Yes, you can take acetaminophen and ibuprofen together safely. When used correctly, this combination is not only safe but is considered the clinical gold standard for over-the-counter pain relief. Known as multimodal analgesia, it targets pain through two different biological pathways and often provides relief comparable to opioids, without the addiction risk.
Table of Contents
You are standing in the pharmacy aisle with a throbbing headache or a twisted ankle demanding attention. In one hand, you have a bottle of Tylenol. In the other, a bottle of Advil. And you are stuck on the question I hear almost daily in my clinical practice: can you take acetaminophen and ibuprofen together, or is that a dangerous combination?

The short answer is yes. But the difference between a safe pain management strategy and a trip to the emergency room comes down to dosing, timing, and your personal medical history. As a Pharmacotherapy Specialist, I have seen this combination work brilliantly for patients looking to avoid opioids. I have also seen what happens when it is misused.
Modern medicine has moved past the idea of relying on a single “magic bullet” for pain. Instead, we use multimodal analgesia, combining drugs with different mechanisms to create a synergistic effect. By the time you finish this guide, you will know the precise biological interactions at play, how to schedule your doses for maximum coverage, and which red flags should make you stop and call your doctor.
Key Statistics at a Glance
- Combined Efficacy: Clinical trials show this combination provides greater pain relief than either drug alone, or even opioid-acetaminophen combinations, for dental pain.
- Acetaminophen Limit: 4,000mg per 24 hours (healthy adults), though 3,000mg is the preferred safety cap.
- Ibuprofen Limit: 1,200mg per 24 hours (OTC labeling).
- Onset of Action: Combined relief typically kicks in within 30 to 45 minutes.
- Safety Profile: Adverse events stay below 5% when daily maximums are strictly respected.
The Science of Analgesic Synergy: Why This Combination Works
To really understand why you can take acetaminophen and ibuprofen together so effectively, you need to understand analgesic synergy. In pharmacology, synergy happens when two drugs interact to produce a total effect greater than the sum of their individual effects. In this specific case, 1 + 1 truly equals 3.
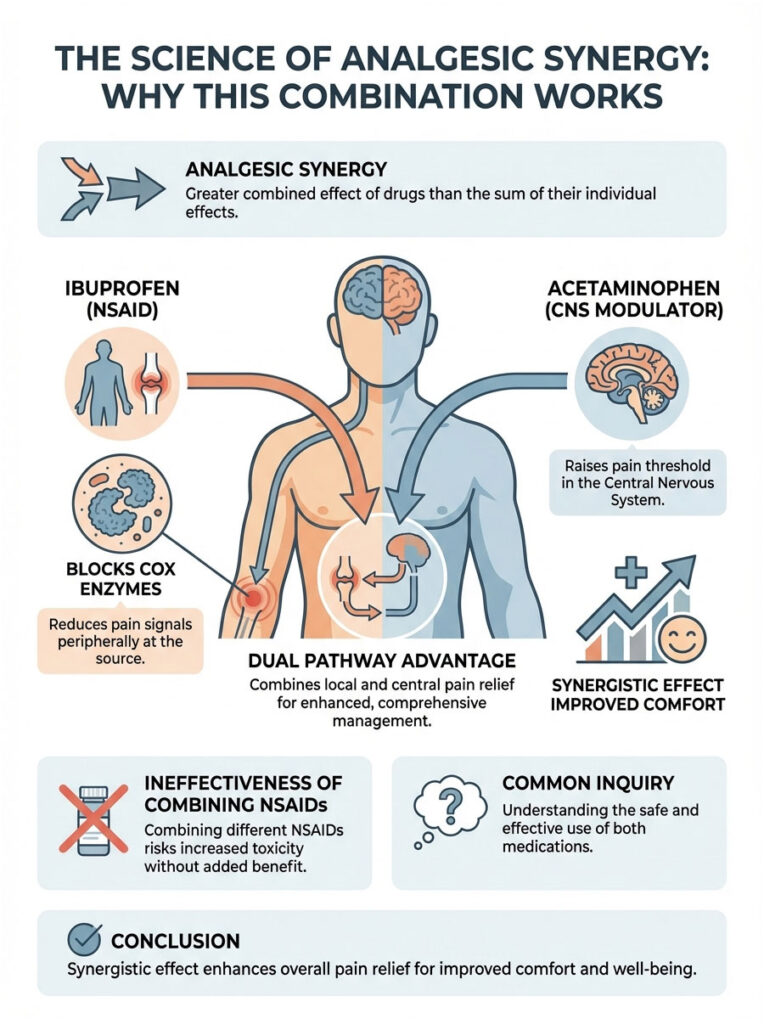
This works because these two medications fight pain on completely different battlefields inside your body. They do not compete for the same receptors, so they work concurrently without blocking each other. This is very different from taking two NSAIDs like ibuprofen and naproxen, which would fight over the same enzymes and increase toxicity without improving pain relief.
Ibuprofen: The Peripheral Defender
Ibuprofen belongs to the Non-Steroidal Anti-Inflammatory Drug (NSAID) class. Its primary mechanism works at the site of injury, the periphery. Whether you have a swollen knee or an inflamed tooth, the trauma triggers a chemical cascade.
When tissue is damaged, your body releases enzymes known as Cyclooxygenase (COX-1 and COX-2). These enzymes produce prostaglandins, lipid compounds that signal inflammation, swelling, and pain to the brain. Ibuprofen blocks these enzymes. By inhibiting COX-2 specifically, it stops prostaglandin production at the source. It effectively turns down the volume of the pain signal before it even travels up the spinal cord to the brain.
