Your liver is the only organ in your body capable of regenerating itself completely. This biological superpower is your greatest asset when living with the Hepatitis B virus (HBV). While antiviral medications play a critical role in suppressing the viral load, the food you eat determines the environment in which your liver fights and heals. Nutrition is not just fuel; it is a therapeutic tool that can either accelerate recovery or contribute to inflammation. When you control what goes on your plate, you directly influence the longevity and vitality of your liver.
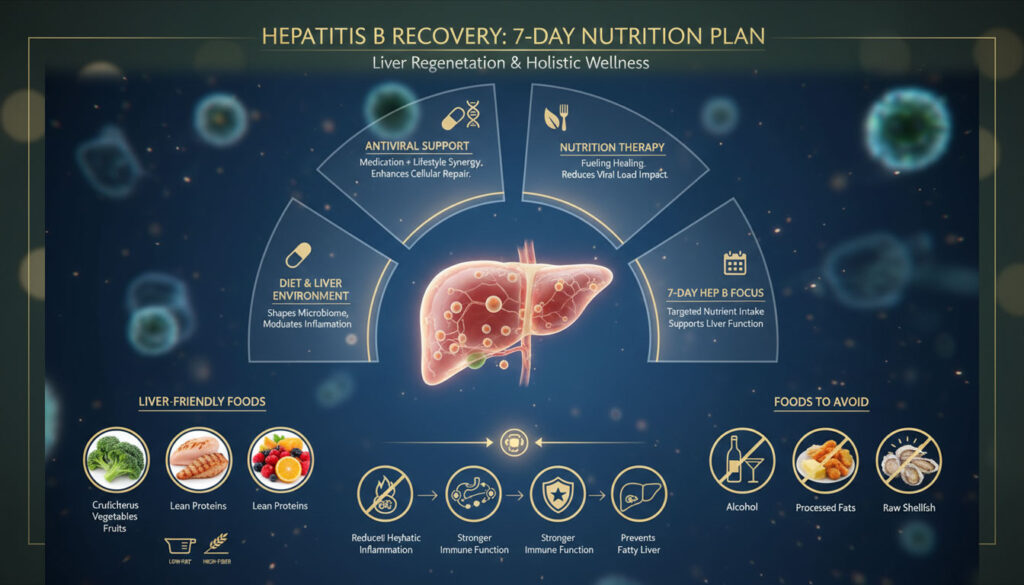
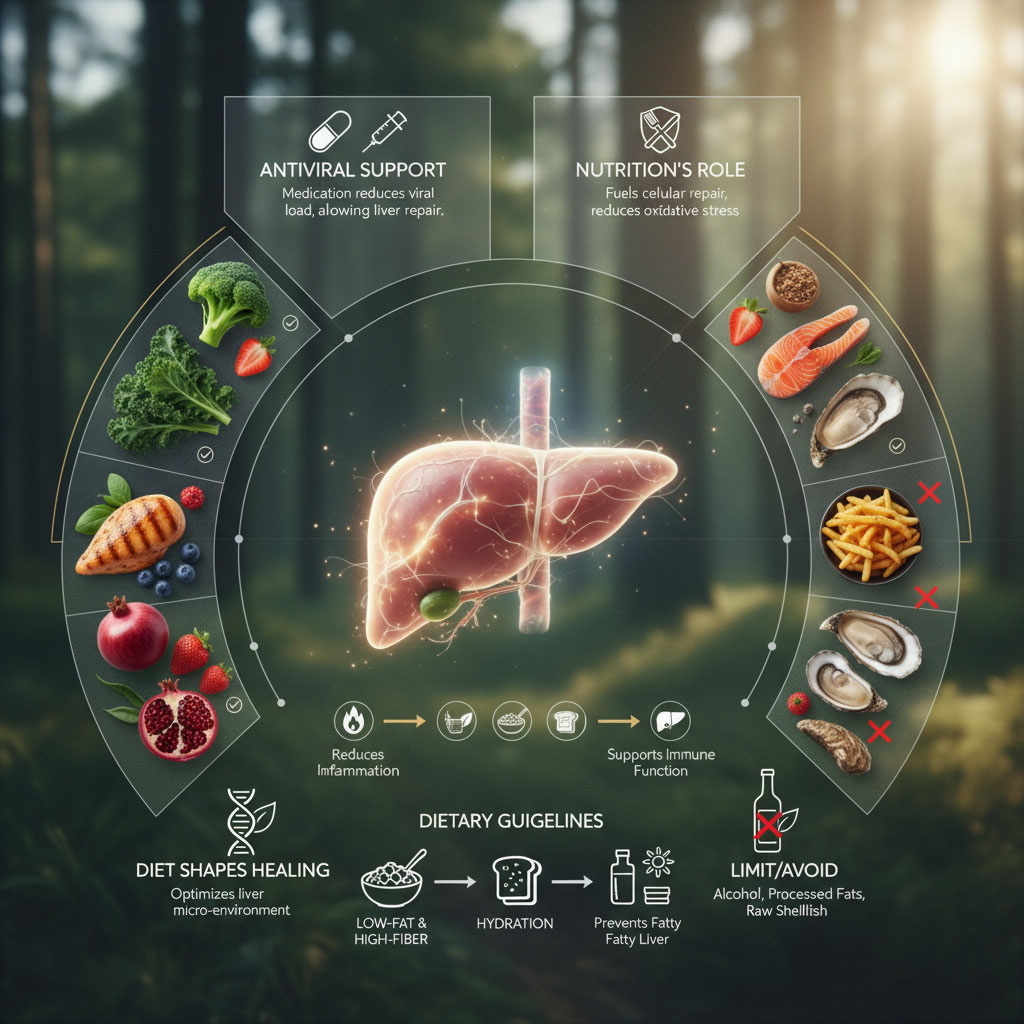
A structured 7-day meal plan for Hepatitis B focuses on reducing hepatic inflammation and preventing metabolic complications like fatty liver disease. The primary goal of these Hepatitis B diet guidelines is to maintain a healthy weight and support immune function. This involves prioritizing liver-friendly foods such as cruciferous vegetables, lean proteins, and high-antioxidant fruits while strictly eliminating alcohol, processed fats, and raw shellfish. By adopting a low-fat, high-fiber diet, patients can significantly reduce the metabolic workload on the liver and support long-term health.
The Biological Basis of the Hepatitis B Diet
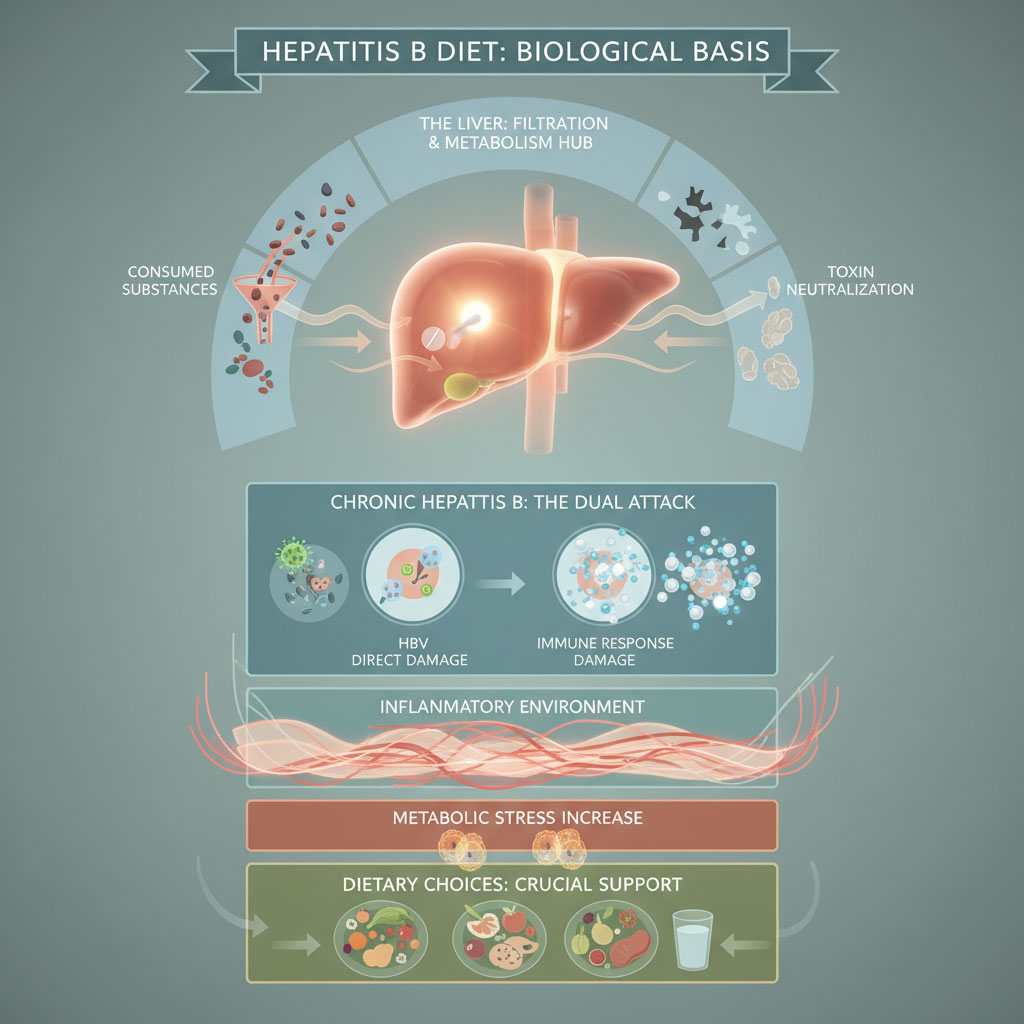
To understand why specific dietary choices matter, we must first look at what happens inside the liver during a chronic infection. The liver acts as the body’s primary filtration system. It processes everything you consume, metabolizes drugs, and neutralizes toxins. When infected with Hepatitis B virus (HBV), the liver cells, known as hepatocytes, are under constant attack. This attack comes not just from the virus itself, but from the immune system trying to eliminate the virus. This battleground creates inflammation.
Reducing Metabolic Stress and Inflammation
The cornerstone of nutritional therapy for chronic hepatitis is reducing metabolic stress. Every time you eat, your liver must process nutrients, filter out byproducts, and regulate blood sugar. When you consume foods high in saturated fats or refined sugars, the liver must work harder to process them. This extra workload can lead to oxidative stress and inflammation. Over time, chronic inflammation triggers the activation of stellate cells, which produce collagen scar tissue. This process leads to fibrosis. A healthy diet for liver health aims to minimize this stress by providing nutrients that require less effort to metabolize, essentially giving your liver a “break” so it can focus on repair rather than processing heavy fats and toxins.
