Quick Summary: Congenital hypothyroidism is a condition babies are born with where the thyroid gland is either missing, too small, or unable to make enough thyroid hormone. That hormone is essential. It fuels brain development and physical growth. The good news? Newborn screening catches it early. When treatment with levothyroxine starts within the first two weeks of life, children with congenital hypothyroidism grow up healthy, hit all their milestones, and reach their full intellectual potential.
Table of Contents
When the Phone Call Changes Everything
The phone rings. It’s your pediatrician. They ask if you have a minute. Your stomach drops. And then you hear it: “Your baby’s newborn screening came back abnormal.”
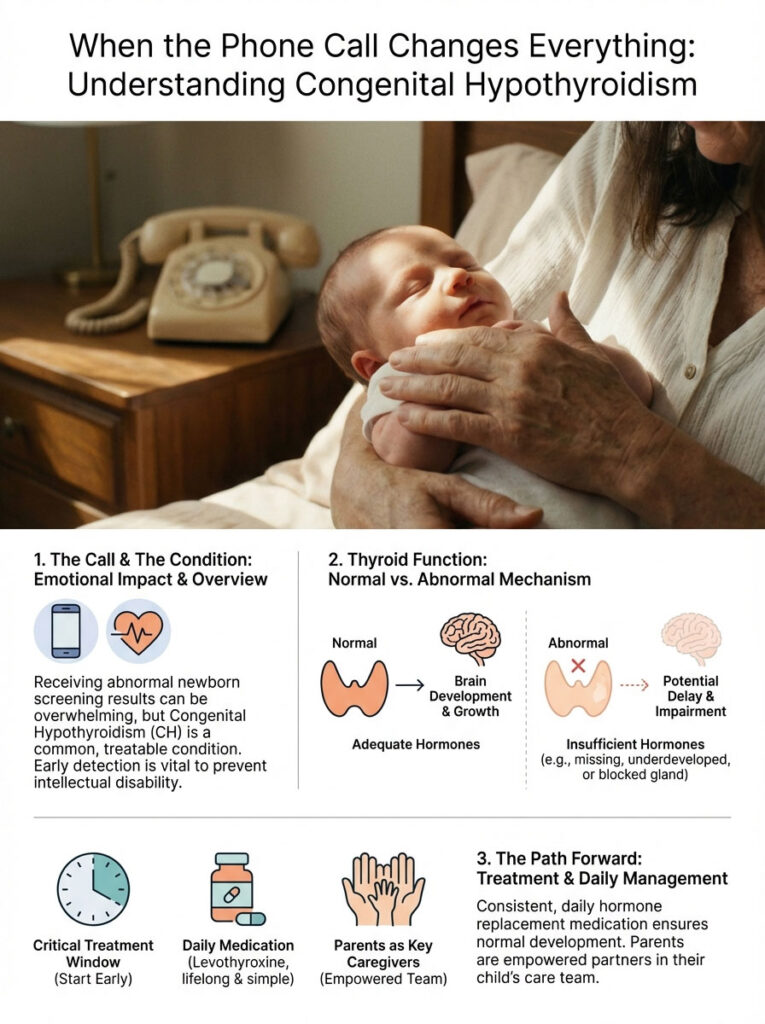
If that’s how you ended up here, I get it. Maybe you’re sitting in a waiting room right now, or maybe you’re holding a baby who looks completely fine and wondering how anything could possibly be wrong.
I’ve been on the other side of this conversation thousands of times. And here’s what I always tell parents first: take a breath. Congenital hypothyroidism is one of the most treatable conditions in all of pediatrics. The fact that it was caught means your child is going to be okay.
This is actually the most common preventable cause of intellectual disability worldwide. The key word there is preventable. After nearly two decades as a pediatric endocrinologist, I don’t see this diagnosis as bad news. I see it as modern medicine doing exactly what it’s supposed to do, catching a problem early and fixing it.
This guide is your roadmap. We’ll cover how your baby’s thyroid works, what went wrong, the critical treatment window, and how to give the medication day to day. You’re now the most important person on your child’s care team. Let’s get started.
Key Statistics at a Glance
- 1 in 2,000 to 1 in 4,000 newborns are affected by congenital hypothyroidism
- 85% of cases are caused by thyroid dysgenesis (the gland didn’t form correctly)
- 14 days: the “Golden Window” to start treatment and protect normal brain development
- 10-15 mcg/kg: the typical starting dose of levothyroxine for newborns
- 7 days: the approximate half-life of T4 in the blood
- 2:1 female-to-male ratio in thyroid dysgenesis cases
How Your Baby’s Thyroid Works (And Why It Matters So Much)
Before we talk treatment, it helps to understand the basics. The thyroid is a small, butterfly-shaped gland sitting at the base of the neck. In a healthy baby, it acts like the body’s engine controller. It regulates heart rate, metabolism, and most importantly for infants, it drives brain development.