Acetaminophen: The Central Modulator
Acetaminophen (APAP) takes a completely different approach. While its exact mechanism is still being actively studied, we know it acts primarily in the Central Nervous System (CNS), the brain and spinal cord. It does not significantly reduce inflammation at the injury site, which is why it is not classified as an NSAID.
What acetaminophen does is elevate your pain threshold. It makes it harder for the brain to register pain signals that do get through. It also acts on the heat-regulating center of the hypothalamus to bring down fever. Recent research suggests it may also influence the endocannabinoid system, which modulates our perception of discomfort.
The Dual Pathway Advantage
Think of pain management like fighting a house fire. Ibuprofen is the team spraying water directly on the flames (the injury site) to put them out. Acetaminophen is the team cooling down the surrounding structure and foundation (the central nervous system) to prevent the heat from spreading. When you use both, you attack the pain from both ends.
This is exactly why “can you take acetaminophen and ibuprofen together” is such a common question. People intuitively feel that one medication alone is not always enough. When you combine them, you dampen the signal at the source and dull the receiver in the brain.
Drug Profiles and Metabolic Pathways
Safety comes down to metabolism. The reason this combination is safer than taking two NSAIDs together is that each drug is processed by a different organ. This distribution of labor prevents placing too much stress on any single organ system, as long as you are generally healthy.
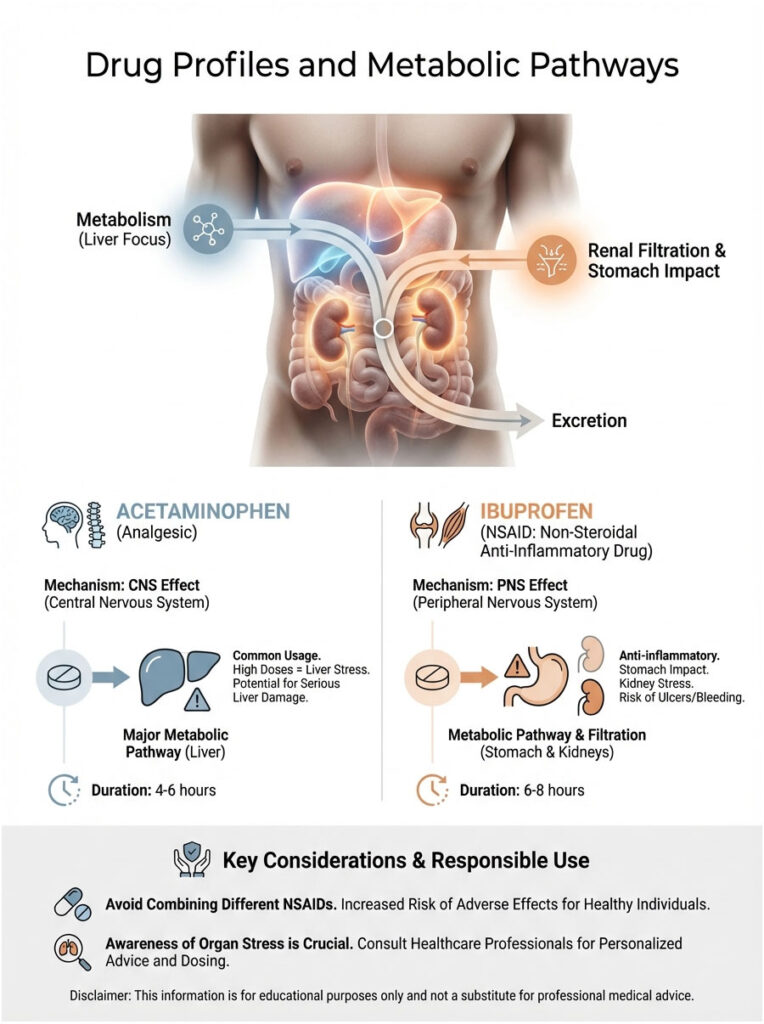
Acetaminophen (Tylenol) Profile
Acetaminophen shows up in hundreds of OTC products. But that familiarity can breed complacency. It is a potent drug with a very specific metabolic pathway.
- Class: Non-aspirin analgesic / Antipyretic.
- Primary Metabolism: Hepatic (Liver).
- The Safety Constraint: Your liver processes acetaminophen into non-toxic compounds that get excreted in urine. However, a small fraction converts into a toxic metabolite called NAPQI (N-acetyl-p-benzoquinone imine). At normal doses, your liver neutralizes NAPQI using a substance called glutathione. If you overdose, glutathione stores run out. Once depleted, NAPQI attacks liver cells and causes necrosis.
Ibuprofen (Advil, Motrin) Profile
Ibuprofen is a powerhouse for inflammation, but it comes with its own biological costs. It is an organic acid derivative that relies on the kidneys for filtration.
- Class: NSAID (Propionic acid derivative).
- Primary Clearance: Renal (Kidneys).
- The Safety Constraint: NSAIDs inhibit prostaglandins. Unfortunately, prostaglandins also protect your stomach lining and maintain blood flow to the kidneys. Chronic use or high doses can strip away that protection, leading to gastric ulcers or reduced kidney function, particularly if you are dehydrated.
Drug Profile Comparison
| Feature | Acetaminophen (Tylenol) | Ibuprofen (Advil/Motrin) |
|---|---|---|
| Drug Class | Analgesic / Antipyretic | NSAID |
| Primary Mechanism | Central Nervous System (Pain Threshold) | Peripheral Nervous System (Inflammation) |
| Primary Organ Stress | Liver (Hepatic) | Kidneys (Renal) and Stomach |
| Anti-Inflammatory? | No | Yes |
| Typical Duration | 4 to 6 hours | 6 to 8 hours |
Practical Dosing Strategies: Schedules That Actually Work
Knowing that you can take acetaminophen and ibuprofen together safely is only half the battle. Knowing how to take them is where the real benefit lies. In clinical pharmacy, we generally recommend one of two strategies depending on your type of pain. Sticking to a schedule is often more important than the dose itself.
