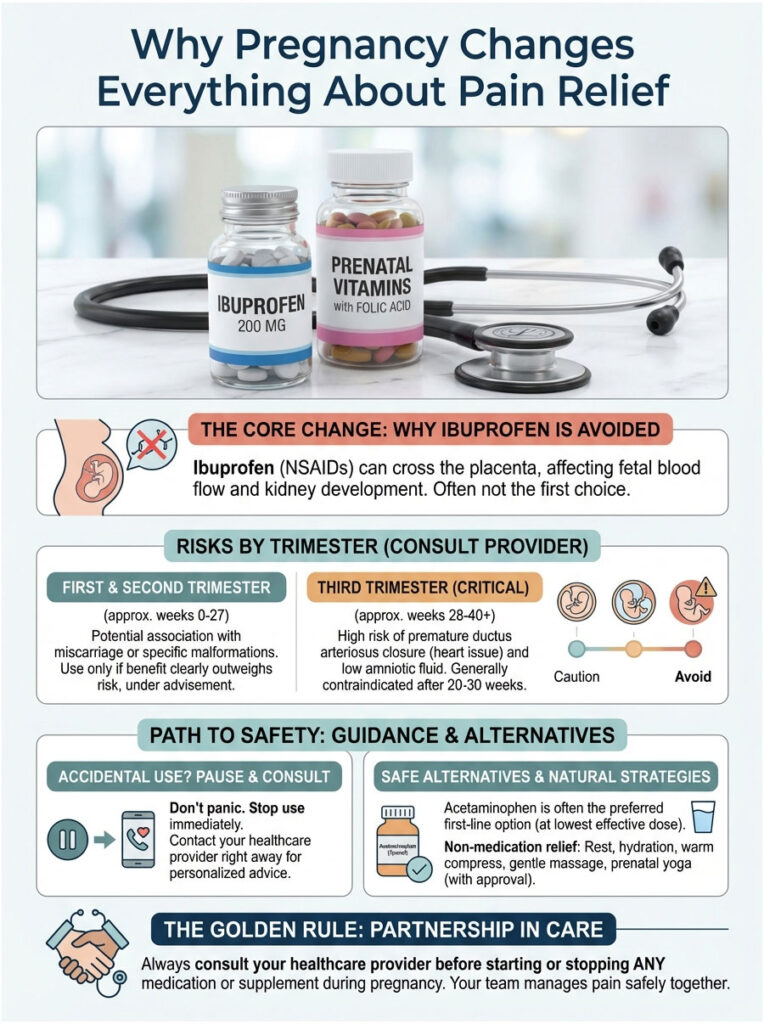
Quick Answer: In most cases, no. Ibuprofen is generally avoided during the first trimester because of miscarriage concerns, and it is strictly off-limits after 20 weeks due to serious risks to your baby’s kidneys and heart. Acetaminophen (Tylenol) is the preferred pain reliever during pregnancy. Always check with your obstetrician before taking any NSAID.
Table of Contents
Why Pregnancy Changes Everything About Pain Relief
Pregnancy comes with aches and pains that most people don’t expect. Between headaches, round ligament pain, back soreness, and the occasional fever, your first thought might be to reach for ibuprofen (sold as Advil or Motrin). Before you were pregnant, it probably worked like a charm. But now? The rules are completely different.
“Can you take ibuprofen while pregnant?” is one of the most common questions we hear in obstetrics. As someone who works in maternal-fetal medicine, I regularly see patients who are worried because they popped a pill before they even knew they were expecting. Others are dealing with pain so severe that functioning without relief feels impossible.
The answer is nuanced, but the safety guidelines exist for very good reasons. In this guide, we will walk through the actual science behind why ibuprofen is risky during pregnancy, break down the dangers trimester by trimester, cover what to do if you accidentally took some, and lay out the safe alternatives that can keep you comfortable.
Key Statistics and Data Points
- FDA Warning (2020): The FDA formally advises against all NSAID use after 20 weeks of gestation due to the risk of fetal renal dysfunction.
- Miscarriage Risk: Some research suggests that NSAID use around the time of conception may increase spontaneous abortion risk by up to 50% (American Journal of Obstetrics & Gynecology).
- Prevalence: Despite warnings, roughly 28% of pregnant women report taking ibuprofen at some point during pregnancy.
- Amniotic Fluid Impact: Low amniotic fluid (oligohydramnios) can develop within 48 hours of regular NSAID use in the second half of pregnancy.
- Acetaminophen Use: Acetaminophen remains the most widely recommended pain reliever for pregnant women and is used by over 65% of expecting mothers in the U.S.
How NSAIDs Work in the Pregnant Body
To really understand the risks, it helps to know what ibuprofen actually does inside your body. Ibuprofen is a Non-Steroidal Anti-Inflammatory Drug (NSAID). It works by blocking two enzymes, COX-1 and COX-2, which stops your body from making prostaglandins.