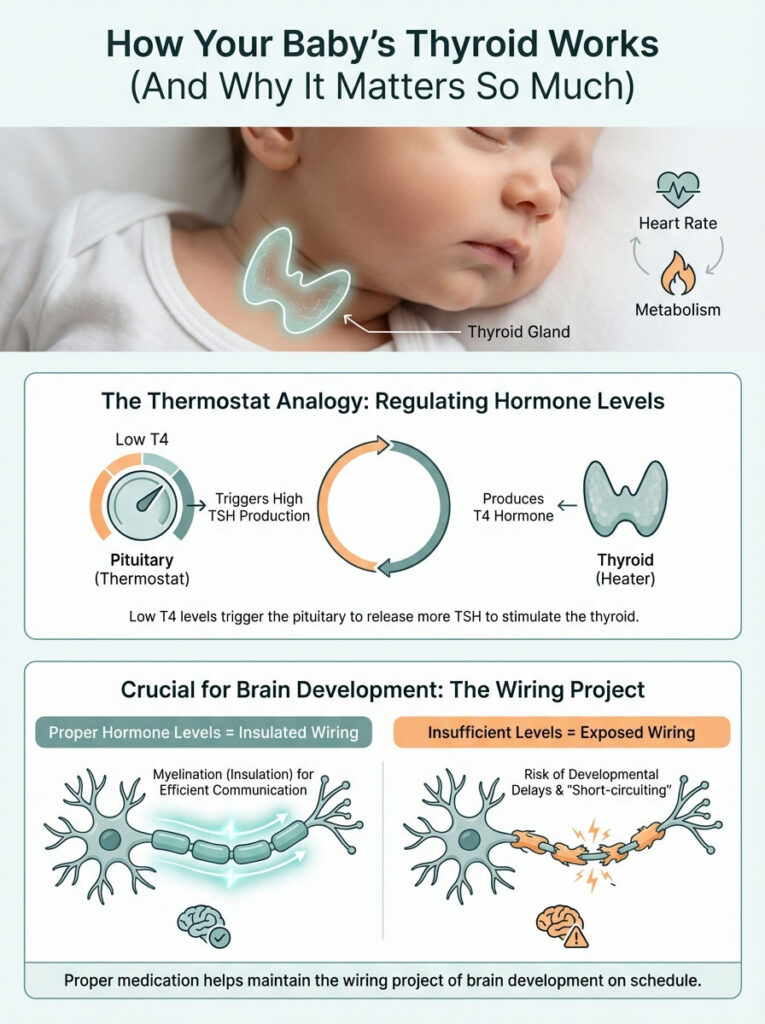
The Thermostat Analogy
I explain the thyroid system to parents using a thermostat analogy. It makes the lab numbers much easier to understand.
- The House (your baby’s body): Needs heat to function properly.
- The Furnace (the thyroid gland): Produces the heat. In this case, the “heat” is thyroid hormone, specifically T4.
- The Thermostat (the pituitary gland): Sits in the brain and constantly monitors how much T4 is circulating.
- The Signal (TSH): Thyroid Stimulating Hormone. Think of it as the wire connecting the thermostat to the furnace.
Here’s how this plays out clinically. When T4 levels drop too low, the pituitary goes into overdrive and floods the system with TSH, essentially screaming at the thyroid to produce more hormone. That’s why a high TSH reading means the thyroid is underperforming. The brain is demanding hormone that the gland can’t deliver.
Why Thyroid Hormone Is Non-Negotiable for Brain Development
In babies, thyroid hormone isn’t just about metabolism. It’s about building the brain’s wiring. Specifically, it’s needed for myelination, the process of coating nerve fibers with a protective insulation called myelin. Without enough hormone during the first three years of life, those nerve connections don’t insulate properly, and signals travel too slowly. That’s the biological reason untreated cases can lead to developmental delays.
Think of it like a huge wiring project. Thyroid hormone provides the coating for the wires. No coating, and the wires short-circuit. By giving the medication, we supply the coating, and the wiring project stays on schedule.
What Causes Congenital Hypothyroidism?
This is one of the first things parents ask me: “What did I do wrong?” The answer, in nearly every case, is nothing. Most cases of congenital hypothyroidism happen randomly during fetal development. There’s no food you ate, no activity you did, no choice you made that caused this. We group the causes into two main categories.
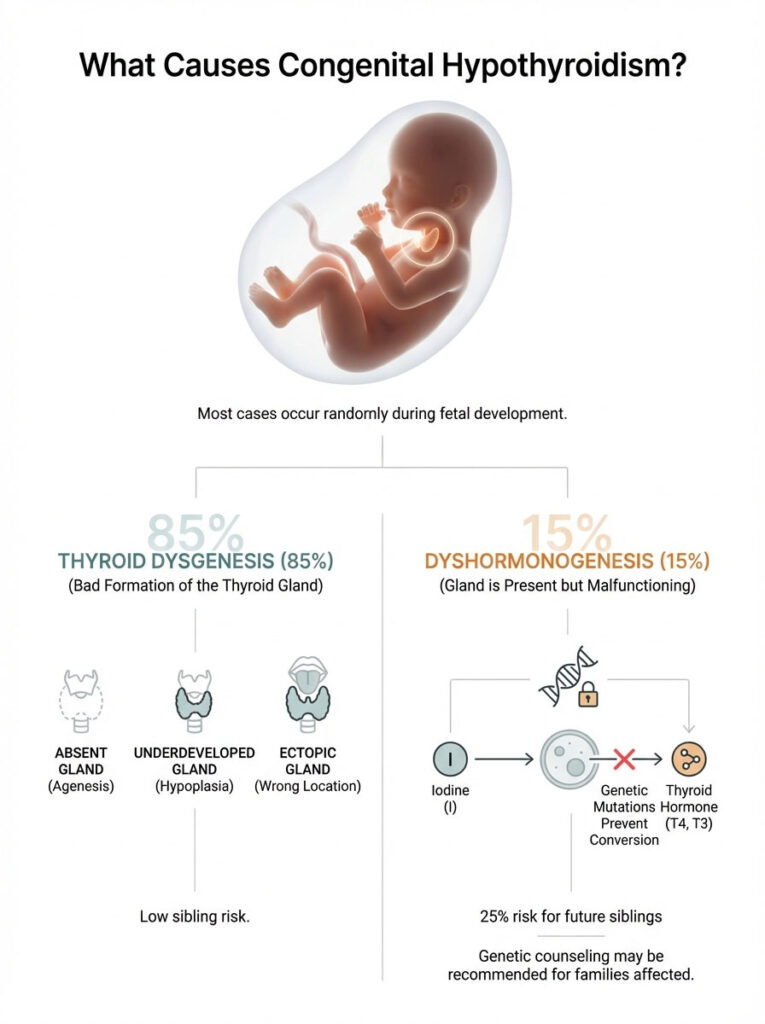
Thyroid Dysgenesis (About 85% of Cases)
This literally means “bad formation.” The thyroid gland didn’t develop properly during the early weeks of pregnancy. It shows up in three ways:
- Agenesis: The baby is born without a thyroid gland at all.
