You are standing in the pharmacy aisle, probably hurting or looking after someone who is. The shelves are packed with colorful boxes, and the choices feel overwhelming. One question I hear almost every day at the pharmacy counter: can you take Tylenol and ibuprofen together for better pain relief?
Table of Contents
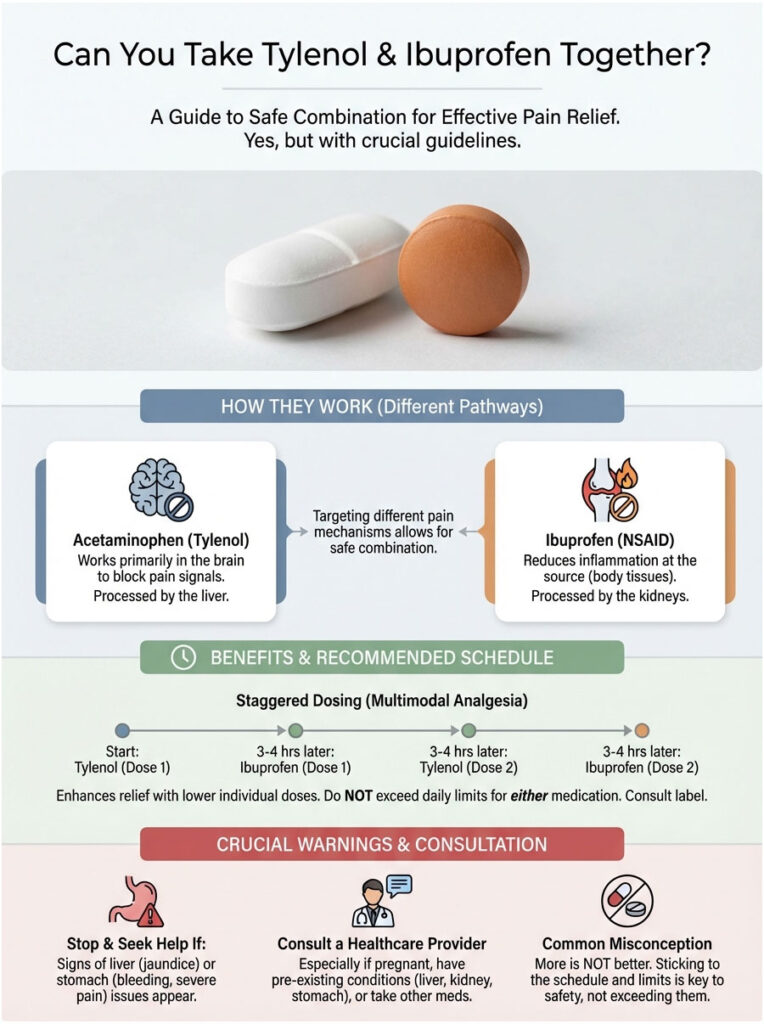
The short answer is yes. When you follow the right guidelines, this combination is not only safe but often more effective than some prescription options.
As a clinical pharmacist, I work with patients every day who are dealing with dental pain, post-surgical recovery, or fevers that just will not break. Many of them assume they have to pick one or the other. That is not true. By combining these medications, you are attacking pain from two completely different angles. But safety comes first. You need to respect the dosing limits to protect your liver and kidneys.
This guide gives you the medical clarity you need. We will cover the science behind why this works, the exact staggered schedule you should follow, and the warning signs that mean you need to stop immediately.
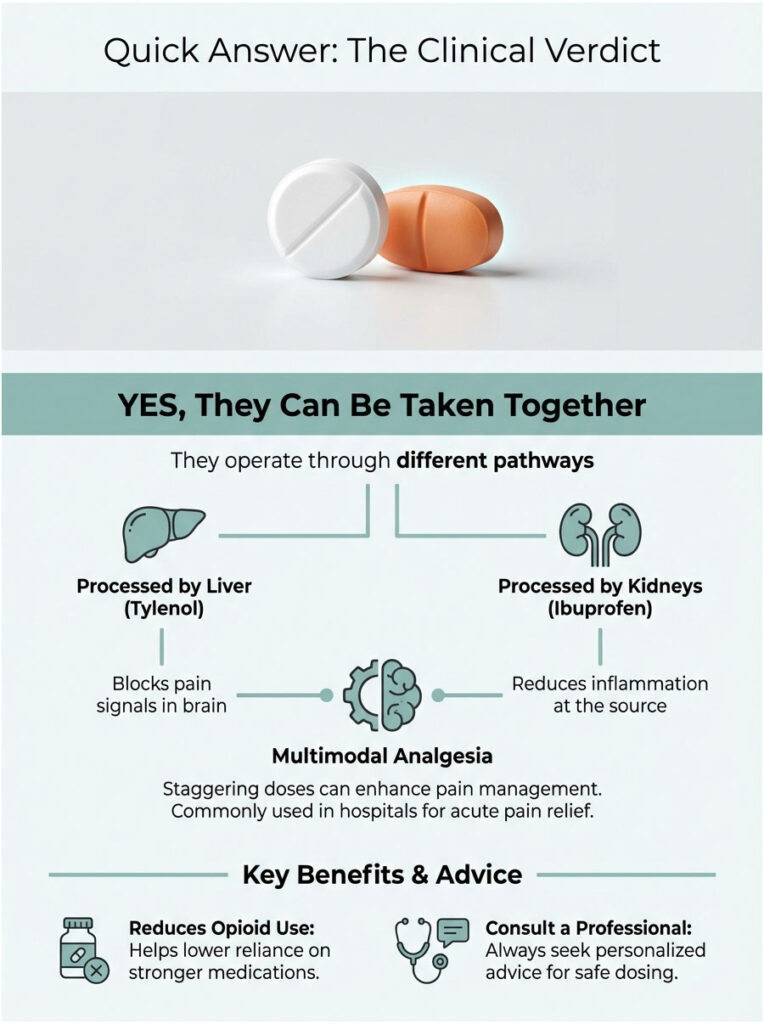
Quick Answer: The Clinical Verdict
Yes, you can take Tylenol and ibuprofen together. Because they work through different pathways and are processed by different organs (the liver handles Tylenol, the kidneys handle ibuprofen), they can be taken at the same time or staggered. This strategy is called multimodal analgesia, and it is a standard protocol used in hospitals to manage acute pain without opioids.
Key Facts at a Glance
- 4,000 mg: The absolute maximum daily limit of acetaminophen for healthy adults (FDA).
- 3,200 mg: The maximum daily prescription limit for ibuprofen (OTC limits are lower at 1,200 mg).
- 30-60 minutes: The average onset time for both medications to start working.
- ~30% greater relief: Studies suggest the combination offers roughly 30% more pain relief than either drug alone.
- 2020: The year the FDA approved the first fixed-dose combination pill (Advil Dual Action) in the US.