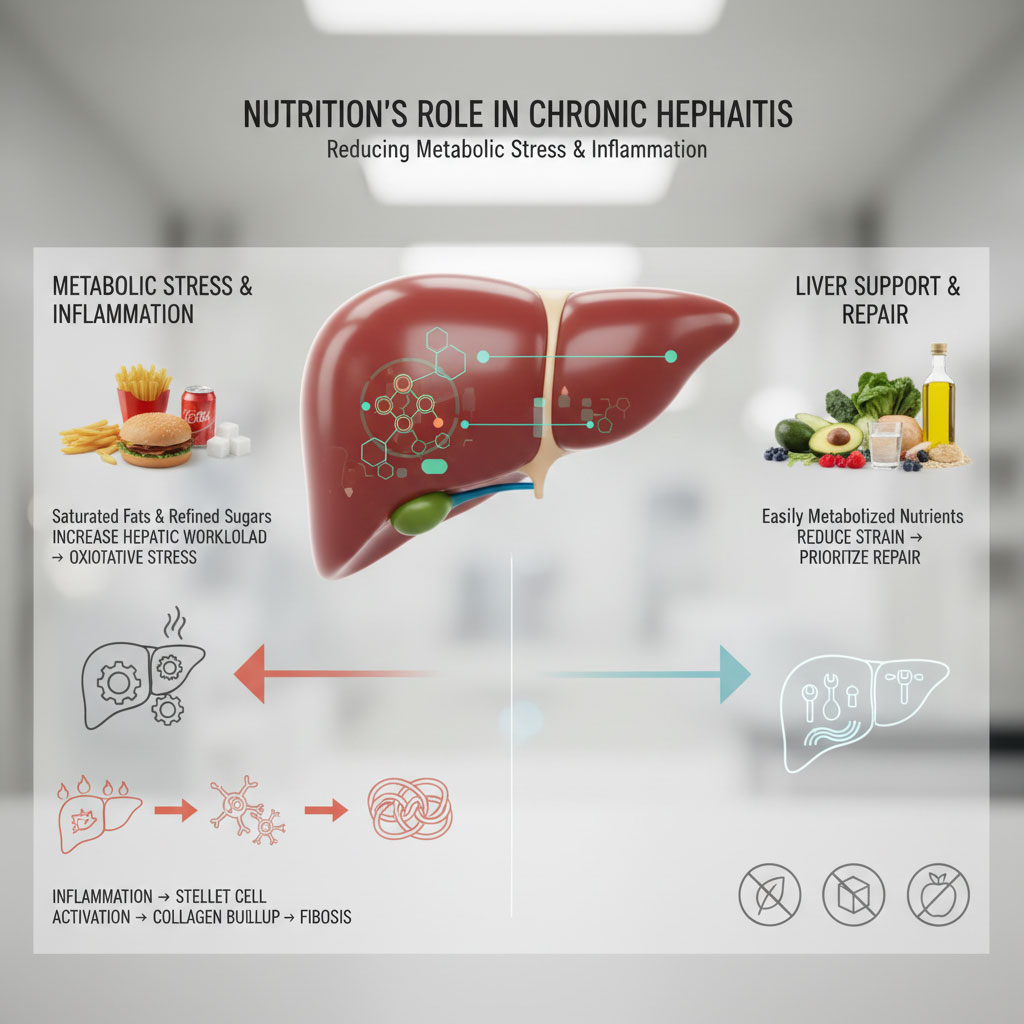
The Connection to Fatty Liver Disease
In the United States, a significant concern for HBV patients is the co-occurrence of Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), formerly known as fatty liver. The Standard American Diet is often high in calories and low in nutrients, leading to fat accumulation in liver cells. This fat buildup is dangerous because it acts as a “second hit” to the liver. A liver that is already fighting a viral infection cannot afford the additional burden of fat toxicity. Fat accumulation accelerates liver damage caused by the virus and increases the risk of cirrhosis. Therefore, a Hepatitis B nutrition plan must be calorie-conscious and nutrient-dense to prevent steatosis (fatty liver).

The Gut-Liver Axis
Emerging science highlights the critical importance of the gut-liver axis. The blood leaving your digestive system goes directly to the liver through the portal vein. If your gut is unhealthy or “leaky” due to a poor diet, bacterial toxins can translocate directly to the liver, triggering massive inflammation. A diet high in fiber and probiotics supports a healthy gut barrier, which acts as the first line of defense for your liver.
Foods to Include: Building Your Liver Defense System
Building a resilient liver requires specific raw materials. By stocking your kitchen with liver-supportive nutrients, you provide your body with the tools it needs to repair cell damage and regulate enzymes like ALT and AST.
Antioxidant Powerhouses
Oxidative stress is a major driver of liver damage. To combat this, you need foods rich in antioxidants for hepatitis. These compounds neutralize free radicals that damage liver cells.

- Vitamin E: This is a potent antioxidant that protects cell membranes from damage. It has been shown in clinical settings to improve liver histology in patients with fatty liver. Sources include sunflower seeds, almonds, spinach, and avocados.
- Selenium: This trace mineral is vital for the production of glutathione peroxidase, an enzyme that protects the liver from oxidative damage. Studies have linked low selenium levels to an increased risk of liver cancer. Brazil nuts are the richest natural source; just one or two nuts can meet your daily requirement.
- Berries: Blueberries, strawberries, and raspberries contain anthocyanins and polyphenols that have been shown to slow down the development of lesions and fibrosis in animal studies. They are also low in sugar compared to tropical fruits.
Safe Protein Sources
Protein is essential for repairing tissue and preventing muscle wasting (sarcopenia), which is a risk in advanced liver disease. However, the liver must process the byproducts of protein digestion, specifically ammonia. Therefore, choosing safe protein sources is crucial.
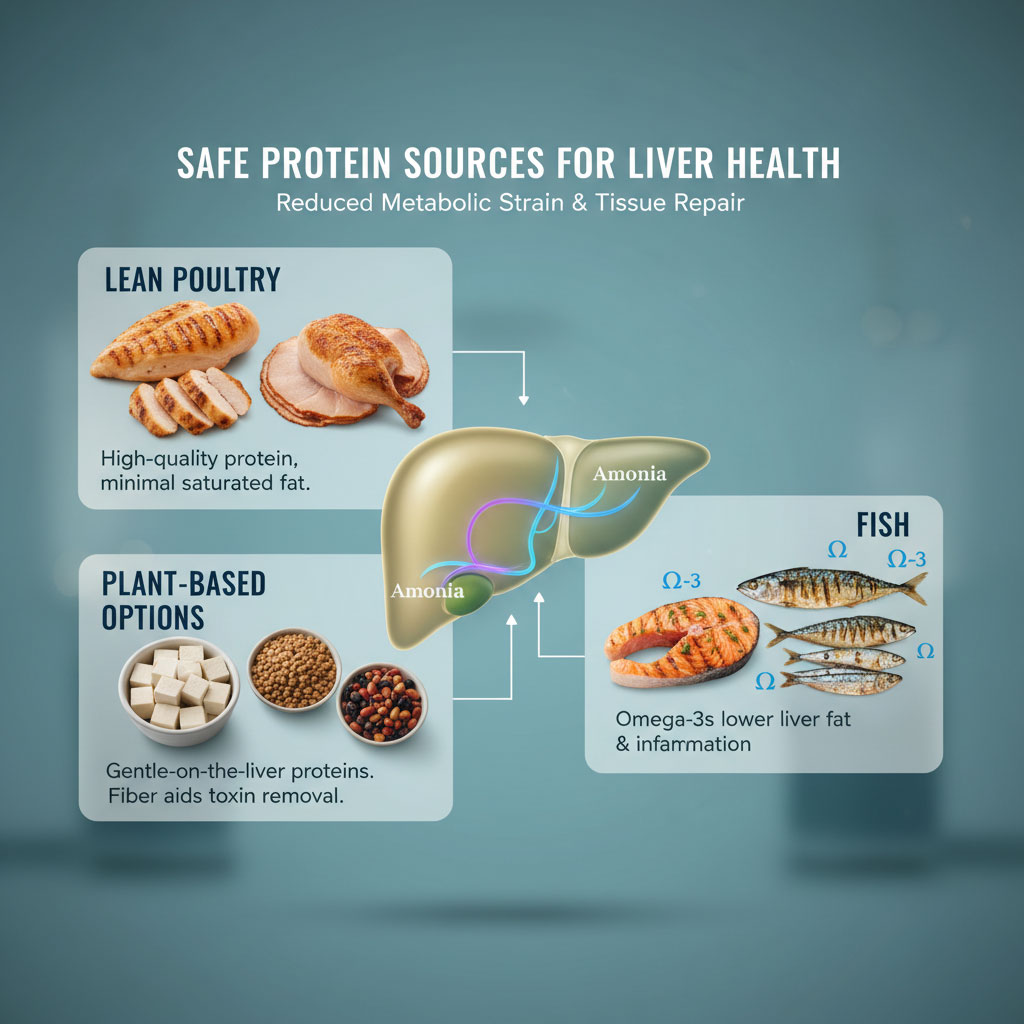
- Lean Poultry: Skinless chicken and turkey provide high-quality protein without the saturated fat found in red meat.
- Plant-Based Options: Tofu, lentils, and beans are excellent choices. They are less taxing on the liver and provide fiber that helps flush out toxins. Plant proteins also have a better profile of amino acids for those with liver concerns.
- Fish: Fatty fish like salmon, mackerel, and sardines are rich in Omega-3 fatty acids. These healthy fats help reduce liver fat levels and systemic inflammation.
