uterus. Prostaglandins are the chemicals that cause the uterus to contract to shed its lining. Excessive prostaglandins lead to Dysmenorrhea. This manifests as severe, cramping pain during menstruation.
If your periods are not just heavy but also excruciatingly painful, we must look at antibodies. We must lower the systemic inflammation to lower the pain. Ibuprofen helps, but it doesn’t stop the immune attack.
Molecular Mimicry and Ovarian Reserve
Furthermore, there is evidence of “molecular mimicry.” There is also cross-reactivity. Research suggests that in some women, the antibodies attacking the thyroid (TPO and TgAb) may also affect ovarian tissue. This can potentially impact ovarian reserve.
This is why addressing the immune component is critical. We often use diet (like gluten elimination) and stress reduction. This is as important as taking hormone replacement. We are treating the immune system, not just the gland.
Comprehensive Diagnostic Evaluation
If you walk into a doctor’s office with complaints of heavy menstrual bleeding and fatigue, they might only test your TSH. If they do, they are missing the full picture. TSH is merely a messenger. It does not tell us how much fuel is in the tank. It does not tell us how well the engine is running.
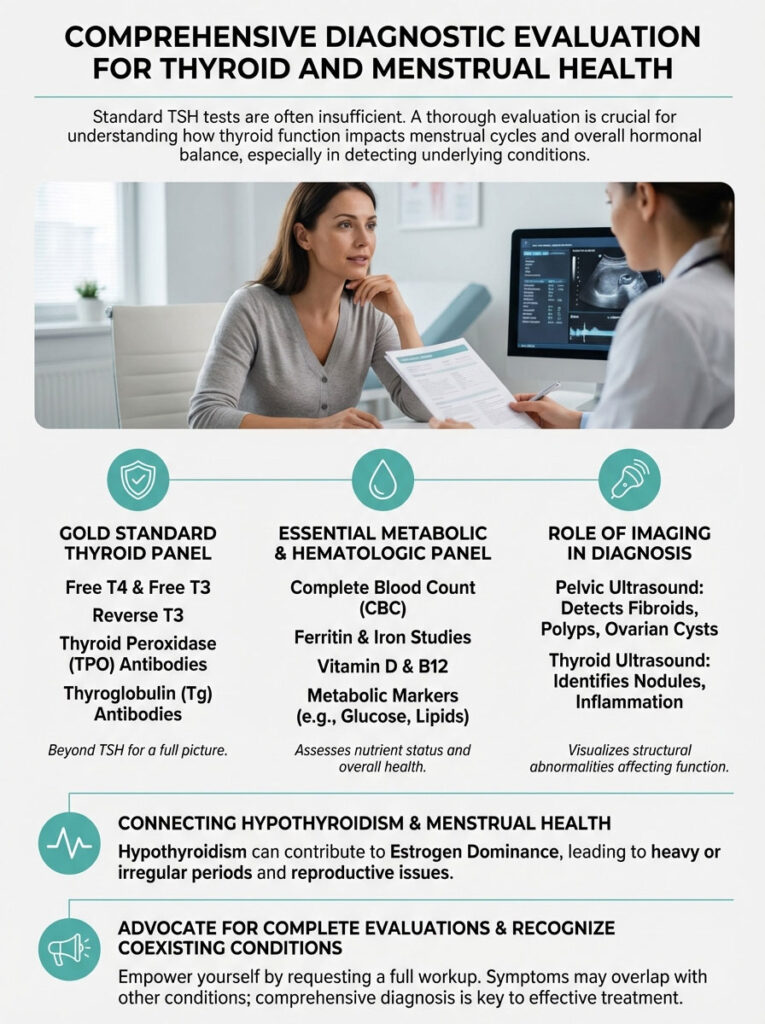
To truly understand the impact of your thyroid on your cycle, you need the “Gold Standard” panel. You must advocate for these specific markers.
The Essential Thyroid Panel
- TSH (Thyroid Stimulating Hormone): The pituitary signal. High means low function.
- Free T4 (Thyroxine): The storage hormone. It must be “Free” (unbound) to be useful.
