To prevent debilitating low blood sugar crashes, you must strictly limit high-glycemic foods that trigger rapid insulin spikes followed by aggressive drops. Key foods to avoid include liquid sugars (soda, fruit juice), processed carbohydrates (white bread, instant oatmeal), and high-sugar fruits like watermelon, dried dates, and pineapples. Never consume alcohol on an empty stomach, as it blocks glucose production. Instead, prioritize a reactive hypoglycemia diet rich in complex carbohydrates paired with protein and healthy fats.
Table of Contents
You know the feeling. It usually starts about two or three hours after a meal. First comes the brain fog, a slight difficulty in focusing on your computer screen. Then, a subtle trembling begins in your hands. Suddenly, you are sweating, your heart is racing, and you are overcome by an intense, almost primal anxiety. You are frantically looking for something sweet to eat, convinced you might pass out if you don’t find food within minutes.
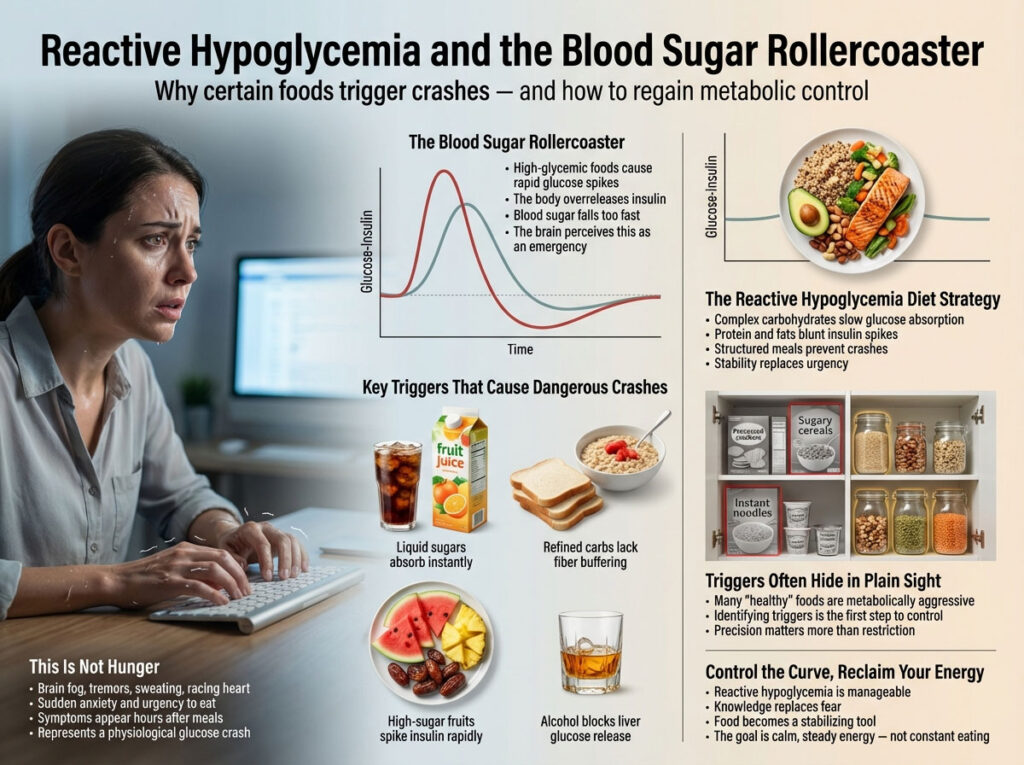
This is not just hunger. This is a biological emergency known as the “Blood Sugar Rollercoaster.”
For millions of people in the USA, this cycle is a daily reality. It is often driven by reactive hypoglycemia, a condition where the body overreacts to sugar intake. The standard medical advice to “just eat balanced meals” is often too vague to be actionable. To truly stop the shaking and regain control of your energy, you need to identify the specific triggers hiding in your pantry.
The following guide provides a deep-dive analysis of the 20 foods to avoid with low blood sugar and outlines a comprehensive reactive hypoglycemia diet strategy to stabilize your levels permanently.
The Science of Reactive Hypoglycemia and the Insulin Rebound Effect
Before we list the specific foods, it is critical to understand the biological mechanism behind the crash. This knowledge is your best defense against future episodes and helps you understand why a reactive hypoglycemia diet is so specific.
