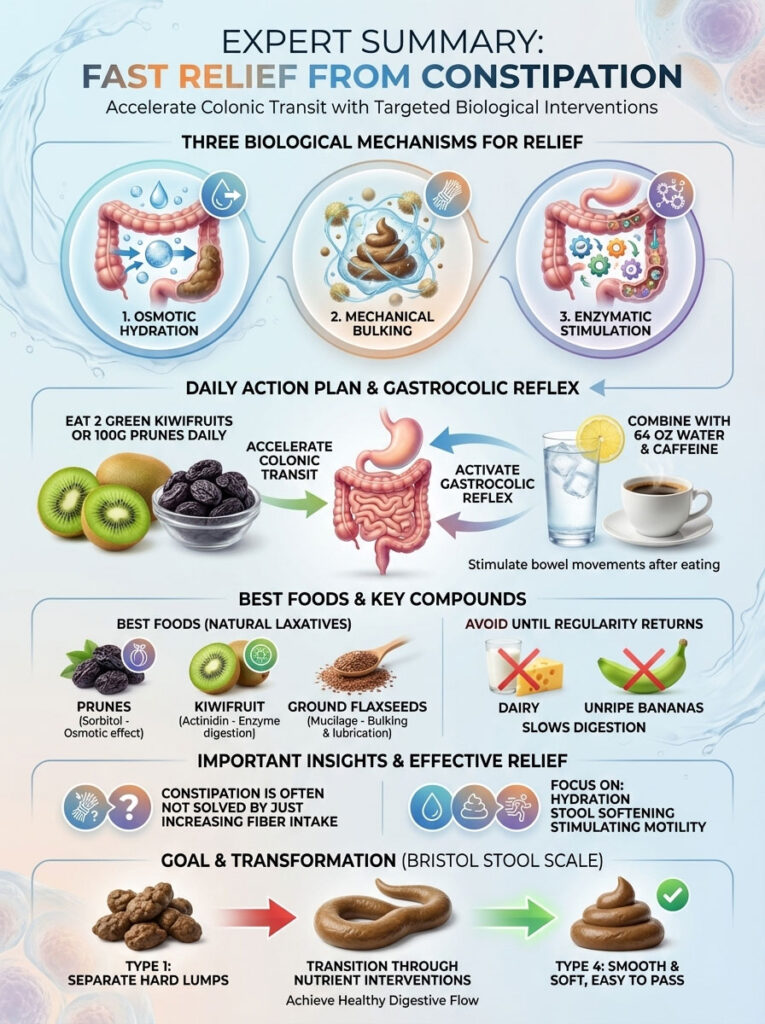
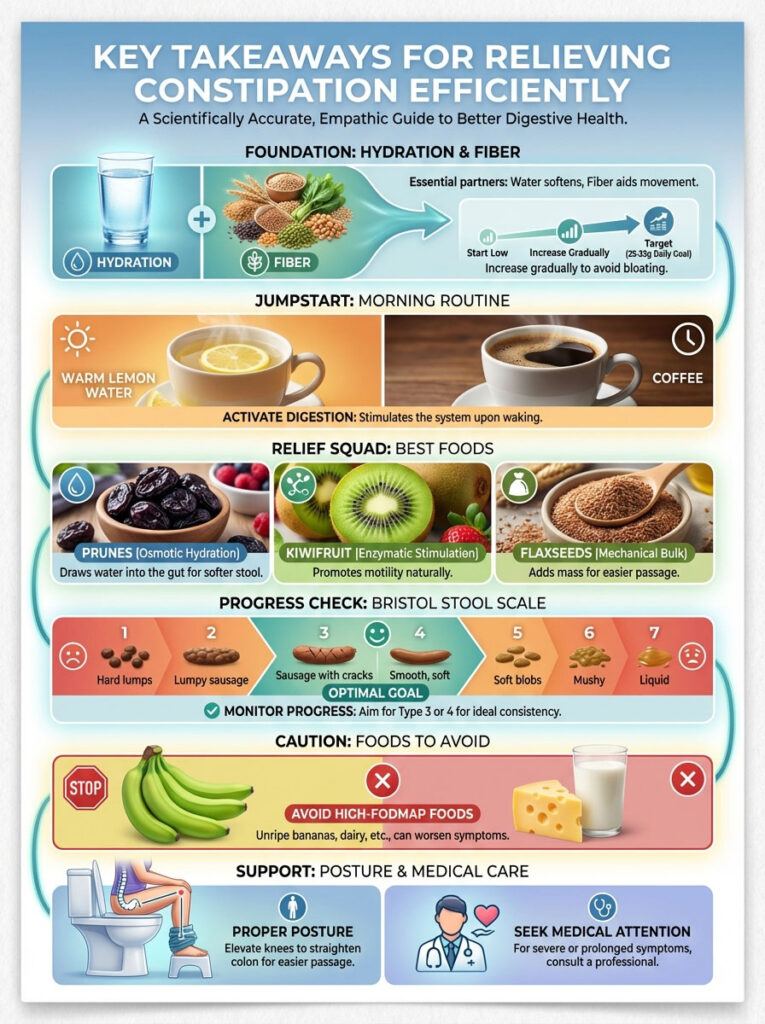
To relieve constipation fast, you must trigger three biological mechanisms: osmotic hydration, mechanical bulking, and enzymatic stimulation. Clinical data confirms that eating two green kiwifruits daily or 100g of prunes significantly accelerates colonic transit. For immediate results, combine these foods with 64 ounces of water and caffeine to activate the gastrocolic reflex. The best foods for constipation relief include prunes for sorbitol, kiwifruit for actinidin, and ground flaxseeds for mucilage. Avoid dairy and unripe bananas until regularity returns.
Table of Contents
Constipation is rarely just about “eating more fiber.” In my clinical practice, I see patients daily who consume massive amounts of roughage yet still suffer. They experience bloating. They strain. They feel an incomplete evacuation.
The problem usually isn’t the effort. It is the mechanics. Constipation acts as a physiological bottleneck. Peristalsis is the rhythmic muscle contraction of the gut. When it stalls, it is often due to dehydration, lack of stool bulk, or insufficient enzymatic activity.
As a Registered Dietitian Nutritionist specializing in functional gastroenterology, I approach this differently. We do not just throw roughage at a sluggish gut. That is like adding cars to a traffic jam. Instead, we select specific nutrient interventions.
