Individuals managing hypotension should actively avoid foods that function as natural vasodilators or diuretics. The primary foods and fruits to avoid with low blood pressure include grapefruit due to dangerous medication interactions, watermelon and beetroot for their nitric oxide content, and celery for its diuretic properties. Additionally, limiting alcohol and large portions of refined carbohydrates is essential to prevent rapid drops in pressure known as postprandial hypotension.
Table of Contents
Most health advice you encounter in the United States screams at you to lower your blood pressure. We are surrounded by “heart-healthy” labels urging us to cut salt, eat more beets, and load up on potassium. But for the millions of Americans living with hypotension (chronic low blood pressure), this standard advice is not just unhelpful; it is dangerous.

If your readings consistently hover below 90/60 mmHg, eating the wrong “superfood” can send your pressure plummeting further. This can lead to dizziness, fainting (syncope), brain fog, and falls that result in serious injury. You do not need to lower your pressure; you need to stabilize it. The physiology of a hypotensive body is fundamentally different from the general population, meaning your nutritional needs are often the exact opposite of the standard dietary guidelines issued by major health organizations.
This comprehensive guide flips the script on standard nutrition. We will explore the specific foods to avoid with low blood pressure, backed by the biochemistry of how certain compounds like L-citrulline, nitrates, and furanocoumarins interact with your vascular system. We will also delve into the nuances of food-drug interactions and the critical balance of electrolytes required to keep you standing upright.
The Physiology of Food and Hypotension: Why Diet Matters
To understand why a healthy fruit can be a hazard for you, we must first look at the mechanics of blood pressure regulation. Your blood pressure is essentially determined by three main factors: the pump (heart), the pipes (blood vessels), and the fluid (blood volume). In a healthy individual, these three work in perfect harmony to fight gravity and keep blood flowing to the brain.
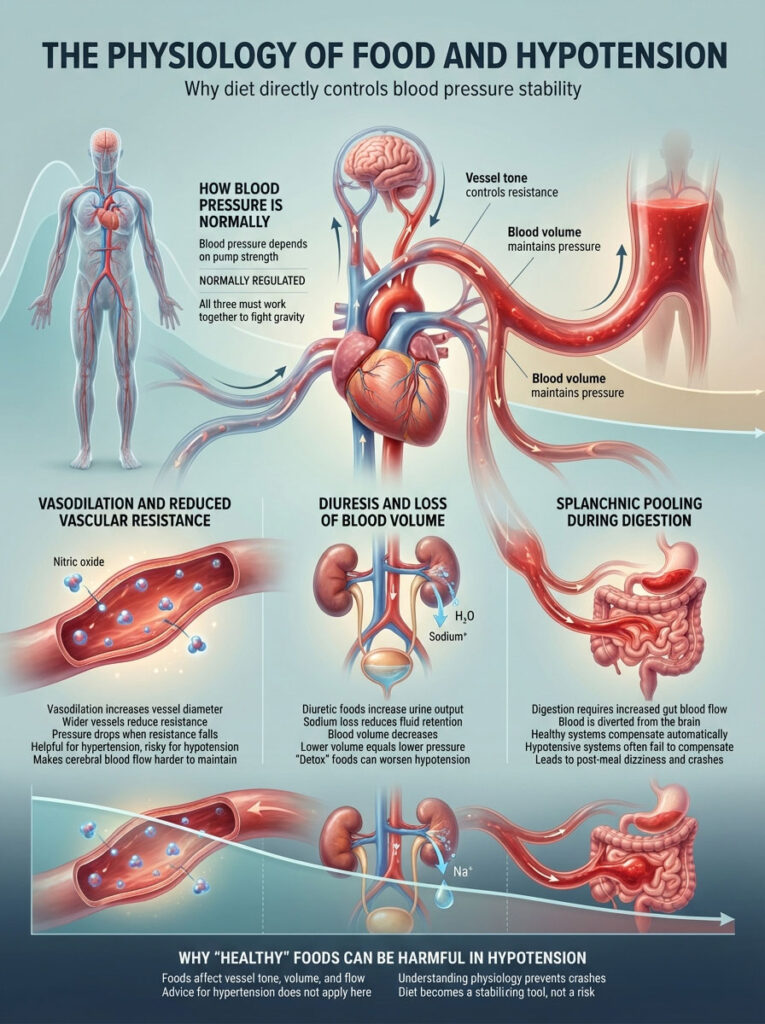
In patients with hypotension, one or more of these systems is compromised. Certain foods manipulate these factors in ways that are beneficial for hypertensive patients but risky for you. Understanding these mechanisms is the first step in mastering a low blood pressure diet.
Vasodilation and Vascular Resistance
Vasodilation is the widening of blood vessels. When the smooth muscles lining your arteries relax, the diameter of the vessel increases. Imagine water flowing through a garden hose; if you widen the hose without turning up the tap, the water pressure drops. Foods rich in nitric oxide boosters force this relaxation. For someone with high blood pressure, this is life-saving. For someone with low blood pressure, it reduces systemic vascular resistance, making it harder for the heart to push blood up to the head.