- Ectopic gland: The gland formed but migrated to the wrong spot, often ending up at the back of the tongue (called a lingual thyroid). These misplaced glands are usually too small to keep up with demand.
- Hypoplasia: The gland is in the right location but is underdeveloped and too small to function adequately.
Dyshormonogenesis (About 15% of Cases)
In these babies, the thyroid gland is present, and sometimes even enlarged, but the internal machinery is faulty. Genetic mutations prevent the gland from converting iodine into usable thyroid hormone. Unlike dysgenesis, this form is hereditary and follows a recessive inheritance pattern.
Worth knowing: If your child has thyroid dysgenesis (a missing or misplaced gland), the chance of a future sibling having the same condition is very low, roughly the same as the general population. But if your child has dyshormonogenesis, each future sibling has a 25% chance. That’s why genetic counseling may be recommended.
How Congenital Hypothyroidism Is Diagnosed
The Newborn Screening Process
In the United States, every baby undergoes a heel prick test (Newborn Screening or NBS) between 24 and 48 hours after birth. This is the safety net that catches congenital hypothyroidism early enough to prevent lasting damage.

Timing matters here. Newborns experience a natural surge in TSH right after birth due to the temperature shock of entering the world. Testing too early (before 24 hours) produces false positives. Testing too late risks losing precious treatment time.
Different states use different screening methods. Some check T4 first, others lead with TSH. Either way, the goal is the same: flag any baby whose thyroid levels fall outside safe margins. An abnormal screening result doesn’t always mean permanent disease, but it does require immediate follow-up.
Confirmatory Blood Work
When your doctor calls about an abnormal screen, the next step is a venous blood draw. The heel prick filter paper isn’t precise enough for diagnosis. We need actual blood levels. The pattern we look for:
- Elevated TSH: Usually above 20 mIU/L (though labs vary slightly).
- Low Free T4: This confirms the body isn’t getting the thyroid hormone it needs.
Sometimes TSH is high but T4 is still in the normal range. We call this compensated hypothyroidism. The gland is struggling but barely hanging on. We still treat these cases because the gland will eventually fail as the baby grows.
Imaging the Thyroid Gland
Your doctor may order a thyroid ultrasound or a nuclear medicine uptake scan. The ultrasound is non-invasive and shows whether the gland is in the neck. The uptake scan uses a tiny amount of tracer to locate ectopic glands, like those hidden at the base of the tongue. Knowing the anatomy helps predict whether the condition is permanent or transient.
The “Golden Window”: Why Starting Treatment Fast Matters
In pediatric endocrinology, we talk about the “Golden Window,” which refers to the first 14 days of life. Research from the New England Collaborative and other landmark studies shows a clear outcome difference based on when treatment begins.

Why the First Two Weeks Are Critical
Babies who start levothyroxine within the first two weeks of life have IQ scores that are statistically identical to their peers without the condition. When treatment is delayed beyond a month, subtle deficits in attention, memory, and verbal processing start to appear. That’s why we move fast. There’s no “wait and see” approach with congenital hypothyroidism.
Levothyroxine: Simple, Effective, Essential
The treatment is beautifully straightforward. We replace what the body can’t make on its own. Levothyroxine is synthetic T4, bio-identical to the hormone a healthy thyroid produces. When you give this to your baby, you’re not medicating them in the way most people think of medication. You’re completing their biology.
Infant dosing is aggressive by design. We typically start at 10 to 15 micrograms per kilogram of body weight, roughly ten times the weight-adjusted adult dose. Babies burn through thyroid hormone rapidly because their growth rate is so high.
How to Give Levothyroxine to a Newborn (Step by Step)
This is the part that scares most parents. How do you get a pill into a week-old baby? In the US, levothyroxine usually comes in tablet form. Liquid versions exist but are often not covered by insurance or lack long-term stability data. Here’s the technique I teach in my clinic:
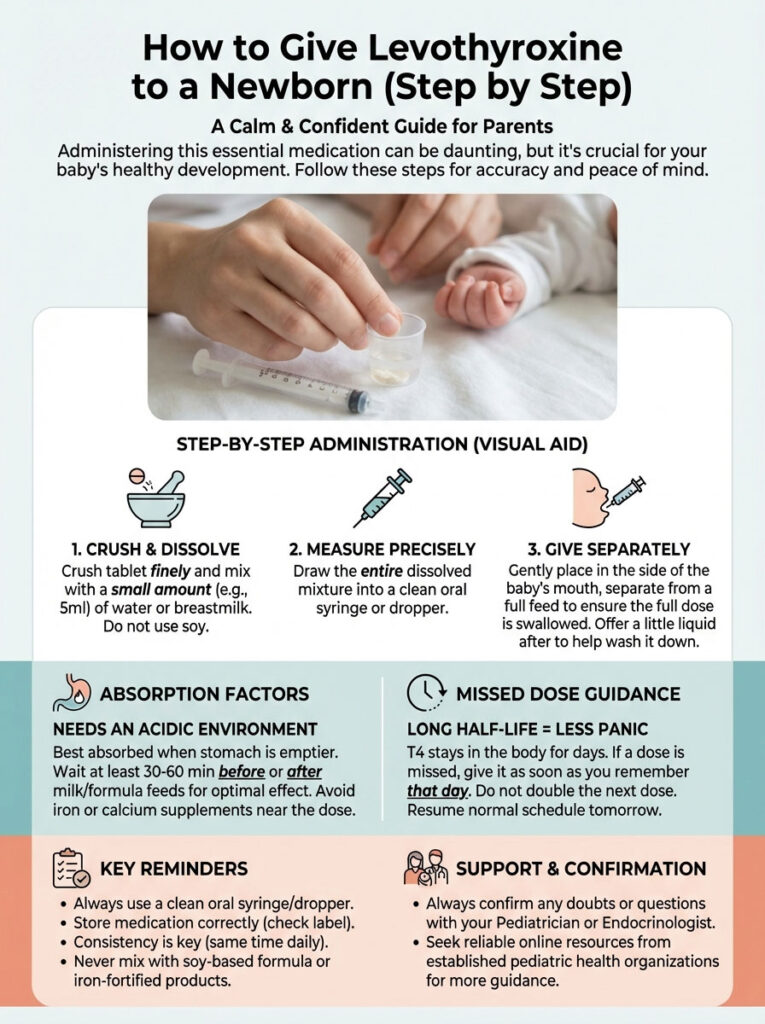
- Crush: Place the tablet between two metal spoons and press firmly to create a fine powder. A pill crusher works too, but spoons are perfectly fine.