We target the root cause of the delay. Whether you are dealing with travel-induced blockage or chronic idiopathic constipation, the strategy remains the same. We must hydrate the colon. We must soften the stool. We must stimulate motility.
In this comprehensive guide, we will move beyond generic advice. We will analyze the biochemistry of the best foods for constipation relief. You will learn how to transition from a Type 1 to a Type 4 on the Bristol Stool Scale naturally.
Key Statistics: The Reality of Constipation
- 16% of Adults: Approximately 16 out of 100 adults in the U.S. report symptoms of constipation (NIDDK).
- 33% of Older Adults: The prevalence jumps to 33% for adults over age 60 due to slower metabolism and medication use.
- $235 Million: The estimated annual expenditure on over-the-counter laxatives in the USA alone.
- 2.5 Million: The number of doctor visits annually specifically for constipation relief.
- 12 to 24 Hours: The typical onset time for osmotic foods like prunes to produce a bowel movement.
- 95% of Fiber Needs: Studies show 95% of Americans do not meet the recommended daily fiber intake.
Understanding Gut Motility and the Bristol Stool Scale
Before we discuss specific foods, we must establish what is happening inside your gastrointestinal tract. Digestion relies on peristalsis. This is a wave-like series of muscle contractions. It moves food from the esophagus to the rectum.
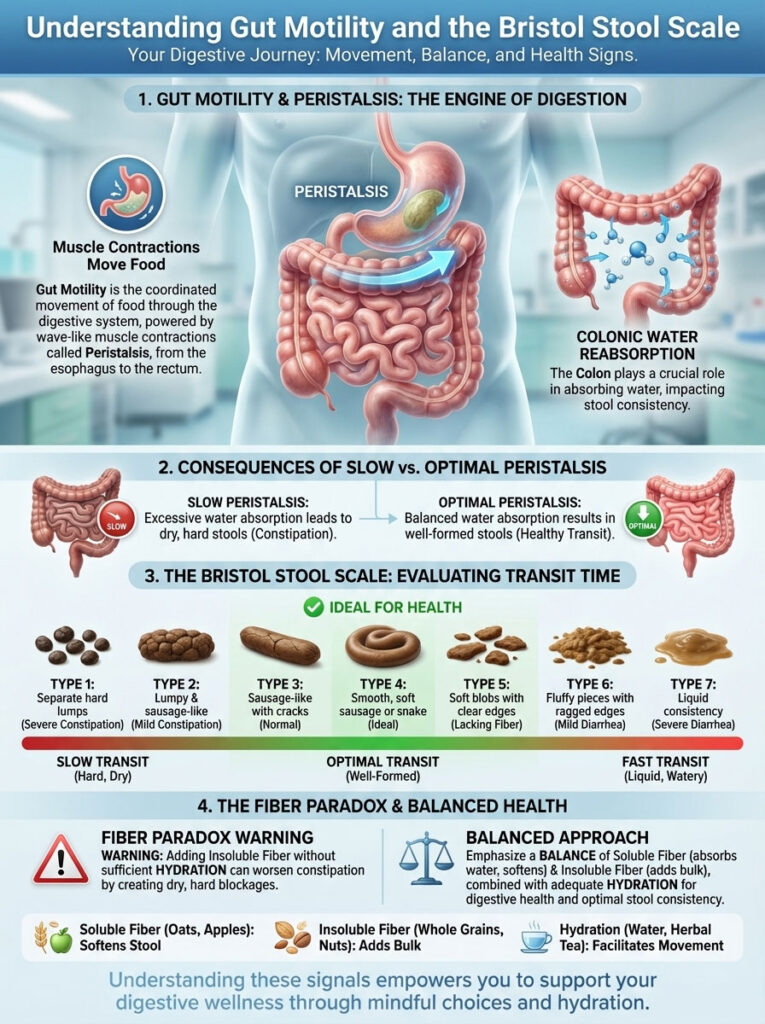
Think of it like a conveyor belt. When this rhythm slows down, the stool sits in the colon for too long. The colon’s job is to reabsorb water. If stool lingers, the colon sucks it dry. This results in dry, hard rocks that are painful to pass.
The Diagnostic Tool: Bristol Stool Scale
In clinical settings, we use the Bristol Stool Scale to evaluate transit time. It is vital that you identify where you stand. This helps us choose the right food intervention.
- Type 1 & 2: Hard nuts or lumpy sausage. This indicates significant dehydration and slow transit. You need osmotic foods here.
- Type 3 & 4: Sausage-like with cracks or a smooth snake. This is the goal. This indicates healthy hydration and transit.
- Type 5, 6, & 7: Soft blobs to liquid. This indicates rapid transit or diarrhea.
The objective of eating the best foods for constipation relief is to manipulate stool consistency. We want to align with Type 3 or 4. If you are at a Type 1, simply adding dry bran cereal is dangerous. This is the “Fiber Paradox.”
Insoluble fiber adds bulk. But bulk requires hydration to move. Adding bulk to a dry colon creates a larger blockage. According to the American Gastroenterological Association (AGA), successful management requires a balance. You need soluble fiber to hold water. You need insoluble fiber to scrub. You need fluid to keep it moving.
Mechanism 1: The Osmotic Laxatives (Drawing Water In)
The first line of defense is hydration. But drinking water isn’t always enough. We need to draw water into the stool itself. Osmotic laxatives work by introducing compounds the body cannot fully digest.

These compounds remain in the gut. They create an osmotic gradient. This pulls fluid from the surrounding tissue into the colon. This hydration softens the stool. It makes it pliable and easy to pass.
1. Prunes (Dried Plums): The Clinical Gold Standard
Prunes are widely recognized as one of the best foods for constipation relief. This is not an old wives’ tale. It is biochemistry. Their efficacy comes from a dual-action mechanism.
First, they are high in insoluble fiber. This adds bulk. Second, and more importantly, they contain high concentrations of sorbitol. Sorbitol is a sugar alcohol. It is absorbed very slowly into the bloodstream.
As sorbitol lingers in the gut, it acts like a sponge for water. It prevents the stool from drying out. A study published in Alimentary Pharmacology & Therapeutics confirmed this. It found that prunes were superior to psyllium husk for improving stool frequency.
RDN Pro Tip: Start with 3 to 4 prunes daily. Sorbitol can cause gas in sensitive individuals. Assess your tolerance. To relieve constipation fast, work your way up to 10 prunes (approx. 100g) spread throughout the day.