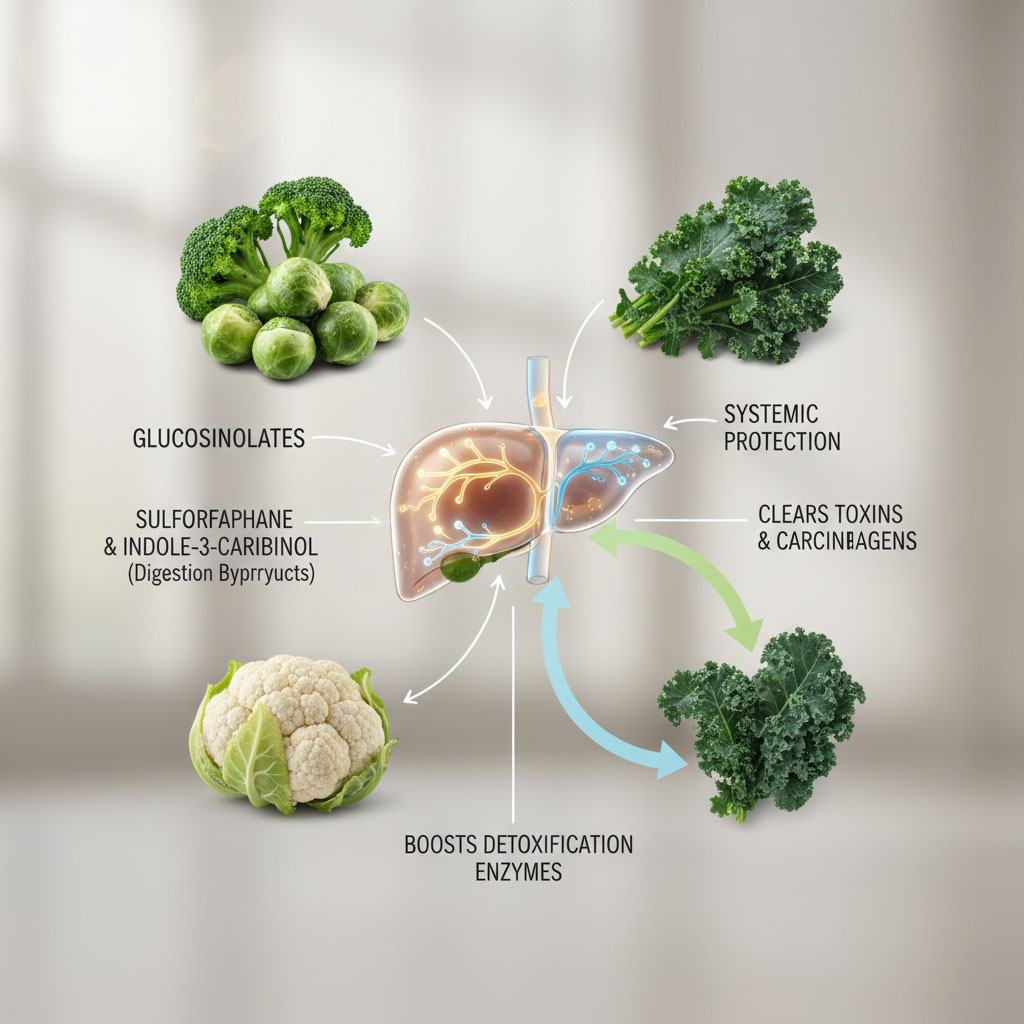
Cruciferous Vegetables and Detox Enzymes
Vegetables like broccoli, Brussels sprouts, cauliflower, and kale are non-negotiable in a liver-healthy diet. They contain compounds called glucosinolates. When digested, these break down into substances like sulforaphane and indole-3-carbinol. These compounds boost the liver’s natural detoxification enzymes (Phase II detoxification), helping the organ clear toxins and carcinogens from the blood more efficiently. Including these liver-friendly foods daily supports the organ’s ability to perform its vital functions.
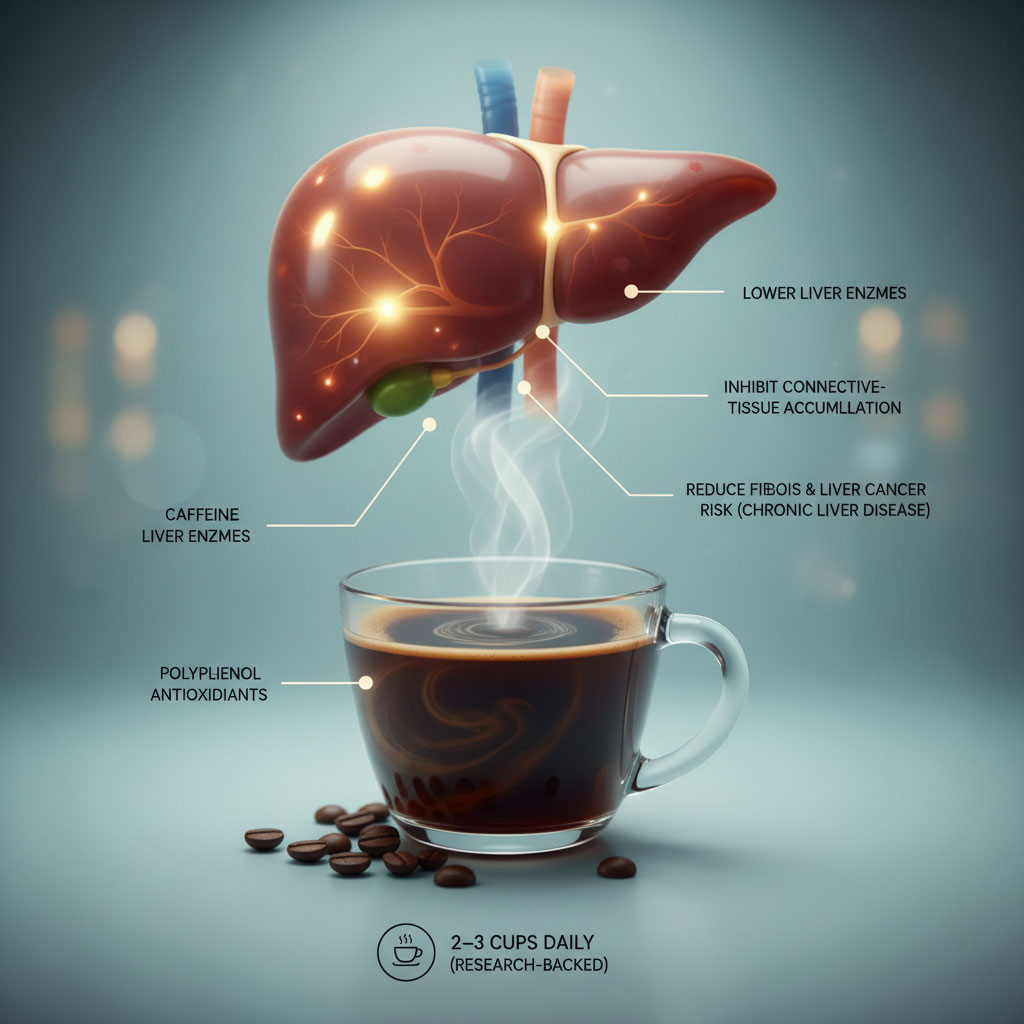
The Role of Coffee
One of the most surprising but well-supported facts in hepatology is the benefit of coffee. Multiple large-scale studies indicate that drinking black coffee can reduce the risk of liver scarring and even liver cancer in patients with chronic liver disease. The caffeine and specific polyphenol antioxidants in coffee help lower liver enzymes and prevent the accumulation of connective tissue. Aiming for 2 to 3 cups of regular, black coffee daily can be a powerful therapeutic addition to your routine.
The Danger Zone: Foods to Avoid with Hepatitis B
Knowing what not to eat is just as important as knowing what to eat. Certain foods and substances act as direct toxins to hepatocytes or increase the viral replication environment. These are the foods to avoid with Hepatitis B to prevent unnecessary damage.
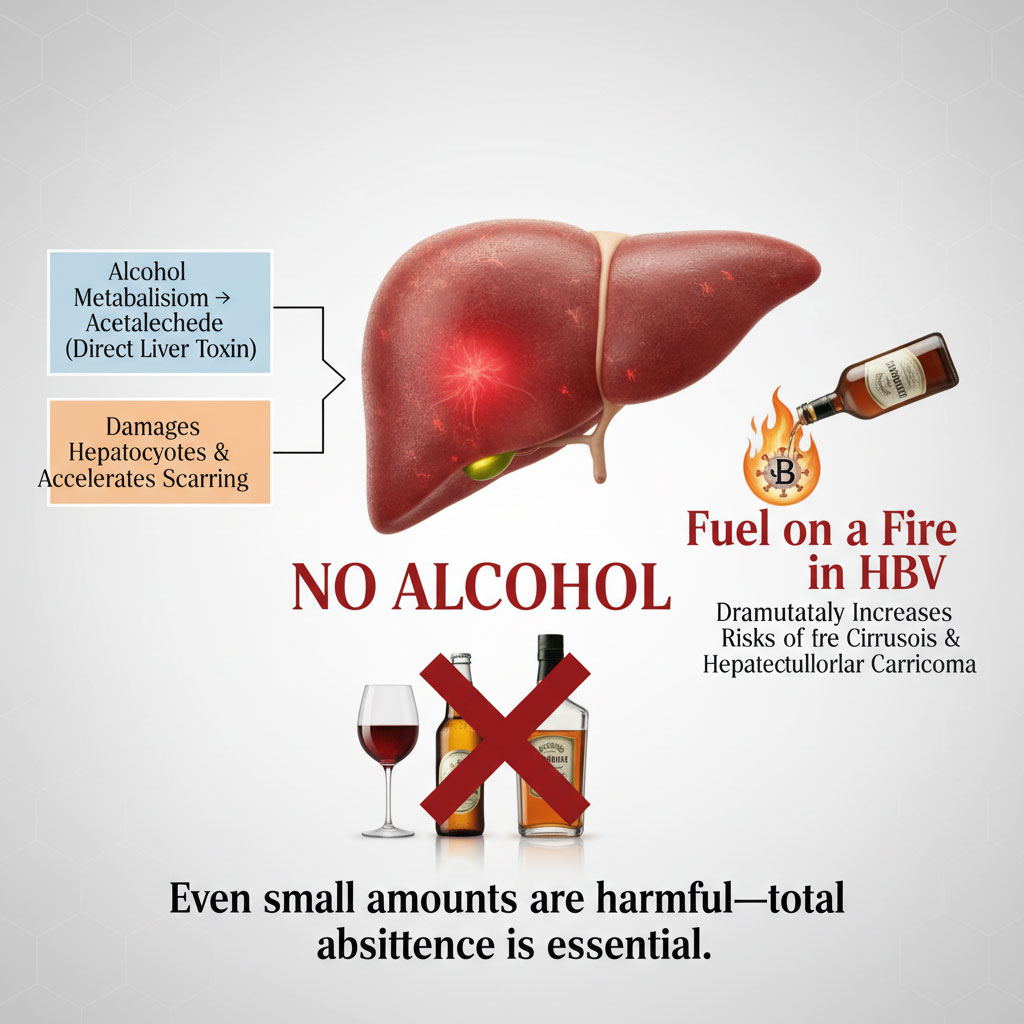
Alcohol: The Non-Negotiable Exclusion
Alcohol is a direct liver toxin. When the liver processes alcohol, it produces acetaldehyde, a substance that damages liver cells and promotes scarring. For someone with Hepatitis B virus (HBV), drinking alcohol is like pouring gasoline on a fire. It dramatically increases the risk of cirrhosis and hepatocellular carcinoma (liver cancer). Even small amounts can be harmful because the liver is already compromised. Total abstinence is the only safe recommendation for preserving liver health.