- Mix: Add the powder to a small volume of liquid, about 1 to 2 milliliters. Breast milk, formula, or water all work.
- Draw: Pull the mixture into a small oral syringe, or collect it on a clean finger.
- Place: Squeeze or wipe the mixture into the side of the baby’s cheek (the buccal pouch). Don’t squirt it straight to the back of the throat. That triggers gagging.
- Chase: Follow immediately with a regular feeding to wash it down.
Critical tip: Never put the medication into a full bottle. If the baby only finishes half, they only get half the dose. Always give the medication separately so you know the full dose was consumed.
What Interferes with Absorption
Levothyroxine is a finicky molecule. It needs an acidic environment and doesn’t play well with certain binding agents that trap it in the stomach before it can reach the bloodstream.
- Soy formula: Soy protein binds to thyroxine. If your baby needs soy formula, it doesn’t mean they can’t take the medication. It means we may need to increase the dose to compensate. Let your endocrinologist know if you switch formulas.
- Iron and calcium supplements: These minerals bind to levothyroxine like magnets. Separate them from the thyroid dose by at least four hours.
What If You Miss a Dose?
You’re a new parent. You’re exhausted. It happens. The good news is that T4 has a long half-life, about seven days. One missed dose won’t cause a crisis. Give it as soon as you remember. If you’ve already reached the next day, it’s generally safe to double up. But always confirm with your doctor first.
Brand Name vs. Generic Levothyroxine: What Parents Should Know
You’ll likely run into this question at the pharmacy. It’s a real debate in the thyroid world, and it matters more for babies than it does for adults.

The Narrow Therapeutic Index
Levothyroxine is classified as a narrow therapeutic index drug. That means even small changes in the amount absorbed can meaningfully affect blood levels. Because infants are so small, a minor variance in the pill can translate to a big variance in their lab results.
Why Consistency Matters
The American Thyroid Association recommends consistency above all else. Brand-name formulations (Synthroid, Unithroid, Tirosint-Sol) are manufactured with very tight quality controls. Generics are FDA-approved and effective, but different manufacturers use different fillers, and those fillers can affect absorption slightly.
Here’s the real risk: if your pharmacy switches from one generic manufacturer to another between refills, the absorption may shift. For a 150-pound adult, that’s a minor issue. For an 8-pound baby, it can change lab results.
My recommendation: If your insurance covers brand name, use it. If you need generic, ask your pharmacist to keep you on the same manufacturer for every refill. If they do switch, tell your doctor. We may want to check labs sooner than usual.
Monitoring During the First Year: Blood Work and Growth
Once treatment starts, the big question shifts from “What is this?” to “Is it working?” We track this closely.
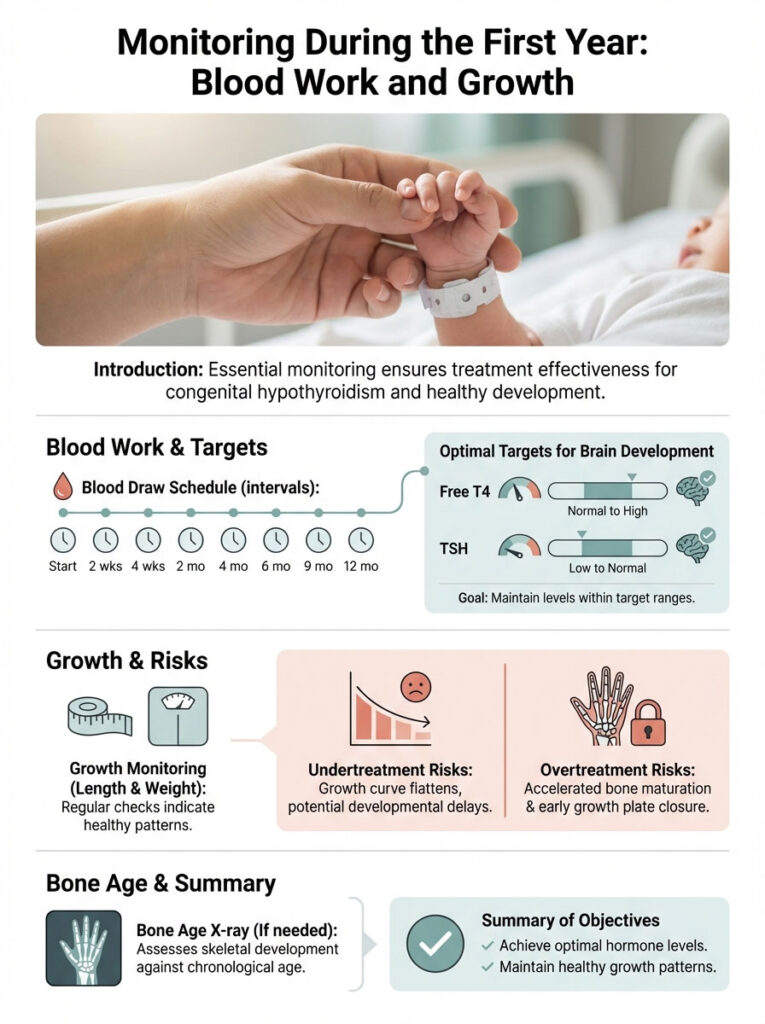
The Blood Draw Schedule
Expect to become very familiar with your phlebotomist. Standard guidelines call for labs at these intervals:
- Two weeks after starting treatment
- Four weeks after starting treatment
- Every 1 to 2 months during the first 6 months
- Every 3 to 4 months between 6 months and 3 years of age
The goal is to keep Free T4 in the upper half of the normal range and TSH in the lower half. This aggressive target makes sure the brain has plenty of fuel during this critical developmental period.