Diuresis and Blood Volume
Blood pressure relies heavily on the total volume of blood circulating in your body. This volume is largely dictated by fluid and sodium levels. Diuresis refers to the increased production of urine. Diuretic foods and beverages flush sodium and water out of the body through the kidneys. Since sodium helps hold fluid in your veins through osmotic pressure, losing it decreases your total blood volume. Lower volume means lower pressure. Many “detox” foods act as diuretics, which can be catastrophic for a hypotensive patient already struggling to retain fluids.
Splanchnic Pooling and Digestion
Digestion is an energy-intensive process. When you eat, your body diverts a significant amount of blood from your brain and extremities to your stomach and intestines to aid in digestion and nutrient absorption. This is known as splanchnic pooling. In a healthy person, the autonomic nervous system compensates by constricting blood vessels in the legs and increasing the heart rate. In those with hypotension, this compensation often fails. The blood pools in the gut, and the rest of the body is left with insufficient pressure, leading to a post-meal crash.
The “Healthy” Vasodilators: Fruits to Avoid With Low Blood Pressure
The following fruits are celebrated in medical literature for their ability to lower blood pressure. For you, that is exactly why they belong on the “caution” list. While they are nutritious, their chemical impact on your vascular tone can trigger symptoms.
1. Watermelon (The L-Citrulline Factor)
Watermelon is often the summer fruit of choice, refreshing and hydrating. However, it poses a hidden, biochemical risk for hypotensive individuals due to its amino acid profile. It is the richest natural source of an amino acid called L-citrulline.
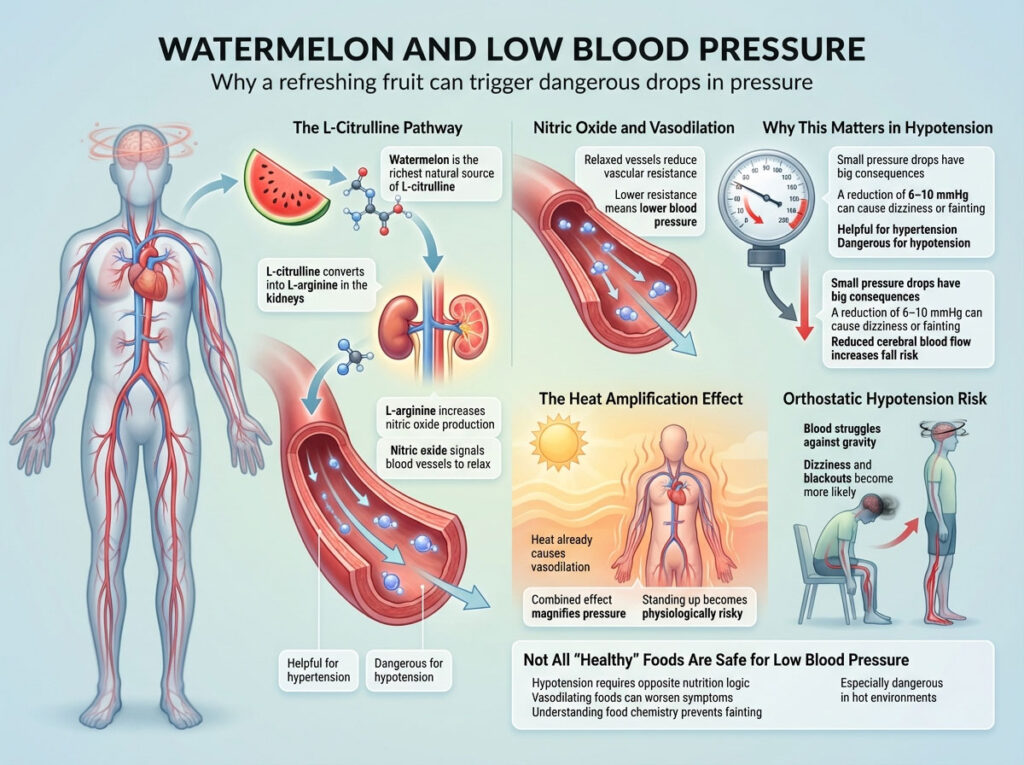
The Scientific Mechanism of L-Citrulline
The danger lies in how the body processes this compound. When you consume watermelon, your kidneys convert L-citrulline into L-arginine. This amino acid is a direct precursor to Nitric Oxide (NO). Nitric oxide is a gas signaling molecule that acts on the endothelium (inner lining) of blood vessels, telling the smooth muscles to relax.
A study published in the American Journal of Hypertension demonstrated that watermelon extract supplementation effectively reduced ankle and brachial blood pressure. While a drop of 6 to 10 mmHg is a victory for someone with hypertension, it can be the difference between standing upright and fainting for someone running at 85/55 mmHg.