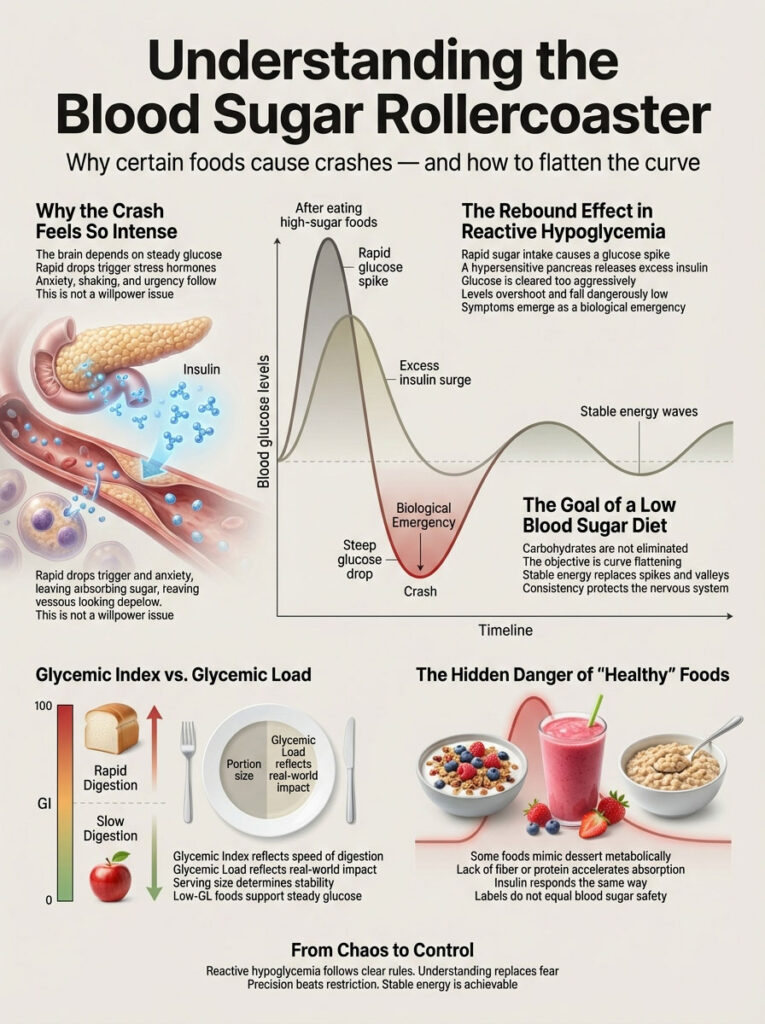
Understanding the Blood Sugar Rollercoaster Mechanism
When you consume foods that cause blood sugar crash, such as candy, white pasta, or fruit juice, your blood glucose levels skyrocket. This is called a “spike.” In a perfectly healthy metabolism, the pancreas releases a measured amount of insulin to unlock your cells and let that glucose in for energy.
However, in people with reactive hypoglycemia, the pancreas is hypersensitive. It detects the rapid influx of sugar and hits the panic button, releasing an excessive surge of insulin. This flood of insulin clears the glucose so rapidly that your levels don’t just return to normal—they overshoot the baseline and plummet dangerously low. This phenomenon is clinically known as the “Rebound Effect” or postprandial hypoglycemia.
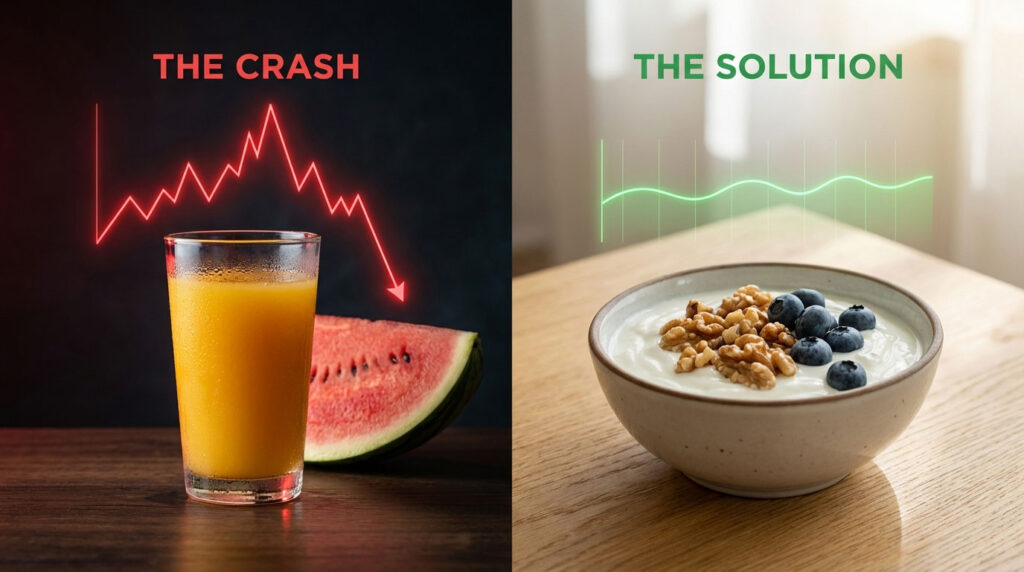
The goal of a low blood sugar diet plan is not necessarily to eliminate carbohydrates entirely but to flatten that curve. We want rolling hills of energy, not the steep peaks and valleys of Mount Everest.
Glycemic Index vs. Glycemic Load for Stable Glucose
To master your reactive hypoglycemia diet, you must understand the difference between Glycemic Index (GI) and Glycemic Load (GL).
- High GI (70+): These foods digest rapidly and cause immediate spikes. These are the primary foods to avoid with low blood sugar.
- Medium GI (56-69): Moderate impact.
- Low GI (55 or less): Slow, sustained energy release.
However, GI isn’t the whole story. We also look at Glycemic Load (GL), which accounts for the serving size. For example, watermelon has a high GI, but a low GL if you only eat one bite. But who eats just one bite? A comprehensive low blood sugar diet plan focuses on low-GL foods that provide stable blood glucose levels.
The Hidden Danger of “Healthy” Food Imposters
This is where many people get confused and frustrated. You might be eating yogurt, fruit smoothies, or oatmeal which foods traditionally labeled as “heart-healthy” by the FDA or nutrition gurus. Yet, you are still crashing by 11:00 AM.
Why? Because many “healthy” foods are chemically similar to dessert once they hit your bloodstream. Without fiber or protein to slow them down, they cause the same insulin spike as a donut. Identifying these imposters is the key to stopping the cycle.