The Risk of Aflatoxins
Aflatoxins are toxins produced by a fungus that can grow on crops like corn, peanuts, and grains if they are stored in warm, humid conditions. The liver is responsible for breaking down these toxins. However, aflatoxins are potent carcinogens. In people with HBV, exposure to aflatoxins significantly multiplies the risk of liver cancer. To avoid this, always buy high-quality, commercial-grade nuts and grains from reputable brands. Discard any food that shows signs of mold, moisture, or discoloration.

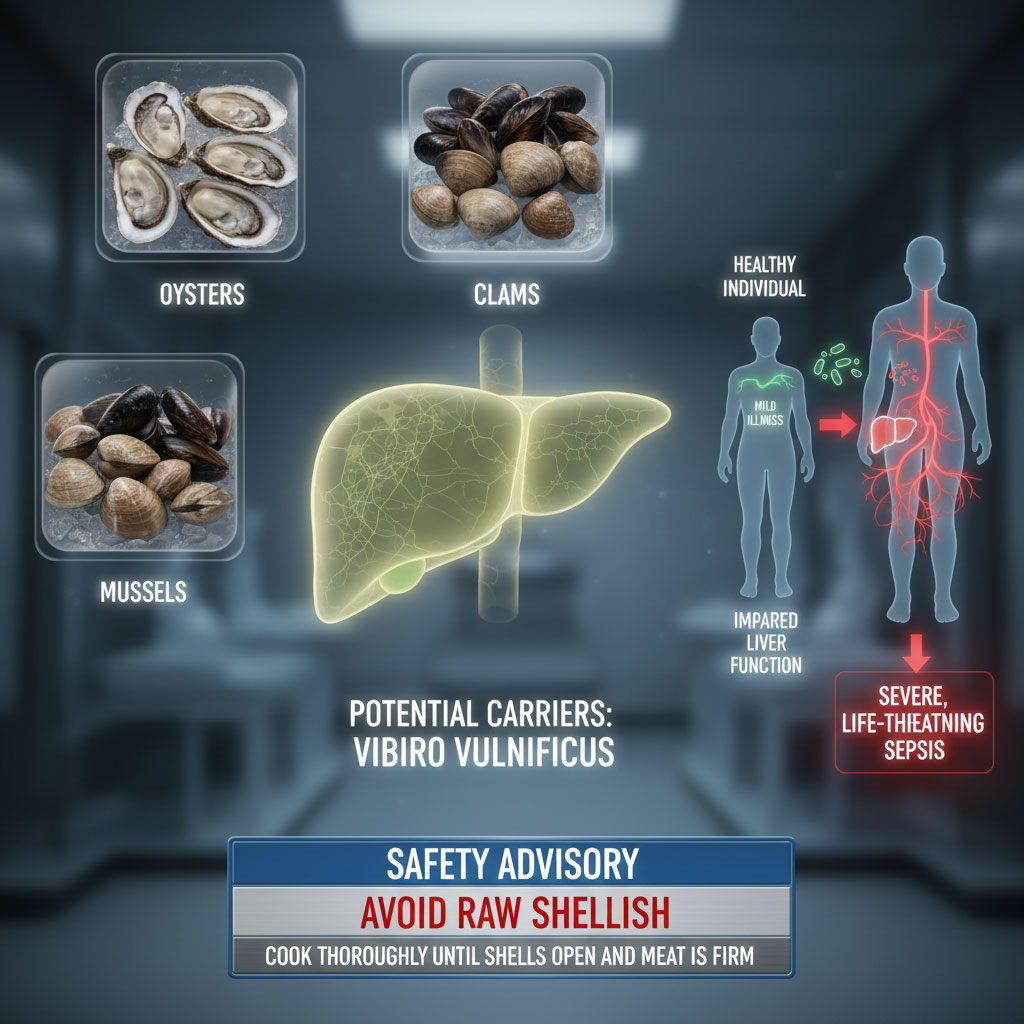
Raw Shellfish and Bacterial Risks
Patients with liver disease must be extremely cautious with raw seafood. Oysters, clams, and mussels can carry a bacteria called Vibrio vulnificus. In a healthy person, this might cause a mild stomach upset. In a person with compromised liver function, the liver cannot effectively filter this bacteria from the blood, leading to a severe, life-threatening infection called sepsis. Always ensure shellfish is cooked thoroughly until the shells open and the meat is firm.
Processed Foods and Hidden Sodium
High sodium intake can lead to fluid retention, a condition known as ascites in advanced liver disease. Processed foods like canned soups, deli meats, frozen dinners, and salty snacks are major culprits. Furthermore, these foods are often high in trans fats and preservatives that increase liver stress. A healthy diet for liver health relies on fresh, whole ingredients. Reading labels is essential; aim for less than 2,000 mg of sodium per day, or less if advised by your physician.

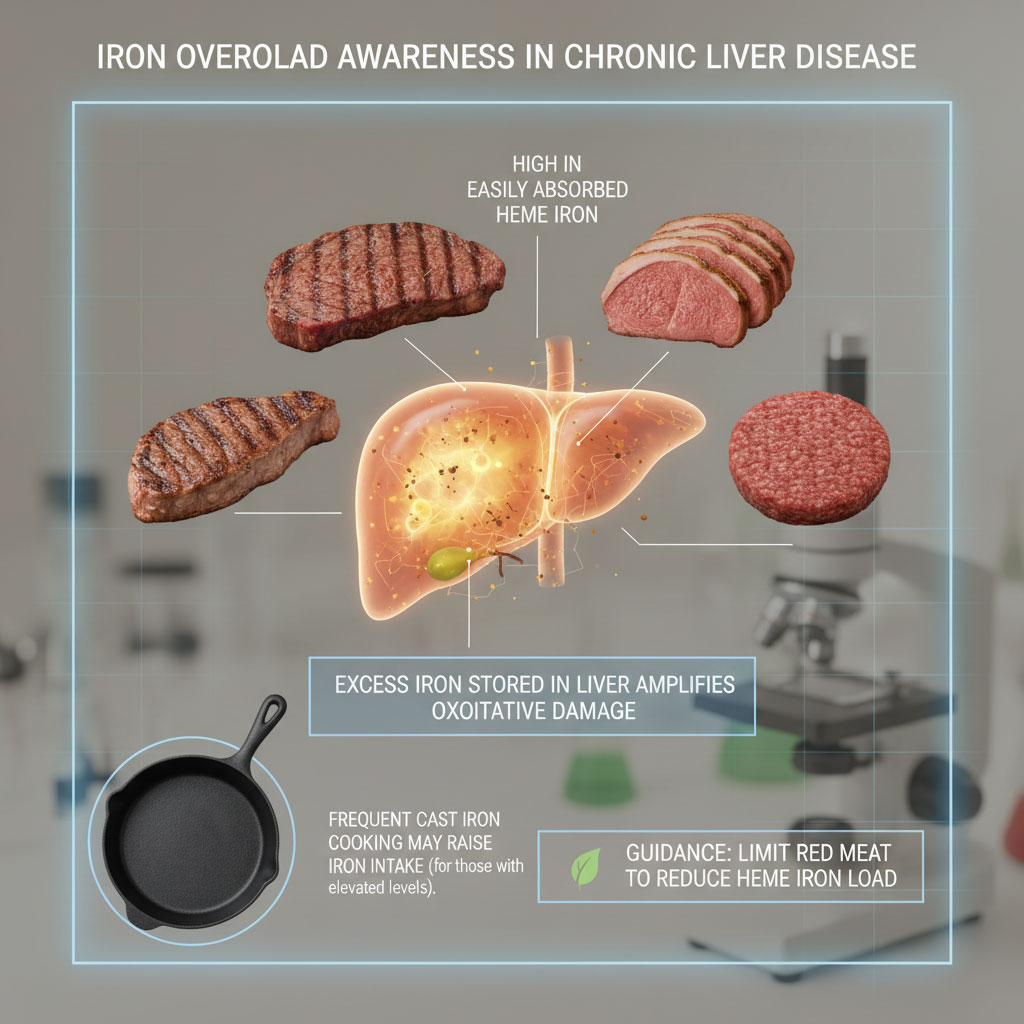
Iron Overload Awareness
While iron is necessary for blood health, excess iron is stored in the liver. In chronic liver disease, iron can accumulate and cause further oxidative damage. Red meat is very high in heme iron, which is easily absorbed. Limiting red meat consumption helps prevent this iron overload. Additionally, avoid cooking in cast iron skillets for every meal if your iron levels are already high.
Liver-Friendly Swap List
Making dietary changes can be challenging. The table below provides practical alternatives to common foods that may stress the liver.
| Food Category | ❌ AVOID (Liver Stressors) | ✅ INCLUDE (Liver Healers) | Why? (Mechanism) |
| Proteins | Red meat, processed deli meats, bacon, pepperoni | Skinless chicken breast, tofu, lentils, white fish (cod, tilapia) | Red meat increases ammonia levels; processed meats contain nitrates and high sodium. |
| Grains | White bread, sugary cereals, pastries, white pasta | Steel-cut oats, quinoa, brown rice, barley | Whole grains provide sustained energy and fiber; refined grains spike insulin and liver fat. |
| Fats | Margarine, soybean oil, deep-fried foods, lard | Extra virgin olive oil, avocado oil, walnuts, flaxseeds | Omega-3s and monounsaturated fats reduce inflammation; trans fats increase liver inflammation. |
| Snacks | Potato chips, candy bars, salted pretzels | Unsalted almonds, fresh berries, Greek yogurt, apple slices | High sodium causes fluid retention; antioxidants in fruit help repair cell damage. |
| Beverages | Soda, energy drinks, alcohol, sweetened teas | Black coffee, green tea, water with lemon, herbal infusions | High fructose corn syrup drives fatty liver; coffee polyphenols protect liver cells. |
The Ultimate 7-Day Meal Plan for Hepatitis B
This 7-day meal plan for Hepatitis B is designed to be practical, delicious, and liver-protective. It follows a low-fat, high-fiber diet structure and incorporates key liver-supportive nutrients. Remember to stay hydrated by drinking water throughout the day to assist the kidneys in flushing out toxins processed by the liver.