The Science of Synergy: Why This Combination Works
To understand why you can take Tylenol and ibuprofen together safely, you need to look at the chemistry. In pharmacology, this is called therapeutic synergy. It basically means that one plus one equals three. The combined effect is greater than what you would get from either drug on its own.
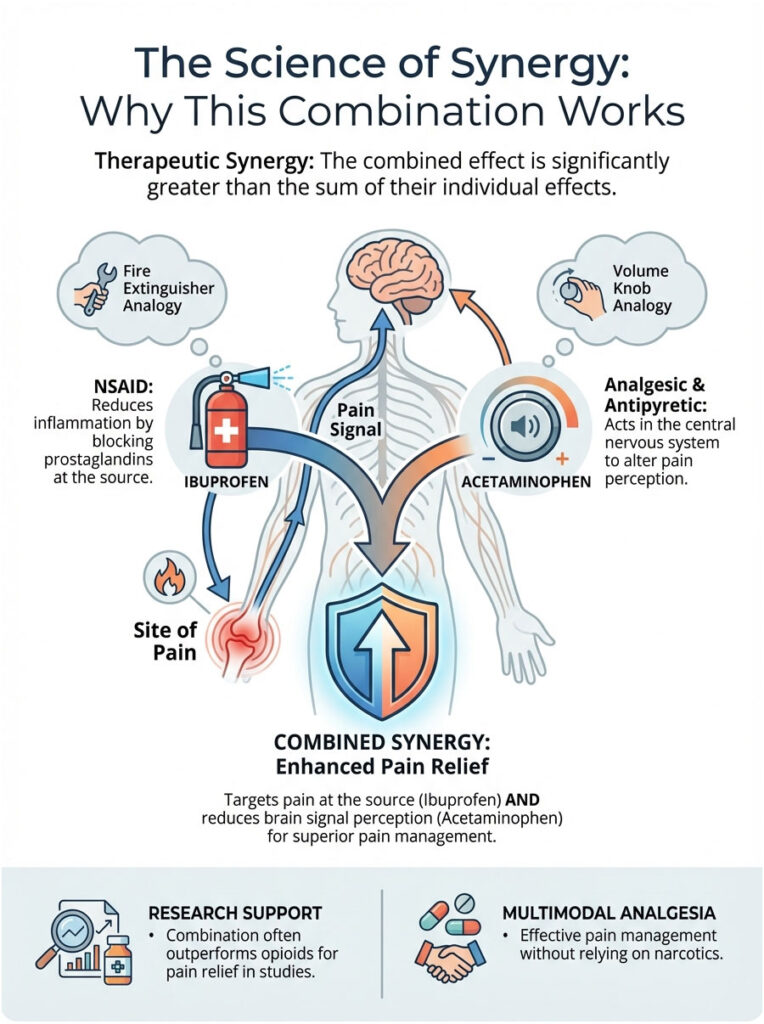
Pain is not a simple, single signal. It is a complex cascade of chemical reactions and electrical impulses. Treating it with just one medication is like trying to put out a house fire with only one hose while ignoring the sprinkler system. Two medications activate multiple systems to suppress the sensation of pain.
How Acetaminophen (Tylenol) Works
Acetaminophen is an analgesic (pain reliever) and antipyretic (fever reducer). While its exact mechanism is still being studied, we know it works primarily in the central nervous system. It acts on heat-regulatory centers in the hypothalamus to lower fever and raises the pain threshold in the brain. Essentially, it changes how your brain perceives pain. Notably, acetaminophen has very little effect on inflammation at the site of injury.
Think of acetaminophen as a volume knob. It does not stop the source of the music (the pain), but it turns the volume down so your brain is not as bothered by it. It is especially effective for headaches and general aches where swelling is not the main issue.
How Ibuprofen (Advil/Motrin) Works
Ibuprofen is a Non-Steroidal Anti-Inflammatory Drug (NSAID). It works peripherally, meaning right at the site of the pain. It blocks enzymes called COX-1 and COX-2, which produce prostaglandins. Prostaglandins are the chemicals that signal pain and cause swelling. By cutting off prostaglandin production, ibuprofen reduces the “fire” of inflammation.
If Tylenol is the volume knob, ibuprofen is the fire extinguisher. It goes directly to the source of the injury, whether that is a swollen gum, a twisted ankle, or an inflamed joint, and reduces the chemical reaction causing the pain.
The Power of Multimodal Analgesia
When you combine them, you are fighting on two fronts. Ibuprofen puts out the fire at the tissue level, while Tylenol turns down the volume of the pain signal reaching your brain. This is exactly why the acetaminophen and ibuprofen combination is so effective. Research from the Cochrane Library suggests that for dental pain, this combination often outperforms opioids like codeine.
This approach delivers superior pain relief without resorting to narcotics. In today’s medical landscape, avoiding opioids is a priority for both doctors and patients. Multimodal analgesia is the gold standard for achieving that.
Detailed Drug Profiles: Know What You Are Taking
It is important to understand that these two medications are chemically distinct. Many patients use the names interchangeably, but they are not the same thing. Review the comparison below before combining them. Understanding these differences is the first step in avoiding toxicity.
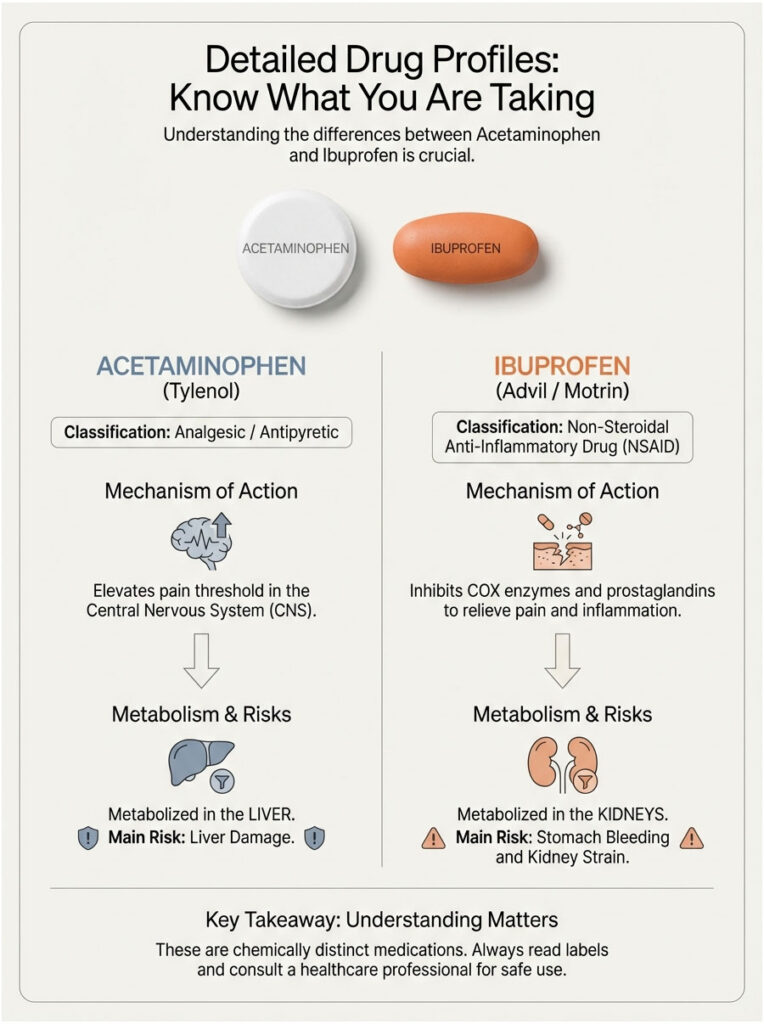
| Feature | Acetaminophen (Tylenol) | Ibuprofen (Advil/Motrin) |
| Drug Class | Analgesic / Antipyretic | NSAID |
| Primary Action | Elevates pain threshold in CNS | Inhibits COX enzymes & prostaglandins |
| Metabolism Site | Liver (Hepatic) | Kidneys (Renal) |
| Primary Toxicity Risk | Liver Damage (Hepatotoxicity) | Stomach Bleeding / Kidney Strain |
| Anti-Inflammatory? | No | Yes |
| Take with Food? | Optional | Highly Recommended |
Metabolic Pathways: Why It Is Safe to Combine Them
Safety is usually the first concern, and rightfully so. The reason you can take Tylenol and ibuprofen together without immediate toxicity comes down to their “exit routes” from the body.