Tracking Growth and Bone Age
We monitor length and weight carefully. A child whose congenital hypothyroidism is undertreated will show a flattening growth curve. Overtreatment, on the other hand, can accelerate bone maturation and cause growth plates to close prematurely. Occasionally, we order a bone age X-ray of the left hand and wrist to confirm that skeletal development is keeping pace with the child’s actual age.
Transient vs. Permanent Congenital Hypothyroidism
Not every baby diagnosed with congenital hypothyroidism will need lifelong medication. Some cases are transient, meaning the condition resolves on its own. This can happen when maternal antibodies cross the placenta and temporarily suppress the baby’s thyroid, or when the baby is exposed to excess iodine (often from antiseptics) during delivery.
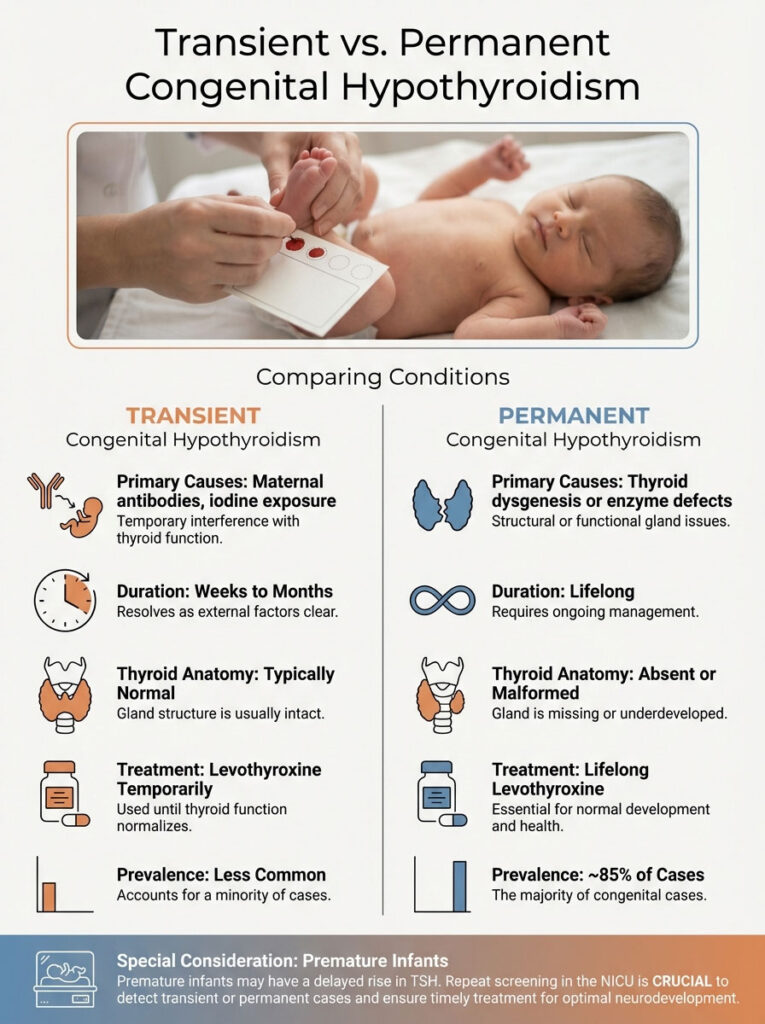
When the gland looks normal on ultrasound but lab numbers are off, we treat until age 3. At that point, when brain development is less dependent on thyroid hormone, we may stop the medication for a few weeks and retest. If TSH shoots back up, the condition is permanent. If it stays normal, the child is cured.
Transient vs. Permanent Congenital Hypothyroidism
| Feature | Transient | Permanent |
| Primary Cause | Maternal antibodies, iodine exposure, prematurity | Thyroid dysgenesis or enzyme defects |
| Duration | Weeks to months; typically resolves by age 3 | Lifelong medication required |
| Thyroid Anatomy | Usually normal size and location | Absent, ectopic, or malformed |
| Treatment | Levothyroxine temporarily | Levothyroxine for life |
| Prevalence | Less common | More common (~85% of cases) |
A Note on Premature Infants
Preemies are a special case. Their HPT axis is often immature, which can cause what we call a “delayed TSH rise.” The first screening may come back normal, but the second one flags an issue. That’s why repeat screening is standard practice in the NICU.