High-Glycemic Fruits to Avoid With Low Blood Sugar
Fruit is nature’s candy, full of vitamins and antioxidants. However, for someone sensitive to sugar drops, specific high-sugar fruits are dangerous triggers. A major component of a reactive hypoglycemia diet is knowing which fruits to embrace and which to skip. Here are the top fruits to watch out for.
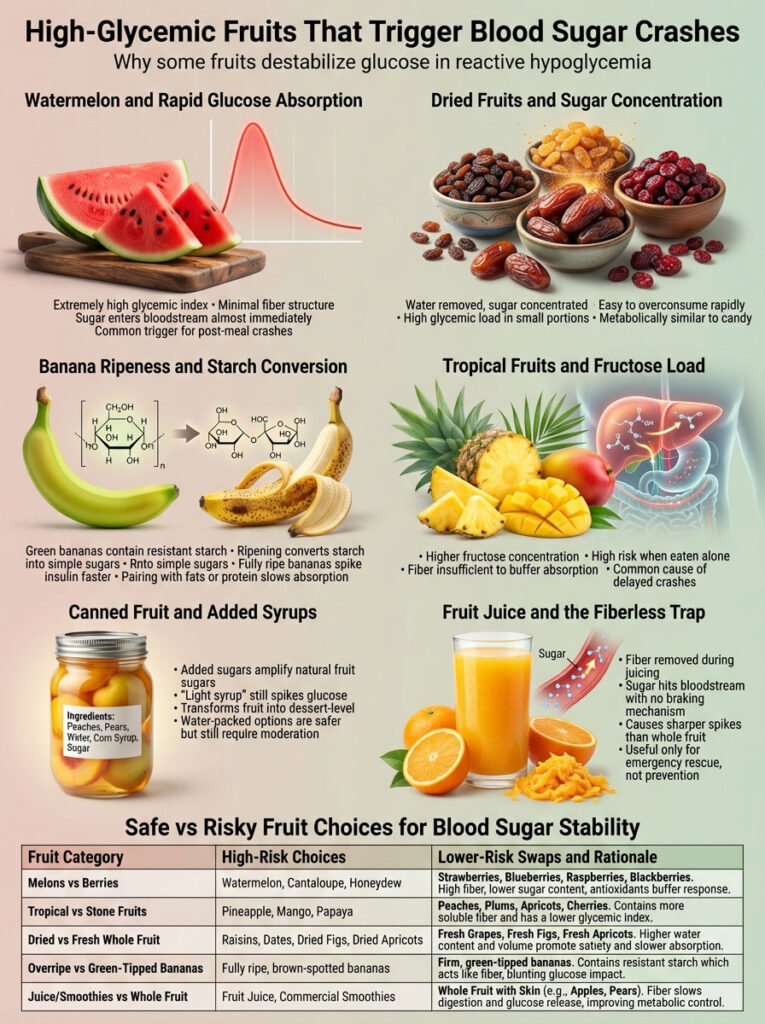
1. Why Watermelon Causes Rapid Blood Sugar Crashes
Watermelon is a staple of American summer picnics, but it is one of the worst offenders for blood sugar stability. It has a very high Glycemic Index (often cited between 72 and 80).
The Metabolic Impact:
Watermelon is composed almost entirely of water and dissolved sugar. Crucially, it lacks the dense fibrous matrix found in apples or pears. When you eat it, the sugar hits your bloodstream almost instantly, bypassing mechanical digestion. This triggers a massive insulin spike. For a diabetic, this might require a large insulin dose; for a hypoglycemic, it triggers an overproduction of insulin that leads to a crash 90 minutes later. If you are wondering what fruit is bad for low blood sugar, this is at the top of the list.
2. Dried Fruits: Raisins, Dates, and Cranberries
Dried fruit is essentially candy in disguise. The drying process removes all the water, concentrating the sugar density and reducing volume.
The Instance:
Consider a small box of raisins. It contains the same amount of sugar as a cup of grapes but can be eaten in seconds. The glycemic load is massive. Dates are even more potent; they are often used as a natural sugar substitute in baking because they are pure glucose fuel. A single Medjool date can contain 16g of sugar. For stable blood glucose levels, stick to fresh fruit where the water volume provides satiety.
3. The Risk of Ripe Bananas for Hypoglycemia
Not all bananas are created equal. The ripeness of the banana fundamentally changes its chemical composition. A green banana is rich in resistant starch, which digests slowly and acts like a fiber.
The Transformation:
As a banana ripens and develops brown spots, that resistant starch converts into simple glucose and fructose. A fully ripe, brown-spotted banana has a much higher GI than a green-tipped one. If you must eat a banana on your low blood sugar diet plan, choose one that is slightly green and always pair it with almond butter or nuts to buffer the absorption.
4. Pineapple and Mango: High Fructose Triggers
Tropical fruits tend to have significantly higher sugar content than temperate fruits like berries or stone fruit. Pineapple and mango are delicious, but they are very high in fructose.
Why avoid it:
The fiber structure in pineapple is not sufficient to blunt the sugar impact for those with severe postprandial hypoglycemia. Eating a bowl of cubed pineapple on an empty stomach is a guaranteed way to induce a crash. The fructose load can also put immediate stress on the liver, which plays a role in glucose regulation.
5. Canned Fruit in Syrup and Added Sugars
This is a pantry staple in many households, especially for children, but it is disastrous for blood sugar control.
