The 7-Day Gastritis Healing Meal Plan is a specialized nutritional protocol designed to neutralize excess stomach acid and accelerate the repair of the compromised gastric mucosa. This regimented diet prioritizes low-acid foods with a pH above 5.0 to deactivate pepsin enzymes, which are responsible for tissue damage during flare-ups.
Table of Contents
The protocol follows three distinct clinical phases: an initial “Gastric Rest” phase (24–48 hours) utilizing liquid nutrition like bone broth to stop acute pain; a soft-solid transition phase (Days 3–5) incorporating lean proteins such as egg whites and white fish; and a final restoration phase (Days 6–7) focused on soluble fibers and probiotics for gastritis relief. By eliminating inflammatory irritants like caffeine, alcohol, and capsaicin, this plan facilitates immediate relief for gastritis and supports long-term stomach lining repair.
The Burning Reality of Gastritis and the Path to Recovery
Living with gastritis is a relentless physical challenge that affects every aspect of your daily existence. It feels like carrying a dormant fire in the pit of your stomach that flares up unpredictably. The gnawing ache in the upper abdomen, the bloating that makes clothes feel tight, and the persistent nausea that ruins your appetite are not just minor inconveniences. For millions of people across the USA, these symptoms disrupt sleep cycles, lower work productivity, and create deep anxiety around the simple act of eating.

You may have already visited a gastroenterologist or spent weeks relying on over-the-counter acid reducers or Proton Pump Inhibitors (PPIs). While medication can effectively lower acid levels, pills alone cannot rebuild damaged tissue. The true path to recovery and permanent stomach lining repair begins in your kitchen.
This comprehensive guide provides a scientifically grounded 7-Day Gastritis Healing Meal Plan for Immediate Relief. We will move far beyond generic “eat bland food” advice. Instead, we will explore the biochemistry of the gastric mucosa, identify specific foods that kill H. pylori, and outline a precise transition from acute pain management to long-term gut health. Whether you are battling a sudden flare-up from NSAID use or managing chronic erosive gastritis, this blueprint offers the strategic tools required to heal your gut from the inside out.
Understanding Gastritis Symptoms and the Mucosal Barrier Defense
To effectively implement a diet for gastritis relief, it is critical to understand the biological battlefield inside your stomach. Your stomach is lined with a specialized layer of cells known as the gastric mucosa. This mucosal barrier is an engineering marvel. It is designed to withstand the highly corrosive environment of hydrochloric acid (pH 1.5 to 3.5) which is necessary for digesting protein and killing pathogens.
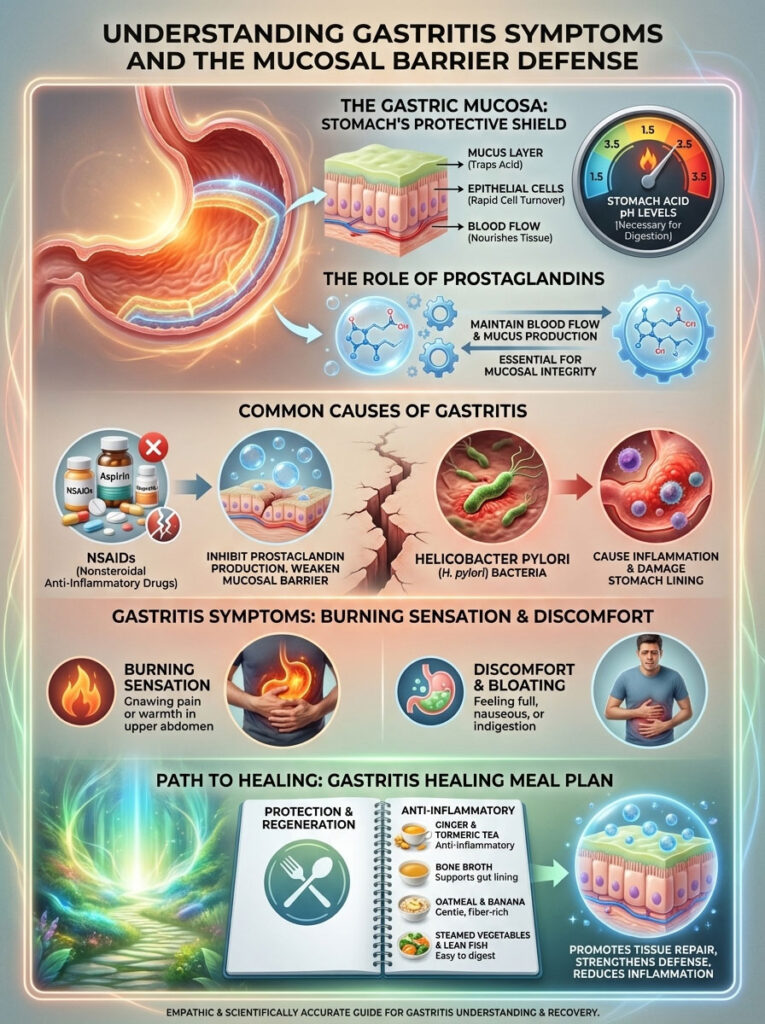
Under normal conditions, this barrier is maintained by prostaglandins. These are lipid compounds that encourage blood flow and mucus production. Gastritis occurs when this protective layer is stripped away or compromised.