Signs of Over-Treatment vs. Under-Treatment
Lab work is the gold standard, but parents should also watch for these clinical signs between appointments:

| Category | Under-Treatment (Hypo) | Over-Treatment (Hyper) |
| Sleep | Excessive sleeping, hard to wake | Insomnia, restless sleep |
| Digestion | Constipation | Diarrhea, frequent stools |
| Behavior | Lethargic, unusually quiet | Irritable, jittery, flushed skin |
| Heart Rate | Slow pulse (bradycardia) | Fast pulse (tachycardia) |
Developmental Milestones to Watch For
With proper treatment, your child should hit milestones right on schedule. That said, keeping an eye on development helps us confirm the dose is doing its job.
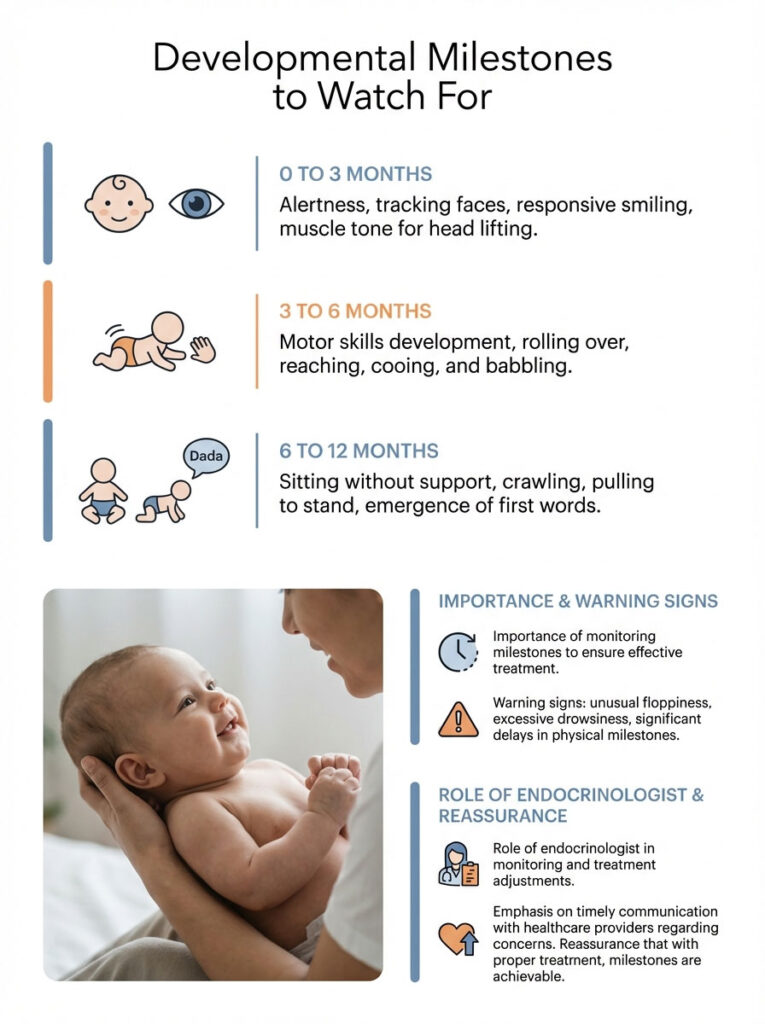
0 to 3 Months
Look for alertness. A well-treated baby should track faces with their eyes, begin smiling responsively, and have enough muscle tone to briefly lift their head during tummy time. If your baby seems unusually floppy or too drowsy to feed, call your endocrinologist.
3 to 6 Months
Motor skills pick up here. Rolling over, reaching for objects, bringing things to the mouth. These are all expected. You should also hear cooing and babbling, which are healthy signs of developing language.
6 to 12 Months
Sitting without support, crawling, and pulling to stand typically happen during this window. First words usually appear around the one-year mark. If your child is significantly behind on physical milestones, we’ll check thyroid levels right away to rule out under-treatment.
The Emotional Side: Coping with Your Baby’s Diagnosis
We spend a lot of time talking about TSH and T4. We don’t talk nearly enough about the parents. Getting a chronic condition diagnosis in the first week of your child’s life is jarring. It disrupts the newborn bubble, and it’s okay to feel that.

Grieving What You Expected
It’s normal to grieve. You’re mourning the idea of a complication-free start. You’re processing the loss of simplicity. Let yourself feel that. But don’t stay there. Unlike many pediatric conditions, this one has a clear, effective fix. The medication works.
Explaining It to Family and Friends
People will have questions. Grandparents may ask if iodine drops will help (they won’t) or if you should change your diet (you shouldn’t). Here’s a simple script that works: “The baby’s thyroid gland didn’t form quite right. It’s a random thing that happens. We give a replacement hormone every day, and as long as we do that, the baby is perfectly healthy.”
Long-Term Outlook: From Childhood Through Adulthood
The short answer? A normal life. But there are specific stages where management needs some adjustment.