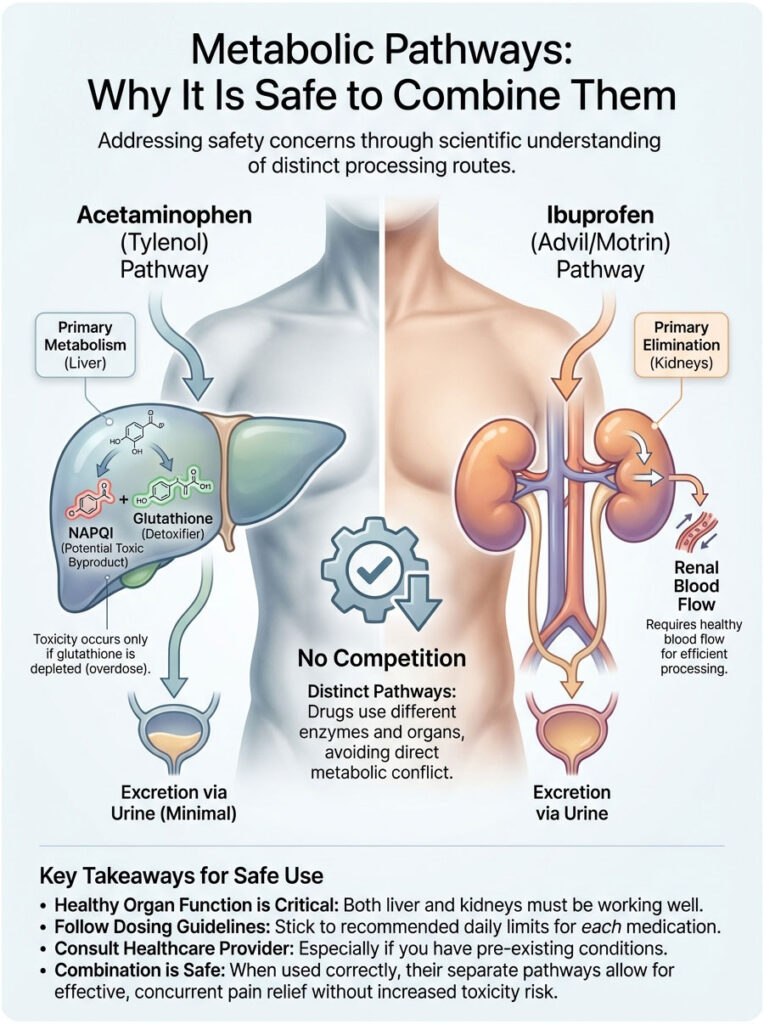
Acetaminophen is processed almost entirely by the liver through a process called conjugation. If the liver gets overwhelmed, it produces a toxic byproduct called NAPQI. At normal doses, the liver handles this without any trouble.
Ibuprofen, on the other hand, is primarily processed and eliminated by the kidneys. It depends on renal blood flow to be filtered out. Because these two drugs do not compete for the same metabolic pathway, they do not overload a single organ system when taken together, as long as your liver and kidney function are healthy.
Dosing Strategy 1: The Simultaneous “Knockout” Method
Knowing you can take Tylenol and ibuprofen together is only half the picture. How you take them matters just as much. In clinical practice, we recommend two primary strategies depending on the type of pain you are dealing with. The first is simultaneous dosing.
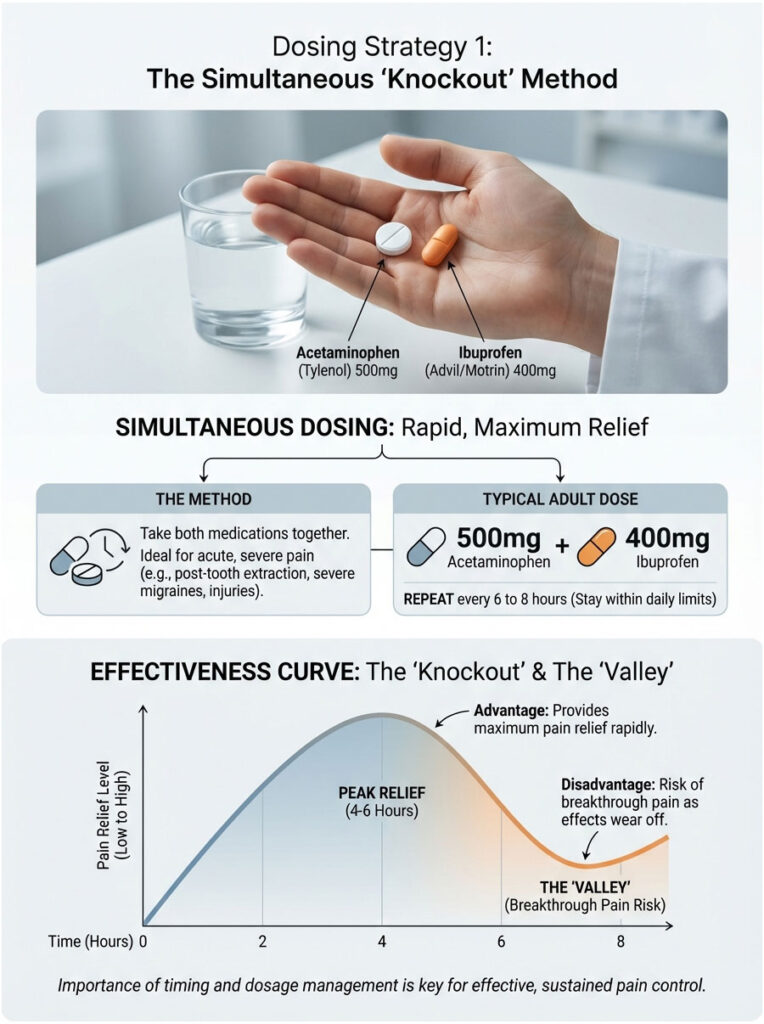
This means taking both pills at the exact same time. It creates a high peak of pain relief and is best suited for acute, severe pain, like the first 24 hours after a tooth extraction, a severe migraine, or right after an injury like a sprain or fracture.