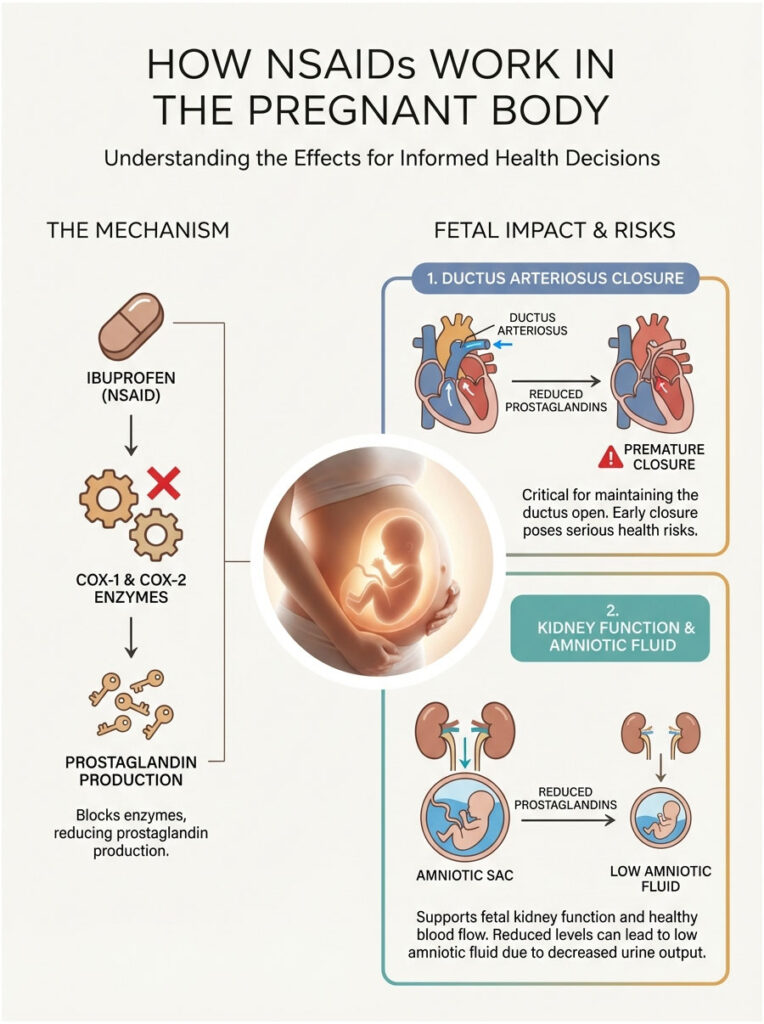
For a non-pregnant adult, fewer prostaglandins means less pain, lower fever, and reduced swelling. That is why ibuprofen is so effective in everyday life. But in a developing baby, prostaglandins serve a completely different and essential purpose.
Why Prostaglandins Matter for Your Baby
Inside the fetal circulatory system, prostaglandins are not just involved in inflammation. They are critical maintenance workers. One of their most important jobs is keeping a blood vessel called the ductus arteriosus open. This vessel allows blood to bypass the baby’s fluid-filled lungs and sends oxygen-rich blood directly where it is needed.
If ibuprofen suppresses prostaglandin production, that vessel can constrict or even close too early, which is a serious problem.
On top of that, fetal kidneys depend on prostaglandins to maintain healthy blood flow. When prostaglandin levels drop, kidney function slows down. Since amniotic fluid in the second half of pregnancy is mostly made up of fetal urine, reduced kidney output leads directly to dangerously low amniotic fluid levels.
First Trimester Risks (Weeks 0 to 12): Miscarriage and Birth Defects
The first trimester is the period of organogenesis, when your baby’s organ systems are being built from scratch. This is the window when the fetus is most vulnerable to teratogens (substances that can cause birth defects).
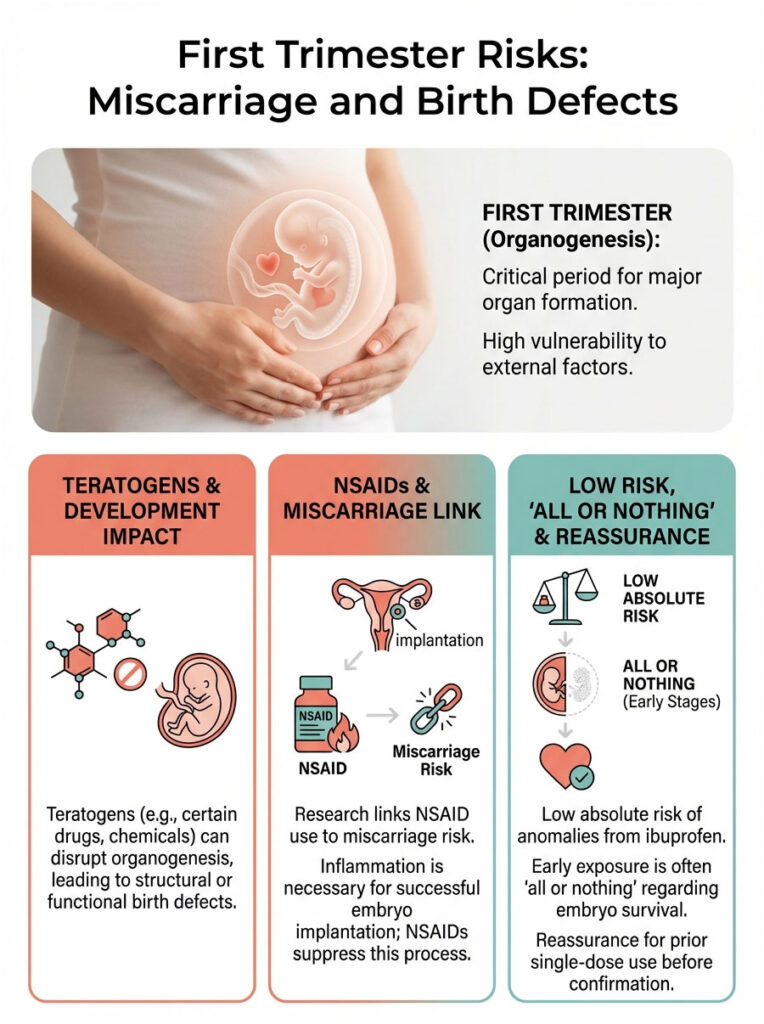
The Miscarriage Connection
Research from the American Journal of Obstetrics & Gynecology has found a link between NSAID use and spontaneous abortion. The leading theory is that successful embryo implantation in the uterine wall actually requires a small amount of inflammation. By taking a strong anti-inflammatory drug, you might unintentionally interfere with that delicate attachment process.