Common culprits for this damage include the frequent use of NSAIDs (Non-steroidal anti-inflammatory drugs like ibuprofen, naproxen, or aspirin), which chemically block prostaglandin production. Another major cause is Helicobacter pylori (H. pylori), a spiral-shaped bacterium that burrows into the stomach lining and neutralizes local acid to survive, causing chronic inflammation. According to data from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), H. pylori affects a significant portion of the population and is a leading cause of peptic ulcers.
When the mucus layer is thin, gastric juices begin to digest the stomach wall itself. This results in the burning sensation known as gastritis. Therefore, the goal of a gastritis healing meal plan is not just to neutralize acid. The goal is to physically protect the raw tissue and supply the building blocks for cellular regeneration.
The pH 5.0 Rule for Immediate Gastritis Relief
One of the most effective strategies for stopping pain fast is the “pH 5.0 Rule.”
During an acute gastritis flare-up, your primary nutritional goal is to consume items that have a pH level of 5.0 or higher. This is based on the behavior of pepsin. Pepsin is a powerful digestive enzyme responsible for breaking down proteins. It becomes highly active in acidic environments (pH below 4.0).
If your stomach acid is too high and your protective lining is damaged, pepsin does not distinguish between the steak you ate for dinner and your own stomach cells. It effectively begins to digest the stomach tissue. This causes severe pain and erosion.
By strictly adhering to a low-acid foods list, you raise the gastric pH slightly. This deactivates pepsin and provides the mucosa a safe window to regenerate. This is why highly acidic foods like lemons, cranberries, and vinegar must be strictly avoided during the initial healing phase. Even foods that are traditionally considered “healthy” can be damaging if their pH is too low during an acute flare.
Strategic Phases of the Gastritis Healing Meal Plan Protocol
A successful gastritis healing meal plan is not static. It must evolve as your symptoms improve. Attempting to digest complex fibers or dense proteins on Day 1 will likely result in failure and increased pain. We break this protocol down into three distinct clinical phases to ensure safety and efficacy.

Phase 1: Acute Gastritis Diet Protocol for Immediate Symptom Control (Days 1–2)
Goal: Total symptom suppression, hydration, and “Gastric Rest.”
This phase is critical for stopping the cycle of inflammation. The objective is to minimize the mechanical and chemical work the stomach must perform. We rely on liquid nutrition and very soft textures to ensure the stomach does not have to churn vigorously.
- Key Focus: Hydration, electrolytes, and amino acids.
- Primary Foods: Bone broth, warm alkaline water, aloe vera juice, and herbal teas.
- Why Bone Broth? Homemade chicken bone broth is essential for this phase. It is rich in glutamine and glycine. Glutamine is the primary fuel source for the epithelial cells lining the stomach and small intestine. It directly supports stomach lining repair by tightening the junctions between cells.
- Expert Insight: The American College of Gastroenterology guidelines often suggest avoiding high-fat liquids (like whole milk or cream soups) during this phase because fat delays gastric emptying. This keeps acid in the stomach longer, increasing the chance of irritation.
Phase 2: Transition to Soft Solids and Low-Residue Foods (Days 3–5)
Goal: Reintroducing solids without mechanical abrasion.
Once the constant burning sensation subsides, we introduce soft solids. These foods are classified as “low-residue,” meaning they are almost fully digested and leave very little fibrous material behind to irritate the digestive tract.
- Key Focus: Lean protein synthesis and soft carbohydrates.
- Primary Foods: Mashed sweet potatoes, soft-boiled eggs, steamed white fish, and well-cooked carrots.
- Strategy: This is the core of the stomach-friendly meal plan. We strictly avoid any food with a rough texture, such as raw vegetables, nuts, seeds, or skins of fruits. The texture of your food should be similar to baby food to reduce the need for mechanical churning.
Phase 3: Restoration and Microbiome Support (Days 6–7)
Goal: Strengthening the mucosal lining and preventing recurrence.
In the final days of the week, we introduce specific soluble fibers and probiotics. This is critical for the long-term management of chronic gastritis.
- Key Focus: Microbiome diversity and anti-inflammatory foods for stomach health.