- Free T3 (Triiodothyronine): The active hormone. This enters cells and regulates the ovaries.
- Reverse T3: The metabolic “brake.” High levels indicate stress, iron issues, or inflammation.
- Thyroid Antibodies (TPO & TgAb): To confirm or rule out Hashimoto’s.
The Essential Metabolic & Hematologic Panel
- Ferritin: Essential for ruling out the iron-deficiency loop. In my practice, I look for levels above 50-70 ng/mL for optimal hair growth and thyroid function.
- CBC (Complete Blood Count): To check hemoglobin and platelet function.
- Prolactin: To ensure TRH hasn’t spiked this hormone and shut down ovulation.
- SHBG: To check for estrogen dominance potential.
Imaging Considerations
Imaging is also relevant. A pelvic ultrasound is often necessary. We must ensure that the heavy bleeding isn’t being caused by uterine fibroids or polyps. These can coexist with thyroid dysfunction. Interestingly, some studies suggest that the estrogen dominance caused by hypothyroidism may actually fuel fibroid growth.
Medical Management and Recovery Timeline
The good news is that hypothyroidism and periods are highly responsive to treatment. Unlike conditions that require surgery, this is a biochemical problem. It has a biochemical solution. We just need to find the right dosage.
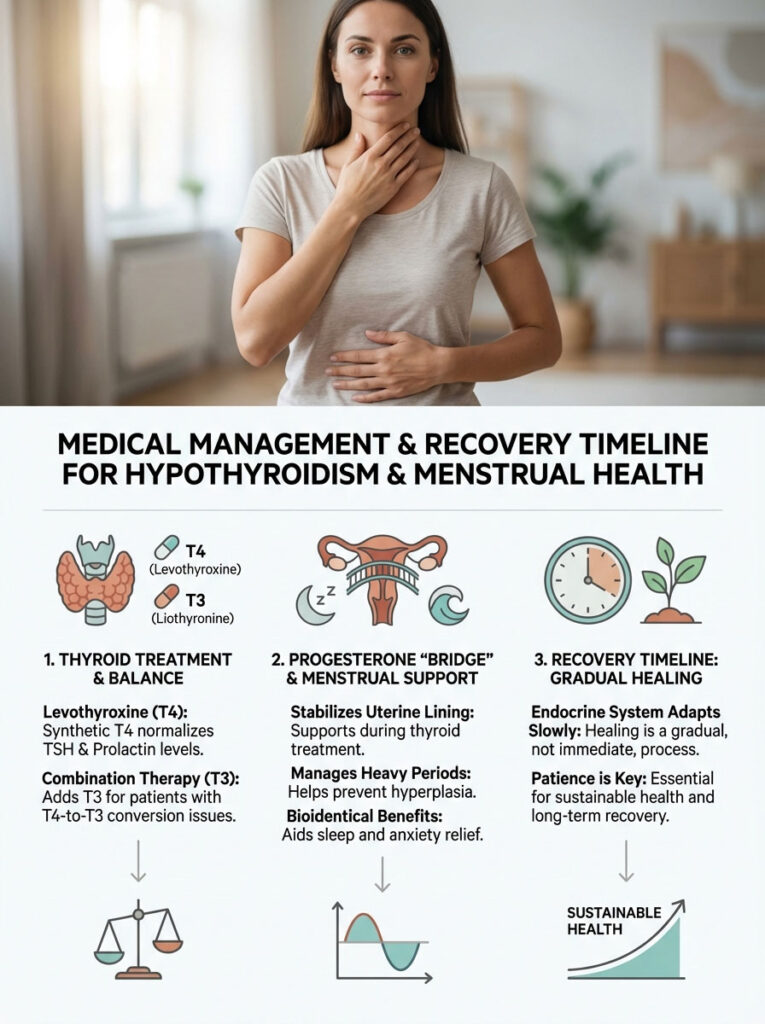
Levothyroxine and Combination Therapy
Standard treatment involves Levothyroxine (synthetic T4). By normalizing T4 levels, we lower TSH. We reduce the overproduction of Prolactin. This allows the HPO axis to reset. GnRH can pulse normally again. Ovulation resumes.