Possible Congenital Anomalies
While the absolute risk is low, studies have examined possible connections between taking ibuprofen in the first trimester and certain birth defects, including:
- Gastroschisis: A defect where the abdominal wall does not close properly, allowing intestines to protrude.
- Cardiac Septal Defects: Commonly referred to as “holes” in the heart.
- Cleft Palate: Problems with the formation of the lip or mouth.
A note if you took a dose before you knew: If you took a single dose of ibuprofen before finding out you were pregnant, especially in the first four weeks, try not to panic. This very early phase is often considered “all or nothing.” The embryo typically either survives completely unaffected, or it does not implant at all. A single exposure rarely causes a structural defect.
Second Trimester (Weeks 13 to 27): The Gray Zone and the 20-Week Cutoff
The second trimester is the period that confuses many patients. You might hear conflicting advice from friends or older family members. Years ago, doctors treated this window as a relatively safer time for occasional NSAID use. But our understanding has changed, and the guidelines are now much stricter.
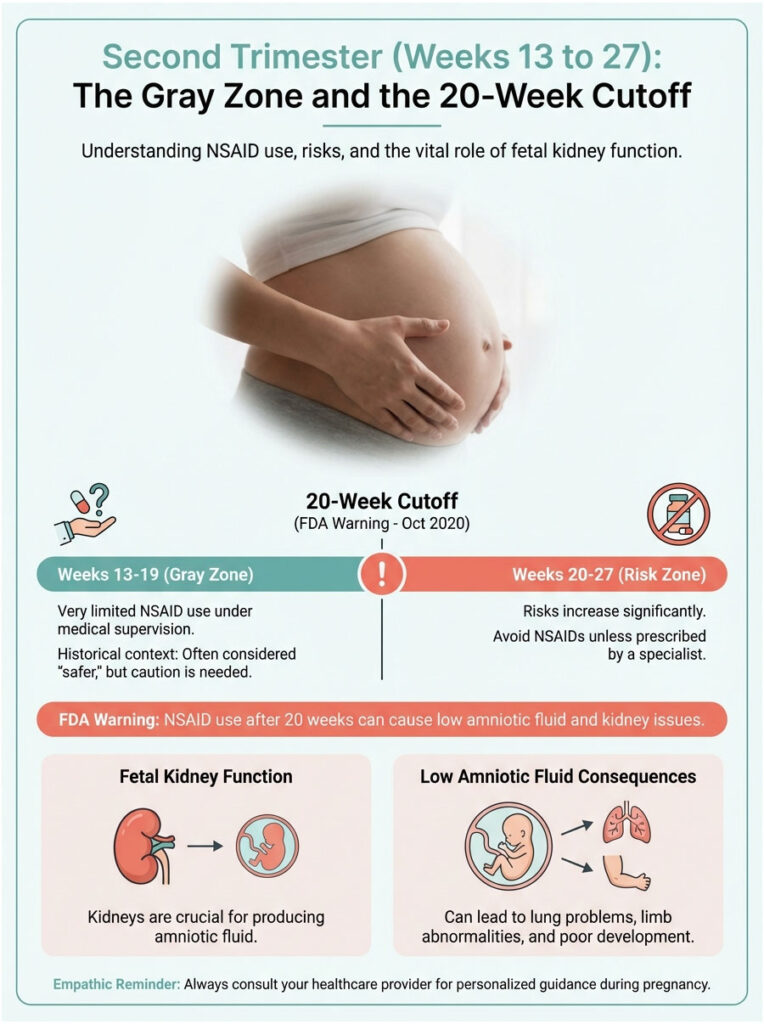
Weeks 13 to 19: Very Limited Use, Only Under Medical Supervision
Between weeks 13 and 19, the risk of miscarriage drops significantly. The risk of premature ductus closure is also lower than in the third trimester. In rare and severe situations, a doctor might prescribe a very short course of NSAIDs, perhaps if a mother is passing a kidney stone or dealing with debilitating migraines. This kind of use is typically limited to 48 hours, never for self-medication, and always managed by a physician.
The FDA Warning at 20 Weeks and Beyond
In October 2020, the FDA released a formal Drug Safety Communication warning against NSAID use after 20 weeks of gestation. They required updated labeling on all NSAIDs to reflect this risk.