Do not rely solely on prune juice. The juice lacks the fiber matrix found in the whole fruit. The whole fruit provides the bulk necessary to stimulate the colon walls. If you dislike the texture, try stewing them in warm water with a cinnamon stick.
2. Pears and Apples (With Skin)
Apples and pears are accessible and gentle. Like prunes, pears contain significant amounts of fructose and sorbitol. However, the key here is the skin. Do not peel your fruit.
The skin contains high levels of insoluble fiber. The flesh provides pectin. Pectin is a soluble fiber. It dissolves in water to form a gel. It is also fermented by bacteria in the colon.
This fermentation produces short-chain fatty acids. These acids act as a natural osmotic agent. They pull water into the bowel. To use these as natural laxative foods, consume them raw. Cooking breaks down some of the structural fiber.
3. Stone Fruits (Peaches, Plums, Apricots)
During the summer months, fresh stone fruits are excellent alternatives. They possess a similar sorbitol profile to prunes. They also come with a higher water content. This makes them less calorie-dense.
They provide the osmotic pressure needed to hydrate the colon. If you cannot find fresh options, dried apricots are a concentrated source. Be mindful of portion sizes with dried fruit. The sugar concentration is higher.
4. Figs (Fresh or Dried)
Figs are often overlooked. They are a powerhouse for gut health. Three dried figs contain about 5 grams of fiber. They also contain an enzyme called ficin.
Ficin is similar to enzymes found in kiwifruit. It aids in digestion. Figs also have a high ratio of soluble to insoluble fiber. This makes them excellent for softening hard stools. They are particularly rich in calcium as well.
Mechanism 2: Enzymatic Stimulation (The New Clinical Frontier)
Fiber and water are the old guard of relief. Enzymatic stimulation is the modern clinical frontier. Certain fruits contain naturally occurring enzymes. These enzymes break down proteins.
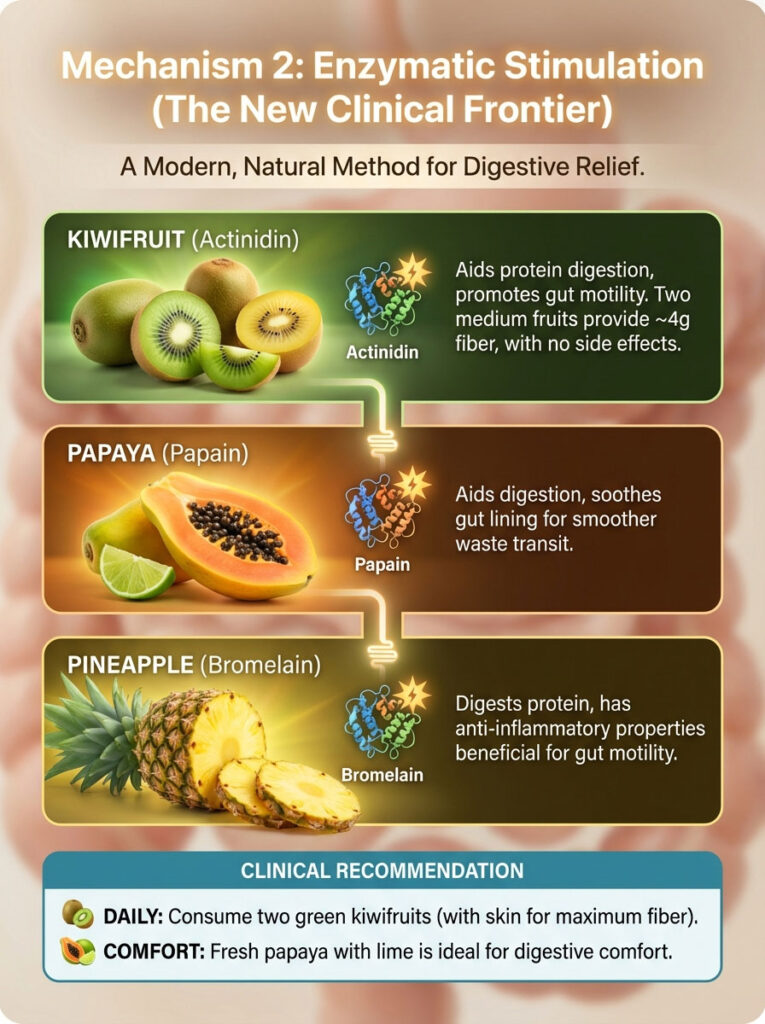
They also stimulate receptors in the gut lining. This encourages movement. It is a chemical signal to the gut to “wake up.”
5. Kiwifruit (Green and Gold)
If prunes are the old reliable, kiwifruit is the modern specialist. Research indicates that green kiwifruit contains a proteolytic enzyme called actinidin. This enzyme is unique.
Actinidin aids in protein digestion in the upper GI tract. More importantly, it stimulates receptors in the colon to promote motility. Two medium kiwifruits provide about 4 grams of fiber.
The major advantage of kiwifruit is the lack of side effects. Legumes and prunes can cause bloating. Kiwifruit is low in fermentable oligosaccharides (FODMAPs). It is one of the best foods for constipation relief for patients with IBS-C.
Clinical Recommendation: Eat two green kiwifruits per day. You can scoop out the flesh. For maximum fiber, wash the skin thoroughly and eat it like an apple. The fuzzy skin is edible and rich in insoluble fiber.
6. Papaya
Papaya contains an enzyme called papain. Papain helps digest tough protein fibers. These protein fibers can sometimes slow down digestion. While less potent than actinidin for motility, papaya is excellent for comfort.
It creates a smoother transit for waste products. It is soothing to the gut lining. When looking for foods to help you poop without cramping, papaya is a top choice. It is best eaten fresh with a squeeze of lime.
7. Pineapple
Pineapple contains bromelain. This is an enzyme mixture that digests protein. It also has mild anti-inflammatory properties. Inflammation in the gut lining can contribute to dysmotility.
By reducing inflammation, pineapple supports the mechanical process. The core of the pineapple contains the highest concentration of bromelain. Do not discard it. Chop it finely and include it in your smoothie.
Mechanism 3: Mechanical Bulk & Insoluble Fiber (The “Scrub Brush”)
Insoluble fiber is the “scrub brush” of the colon. It does not dissolve in water. It adds weight and volume to the stool. This bulk stretches the colon wall.