However, some patients have trouble converting T4 to T3. This is common in those with heavy periods and low iron. For these women, I often prescribe Combination Therapy. I add Liothyronine (T3) to the regimen. This ensures the ovaries receive the active hormone they need immediately. We bypass the conversion bottleneck.
The Progesterone “Bridge”
While waiting for the thyroid medication to work, we cannot let a patient bleed out. I frequently use bioidentical progesterone during the luteal phase (days 14-28 of the cycle). This stabilizes the uterine lining. It prevents hyperplasia.
This acts as a bridge. It ensures a lighter, more controlled bleed while the thyroid heals. It also helps with sleep and anxiety, which are common hypothyroid symptoms. It is a temporary measure with long-term benefits.
The Recovery Timeline
Patience is required. The endocrine system is slow to turn. It is like a large ship, not a speedboat.
- Month 1: Biochemical improvement. Blood levels of T4 and T3 stabilize.
- Month 2: Symptomatic relief. Energy improves. Fluid retention decreases.
- Month 3: Menstrual regulation. This is typically when we see the heavy menstrual bleeding subside. Cycle length normalizes. Anovulation resolves.
Fertility Implications and TSH Targets
Many of my patients are trying to conceive. They are terrified that their heavy periods mean they are infertile. This is rarely the case permanently. However, untreated hypothyroidism poses risks for miscarriage and implantation failure.
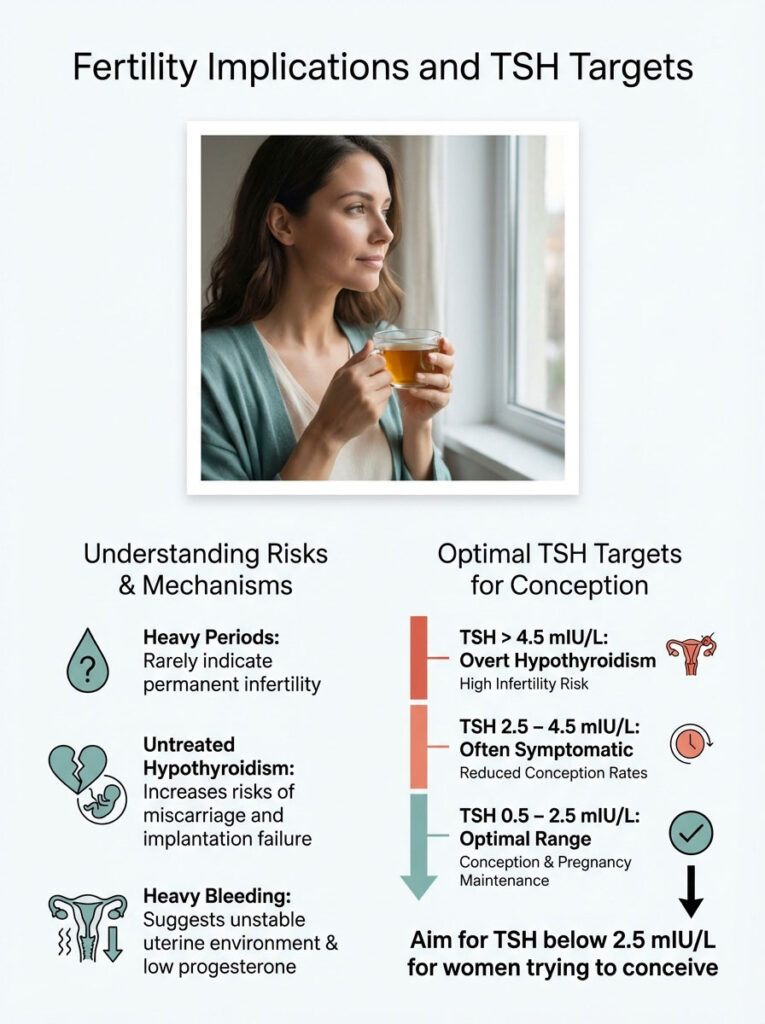
The heavy bleeding indicates the uterine environment is not optimal. The lining is unstable. The clotting factors are low. The progesterone is missing. This makes implantation difficult.
