You’re about to pop an ibuprofen, but something gives you pause. Maybe you take daily aspirin for your heart. Maybe you’ve got surgery coming up next week. So you wonder: does ibuprofen thin your blood enough to cause a real problem?
Table of Contents
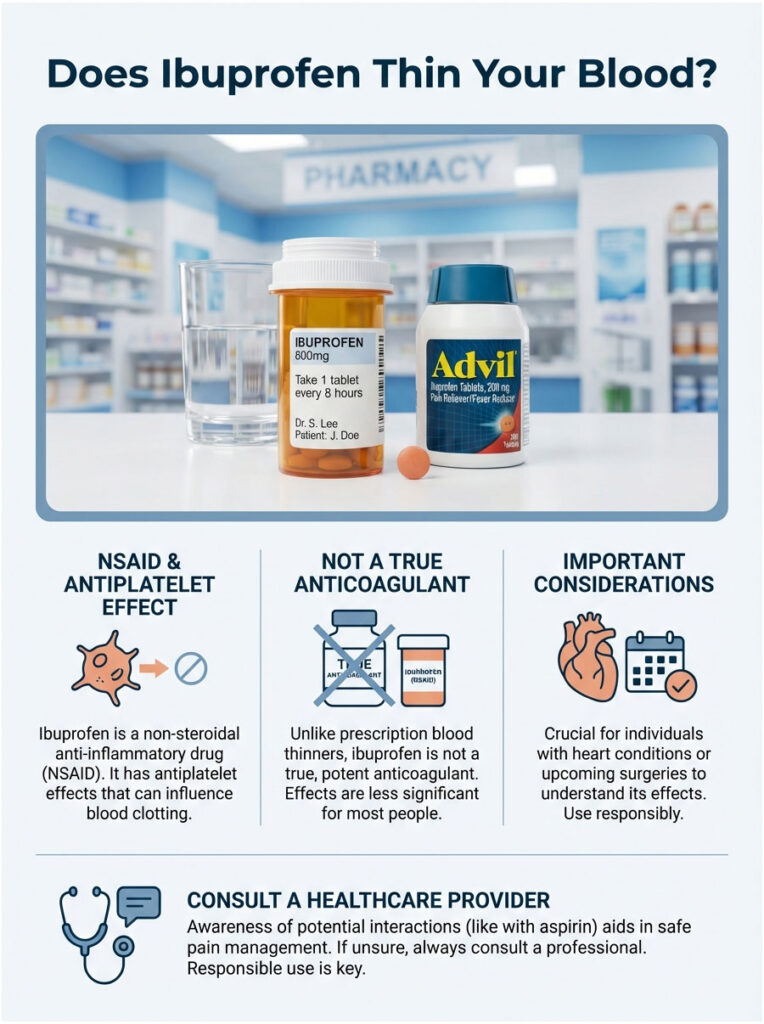
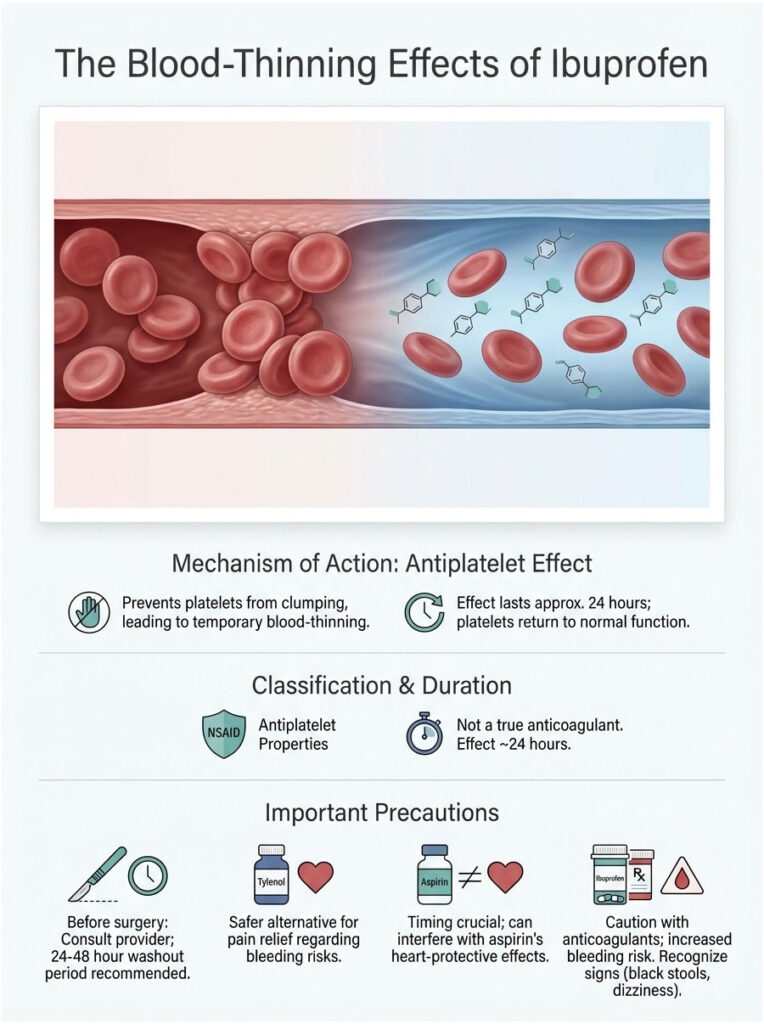
It’s one of the most common questions pharmacists hear. And the honest answer is yes, ibuprofen does affect your blood’s ability to clot. But it doesn’t work the way prescription blood thinners do. Ibuprofen is a non-steroidal anti-inflammatory drug (NSAID) that happens to have antiplatelet side effects. It’s not a true anticoagulant. That distinction matters more than most people realize.