- Primary Foods: Oatmeal (beta-glucan), bananas, lean chicken breast, kefir (if dairy is tolerated), and broccoli sprouts.
- The Fiber Connection: Soluble fiber dissolves in water to form a gel-like substance. This gel coats the stomach lining, acting as a secondary physical barrier against acid while also feeding beneficial gut bacteria.
Critical Gastritis Diet Food List and Trigger Avoidance
Navigating the grocery store is difficult when you are in pain and unsure what is safe. The following categorization serves as your definitive guide for a diet for gastritis relief.

| Category | Foods to Embrace (Healing) | Foods to Avoid (Triggers) |
| Proteins | Chicken breast, turkey, egg whites, white fish (cod, tilapia), tofu | Red meat (beef, lamb), sausages, bacon, fried chicken, fatty cuts |
| Grains | White rice, oatmeal, sourdough bread, gluten-free pasta | Whole wheat (coarse fiber), granola with nuts, pastries, croissants |
| Vegetables | Carrots, zucchini, pumpkin, green beans, potatoes, sweet potato | Raw onions, garlic, tomatoes, chili peppers, raw broccoli, cauliflower |
| Fruits | Bananas, melons (cantaloupe, honeydew), papaya, cooked apples | Citrus fruits (lemons, oranges, grapefruits), tart berries, pineapple |
| Beverages | Alkaline water, herbal tea (chamomile, fennel), bone broth | Coffee (caffeine & decaf), alcohol, soda, energy drinks, peppermint tea |
| Dairy | Low-fat yogurt, kefir, almond milk, oat milk, hemp milk | Whole milk, heavy cream, spicy cheeses, chocolate milk |
| Condiments | Manuka honey, olive oil (small amounts), dried oregano, thyme | Black pepper, chili flakes, BBQ sauce, vinegar, mustard, ketchup |
Deep Dive Analysis of Triggers:
You will notice that tomatoes and onions are strictly placed on the “Avoid” list. Although generally considered healthy, tomatoes are highly acidic due to citric and malic acid content. Onions contain fructans, a type of carbohydrate that can cause significant bloating and gas. When the stomach is inflamed, gas pressure stretches the stomach wall. This leads to acute pain. For a successful gastritis healing meal plan, these must be eliminated entirely during the healing phase. Additionally, peppermint tea, often used for nausea, relaxes the lower esophageal sphincter and can actually worsen reflux-related gastritis symptoms.
The Complete 7-Day Gastritis Healing Meal Plan Menu
This section outlines your daily nutritional blueprint. It serves as your definitive gastritis diet food list and menu. The portion sizes should be kept small to prevent gastric distension. Aim for 5 to 6 small meals per day rather than 3 large ones. Do not skip meals. An empty stomach accumulates acid which can damage the lining just as much as bad food.
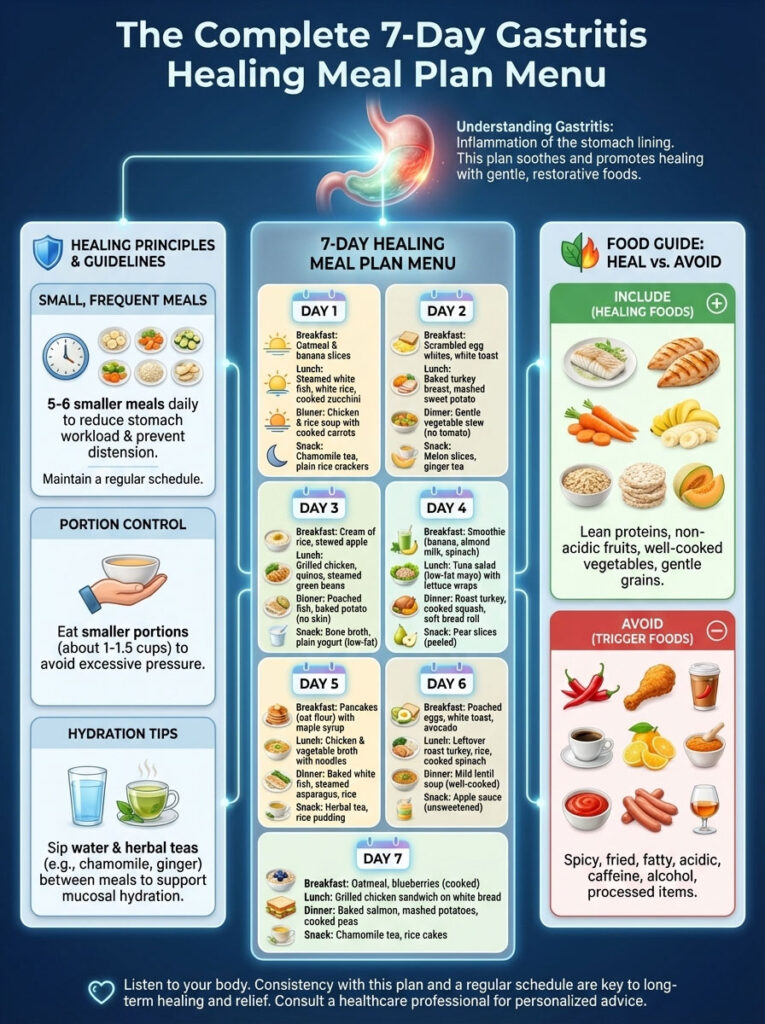
Days 1 & 2 Menu for Soothing the Fire
The priority here is immediate relief for gastritis. If you feel sharp pain after eating any item, stop immediately and revert to room-temperature water or herbal tea.
