Understanding the correct blood test fasting rules is fundamental to ensuring your lab results are accurate and provide a true picture of your health. Fasting typically involves abstaining from all food and most drinks for a specific period, usually 8 to 12 hours, to create a stable baseline for measuring key health markers. This comprehensive guide provides a clear “fast by test” reference, a practical prep checklist, and expert advice on what to do if you accidentally break your fast.
Table of Contents
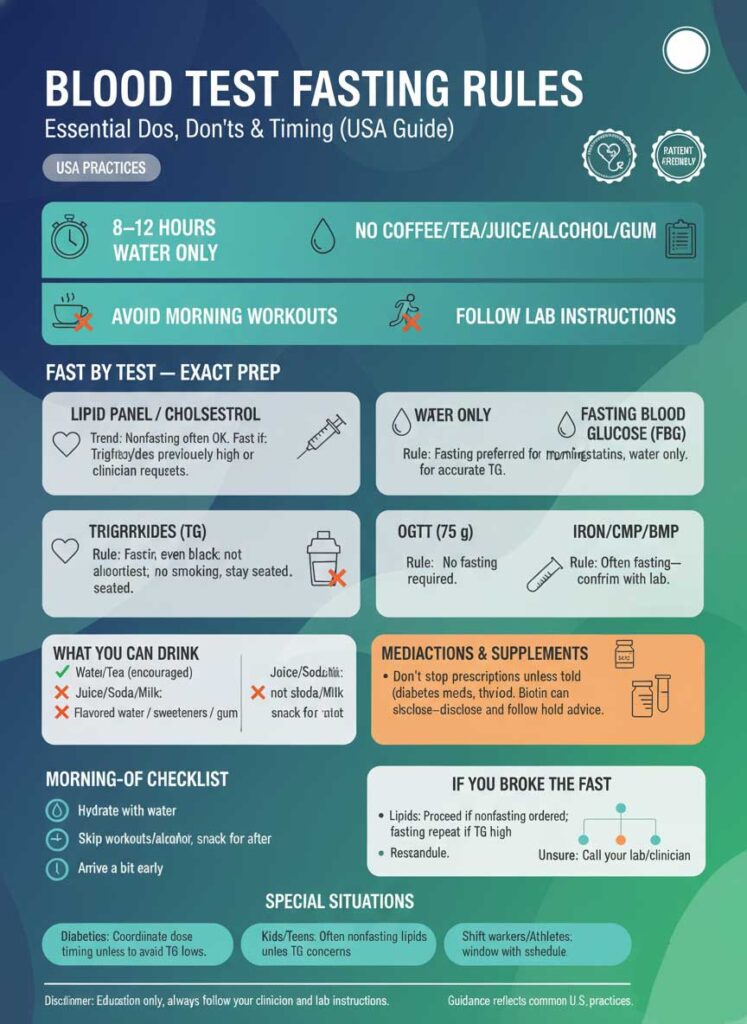
While the medical community in the USA is increasingly adopting nonfasting lipid panels for routine screening, it’s crucial to recognize that many vital tests still demand strict adherence to these rules. Getting the preparation right prevents the need for re-testing, saves you time, and gives your healthcare provider the reliable data they need to guide your care.
What is the Difference Between Fasting and Non-Fasting Tests?