For a standard adult, this usually looks like 500mg of acetaminophen combined with 400mg of ibuprofen. You can repeat this every 6 to 8 hours, but you must stay under the daily maximums for both drugs.
The advantage is simplicity and power. You get the maximum possible relief all at once. The downside is the “valley” effect. Since both drugs wear off around the same time (roughly the 4 to 6 hour mark), you may experience a sharp return of pain before your next dose is safe. This is often called breakthrough pain.
Dosing Strategy 2: The Staggered “Steady State” Method
Staggering Tylenol and ibuprofen is often the better method for sustained issues like the flu, persistent fevers, or post-injury recovery that stretches over several days. The goal is to maintain a steady level of pain relief so you never hit that painful “crash.”
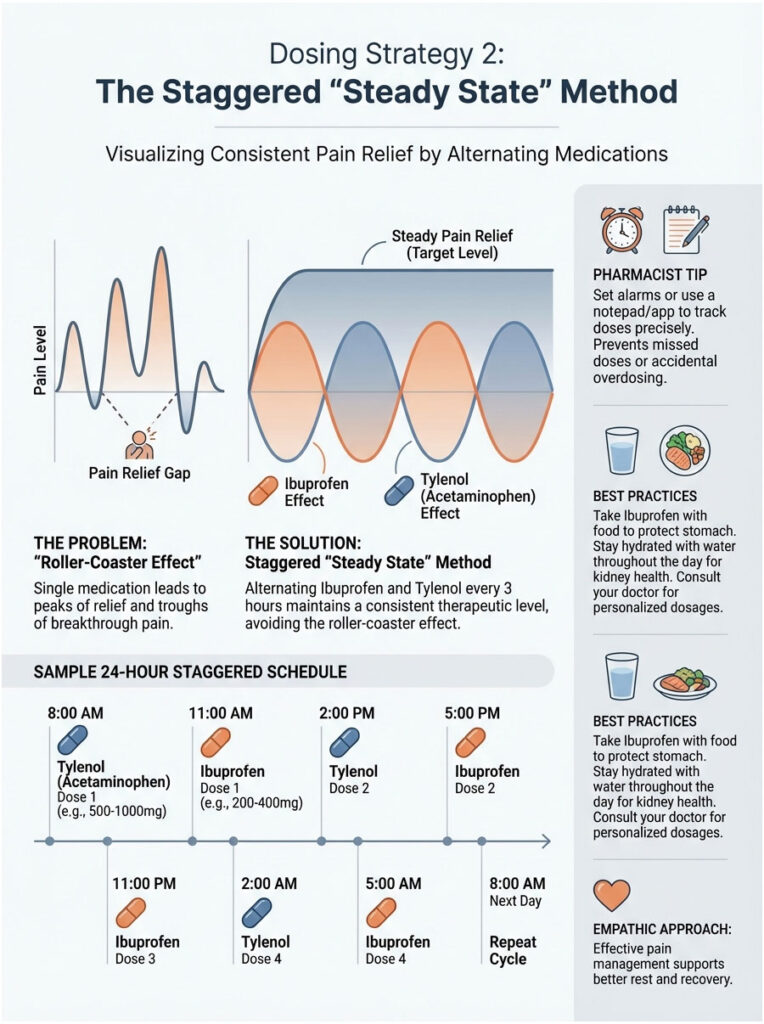
By alternating the medications every 3 hours (each individual drug taken every 6 hours), you make sure that as one medication dips, the other is reaching its peak. This prevents the roller-coaster effect of pain returning before your next dose is due. It takes a bit more attention to the clock, but it provides the smoothest coverage.
Pharmacist Tip: The Alarm Trick
When you are staggering medications, confusion is your enemy. It is incredibly easy to forget which pill you took last. I always tell my patients to set phone alarms or keep a simple notepad handy. Write down the time and the specific drug immediately after taking it. Do not rely on memory when you are in pain or running a fever.
Sample 24-Hour Staggered Schedule
| Time | Medication | Dosage | Notes |
| 8:00 AM | Ibuprofen | 400 mg | Take with breakfast to protect stomach |
| 11:00 AM | Acetaminophen | 500 mg | Can take on an empty stomach |
| 2:00 PM | Ibuprofen | 400 mg | Take with a snack or milk |
| 5:00 PM | Acetaminophen | 500 mg | Stay hydrated |
| 8:00 PM | Ibuprofen | 400 mg | Take with dinner |
| 11:00 PM | Acetaminophen | 500 mg | Before bed |
Maximum Daily Limits: The Line You Must Not Cross
You absolutely must respect the dosage ceiling. Taking more than recommended does not give you extra relief. It only increases toxicity. This is called the analgesic ceiling. Once you hit it, the receptors in your body are saturated. Adding more drug molecules will not stop more pain, but it will put serious strain on your liver and kidneys.
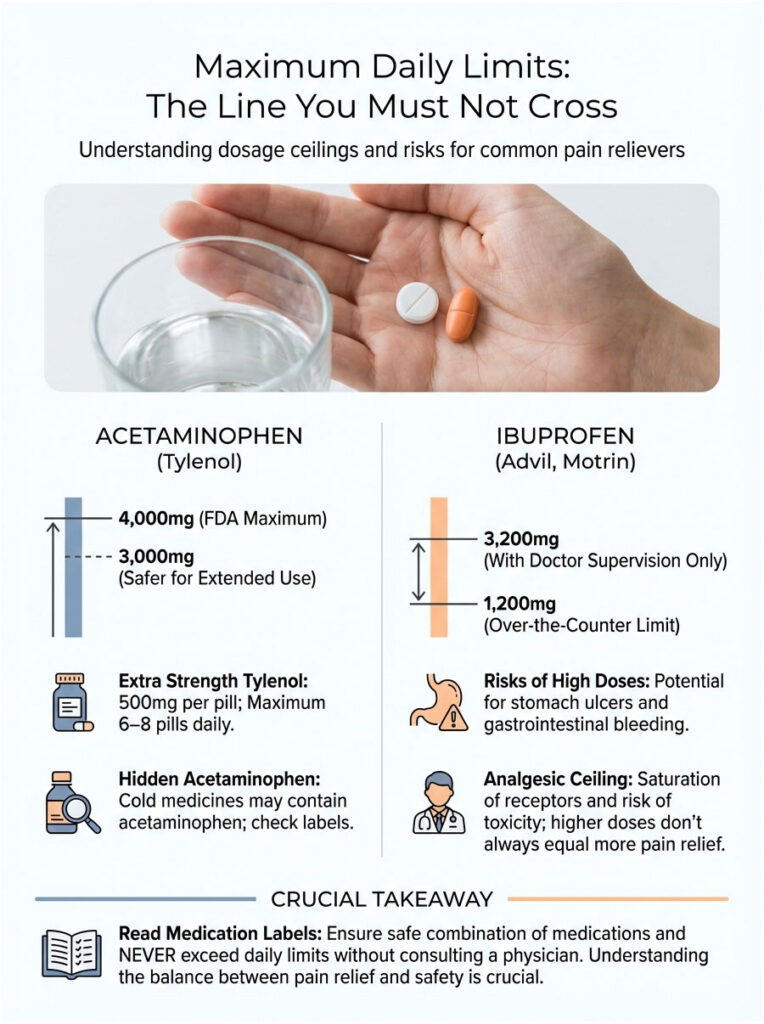
Acetaminophen Limits
The FDA sets the limit at 4,000mg per day for healthy adults. However, many liver specialists and pharmacists prefer a safety buffer of 3,000mg per day, especially if you are taking it for several days in a row. If you buy Extra Strength Tylenol, each pill is 500mg. That means 6 to 8 pills is your absolute daily maximum.