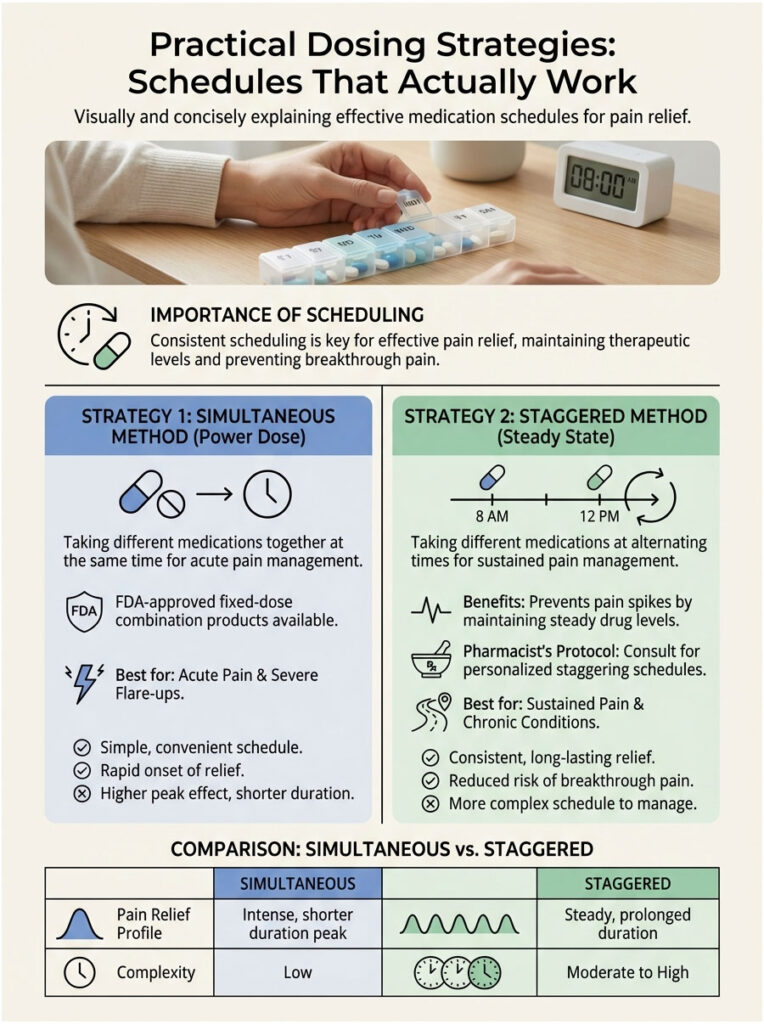
Strategy 1: The Simultaneous Method (The Power Dose)
This approach means taking both medications at the exact same time. It is best reserved for severe, acute pain spikes where you need maximum relief immediately. Think dental extractions, severe back spasms, or acute injuries like fractures.
The FDA recently recognized this method’s value by approving fixed-dose combination products (like Advil Dual Action), which combine both drugs in a single tablet. You can achieve the same result with generic bottles from your medicine cabinet.
- Protocol: Take 500mg Acetaminophen + 400mg Ibuprofen together.
- Frequency: Repeat every 8 hours. Do not shorten the interval to less than 6 hours to avoid ibuprofen accumulation.
- The Benefit: You get a powerful spike in pain relief that hits both pathways at once.
Strategy 2: The Staggered Method (The Steady State)
This is the preferred approach for sustained issues like fevers, viral body aches, or post-surgical recovery. By staggering your medications, you make sure that as one drug’s effect starts to fade, the other is reaching its peak. This maintains a constant level of pain relief in your bloodstream.
This method prevents the “rollercoaster” effect where pain comes roaring back before your next dose. It keeps pain manageable at a baseline level instead of chasing it once it has already spiked.
Pharmacist’s Staggering Protocol:
- 8:00 AM: Acetaminophen (500mg)
- 11:00 AM: Ibuprofen (400mg)
- 2:00 PM: Acetaminophen (500mg)
- 5:00 PM: Ibuprofen (400mg)
Repeat as needed, making sure you do not exceed daily maximums. Notice the 3-hour gap between different drugs, which gives you a 6-hour interval for the same drug.
Dosing Strategy Comparison
| Dosing Strategy | Pros | Cons | Best For |
|---|---|---|---|
| Simultaneous (Together) | Maximum peak relief, fewer pill times | Effects wear off at the same time, higher pill burden at once | Acute injury, severe headache, before sleep |
| Staggered (Alternating) | Constant coverage, no pain rollercoaster | Harder to track, requires watching the clock | Fevers, post-op recovery, all-day pain |
Safety Thresholds: Understanding the Ceiling Effect
In pharmacology, more is not always better. Both drugs have a ceiling effect. Once you reach a certain dosage, taking more provides zero additional pain relief but exponentially increases the risk of toxicity. Knowing these limits is essential for avoiding accidental overdose.