- Breakfast: Warm oatmeal gruel.
- Preparation: Use rolled oats cooked with water until they break down completely into a smooth porridge. Strain if necessary to remove husks. Add a tiny pinch of mineral salt. Do not add sugar or heavy milk.
- Morning Snack: Chamomile tea with a teaspoon of Manuka honey.
- Instance: Look for Manuka honey with a UMF rating of 10+ or MGO 263+. Clinical studies indicate its potent antibacterial properties help fight H. pylori without the side effects of antibiotics. It acts as a natural wound dressing for the stomach.
- Lunch: 1 cup of homemade Chicken Bone Broth.
- Nutrients: High bio-availability of collagen and gelatin helps coat the raw stomach lining. Ensure the fat is skimmed off the top, as fat slows digestion.
- Afternoon Snack: 4 ounces of unsweetened Aloe Vera juice.
- Note: Ensure you buy “inner leaf” juice or gel. The outer leaf contains latex (aloin), which is a strong laxative and can cause cramping.
- Dinner: Pureed zucchini and potato soup.
- Recipe: Peel potatoes and zucchini. Boil until soft. Blend with a drizzle of olive oil. No dairy. No black pepper. This provides potassium and easy-to-digest carbohydrates.
Days 3 & 4 Menu for Gentle Reintroduction
As inflammation decreases, we introduce more low-acid foods and solid proteins to prevent muscle loss and stabilize blood sugar.
- Breakfast: Scrambled egg whites with spinach.
- Tip: Steam the spinach until very soft before adding to the eggs. Egg yolks are high in fat and sulfur, which may trigger some sensitive individuals; whites are generally safer.
- Morning Snack: A ripe banana.
- Why: Bananas have a natural antacid effect and contain pectin, a gentle soluble fiber that aids digestion. Ensure the banana is ripe (yellow/brown spots) rather than green, as green bananas are harder to digest.
- Lunch: Baked Cod or Tilapia with white rice.
- Fish Choice: White fish is significantly lower in fat than salmon or mackerel. Since fat slows digestion, we stick to lean options during the healing window. Season with a little salt and dried parsley.
- Afternoon Snack: Rice cakes with a thin layer of almond butter.
- Texture check: Ensure the almond butter is smooth and creamy. Avoid crunchy varieties. Nuts are high in fat, so keep this layer thin.
- Dinner: Slow-cooked shredded chicken breast with mashed pumpkin.
- Flavoring: Season with dried oregano or thyme. Avoid chili powder, garlic powder, or onion powder. Pumpkin is soothing and lower in fiber than some other squashes.
Days 5, 6, & 7 Menu for Nutritional Restoration
This phase solidifies your gastritis healing meal plan and prepares you for a long-term maintenance diet.
- Breakfast: Healing Stomach Smoothie.
- Ingredients: Unsweetened almond milk, half a papaya, and a scoop of unflavored pea protein.
- Enzymatic Support: Papaya contains papain, a proteolytic enzyme that helps break down proteins. This reduces the workload on your stomach acid.
- Morning Snack: Baked apple with cinnamon.
- Note: You must peel the apple. Cooking breaks down the insoluble fiber, making it a perfect addition to a stomach-friendly meal plan. Cinnamon is anti-inflammatory but use it sparingly.
- Lunch: Turkey wrap.
- Components: Gluten-free tortilla (rice-based), sliced turkey breast (low sodium/nitrate-free), avocado, and peeled cucumber.
- Why Turkey: Turkey contains tryptophan, which can help with sleep and relaxation, further aiding the gut-brain axis.
- Afternoon Snack: Low-fat yogurt or Kefir.
- Probiotic Boost: Introduce beneficial bacteria to crowd out H. pylori. If you are dairy-intolerant, use coconut kefir or water kefir.
- Dinner: Grilled tofu with steamed green beans and sweet potato.