Day 1: The Anti-Inflammatory Start

- Nutritional Goal: Kickstart the week with high antioxidant intake to reduce weekend inflammation.
- Breakfast: Steel-cut oatmeal prepared with water or unsweetened almond milk. Stir in a tablespoon of ground flaxseeds (for fiber) and top with a cup of fresh blueberries. Serve with black coffee.
- Lunch: Grilled chicken breast salad featuring mixed dark leafy greens (spinach, arugula), cucumber, cherry tomatoes, and radishes. Dress with extra virgin olive oil and fresh lemon juice.
- Snack: A medium apple sliced and served with a few walnuts. Walnuts are the top nut for liver health due to their high Omega-3 and antioxidant content.
- Dinner: Baked salmon seasoned with turmeric and black pepper. The piperine in pepper increases the absorption of curcumin from the turmeric. Serve with a side of steamed broccoli and a half-cup of quinoa.
Day 2: Plant-Based Power
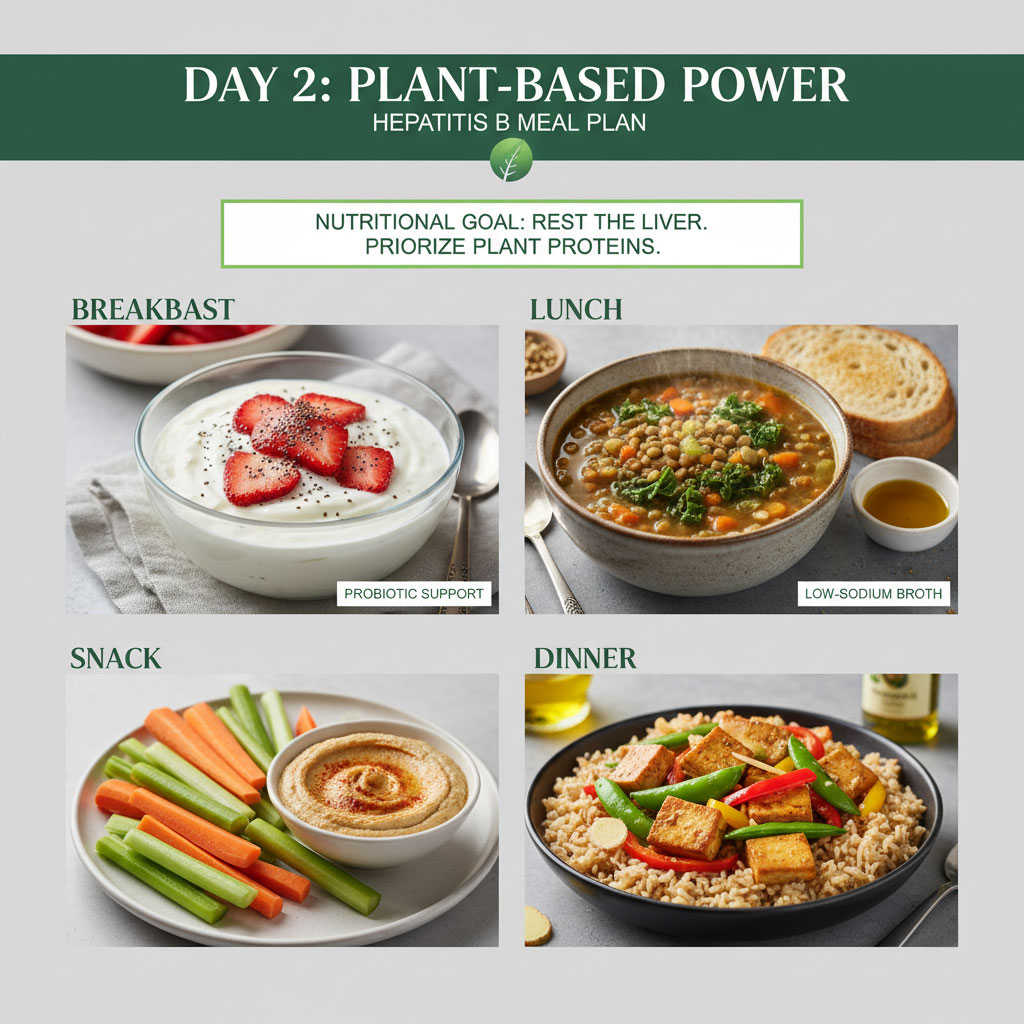
- Nutritional Goal: Give the liver a rest from metabolizing animal proteins by focusing on plant sources.
- Breakfast: Low-fat Greek yogurt mixed with chia seeds and sliced strawberries. Greek yogurt provides probiotics for gut health.
- Lunch: Hearty lentil vegetable soup. Use low-sodium vegetable broth and load it with carrots, celery, and kale. Pair with a slice of whole-grain bread dipped in olive oil.
- Snack: Carrot sticks and celery with hummus.
- Dinner: Tofu stir-fry. Cube firm tofu and sauté in a small amount of avocado oil with bell peppers, snap peas, and fresh ginger. Ginger is excellent for digestion and reducing inflammation. Serve over brown rice.
Day 3: High-Fiber Focus
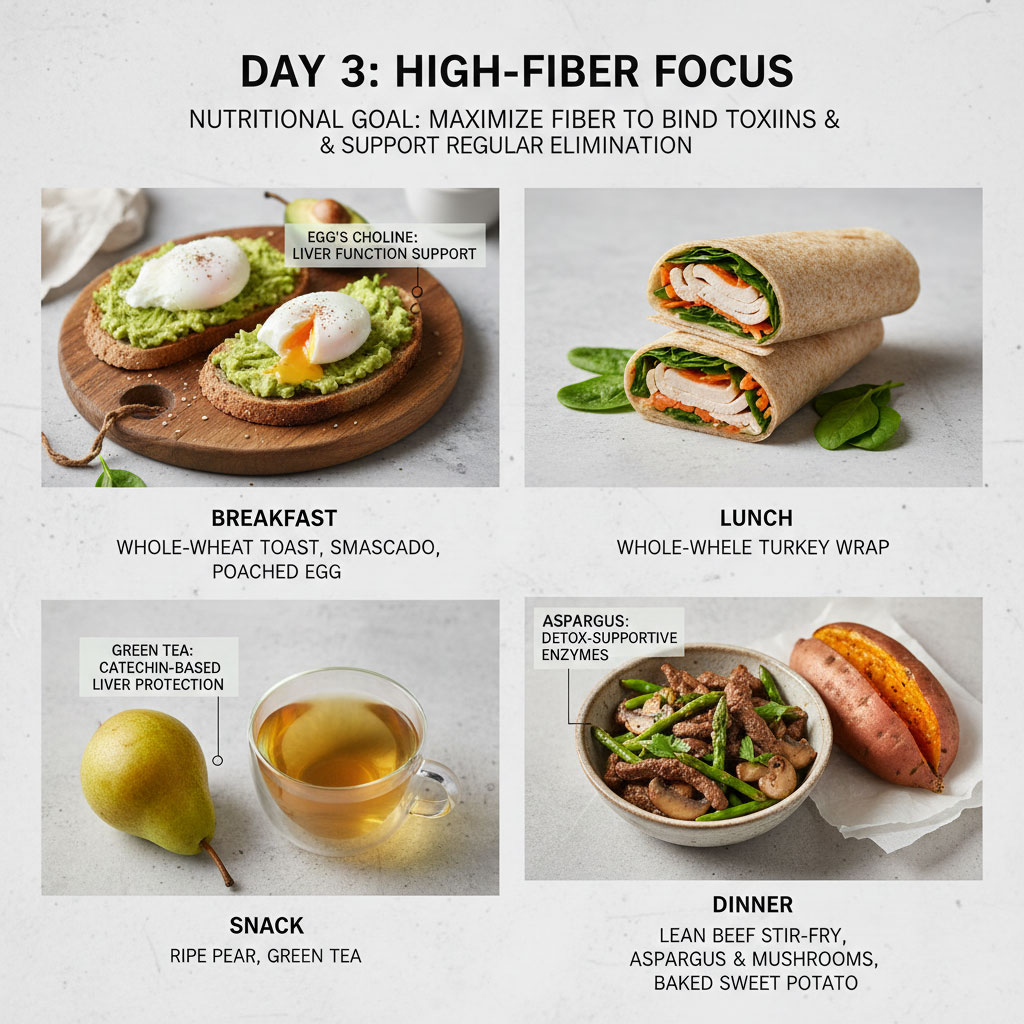
- Nutritional Goal: Maximize fiber intake to bind to toxins in the gut and promote regular elimination.
- Breakfast: Two slices of whole-wheat toast topped with smashed avocado and a poached egg. The egg provides choline, which is essential for liver function.
- Lunch: Turkey wrap using a whole-wheat tortilla. Fill with lean turkey breast (fresh roasted, not deli meat), spinach, and shredded carrots.
- Snack: A ripe pear and a cup of green tea. Green tea contains catechins which are highly protective of liver cells.
- Dinner: Lean beef loin (limited portion, approx 3-4 oz) stir-fried with asparagus and mushrooms. Asparagus has been shown to boost alcohol dehydrogenase enzymes (though you aren’t drinking, these enzymes help detoxify other compounds). Serve with a baked sweet potato.
Day 4: Detox and Repair

- Nutritional Goal: Focus on sulfur-rich foods to boost glutathione production.
- Breakfast: Green smoothie made with spinach, half a banana, protein powder (whey isolate or pea protein), and water. Add a squeeze of lemon.
- Lunch: Quinoa bowl mixed with black beans, corn, cilantro, and a lime vinaigrette. This provides a complete protein profile from plant sources.
- Snack: A handful of unsalted almonds. Almonds are high in Vitamin E.
- Dinner: Baked cod with roasted Brussels sprouts and wild rice. Cod is a very lean protein source, easy for the liver to break down.