Quick Summary: The Pharmacist’s Take
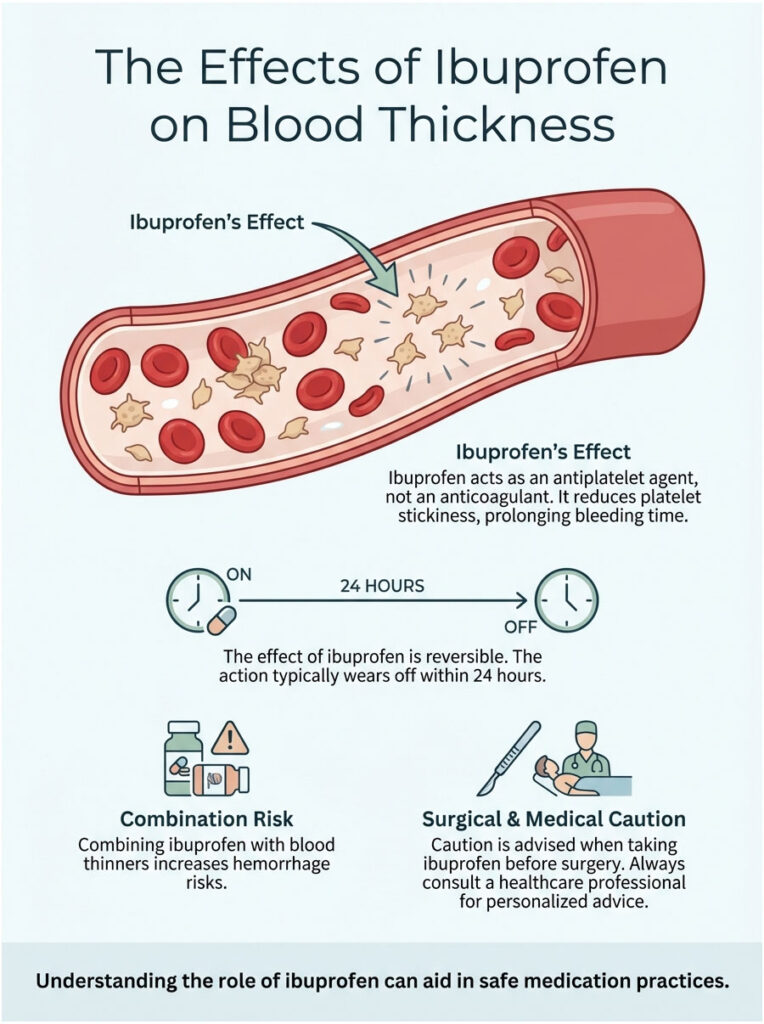
Does ibuprofen thin your blood? Yes, but as an antiplatelet agent, not an anticoagulant. It makes your platelets less sticky, which prolongs the time it takes for bleeding to stop. Unlike aspirin, this effect is reversible. It typically wears off within 24 hours as your body clears the drug. That said, combining ibuprofen with other blood thinners or taking it before surgery can create serious hemorrhage risks.
Key Statistics Worth Knowing
- 15 to 35% of all adverse drug reaction reports involve NSAIDs like ibuprofen.
- Regular NSAID use increases the risk of gastrointestinal bleeding by 400% in elderly patients.
- Taking ibuprofen with aspirin can reduce aspirin’s heart-protecting benefit by up to 90% if the timing is wrong.
- Over 30 million Americans take NSAIDs daily for pain relief.
- Bleeding risk rises significantly when ibuprofen is taken for more than 3 consecutive days.
What “Blood Thinning” Actually Means in Medical Terms
When patients ask “does ibuprofen thin your blood,” they’re usually worried about bleeding. But in medical terms, we don’t literally make blood thinner like watering down paint. What we’re really talking about is preventing blood cells from clumping together.
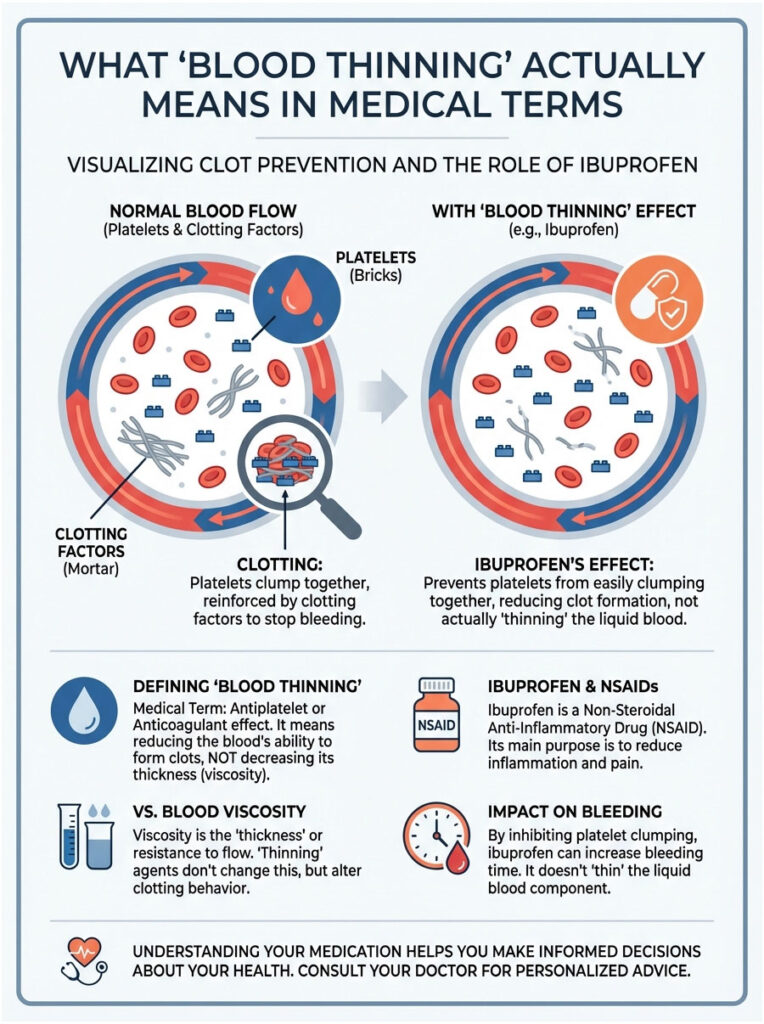
Blood viscosity refers to how thick and sticky your blood is. True “thinning” would mean changing the plasma content itself. Ibuprofen doesn’t do that. What it does is change the behavior of the solid components floating within the plasma, specifically your platelets.
The Pharmacological Distinction
Ibuprofen (sold as Advil or Motrin) belongs to the NSAID class. Its main purpose is fighting inflammation and pain. But as a side effect of how it works, it interferes with the clotting process. It doesn’t lower your blood’s viscosity. It does increase your “bleeding time,” which is how long it takes for a cut to stop bleeding.