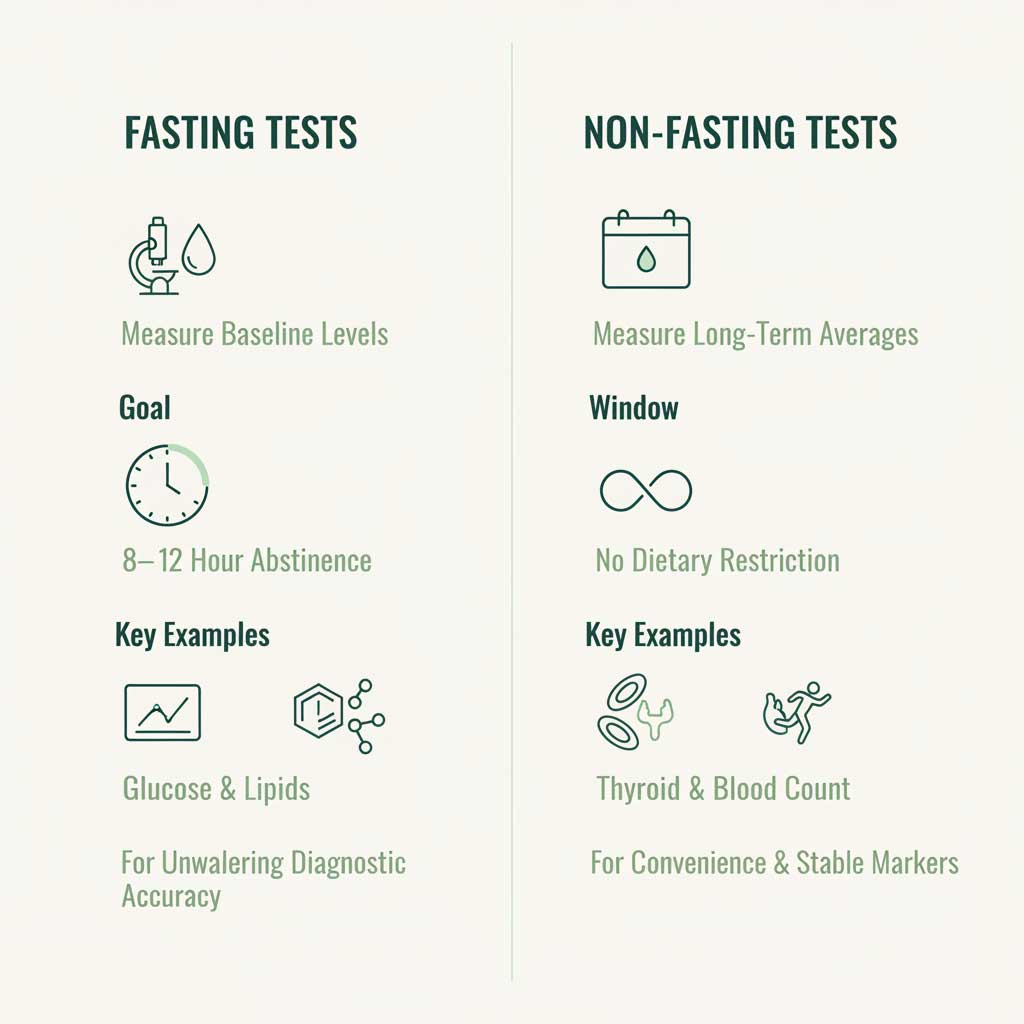
| Feature | Fasting Tests | Non-Fasting Tests |
| Primary Goal | Measure baseline levels without influence from recent meals. | Measure analytes unaffected by food or assess long-term averages. |
| Typical Window | 8–12 hours of no food, water only. | No specific dietary restrictions are required before the test. |
| Key Examples | Fasting Blood Glucose, OGTT, Triglyceride-focused panels. | HbA1c, Complete Blood Count (CBC), Kidney Function, Thyroid (TSH). |
| Why It’s Done | To accurately diagnose conditions like diabetes or hypertriglyceridemia. | For convenience and to measure markers that remain stable regardless of meals. |
Core Concept & Definitions
To properly follow blood test fasting rules, it’s essential to understand exactly what the term “fasting” means in a medical context and why this simple act is so critical for accuracy.
What “fasting” means in medical testing