The Environmental Context
Consider the context in which watermelon is usually eaten: hot summer days. Heat is already a potent vasodilator because the body sends blood to the skin to cool down. If you combine the heat-induced vasodilation with the chemical vasodilation from the L-citrulline in watermelon, you create a “double hit” effect. This can lead to severe orthostatic hypotension, where you feel dizzy or black out upon standing.
2. Beetroot and Beet Juice (Nature’s Nitroglycerin)
Beetroot has gained massive popularity in the athletic world and the wellness community for its ability to boost blood flow and lower blood pressure. It achieves this through a high concentration of dietary nitrates.
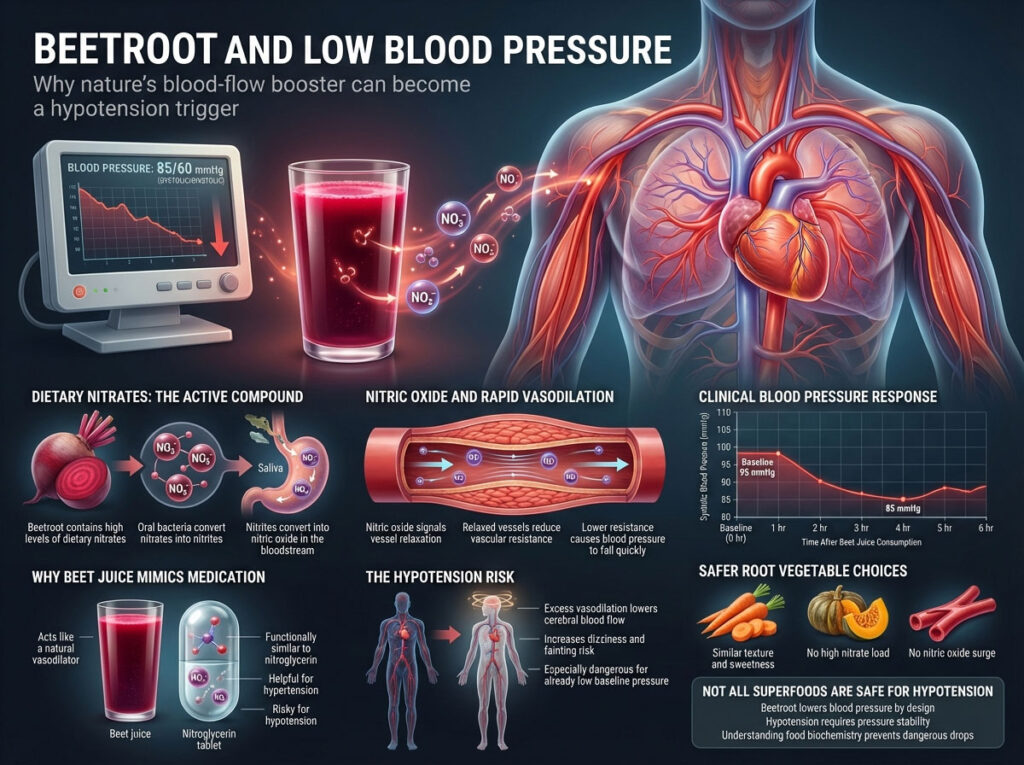
The Nitrate-Nitrite-Nitric Oxide Pathway
The mechanism here is potent. Your saliva contains microbiome bacteria that convert dietary nitrates from beets into nitrites. Once swallowed, these nitrites are further converted into nitric oxide in the blood. The effect is rapid and measurable. Clinical trials have shown that a single glass of beet juice can lower systolic blood pressure significantly within just 3 to 6 hours of consumption.
For a patient with hypotension, drinking beet juice is chemically similar to taking a mild dose of a prescription vasodilator like nitroglycerin. If you are struggling to keep your numbers up, beets act as a sabotaging agent. The drop is often most pronounced in the systolic reading (the top number), which is crucial for brain perfusion.
Safe Alternatives to Beets
If you enjoy root vegetables, opt for carrots or roasted squash instead. These provide similar textures and sweetness without the high nitrate load that triggers vascular relaxation.
3. Berries and High-Potassium Fruits
Potassium is a vital mineral that regulates muscle contractions and nerve signals. However, it functions as the biological counterweight to sodium. Sodium raises blood pressure by retaining fluid; potassium lowers it by helping your vessel walls relax and forcing the kidneys to excrete sodium.

The Sodium-Potassium Balance
If your diet is heavy in bananas, apricots, cantaloupe, and berries, but low in salt, you are tipping the physiological scales toward hypotension. While you do not need to eliminate these entirely, consuming them in excess without adequate sodium intake can worsen your symptoms.
For example, a morning smoothie packed with two bananas and a cup of spinach (another high-nitrate, high-potassium food) delivers a massive dose of blood-pressure-lowering minerals. Without a savory element to counterbalance this, you may find your mid-morning energy crashing as your pressure drops.
The Medication Disruptors: Dangerous Interactions
Food-drug interactions are a critical, often overlooked aspect of managing health. One specific fruit stands out as a severe risk for those on blood pressure medication or other heart-related drugs, potentially causing toxic drops in pressure.