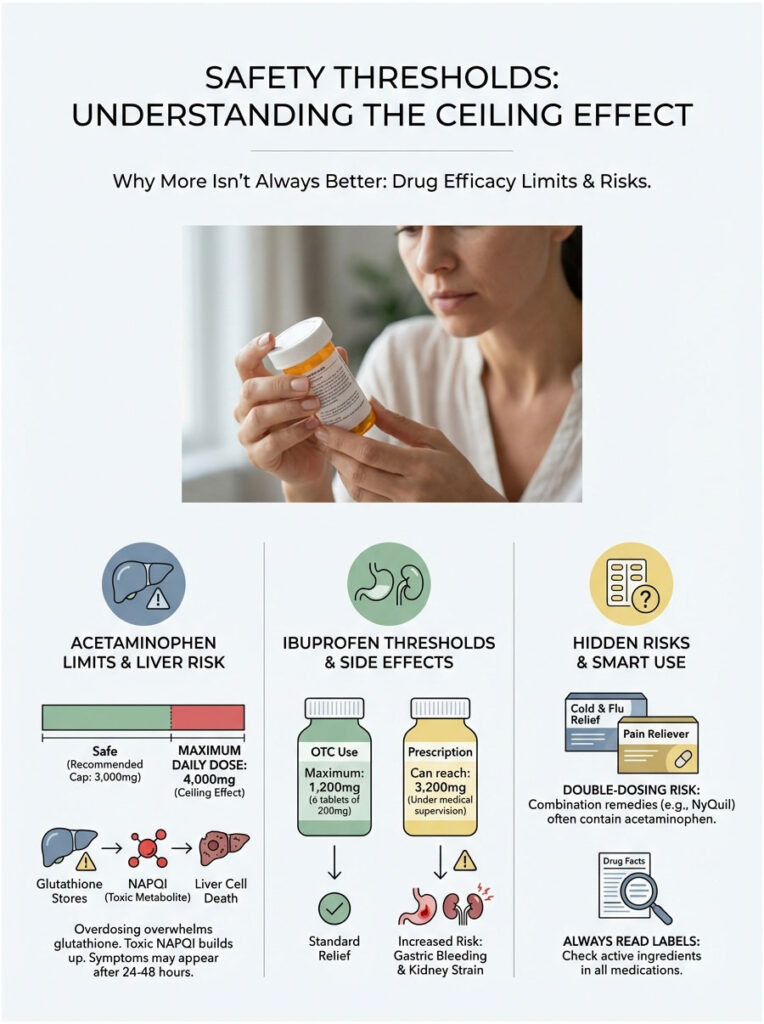
Acetaminophen Limits and Liver Health
The generally accepted maximum daily dose for a healthy adult is 4,000mg (4 grams) per 24 hours. However, many liver specialists and updated guidelines recommend a conservative cap of 3,000mg, especially if you are using it for several days running. This gives you a safety buffer.
Going over this limit overwhelms the liver’s glutathione stores. Without glutathione, the toxic metabolite NAPQI binds to liver proteins and causes cell death. What makes this especially dangerous is that symptoms often do not show up until 24 to 48 hours after ingestion.
Ibuprofen Limits and Kidney Strain
For over-the-counter use, the maximum is 1,200mg per 24 hours (typically 6 tablets of 200mg). Under strict physician supervision, prescription doses can go higher (up to 3,200mg), but this significantly raises the risk of gastric bleeding and kidney stress. Do not attempt prescription-level dosing without your doctor’s explicit instruction.
Here is a critical detail many people miss. If you are asking “can you take acetaminophen and ibuprofen together” while also sipping NyQuil for a cold, you may already be double-dosing. NyQuil and many other combination remedies already contain acetaminophen. Always read the Drug Facts label on every medication to check if acetaminophen or ibuprofen is listed as an active ingredient.
Contraindications and Red Flag Populations
While the answer to “can you take acetaminophen and ibuprofen together” is generally yes, there are specific groups for whom this advice changes. Personal physiology can rewrite the rules of pharmacology.
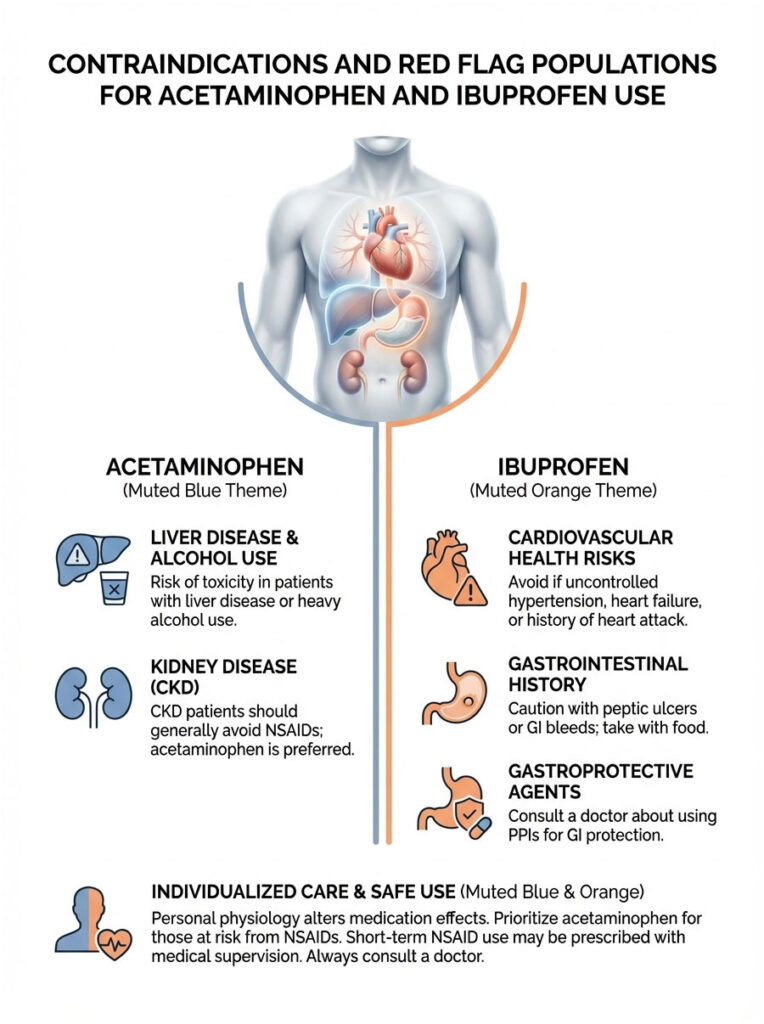
Cardiovascular Health Risks
NSAIDs like ibuprofen carry an FDA Black Box Warning for increased risk of heart attack and stroke. If you have uncontrolled hypertension, heart failure, or a history of heart attack, you should avoid regular ibuprofen use. NSAIDs cause the kidneys to retain sodium and water, increasing blood volume and placing extra strain on the heart.