Here’s a helpful way to picture it. Think of your platelets as bricks and your clotting factors as mortar. Anticoagulants like Warfarin mess with the mortar. Antiplatelets like ibuprofen mess with the bricks. Ibuprofen essentially makes the bricks slippery so they can’t stack up to form a wall.
How Ibuprofen Affects Clotting: The COX-1 Pathway
Here’s the science behind the bleeding risk. Ibuprofen blocks an enzyme called Cyclooxygenase, or COX for short. There are two main types, COX-1 and COX-2.
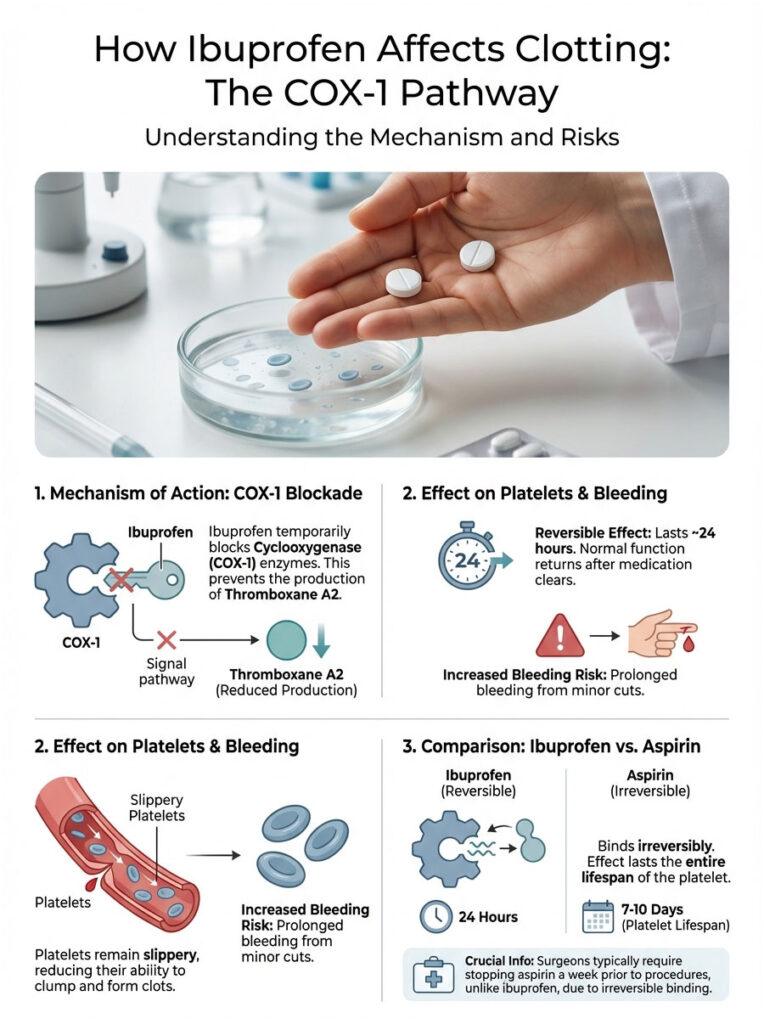
- COX-1 produces a lipid called Thromboxane A2.
- Thromboxane A2 is essentially a “glue signal.” It tells your platelets to activate, change shape, and stick together to plug a wound.
When you take ibuprofen, you temporarily shut down Thromboxane A2 production. Without that chemical signal, your platelets stay slippery. They slide past each other instead of clumping. This is why a shaving nick might bleed longer than usual after you’ve taken Advil.
Why Ibuprofen’s Effect Is Reversible (and Aspirin’s Isn’t)
This is the most important concept to understand. Ibuprofen binds to the platelet reversibly. Think of a key inserted into a lock but never turned. Once your body metabolizes the drug, the “key” falls out and the platelet goes back to working normally. This usually happens within 24 hours.
Aspirin, on the other hand, binds irreversibly. It breaks the lock. The effect lasts for the entire 7 to 10 day lifespan of that platelet. This is why surgeons stop aspirin a full week before a procedure but may only require stopping ibuprofen 24 to 48 hours beforehand.
Ibuprofen vs. Common Blood Thinners: Know the Difference
Lumping all “blood thinners” into one category is a mistake I see patients make frequently. They assume because ibuprofen is over the counter, it must be weak. But when mixed with other medications, it can be surprisingly potent.
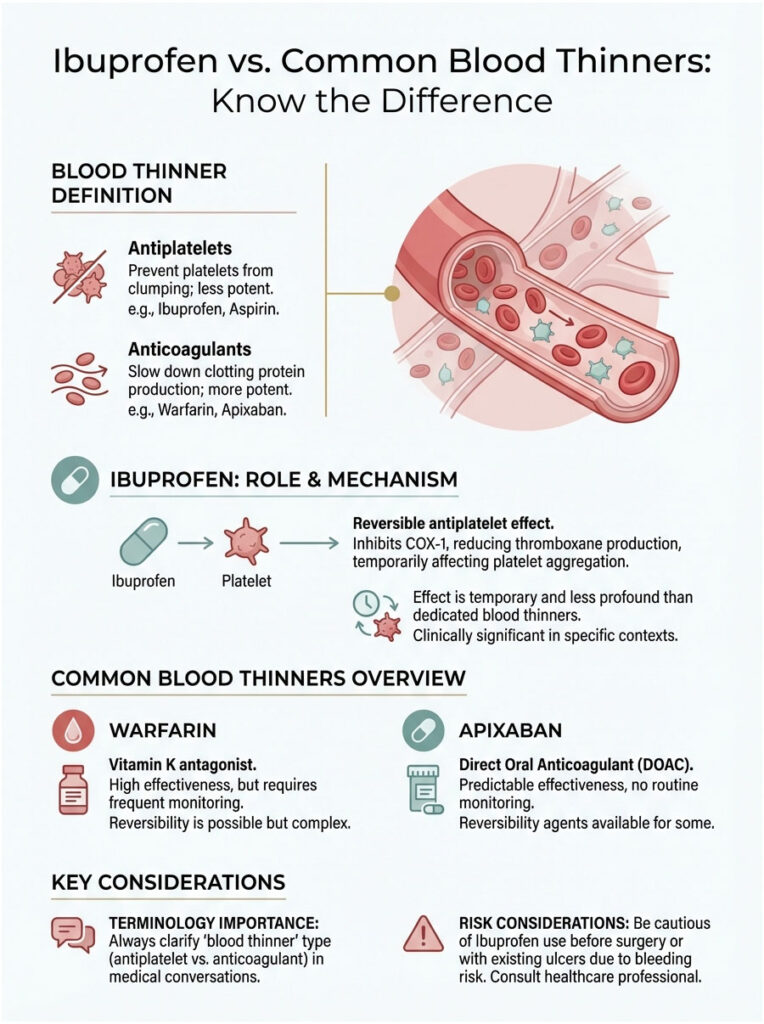
The key distinction: antiplatelets target the blood cells themselves, while anticoagulants target proteins in the plasma. Ibuprofen is an antiplatelet. Warfarin is an anticoagulant. Taking both attacks your clotting system from two completely different directions.