Watch out for hidden acetaminophen. Cold medicines like NyQuil and DayQuil also contain acetaminophen. Taking Tylenol alongside these products can accidentally push you into the overdose zone. Always read the Drug Facts label on every cold and flu product.
Ibuprofen Limits
The over-the-counter limit is generally 1,200mg per day, which works out to six 200mg tablets. Under a doctor’s supervision, this can go up to 3,200mg, but never attempt high doses without medical approval. High doses of ibuprofen taken over extended periods are a leading cause of stomach ulcers and gastrointestinal bleeding.
Critical Safety Risks and Contraindications
While the answer to “can you take Tylenol and ibuprofen together” is yes for most people, it is not a free pass for everyone. These drugs carry serious risks if misused or if you have underlying health conditions. Let us look at the specific organs involved.
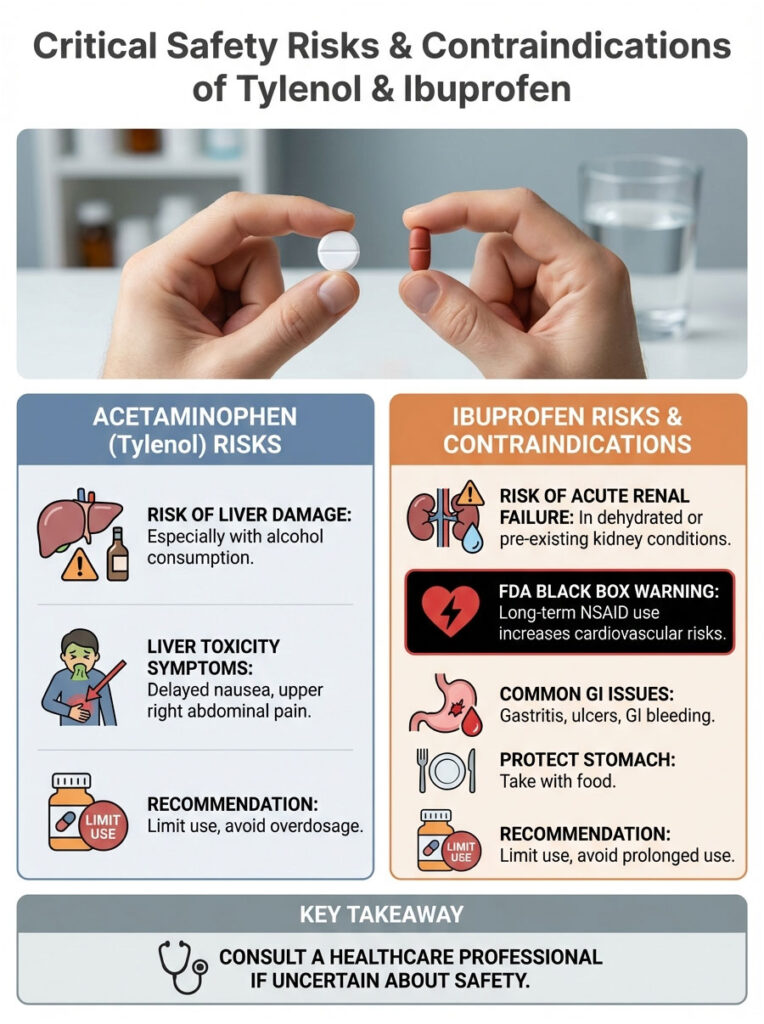
Liver Damage (Hepatotoxicity)
Acetaminophen is generally safe, but it has a narrow therapeutic window. The liver metabolizes it using a substance called glutathione. If you take too much Tylenol, or if you drink alcohol (which depletes glutathione), toxic byproducts build up. This can lead to acute liver failure.
This is why mixing alcohol with acetaminophen is strongly warned against. If you are having more than three alcoholic drinks a day, you should not take Tylenol. The combination acts like a double hit to your liver cells. Symptoms of liver toxicity are often delayed and can be vague, like nausea or pain in the upper right side of your abdomen, making it a silent danger.
Kidney Damage and Cardiovascular Risk
Ibuprofen affects the kidneys. NSAIDs constrict blood vessels leading into the kidneys, which can reduce blood flow. For a healthy person, this effect is temporary and harmless. For someone who is dehydrated or has existing kidney problems, it can trigger acute renal failure.
Long-term NSAID use also carries an FDA Black Box Warning regarding cardiovascular events. This means they can increase the risk of heart attack or stroke, particularly in people with pre-existing heart conditions. The risk goes up the longer you use them. This is why ibuprofen is meant for short-term use only.
Gastrointestinal Injury
The most common complaint I hear about ibuprofen is stomach pain. Prostaglandins protect the stomach lining. When ibuprofen blocks them to reduce pain, it also thins that protective mucus layer. This leaves the stomach wall exposed to acid, which can lead to gastritis, ulcers, and GI bleeding. Always take ibuprofen with food. A few crackers or a glass of milk is usually enough to buffer the acid.
Who Should Avoid This Combination?
Certain groups need to exercise extreme caution or avoid this combination entirely. If you fall into any of these categories, the general advice that taking Tylenol and ibuprofen together is safe does not apply to you without a doctor’s explicit approval.