This stretching is crucial. It triggers the mechanoreceptors in the gut. These receptors signal the brain that it is time to evacuate.
8. Chia Seeds
Chia seeds are a powerhouse among high fiber foods for constipation. They are unique because of their hydrophilic properties. They love water.
When exposed to liquid, they form a mucilaginous gel. This gel provides two benefits. First, it lubricates the passage of stool. Second, it retains moisture to prevent hardening.
Preparation Warning: You must soak chia seeds before eating them. Eating dry chia seeds followed by water is risky. They can expand in the esophagus. Mix 2 tablespoons into oatmeal or yogurt. Let it sit for 10 minutes to gel.
9. Ground Flaxseeds
Similar to chia, flaxseeds are high in mucilage gums. They also provide Omega-3 fatty acids. These fats help lubricate the intestinal lining. This reduces friction during bowel movements.
I recommend ground flaxseeds over whole seeds. Whole seeds often pass through the digestive tract undigested. You miss out on the fiber benefits. Add a tablespoon of ground flax to your morning smoothie. It is an easy way to integrate natural laxative foods.
10. Oat Bran and Whole Oats
Oats are rich in beta-glucan. This is a soluble fiber that ferments in the gut. This fermentation process increases bacterial mass. It sounds unappealing, but it is necessary.
Bacterial mass makes up a significant portion of stool weight. A heavier stool is easier for peristalsis to move. Old-fashioned rolled oats are superior to instant packets. Instant packets often contain added sugar and less structural fiber.
11. Legumes (Lentils, Black Beans, Chickpeas)
Legumes boast the highest fiber-per-cup ratio of almost any food group. One cup of cooked lentils contains nearly 16 grams of fiber. This massive influx of fiber increases fecal bulk significantly.
However, proceed with caution. Because they are high in fermentable carbohydrates, they can cause gas. Introduce them slowly. Start with 1/4 cup. Ensure you are drinking plenty of water to move this bulk.
Mechanism 4: The Gastrocolic Reflex & Lubrication
Sometimes the machinery just needs a jumpstart. The gastrocolic reflex is a physiological reaction. The act of filling the stomach stimulates movement in the colon. This reflex is most active in the morning.
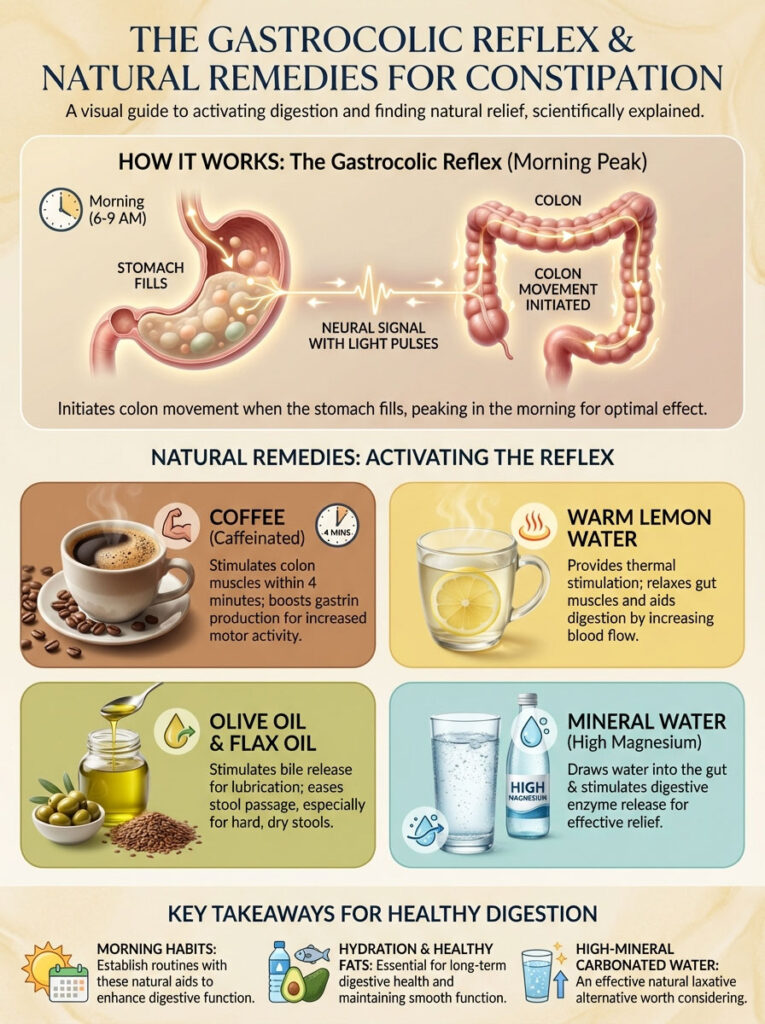
12. Coffee (Caffeinated)
For many, coffee is the primary morning regulator. It is not just a habit. It is science. Caffeine stimulates the distal colon muscles within 4 minutes of ingestion.
It increases the production of gastrin. Gastrin is a hormone that spikes colonic motor activity. While decaf has some effect, caffeinated coffee is significantly more potent. To relieve constipation fast, drink a strong cup approximately 30 minutes after waking.
13. Warm Lemon Water
Lemon water is often touted as a “detox” miracle. Its value for constipation is simpler. It provides thermal stimulation. Warm liquids relax the gut muscles.
They act as a vasodilator. This increases blood flow to the digestive tract. The acidity of the lemon may stimulate gastric acid production. This aids the initial stages of digestion. Drinking 16 ounces of warm water first thing in the morning is a cornerstone habit.
14. Olive Oil and Flax Oil
Fat stimulates the release of bile from the gallbladder. Bile acts as a natural laxative. It is an emulsifier in the intestine. Additionally, consuming healthy fats provides direct lubrication.
It helps the stool slide through the colon easier. A tablespoon of olive oil on an empty stomach is a traditional remedy. It holds up to physiological scrutiny. It is particularly helpful for those with very hard, dry stools.
15. Mineral Water (High Magnesium)
Not all water is created equal. Some natural mineral waters are high in magnesium and sulfates. Brands like Donat Mg are famous for this.
Magnesium draws water into the gut. Sulfates stimulate the pancreas to release digestive enzymes. If plain water isn’t working, try a glass of high-mineral carbonated water. It can be a powerful natural laxative.
Mechanism 5: Prebiotics & Magnesium (The Long-Term Fix)
To prevent constipation from returning, we must look at the microbiome. We must also look at muscle function. Prebiotics feed the good bacteria. Magnesium relaxes the smooth muscles of the gut.