Day 5: Antioxidant Boost
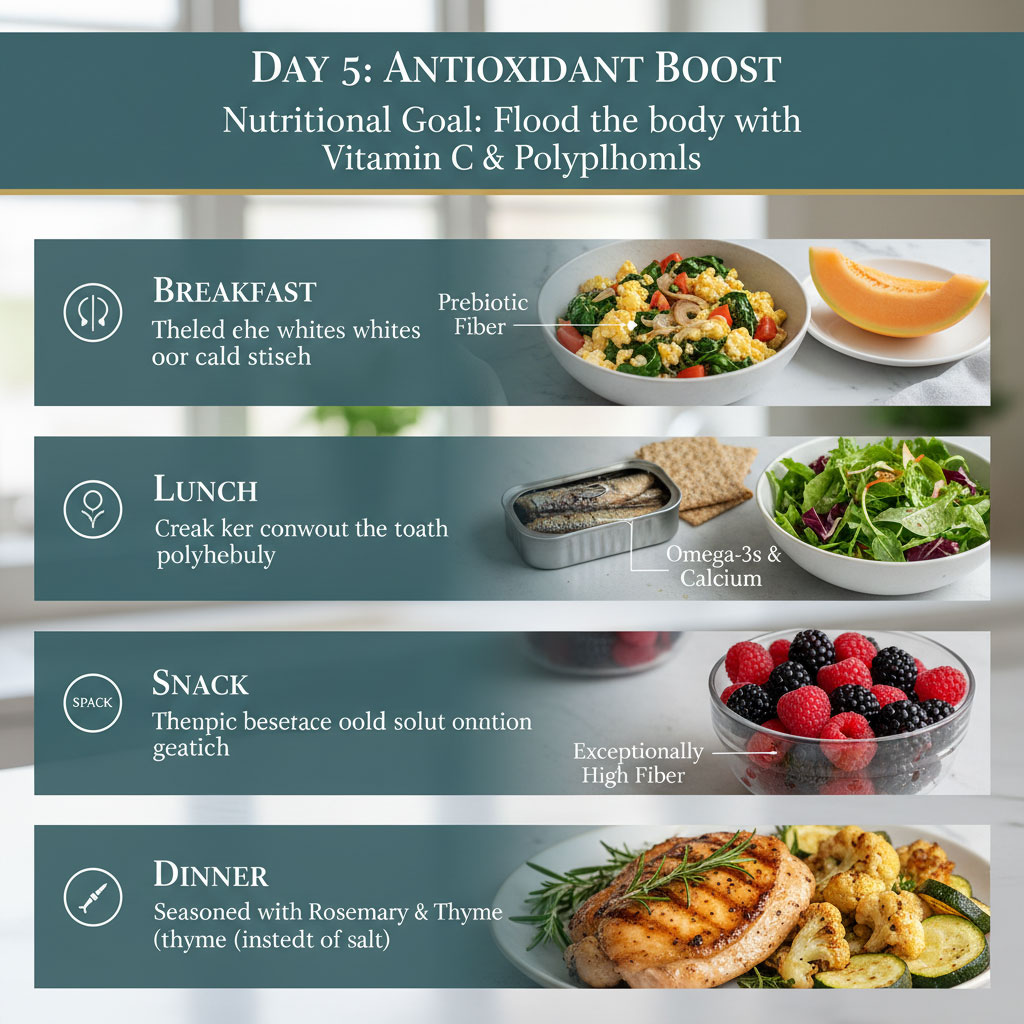
- Nutritional Goal: Flood the body with Vitamin C and polyphenols.
- Breakfast: Scrambled egg whites with spinach, tomatoes, and onions. Onions provide prebiotic fiber. Serve with a slice of cantaloupe melon.
- Lunch: Canned sardines (packed in water, drained) or tuna on whole-grain crackers. Serve with a side salad of mixed greens. Sardines are a powerhouse of nutrients including calcium and Omega-3s.
- Snack: Fresh raspberries or blackberries. These have the highest fiber content of most fruits.
- Dinner: Grilled chicken thigh (skinless) with roasted cauliflower and zucchini. Season with herbs like rosemary and thyme instead of salt.
Day 6: Light and Nutrient Dense

- Nutritional Goal: Keep meals light to prevent lethargy and support energy levels for the weekend.
- Breakfast: Overnight oats prepared the night before. Mix rolled oats, almond milk, chia seeds, and diced apple. The oats soften overnight, making them easy to digest.
- Lunch: Grilled vegetable sandwich. Use slices of eggplant, zucchini, and red pepper. Grill them and place on whole-grain bread with a thin spread of goat cheese or hummus.
- Snack: Low-fat cottage cheese with fresh pineapple chunks. Pineapple contains bromelain, an enzyme that aids digestion.
- Dinner: Shrimp stir-fry. Ensure shrimp are cooked thoroughly until pink and firm. Toss with bok choy and snap peas over soba (buckwheat) noodles.
Day 7: The Reset
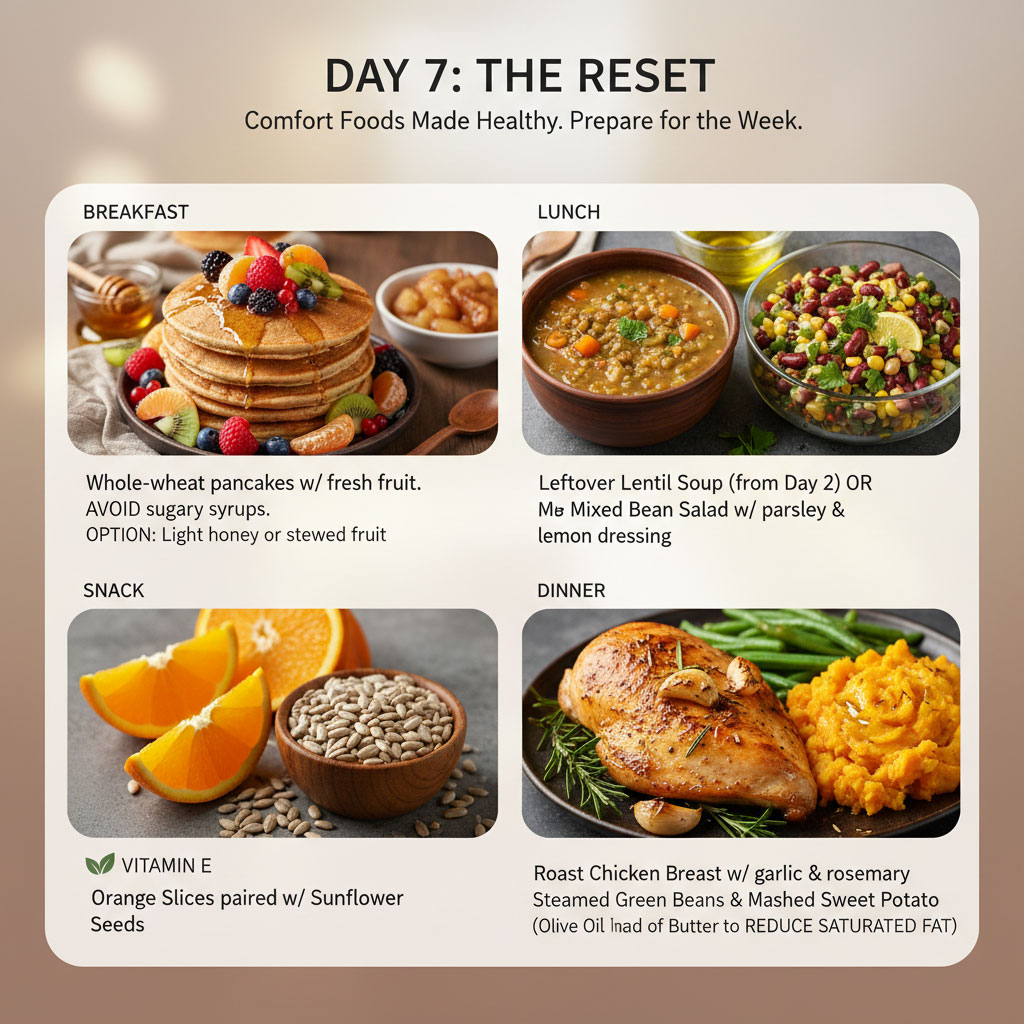
- Nutritional Goal: Prepare for the week ahead with comfort foods made healthy.
- Breakfast: Whole-wheat pancakes topped with fresh fruit. Avoid sugary syrups; use a small amount of honey or stewed fruit if needed.
- Lunch: Leftover lentil soup from Day 2 or a large mixed bean salad with plenty of parsley and a lemon dressing.
- Snack: Orange slices and sunflower seeds. Sunflower seeds are excellent for Vitamin E.
- Dinner: Roast chicken breast with cloves of garlic and sprigs of rosemary. Serve with steamed green beans and mashed sweet potato (mash with olive oil instead of butter to reduce saturated fat).
Mastering the Hepatitis B Kitchen: Prep and Cooking Techniques
Having a plan is only the first step; how you prepare these foods is just as critical as the ingredients themselves. The method of cooking can either preserve the liver-supportive nutrients or destroy them. Furthermore, because fatigue is a common symptom of Hepatitis B virus (HBV), learning to cook efficiently is essential for maintaining this diet long-term without exhaustion.
Liver-Safe Cooking Methods
To maximize the benefits of your Hepatitis B nutrition plan, avoiding added fats and charring is crucial. High-heat cooking methods like frying can create advanced glycation end products (AGEs), which promote inflammation.

- Steaming and Poaching: These are the gold standards for liver health. Steaming vegetables like broccoli and Brussels sprouts preserves the water-soluble vitamins and enzymes that aid detoxification. Poaching fish or chicken in water or broth ensures the protein remains moist without the need for added oils or butter.
- Baking and Roasting: These methods develop flavor through caramelization without submersion in fat. However, use parchment paper on your baking sheets to minimize the need for oil. When roasting nuts or seeds (like selenium-rich Brazil nuts), keep temperatures low to protect their delicate healthy fats from oxidizing.
- Avoid Deep Frying: Submerging food in hot oil creates trans fats and aldehydes, which directly increase inflammation and liver stress. If you crave a crispy texture, use an air fryer with a light mist of olive oil. This mimics the texture of fried food with a fraction of the fat.