Why 20 weeks specifically? This is the point in pregnancy when fetal kidneys become the main producers of amniotic fluid. Taking ibuprofen after this milestone can trigger fetal renal dysfunction. Here is the chain reaction:
- The mother takes ibuprofen.
- The drug crosses the placenta.
- Fetal kidney blood vessels constrict.
- The baby’s urine output drops.
- Amniotic fluid levels fall (oligohydramnios).
Low amniotic fluid is dangerous because it cushions the umbilical cord, protects the baby, and allows the lungs to develop properly. Without enough fluid, the baby may develop lung hypoplasia (underdeveloped lungs) or limb contractures.
Third Trimester (Weeks 28 to Birth): Cardiac and Delivery Risks
Once you reach the third trimester, the answer to “Can you take ibuprofen while pregnant” becomes a firm no. The risks shift from kidney concerns to immediate cardiac dangers for the baby.
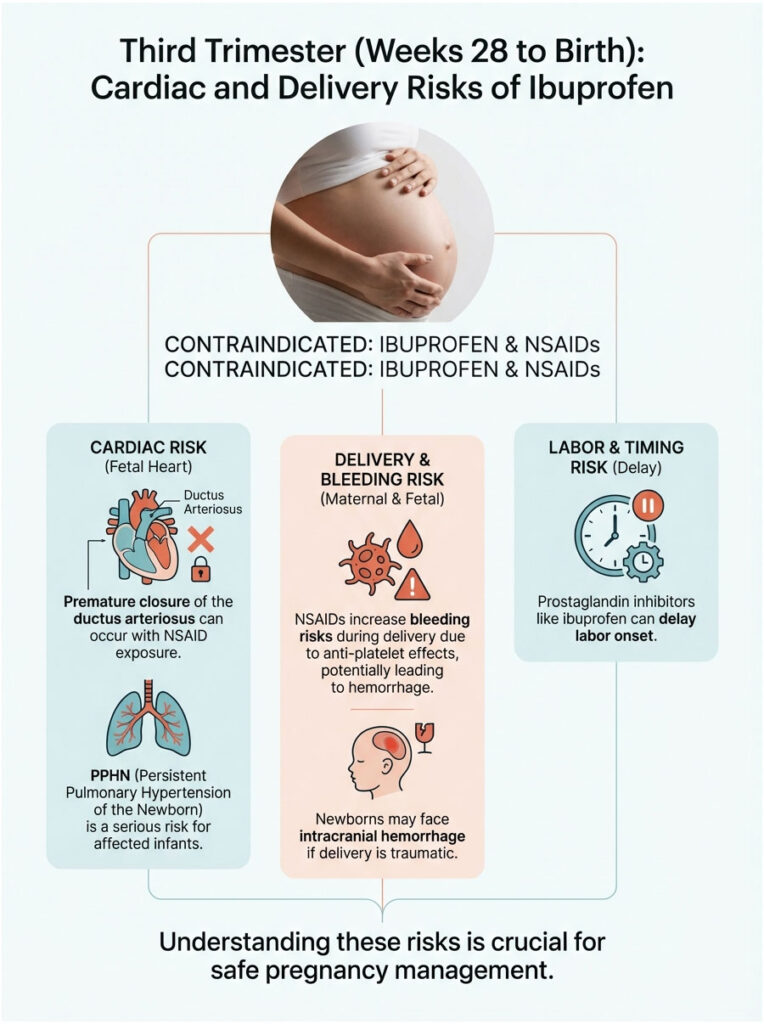
Premature Closure of the Ductus Arteriosus
The ductus arteriosus becomes extremely sensitive to NSAIDs in the third trimester. Exposure to ibuprofen can cause it to constrict while the baby is still in the womb. This forces blood into the lungs before they are ready, leading to a life-threatening condition called Persistent Pulmonary Hypertension of the Newborn (PPHN). Babies with PPHN often need intensive care immediately after birth.
Bleeding Risks and Labor Inhibition
NSAIDs also have an anti-platelet effect, meaning they thin the blood. Taking them close to your delivery date raises the risk of hemorrhage during birth. It can also increase the chance of intracranial hemorrhage (brain bleeding) in the newborn, especially if the delivery is traumatic or involves instruments.
There is another catch, too. Prostaglandins are the hormones that tell your cervix to ripen and your uterus to contract. Taking a prostaglandin inhibitor like ibuprofen can delay or prolong labor.
Pain Relief Safety Comparison During Pregnancy
The table below compares the most common pain medications and their safety profiles throughout pregnancy.

| Medication | Generic Name | 1st Tri | 2nd Tri | 3rd Tri | Primary Risks |
| NSAID | Ibuprofen (Advil, Motrin) | Avoid | Avoid (after 20 wks) | Contraindicated | Low fluid, ductus closure, miscarriage |
| Analgesic | Acetaminophen (Tylenol) | Safe | Safe | Safe | Liver toxicity in high doses only |
| Salicylate | Aspirin (High Dose) | Avoid | Avoid | Contraindicated | Bleeding, cardiac risks like NSAIDs |
| Salicylate | Aspirin (Low-Dose, 81mg) | Safe (Rx) | Safe (Rx) | Safe (Rx) | Used to prevent preeclampsia; MD supervision |
| Opioid | Codeine / Oxycodone | Caution (Rx) | Caution (Rx) | Caution (Rx) | Neonatal withdrawal, respiratory depression |
What to Do If You Accidentally Took Ibuprofen While Pregnant
It happens. You have a pounding headache, you are exhausted, and you grab the wrong bottle from the counter before thinking twice. If you accidentally took ibuprofen during pregnancy, here is the action plan we recommend.
