The weeks and months following childbirth represent a profound physiological transition that is often underestimated in standard health advice. You are not simply “recovering” from a major medical event; you are actively sustaining another human life through your own metabolic processes.
Table of Contents
This period, frequently called the fourth trimester, is characterized by sleepless nights, hormonal fluctuations, and a hunger that can feel insatiable. New mothers in the USA often find themselves navigating a maze of conflicting dietary advice while trying to heal their own bodies and ensure their infants thrive.

Nutrition during this phase is the foundation of your well-being. It dictates your energy levels, influences your mood, and provides the essential building blocks for the milk your baby consumes. While the body is incredibly resilient and will prioritize the nutrient content of breast milk even if your diet is less than perfect, this often comes at a cost to your own nutrient stores.
This depletion can lead to fatigue, hair loss, and a slower recovery. This guide serves as a comprehensive, evidence-based roadmap. We will move beyond generic advice and delve deep into the biochemistry of lactation, exploring how specific nutrients influence milk volume and maternal health. We present a detailed, dietitian-designed 7-day breastfeeding meal plan tailored to boost milk supply, enhance energy, and facilitate deep postpartum recovery.
Nutritional Requirements for Breastfeeding Mothers and Milk Production
Understanding the caloric and nutritional demands of lactation is the first step toward creating a sustainable meal plan. Producing breast milk is an energy-intensive process. The body burns calories to synthesize the fats, proteins, and lactose found in human milk.

Caloric Intake for Lactation and Energy Balance
The caloric cost of exclusive breastfeeding is significant. Health organizations like the USDA and the CDC estimate that a nursing mother requires an additional 330 to 500 calories per day during the first six months of lactation. This brings the total daily requirement for many women to between 2,200 and 2,500 calories, though this varies based on pre-pregnancy BMI and activity levels.
It is crucial to understand that these “extra” calories should not come from empty sources like sugary beverages or processed snacks. The goal is nutrient density. Your body needs fuel to maintain the glandular tissue in the breasts and to support the “let-down” reflex regulated by oxytocin. If caloric intake drops too low—typically below 1,500 to 1,800 calories—the body may enter a conservation mode which can negatively impact milk volume. A breastfeeding diet plan must focus on abundance rather than restriction. This ensures that you have the stamina to handle the physical demands of caring for a newborn while maintaining a robust milk supply.
Importance of Hydration and Electrolytes for Milk Volume
Breast milk is approximately 87% water. This simple fact highlights why hydration is a non-negotiable aspect of a breastfeeding nutrition plan. When you nurse, oxytocin triggers thirst, a biological signal ensuring you replenish the fluids lost during the feeding. However, water alone is sometimes insufficient. Electrolytes like potassium, magnesium, and sodium play a key role in cellular hydration and muscle function.
The general recommendation for lactating women in the US is to consume about 128 ounces (16 cups) of total fluid daily. This total includes water, milk, herbal teas, and high-water-content foods like melons, cucumbers, and soups. Dehydration can manifest as headaches, lethargy, and a perceived drop in milk output. A practical strategy is to keep a large water bottle at every nursing station in your home. Drink to thirst, and monitor your urine color; pale yellow indicates optimal hydration.
Macronutrients Breakdown for Postpartum Recovery
To support tissue repair after birth, whether from a vaginal delivery or a C-section, and to ensure high-quality milk, your meals must be balanced with the right macronutrients.
High-Quality Protein Sources for Tissue Repair
Protein is essential for healing the uterus and perineal tissues. It is also a critical component of breast milk immune factors, including lactoferrin and immunoglobulins. Nursing mothers should aim for at least 65 to 70 grams of protein daily, though some experts suggest going up to 100 grams depending on activity levels. Incorporate diverse sources such as lean chicken, turkey, grass-fed beef, eggs, Greek yogurt, lentils, and tofu. Distributing protein intake across all meals helps stabilize blood sugar and prevents the mid-afternoon energy slump.
Complex Carbohydrates for Sustained Energy Levels
Carbohydrates are the body’s primary energy source. For a breastfeeding mom, complex carbohydrates are superior to simple sugars. Whole grains like oats, quinoa, brown rice, and whole wheat contain fiber which aids in digestion—a common concern postpartum. They provide a steady release of glucose into the bloodstream. This steady energy is vital for coping with fragmented sleep. Furthermore, carbohydrates stimulate the brain to produce serotonin, a neurotransmitter that aids in sleep and mood regulation.