Flavoring Without Sodium
Sodium causes fluid retention, which stresses the liver and kidneys. In advanced stages, this contributes to ascites (fluid in the abdomen) and edema (swelling in the legs). However, a healthy diet for liver health should not be bland. Replace salt with anti-inflammatory herbs and spices:
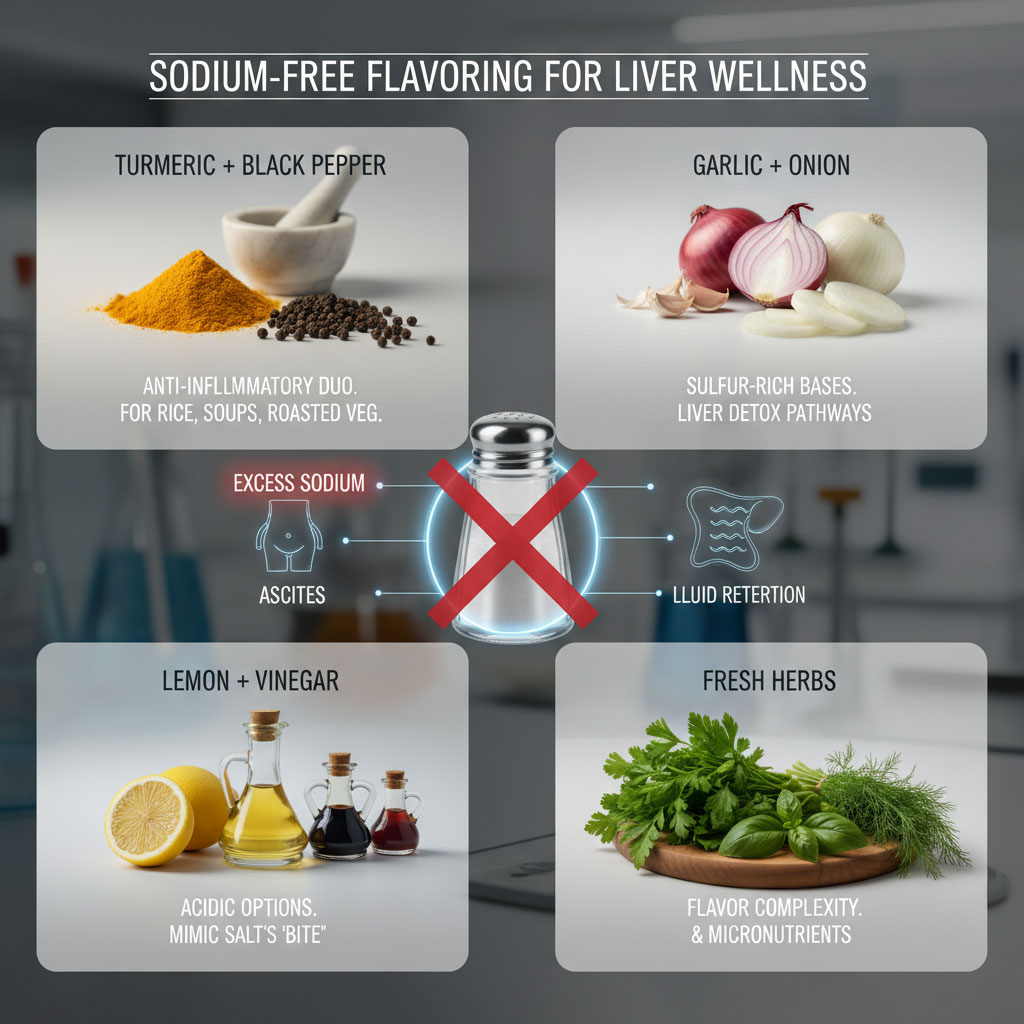
- Turmeric and Black Pepper: A powerful combination for reducing inflammation. Use this in rice, soups, and on roasted vegetables.
- Garlic and Onion: These contain sulfur compounds that support liver detoxification pathways. Use them generously as the base for most savory meals.
- Lemon and Vinegar: Acidity mimics the “bite” of salt on the tongue. Squeezing fresh lemon juice over grilled fish or lentil soup brightens the flavor instantly without the sodium load.
- Fresh Herbs: Parsley, cilantro, basil, and dill add complexity and micronutrients.
Batch Cooking for Energy Management
Fatigue is a reality for many living with chronic hepatitis. Cooking three fresh meals a day can be overwhelming and lead to ordering unhealthy takeout. To stick to your Hepatitis B diet guidelines, adopt a “Cook Once, Eat Twice” strategy.
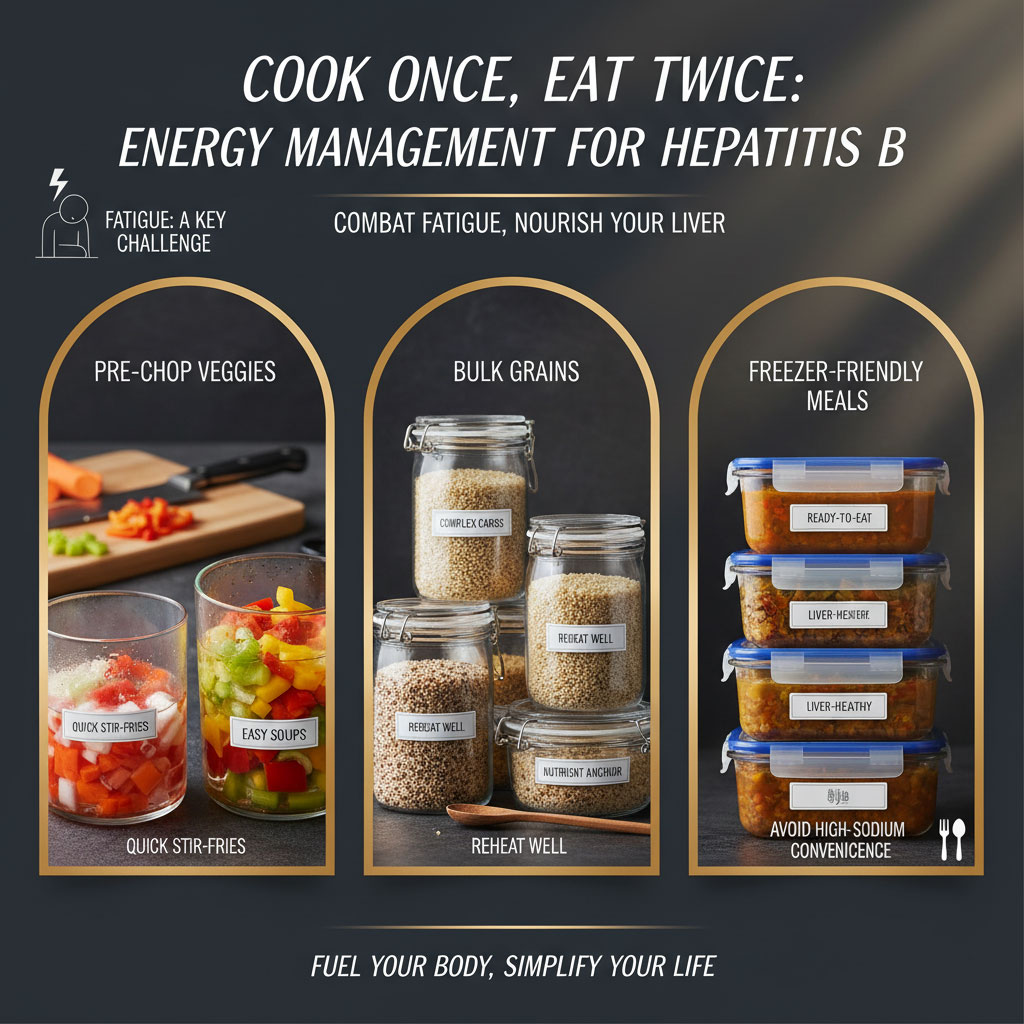
- Pre-Chop Vegetables: On days when you have higher energy, wash and chop carrots, celery, and peppers. Store them in water in the fridge. This makes starting a stir-fry or soup instant later in the week.
- Bulk Grains: Cook a large batch of quinoa or brown rice at the start of the week. These complex carbohydrates reheat well and serve as the base for lunch bowls.
- Freezer Friendly: Soups and stews (like the lentil soup in the meal plan) often taste better the next day and freeze perfectly. Having a liver-healthy meal ready in the freezer prevents the temptation of high-sodium convenience foods on bad days.
Reading Labels for Hidden Liver Stressors
When buying packaged foods, look beyond the calorie count. Two ingredients are particularly harmful to a liver managing HBV:
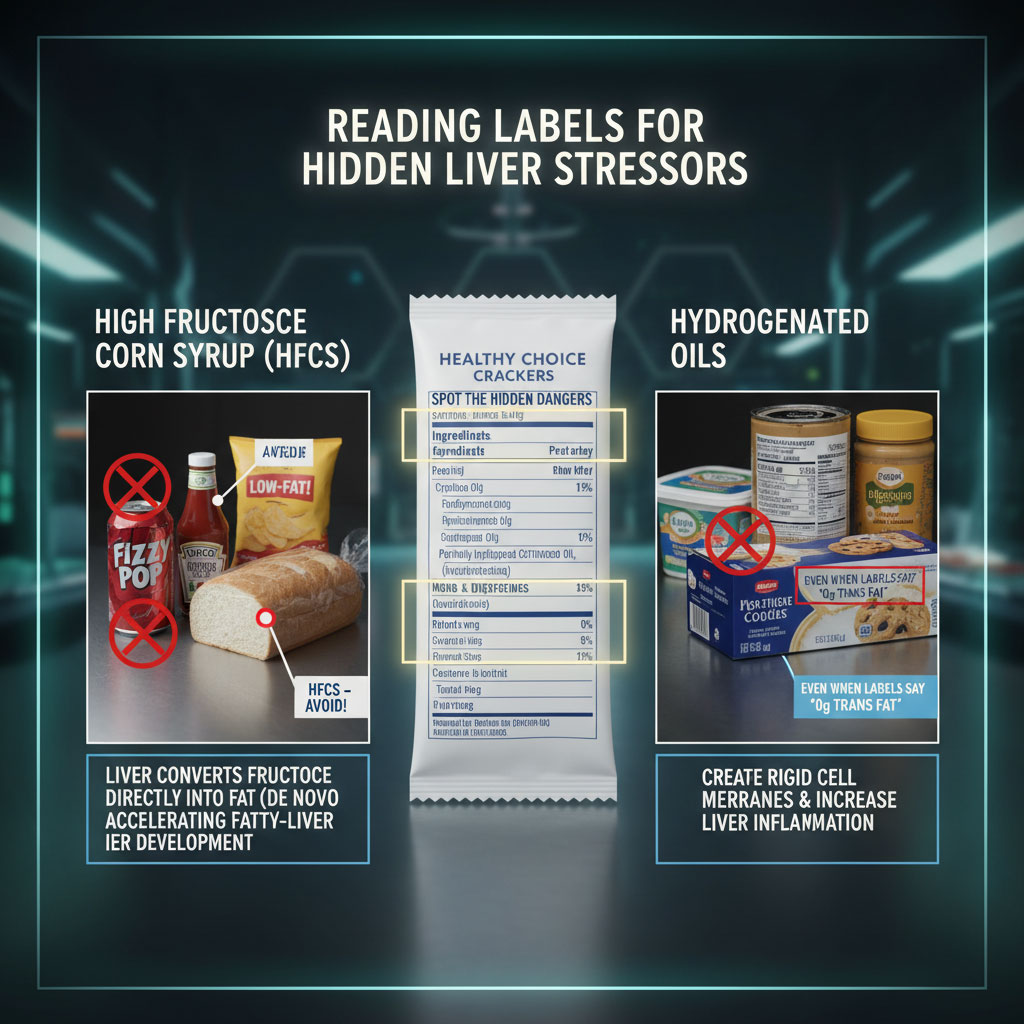
- High Fructose Corn Syrup (HFCS): Found in sodas, breads, condiments, and “low-fat” snacks. The liver turns fructose directly into fat (triglycerides) via a process called de novo lipogenesis. This leads to fatty liver significantly faster than other sugars.