| Drug | Class | How It Works | Effect on Platelets | Reversibility |
|---|---|---|---|---|
| Ibuprofen (Advil, Motrin) | NSAID | Inhibits COX-1 and COX-2 | Reduces aggregation (stickiness) | Reversible (clears in ~24 hrs) |
| Aspirin (Bayer) | Salicylate NSAID | Irreversibly inhibits COX-1 | Permanently disables platelet clumping | Irreversible (lasts 7-10 days) |
| Warfarin (Coumadin) | Vitamin K Antagonist | Reduces clotting factors II, VII, IX, X | Minimal direct effect; targets plasma | Reversible (requires Vitamin K) |
| Apixaban (Eliquis) | DOAC (Factor Xa Inhibitor) | Blocks Factor Xa in clotting cascade | No direct platelet effect | Reversible (short half-life) |
| Acetaminophen (Tylenol) | Analgesic / Antipyretic | Acts centrally in brain and spine | None | N/A |
Why Terminology Matters in Practice
When you ask a doctor “does ibuprofen thin your blood” and they say “not technically,” they mean it’s not an anticoagulant. But for a patient facing surgery, the practical answer is effectively yes. For a patient with a stomach ulcer, the answer is also yes. The antiplatelet effect is clinically significant enough to shift your risk profile from “stroke prevention” to “hemorrhage risk.”
The Aspirin Interaction: A Cardiac Safety Issue
If you take low-dose aspirin (81mg) daily to prevent heart attacks or strokes, you need to be extremely careful with ibuprofen. This drug interaction gets overlooked constantly. The FDA has issued specific warnings about it, and for some cardiac patients, it’s genuinely a matter of life and death.
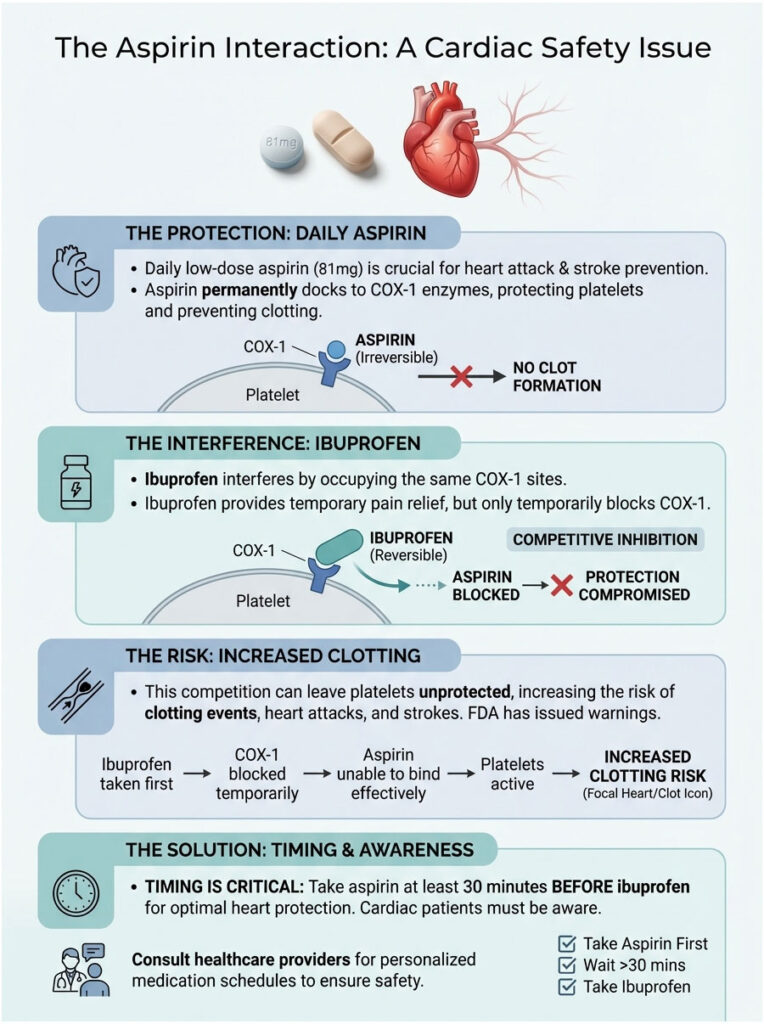
The Receptor Competition Problem
Both aspirin and ibuprofen target the same docking station on the platelet, the COX-1 enzyme. Aspirin wants to dock there permanently to protect your heart. Ibuprofen wants to dock there temporarily to relieve your pain.
This creates a biological traffic jam. If you take ibuprofen first, it occupies the docking station. The aspirin floats by with nowhere to attach and eventually gets eliminated from your body without ever doing its job.
Once the ibuprofen wears off, your platelets are unprotected. The aspirin is already gone. You’re now vulnerable to a clotting event like a heart attack. This is called competitive inhibition, and it can render your heart medication completely useless.
The Timing Rule Every Cardiac Patient Should Know
To keep your heart protected while still treating pain:
- Take your aspirin at least 30 minutes before taking ibuprofen.
- OR wait at least 8 hours after taking ibuprofen before taking your aspirin.
This window lets the aspirin lock onto platelets first, establishing heart protection before ibuprofen enters the picture.
Pre-Surgery Guidelines: When to Stop Ibuprofen
Surgeons worry about uncontrolled bleeding because it obscures their view and causes complications. Since NSAIDs impair your body’s primary method of stopping blood flow, strict “washout” periods are required before procedures.