In these cases, acetaminophen alone is the safer option. If NSAIDs are absolutely necessary, doctors may prescribe them for a very short duration. But self-medicating with ibuprofen when you have heart disease is a risk not worth taking.
Gastrointestinal History
Patients with a history of peptic ulcers, GI bleeds, or gastritis need to be careful with the ibuprofen component. Ibuprofen inhibits the prostaglandins that protect your stomach lining from its own acid. Without that protective mucus layer, stomach acid can burn the tissue directly.
If you must take it, make sure you have food in your stomach. You can also ask your doctor about taking a gastroprotective agent like a Proton Pump Inhibitor (PPI) alongside it. Never take ibuprofen on an empty stomach if you have a sensitive GI tract.
Kidney Disease (CKD)
Your kidneys depend on prostaglandins to maintain proper blood flow, especially when they are under stress. Ibuprofen constricts the afferent arterioles in the kidneys and reduces blood flow. For a healthy person, this is temporary and harmless.
For someone with Chronic Kidney Disease, this constriction can trigger acute renal failure. CKD patients should generally avoid NSAIDs entirely unless a nephrologist says otherwise. Acetaminophen is usually the preferred pain reliever for kidney patients because it is processed by the liver.
Liver Disease and Alcohol Use
Acetaminophen is processed by the liver. If you have cirrhosis, hepatitis, or drink three or more alcoholic beverages daily, your liver’s capacity to handle the drug is compromised. The threshold for toxicity drops significantly.
Alcohol induces the enzyme CYP2E1, which converts acetaminophen into its toxic form. At the same time, alcohol depletes glutathione. This creates a perfect storm for liver damage, even at doses that would normally be safe.
Adverse Effects: What to Watch For
Even with a proper acetaminophen and ibuprofen schedule, side effects can occur. Knowing which symptoms point to which drug helps you figure out what to stop. Early recognition of toxicity can save lives.
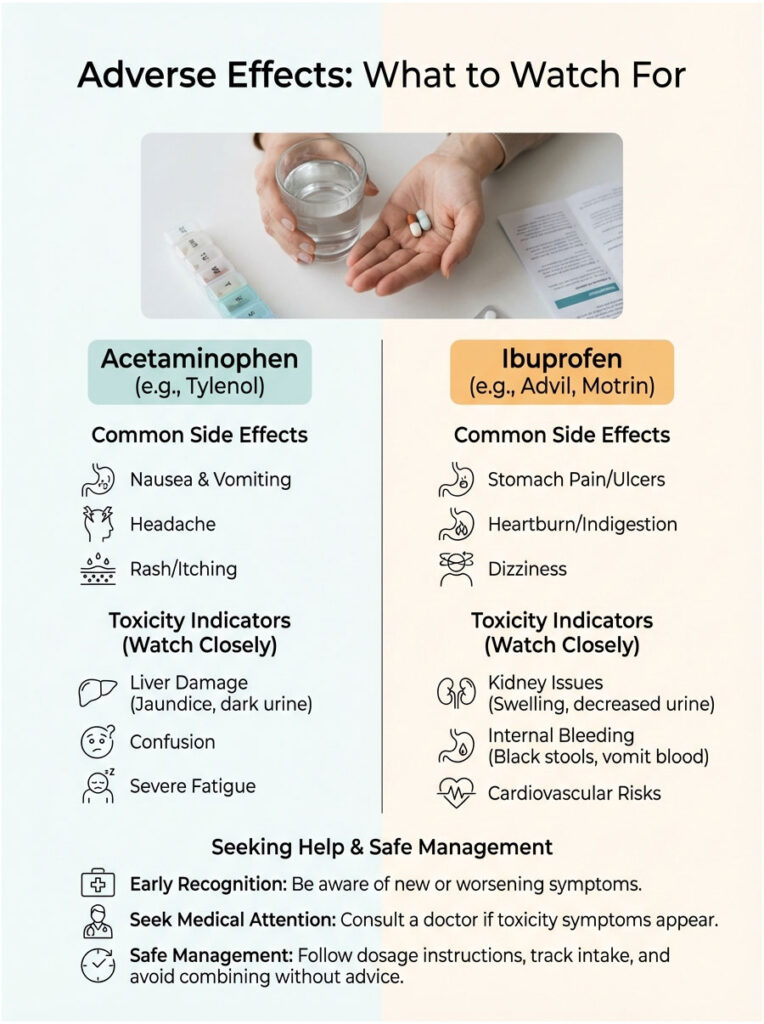
- Acetaminophen Toxicity Signs: Often silent in the early stages, which is what makes it so dangerous. Later signs include nausea, vomiting, sweating, and pain in the upper right abdomen (where the liver sits). Yellowing of the eyes (jaundice) is a late and serious warning sign.