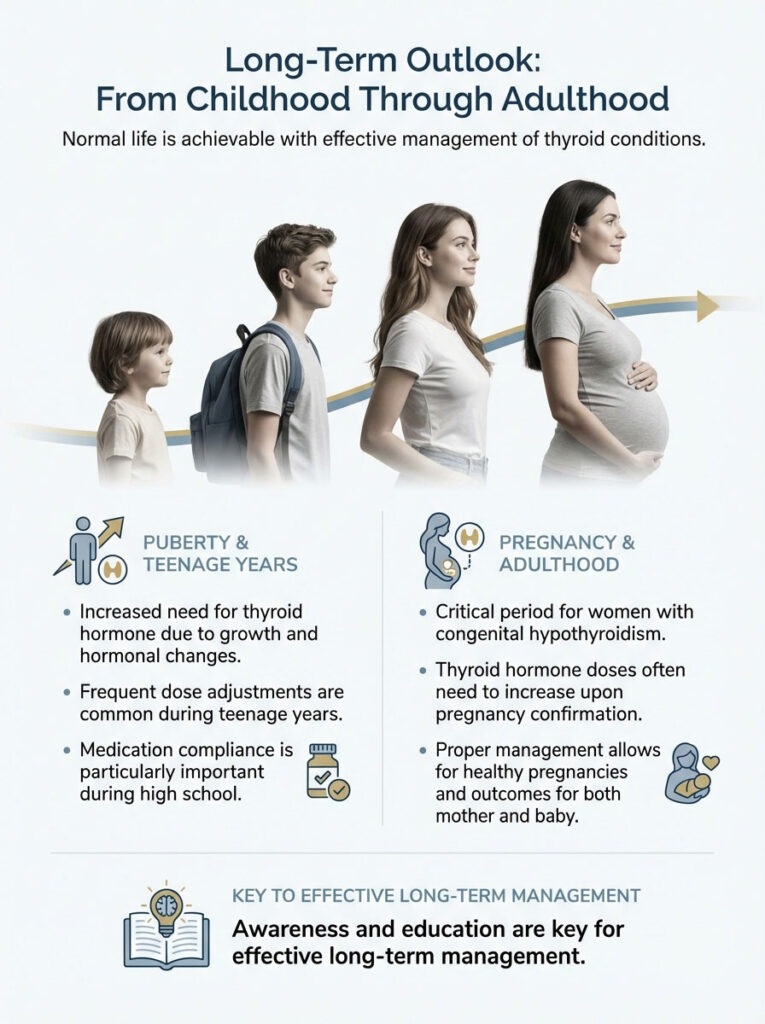
Puberty
Puberty brings rapid growth and hormonal shifts, which increase the body’s demand for thyroid hormone. Dose adjustments happen frequently during the teenage years. Teens also tend to push back on taking daily medication, so staying on top of compliance during high school is important.
Pregnancy
For women with congenital hypothyroidism, pregnancy is a critical period. The thyroid dose typically needs to increase as soon as pregnancy is confirmed to support both mother and developing baby. With proper management, women with this condition have healthy pregnancies and healthy children.
What to Remember: Your Child Is Going to Be Okay
Hearing the words “congenital hypothyroidism” is overwhelming. But in the world of pediatric diagnoses, this is the one we want. We understand it completely. We treat it easily. We monitor it precisely.
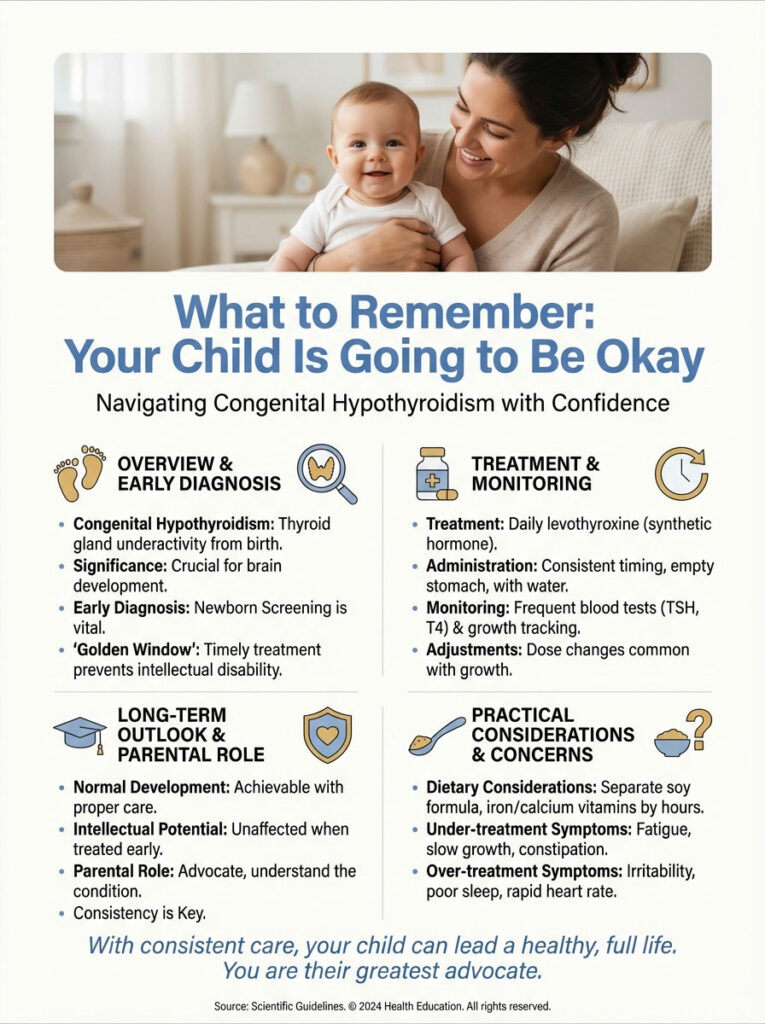
Your child has a condition, but they are not defined by it. They’ll play sports, struggle with homework, make friends, and grow to their full height, just like any other kid. The only difference is one small pill, once a day, crushed on a spoon. That pill is the key that unlocks their full potential.
Action Steps for Parents
- Start immediately. Don’t delay levothyroxine once it’s prescribed. Every day counts in that Golden Window.
- Give it correctly. Crush the pill, avoid soy if possible, and separate from iron or calcium supplements by four hours.
- Keep every blood work appointment. Your baby grows fast, and the dose needs to keep up.
- Trust the science. This treatment works. Millions of healthy adults are living proof.
You’re already doing the right thing by learning about this condition. Your child has the best advocate they could ask for: you.