Healthy Fats and Omega-3 DHA for Infant Brain Development
Fat is the most variable macronutrient in breast milk and is crucial for the infant’s rapid brain growth. The amount of fat in your milk fluctuates during a feed (hindmilk is richer in fat), but the type of fat you eat influences the fatty acid profile of your milk. Docosahexaenoic acid (DHA), an Omega-3 fatty acid, is particularly important for the development of the baby’s eyes and nervous system. Dietary sources include fatty fish like salmon, sardines, and trout, as well as plant-based sources like walnuts, chia seeds, and flaxseeds. Aiming for 200 to 300 mg of DHA daily is a standard recommendation for lactating women.
Essential Micronutrients and Vitamins for Breastfeeding Moms
While macronutrients provide the energy, micronutrients act as the catalysts for biological processes. During lactation, the need for certain vitamins and minerals increases significantly compared to pregnancy.

Iron Rich Foods to Combat Postpartum Fatigue
Iron deficiency anemia is a prevalent issue among new mothers due to blood loss during childbirth and the cessation of prenatal vitamins. Iron is vital for transporting oxygen in the blood. Low iron levels are directly linked to exhaustion, irritability, and even a decrease in milk supply. The Recommended Dietary Allowance (RDA) for iron during lactation is 9-10 mg per day, but many women need more to replenish stores. Heme iron from animal products (beef, dark poultry meat) is absorbed most efficiently. Non-heme iron from plants (spinach, lentils, fortified cereals) should be paired with Vitamin C-rich foods like bell peppers or strawberries to enhance absorption.
Calcium and Vitamin D for Maternal Bone Health
During lactation, if a mother’s diet is deficient in calcium, the body will resort to bone resorption—leaching calcium from the mother’s bones to ensure the breast milk remains calcium-rich for the baby. To protect your long-term bone density, aim for 1,000 mg of calcium daily. Good sources include dairy products, fortified plant milks, tofu set with calcium sulfate, and leafy greens like bok choy and kale. Vitamin D works in tandem with calcium. Since breast milk is naturally low in Vitamin D, mothers are often advised to supplement with 6,400 IU daily (if not giving drops to the baby) or ensure the baby receives Vitamin D drops directly, per AAP guidelines.
Choline and Iodine for Infant Neurodevelopment
Choline is a nutrient that has gained significant attention in recent years for its role in brain development, similar to folate. It supports the structure of cell membranes and memory function. Eggs (specifically the yolk), lean meats, and fish are excellent sources. Iodine is another critical mineral, required for the production of thyroid hormones which regulate metabolism and growth. The demand for iodine increases during breastfeeding. Using iodized salt and consuming dairy or seafood can help meet the recommended 290 mcg daily intake.
Comparison of Nutrient Needs: Pregnancy vs. Lactation
The table below illustrates how your nutritional requirements shift from the third trimester of pregnancy to the lactation period. Note the increased need for specific nutrients like Vitamin A, C, and Iodine, and the continued need for hydration and energy.
| Nutrient Category | Requirement During Pregnancy (3rd Trimester) | Requirement During Lactation (0-6 Months) | Primary Function in Breastfeeding |
| Daily Calories | +300 to +450 kcal | +330 to +500 kcal | Fuels milk synthesis and maternal metabolism. |
| Protein | 71 g/day | 71 g/day (often higher advised) | Supports tissue repair and milk protein synthesis. |
| Hydration | ~80 oz (10 cups) | ~128 oz (16 cups) | Maintains milk volume and maternal electrolyte balance. |
| Iron | 27 mg/day | 9–10 mg/day (varies by blood loss) | Prevents maternal anemia and fatigue. |
| Calcium | 1,000 mg/day | 1,000 mg/day | Preserves maternal bone density. |
| Folate | 600 mcg/day | 500 mcg/day | Supports cell division and growth. |
| Iodine | 220 mcg/day | 290 mcg/day | Critical for infant thyroid and brain development. |
| Vitamin A | 770 mcg/day | 1,300 mcg/day | Supports immune function and vision. |
| Vitamin C | 85 mg/day | 120 mg/day | Tissue repair and iron absorption enhancer. |
Top Galactagogue Foods to Increase Milk Supply Naturally
In many cultures, specific foods are revered for their ability to promote milk production. These are known as galactagogues. While scientific data on some of these foods is mixed, they are generally nutrient-dense whole foods that support overall health, making them a safe and beneficial addition to a breastfeeding diet to increase milk supply.