- Ibuprofen Toxicity Signs: Burning pain in the center of the chest or stomach (epigastric pain), severe heartburn, vomiting material that looks like coffee grounds (blood), tarry black stools (melena), or swelling in the ankles (edema) from fluid retention. Ringing in the ears (tinnitus) can also signal high ibuprofen levels.
Drug Interactions to Be Aware Of
Be especially mindful if you take blood thinners. If you are on Warfarin (Coumadin) or Eliquis, adding ibuprofen increases your bleeding risk significantly. Ibuprofen affects platelet aggregation, and when combined with anticoagulants, the risk of internal bleeding goes up considerably.
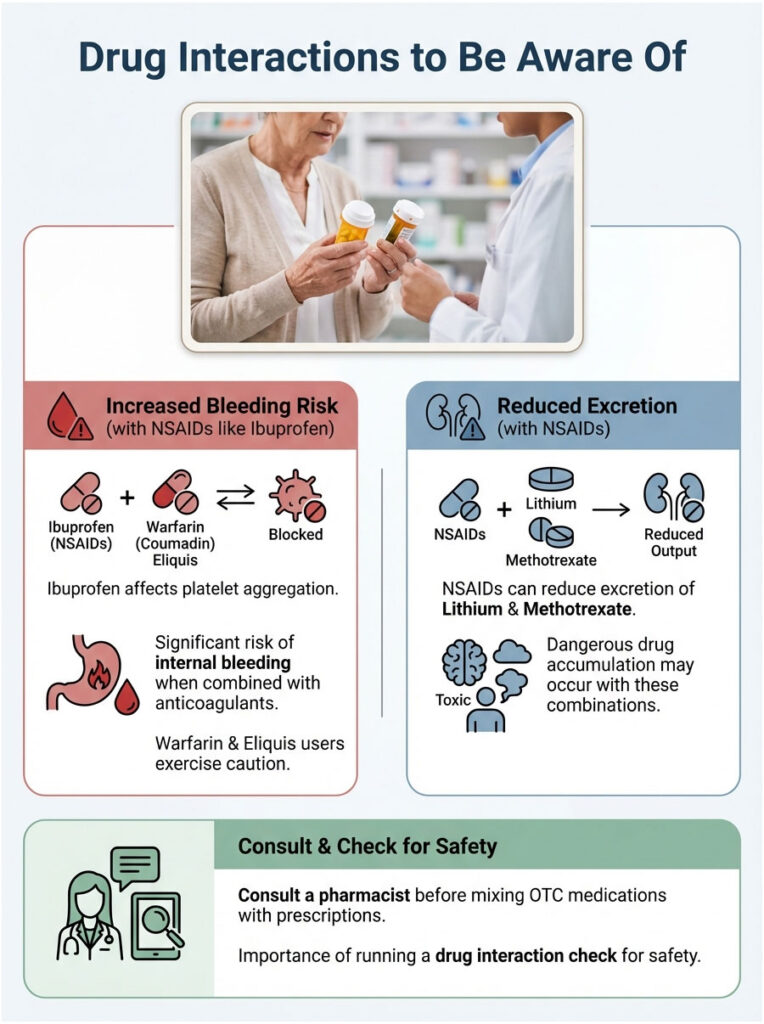
NSAIDs can also reduce the excretion of Lithium and Methotrexate, leading to dangerous drug accumulation. If you take prescription medication for mood disorders or autoimmune diseases, run a drug interaction check or ask your pharmacist before combining these OTC medications.
Practical Tips for Safe Use
To get the most out of this combination while keeping risks low, follow these clinical best practices. These small adjustments can make a meaningful difference in safety.
- Food Matters: Always take ibuprofen with food or a glass of milk. This buffers the stomach lining against direct irritation. Acetaminophen can be taken on an empty stomach without issue, though food may slightly delay its onset.
- Stay Hydrated: Water intake supports kidney clearance. Proper hydration helps your kidneys filter ibuprofen metabolites efficiently. Dehydration concentrates the drug in the kidneys, increasing the risk of damage.
- Track Your Doses: When using the staggered method, it is easy to lose track. Use a smartphone app or a simple pen-and-paper log. Writing it down prevents the “did I take that an hour ago?” confusion that can lead to accidental double-dosing.
- The 3-Day Rule: If your pain requires this combination for more than 3 days, or if you have a fever lasting more than 3 days, stop and see a doctor. Persistent pain needs a diagnosis, not just suppression. Masking pain for too long can hide serious underlying conditions.
Common Concerns and Myths Cleared Up
There is a lot of misinformation about OTC painkillers. Let’s address the most frequent points of confusion.