Frequently Asked Questions
What exactly is congenital hypothyroidism and how does it affect my baby?
Congenital hypothyroidism is a condition present at birth where the thyroid gland is either missing, misplaced, or unable to produce sufficient thyroid hormone. As a pediatric endocrinologist, I explain to parents that this hormone is the essential fuel for brain architecture and metabolic growth. Without it, the brain cannot properly insulate its neural connections, but with early replacement therapy, your baby will develop normally.
How is congenital hypothyroidism diagnosed in newborns?
The diagnosis begins with the mandatory newborn screening (NBS) heel prick test, typically performed within the first 48 hours of life. If the screening shows an elevated TSH or low T4 level, we immediately order a confirmatory venous blood draw. We may also use a thyroid ultrasound or a nuclear medicine uptake scan to visualize the gland’s anatomy and determine if it is in the correct location.
Why did my baby develop this condition and is it my fault?
It is important to understand that this is almost never caused by anything the parents did, ate, or drank during pregnancy. Most cases (85%) are caused by thyroid dysgenesis, which is a random fluke in fetal development where the gland fails to form correctly. Only about 15% of cases are hereditary, involving genetic errors in the hormone-production machinery known as dyshormonogenesis.
What is the Golden Window for starting thyroid treatment?
The “Golden Window” refers to the first 14 days of an infant’s life. Initiating levothyroxine treatment within this two-week period is critical for ensuring the child achieves their full intellectual potential and normal IQ scores. Because the brain undergoes rapid myelination in these early days, we prioritize immediate intervention rather than a “wait and see” approach.
How do I administer levothyroxine tablets to a newborn?
You should crush the small tablet between two metal spoons into a fine powder and mix it with a very small amount (1-2 mL) of breast milk, formula, or water. Use a small oral syringe to place the liquid into the baby’s cheek pouch, followed by a full feeding to ensure the entire dose is swallowed. Never put the medication into a full bottle of milk, as the baby might not finish the bottle and will miss part of the dose.
Can my baby use soy formula if they are taking thyroid medication?
Yes, babies can use soy formula, but we must monitor their blood levels closely because soy protein can interfere with the absorption of thyroxine in the gut. If you choose to use soy formula, we often need to prescribe a higher dose of levothyroxine to overcome this binding effect. Consistency is key; if you switch between soy and milk-based formulas, your endocrinologist needs to know immediately.
What are the symptoms of under-treatment or over-treatment in infants?
Under-treatment may lead to lethargy, constipation, and poor growth, while over-treatment can cause irritability, rapid heart rate, and sleep disturbances. However, because these clinical signs can be subtle in infants, we rely primarily on frequent lab work to ensure the Free T4 and TSH levels remain within the target therapeutic range. Our goal is to keep the “engine” running at the perfect speed for development.
How often will my child need blood tests for monitoring?
During the first six months of life, we typically check thyroid levels every 1 to 2 months to keep up with the baby’s rapid growth. As the growth velocity stabilizes between ages 6 months and 3 years, the frequency usually decreases to every 3 to 4 months. These labs allow us to adjust the dosage precisely as the child gains weight and their metabolic needs change.
Is brand-name Synthroid better than generic levothyroxine for babies?
For infants, consistency is more important than the brand itself, though many specialists prefer brand-name medications like Synthroid or Unithroid due to strict manufacturing tolerances. Levothyroxine has a narrow therapeutic index, meaning small variations in the pill’s potency can significantly impact a small baby’s blood levels. If using a generic, ensure your pharmacist provides the same manufacturer for every refill to avoid absorption fluctuations.
Will my child have to take thyroid medication for the rest of their life?
If the thyroid gland is missing or misplaced (permanent CH), the child will require lifelong levothyroxine. However, some cases are “transient” and may resolve by age three, particularly if caused by maternal antibodies or iodine exposure. We typically perform a “trial off” medication at age three to determine if the child’s own gland can sustain proper hormone levels.
Can I give my baby vitamins or iron with their thyroid dose?
Iron and calcium are “binders” that can stick to the thyroid hormone in the stomach and prevent it from entering the bloodstream. You must separate any multivitamins containing iron or calcium supplements from the levothyroxine dose by at least four hours. This ensures that your baby receives the full benefit of the medication without interference.
What is the long-term outlook for a child with congenital hypothyroidism?
The long-term outlook is excellent; children treated early and consistently live completely normal, healthy lives with full intellectual potential. They will hit their developmental milestones, excel in school, and go through puberty just like their peers. As long as the daily medication routine is maintained and labs are monitored, the diagnosis will not limit their future achievements.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Congenital hypothyroidism is a serious medical condition that requires management by qualified healthcare professionals. Always seek the advice of your physician or a pediatric endocrinologist with any questions you may have regarding a medical diagnosis or treatment plan for your child.
References
- American Academy of Pediatrics (AAP) – pediatrics.aappublications.org – Provides the updated clinical report on newborn screening and therapy for congenital hypothyroidism.
- Pediatric Endocrine Society (PES) – pedsendo.org – Professional guidelines for the management and long-term care of infants with thyroid disorders.
- American Thyroid Association (ATA) – thyroid.org – Offers comprehensive management guidelines for children and adults with hypothyroidism.
- New England Collaborative – NEJM – Longitudinal research studies regarding cognitive outcomes and IQ in children treated for congenital hypothyroidism.
- Journal of Clinical Endocrinology & Metabolism (JCEM) – academic.oup.com/jcem – European Society for Paediatric Endocrinology consensus guidelines on screening and diagnosis.
- U.S. National Library of Medicine – MedlinePlus – Detailed genetic and physiological data on thyroid dysgenesis and dyshormonogenesis.