- Preparation: Press the tofu to remove excess water. Grill lightly using olive oil spray. Avoid soy sauce; use coconut aminos instead for lower acidity.
Deep Dive into Superfoods for Stomach Lining Repair and H. Pylori Eradication
To achieve true stomach lining repair, we can utilize specific functional foods that act almost like medicine. These foods go beyond basic caloric nutrition to influence the biological pathways of inflammation.
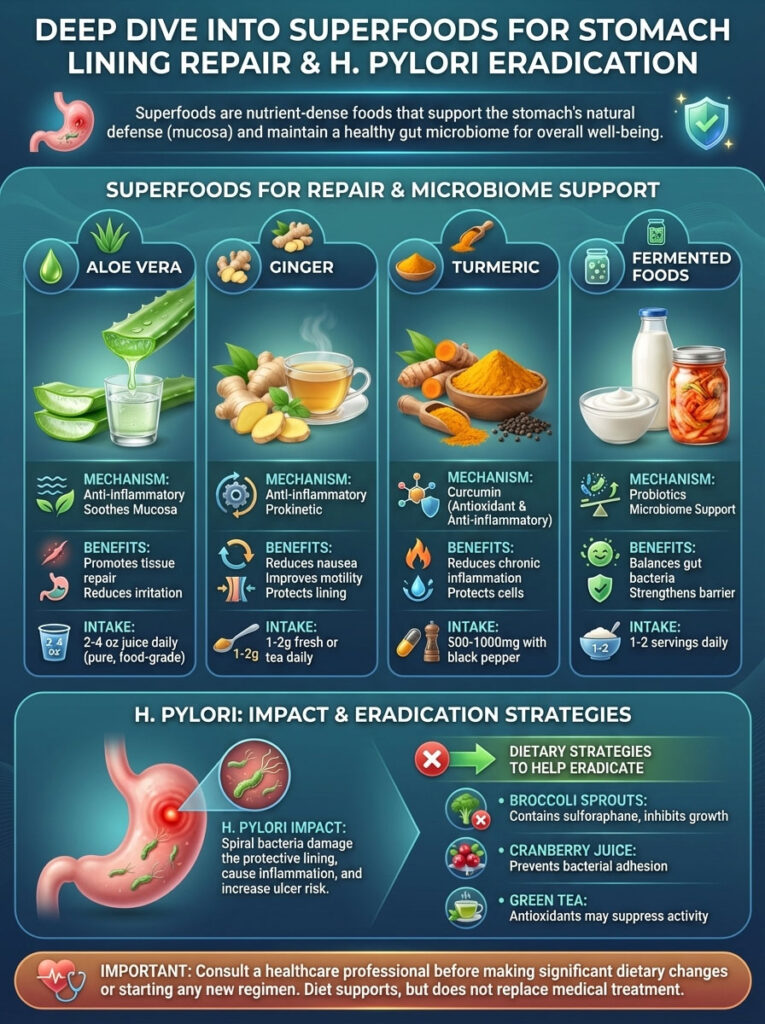
Utilizing Sulforaphane Rich Foods to Fight H. Pylori Naturally
If your gastritis is caused by an H. pylori infection, broccoli sprouts are a powerhouse tool you must include. They contain exceptionally high levels of a compound called sulforaphane.
Research published in various nutritional journals suggests that sulforaphane can inhibit the colonization of H. pylori in the gastric mucosa. It works by inducing cytoprotective enzymes that defend cells against oxidative damage. While mature broccoli contains some sulforaphane, 3-day-old broccoli sprouts can contain 10 to 100 times more.
- How to eat: Broccoli sprouts are best eaten fresh. However, for a sensitive stomach, lightly steaming them reduces the risk of gas while preserving the active compounds. Chewing them thoroughly is essential to activate the sulforaphane.
Probiotics for Gastritis Relief and Microbiome Balance
Restoring the balance of bacteria in your stomach is vital. Probiotics for gastritis relief usually focus on Lactobacillus and Bifidobacterium strains. These beneficial bacteria produce short-chain fatty acids that help lower inflammation in the gut lining.
- Strategy: Fermented foods are often superior to pills because they buffer the bacteria through the digestive tract.
- Recommendation: Start with small amounts (1-2 tablespoons) of non-dairy kefir or coconut yogurt. If you tolerate this well, gradually increase the serving size.
Functional Supplements and Mucilaginous Herbs
While food is the foundation, two specific supplements have shown strong clinical promise for gastritis recovery guide protocols:
- Zinc Carnosine: This is a chelated form of zinc that literally adheres to the stomach wall. It promotes wound healing and helps repair the tight junctions between stomach cells. It is one of the few supplements approved in Japan specifically for the treatment of ulcers.