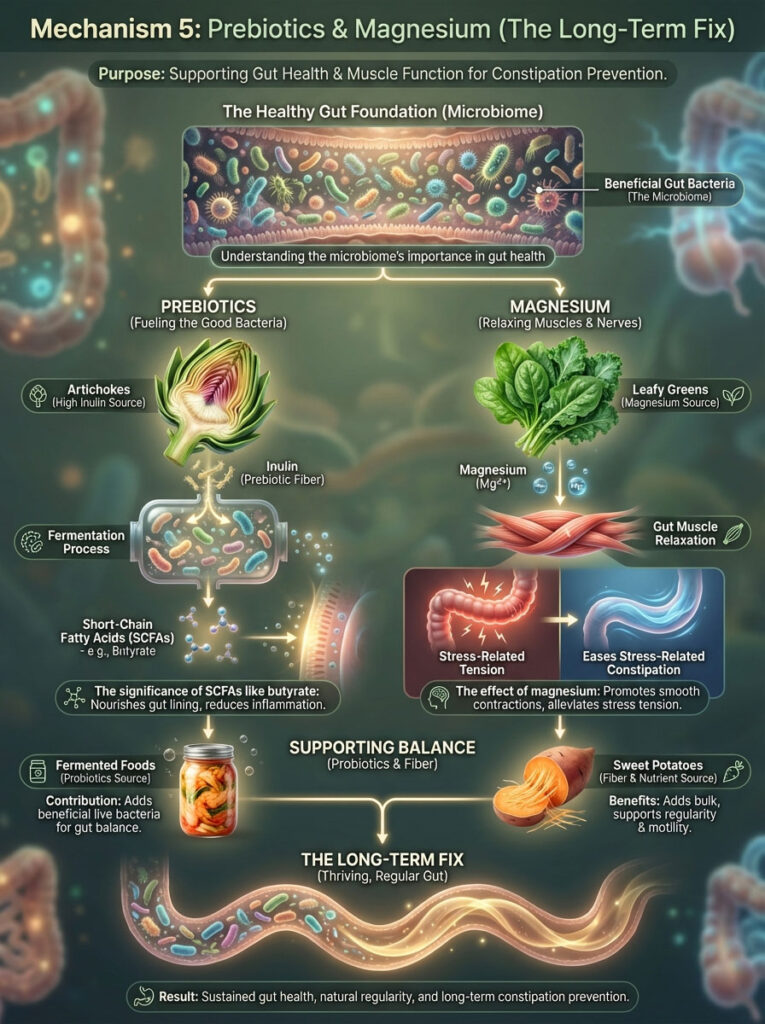
16. Artichokes (Jerusalem and Globe)
Artichokes are incredibly high in inulin. Inulin is a potent prebiotic fiber. It travels to the colon undigested. There, gut bacteria ferment it.
This fermentation creates Short-Chain Fatty Acids (SCFAs) like butyrate. Butyrate provides energy to the cells lining the colon. It keeps them healthy and muscularly active. This makes artichokes one of the best foods for constipation relief for long-term maintenance.
17. Leafy Greens (Spinach, Swiss Chard)
Dark leafy greens are excellent sources of magnesium. Magnesium is an electrolyte. It draws water into the gut. It also helps relax smooth muscle tissue.
If your constipation is related to stress, you need this. A “tight” pelvic floor sensation often indicates a magnesium deficiency. Cooked greens allow you to consume a larger volume. You get more fiber and magnesium per bite than raw salads.
18. Fermented Foods (Kefir, Sauerkraut, Kimchi)
Fermented foods provide probiotics. These are live beneficial bacteria. Strains like Lactobacillus and Bifidobacterium help regulate transit time.
Imbalances in gut bacteria (dysbiosis) can lead to methane production. Methane gas slows down the gut significantly. By crowding out methane-producing bacteria with healthy probiotics, you can normalize your bowel rhythm.
19. Sweet Potatoes (With Skin)
Sweet potatoes contain a balance of soluble and insoluble fiber. They are gentle on the digestive tract. They are often better tolerated than cruciferous vegetables.
They provide bulk without excessive gas. Keep the skin on. That is where the insoluble fiber lives. Roast them with a little olive oil for a dual-action effect.
Comparative Analysis: Choosing the Right Food for Your Symptoms
Not all constipation presents the same way. Some patients have hard, dry stools. Others have soft stools that simply won’t move. Tailoring your food choice to your specific symptom is the mark of an expert approach.
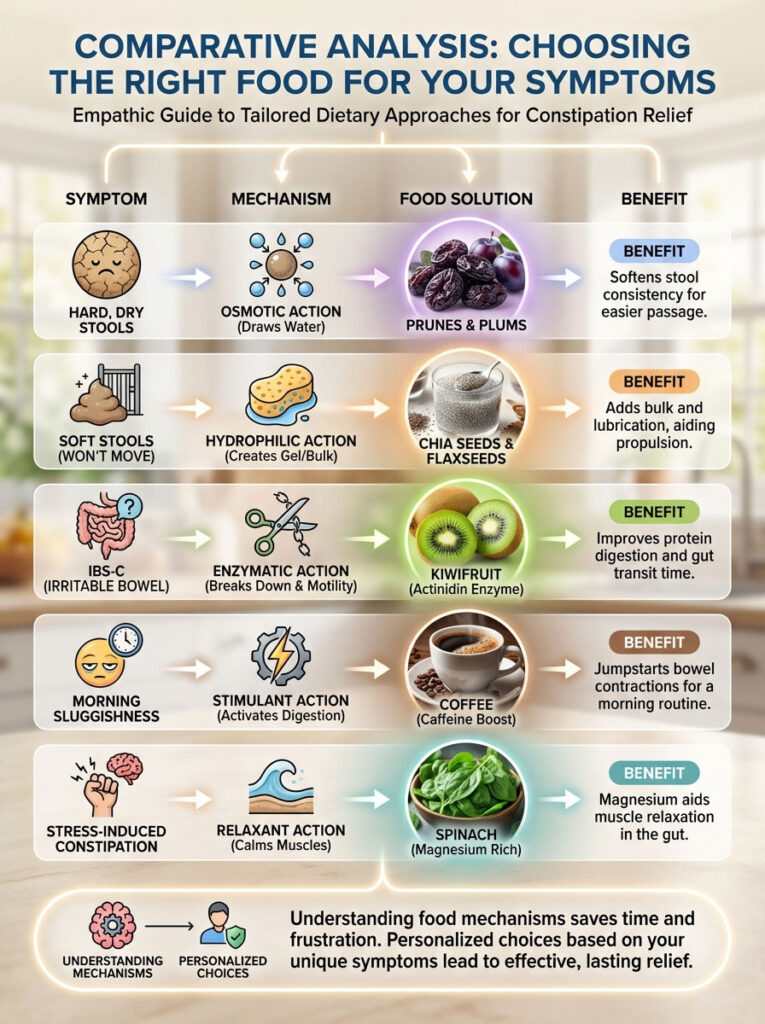
Table 1: Food Mechanism & Best Use Case
| Food Category | Primary Mechanism | Key Active Compound | Best For Patient Profile |
|---|---|---|---|
| Prunes | Osmotic | Sorbitol | Hard, dry stools (Type 1-2); need for predictable relief. |
| Kiwifruit | Enzymatic | Actinidin | IBS-C patients; those prone to bloating from beans/grains. |
| Chia Seeds | Hydrophilic Bulk | Mucilage | Patients with low fiber intake; need for stool softening gel. |
| Coffee | Neural Stimulation | Caffeine/Chlorogenic Acid | Morning routine; patients with slow gastric emptying. |
| Spinach | Relaxant | Magnesium | Stress-induced constipation; tight pelvic floor sensation. |
Understanding these distinctions saves you time. It prevents the frustration of trying remedies that do not match your physiology. If you have IBS, avoid the beans. Go for the kiwi. If you are dehydrated, skip the bran. Go for the pears.