The Hidden Sugar:
Even if the label says “light syrup,” that syrup is essentially added sugar water. You are taking a fruit that already has natural sugar and soaking it in a bath of refined sugar. This turns a healthy snack into a dessert-level trigger. Always choose fruit canned in water or its own juice, and even then, drain it thoroughly.
6. Fruit Juices: The Fiberless Trap
Juice is perhaps the biggest trap in the modern diet. When you juice an orange or an apple, you strip away the fiber (the pulp and skin) which is the most valuable part for blood sugar control.
The Mechanism:
Fiber is the “brake pedal” for digestion. It slows down how fast sugar enters your blood. Juice is “all gas, no brakes.” Drinking 8oz of orange juice causes a sharper insulin spike than eating three whole oranges. While juice is excellent for treating a low (emergency rescue), it is terrible for preventing one.
Safe vs. Unsafe Fruit Choices for Blood Sugar Stability
| Fruit Category | High Risk (Avoid) | Low Risk (Safe Swap) | The “Why” Factor |
| Melons | Watermelon, Cantaloupe | Berries (Strawberries, Blueberries, Raspberries) | Berries are high in fiber and low GI, preventing spikes. |
| Tropical | Pineapple, Mango, Papaya | Peaches, Plums, Apricots | Stone fruits have lower fructose loads and more pectin fiber. |
| Texture | Dried (Raisins, Dates, Figs) | Fresh whole fruit | Water volume adds satiety and slows absorption rate. |
| Banana | Brown/Spotted Peel | Green-tipped Peel | Green bananas contain resistant starch which acts as a prebiotic. |
| Form | Juice / Smoothie | Whole fruit with skin | Chewing signals satiety; skin fiber slows gastric emptying. |
Liquid Sugars and Beverages That Trigger Insulin Spikes
Liquids digest faster than solids. When you drink your calories, they bypass the mechanical breakdown of chewing and the churning of the stomach, arriving in the small intestine rapidly. This speed is the enemy of stable blood glucose levels.
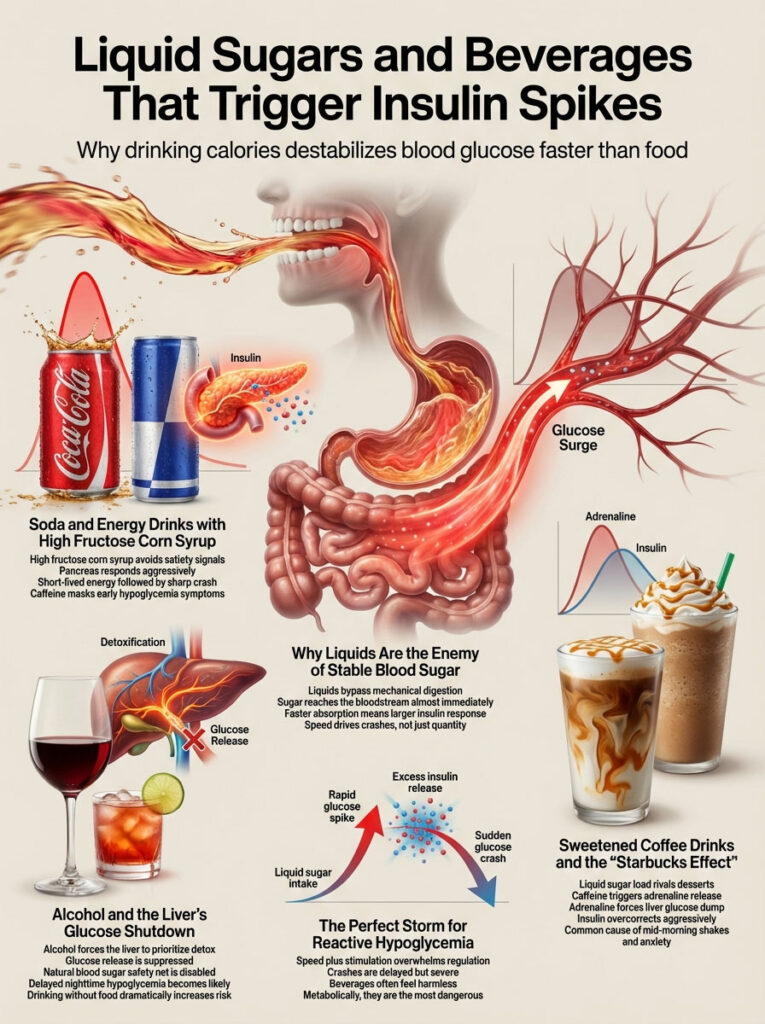
7. Soda and Energy Drinks: The HFCS Danger
It is well known that soda is unhealthy, but for reactive hypoglycemia, it is kryptonite. Most sodas use High Fructose Corn Syrup (HFCS). HFCS does not trigger the “I’m full” hormones (leptin) in the brain, but it does trigger a massive response from the pancreas.
The Outcome:
You get a burst of energy for 30 minutes, followed by a devastating blood sugar crash. Energy drinks are often worse because they combine massive amounts of sugar with caffeine. The caffeine can increase anxiety and palpitations, masking the early warning signs of a drop until it is too late.
8. Does Alcohol Cause Low Blood Sugar? (The Gluconeogenesis Block)
This is a critical section for adults in the USA. Many people ask, “Does alcohol cause low blood sugar?” The answer is a definitive yes, but the mechanism is unique and often misunderstood.