- Slippery Elm & Marshmallow Root: These are known as mucilaginous herbs. When the powder from these roots is mixed with water, it forms a thick, slippery gel. When ingested, this gel coats the throat and stomach. It acts as a physical bandage (demulcent) against acid.
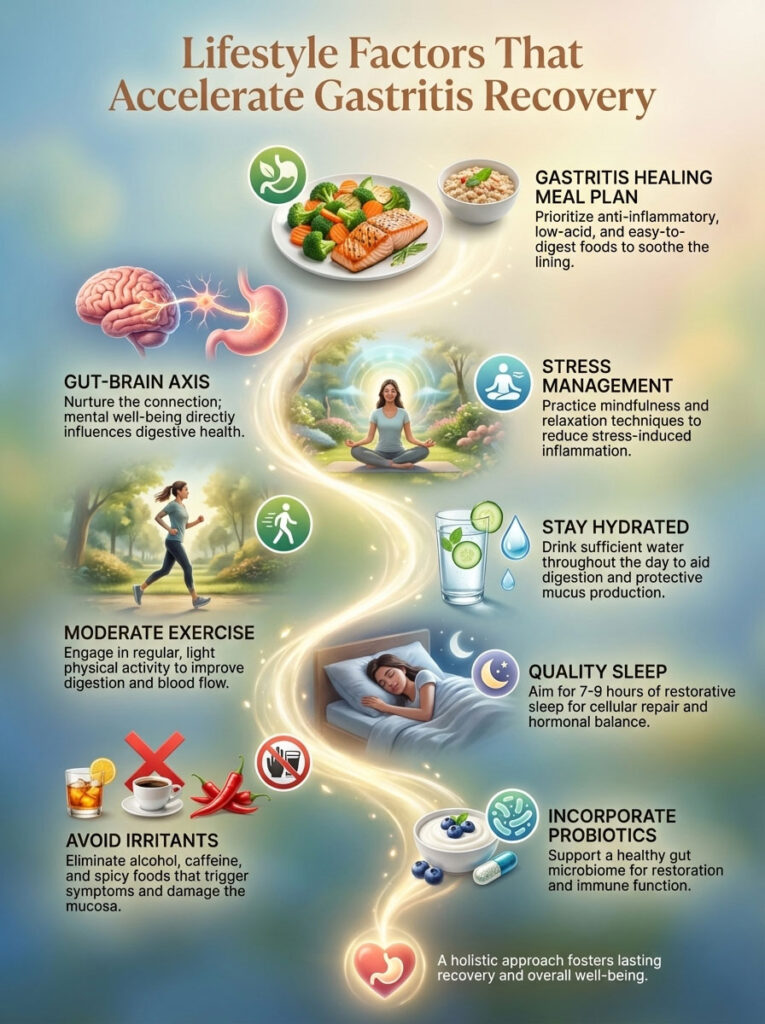
Lifestyle Factors That Accelerate Gastritis Recovery
A gastritis healing meal plan works best when paired with lifestyle changes. The “gut-brain axis” connects your nervous system directly to your stomach via the Vagus nerve. Ignoring this connection can slow down your healing significantly.
The Art of Mastication and Digestive Enzyme Activation
Digestion begins in the mouth, not the stomach. Saliva contains amylase and is naturally alkaline.
- Tip: You should chew your food until it is essentially liquid (approx. 20–30 times per bite). This serves two purposes. First, it mixes the food with alkaline saliva, pre-buffering it before it hits the stomach acid. Second, it reduces the mechanical particle size of the food. If you swallow large chunks, your stomach must produce more acid and churn harder to break them down, aggravating the inflammation.
Managing Stress Gastritis and the Vagus Nerve Connection
Stress is a direct physiological trigger for gastritis. When you are stressed, the body releases cortisol and activates the sympathetic nervous system (the “fight or flight” response). This diverts blood flow away from the digestive tract and towards the muscles. Without adequate blood flow, the stomach lining cannot repair itself efficiently.
- Technique: Practice diaphragmatic breathing (deep belly breathing) for one minute before every meal. This activates the vagus nerve and switches the body into the parasympathetic nervous system (“rest and digest”). This optimizes blood flow to the stomach for stomach lining repair.
Optimal Meal Timing and Frequency for Acid Control
The traditional “Three Square Meals” model is outdated for gastritis sufferers. Large meals distend the stomach, which stimulates the parietal cells to produce a surge of acid.
- Strategy: Eat 5–6 small meals spaced 3 hours apart. This keeps a small amount of food in the stomach to buffer acid without stretching the stomach wall.
- Crucial Rule: Do not eat within 3 hours of bedtime. Lying down with food in the stomach allows acid to pool against the upper stomach and esophagus. Gravity is your friend; keep your torso upright while digesting to prevent nocturnal symptoms.