A Dietitian’s “Fast Relief” Protocol (Sample Day)
When patients come to me asking how to relieve constipation fast, I do not just give them a list. I give them a schedule. Timing matters.

The gut operates on a circadian rhythm. We want to front-load our efforts. We want to strike when the colon is most active.
- Upon Waking (7:00 AM): Drink 16oz of warm lemon water. Follow this with 1 cup of caffeinated coffee. This triggers the gastrocolic reflex immediately.
- Breakfast (7:30 AM): Oatmeal cooked with water. Top with 2 tbsp ground flaxseed and 1 cup of sliced papaya. This provides bulk and enzymes. Avoid dairy milk.
- Mid-Morning Snack (10:00 AM): 2 Green Kiwifruits. Eat them with the skin if you can tolerate the texture. Or scoop the flesh. This delivers the actinidin payload.
- Lunch (12:30 PM): Lentil soup. Lentils are among the high fiber foods for constipation. They provide massive mechanical bulk. Pair with a side of spinach salad for magnesium.
- Afternoon Snack (3:30 PM): 5 to 6 Prunes. This maintains the osmotic pressure in the gut. Drink another 16oz of water here.
- Dinner (6:30 PM): Baked salmon with quinoa and roasted asparagus. The salmon provides healthy fats for lubrication. Asparagus feeds gut bacteria overnight.
- Hydration Goal: You must aim for 80oz of total fluid intake. Without this water, the fiber from the lentils and flax will create a blockage.
Foods to Avoid (The “Cloggers”)
Knowing what not to eat is just as important. You can eat all the prunes in the world, but if you pair them with cheese, you are fighting a losing battle. Certain foods slow down motility.
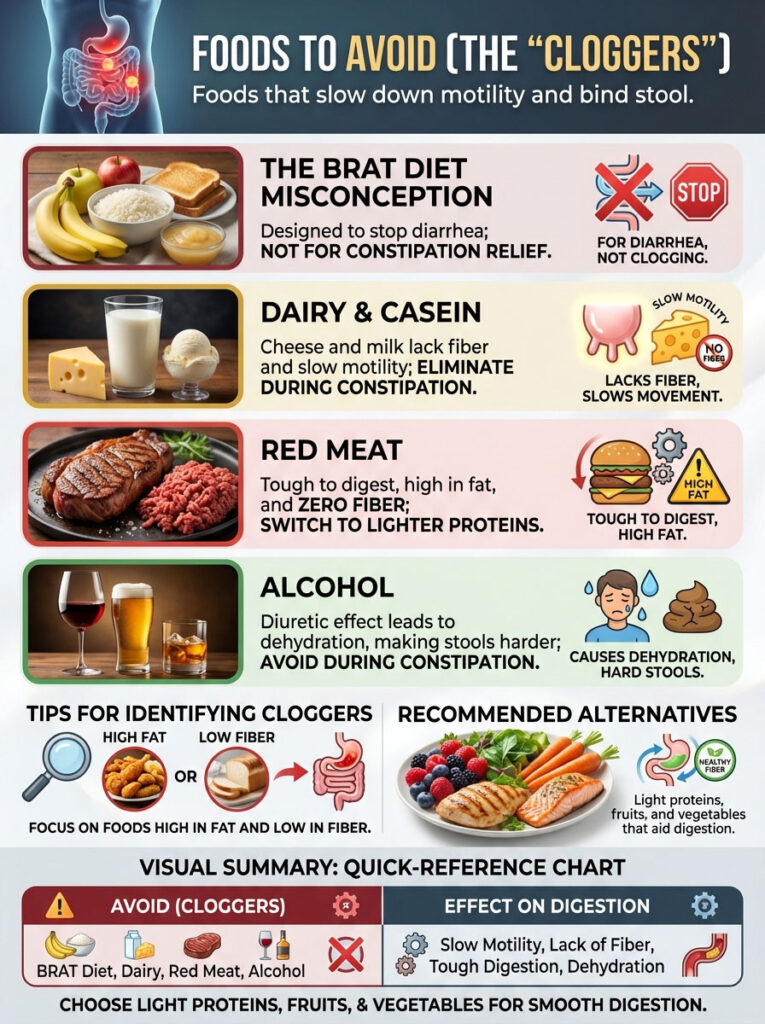
They bind stool. They effectively undo your hard work. We call these the “Cloggers.”
The BRAT Diet Misconception
You may have heard of the BRAT diet. It stands for Bananas, Rice, Applesauce, Toast. This diet is designed for diarrhea. It is meant to stop you up.
It is the enemy of constipation relief.
- Unripe Bananas: High in resistant starch and tannins. These can worsen constipation.
- White Rice: Stripped of fiber. It is highly binding.