The Mechanism (Gluconeogenesis Inhibition):
Your liver has two primary jobs: detoxifying your blood and releasing stored glucose (glycogen) to keep your energy stable between meals. However, the liver cannot do both jobs simultaneously with equal efficiency. When you drink alcohol, the liver views it as a toxin and prioritizes filtering it out above all else.
While the liver is busy scrubbing alcohol, it stops releasing glucose. If your blood sugar drops during this time—perhaps from dancing, talking, or simply time passing—your body’s natural safety net (the liver dump) is turned off. This can lead to severe, delayed hypoglycemia, often happening while you sleep, which is dangerous. Never drink on an empty stomach.
9. Sweetened Coffee Drinks and The “Starbucks Effect”
The modern coffee shop menu is a minefield for those with blood sugar issues. A standard flavored latte or frappuccino can contain 40 to 60 grams of liquid sugar.
The Double Whammy:
You are getting a massive dose of liquid sugar combined with caffeine. Caffeine triggers adrenaline release. Adrenaline prompts the liver to dump sugar. So you get a sugar spike from the drink plus a sugar dump from the liver, followed by a massive insulin overreaction. This “Starbucks Effect” is a common cause of mid-morning shakes and anxiety.
Worst Breakfast Foods for Reactive Hypoglycemia
Breakfast is arguably the most dangerous meal of the day for reactive hypoglycemia. In the morning, cortisol levels are naturally higher (the “Cortisol Awakening Response”), which can make insulin management tricky. A carb-heavy breakfast guarantees a blood sugar crash by 10:30 AM.

10. Sugary Cereals and The Marketing Trap
Walk down the cereal aisle of any American grocery store, and you will see boxes boasting “heart healthy whole grains” that are actually 40% sugar by weight.
Why avoid it:
Processed cereals digest rapidly. They are typically low in protein and healthy fats. Without those buffers, they are just crunchy sugar. Even “healthy” granolas can be loaded with hidden sugars. This is one of the top foods to avoid with low blood sugar because it sets you up for a day of chasing your energy levels.
11. Is Instant Oatmeal Good for Hypoglycemia?
Oatmeal is often prescribed for heart health, but the type of oat matters significantly.
The Distinction:
Steel-cut oats and rolled oats take time to digest because the oat groat is intact or mostly intact. Instant oatmeal, however, has been steamed, rolled thin, and pre-cooked. This processing breaks down the cellular structure. To your body, instant oatmeal looks a lot like sugar. It causes a rapid rise in glucose compared to the slow burn of steel-cut oats. If you eat instant oats with brown sugar, you are inviting a crash.
12. Pancakes, Waffles, and Syrup
This traditional American breakfast is a metabolic disaster. It consists of refined white flour (high GI) covered in syrup (pure sugar).
The Instance:
Eating a stack of pancakes is effectively injecting glucose into your system. There is rarely enough protein in this meal to slow the absorption. The “sugar high” feels good for 45 minutes, but the drop is steep. If you must have pancakes, use almond flour or coconut flour and skip the syrup in favor of smashed berries.
13. Pastries, Donuts, and Trans Fats
Donuts and danishes combine two things that wreck metabolic health: refined sugar and inflammatory oils (trans fats or processed vegetable oils).
Why avoid it:
This combination creates inflammation and contributes to insulin resistance over time. In the short term, the refined flour creates a spike that ensures you will be hungry and shaking within two hours. The fat in donuts is usually not the “healthy” kind that slows absorption beneficially; rather, it often impairs insulin sensitivity.
Refined Carbohydrates and Processed Foods That Cause Crashes
These are the “beige foods” that make up the bulk of the Standard American Diet. They are stripped of nutrients and fiber, leaving only starch that acts like sugar.
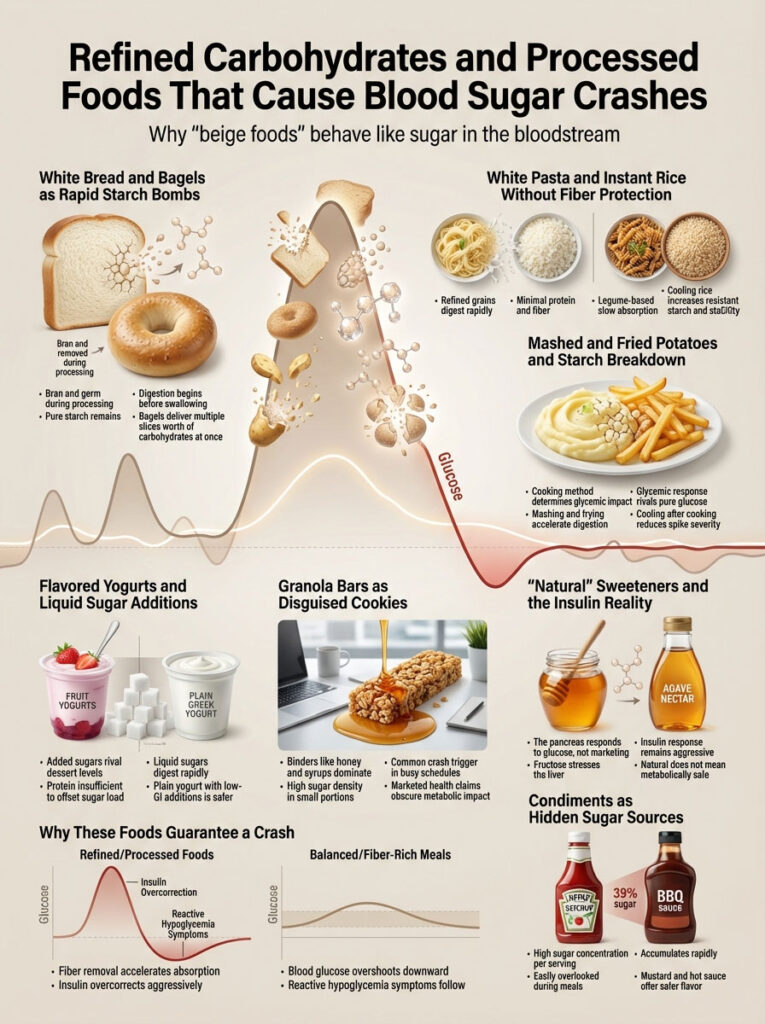
14. White Bread and Bagels: The Starch Bomb
White bread is made from wheat that has had the bran and germ removed. These parts contain the fiber and nutrients. What is left is the endosperm, which is pure starch.