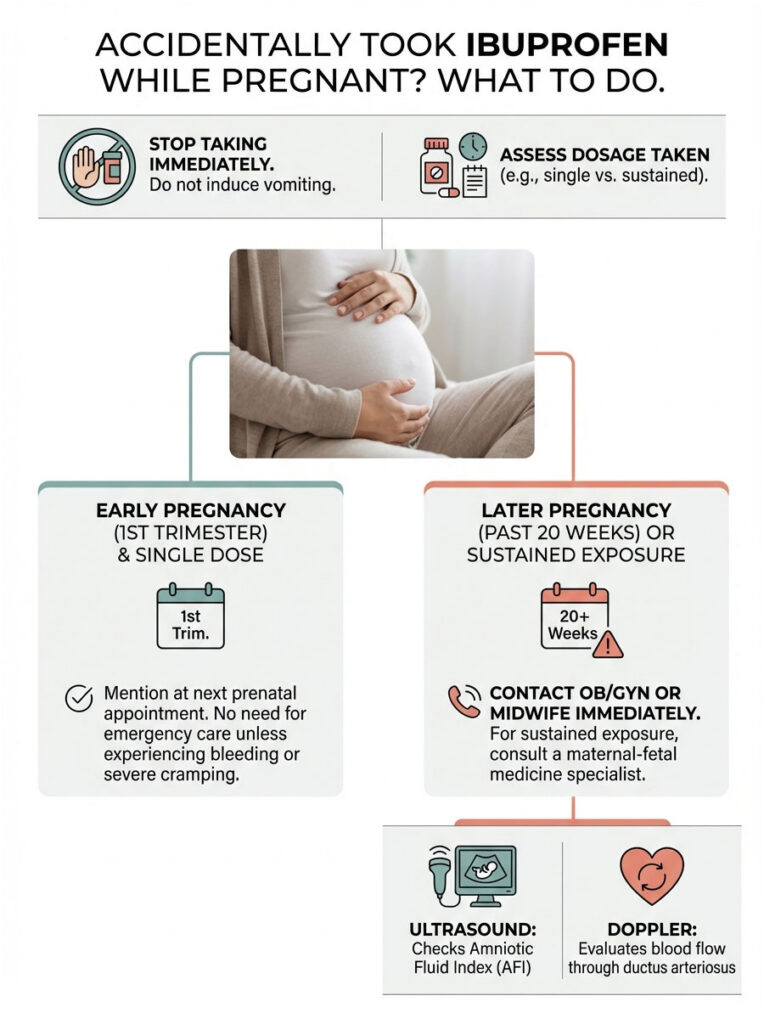
Immediate Steps
First, stop taking the medication right away. Do not try to induce vomiting. Ibuprofen absorbs quickly, and vomiting just adds unnecessary stress. Next, figure out how much you took. Was it a single 200mg pill, or have you been taking 600mg every six hours for several days? The risk profile is very different depending on the dose and duration.
When to Contact Your Doctor
If you are in your first trimester and took a single dose, simply mention it at your next prenatal appointment. There is no need to rush to the ER unless you are experiencing bleeding or severe cramping. However, if you are past 20 weeks, call your OB/GYN or midwife right away.
For sustained exposure (more than a day or two), a maternal-fetal medicine specialist may order an ultrasound to check the Amniotic Fluid Index (AFI). This tells us whether the baby’s kidneys are working properly. We may also use Doppler ultrasound to evaluate blood flow through the ductus arteriosus and make sure it has not started to narrow.
Safe Alternatives for Pain Management During Pregnancy
Just because ibuprofen is off the table does not mean you need to suffer in silence. Unmanaged pain causes stress, which raises cortisol, and that is not ideal for your baby either. The goal is to find relief safely.