Benefits of Oats and Barley for Lactation
Oats are perhaps the most widely recommended food for low milk supply. They are a rich source of beta-glucan, a type of fiber that serves as a precursor to prolactin, the milk-making hormone. Additionally, oats are high in iron and constitute a comforting, warm meal that can help lower stress levels—a known inhibitor of the let-down reflex. Barley contains similar beta-glucan properties and can be used in soups or stews as a hearty grain alternative.
Efficacy of Brewer’s Yeast and Flaxseeds
Brewer’s yeast is a traditional remedy often used in “lactation cookies.” It is a powerhouse of B-vitamins and trace minerals like chromium and selenium. These nutrients support maternal energy levels and mood, which indirectly helps with supply. Flaxseeds (and chia seeds) are loaded with alpha-linolenic acid (ALA) and phytoestrogens. Ground flaxseed is easily digestible and can be sprinkled on yogurt or oatmeal to boost healthy fat intake.
Leafy Greens and Phytoestrogens in Breast Milk
Dark leafy greens such as spinach, kale, Swiss chard, and collard greens are nutritional superstars. They are packed with calcium, iron, and Vitamins A and K. Some greens also contain phytoestrogens, plant compounds that mimic estrogen and may aid in lactation. In Traditional Chinese Medicine (TCM), cooked greens are often recommended to nourish the blood and support milk flow.
Legumes and Nuts for Nutrient Density
Chickpeas (garbanzo beans) and lentils have been used as galactagogues in Mediterranean and Middle Eastern cultures for centuries. They provide a robust combination of plant protein, fiber, and calcium. Nuts, particularly almonds and walnuts, supply healthy fats and antioxidants. Almonds are specifically cited in Ayurvedic traditions as a food that nourishes the milk.
Functional Benefits of Lactation Superfoods
The following table breaks down specific “superfoods” often found in a breastfeeding meal plan, detailing the specific bioactive components that assist in lactation and recovery.
| Superfood Item | Key Bioactive Component | Mechanism of Action for Mom | Benefit Transferred to Baby |
| Rolled Oats | Beta-glucan & Saponins | Stimulates prolactin secretion; supports digestion | Provides consistent energy; may help settle baby |
| Wild Salmon | DHA (Omega-3) & Vitamin D | Reduces inflammation; supports postpartum mood | Essential for retinal and cortical (brain) maturation |
| Brewer’s Yeast | B-Complex Vitamins & Chromium | Combat fatigue; balances blood sugar levels | Supports healthy nervous system development |
| Fennel Seeds | Anethole (Phytoestrogen) | Mimics estrogen to boost supply; aids digestion | Can help relieve gas and colic symptoms via milk |
| Eggs (Whole) | Choline & High-quality Protein | Rebuilds cellular membranes; muscle repair | Choline is critical for memory and cognitive function |
| Greek Yogurt | Calcium, Probiotics, Protein | Protects bone mineral density; gut health | Calcium supports rapid skeletal growth |
| Apricots | Phytoestrogens & Tryptophan | Boosts prolactin; Tryptophan aids sleep/calm | Vitamins A and C support immune system |
| Almonds | Monounsaturated Fats & Calcium | Provides calorie-dense energy; supports satiety | Healthy fats promote weight gain in infants |
Comprehensive 7-Day Breastfeeding Meal Plan to Boost Milk Supply
This practical, dietitian-style meal plan is designed to deliver approximately 2,200 to 2,500 calories per day. It emphasizes whole grains, lean proteins, and hydration. The meals are structured to keep blood sugar stable and energy high. Feel free to adjust portion sizes based on your hunger; your body is the best guide.