Why avoid it:
Your saliva contains an enzyme called amylase which starts breaking down white bread before you even swallow it. It enters the bloodstream rapidly. Bagels are particularly deceptive because they are extremely dense; one large bagel can equal four or five slices of bread in carbohydrate content.
15. White Pasta and Instant Rice
Similar to bread, white pasta and instant rice are stripped carbohydrates.
The Swap:
To maintain stable blood glucose levels, switch to legume-based pastas (chickpea or lentil) which have high protein and fiber content. For rice, choose Basmati (which naturally has a lower GI) or brown rice. Always eat rice with a serving of fat (like olive oil or butter) or cool the rice after cooking to increase resistant starch.
16. Mashed and Fried Potatoes
Potatoes are a vegetable, but their glycemic impact depends heavily on how they are cooked.
The Science:
Boiling and mashing a potato breaks down the starch granules, making them incredibly easy to digest. Mashed potatoes have a GI nearly as high as pure glucose. Fries are similar.
- Note: If you cook a potato and let it cool (like in potato salad), it develops “resistant starch,” which lowers the GI. But generally, hot fluffy potatoes are a trigger for postprandial hypoglycemia.
17. Flavored Yogurts and Hidden Sugars
Yogurt is a great source of protein, but flavored varieties are often loaded with sugar.
The Instance:
Check the label on a “fruit on the bottom” yogurt. You will often see 15 to 25 grams of added sugar. That is more than a glazed donut. The protein in the yogurt is not enough to counteract that much liquid sugar. Always buy plain Greek yogurt and add your own low-GI fruit or a drop of stevia.
18. Granola Bars: The Healthy Cookie
Marketing has convinced us that granola bars are health food. In reality, most are cookies.
Why avoid it:
To make the oats stick together in a bar shape, manufacturers use honey, syrup, or brown rice syrup. These binders drive up the sugar content. They are one of the most common foods that cause blood sugar crash in children and office workers who use them as a “quick fix” for hunger.
19. “Natural” Sweeteners: Honey and Agave Nectar
Many people on a reactive hypoglycemia diet think they can switch from white sugar to honey or agave nectar and be safe.
The Truth:
Your pancreas does not care if the sugar is organic, raw, or “natural.” It only sees the glucose molecule. Agave is particularly high in fructose, which can stress the liver and contribute to insulin resistance. For prevention, these must be limited just like table sugar. While honey has some antimicrobial properties, metabolically, it is still a sugar spike.
20. Condiments: Ketchup and BBQ Sauce
This is the hidden source of sugar that catches everyone off guard.
The Data:
Ketchup is roughly 30% sugar. Barbecue sauce is often up to 40% sugar (molasses and honey). Adding a generous amount of BBQ sauce to your chicken can unknowingly add 20g of sugar to your meal, triggering a crash later. Always read labels and look for “no sugar added” varieties or use mustard and hot sauce.
Strategic Low Blood Sugar Diet Plan and Pairing Protocols
Now that we know the foods to avoid with low blood sugar, what should you eat? The secret is not just what you eat, but how you eat it. This is the core of a successful low blood sugar diet plan.