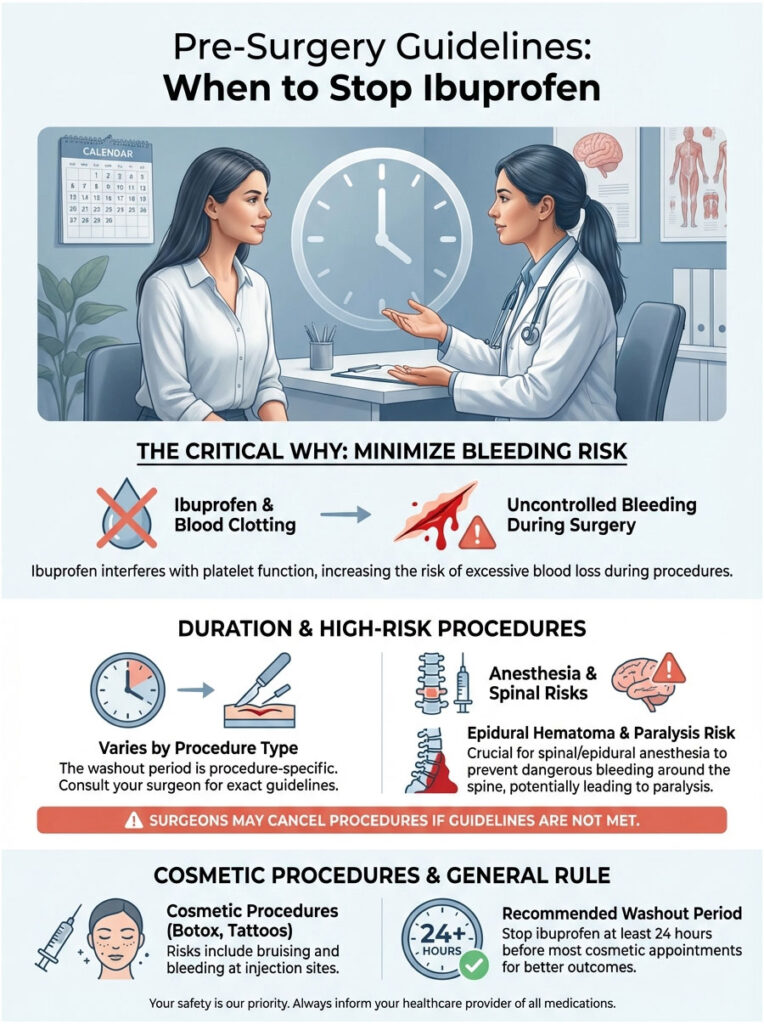
How Long Before Surgery Should You Stop?
The answer depends on the type of procedure and how long the drug stays active in your body.
- Minor procedures (dental work, dermatology): Most providers want you off ibuprofen for 24 to 48 hours beforehand. That’s enough time for the drug to clear and platelet function to normalize.
- Major surgery (orthopedic, abdominal): For high-bleeding-risk operations like hip replacements, the standard window is often 3 to 7 days. While ibuprofen technically clears in 24 hours, surgeons prefer a wide safety margin to ensure zero residual antiplatelet effect.
Anesthesia and Spinal Procedures
The risk goes beyond the surgical incision. If you’re having spinal anesthesia or an epidural, impaired clotting presents a catastrophic risk.
A bleed near the spine can form an epidural hematoma. The pooled blood compresses the spinal cord, potentially leading to permanent paralysis. Anesthesiologists follow strict protocols on this. Many will cancel a surgery outright if they learn the patient took ibuprofen that morning.
Cosmetic Procedures and Tattoos
This is one people tend to forget. Taking ibuprofen before Botox, fillers, or a tattoo is a mistake. It increases bruising significantly.
For tattoos specifically, increased bleeding pushes ink out of the skin. The result is a patchy, unevenly healed tattoo, and it makes the artist’s job much harder. Avoid all NSAIDs for at least 24 hours before these appointments.
Dangerous Drug Combinations: The “Double Hit”
The most severe bleeding cases I’ve seen in hospital settings usually involve patients combining over-the-counter ibuprofen with prescription medications. We call this the “Double Hit” because you’re hitting the clotting system twice from different angles.
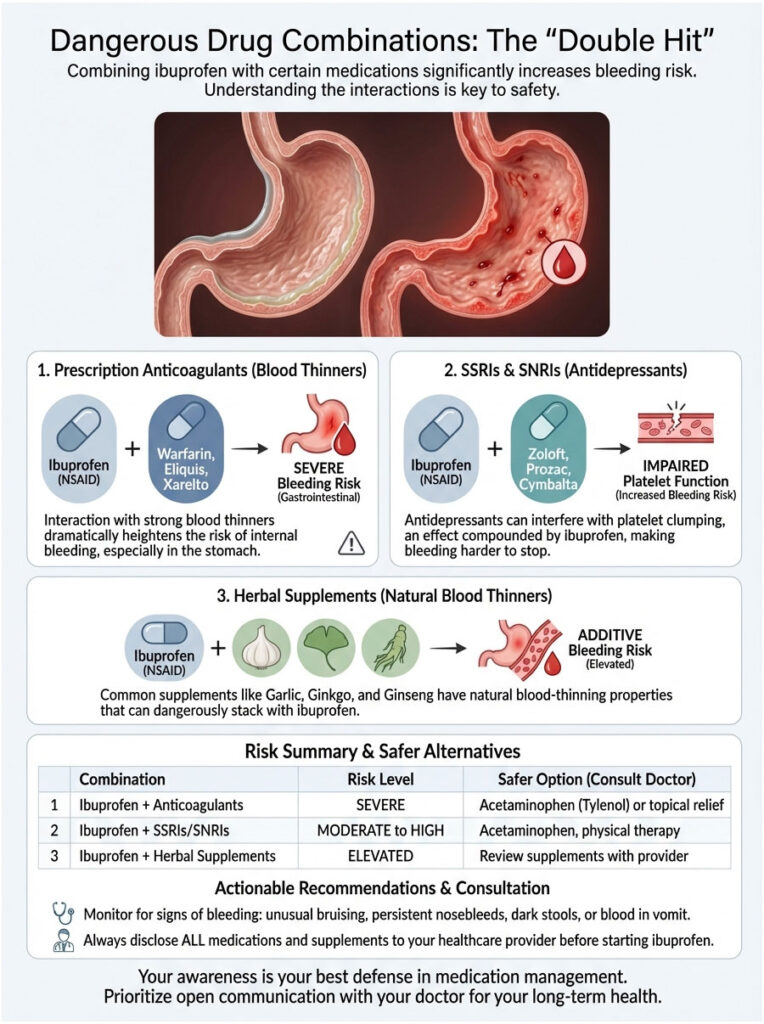
Prescription Anticoagulants
Taking ibuprofen alongside Warfarin (Coumadin), Eliquis, or Xarelto is generally contraindicated. Warfarin blocks clotting factors. Ibuprofen blocks platelets. Disable both mechanisms of hemostasis at once, and the risk of a major gastrointestinal bleed skyrockets. To make it worse, NSAIDs can displace Warfarin from protein binding sites, causing unpredictable spikes in INR levels.