4. Grapefruit and Grapefruit Juice
This is perhaps the most urgent warning in this guide. Grapefruit and blood pressure medication are a volatile mix. This interaction is not mild; it can be life-threatening.
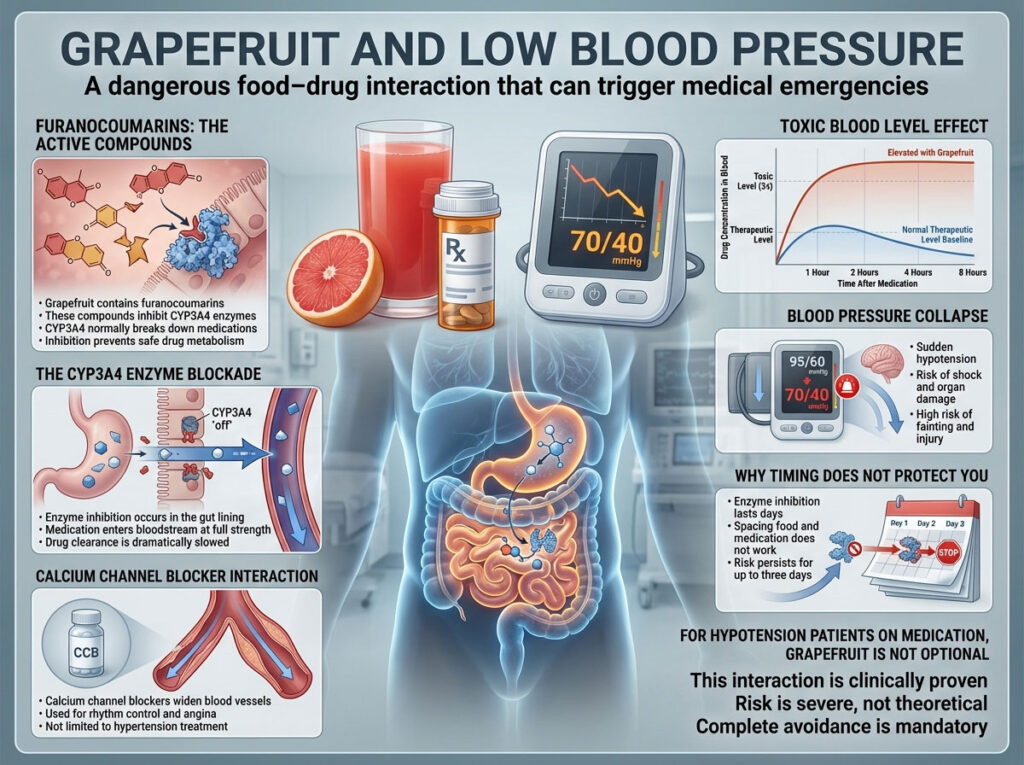
The CYP3A4 Enzyme Blockage
Grapefruit contains organic compounds called furanocoumarins. These chemicals have a unique ability to bind to and inhibit an enzyme in your small intestine known as CYP3A4. This enzyme is the body’s primary defense mechanism for metabolizing (breaking down) many medications before they enter the bloodstream.
Interaction with Calcium Channel Blockers
This is particularly dangerous if you are taking Calcium Channel Blockers (CCBs) such as Nifedipine, Felodipine, or Amlodipine. These drugs are sometimes used for angina or rhythm control, not just high blood pressure. When you consume grapefruit, the enzyme that is supposed to break down the drug is deactivated.
The Consequence: Toxic Overdose
According to FDA data, when the enzyme is blocked, the medication enters your bloodstream at full potency and stays there much longer than intended. This leads to an overdose effect. Even if you took the correct dose of your medication, the grapefruit juice acts as a multiplier, increasing the drug’s concentration in your blood by up to 300%. The result can be an uncontrolled, rapid drop in blood pressure that leads to shock or organ damage.
Expert Note: Many patients ask if they can simply space them out. The answer is a definitive no. The enzyme inhibition caused by grapefruit acts on the gut lining and can last upwards of 24 to 72 hours. If you are on these medications, grapefruit is strictly one of the foods to avoid with low blood pressure.
The Diuretics and Dehydrators: Fluid Thieves
Blood pressure relies heavily on blood volume. If you are dehydrated, there is less fluid filling your veins, and pressure drops naturally. Foods and beverages that encourage fluid loss are counterproductive and should be managed carefully.
5. Celery and Celery Juice
The recent “celery juice movement” suggests drinking 16 ounces of pure juice every morning on an empty stomach. For a hypotensive patient, this trend is ill-advised and potentially symptomatic.