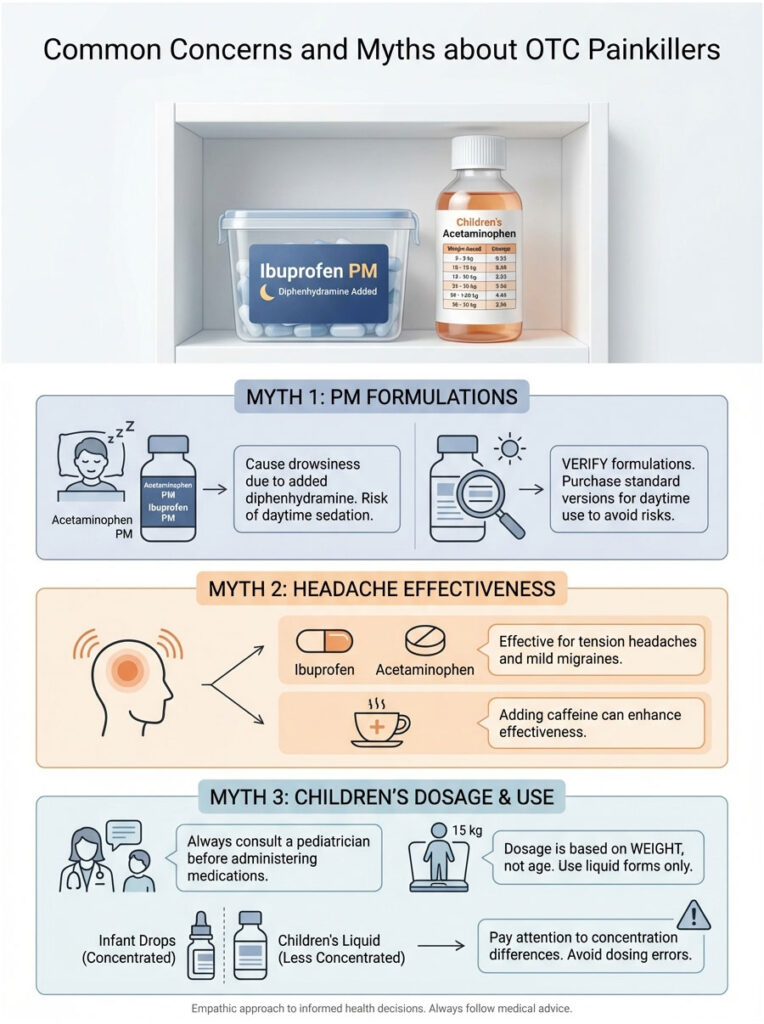
The “PM” Version Trap
Does this combination make you drowsy? No. Neither standard acetaminophen nor ibuprofen causes sedation. But people often accidentally buy “PM” versions (like Tylenol PM or Advil PM). These contain diphenhydramine (Benadryl), which causes significant drowsiness.
If you are taking these medications during the day, double-check that you are buying the standard formulation. Taking a PM version in the morning can impair your ability to drive or work safely.
Does It Work for Migraines?
Yes. This combination is often a first-line treatment for tension headaches and mild migraines. Some commercial migraine products (like Excedrin) add caffeine to a similar mix.
Caffeine acts as a vasoconstrictor, narrowing blood vessels in the brain that dilate during a migraine. It also increases the absorption rate of the pain relievers. If you have a migraine, taking your acetaminophen and ibuprofen with a cup of coffee can boost the analgesic effect noticeably.
Is This Safe for Children?
Pediatricians often recommend alternating these medications for stubborn fevers in children, but the dosing is strictly weight-based, not age-based. Never use adult tablets for children.
You must use the liquid suspension with the measuring device provided. The concentration of infant drops versus children’s liquid can vary, which leads to calculation errors. Always consult a pediatrician for specific milliliter dosages before starting a staggered regimen for a child.
Key Takeaways
So, can you take acetaminophen and ibuprofen together? Yes, and it is one of the most effective pain management strategies available without a prescription. This combination offers analgesic synergy that rivals prescription narcotics for many types of acute pain, including dental work and musculoskeletal injuries.
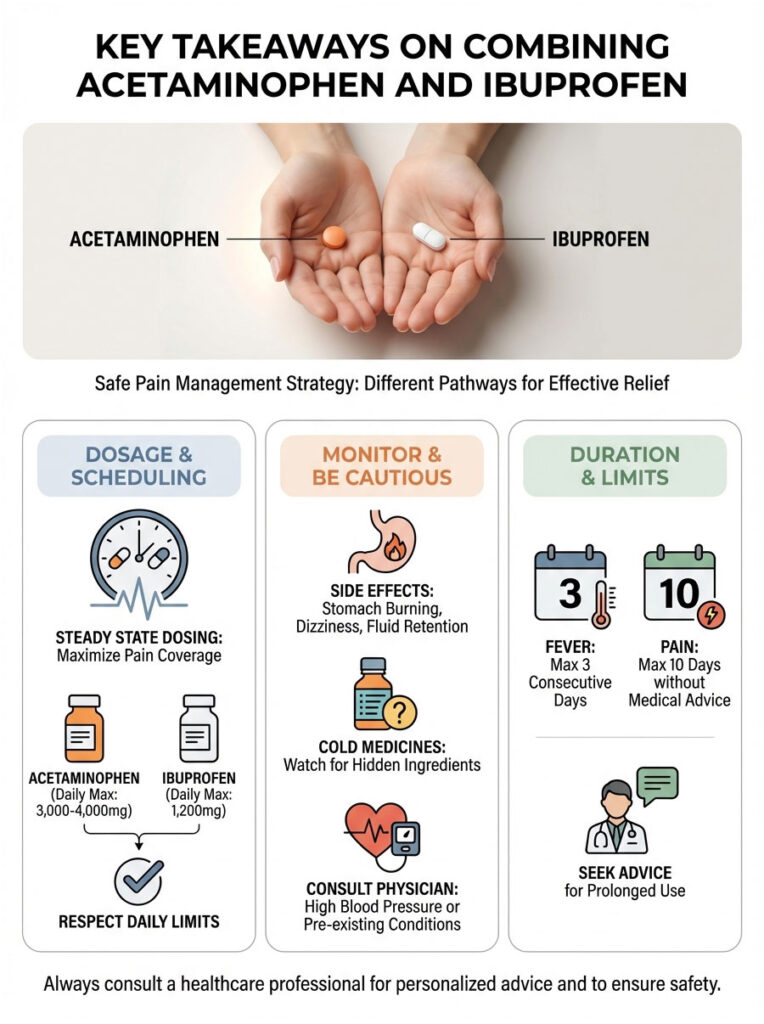
By leveraging different metabolic pathways (hepatic for acetaminophen, renal for ibuprofen), you achieve superior relief without overloading a single organ system. Whether you choose simultaneous dosing for acute pain spikes or a staggered schedule for sustained relief, the key is respecting daily maximums: 3,000-4,000mg for acetaminophen and 1,200mg for ibuprofen (OTC).