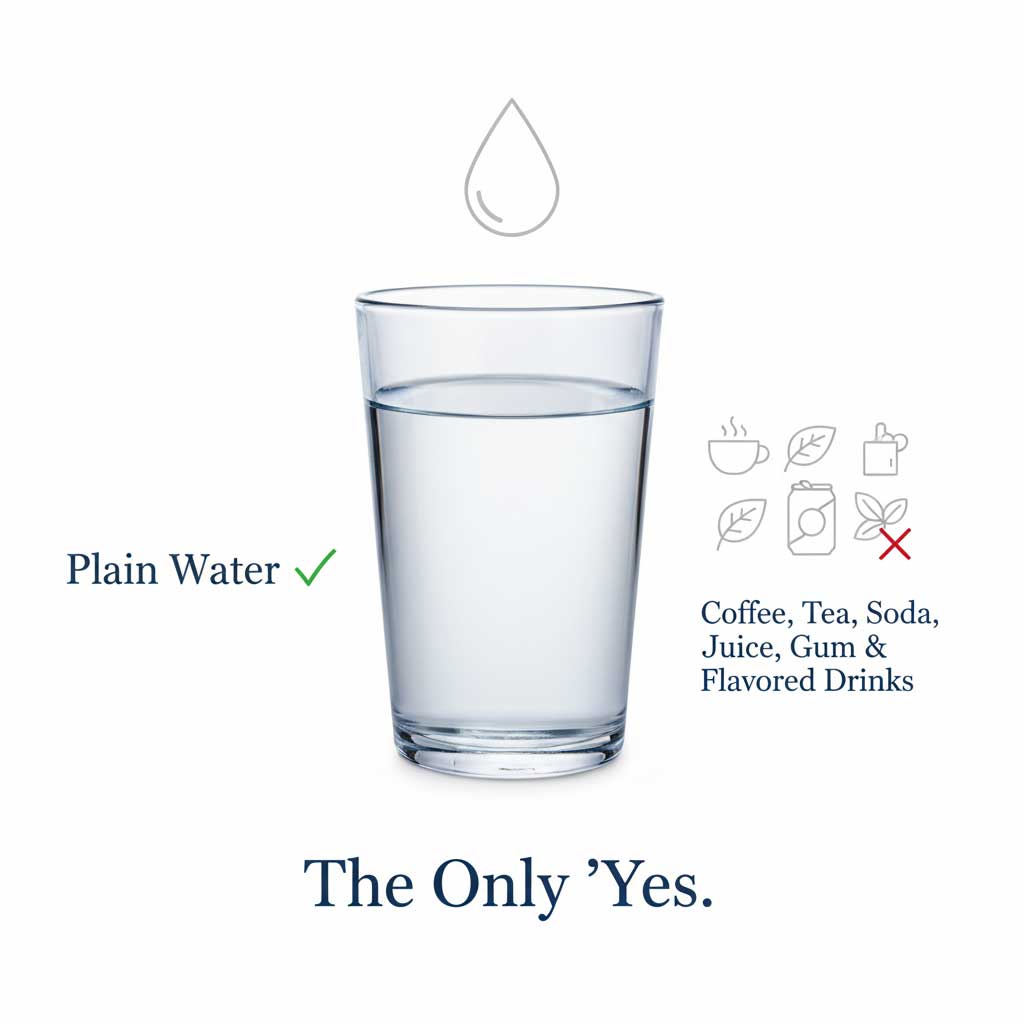
In a clinical setting, “fasting” refers to a water-only fast. This means you must abstain from all food and beverages, with the sole exception of plain water, for a designated period before your blood is drawn. This is not about total calorie restriction for a day; it’s a timed window of abstinence.
Confusion often arises from grey areas, but the rules are strict for a reason. Items like black coffee, tea, flavored water, and chewing gum are not permitted. Even without sugar, they contain compounds that can stimulate your digestive system, alter hormone levels, or affect blood chemistry, thereby breaking the fast and compromising your results.
Quick Glossary of Common Fasting-Related Terms:
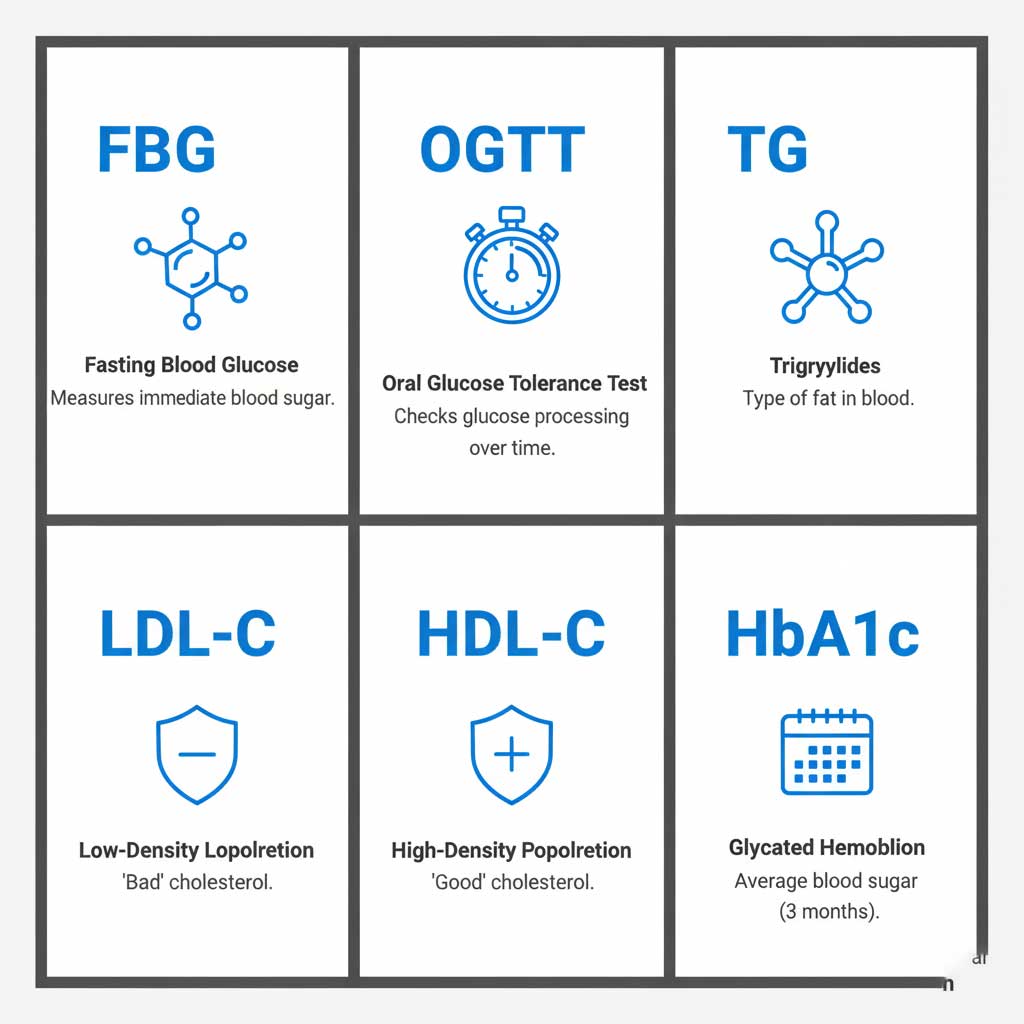
- FBG (Fasting Blood Glucose): Measures the amount of sugar in your blood after an overnight fast to screen for diabetes or prediabetes.