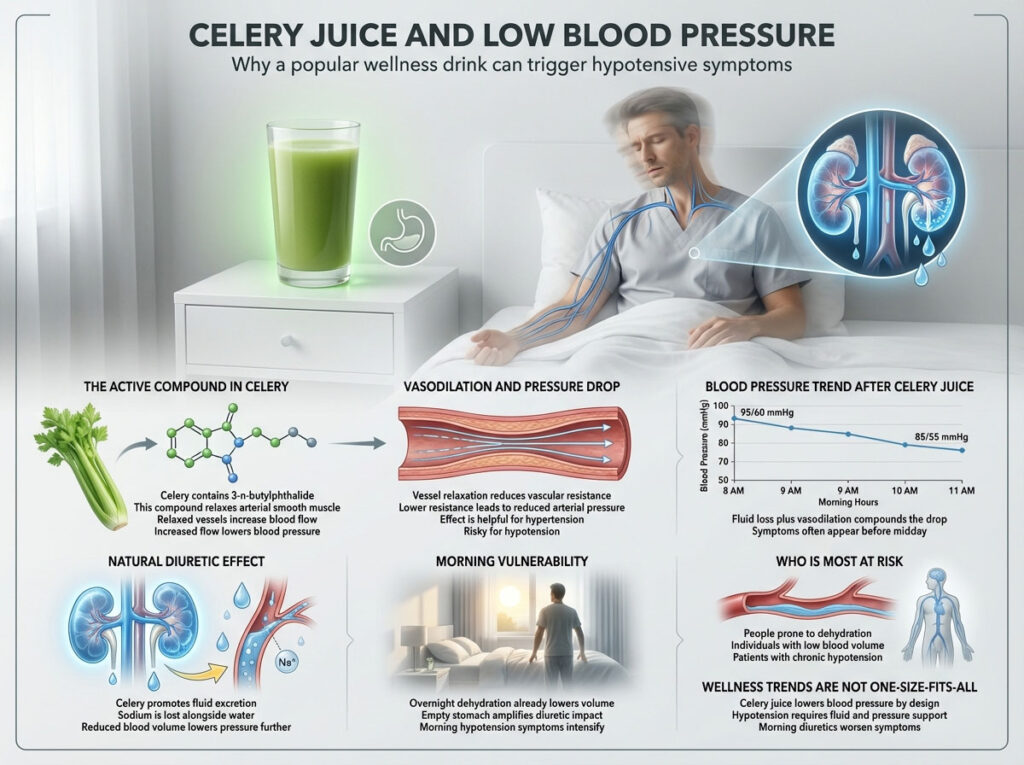
The Mechanism of 3-n-butylphthalide
Celery contains a phytochemical called 3-n-butylphthalide. This compound gives celery its distinct aroma and has been scientifically proven to relax the tissues of the artery walls to increase blood flow and reduce blood pressure. Furthermore, celery acts as a natural diuretic.
If you are already prone to dehydration or low blood volume (hypovolemia), the diuretic effect of celery strips your body of the fluids and sodium it desperately needs to maintain arterial pressure. Starting your day with a diuretic juice can leave you feeling lightheaded and fatigued before lunch.
6. Alcohol (The Double-Edged Sword)
Alcohol is often misunderstood in the context of blood pressure. While chronic heavy drinking can raise BP over years due to arterial stiffening, the immediate, acute effect of alcohol is a sharp drop in pressure.

Vasodilation and Thermal Regulation
First, alcohol acts as a potent vasodilator. This is why your skin might feel warm or look flushed after a drink; blood is rushing to the surface vessels away from the core organs. This peripheral pooling reduces the central blood pressure available to the brain.
Inhibition of Vasopressin
Second, alcohol inhibits the secretion of Vasopressin, also known as the Anti-Diuretic Hormone (ADH), from the pituitary gland. This hormone is responsible for telling your kidneys to reabsorb water back into the bloodstream. When alcohol switches it off, your kidneys flush water out rapidly, leading to frequent urination.
The Orthostatic Risk
This combination—widened vessels plus reduced fluid volume—makes alcohol a primary trigger for Orthostatic Hypotension. This is the dizzy, “blackout” sensation you feel when standing up too quickly. If you have low blood pressure, alcohol exacerbates this risk significantly, increasing the likelihood of falls during or after consumption.
The Silent Trigger: Carbohydrates and Postprandial Hypotension
Sometimes, it is not just what you eat, but how much you eat and the macronutrient composition of the meal. Large meals are a frequent cause of dizziness in the elderly and those with autonomic dysfunction.
7. Refined Carbohydrates (White Rice, Pasta, Pizza)
Have you ever felt the need to nap immediately after a heavy pasta dinner? That “food coma” is often a clinical sign of Postprandial Hypotension.