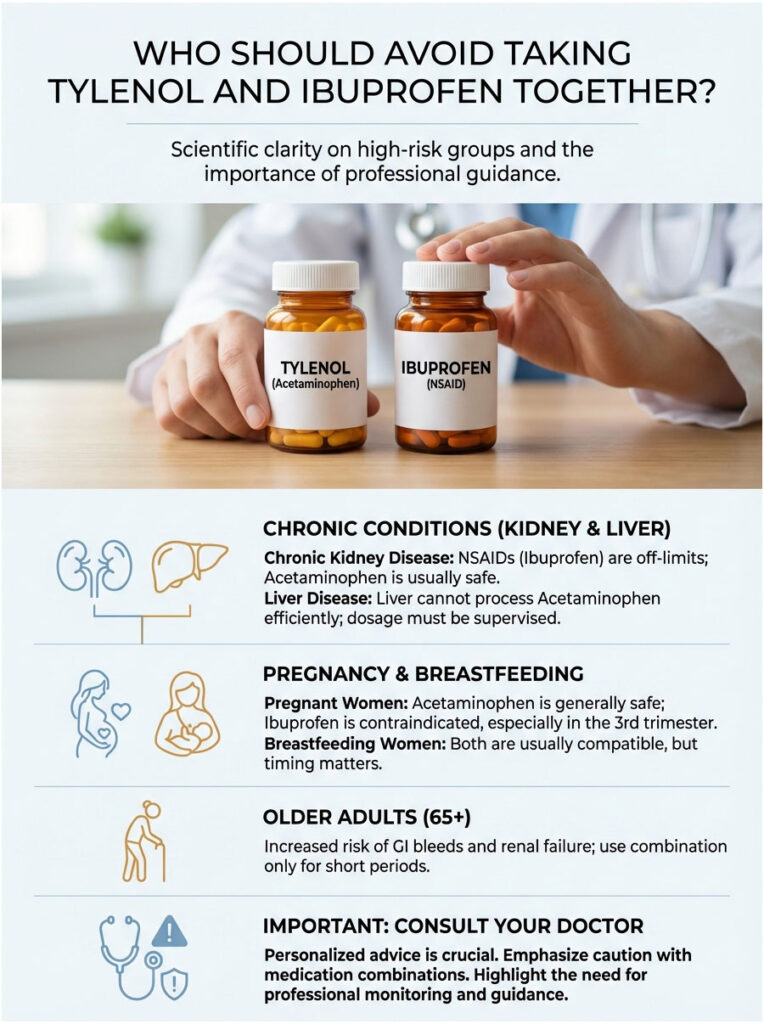
Patients with Chronic Kidney Disease
If you have any stage of kidney disease, NSAIDs like ibuprofen are typically strictly off-limits. The reduction in renal blood flow can cause permanent damage to already compromised kidneys. Acetaminophen is usually the only safe option. Patients on dialysis or with elevated creatinine levels must avoid NSAIDs entirely.
Patients with Liver Disease
For those with cirrhosis, hepatitis, or a history of heavy alcohol use, the liver cannot process acetaminophen efficiently. While small doses might be allowed under strict supervision, the standard dosing schedule is dangerous. Safe dosage in this population is drastically lower or may not exist at all.
Pregnant and Breastfeeding Women
This comes up frequently. Acetaminophen is generally considered safe during pregnancy (Category B). Ibuprofen is a different story. It is generally contraindicated, especially in the third trimester, as it can cause premature closure of the ductus arteriosus in the fetus, a vital blood vessel. Always consult your OB-GYN. For breastfeeding, both are usually considered compatible, but timing matters to minimize transfer to breast milk.
Older Adults (65+)
As we age, our organs process drugs more slowly. The Beers Criteria, a guideline for medication use in older adults, lists NSAIDs as potentially inappropriate due to high risk of GI bleeds and renal failure. Seniors should only use the acetaminophen and ibuprofen combination for very short periods and ideally start with Tylenol alone. Older adults are also more likely to be on other medications that interact with NSAIDs.
Drug Interactions to Watch For
You are probably taking other things, whether that is vitamins, supplements, or prescription medications. Drug interactions are a major source of preventable hospitalizations. Before you open both bottles, check your current medication list against these common interactions.
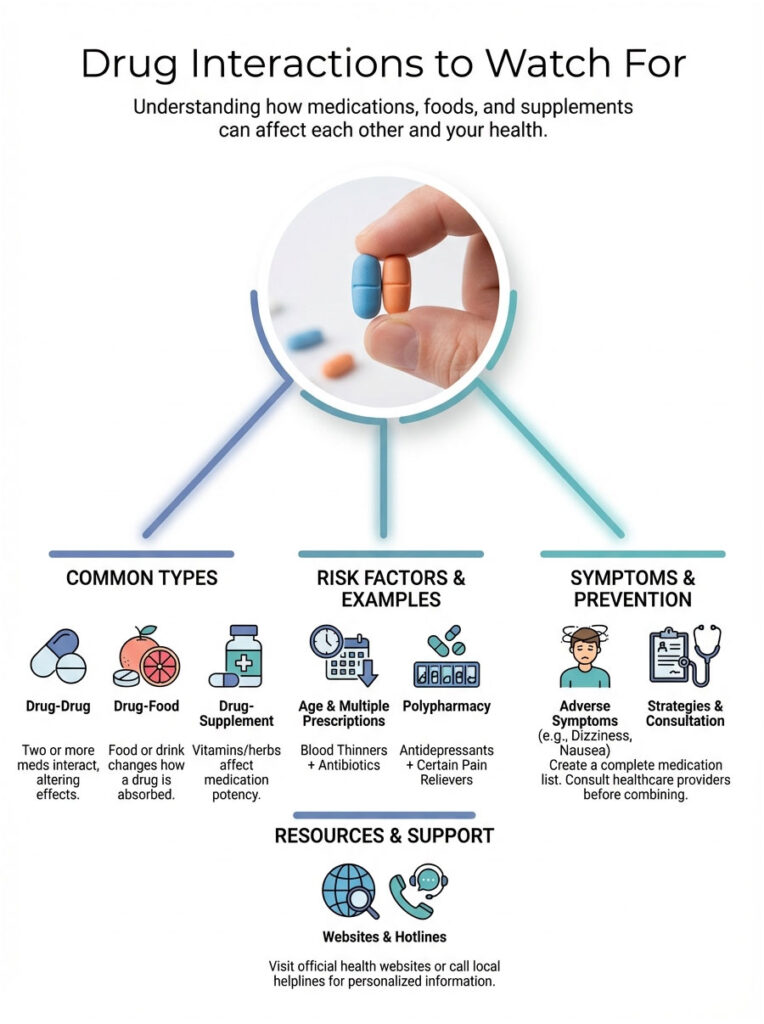
- Blood Thinners (Warfarin, Eliquis, Xarelto): Ibuprofen has anti-platelet effects. Combining it with blood thinners significantly raises the risk of internal bleeding. Tylenol is the safer choice here, though even Tylenol can interact with Warfarin at high doses.
- Blood Pressure Meds (ACE Inhibitors, Diuretics): Ibuprofen can reduce the effectiveness of these drugs and put extra strain on the kidneys. If you are on Lisinopril or a water pill like Hydrochlorothiazide, ask your doctor before combining Advil and Tylenol.
- SSRI Antidepressants: Drugs like Zoloft or Prozac can increase bleeding risk when combined with NSAIDs. This happens because serotonin plays a role in platelet aggregation.