But always listen to your body. If you experience stomach burning, dizziness, or fluid retention, stop the ibuprofen immediately. Pain management should improve your quality of life, not put your long-term health at risk. And while this guide offers expert pharmacological insight, it does not replace the personalized advice of your own healthcare provider.
Frequently Asked Questions
Is it safe to take acetaminophen and ibuprofen at the same time?
Yes, combining these two medications is clinically safe because they belong to different drug classes and utilize distinct metabolic pathways. This strategy, known as multimodal analgesia, allows you to target pain through both the central and peripheral nervous systems simultaneously for superior relief.
Why is combining these two drugs more effective than taking just one?
These medications work through “analgesic synergy,” meaning their combined effect is greater than the sum of their individual parts. Ibuprofen acts as an NSAID to reduce inflammation at the site of injury, while acetaminophen raises your overall pain threshold in the brain, attacking the discomfort from two different biological angles.
What is the best dosing schedule for alternating acetaminophen and ibuprofen?
The most effective staggered method is to take one medication, wait three hours, and then take the other. This “steady state” protocol ensures that as the plasma levels of one drug begin to decline, the other is reaching its peak, providing constant pain coverage and preventing a return of symptoms.
What are the maximum daily limits for this drug combination?
For healthy adults, the maximum daily limit for acetaminophen is 4,000mg, though a conservative cap of 3,000mg is often recommended for safety. For over-the-counter ibuprofen, the daily limit is 1,200mg, which helps prevent excessive renal strain and gastric irritation.
How does the body process these two medications differently?
The liver is primarily responsible for hepatic metabolism of acetaminophen, while the kidneys handle the renal clearance of ibuprofen. This distribution of metabolic labor prevents overtaxing a single organ system, provided the patient does not have pre-existing liver or kidney disease.
Can I take this combination with multi-symptom cold and flu medicines?
You must exercise extreme caution, as many “all-in-one” cold remedies already contain acetaminophen or NSAIDs. Always check the “Drug Facts” label to avoid accidental double-dosing, which can lead to severe complications like hepatotoxicity or acute kidney injury.
Is it safe to use this combination if I have high blood pressure?
Acetaminophen is generally safe for those with hypertension, but NSAIDs like ibuprofen can cause sodium and water retention, potentially raising blood pressure further. If you have uncontrolled hypertension or heart disease, you should consult your physician before using ibuprofen due to the increased cardiovascular risk.
What precautions should I take to protect my stomach while taking ibuprofen?
Ibuprofen can inhibit the prostaglandins that protect your gastric mucosa, increasing the risk of ulcers. To minimize this, always take ibuprofen with a full meal or a glass of milk, and avoid this medication entirely if you have a history of peptic ulcer disease or gastrointestinal bleeding.
Why is it dangerous to mix alcohol with acetaminophen?
Alcohol induces specific enzymes that convert acetaminophen into a toxic metabolite called NAPQI while simultaneously depleting the liver’s glutathione stores. This creates a “perfect storm” for liver necrosis, even at dosages that would otherwise be considered therapeutic.
Does combining these medications help with severe migraines?
Yes, this dual-pathway approach is often highly effective for mild to moderate migraines and tension-type headaches. For enhanced results, some patients find that consuming a small amount of caffeine alongside these medications helps increase the absorption rate and provides additional vasoconstriction.
Can I use a staggered dosing schedule for my child’s fever?
Pediatricians frequently recommend alternating these medications for persistent fevers, but dosing must be calculated strictly by the child’s weight using the provided measuring device. Never use adult tablets for children, and always confirm the specific milliliter dosage with a healthcare provider first.
How many days in a row can I safely use this combination?
This combination should generally not be used for more than three consecutive days for fever or ten days for pain without a formal medical evaluation. Prolonged use increases the risk of systemic side effects and may mask a more serious underlying condition that requires professional diagnosis.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. While the combination of these medications is common, individual health factors like liver disease, kidney function, and heart health can significantly change safety profiles. Always consult a qualified healthcare professional or your pharmacist before starting a new medication regimen or combining over-the-counter drugs.
References
- U.S. Food and Drug Administration (FDA) – https://www.fda.gov – Official guidelines on the approval of fixed-dose acetaminophen and ibuprofen combinations.
- Mayo Clinic – https://www.mayoclinic.org – Clinical overview of NSAIDs and analgesics for acute pain management.
- The Journal of the American Dental Association (JADA) – Clinical study on the efficacy of combined ibuprofen and acetaminophen for post-surgical dental pain.
- Harvard Health Publishing – https://www.health.harvard.edu – Expert insights into the “ceiling effect” and the risks of long-term NSAID use.
- Cochrane Library – Systematic review of multi-modal analgesia and its effectiveness compared to single-drug therapy.
- National Institutes of Health (NIH) – https://www.nih.gov – Research data regarding acetaminophen metabolism and hepatotoxicity risks.