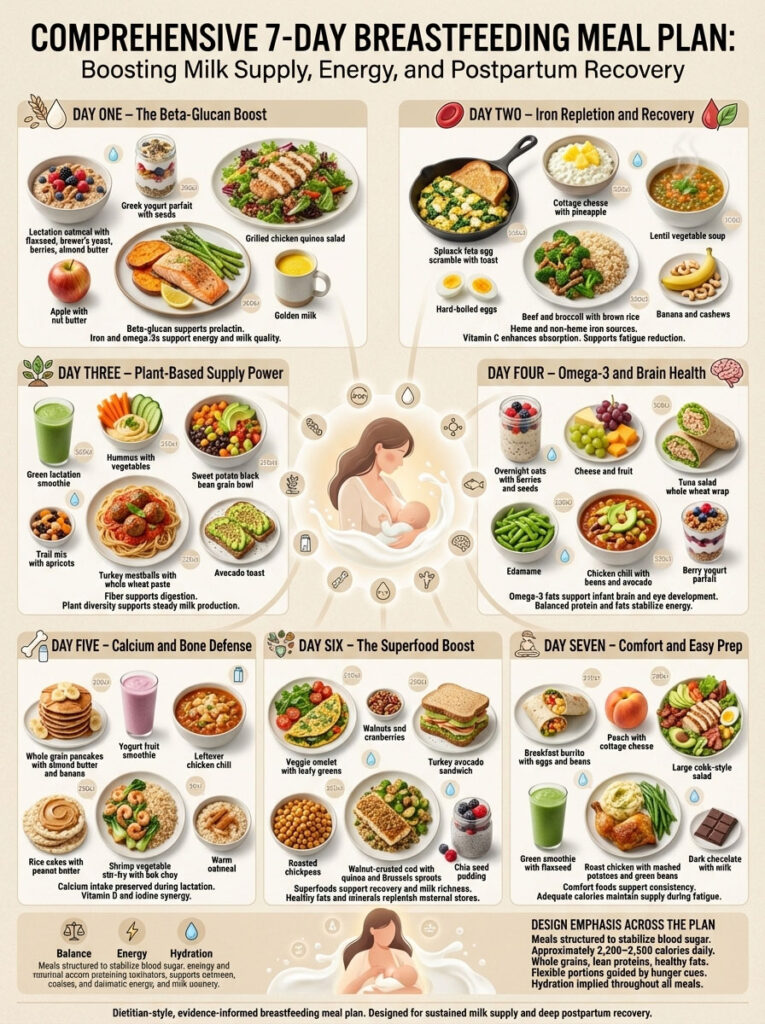
Day 1: The Beta-Glucan Boost
Focus: Establishing a routine with oat-based galactagogues.
- Breakfast: Lactation Oatmeal Bowl. Cook 1/2 cup of rolled oats with 1 cup of fortified oat milk. Stir in 1 tablespoon of ground flaxseed and 1 teaspoon of brewer’s yeast. Top with sliced strawberries and a dollop of almond butter for healthy fats.
- Morning Snack: Greek Yogurt Parfait. 1 cup of plain Greek yogurt layered with granola and pumpkin seeds (zinc source).
- Lunch: Grilled Chicken & Quinoa Salad. 4 oz grilled chicken breast served over a bed of mixed greens, cucumber, and 1/2 cup cooked quinoa. Dress with olive oil and lemon juice.
- Afternoon Snack: Apple & Nut Butter. One large sliced apple with 2 tablespoons of walnut butter.
- Dinner: Baked Salmon with Asparagus. 6 oz salmon fillet seasoned with dill and lemon. Serve with a side of roasted asparagus and a medium baked sweet potato.
- Evening Snack: Golden Milk. Warm almond milk whisked with turmeric, ginger, and a dash of honey.
Day 2: Iron Repletion & Recovery
Focus: Heme and non-heme iron sources to fight fatigue.
- Breakfast: Spinach and Feta Scramble. Three eggs scrambled with a handful of fresh spinach and 1 oz feta cheese. Serve with a slice of sprouted grain toast.
- Morning Snack: Cottage Cheese Bowl. 1 cup cottage cheese topped with fresh pineapple chunks (Vitamin C aids absorption).
- Lunch: Lentil & Vegetable Soup. A hearty bowl of lentil soup made with carrots, celery, and kale. Pair with whole-grain crackers.