- White Toast: Processed wheat acts like glue in the intestinal tract.
Dairy and Casein
Cheese and milk are common culprits. They contain no fiber. They are high in casein. Casein is a protein that slows motility in many adults.
If you are backed up, eliminate dairy completely. Wait until you are regular again. Then reintroduce it slowly.
Red Meat
Red meat is tough to digest. It is high in fat. It contains zero fiber. It takes a long time to pass through the digestive tract.
When you are trying to relieve constipation fast, switch to lighter proteins. Fish or plant-based options are better. They move through the system faster.
Alcohol
Alcohol is a diuretic. It inhibits the anti-diuretic hormone (ADH). This causes you to urinate frequently.
This leads to systemic dehydration. As your body loses water, it pulls moisture from the colon. This makes stools harder. Avoid alcohol during a bout of constipation.
Comparison of Natural Foods vs. OTC Laxatives
Patients often ask if they should just take a pill. While over-the-counter (OTC) laxatives have their place, food should be the first line of defense. Stimulant laxatives like Senna or Bisacodyl can cause dependency.
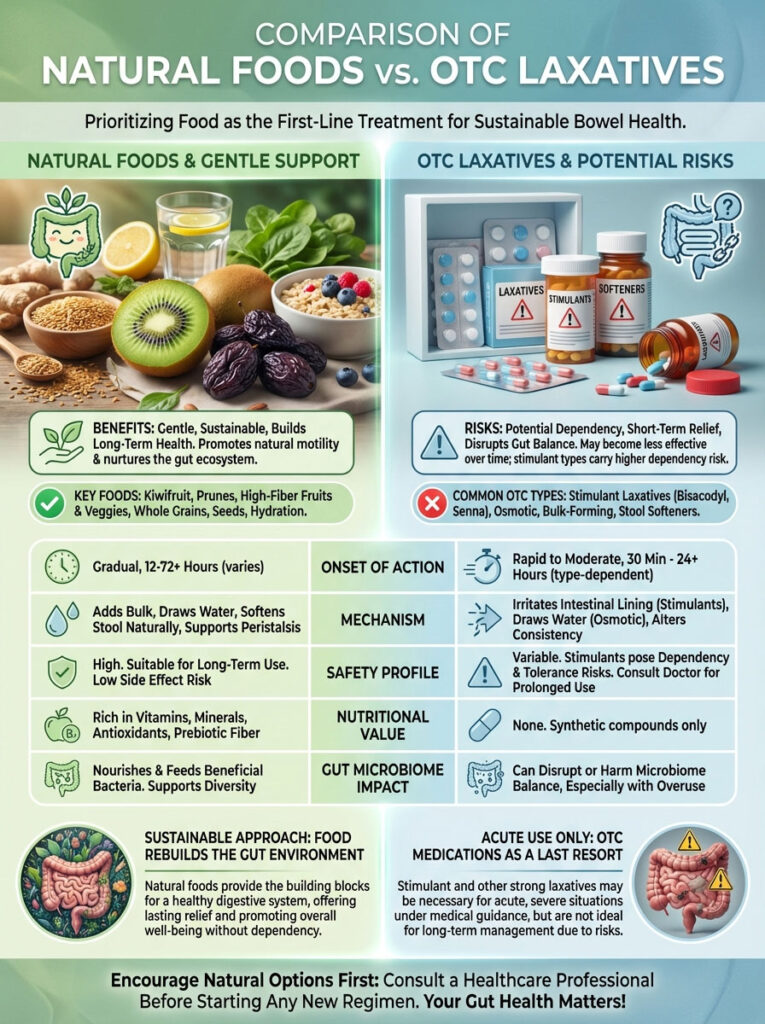
Dependency means your bowel forgets how to work on its own. Natural laxative foods like kiwifruit and prunes do not carry this risk. They train the bowel to work better.
Table 2: Natural Foods vs. OTC Medications
| Feature | Natural Foods (Prunes/Kiwi) | Osmotic Laxatives (Miralax) | Stimulant Laxatives (Dulcolax) |
|---|---|---|---|
| Onset of Action | 12–24 Hours | 24–72 Hours | 6–12 Hours |
| Mechanism | Fiber + Enzymes + Sorbitol | Water Retention | Irritates Nerve Endings |
| Safety Profile | Safe for long-term use | Generally safe | Short-term use only |
| Nutritional Value | High (Vitamins, Antioxidants) | None | None |
| Gut Microbiome | Feeds good bacteria (Prebiotic) | Neutral | Can disrupt microbiome |
The choice is clear. For acute, painful blockage, a stimulant might be necessary once. But for sustainable relief, food is the medicine. It rebuilds the gut environment.
Lifestyle Synergy: Maximizing the Food’s Effect
Food does not work in a vacuum. You can eat the perfect diet, but if you are sedentary, your gut will be too. Movement acts as an external pump for peristalsis.

The Walk After Meals
Walking immediately after a meal helps move food through the stomach faster. It regulates blood sugar. It also mechanically jostles the intestines. Aim for a 15-minute walk after lunch and dinner.
Toilet Posture
Anatomy matters. Modern toilets position us at a 90-degree angle. This pinches the rectum. It makes evacuation difficult. Using a small stool to elevate your feet puts you in a squatting position.
This straightens the anorectal angle. It allows gravity to do the work. It reduces straining. Combine this with your high-fiber diet for best results.
Abdominal Massage
Manual massage can stimulate a sluggish bowel. Lie on your back. Use your fingertips to massage your abdomen in a clockwise motion. This follows the path of the colon.
Start at the right hip (ascending colon). Move up to the ribs (transverse colon). Move down to the left hip (descending colon). Do this for 5 minutes before getting out of bed.
When to Seek Medical Help
While dietary changes resolve most cases, there are exceptions. Constipation can sometimes be a symptom of a larger issue. You must be vigilant.

If you experience severe abdominal pain, seek help. If you see blood in your stool, call your doctor. Unexplained weight loss is another red flag.
If you have gone more than 5 days without a bowel movement, food may not be enough. You may have a fecal impaction. This requires medical intervention, not just prunes.
Summary & Key Takeaways
Relieving constipation is about understanding the biological levers of your digestive system. It is not enough to simply eat “healthy.” You must consume foods that offer specific mechanical advantages.
You need osmotic hydration from prunes and pears. You need enzymatic stimulation from kiwifruit and papaya. You need mechanical bulk from flaxseeds and lentils.