SSRIs and SNRIs (Antidepressants)
This interaction is less well-known but highly relevant. Antidepressants like Sertraline (Zoloft) or Fluoxetine (Prozac) work by keeping serotonin available in the brain. But platelets also use serotonin to signal clumping.
SSRIs deplete platelet serotonin, which mildly impairs their function. Layer ibuprofen on top of that, and the combined bleeding risk is significantly higher than with either drug alone. If you’re on antidepressants, watch for easy bruising as an early warning sign.
Herbal Supplements
Many natural supplements have mild blood-thinning properties. The most common offenders are the “Three Gs”: Garlic, Ginkgo, and Ginseng. Fish oil and Vitamin E also affect clotting. Taking high doses of these supplements alongside regular ibuprofen can lead to unexpected bleeding. Always tell your doctor about your supplement routine.
Drug Combination Risk Summary
| Combination | Bleeding Risk | How It Happens | What to Do |
|---|---|---|---|
| Ibuprofen + Warfarin | Severe / Critical | Clotting impairment + gastric erosion | Avoid entirely. Use Tylenol instead. |
| Ibuprofen + Aspirin | Moderate to High | Reduced heart protection + cumulative bleeding | Follow timing rules strictly. |
| Ibuprofen + SSRIs | Moderate | Platelet serotonin depletion | Monitor for bruising; use lowest dose. |
| Ibuprofen + Alcohol | High | Direct gastric irritation from both | Do not combine. High gastritis risk. |
The Stomach Bleeding Connection
When you ask “does ibuprofen thin your blood,” you should also be asking “does ibuprofen damage my stomach?” The two issues are closely linked.
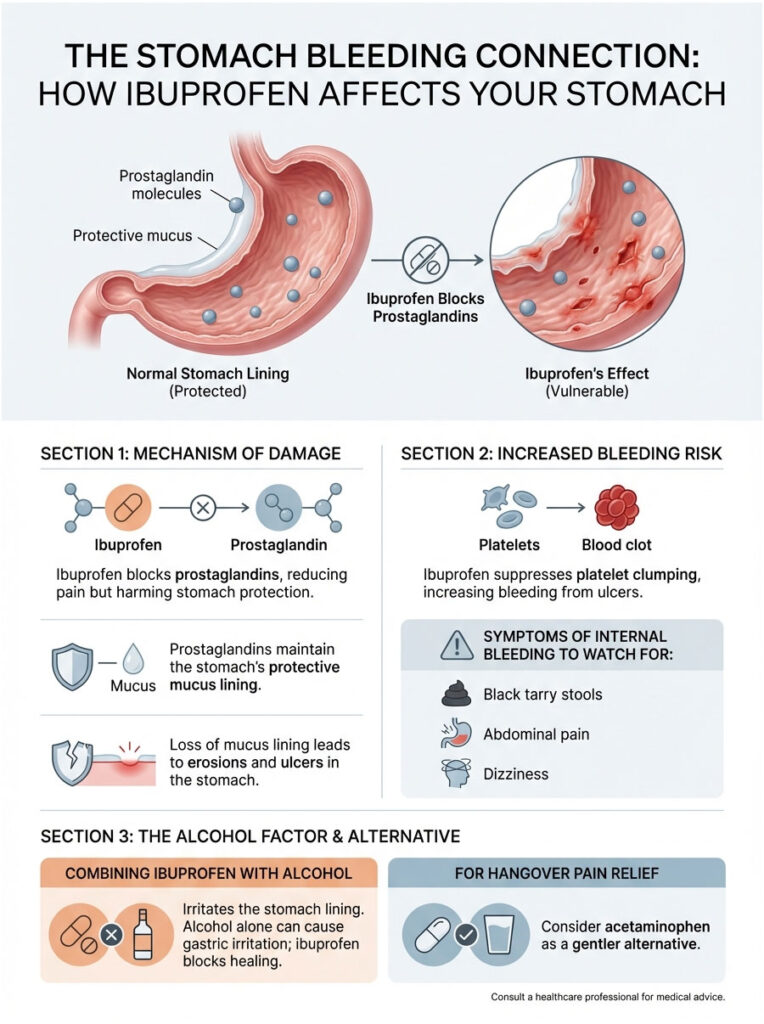
Prostaglandins are chemicals that drive pain and inflammation. But they also maintain the protective mucus lining inside your stomach. By blocking prostaglandins to stop pain, ibuprofen strips away that shield and exposes the stomach lining to harsh acid. Over time, this leads to erosions and ulcers.
Here’s where the double problem kicks in: because ibuprofen also suppresses platelet clumping, any ulcer that forms bleeds more freely. The body can’t clot the wound effectively. It’s a two-pronged attack on the same organ.
Warning Signs of Internal Bleeding
If you’re taking ibuprofen regularly, stay alert for these symptoms:
- Black, tarry stools (melena): This indicates digested blood moving through the digestive tract.
- Coffee-ground vomit (hematemesis): Old blood that’s been sitting in the stomach.
- Dizziness when standing (orthostatic hypotension): A sign of blood volume loss.
Ibuprofen and Alcohol: A Risky Combination
Taking ibuprofen for a hangover is extremely common. It’s also genuinely dangerous. Alcohol irritates the stomach lining on its own. Ibuprofen blocks the repair of that lining. Together, they significantly increase the risk of acute gastritis.