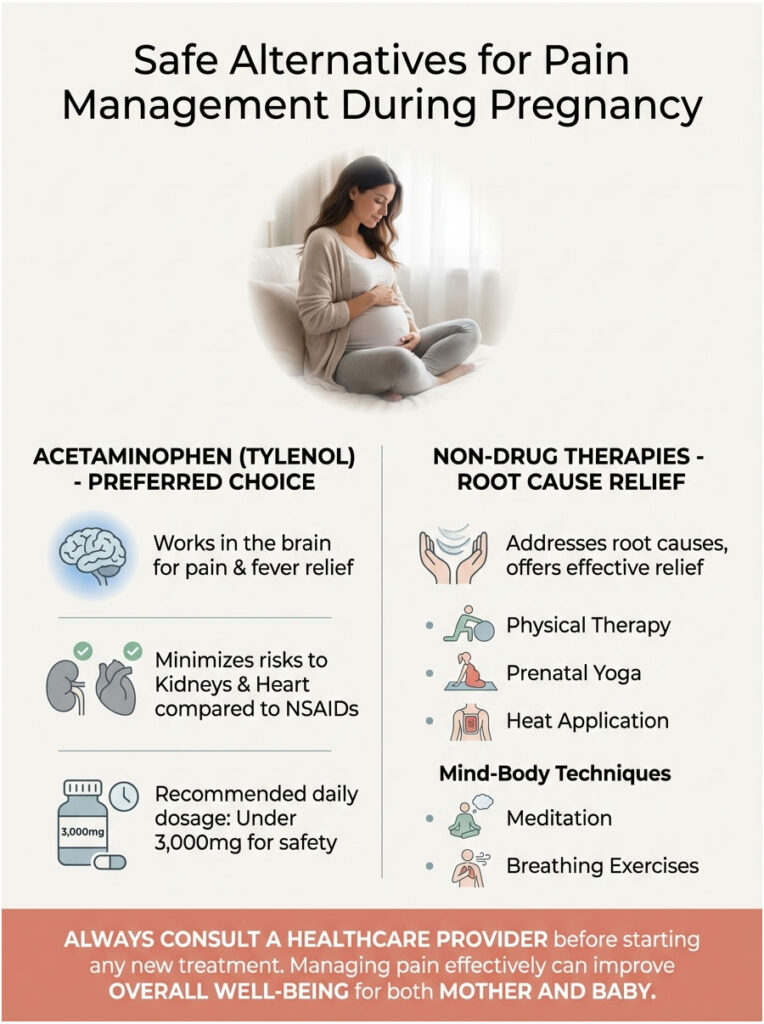
Acetaminophen (Tylenol): The First-Line Choice
When patients ask about acetaminophen vs. ibuprofen during pregnancy, the answer is straightforward. Acetaminophen is the go-to option for pain and fever in all three trimesters. It works in the brain rather than blocking prostaglandins in body tissues, so it does not carry the same kidney or cardiac risks as NSAIDs. Stick to the lowest effective dose, generally under 3,000mg per day.
Non-Drug Therapies That Actually Help
Many times, effective pain relief during pregnancy means treating the root cause, not just masking the symptom.
- Magnesium: Great for tension headaches and leg cramps. Most pregnant women are actually magnesium deficient.
- Hydration and Electrolytes: Your blood volume expands by roughly 50% during pregnancy. Dehydration is a leading trigger for headaches and uterine irritability.
- Physical Therapy: For pelvic girdle pain or sciatica, a physical therapist who specializes in the pelvic floor can often provide more relief than any pill.
- Belly Support Bands: These can lift the weight of the uterus off your lower back and bladder, offering real relief.
- Acupuncture: Many women report significant improvement in back pain and nausea with regular acupuncture sessions.
Special Considerations and Common Questions
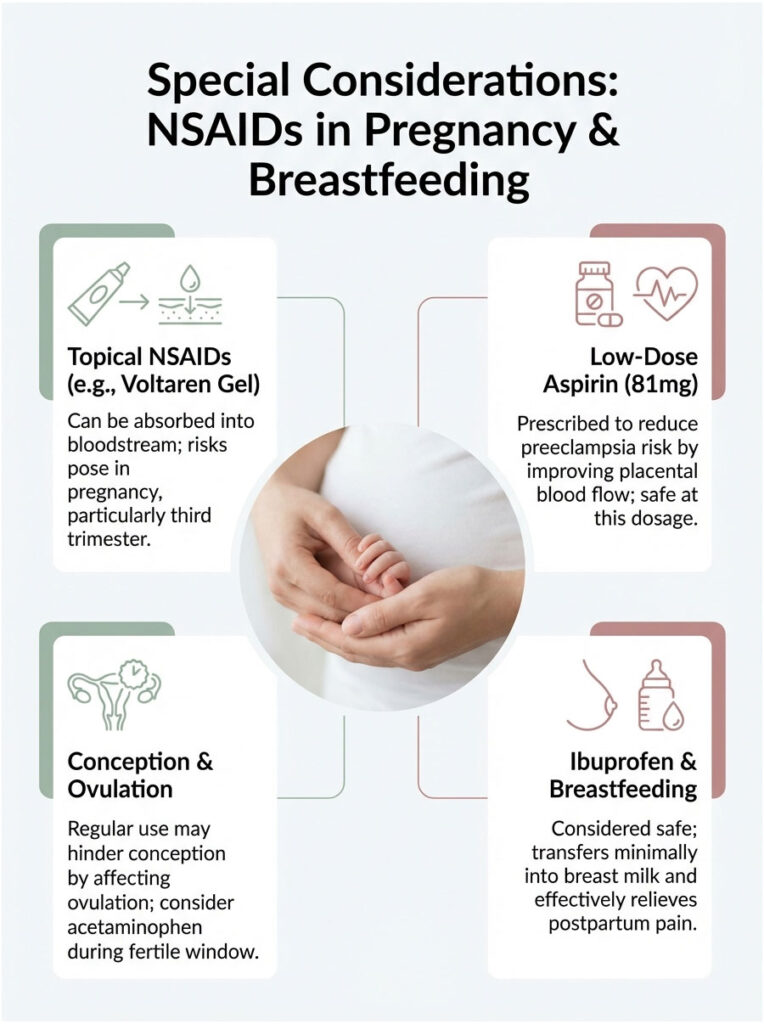
Can You Use Topical NSAIDs Like Voltaren Gel While Pregnant?