- Afternoon Snack: Hard-Boiled Eggs. Two eggs sprinkled with paprika and a pinch of sea salt.
- Dinner: Beef & Broccoli Stir-Fry. 5 oz lean beef strips stir-fried with broccoli, bell peppers, and ginger over brown rice.
- Evening Snack: Banana & Cashews. One banana paired with a small handful of raw cashews.
Day 3: Plant-Based Supply Power
Focus: High fiber and plant proteins to support digestion.
- Breakfast: Green Lactation Smoothie. Blend 1 cup spinach, 1 frozen banana, 1 tablespoon chia seeds, 1 scoop protein powder, and 1.5 cups almond milk.
- Morning Snack: Hummus Plate. 1/2 cup hummus served with sliced red peppers and carrots.
- Lunch: Sweet Potato & Black Bean Bowl. Roasted sweet potato cubes, black beans, corn, and avocado over a base of brown rice. Top with cilantro lime dressing.
- Afternoon Snack: Trail Mix. A mix of almonds, dried apricots (phytoestrogens), and dark chocolate chips.
- Dinner: Turkey Meatballs & Whole Wheat Pasta. Lean ground turkey meatballs served with marinara sauce over whole wheat spaghetti. Side of steamed green beans.
- Evening Snack: Avocado Toast. Half an avocado mashed on a slice of whole-grain bread.
Day 4: Omega-3 & Brain Health
Focus: DHA-rich foods for baby’s neurological development.
- Breakfast: Overnight Oats. Prepare the night before: Oats, chia seeds, milk, and blueberries. Top with hemp hearts in the morning.
- Morning Snack: Cheese & Fruit. A mozzarella cheese stick paired with a pear.
- Lunch: Tuna Salad Wrap. Canned light tuna (low mercury) mixed with Greek yogurt (instead of mayo) and celery, wrapped in a whole wheat tortilla with lettuce.
- Afternoon Snack: Edamame. 1 cup steamed edamame in pods, sprinkled with sea salt.
- Dinner: Slow Cooker Chicken Chili. White beans, chicken breast, corn, and mild green chilies. Top with avocado and a dollop of yogurt.
- Evening Snack: Berry Parfait. Mixed berries with a small serving of yogurt.
Day 5: Calcium & Bone Defense
Focus: ensuring maternal calcium stores are protected.
- Breakfast: Whole Grain Pancakes. Topped with almond butter and banana slices. Serve with a glass of calcium-fortified orange juice.
- Morning Snack: Smoothie Boost. Blend strawberries, yogurt, and a splash of milk.
- Lunch: Leftover Chicken Chili. A generous serving of the chili from the previous dinner.
- Afternoon Snack: Rice Cake & Peanut Butter. Two brown rice cakes topped with natural peanut butter.
- Dinner: Shrimp & Vegetable Stir-Fry. Shrimp (source of iodine) stir-fried with snap peas and bok choy over wild rice.
- Evening Snack: Warm Oatmeal. A small bowl of oats made with milk to promote sleep.
Day 6: The Superfood Saturday
Focus: Incorporating nutrient-dense ingredients for a weekend boost.
- Breakfast: Veggie Omelet. Eggs cooked with mushrooms, onions, and Swiss chard.
- Morning Snack: Walnuts & Cranberries. A handful of walnuts mixed with dried cranberries.
- Lunch: Turkey & Avocado Sandwich. Sliced turkey breast, avocado, lettuce, and tomato on sprouted grain bread.
- Afternoon Snack: Roasted Chickpeas. Crunchy chickpeas seasoned with cumin and paprika.
- Dinner: Cod with Walnut Crust. Baked cod fillets topped with crushed walnuts and herbs. Serve with roasted Brussels sprouts and quinoa.
- Evening Snack: Chia Seed Pudding. Made with coconut milk and a drop of vanilla extract.
Day 7: Easy Prep & Comfort
Focus: Simple, comforting meals that allow for rest.
- Breakfast: Breakfast Burrito. Scrambled eggs, black beans, salsa, and cheddar cheese wrapped in a tortilla.
- Morning Snack: Peach & Cottage Cheese. Sliced fresh peach served with protein-rich cottage cheese.