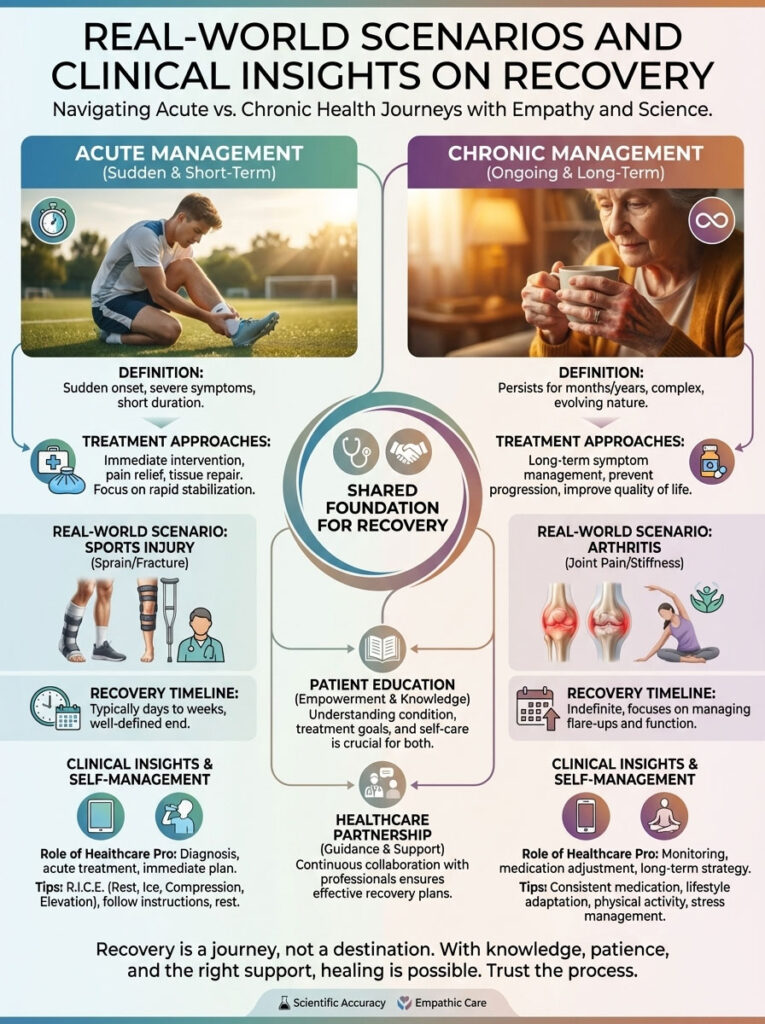
Real-World Scenarios and Clinical Insights on Recovery
To understand how this applies to real life, let’s look at specific scenarios and how to differentiate between acute and chronic management.
Case Study of NSAID-Induced Gastritis Recovery
Consider a scenario involving a patient recovering from knee surgery. Due to high doses of ibuprofen (NSAIDs), they develop acute erosive gastritis.
- The Problem: The medication inhibited prostaglandins, the chemicals that maintain the protective mucus layer.
- The Intervention: Immediate cessation of NSAIDs (under doctor supervision) and adoption of Phase 1 of the gastritis healing meal plan.
- The Result: By utilizing bone broth and removing coffee, the patient reported a 50% reduction in burning pain within 48 hours. Full tolerance of solid foods returned by Day 7.
Comparison of Acute vs Chronic Gastritis Dietary Approaches
It is vital to distinguish between a short-term flare and a long-term condition. The following comparison highlights how your approach should differ based on the duration of your symptoms.
| Feature | Acute Gastritis Diet | Chronic Gastritis Diet |
| Duration | Short-term (2–7 days) | Long-term lifestyle change (Months/Years) |
| Texture Focus | Liquid to mushy/soft solids | Varied textures, focus on thorough chewing |
| Fiber Intake | Very low (to reduce mechanical irritation) | High soluble fiber (to feed good bacteria) |
| Variety | Limited variety (safe foods only) | High variety (to prevent nutrient deficiencies) |
| Supplementation | Usually not recommended immediately | Targeted supplements (B12, Iron) often needed |
Data Point: Patients with chronic gastritis often suffer from malabsorption, specifically of Vitamin B12 and Iron. This is because damaged stomach cells produce less “Intrinsic Factor,” a protein needed to absorb B12. Long-term dietary planning must account for these micronutrients, potentially requiring sublingual B12 supplements.
Summary and Key Takeaways for Long-Term Health
Healing the stomach lining is a biological process that takes time, but relief can be achieved quickly with the right strategy.

- Immediate Relief: Focus on the “pH 5.0 Rule” and stick to the Phase 1 liquid/soft diet for the first 48 hours to allow for “Gastric Rest.”