- Hidden Acetaminophen in Cold Medicines: This is a classic mistake. Patients take Tylenol for a fever, then take NyQuil for a cough. NyQuil contains acetaminophen. You have just accidentally doubled your dose. Always read the Drug Facts label on every cold and flu product.
Fixed-Dose Combination Pills: The Advil Dual Action Option
For decades, patients had to buy two separate bottles and do the math themselves. Recognizing how well this strategy works, the pharmaceutical industry responded. In 2020, the FDA approved Advil Dual Action, a fixed-dose combination pill containing 250mg of acetaminophen and 125mg of ibuprofen.
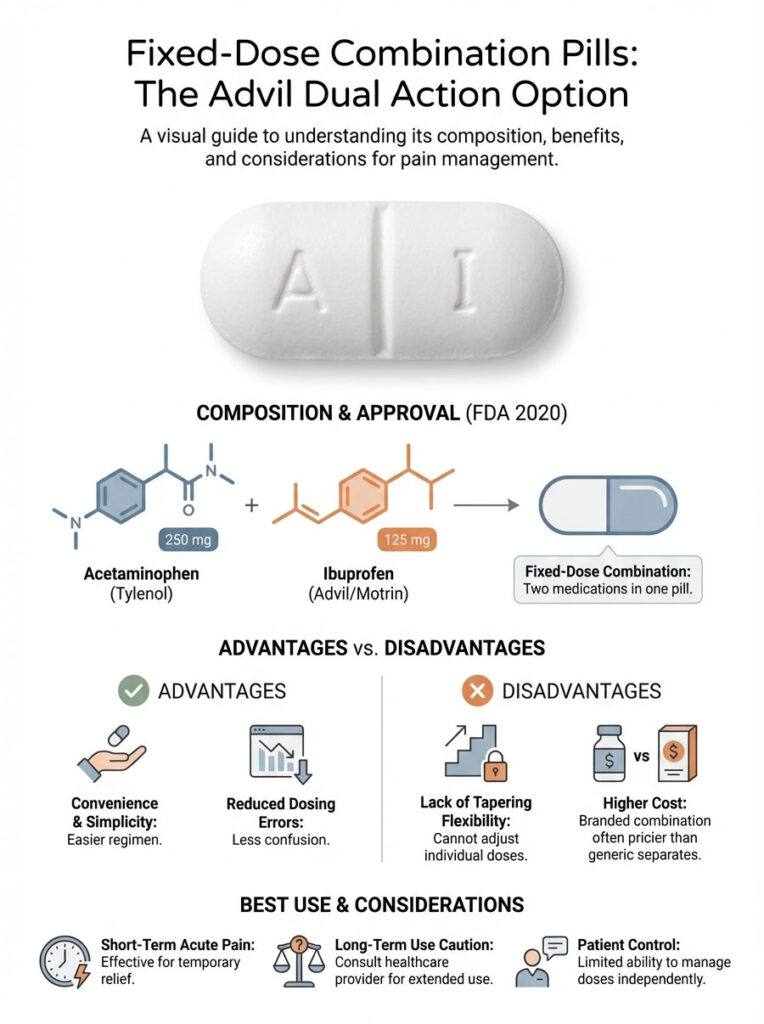
Is it better? That depends on your needs. The advantage is convenience. It prevents dosing errors and simplifies the whole regimen. You do not need to set alarms or remember which pill you took last. The downside is flexibility. With separate pills, you can taper off the ibuprofen (to protect your stomach) while keeping the Tylenol going. With a combo pill, you are locked into both.
For short-term acute pain, the fixed-dose option is excellent. For longer tapering schedules, separate bottles give you more control. Cost is another factor. Generic bottles of ibuprofen and acetaminophen purchased separately are significantly cheaper per dose than the branded combination product.
Common Myths vs. Medical Facts
There is a lot of misinformation floating around about pain relief. Let us clear up a few common myths about this combination.

Myth: “Taking more pills makes them work faster.”
Fact: Absorption time depends on your stomach emptying rate and the drug’s chemistry. A double dose will not speed up relief. It will only increase your toxicity risk.
Myth: “I should take the pills before the pain starts.”
Fact: For surgical or anticipated pain (like after a dental procedure), this is actually true. It is easier to prevent a pain spike than to bring it down once it has built up. For general aches, though, wait until symptoms appear.
Myth: “Tylenol coats the stomach.”
Fact: Tylenol does not coat the stomach. It simply does not irritate the lining the way ibuprofen does. It is gentle on the stomach, but it offers no protective coating.
Final Takeaways
So, can you take Tylenol and ibuprofen together? Yes. It is a scientifically backed, clinically effective strategy for managing acute pain and high fevers. By attacking pain centrally with Tylenol and peripherally with ibuprofen, you achieve superior relief. This multimodal approach allows many patients to skip stronger, more addictive prescription painkillers.
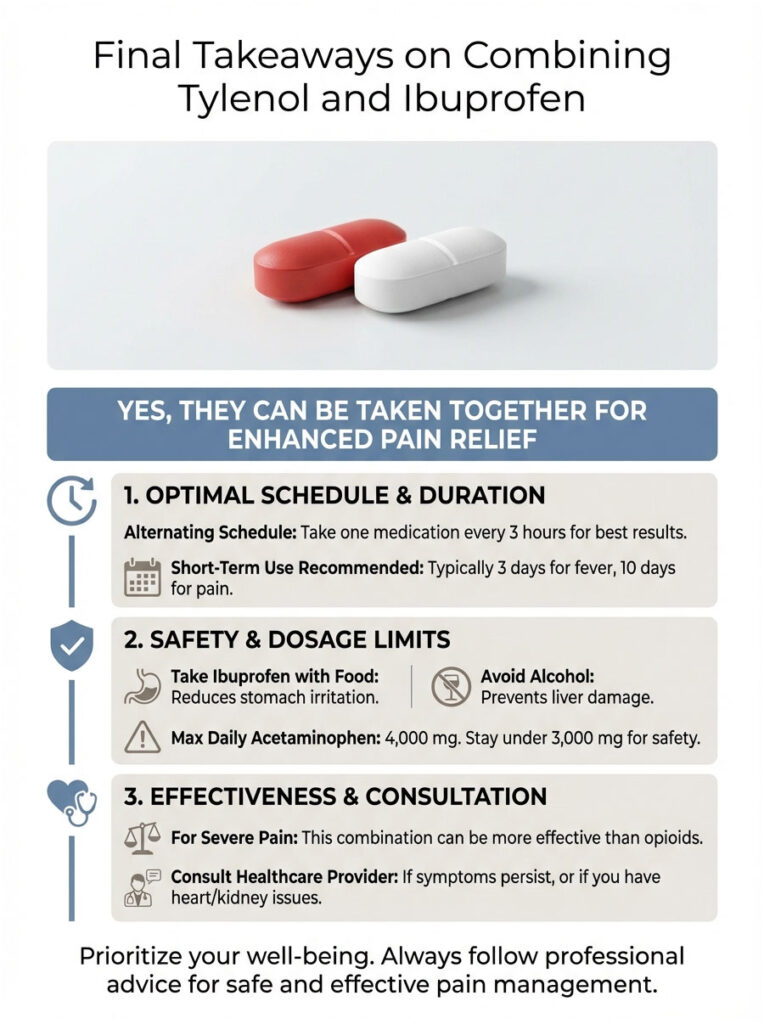
The Golden Rules:
- Respect the Organs. Tylenol affects the liver. Ibuprofen affects the kidneys and stomach. Know your own health history.