- Hydrogenated Oils: Even if a label says “0g Trans Fat,” check the ingredients list. If you see “partially hydrogenated” or “hydrogenated,” put it back. These fats cause rigid cell membranes and increase liver inflammation.
Practical Strategies and Lifestyle Factors
Implementing a Hepatitis B nutrition plan requires practical lifestyle adjustments that go beyond the kitchen. Your environment and daily habits play a synergistic role with your diet.

Grocery Shopping Strategy
When shopping in the USA, learning to read labels is vital. Look for “No Added Sugar” and “Low Sodium” on packaging. Avoid the “Dirty Dozen” (fruits and vegetables with high pesticide residues) by choosing organic versions of strawberries, spinach, kale, and apples when possible. The liver must filter pesticides, so reducing this chemical load is beneficial. If organic is not affordable, wash conventional produce in a solution of water and baking soda to help remove surface residues.
Dining Out Safely
You can still enjoy restaurants while following Hepatitis B diet guidelines, but you must be a proactive diner.
- Choose Simple Preparations: Look for keywords like grilled, baked, steamed, or roasted. Avoid crispy, battered, breaded, or sautéed (which usually implies butter).
- Sauce on the Side: Restaurant sauces are often loaded with sugar, salt, and cream. Ask for dressings and sauces on the side so you can control the amount you consume.
- Avoid Raw Bars: Avoid sushi featuring raw fish or raw seafood bars entirely. The risk of bacterial infection is simply not worth it for a liver patient.
Hygiene and Food Safety
Preventing superinfections is critical. Hepatitis A and E are viruses that attack the liver and are transmitted through contaminated food and water. If you already have Hepatitis B, contracting Hep A or E can lead to acute liver failure.
- Wash Thoroughly: Wash all vegetables and fruits under running water.
- Cook Meat Properly: Use a meat thermometer to ensure poultry and pork are cooked to safe internal temperatures.
- Vaccination: Ensure you are vaccinated against Hepatitis A. This is a standard recommendation for all Hepatitis B patients.
Sleep and Stress Management
Your liver does much of its regenerative work while you sleep. Poor sleep quality is linked to insulin resistance and fatty liver. Aim for 7 to 8 hours of quality sleep per night. Additionally, chronic stress raises cortisol levels. High cortisol can lead to fat deposition in the liver. Incorporating stress-reduction techniques like walking, meditation, or gentle yoga can complement your dietary efforts.
Top Nutrients for Liver Repair
The following table highlights the specific micronutrients that should be prioritized in your diet to support liver regeneration.
| Nutrient | Primary Function for Hep B | Best Natural Sources | Daily Target (General) |
| Selenium | Reduces viral mutation rates & oxidative stress; supports immune response. | Brazil nuts (1-2 per day), Tuna, Halibut, Sardines | 55 mcg |
| Vitamin E | Protects liver cells from fatty deposits and inflammation; slows fibrosis. | Sunflower seeds, Almonds, Spinach, Avocado | 15 mg |
| Choline | Essential for expelling fat from the liver; prevents fatty liver buildup. | Eggs (yolks contain choline), Lean Chicken, Broccoli, Brussels sprouts | 425-550 mg |
| Glutathione | The “Master Antioxidant” used by the liver for detoxification pathways. | Garlic, Onions, Asparagus, Avocado (Consume precursors to help body produce it) | N/A (Focus on precursors) |
| Vitamin D | Modulates the immune system; deficiency is linked to higher viral loads. | Fatty fish, fortified dairy, sunlight exposure | 600-800 IU (Check levels with doctor) |
Case Studies and Real Data
Generalized case studies in hepatology often show a clear correlation between lifestyle and disease progression. For instance, clinical observations frequently note that patients with Hepatitis B virus (HBV) who also struggle with obesity or alcohol use have significantly higher liver enzymes (ALT/AST) and a faster rate of fibrosis progression compared to those who maintain a healthy weight and abstain from alcohol.
Research published in major hepatology journals has shown that a diet high in vegetables and coffee, combined with moderate exercise, can stabilize liver enzymes even without changes in antiviral medication. In one notable instance, a study involving thousands of participants demonstrated that coffee consumption was inversely associated with the severity of hepatic fibrosis. Conversely, data clearly links regular alcohol consumption in Hepatitis B carriers to a significantly higher incidence of Hepatocellular Carcinoma (HCC). These instances underscore a powerful truth: while you may not be able to eliminate the virus completely from your body, you have immense control over the health of the organ it inhabits. The progression of liver disease is not purely viral; it is an interaction between the virus and the environment you create within your body.
Summary and Key Takeaways
Managing Hepatitis B is a marathon, not a sprint. It requires a long-term commitment to a lifestyle that prioritizes organ health. This 7-day meal plan for Hepatitis B provides a blueprint for that lifestyle. It is not a temporary “diet” but a template for how to eat for longevity.
The key takeaways for effective management are consistent:
- Eliminate Toxins: Total avoidance of alcohol and raw shellfish is necessary to prevent immediate danger and long-term scarring.
- Prevent Fatty Liver: Reduce saturated fats, trans fats, and refined sugars to stop fat accumulation, which acts as fuel for viral damage.
- Empower Immunity: Flood your body with foods rich in antioxidants for hepatitis, such as berries, leafy greens, and nuts, to help neutralize the oxidative stress caused by the infection.
- Maintain Hygiene: Strict food safety practices prevent superinfections that could overwhelm the liver.
By strictly adhering to these Hepatitis B diet guidelines, you empower your immune system to keep the virus in check. Remember, a healthy diet for liver health is not about deprivation. It is about abundance—an abundance of colorful vegetables, safe protein sources, and nutrients that allow your liver to thrive despite the presence of the virus. You are taking an active role in your healthcare, one meal at a time.
Frequently Asked Questions (FAQs)
Can I reverse liver damage from Hepatitis B with diet?
While diet cannot “cure” the virus or remove it from the DNA of infected cells, the liver has a remarkable ability to regenerate. A nutritious diet can heal early-stage inflammation and mild fibrosis (scarring). By removing stressors like alcohol and fat, you allow the liver cells to repair themselves. However, extensive scarring (cirrhosis) is more difficult to reverse, though a strict diet can prevent further progression and decompensation.
Is intermittent fasting safe for Hepatitis B?
Intermittent fasting should be approached with extreme caution. Patients with advanced liver disease often have low glycogen stores. Fasting can force the body to break down muscle tissue for energy, leading to sarcopenia (muscle wasting), which is a poor prognostic indicator in liver disease. It is best to consult a hepatologist before starting any fasting regimen to ensure it doesn’t cause metabolic stress.
What is the best vitamin for Hepatitis B patients?
Vitamin D and Vitamin E are often cited as the most beneficial. Vitamin D supports immune function and helps the body respond to the virus, while Vitamin E is a powerful antioxidant that protects liver cells. However, it is always better to get these from food sources like fatty fish, nuts, and seeds rather than relying solely on supplements, as high doses of certain vitamins can be toxic.
Why do I feel tired after eating with Hepatitis B?
Fatigue is a very common symptom. If the liver is sluggish or inflamed, it may struggle to mobilize energy stores efficiently. Additionally, eating large, heavy meals diverts significant blood flow to the digestive system, which can increase feelings of fatigue. Following a plan with small, frequent meals containing complex carbohydrates can help manage energy levels more effectively.
Is turmeric good for Hepatitis B?
Turmeric contains curcumin, which has strong anti-inflammatory and antioxidant properties. Many patients find it helpful. However, be cautious with high-dose turmeric supplements, as there have been rare reports of drug-induced liver injury in sensitive individuals. Using turmeric spice in cooking (with black pepper) is the safest and most natural method to get the benefits.
Can I drink lemon water for my liver?
Lemon water is a healthy habit. It helps with hydration and provides a small amount of Vitamin C, which is an antioxidant. While it is not a “miracle detox cure” that flushes the virus out, staying hydrated is essential for optimal liver function, so lemon water is a far better choice than soda or sugary juice.
How much protein do I need if I have Hepatitis B?
Most patients need a normal amount of protein (about 1 to 1.2 grams per kilogram of body weight). Protein is vital for liver repair and enzyme production. Only in very advanced stages of liver failure, specifically if a patient has hepatic encephalopathy (confusion caused by toxins), might protein need to be temporarily restricted under strict medical supervision.
Are eggs bad for the liver?
No, eggs are generally good for the liver. They are an excellent source of high-quality protein and choline. Choline is necessary for the liver to export fat; without it, fat accumulates in the liver. However, if you have high cholesterol or gallbladder issues alongside Hepatitis B, you may need to moderate your yolk intake or focus on egg whites.
What is the “Ascites diet”?
This refers to a very low-sodium diet prescribed for patients who have fluid buildup in the abdomen, a condition called ascites. It typically involves limiting salt intake to less than 2,000 mg (or sometimes 1,500 mg) per day to prevent water retention. If you have ascites, this diet is a critical medical prescription, not just a suggestion.
Does sugar increase viral load?
Sugar does not directly increase the replication of the virus. However, high sugar intake suppresses the immune system and leads to fatty liver. A fatty, inflamed liver provides a compromised environment where the immune system is less effective at controlling the infection. Therefore, reducing sugar indirectly helps your body manage the virus better.
Can I drink non-alcoholic beer?
It is generally recommended to avoid non-alcoholic beer. Many brands still contain trace amounts of alcohol (up to 0.5%). Furthermore, the taste and ritual can act as a psychological trigger for those who previously enjoyed alcohol, potentially leading to a relapse in drinking habits. Given that alcohol is so dangerous for Hepatitis B patients, it is safer to stick to water, tea, or coffee.
How often should I eat?
Eating small, frequent meals (every 3 to 4 hours) is often better than three large meals. This prevents the liver from being overwhelmed by a large influx of nutrients at once, which helps manage metabolic stress. It also helps maintain stable blood sugar levels throughout the day, preventing the energy crashes common with liver issues. A small snack before bed containing complex carbs and protein can also help prevent muscle breakdown during the night.