- Consistency is Key: A single cup of coffee or a spicy taco can undo days of progress. Adhere strictly to the gastritis diet food list until you are symptom-free for at least two weeks.
- Holistic Approach: Combine your stomach-friendly meal plan with stress management and proper chewing to treat the root cause, not just the symptoms.
Your stomach is resilient. With the removal of irritants and the addition of healing nutrients like glutamine and sulforaphane, you create the perfect environment for stomach lining repair. Start Day 1 today.
Frequently Asked Questions (FAQ)
How fast can a gastritis meal plan provide relief?
A strict protocol can provide significant symptom reduction within 24 to 48 hours. This is primarily achieved by removing irritants (coffee, alcohol, spice) and switching to liquid or soft nutrition, which allows the “gastric rest” necessary for the inflammation to subside. However, full healing of the mucosa may take several weeks.
Is fasting good for gastritis?
Intermittent fasting or “gastric rest” can be beneficial for short periods (12–16 hours) to allow the stomach to empty. However, prolonged fasting (24+ hours) may backfire for some because an empty stomach still produces acid. Without food to buffer this acid, it can irritate the lining further. Small, frequent meals are generally safer for most people.
Can I drink milk to soothe heartburn?
It is a common myth that milk cures gastritis. While the calcium temporarily neutralizes acid, milk proteins (casein) and calcium can actually stimulate the stomach to produce more acid later, leading to a “rebound” effect. Plant-based milks like almond or oat milk are safer alternatives for a gastritis healing meal plan.
What is the best breakfast for gastritis?
The best breakfast is warm oatmeal made with water, topped with sliced banana. This provides soluble fiber which coats the stomach lining without being abrasive. Egg whites are also an excellent high-protein option that is easy to digest. Avoid bacon, sausages, or hash browns.
Does stress cause gastritis or just make it worse?
Both are true. “Stress gastritis” is a real physiological condition where severe physiological stress (like trauma, surgery, or burns) causes gastric erosion. However, everyday psychological stress exacerbates existing gastritis by increasing acid secretion and slowing down digestion via the gut-brain axis.
Are potatoes good for gastritis?
Yes, potatoes are excellent low-acid foods, provided they are prepared correctly. Boiled, baked, or mashed potatoes are soothing and easy to digest. However, fried potatoes (french fries) or potato chips are high in fat and sharp edges, making them major triggers.
How do I know if my gastritis is healing?
Signs of healing include a reduction in the burning sensation (heartburn), less bloating after meals, and the return of a normal appetite. You may also notice you can sleep through the night without waking up in pain. As healing progresses, you will be able to tolerate a wider variety of foods.
Can I eat bread on a gastritis diet?
Yes, but the type matters significantly. During a flare-up, white bread or genuine sourdough is often better tolerated than whole wheat bread. The coarse insoluble fiber in whole wheat can mechanically irritate an inflamed stomach lining. Toasting the bread makes it easier to digest.
Is apple cider vinegar safe for gastritis?
Generally, no. While popular for digestion issues like low acid, adding acetic acid (vinegar) to an already inflamed and acidic environment usually causes more pain. It is safer to stick to alkaline or neutral beverages until the mucosa is fully healed.
What sweets can I eat with gastritis?
Sugary treats should be limited, but you can enjoy Manuka honey, maple syrup (in moderation), and non-acidic fruits like melons and papaya. Avoid chocolate, as it relaxes the esophageal sphincter and contains caffeine, both of which can worsen symptoms.
Do I need to take probiotics?
Probiotics are highly recommended, especially if your gastritis is linked to H. pylori. Strains like Lactobacillus help balance the gut microbiome. However, start slowly. Introducing high doses too quickly can cause gas and bloating, which can mimic gastritis pain.
Can H. pylori be cured by diet alone?
Diet plays a massive role in suppressing bacterial growth and managing symptoms, but it rarely eradicates an established H. pylori infection on its own. Medical treatment (usually a combination of antibiotics and acid suppressors) prescribed by a doctor is typically required for a cure, supported by a H. pylori diet protocol.
Disclaimer: The information provided in this article is for educational purposes only and does not constitute medical advice. Gastritis can mimic other serious conditions such as ulcers or gallbladder disease. Always consult with a gastroenterologist or healthcare provider for proper diagnosis and treatment plans tailored to your specific medical history.
References:
- American College of Gastroenterology. (Guidelines on Dyspepsia and H. pylori).
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (Gastritis).
- Journal of Clinical Biochemistry and Nutrition. (Effects of Sulforaphane on Gastric Mucosa).
- University of Maryland Medical Center (Gastritis and Peptic Ulcer Disease).