Patients often assume that because Voltaren is a cream, it stays on the skin and never reaches the baby. While systemic absorption from topical NSAIDs is lower than from a pill, it is not zero. NSAIDs do get absorbed into the bloodstream through the skin. For that reason, we generally advise against using topical NSAIDs in the third trimester, since the potential effects on the fetal heart remain a concern.
Is Ibuprofen Safe While Breastfeeding?
Here is where the rules change. Once your baby is born, ibuprofen is actually preferred over opioids for postpartum pain. Very little of it transfers into breast milk, and the American Academy of Pediatrics considers it safe for breastfeeding mothers. It works especially well for the cramping pain (afterpains) that comes as the uterus shrinks back to its normal size.
NSAIDs and Trying to Conceive
If you are trying to get pregnant, regular NSAID use might actually be working against you. Prostaglandins play a role in ovulation, specifically in helping the follicle rupture and release the egg. High doses of NSAIDs can cause something called Luteinized Unruptured Follicle Syndrome, where the egg never releases. If you are struggling to conceive, switching to acetaminophen during your fertile window is worth considering.
Why Does My Doctor Prescribe Baby Aspirin If NSAIDs Are Risky?
This is a common source of confusion. Low-dose aspirin (81mg) is technically a salicylate, but at this small dosage it works differently than a full-strength NSAID. It selectively targets platelets to prevent clots and improve blood flow to the placenta, which reduces the risk of preeclampsia. At this low dose, it does not have the same strong effect on fetal kidneys or the ductus arteriosus that a 200mg+ dose of ibuprofen would. It is considered safe specifically because the dose is low and the clinical benefit is high.
Trimester-by-Trimester Quick Reference
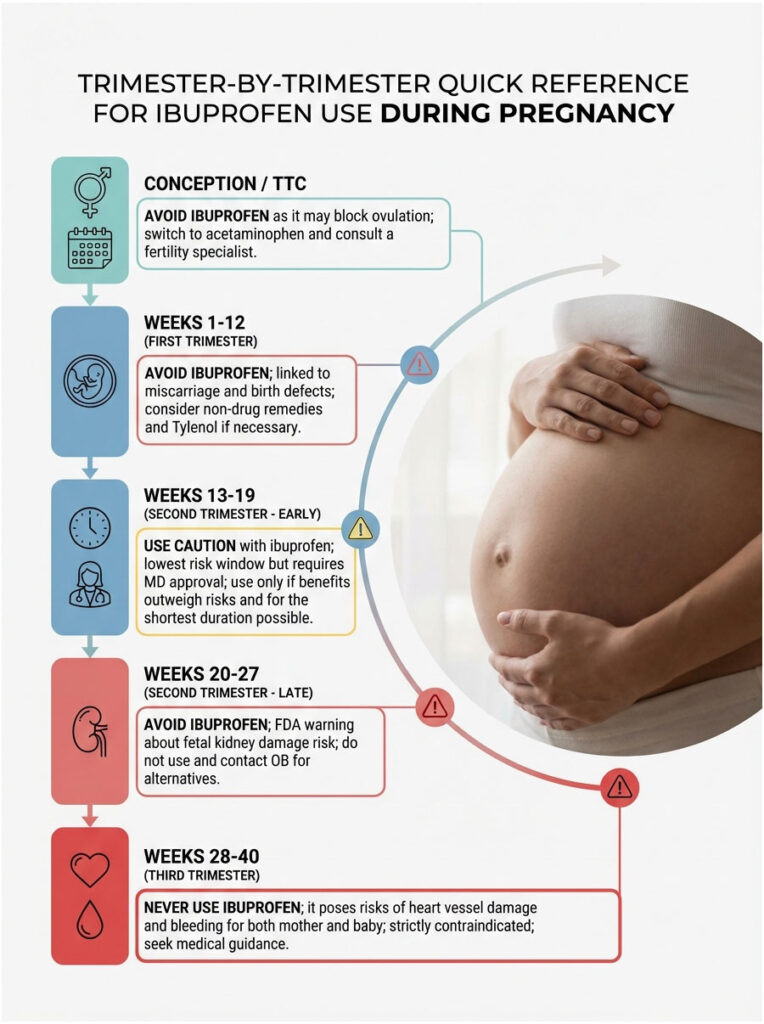
Use this as a quick-reference guide:
| Stage | Ibuprofen? | Why? | What to Do Instead |
| Conception / TTC | Avoid | May block ovulation | Switch to acetaminophen; consult fertility specialist |
| Weeks 1-12 | Avoid | Linked to miscarriage and defects | Non-drug remedies; Tylenol if needed |
| Weeks 13-19 | Caution | Lowest risk window, but still needs MD approval | Only if benefits outweigh risks; shortest course possible |
| Weeks 20-27 | Avoid | FDA warning: fetal kidney damage risk | Do not use; contact OB for alternatives |
| Weeks 28-40 | NEVER | Heart vessel damage; bleeding risk to mother and baby | Strictly contraindicated; seek medical guidance |
Final Thoughts
“Can you take ibuprofen while pregnant?” is one of those questions in obstetrics where the answer is almost always no, especially from 20 weeks onward. Ibuprofen might be a household staple for everyday aches, but it is not safe during pregnancy. Your growing baby’s kidneys and the temporary vessels in their heart are extremely sensitive to how NSAIDs work, and the consequences can be severe.