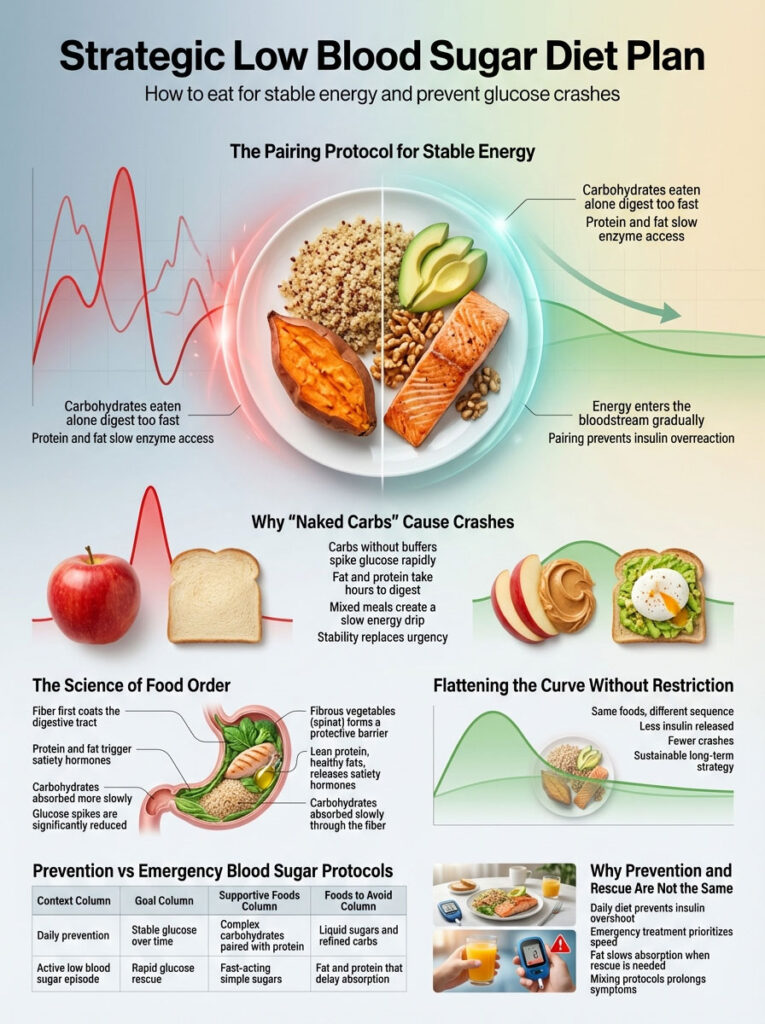
The “Pairing Protocol” for Stable Energy
This is the golden rule of hypoglycemia management. Never eat a naked carb. A “naked carb” is a carbohydrate eaten alone (e.g., an apple, a piece of toast, a handful of crackers).
The Solution:
Always “clothe” your carbs with protein, healthy fats, or fiber.
- Bad: Eating an apple alone.
- Good: Eating an apple with peanut butter.
- Bad: Eating dry toast.
- Good: Eating toast with avocado and a hard-boiled egg.
Fat and protein take hours to digest. When you mix them with carbs in the stomach, they physically block the enzymes from breaking down the sugar too fast. This creates a slow, steady trickle of energy into the bloodstream rather than a flood.
The Science of Food Order
Recent research suggests that the order in which you eat food matters for insulin response.
- Eat Vegetables First: The fiber coats the stomach lining and slows gastric emptying.
- Eat Protein/Fat Second: This signals the body to start slow digestion and release satiety hormones.
- Eat Carbs Last: By the time the carbs hit your stomach, digestion is already slowed down, and the glucose spike is blunted.
This simple change can reduce the post-meal glucose spike by up to 50%, promoting stable blood glucose levels without changing the food on your plate.
Prevention Diet vs. Emergency Treatment Protocols
It is vital to distinguish between preventing a low and fixing one that is already happening. Mixing these up is a common mistake.
| Scenario | Goal | Recommended Foods | Foods to Avoid |
| Prevention (Daily Diet) | Stable Blood Glucose Levels | Complex Carbs + Protein<br>(Greek yogurt, nuts, chicken, sourdough bread, beans) | Simple Sugars<br>(Juice, soda, white bread, candy, dried fruit) |
| Emergency (Low <70 mg/dL) | Rapid Spike (Rescue) | Fast-Acting Sugar<br>(4oz Juice, Glucose Tabs, Tablespoon of Honey, Skittles) | Fat/Protein<br>(Chocolate, nuts, peanut butter) – Fat slows absorption when speed is critical. |
Emergency Treatment: The 15-15 Rule for Low Blood Sugar
If you accidentally eat a trigger food and find yourself crashing, you need a medical protocol. Do not just eat everything in the kitchen (a common reaction called “panic eating”).
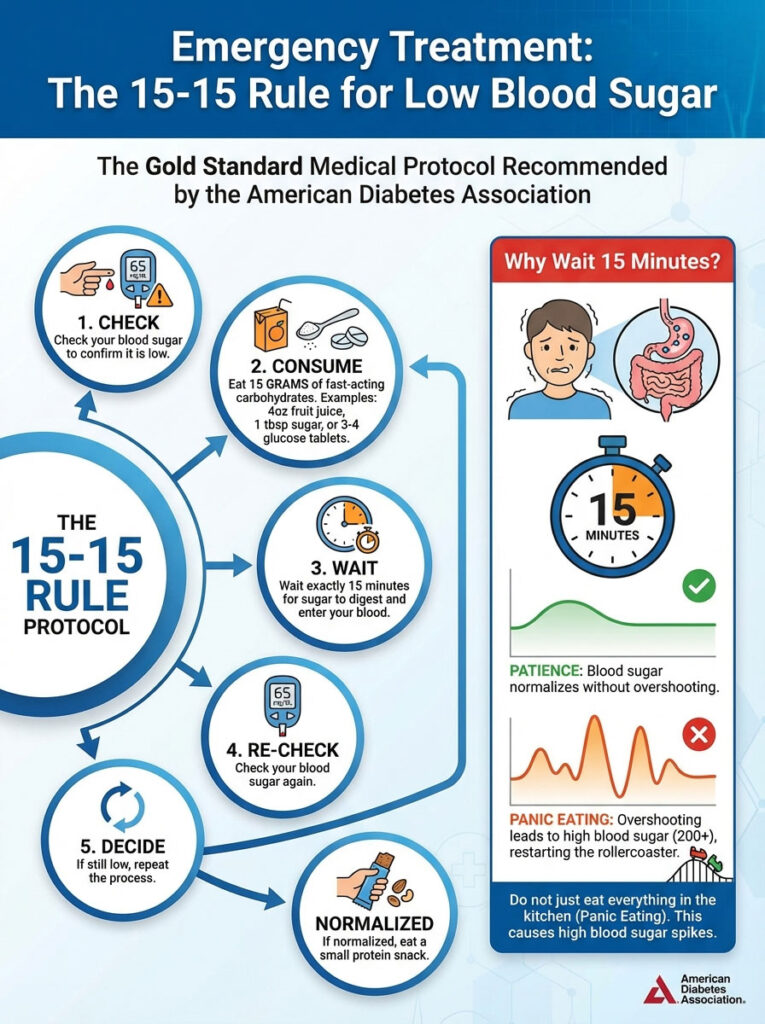
The 15-15 Rule Protocol
The 15-15 rule for low blood sugar is the gold standard recommended by the American Diabetes Association.