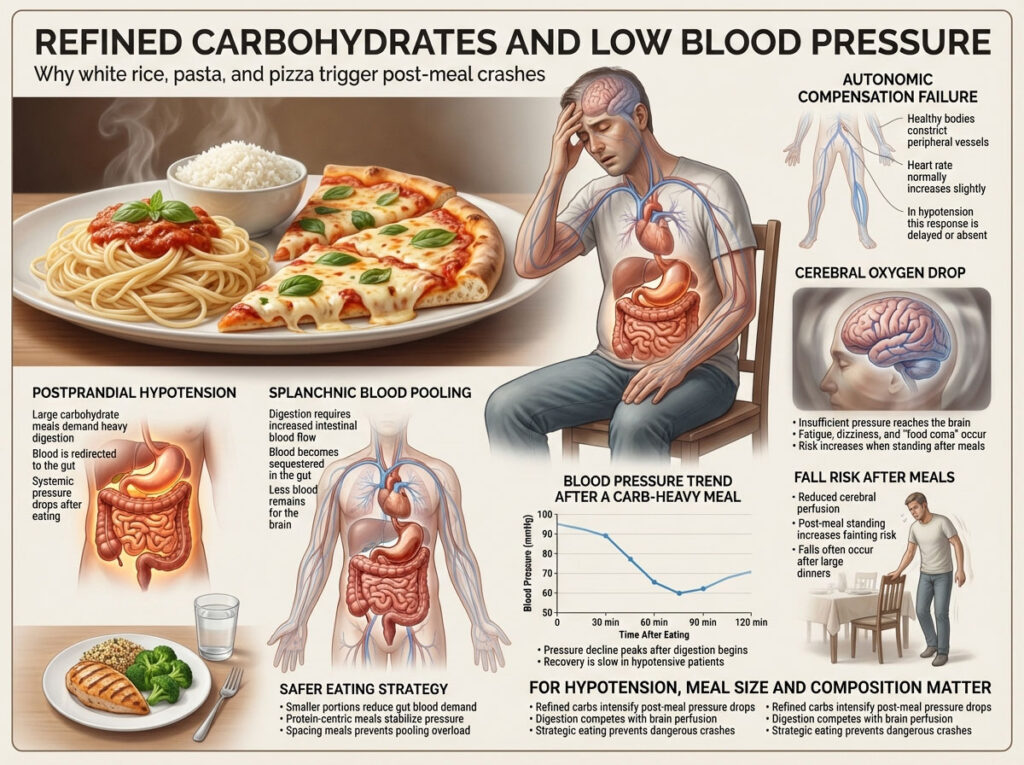
The Mechanics of Splanchnic Pooling
When you consume a massive load of simple carbohydrates (like a bowl of white rice, sugary cereals, or a large pizza), your digestive system has to work overtime to break down the sugars. To fuel this metabolic process, the body shunts a significant amount of blood flow to the stomach and intestines. This is called splanchnic pooling.
The Autonomic Failure
In a healthy body, the autonomic nervous system detects this shift and immediately constricts blood vessels in the legs and arms to maintain systemic pressure. It also increases the heart rate slightly. In hypotensive patients, this reflex is often slow or absent. The blood pools in the gut, sequestered away from the main circulation, leaving the brain with insufficient oxygen.
The Instance
Statistics indicate that postprandial hypotension affects up to 30% of older adults in care facilities in the USA and is a leading cause of unexplained falls after meals. The drop in pressure usually peaks 30 to 60 minutes after eating. To avoid this, skip the large carb-heavy plates and opt for smaller, protein-centric meals spaced throughout the day.
Comparative Analysis: Foods to Avoid vs. Safe Alternatives
To simplify your low blood pressure diet, we have categorized the risks and provided safer alternatives that will not crash your numbers. This table serves as a quick reference guide for grocery shopping.
| Food Category | Foods to Avoid (Hypotension Risk) | The Mechanism (Why it Drops BP) | Safe Alternatives |
| Fruits | Watermelon, Grapefruit | High L-Citrulline; Blocks CYP3A4 enzyme; Increases Nitric Oxide | Berries, Apples, Grapes, Cherries |
| Vegetables | Beetroot, Celery, Spinach (Excess) | High Nitrates; Natural Diuretic properties; Vasodilation | Carrots, Green Beans, Squash, Sweet Potatoes |
| Beverages | Alcohol, Beet Juice, Sugary Sodas | Dehydration; Vasodilation; ADH Inhibition; Glucose Spikes | Tomato Juice (Sodium), Herbal Tea, Electrolyte Water |
| Grains | White Rice, Large Pasta Portions | Triggers Postprandial Hypotension via splanchnic pooling | Quinoa, Barley, Brown Rice (Low Glycemic) |
| Herbs | Garlic Supplements (High Dose) | Acts as mild ACE-inhibitor; Increases Nitric Oxide | Rosemary, Thyme, Himalayan Salt, Soy Sauce |
Strategic Diet Plan for Hypotension: What to Eat
Knowing the foods to avoid with low blood pressure is only half the battle. You also need to know what to embrace to actively support your vascular health. A hypotension diet is often the exact opposite of the standard American healthy diet, requiring a shift in mindset regarding salt and fats.

The Sodium Strategy: Salt is Medicine
For the general US population, salt is the enemy. For you, it is a vital therapeutic tool. Sodium helps your body retain fluid, which increases blood volume and raises blood pressure.