- Watch the Clock. Use a staggered schedule (every 3 hours) for sustained relief, or simultaneous dosing (every 6-8 hours) for a knockout effect.
- Hydrate and Eat. Always take ibuprofen with food and drink plenty of water to support kidney function.
- Know Your Limits. Stop if you experience stomach pain, ringing in your ears, or dizziness. These are signs your body has had enough.
Remember, this advice applies to short-term use, typically 3 days for fever and 10 days for pain. If your symptoms persist beyond that, put the bottles down and see a professional. Pain is a signal from your body that something is wrong. Medication silences the signal, but it does not always fix the problem.
Frequently Asked Questions
Is it safe to take Tylenol and ibuprofen at the same time?
Yes, clinical pharmacists often recommend this multimodal analgesia approach because the drugs are metabolized by different organs—the liver for Tylenol and the kidneys for ibuprofen. Taking them together provides a synergistic effect, meaning they work better in combination than either does alone. Always ensure you stay within the daily maximum dosage for each medication to avoid toxicity.
What is the best schedule for staggering Tylenol and ibuprofen?
For sustained relief, I recommend an alternating schedule where you take one medication every six hours, but stagger them so you are taking a dose every three hours. For example, take ibuprofen at 8:00 AM, Tylenol at 11:00 AM, and ibuprofen again at 2:00 PM. This steady state method prevents the return of breakthrough pain as one drug’s efficacy begins to wane.
How many milligrams of acetaminophen can I take in 24 hours?
The FDA sets the absolute maximum limit at 4,000 mg per day for healthy adults, though many clinical guidelines suggest staying under 3,000 mg for added safety. Exceeding these limits poses a severe risk of hepatotoxicity, or liver damage, especially if taken over several days. Always check the labels of other medications, like cold and flu products, to ensure they do not contain hidden acetaminophen.
Why is it better to take ibuprofen with food?
Ibuprofen is a Non-Steroidal Anti-Inflammatory Drug (NSAID) that can irritate the gastric mucosa by inhibiting protective prostaglandins in the stomach lining. Taking it with a small meal or a glass of milk helps mitigate the risk of gastritis or stomach ulcers. Acetaminophen, conversely, is generally safe to take on an empty stomach as it does not affect the stomach lining.
Can I drink alcohol while taking Tylenol and ibuprofen?
It is highly recommended to avoid alcohol, particularly when taking acetaminophen, as both substances are processed by the liver and can deplete glutathione stores. This double hit significantly increases the risk of acute liver failure. If you consume more than three alcoholic drinks daily, you should consult a healthcare provider before using these medications.
Is the combination of Tylenol and ibuprofen more effective than opioids?
Research indicates that for acute issues like dental pain, the combination of acetaminophen and ibuprofen is often more effective than prescription narcotics like codeine. This multimodal approach targets pain through both the central nervous system and peripheral inflammation. It is a preferred clinical strategy to manage severe pain while avoiding the addiction risks associated with opioid use.
What are the risks of taking ibuprofen if I have heart or kidney issues?
Ibuprofen can reduce renal blood flow and increase the risk of cardiovascular thrombotic events, which is why it carries a Black Box Warning for those with pre-existing heart conditions. Patients with chronic kidney disease (CKD) should generally avoid NSAIDs entirely, as they can trigger acute renal failure. In these cases, acetaminophen is typically the safer analgesic alternative.
Can I take Advil Dual Action instead of two separate pills?
Advil Dual Action is an FDA-approved fixed-dose combination that provides 250 mg of acetaminophen and 125 mg of ibuprofen in a single tablet for convenience. While this simplifies the dosing regimen and reduces the chance of errors, separate bottles allow for more flexible tapering of individual medications. Choose the combination pill for short-term acute relief, but stick to separate bottles if you need to adjust doses independently.
Is it safe to take ibuprofen and Tylenol during pregnancy?
Acetaminophen is generally considered safe during pregnancy when used at recommended doses, but ibuprofen should be avoided, especially during the third trimester. NSAIDs can cause the premature closure of the ductus arteriosus in the fetus, leading to serious complications. Always consult your OB-GYN before starting any medication regimen while pregnant or breastfeeding.
How long does it take for the Tylenol and ibuprofen combination to start working?
Most patients begin to feel relief within 30 to 60 minutes after ingestion, as both medications have similar onset times. For acute or anticipated pain, such as after a surgical procedure, taking the medications before the pain peaks is more effective than trying to catch up later. The full analgesic effect typically peaks around the two-hour mark.
What are the warning signs that I should stop taking these medications?
You should immediately discontinue use and contact a provider if you experience symptoms like ringing in the ears (tinnitus), severe stomach pain, or signs of an allergic reaction. Other red flags include dark urine or yellowing of the skin, which may indicate liver distress, or sudden swelling and decreased urination, which can signal kidney strain. These medications are intended for short-term use, usually not exceeding 10 days for pain.
Does Tylenol treat inflammation like ibuprofen does?
No, acetaminophen is an analgesic and antipyretic that works primarily in the central nervous system to elevate your pain threshold and reduce fever. It lacks the significant anti-inflammatory properties found in NSAIDs like ibuprofen, which work peripherally to inhibit COX enzymes and reduce swelling. This is exactly why the combination is so effective; one reduces the sensation of pain while the other treats the underlying inflammation.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. I am a pharmacist, but I am not your pharmacist. Always consult a qualified healthcare professional or your primary physician before starting any new medication regimen, especially if you have pre-existing health conditions, are pregnant, or are taking other prescription drugs.
References
- U.S. Food and Drug Administration (FDA) – fda.gov – Official guidelines on Acetaminophen (Tylenol) daily dosage limits and liver safety warnings.
- Cochrane Library – cochranelibrary.com – Clinical review of the efficacy of combining paracetamol and ibuprofen for acute postoperative pain.
- National Kidney Foundation – kidney.org – Information regarding the impact of NSAIDs like ibuprofen on renal blood flow and kidney health.
- American Liver Foundation – liverfoundation.org – Expert insights on hepatotoxicity and the risks of mixing acetaminophen with alcohol.
- Journal of the American Dental Association (JADA) – jada.ada.org – Research data comparing multimodal analgesia (Tylenol + Ibuprofen) to opioid-based pain management.
- FDA Drug Approvals – accessdata.fda.gov – Approval documentation for the first fixed-dose combination of ibuprofen and acetaminophen (2020).