If you’ve been drinking heavily, stick to water and electrolytes. If you need a pain reliever, acetaminophen is gentler on the stomach, though you should be cautious with the dose if your liver is already stressed from alcohol.
The Cardiovascular Paradox: “Thinner” Blood but Higher Stroke Risk?
This is one of the more confusing aspects of ibuprofen. We’ve established that it has antiplatelet effects, which should theoretically prevent clots. Yet ibuprofen carries a Black Box Warning for increasing the risk of heart attack and stroke. How can something that thins the blood also cause strokes?
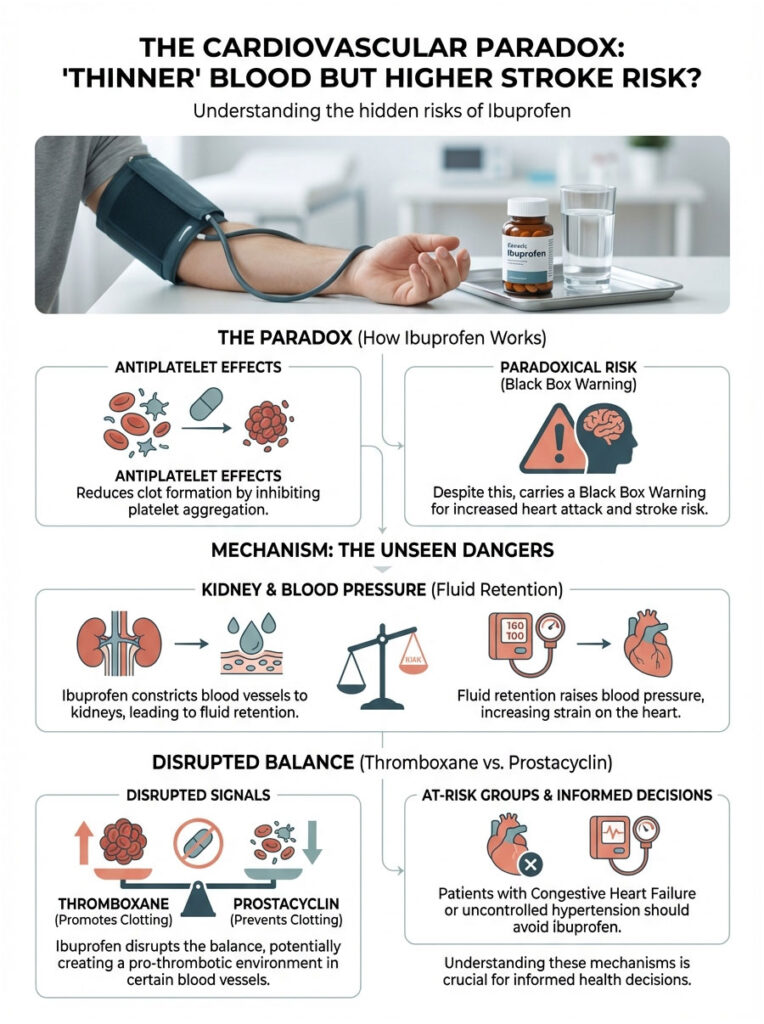
The answer involves your kidneys and blood pressure. NSAIDs constrict blood vessels leading to the kidneys, causing your body to retain sodium and water. That fluid retention raises blood pressure and puts extra strain on the heart.
There’s also a more subtle mechanism at play. Your body maintains a careful balance between Thromboxane (which promotes clotting) and Prostacyclin (which prevents clotting and relaxes blood vessels). Ibuprofen disrupts this balance, and in some blood vessels, it can actually create a pro-thrombotic environment despite its antiplatelet effects elsewhere. This is why patients with Congestive Heart Failure or uncontrolled hypertension should avoid ibuprofen entirely.
Safer Alternatives for Pain Relief
If the answer to “does ibuprofen thin your blood” concerns you because of your medical history, you have other options. You don’t have to just tough it out.

Acetaminophen (Tylenol)
Acetaminophen is the go-to pain reliever for patients on anticoagulants. It works in the brain to block pain signals and has virtually no effect on COX-1 in the bloodstream. It doesn’t suppress platelet function. It doesn’t erode the stomach lining. For patients taking Warfarin or Eliquis, it’s the safest choice.
Topical NSAIDs (Diclofenac/Voltaren Gel)
For localized joint pain in the knees or hands, topical diclofenac gel is an excellent option. It delivers the anti-inflammatory medication directly to the joint. While some systemic absorption does occur, blood levels remain far lower than with oral pills. This dramatically reduces the risk of both systemic bleeding and stomach ulcers while still providing the benefit of an NSAID.
Non-Drug Approaches
Don’t overlook physical therapies. The RICE method (Rest, Ice, Compression, Elevation) works well for acute injuries. TENS units can help manage chronic muscle pain. Turmeric and curcumin supplements act as natural anti-inflammatories, though they also carry mild blood-thinning properties and should be discussed with your doctor first.
Special Populations: Who Needs Extra Caution?

Pregnancy
Ibuprofen is generally off-limits during the third trimester. It can cause premature closure of the ductus arteriosus, a vital vessel in the fetal heart. Its blood-thinning effect also raises the risk of hemorrhage for the mother during delivery. Acetaminophen is the preferred pain reliever throughout pregnancy.
Older Adults
The Beers Criteria, a widely used medication safety guideline for seniors, lists NSAIDs as “potentially inappropriate” for older adults. Aging kidneys clear drugs more slowly. The aging stomach lining is thinner and more vulnerable. The risk of a life-threatening GI bleed from ibuprofen climbs sharply after age 65. Topical NSAIDs or acetaminophen are almost always the better call.
Blood Donation
Can you donate blood after taking ibuprofen? For whole blood donations, generally yes, as long as you’re feeling well. However, if you’re donating platelets specifically (apheresis), you’ll need to wait. The typical requirement is 48 hours after your last dose to ensure the platelets you donate are fully functional for the recipient.
The Bottom Line
So, does ibuprofen thin your blood? In practical terms, yes. It prevents platelets from clumping together. While the effect is temporary and reversible, it’s strong enough to cause real complications, especially during surgery or when combined with other medications.
What You Should Do
- Check your labels. Many cold and sinus medications already contain ibuprofen. Don’t accidentally double dose by taking Advil on top of them.
- Respect the washout period. Stop ibuprofen at least 24 to 48 hours before any surgery or dental work.