- Actionable Tip: Incorporate foods like pickles, olives, cottage cheese, canned soups, and cured meats.
- Precaution: Always consult your cardiologist before radically increasing salt intake, especially if you have heart failure or kidney concerns. The goal is to raise pressure, not to overload the heart.
Hydration Volume and Electrolytes
You must drink to keep your pressure up. Aim for 2 to 3 liters of fluids daily. However, plain water acts as a diuretic if consumed in isolation without electrolytes.
- Electrolytes Matter: Water follows salt. If you drink gallons of plain water without enough sodium, potassium, and magnesium, you may dilute your blood sodium levels (hyponatremia), which is dangerous.
- The Solution: Use electrolyte powders or add a pinch of sea salt and lemon to your water. Tomato juice is an excellent high-sodium, hydrating beverage.
Vitamin B12 and Folate for Blood Quality
Deficiencies in Vitamin B12 and Folate can lead to anemia. Anemia means your body does not produce enough red blood cells, which decreases the viscosity and volume of your blood, leading to lower pressure.
- Sources: Ensure your diet includes eggs, fortified cereals, nutritional yeast, and lean meats to cover these bases. Vegetarians should be especially vigilant about B12 supplementation.
The Caffeine Boost: Timing is Key
Caffeine acts as a vasoconstrictor, meaning it tightens blood vessels and temporarily raises blood pressure.
- Morning Routine: A cup of strong coffee in the morning can be an effective tool to combat morning hypotension.
- Tolerance: Be aware that regular users may develop a tolerance to this effect. It works best as a targeted intervention (e.g., before standing for long periods) rather than a constant drip.
Real-World Scenarios and Case Studies
To demonstrate the importance of these dietary choices, let us look at how these interactions play out in real life scenarios.

Scenario 1: The “Healthy” Breakfast Collapse
A 65-year-old retired teacher in Florida, prescribed Nifedipine for stable angina, decided to start a “heart-healthy breakfast” routine involving fresh grapefruit juice every morning. Within three days, he began experiencing severe dizziness and eventually collapsed in his kitchen. At the ER, his blood pressure was found to be 70/40 mmHg. The grapefruit had blocked the metabolism of his medication, effectively overdosing him. This is a textbook example of why grapefruit and blood pressure meds do not mix.
Scenario 2: The Post-Sunday Lunch Faint
A resident in an assisted living facility consistently felt lightheaded and required bed rest after Sunday lunches. The meal was typically lasagna with garlic bread—a high-carb, low-protein load. The diagnosis was postprandial hypotension. The massive influx of carbohydrates caused blood to pool in her abdomen for digestion, starving her brain of oxygen. By switching to smaller meals and reducing the pasta portion size in favor of chicken and vegetables, the fainting spells ceased.
Scenario 3: The Summer Dehydration Incident
A young woman with constitutionally low blood pressure attended an outdoor summer festival. She consumed several alcoholic beverages and ate watermelon to stay cool. The combination of heat (vasodilation), alcohol (diuresis + vasodilation), and watermelon (L-citrulline vasodilation) caused a syncopal episode (fainting). She was treated with IV fluids to restore blood volume. This highlights the cumulative effect of stacking multiple vasodilators.
Comprehensive Data on Glycemic Load and Blood Pressure
To further assist in meal planning, it is crucial to understand which carbohydrates are most likely to trigger a postprandial crash. Foods with a high Glycemic Index (GI) and Glycemic Load (GL) cause faster spikes in blood sugar, requiring more rapid digestion and blood diversion.
| Carbohydrate Source | Glycemic Index (GI) | Risk of Postprandial Drop | Recommendation for Hypotension |
| White Rice | 73 (High) | High | Avoid large bowls; mix with protein/fat |
| Mashed Potatoes | 82 (High) | High | Limit portion; eat with skin on |
| Instant Oatmeal | 79 (High) | Moderate/High | Switch to steel-cut oats |
| Quinoa | 53 (Low) | Low | Excellent staple choice |
| Barley | 28 (Low) | Low | Best grain for blood sugar/pressure stability |
| Lentils | 32 (Low) | Low | High in Folate and protein; highly recommended |
Summary and Key Takeaways
Managing hypotension requires a vigilant approach to diet that defies conventional wisdom. While society pushes for vascular relaxation and low salt, your body requires stability, fluids, and sodium. The goal is to prevent the sharp drops that lead to symptoms, allowing you to live an active, safe life.

Here is your checklist for safety:
- Eliminate Grapefruit completely if you are on calcium channel blockers or statins.
- Limit Watermelon and Beets to avoid excess nitric oxide production during hot weather or when feeling faint.
- Monitor Alcohol intake to prevent dehydration and orthostatic drops; drink water between alcoholic beverages.
- Avoid Large Carb Meals to stop blood from pooling in your gut; adopt a “grazing” style of eating with 5-6 small meals.
- Increase Sodium and Fluids strategically to maintain blood volume, using pickles, olives, and electrolyte drinks.