COMPARISON TABLE 2: Impact of TSH Levels on Reproductive Health
Your lab report might say your TSH is “normal.” But normal is not optimal. This is especially true for reproductive health. The ranges for fertility are much tighter.
| TSH Range (mIU/L) | Clinical Interpretation | Impact on Menstrual Cycle | Fertility Implication |
|---|---|---|---|
| > 4.5 | Overt Hypothyroidism | High risk of Menorrhagia, Anovulation, and long cycles | High risk of infertility and miscarriage |
| 2.5 – 4.5 | Subclinical Hypothyroidism | “Normal” by lab standards but often symptomatic; irregular spotting | Reduced conception rates; potential implantation failure |
| 0.5 – 2.5 | Optimal Therapeutic Range | Regular ovulation; stabilized lining; normal flow | Ideal for conception and pregnancy maintenance |
| < 0.4 | Hyperthyroidism Risk | Scanty periods (Hypomenorrhea), lighter flow, anxiety | Risk of implantation failure due to hyper-metabolism |
We aim for a TSH below 2.5 mIU/L for any woman trying to conceive. This provides the safest buffer for early pregnancy demands.
Holistic and Lifestyle Interventions
While medication is the cornerstone of treatment for hypothyroidism and periods, lifestyle factors play a significant supporting role. We must create an environment where the thyroid can thrive. You cannot medicate your way out of a poor lifestyle.
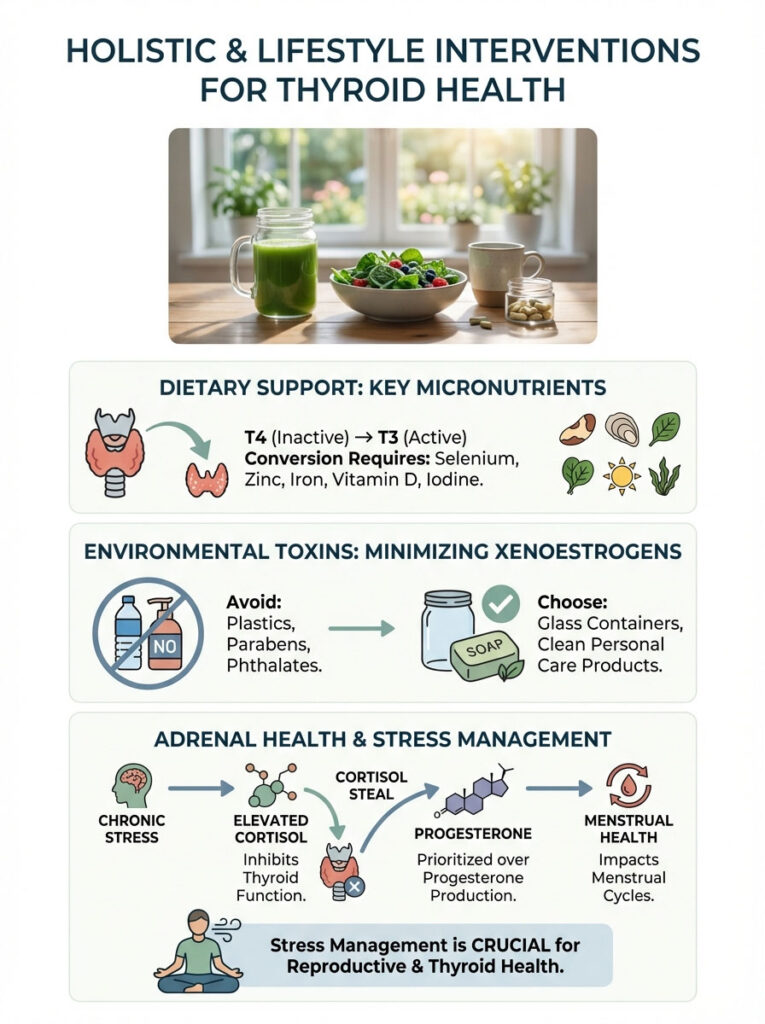
Dietary Support for Conversion
The thyroid needs specific micronutrients to convert T4 into the active T3. Without these, your medication may not work effectively.