That said, this does not mean you need to white-knuckle your way through nine months of discomfort. Pain management is a real and valid medical need. The key is swapping your toolkit. Replace NSAIDs with acetaminophen. Stay well hydrated. Look into physical therapy. Keep an open line of communication with your provider. If you have a chronic condition that normally requires anti-inflammatory medication, talk to your doctor as soon as you find out you are pregnant. In most cases, there are safer alternatives that can keep you comfortable while protecting your baby.
Frequently Asked Questions
Can you take ibuprofen while pregnant?
Generally, ibuprofen is not recommended at any stage of pregnancy and is strictly contraindicated after 20 weeks. It belongs to the NSAID class, which can interfere with fetal development, particularly affecting the baby’s heart and kidneys. Acetaminophen is the clinically preferred alternative for managing pain or fever during gestation.
Does taking Advil in the first trimester increase the risk of miscarriage?
Clinical research suggests that taking NSAIDs like Advil around the time of conception or in early pregnancy may increase the risk of spontaneous abortion by up to 50%. This is likely because prostaglandins, which NSAIDs block, are necessary for the successful implantation of the embryo into the uterine lining.
Why did the FDA issue a warning against using ibuprofen after 20 weeks?
The 2020 FDA warning was issued because NSAID use after 20 weeks gestation can cause rare but serious fetal kidney problems. These renal issues lead to low levels of amniotic fluid (oligohydramnios), which is vital for the baby’s lung development and provides a protective cushion in the womb.
What is the difference between acetaminophen and ibuprofen safety during pregnancy?
Acetaminophen (Tylenol) is considered the first-line analgesic because it works centrally and does not inhibit prostaglandins in fetal tissues. Ibuprofen is a systemic prostaglandin inhibitor, which poses specific risks to the fetal circulatory system and renal function that acetaminophen does not carry.
Can ibuprofen cause heart defects in a developing baby?
In the third trimester, ibuprofen can cause the premature closure of the ductus arteriosus, a critical blood vessel in the fetal heart. If this vessel closes before birth, it can lead to persistent pulmonary hypertension in the newborn, a life-threatening condition requiring neonatal intensive care.
What should I do if I accidentally took ibuprofen before realizing I was pregnant?
If you took a single dose in the very early weeks, try not to panic, as a one-time exposure rarely causes structural defects during the \”all or nothing\” phase of development. You should stop taking the medication immediately and inform your obstetrician at your next prenatal visit to discuss any necessary monitoring.
Is it safe to use topical NSAID gels like Voltaren while pregnant?
While topical NSAIDs have lower systemic absorption than oral pills, the medication still enters your bloodstream and can reach the fetus. Therefore, we generally advise against using products like Voltaren gel, especially after 20 weeks, to avoid any potential impact on fetal kidney or heart health.
How does ibuprofen use affect amniotic fluid levels?
Fetal urine is the primary source of amniotic fluid in the second half of pregnancy, and fetal kidneys require prostaglandins to maintain blood flow. Because ibuprofen blocks these prostaglandins, it can reduce fetal urine output, leading to a condition called oligohydramnios within just 48 hours of use.
Why is low-dose aspirin allowed but ibuprofen is restricted?
Low-dose aspirin (81mg) is used under medical supervision to prevent preeclampsia and improve placental blood flow. At this specific micro-dose, it does not carry the same high risks for fetal renal dysfunction or premature ductus closure that full-strength doses of ibuprofen (200mg or more) do.
Does taking ibuprofen impact fertility or ovulation?
Yes, chronic NSAID use can interfere with the rupture of the follicle, potentially leading to Luteinized Unruptured Follicle Syndrome. If you are trying to conceive, it is best to avoid ibuprofen during your fertile window to ensure successful ovulation and embryo implantation.
Is ibuprofen safe for pain relief while breastfeeding?
Unlike during pregnancy, ibuprofen is considered safe and is often the preferred choice for postpartum pain relief while breastfeeding. Very little of the drug passes into breast milk, and it is highly effective at managing the uterine cramping experienced after delivery.
Can taking NSAIDs like Motrin delay the start of labor?
Prostaglandins are essential for ripening the cervix and triggering uterine contractions during labor. Because ibuprofen is a potent prostaglandin inhibitor, taking it near your due date can potentially delay the onset of labor or prolong the birthing process significantly.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The safety of medication during pregnancy depends on individual health factors and gestational age. Always consult a qualified healthcare professional, such as your obstetrician or midwife, before taking any medication or making health decisions during pregnancy.
References
- U.S. Food and Drug Administration (FDA) – Drug Safety Communication – Official warning regarding NSAID use after 20 weeks gestation and risks of fetal kidney issues.
- American Journal of Obstetrics & Gynecology (AJOG) – ajog.org – Research regarding the correlation between NSAID use during conception and increased miscarriage risk.
- American College of Obstetricians and Gynecologists (ACOG) – acog.org – Clinical guidelines on the management of pain and the use of analgesics during pregnancy.
- Mayo Clinic – Expert Answers – Overview of the safety profile of ibuprofen and potential birth defects.
- National Institutes of Health (NIH) – PubMed Central – Study on the effects of prostaglandin inhibitors on the fetal ductus arteriosus.
- American Academy of Pediatrics (AAP) – healthychildren.org – Information regarding the safety of ibuprofen during the postpartum and breastfeeding period.