- Lunch: Large Cobb Salad. Mixed greens topped with grilled chicken, hard-boiled egg, sunflower seeds, and vinaigrette.
- Afternoon Snack: Green Smoothie. Spinach, pineapple, flaxseed, and water or coconut water.
- Dinner: Roast Chicken Dinner. Roasted chicken leg/thigh (dark meat for iron) with mashed potatoes and green beans.
- Evening Snack: Dark Chocolate & Milk. A square of 70% dark chocolate and a glass of milk.
Adapting the Breastfeeding Diet for Special Needs and Weight Loss
Every mother’s journey is different. You may encounter specific challenges such as infant allergies, dietary preferences, or the desire to return to pre-pregnancy weight.

Dairy-Free Breastfeeding Diet Plan for Colicky Babies
Cow’s Milk Protein Allergy (CMPA) is a common issue where proteins from the dairy the mother eats pass into the breast milk, causing reactions in the baby. Symptoms include mucousy or bloody stools, eczema, and extreme fussiness. If a pediatrician advises a dairy elimination diet, you must ensure you replace the lost calcium and protein.
- Substitutes: Use fortified oat, almond, or soy milk. Look for yogurts made from coconut or almond milk.
- Hidden Dairy: Read labels for casein, whey, and lactoglobulin.
- Calcium Sources: Increase intake of calcium-set tofu, broccoli, bok choy, and fortified orange juice to meet the 1,000 mg daily requirement.
Vegetarian and Vegan Breastfeeding Meal Plan Essentials
A plant-based diet can support healthy lactation, but it requires vigilance regarding Vitamin B12, Iron, and Zinc.
- Vitamin B12: This vitamin is found almost exclusively in animal products. Vegan mothers must take a supplement or consume significant amounts of fortified nutritional yeast to prevent neurological damage in the infant.
- Protein Combining: Ensure you are getting all essential amino acids by varying your protein sources—rice and beans, hummus and pita, or quinoa (a complete protein).
- Algae-Based DHA: Since fish is off the table, consider an algae-based Omega-3 supplement to ensure your breast milk contains adequate DHA for brain development.
Safe Weight Loss Strategies While Maintaining Milk Supply
The pressure to “bounce back” is culturally pervasive in the USA, but aggressive dieting can be dangerous. Rapid weight loss releases toxins stored in body fat into the bloodstream, which can end up in milk. Furthermore, a severe caloric deficit triggers a stress response that can lower milk supply.
- Timeline: Wait until breastfeeding is well-established (6-8 weeks) before actively trying to lose weight.
- The Approach: Aim for a slow loss of about 1 pound per week. Maintain a minimum of 1,800 calories.
- Volume Eating: Focus on high-volume, low-calorie foods like vegetables and broths to keep you full without blowing your calorie budget.
Foods to Avoid and Safety Guidelines for Nursing Mothers
Navigating food safety while breastfeeding is less restrictive than during pregnancy, but there are still important guidelines to follow to ensure the safety of the baby.

Managing Caffeine and Alcohol Intake While Nursing
- Caffeine: Caffeine does pass into breast milk. While most babies tolerate moderate amounts, younger infants metabolize it very slowly. It accumulates in their system, leading to wakefulness and irritability. Limit intake to roughly 300 mg per day (2-3 cups of coffee).
- Alcohol: Alcohol moves freely between the blood and breast milk. The concentration in your milk is the same as in your blood. The safest practice is to avoid alcohol. However, an occasional drink is generally considered safe if you wait 2 hours per drink before nursing. “Pumping and dumping” does not remove alcohol from the milk already in the breast; it only relieves pressure. The alcohol leaves the milk as it leaves your bloodstream.
High Mercury Fish and Safe Seafood Choices
Mercury is a neurotoxin that can impair the developing nervous system of the infant. While fish is an excellent source of protein and DHA, you must be selective.
- Avoid: Shark, Swordfish, King Mackerel, Tilefish, and Bigeye Tuna.
- Choose: Salmon, Pollock, Catfish, Shrimp, and Canned Light Tuna. These can be eaten 2-3 times a week.
Supplements and Herbal Safety Precautions
Not all “natural” herbs are safe. Fenugreek, while popular, can cause gastrointestinal distress in the mother and gas in the baby. It can also interfere with thyroid medication and blood sugar levels. Always consult an International Board Certified Lactation Consultant (IBCLC) or healthcare provider before starting high-dose herbal supplements. Stick to trusted brands with third-party testing to avoid contamination.