- Selenium: Acts as a cofactor for the deiodinase enzymes. These enzymes activate thyroid hormone. Brazil nuts are a potent source.
- Zinc: Essential for TSH synthesis and receptor sensitivity. It also supports follicle health in the ovaries.
- Myo-Inositol: Particularly helpful for women with overlapping PCOS and thyroid issues. Inositol improves insulin sensitivity. It supports regular ovulation.
Environmental Toxins and Xenoestrogens
We must address endocrine disruptors. Specifically, we look for xenoestrogens found in plastics, parabens, and phthalates. These chemicals mimic estrogen in the body. They worsen the estrogen dominance that already exists due to low SHBG.
I advise patients to switch to glass containers. Use “clean” personal care products. This reduces the total estrogen load on the uterus. It gives the liver a break. It allows SHBG to catch up.
Stress Management: The Cortisol Steal
Adrenal health is inextricably linked to thyroid health. High cortisol (stress hormone) suppresses TSH production. It blocks the conversion of T4 to T3. Furthermore, the body uses the same raw materials (pregnenolone) to make both cortisol and progesterone.
When you are chronically stressed, your body prioritizes survival (cortisol) over reproduction (progesterone). We call this the “Cortisol Steal.” This exacerbates the progesterone deficiency that causes heavy menstrual bleeding. Managing stress is not a luxury. It is a medical necessity for your cycle.
Summary & Key Takeaways
Your period is a vital sign. If you are suffering from heavy menstrual bleeding, clots, or irregular cycles, do not accept it as your fate. It is often a systemic cry for help. It signals that your thyroid is underactive. The connection between hypothyroidism and periods is undeniable. It is rooted in coagulation defects, hormonal imbalances, and failed ovulation.
The Patient Checklist:
- Don’t Normalize the Bleeding: Soaking a pad or tampon in less than two hours is a medical issue. It requires investigation.
- Demand the Full Panel: TSH alone is insufficient. Request Free T3, Free T4, and TPO antibodies.
- Check Your Iron: Ferritin must be tested. If it is low, thyroid medication alone will not fix the problem. You need iron to make thyroid hormone work.
- Trust the Timeline: Expect a 3-month window for your cycle to regulate once medication is started. Be patient with your body.
- Monitor for Ovulation: Use basal body temperature or test strips. Confirming ovulation is the best sign that your treatment is working.
Correcting your thyroid function often eliminates the need for invasive procedures. We can often avoid ablation or hysterectomy. By treating the root cause, we restore not just your energy. We restore your reproductive rhythm.
Frequently Asked Questions
Why does hypothyroidism cause heavy menstrual bleeding?
Hypothyroidism triggers heavy flow through a “triple-threat” mechanism: it reduces the production of essential blood-clotting proteins, lowers SHBG which causes estrogen dominance, and often prevents ovulation. Without enough thyroid hormone, the uterine lining thickens excessively and lacks the progesterone “brake” needed to regulate shedding, leading to menorrhagia.
How can I tell if my heavy periods are due to thyroid dysfunction or perimenopause?
While both conditions cause irregular bleeding, thyroid-induced issues often present with low basal body temperature, fluid retention, and diffuse hair thinning. Perimenopause is typically characterized by hot flashes and elevated FSH levels, whereas hypothyroidism is confirmed through high TSH and low Free T4/T3 markers.
What thyroid labs are necessary to evaluate menstrual irregularities?
To get a full clinical picture, you must look beyond a simple TSH test and request Free T4, Free T3, Reverse T3, and Thyroid Antibodies (TPO and TgAb). These markers reveal how well your body is converting hormones and whether autoimmune inflammation from Hashimoto\’s is disrupting your reproductive axis.
Can an underactive thyroid prevent ovulation?