- Protect your stomach. Take ibuprofen with food to buffer acid, but understand this doesn’t fully prevent systemic mucosal damage.
- Talk to your pharmacist. If you’re on Warfarin, Eliquis, or daily aspirin, ibuprofen probably isn’t the right pain reliever for you. Ask about alternatives.
Pain relief and bleeding risk are always a balancing act, and the right answer depends on your individual health profile. When in doubt, ask your pharmacist or physician. Being informed is your best protection against adverse drug events.
Frequently Asked Questions
Is ibuprofen considered a clinical blood thinner?
Technically, ibuprofen is classified as a non-steroidal anti-inflammatory drug (NSAID) with antiplatelet properties, rather than a true anticoagulant like Warfarin. While it does not change the thickness of the blood’s plasma, it interferes with the blood’s ability to clot by making platelets less sticky. This effectively increases your bleeding time, which is why it is often referred to as a “blood thinner” in a layperson’s terms.
How exactly does ibuprofen affect the blood clotting process?
Ibuprofen works by inhibiting the COX-1 enzyme, which is responsible for producing a lipid called Thromboxane A2. Thromboxane A2 acts as a chemical signal that instructs platelets to clump together to form a clot. By blocking this signal, ibuprofen makes the platelets “slippery,” preventing them from aggregating to plug a wound or stop a bleed.
How long does the blood-thinning effect of ibuprofen stay in your system?
The antiplatelet effect of ibuprofen is reversible, meaning the platelets return to normal function once the drug is metabolized. For most healthy adults, this process takes approximately 24 hours. This is a significant clinical difference compared to aspirin, which disables platelets permanently for their entire 7 to 10-day lifespan.
When should I stop taking ibuprofen before a scheduled surgery?
Most surgeons and anesthesiologists recommend a “washout” period of at least 24 to 48 hours for minor procedures like dental work or dermatology. For major surgeries with high bleeding risks, such as orthopedic or abdominal procedures, you may be asked to stop taking NSAIDs up to 7 days in advance. Always follow your surgical team’s specific pre-operative guidelines to avoid complications like epidural hematomas or excessive hemorrhage.
Is Tylenol a safer alternative to Advil if I am worried about bleeding?
Yes, acetaminophen (Tylenol) is generally considered the safer choice for patients concerned about bleeding or those taking anticoagulants. Unlike ibuprofen, acetaminophen works centrally in the brain and spinal cord and does not inhibit COX-1 enzymes in the blood. This means it has no significant effect on platelet aggregation and does not increase the risk of gastrointestinal bleeding.
Can I take ibuprofen if I am on a daily low-dose aspirin regimen for my heart?
You must be very careful with the timing because ibuprofen can interfere with aspirin’s ability to protect your heart. If taken too close together, ibuprofen blocks the docking site on the platelet, preventing the aspirin from binding and leaving you vulnerable to a heart attack. The FDA recommends taking aspirin at least 30 minutes before ibuprofen, or waiting 8 hours after an ibuprofen dose before taking your aspirin.
Is it safe to take Motrin while on prescription anticoagulants like Eliquis or Warfarin?
Taking ibuprofen with prescription anticoagulants is generally contraindicated due to the “Double Hit” phenomenon. This combination attacks the body’s clotting mechanism from two different angles—the platelets and the plasma proteins—which causes the risk of major internal or gastrointestinal bleeding to skyrocket. Patients on these medications should consult their healthcare provider before using any NSAID.
What are the warning signs of internal bleeding caused by ibuprofen use?
Patients should be vigilant for symptoms of gastrointestinal bleeding, such as melena (black, tarry stools) or hematemesis (vomit that looks like coffee grounds). Other systemic signs include feeling lightheaded when standing up, which may indicate a loss of blood volume. If you experience these symptoms while taking NSAIDs, seek medical attention immediately.
Why does ibuprofen have a heart attack warning if it prevents blood from clotting?
This cardiovascular paradox exists because ibuprofen causes the body to retain sodium and water, which increases blood pressure and puts stress on the heart. Additionally, it can disrupt the delicate balance between clotting and anti-clotting factors in the blood vessels. For those with existing heart disease or hypertension, these systemic effects can outweigh the minor antiplatelet benefit.
Can I take ibuprofen for a headache after drinking alcohol?
It is highly discouraged to combine alcohol and ibuprofen because both are known gastric irritants. Alcohol inflames the stomach lining while ibuprofen inhibits the prostaglandins that protect that lining, creating a high risk for acute gastritis or ulcers. For post-alcohol pain relief, hydration and electrolytes are safer, though acetaminophen should also be used with caution if the liver is stressed.
Is ibuprofen safe to use for pain relief during pregnancy?
Ibuprofen is typically avoided, especially during the third trimester of pregnancy. It can cause the premature closure of a vital fetal heart vessel called the ductus arteriosus and may increase the risk of maternal hemorrhage during delivery. Acetaminophen is the preferred analgesic for pregnant women under the guidance of a physician.
Does taking ibuprofen disqualify me from donating blood or platelets?
While you can usually donate whole blood after taking ibuprofen, it does affect platelet donation (apheresis). Because the drug impairs platelet function, the American Red Cross typically requires a 48-hour waiting period after your last dose before you can donate platelets. This ensures that the platelets received by a patient are fully functional and capable of clotting.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Ibuprofen and other NSAIDs carry significant risks for certain populations. Always consult a qualified healthcare professional or your pharmacist before starting new medications, especially if you are taking prescription blood thinners, have upcoming surgery, or have a history of stomach ulcers.
References
- U.S. Food and Drug Administration (FDA) – fda.gov – Official safety communications regarding NSAIDs and cardiovascular/gastrointestinal risks.
- American Heart Association (AHA) – heart.org – Clinical guidelines on the interaction between ibuprofen and low-dose aspirin therapy.
- Mayo Clinic – mayoclinic.org – Comprehensive patient data on NSAID pharmacology and side effect profiles.
- The Lancet – thelancet.com – Research studies regarding the relative risk of GI bleeding in elderly patients using NSAIDs.
- American Red Cross – redcrossblood.org – Eligibility requirements for blood and platelet donation following NSAID use.
- Journal of Clinical Pharmacy and Therapeutics – Peer-reviewed analysis of the “Double Hit” phenomenon between SSRIs and antiplatelet agents.