Frequently Asked Questions
What specific foods will increase my milk supply within 24 hours?
While no single food works like a switch, consuming oats, brewer’s yeast, and ensuring aggressive hydration can help optimize your body for production. However, the most effective way to increase supply quickly is “power pumping” or nursing more frequently to signal demand to your body.
How many additional calories do I strictly need to eat while breastfeeding?
Standard guidelines recommend an extra 330 to 500 calories per day over your pre-pregnancy needs. This usually equates to one additional balanced meal or two substantial snacks. However, listen to your hunger cues; some women may need more during growth spurts.
Does drinking excessive water actually boost breast milk volume?
Drinking beyond thirst does not increase milk volume and can technically be uncomfortable. However, being dehydrated will lower volume. The goal is to stay hydrated enough that your urine is pale yellow. Forced over-hydration is not necessary.
Is it safe to eat spicy foods like chili or curry while nursing?
Yes, spicy foods are safe. The flavor of breast milk changes based on your diet, which can actually help broaden your baby’s palate. Unless you notice your baby becoming fussy or gassy specifically after you eat spice, there is no reason to avoid it.
Can I follow a low-carb or keto diet while breastfeeding?
Strict keto is generally not recommended during the establishment of lactation because carbohydrates are crucial for milk synthesis and maintaining serotonin levels. A moderate low-carb approach focusing on complex carbs (sweet potatoes, oats) is safer and more sustainable for energy.
What are the signs that my baby has a food sensitivity to my diet?
Symptoms often include skin rashes (eczema), persistent congestion, bloody or mucous-filled stools, and excessive, inconsolable crying (colic). If you suspect a sensitivity, try an elimination diet under the guidance of a pediatrician or dietitian.
How can I get enough protein on a vegetarian breastfeeding diet?
Prioritize eggs and dairy if you eat them. If not, combine plant proteins like beans and rice, use tofu and tempeh, and incorporate high-protein grains like quinoa. A clean, plant-based protein powder can also be a helpful supplement.
Do commercially bought lactation cookies really work?
They can be helpful because they contain galactagogues like oats and yeast, but they are not a medical cure. They are often high in sugar and calories. They should be treated as a supplement to a healthy diet, not a replacement for meals or frequent nursing.
Will caffeine keep my breastfed baby awake at night?
It is possible. Newborns take a long time to process caffeine. If you notice your baby is wide awake or jittery after you drink coffee, try limiting your intake to the morning hours or switching to decaf to see if sleep improves.
What are the best snacks for middle-of-the-night breastfeeding hunger?
Keep shelf-stable, one-handed snacks near your nursing chair. Good options include almonds, beef jerky, lactation bars, bananas, or squeezy apple sauce pouches. These provide quick fuel without the need for preparation.
Why do I feel ravenously hungry all the time while nursing?
Prolactin, the hormone that drives milk synthesis, also stimulates appetite. Additionally, your body is working harder than it did during pregnancy to produce milk. This hunger is a biological safety mechanism to ensure you take in enough energy.
Is it safe to take collagen peptides while breastfeeding?
generally, collagen is considered safe and provides extra protein which can help with tissue repair and hair loss. However, always check the label for added herbs or stimulants and consult your doctor to be sure.
Disclaimer
This article is intended for educational and informational purposes only and does not constitute medical advice, diagnosis, or treatment. The nutritional needs of every mother and infant are unique. Always seek the advice of your physician, pediatrician, or a qualified International Board Certified Lactation Consultant (IBCLC) with any questions you may have regarding a medical condition or dietary changes. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
References
- Centers for Disease Control and Prevention (CDC): Maternal Diet and Breastfeeding.
- United States Department of Agriculture (USDA): Dietary Guidelines for Americans, 2020-2025 (Lactation).
- National Institutes of Health (NIH): Drugs and Lactation Database (LactMed).
- Academy of Nutrition and Dietetics: Nutrition for Nursing Mothers.
- American Academy of Pediatrics (AAP): Policy Statement on Breastfeeding and the Use of Human Milk.