Yes, hypothyroidism frequently leads to anovulation by disrupting the Hypothalamic-Pituitary-Ovarian (HPO) axis. When thyroid levels are low, the brain releases excess Thyrotropin-Releasing Hormone (TRH), which inadvertently spikes Prolactin levels and shuts down the GnRH pulses required for the ovaries to release an egg.
Why do I have large blood clots in my period flow when my thyroid is low?
Large clots are a hallmark of a thyroid-induced coagulation deficit or severe estrogen dominance. Because hypothyroidism slows the synthesis of clotting factors like Factor VII and VIII in the liver, your body struggles to stem the blood flow effectively, allowing large clots to form as the thickened uterine lining sheds.
How does iron deficiency affect thyroid function and menstrual flow?
This creates a dangerous feedback loop where heavy periods deplete your iron stores, and low ferritin then impairs the Thyroid Peroxidase (TPO) enzyme needed to make thyroid hormone. Without adequate iron, you also cannot convert T4 into the active T3 hormone, which further slows your metabolism and makes your periods even heavier.
When will my periods become lighter after starting thyroid medication?
While biochemical levels may stabilize within a month, it typically takes about three full menstrual cycles (90 days) for the HPO axis to reset and for the flow to lighten. This timeline allows for the resolution of endometrial hyperplasia and the restoration of a regular ovulatory rhythm.
What is the ideal TSH range for fertility and regular cycles?
For optimal reproductive health and regular ovulation, most reproductive endocrinologists aim for a TSH between 0.5 and 2.5 mIU/L. Levels above 2.5, even if labeled “normal” by standard labs, are associated with higher risks of anovulation, implantation failure, and early miscarriage.
Does Hashimoto’s Thyroiditis make period cramps worse?
Yes, the systemic inflammation associated with Hashimoto’s increases the production of prostaglandins in the uterine tissue. These chemicals trigger more intense uterine contractions, leading to severe dysmenorrhea (painful cramping) in addition to the heavy bleeding caused by the thyroid hormone deficiency itself.
Why is progesterone deficiency common in hypothyroid women?
Progesterone is only produced in significant amounts after ovulation occurs via the corpus luteum. Because hypothyroidism often prevents a healthy follicle from maturing, ovulation fails to happen, leaving the body without the progesterone needed to stabilize the uterine lining and limit blood loss during menstruation.
Could I still have thyroid-related period issues if my TSH is normal?
Absolutely, as you may have a “cellular hypothyroidism” or a conversion issue where your body isn\’t effectively turning T4 into active T3. If your Free T3 is low or your Reverse T3 is high, your ovaries may not be receiving the metabolic signal they need to function correctly, regardless of a normal TSH reading.
What supplements support thyroid health and menstrual regulation?
Selenium and zinc are essential cofactors for the deiodinase enzymes that activate thyroid hormone, while Myo-inositol can help improve insulin sensitivity and support regular ovulation. Additionally, maintaining ferritin levels above 50-70 ng/mL is crucial for ensuring your thyroid medication can actually work at the cellular level.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The connection between hypothyroidism and periods involves complex endocrine pathways; always consult a qualified reproductive endocrinologist or healthcare professional before beginning new treatments or interpreting lab results.
References
- American Thyroid Association – thyroid.org – Detailed statistics on thyroid disorders in women and their impact on reproductive health.
- The Endocrine Society – Journal of Clinical Endocrinology & Metabolism – Research regarding the HPO axis and thyroid hormone’s role in ovarian sensitivity.
- Mayo Clinic – mayoclinic.org – Clinical overview of menorrhagia (heavy menstrual bleeding) and systemic causes like thyroid disease.
- American College of Obstetricians and Gynecologists (ACOG) – Practice Bulletin on Management of Abnormal Uterine Bleeding – Guidelines on screening for thyroid dysfunction.
- National Institutes of Health (NIH) – PubMed Central – Studies on the link between subclinical hypothyroidism and coagulation factor deficiencies (Factor VII, VIII).
- Fertility and Sterility Journal – Research paper on the impact of TSH levels on implantation success and menstrual regularity.
- Cleveland Clinic – clevelandclinic.org – Information on the relationship between ferritin, iron deficiency, and thyroid peroxidase (TPO) function.