- Check: Check your blood sugar (if possible) to confirm it is low.
- Consume: Eat 15 grams of fast-acting carbohydrates. Good examples include 4oz of fruit juice, 1 tablespoon of sugar, or 3-4 glucose tablets.
- Wait: Wait exactly 15 minutes.
- Re-check: Check your blood sugar again.
- Decide: If it is still low, repeat the process. If it has normalized, eat a small protein snack.
Why wait 15 minutes?
It takes about 15 minutes for sugar to digest and enter your blood. If you keep eating during that 15 minutes because you still feel shaky, you will overshoot and end up with high blood sugar (200+), which restarts the blood sugar rollercoaster.
Frequently Asked Questions (FAQs)
What specific foods trigger reactive hypoglycemia?
The primary triggers are foods with a high Glycemic Index (over 70). This includes sugary beverages, white bread, white rice, pasta, and high-sugar fruits like watermelon. These foods cause a rapid insulin spike, leading to a subsequent crash.
Is watermelon bad for low blood sugar?
Yes, watermelon is considered one of the foods to avoid with low blood sugar. It has a high glycemic load and lacks the fiber necessary to slow down sugar absorption, often causing rapid drops in glucose levels an hour after eating.
Why do I crash after eating fruit?
You likely crash because you are eating high-fructose fruits (like mango or ripe bananas) without pairing them with protein or fat. The sugar enters your bloodstream too fast. Always eat fruit with nuts, cheese, or yogurt to maintain stable blood glucose levels.
Does alcohol cause low blood sugar in non-diabetics?
Yes. Alcohol inhibits gluconeogenesis, which is the liver’s process of making new glucose. If you drink on an empty stomach, your liver is too busy processing the alcohol to release sugar into your blood, leading to a risk of severe hypoglycemia.
What is the best breakfast for hypoglycemia?
The best breakfast for hypoglycemia is savory, not sweet. Focus on high protein and healthy fats. Examples include scrambled eggs with spinach and avocado, or plain Greek yogurt with walnuts and berries. Avoid cereal, toast, and juice.
Can caffeine cause sugar crashes?
Caffeine stimulates the adrenal glands to release adrenaline and cortisol. This can cause a temporary spike in blood sugar followed by a crash. Additionally, caffeine symptoms (shaking, anxiety) can mimic and mask the actual signs of low blood sugar.
What should I eat before bed to prevent low blood sugar?
To prevent nighttime drops, eat a slow-digesting snack containing protein and fat. Good options include a handful of almonds, a slice of whole-grain toast with peanut butter, or cottage cheese. This provides a steady release of energy throughout the night.
Is honey good for low blood sugar?
Honey is good for treating a crash because it acts fast, but it is bad for preventing one. It is a simple sugar that spikes insulin. Do not use honey as a sweetener if you are trying to follow a reactive hypoglycemia diet.
How long after eating does a sugar crash happen?
Postprandial hypoglycemia typically occurs 2 to 4 hours after a meal. If you feel shaky immediately after eating, it might be a different issue (like dumping syndrome), but the classic “crash” is a delayed reaction to the insulin spike.
What is the difference between simple and complex carbohydrates?
Simple carbohydrates (sugar, white flour) have short molecular chains and digest instantly, causing spikes. Complex carbohydrates (beans, vegetables, whole grains) have long chains and fiber, requiring more time to break down, which supports a low blood sugar diet plan.
Can I eat potatoes on this diet?
You should avoid hot, mashed, or fried white potatoes as they have a very high GI. However, waxy potatoes or sweet potatoes eaten with the skin on, and paired with protein, are generally safer. Cooling cooked potatoes also increases resistant starch, lowering the GI.
Why do I shake when I’m hungry?
The shaking is caused by the release of adrenaline. When blood sugar drops, the body releases stress hormones to signal the liver to dump stored sugar. These hormones cause the physical symptoms of trembling, sweating, and anxiety associated with a blood sugar crash.
Disclaimer: This content is for informational purposes only and does not constitute medical advice. Reactive hypoglycemia can be a symptom of underlying conditions such as pre-diabetes or insulin resistance. Always consult with a healthcare provider or a registered dietitian before making significant changes to your diet or if you experience frequent unexplained blood sugar drops.
References:
- Mayo Clinic: Reactive Hypoglycemia – Causes and Treatments.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Low Blood Glucose (Hypoglycemia).
- Harvard T.H. Chan School of Public Health: Glycemic Index and Glycemic Load.
- American Diabetes Association: Standards of Care in Diabetes.