By removing the foods to avoid with low blood pressure from your daily routine and substituting them with stabilizing alternatives, you can regain control over your energy levels and reduce the risk of dangerous falls.
Frequently Asked Questions (FAQ)
What foods instantly raise blood pressure?
There are no foods that “instantly” raise pressure like a switch, but salty foods like pickles, canned soup, or drinking 16oz of water rapidly can provide a quick boost. The “osmopressor response” from drinking water quickly can raise systolic pressure by 20-30 mmHg in hypotensive patients. Caffeine also acts as a fast-acting vasoconstrictor to temporarily spike pressure.
Why do I feel dizzy after eating rice or pasta?
This is likely postprandial hypotension. When you eat large portions of refined carbohydrates, blood rushes to your digestive system to process the sugars. In people with hypotension, the body fails to compensate by constricting other vessels, leading to a system-wide pressure drop 30 to 60 minutes after eating.
Is banana good for low blood pressure?
Bananas are high in potassium, which naturally lowers blood pressure. If you have hypotension, you should only eat bananas if you are balancing them with enough sodium. Eating too much potassium without salt can worsen your condition by upsetting the sodium-potassium balance in your kidneys.
Can drinking water raise blood pressure?
Yes. Clinical studies show that drinking about 16 ounces (500ml) of water quickly (within 5 minutes) can induce an autonomic reflex known as the “osmopressor response.” This can raise systolic blood pressure significantly in people with autonomic failure, making it a great emergency tool if you feel faint.
Does chocolate help low blood pressure?
Dark chocolate contains flavanols that boost nitric oxide and lower blood pressure, so it should be consumed in moderation. However, milk chocolate contains caffeine and sugar, which might provide a short energy burst but is not a reliable treatment. For hypotensive patients, the vasodilation from dark chocolate makes it a food to limit.
What is the best breakfast for someone with hypotension?
A protein-rich and salty breakfast is ideal to prevent a mid-morning slump. Try eggs (rich in B12) with salted avocado toast or cottage cheese with nuts. Avoid sugary cereals, pastries, or sweet smoothies, as the sugar crash can trigger dizziness and palpitations later in the morning.
Is lemon water good for low blood pressure?
Lemon water itself hydrates you, which is positive. However, lemon does not have special BP-raising properties. To make it effective for hypotension, add a pinch of Himalayan salt to turn it into a natural electrolyte drink. This helps your body retain the fluid.
Can I drink alcohol if I have low blood pressure?
It is risky. Alcohol dehydrates you and dilates blood vessels, leading to a “double drop” in pressure. If you choose to drink, do so slowly, never on an empty stomach, and alternate every drink with a full glass of water. Avoid hot environments while drinking, like hot tubs or crowded clubs.
Does garlic lower blood pressure immediately?
Garlic has a cumulative effect rather than an immediate one. It increases nitric oxide production over time. If you take high-dose garlic supplements, you may notice your baseline blood pressure dropping, which could be detrimental for hypotensive patients. Culinary amounts are generally safe, but supplements should be avoided.
Why should I avoid grapefruit with BP meds?
Grapefruit blocks the CYP3A4 enzyme in your gut. If you take drugs like Nifedipine or Felodipine, this blockage prevents the drug from breaking down, causing it to build up in your blood. This can lead to a toxic overdose and a dangerous crash in blood pressure, potentially causing shock.
Is yogurt good for low blood pressure?
Yes, yogurt can be beneficial, especially if it is fortified with Vitamin B12. A B12 deficiency is a common cause of anemia-related low blood pressure. Greek yogurt also provides protein, which helps stabilize blood sugar. Adding salted nuts to yogurt makes it an even better snack for this condition.
What deficiency causes low blood pressure?
The most common nutritional deficiencies linked to low blood pressure are Vitamin B12, Folate (Vitamin B9), and Iron. A lack of these nutrients prevents the body from producing enough healthy red blood cells, resulting in anemia. This reduces the oxygen-carrying capacity and volume of the blood, leading to chronic hypotension.
Disclaimer: The content provided in this article is for educational purposes only and does not constitute medical advice. Hypotension can be a symptom of underlying medical conditions. Always consult with a cardiologist or healthcare provider before making significant changes to your diet, salt intake, or medication regimen, especially if you have a history of heart disease or kidney issues.
References:
- FDA. (2021). Grapefruit Juice and Some Drugs Don’t Mix. U.S. Food and Drug Administration.
- Figueroa, A., et al. (2013). Effects of Watermelon Supplementation on Aortic Blood Pressure and Wave Reflection in Individuals With Prehypertension: A Pilot Study. American Journal of Hypertension.
- Mayo Clinic. (2023). Postprandial Hypotension: Causes, Symptoms, and Treatments.
- American Heart Association. (2024). Understanding Low Blood Pressure and its Management.
- Jansen, P. A., et al. (1995). Contribution of inappropriate vasopressin secretion to the hyponatremia caused by beer potomania. American Journal of Medicine.