The Bottom Line? Hydration is the vehicle. Fiber is the passenger. You need both to move forward. Aim for 25 to 35 grams of fiber daily.
Reach that number slowly. If you rush, you will get bloated. Consistency is key. The gut thrives on routine.
If you incorporate the best foods for constipation relief into a daily protocol, you can restore your body’s natural rhythm. Start with warm water and coffee. Follow with enzymatic fruits and bulking grains.
Your body knows how to do this. Sometimes, it just needs the right tools. Give it the right fuel, and it will get back to work..
Frequently Asked Questions
What are the best foods to relieve constipation fast?
To achieve rapid relief, clinical data highlights green kiwifruit and prunes as the top choices. Kiwifruit uses the enzyme actinidin to stimulate motility, while prunes provide sorbitol to draw water into the colon via an osmotic gradient. For the best results, consume these alongside 64 ounces of water to ensure the fiber has adequate hydration to move through the digestive tract.
How does kiwifruit help with bowel movements compared to other fruits?
Kiwifruit is unique because it contains actinidin, a proteolytic enzyme that improves protein digestion and stimulates receptors in the colon to increase peristalsis. Unlike legumes or grains, kiwifruit is low in fermentable oligosaccharides (FODMAPs), making it an ideal choice for patients who experience bloating or have IBS-C. Research suggests eating two green kiwifruits daily can significantly increase stool frequency and ease of evacuation.
Why are prunes considered the gold standard for natural constipation relief?
Prunes are highly effective because they contain high concentrations of sorbitol, a sugar alcohol that acts as a natural osmotic laxative by pulling water into the large intestine. This process softens Type 1 and Type 2 stools on the Bristol Stool Scale, making them easier to pass. Additionally, their high phenolic content and insoluble fiber matrix provide the mechanical bulk necessary to trigger the colon\’s stretch receptors.
Can eating too much fiber actually make constipation worse?
Yes, this is known as the “Fiber Paradox.” If you increase insoluble fiber intake without significantly increasing water consumption, the fiber can sit in a dehydrated colon and create a larger, harder blockage. Successful management requires a balance of soluble fiber to hold water and mechanical stimulation to keep the stool moving through the gastrointestinal tract.
What should I drink first thing in the morning to stimulate a bowel movement?
I recommend starting with 16 ounces of warm lemon water followed by a cup of caffeinated coffee to activate the gastrocolic reflex. Caffeine increases the production of gastrin, a hormone that spikes colonic motor activity, while the thermal stimulation of warm liquid helps relax the gut muscles. This combination jumpstarts peristalsis during the morning hours when the colon is naturally most active.
Which foods are best for constipation if I also suffer from bloating or IBS?
For those prone to gas and bloating, low-FODMAP options like kiwifruit, papaya, and cooked spinach are superior to high-fiber “cloggers” like beans or bran. Papaya contains papain, which aids in breaking down tough proteins, while spinach provides magnesium to help relax the smooth muscles of the gut. These foods provide relief without the excessive fermentation that causes abdominal distension.
How can I tell if my diet is effectively improving my transit time?
In clinical practice, we monitor progress using the Bristol Stool Scale, aiming for Type 3 or Type 4 (smooth, sausage-like stools). If you are consistently producing Type 1 or 2 (hard lumps), your transit time is too slow, and you likely need more osmotic hydration. Improvements in stool consistency and a reduction in straining are the primary indicators that your dietary interventions are working.
How do I use chia and flaxseeds safely for digestive health?
Chia seeds should always be soaked for at least 10 minutes before consumption to allow them to form a mucilaginous gel that lubricates the colon. For flaxseeds, I recommend using ground versions, as whole seeds often pass through the digestive tract undigested, providing no nutritional or mechanical benefit. Both seeds offer excellent hydrophilic properties that help retain moisture within the stool.
What common “healthy” foods should I avoid when I am backed up?
You should avoid unripe bananas, as they are high in tannins and resistant starch which can significantly slow motility. Additionally, dairy products containing casein and processed white rice are highly binding and can exacerbate a blockage. While these foods may be part of a “BRAT” diet for diarrhea, they are counterproductive when you are seeking constipation relief.
Are natural laxative foods as effective as over-the-counter medications?
Natural foods like prunes and kiwifruit are often as effective as osmotic OTC options like Miralax, but with the added benefit of providing vitamins and prebiotics. Unlike stimulant laxatives, which can cause dependency by irritating the nerve endings in the gut, whole foods rebuild the gut environment and train the bowel to function autonomously. For chronic management, food-based interventions are the safer, more sustainable choice.
Does toilet posture really affect the success of a high-fiber diet?
Yes, posture is a critical mechanical factor; modern toilets place the body at a 90-degree angle which pinches the puborectalis muscle and hinders evacuation. Using a stool to elevate your feet into a squatting position straightens the anorectal angle, allowing the bulk provided by your diet to pass more easily. This simple adjustment reduces the need for straining and prevents the development of hemorrhoids.
When is constipation a medical emergency that diet cannot fix?
Dietary changes are for functional constipation, but you must seek medical help if you experience “red flag” symptoms like blood in the stool, severe abdominal pain, or unexplained weight loss. If you have gone more than five days without a movement, you may have a fecal impaction. In such cases, the blockage requires professional medical intervention rather than dietary fiber.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The dietary strategies mentioned are intended for general educational use. Always consult a qualified healthcare professional or Registered Dietitian before making significant changes to your diet, especially if you have chronic health conditions, are pregnant, or are experiencing severe abdominal pain.
References
Bristol Stool Chart Official Resource – https://www.continence.org.au – Diagnostic criteria for evaluating stool consistency and transit time.
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – https://www.niddk.nih.gov – Source for statistics on the prevalence of constipation in U.S. adults.
American Gastroenterological Association (AGA) – https://gastro.org – Clinical guidelines on the management of chronic idiopathic constipation and the fiber paradox.
Alimentary Pharmacology & Therapeutics – “Randomised clinical trial: dried plums (prunes) vs. psyllium for constipation.” – Clinical study confirming the efficacy of sorbitol in prunes.
The Lancet Gastroenterology & Hepatology – “Exploration of actinidin in green kiwifruit for colonic transit.” – Research on enzymatic stimulation of the gut lining.
Journal of Nutrition and Metabolism – “The role of dietary fiber and magnesium in gastrointestinal motility.” – Data regarding the osmotic effects of dark leafy greens and mineral water.