- OGTT (Oral Glucose Tolerance Test): A timed test that measures your body’s response to a specific amount of sugar, used to diagnose gestational diabetes and type 2 diabetes.
- Lipid Panel: A group of tests that measure fats in the blood, including total cholesterol, LDL-C, HDL-C, and triglycerides.
- TG (Triglycerides): A type of fat in your blood that is highly sensitive to recent food intake.
- LDL-C (Low-Density Lipoprotein Cholesterol): Often called “bad” cholesterol. Its level can be calculated based on other lipids, a calculation that is more accurate in a fasting state.
- HDL-C (High-Density Lipoprotein Cholesterol): Known as “good” cholesterol.
- HbA1c (Hemoglobin A1c): Measures your average blood sugar over the past 2–3 months. Critically, this test does not require fasting.
Why fasting matters for accuracy
The food and drinks you consume are broken down into sugars, fats, proteins, and other nutrients that are absorbed directly into your bloodstream. This natural process can temporarily—but significantly—alter the levels of substances that your blood test is designed to measure.
Fasting ensures that your clinician is looking at your body’s baseline state, free from the immediate influence of your last meal. Here’s how recent intake affects key tests:
- Post-prandial lipemia: After you eat, particularly a meal high in fat, your blood’s triglyceride levels spike. This can make the plasma appear milky and directly inflates your TG measurement. High TGs can also interfere with the calculation used to determine your LDL-C level, a key marker for heart disease risk.
- Glucose Spikes: Carbohydrates are converted to glucose, causing your blood sugar to rise. A fasting blood glucose test needs to measure your sugar level when it’s stable, providing a clear view of how your body manages glucose without the immediate influence of food.
- Analyte Fluctuation: Other markers, such as iron and certain components of a comprehensive metabolic panel (CMP), can also fluctuate after a meal. Fasting provides a more consistent and reliable measurement.
For most fasting blood tests, you must fast for 8–12 hours. During this fasting window, you should adhere to these essential rules:

- Drink only plain water.
- Do not consume food, coffee, tea, soda, or alcohol.
- Avoid chewing gum and mints.
- Refrain from vigorous morning exercise before your blood draw.
- Always follow the specific instructions provided by your healthcare provider or the laboratory.
Fast by Test: Exact Dos, Don’ts & Timing
Different tests have different requirements. While the trend for a routine fasting for cholesterol test is shifting, other tests remain rigidly structured. Here is your authoritative guide to the most common labs.
Lipid Panel / Cholesterol (LDL, HDL, TG)
The rules for a fasting for lipid panel have evolved. While non-fasting tests are increasingly acceptable for general screening, there are key situations where fasting is still required.
- When Fasting Still Matters: Your doctor will almost certainly order a fasting test if you have a history of high triglycerides (e.g., over 400 mg/dL), if they are diagnosing a complex lipid disorder, or before starting certain medications that can affect lipids. The fasting vs nonfasting debate often ends when triglycerides are the primary concern.
- When Nonfasting Is Okay: For routine cardiovascular risk screening in many adults, a nonfasting lipid panel provides sufficient accuracy for HDL-C and total cholesterol. Most modern labs can also directly measure or reliably estimate LDL-C in a nonfasting state unless triglycerides are very high.
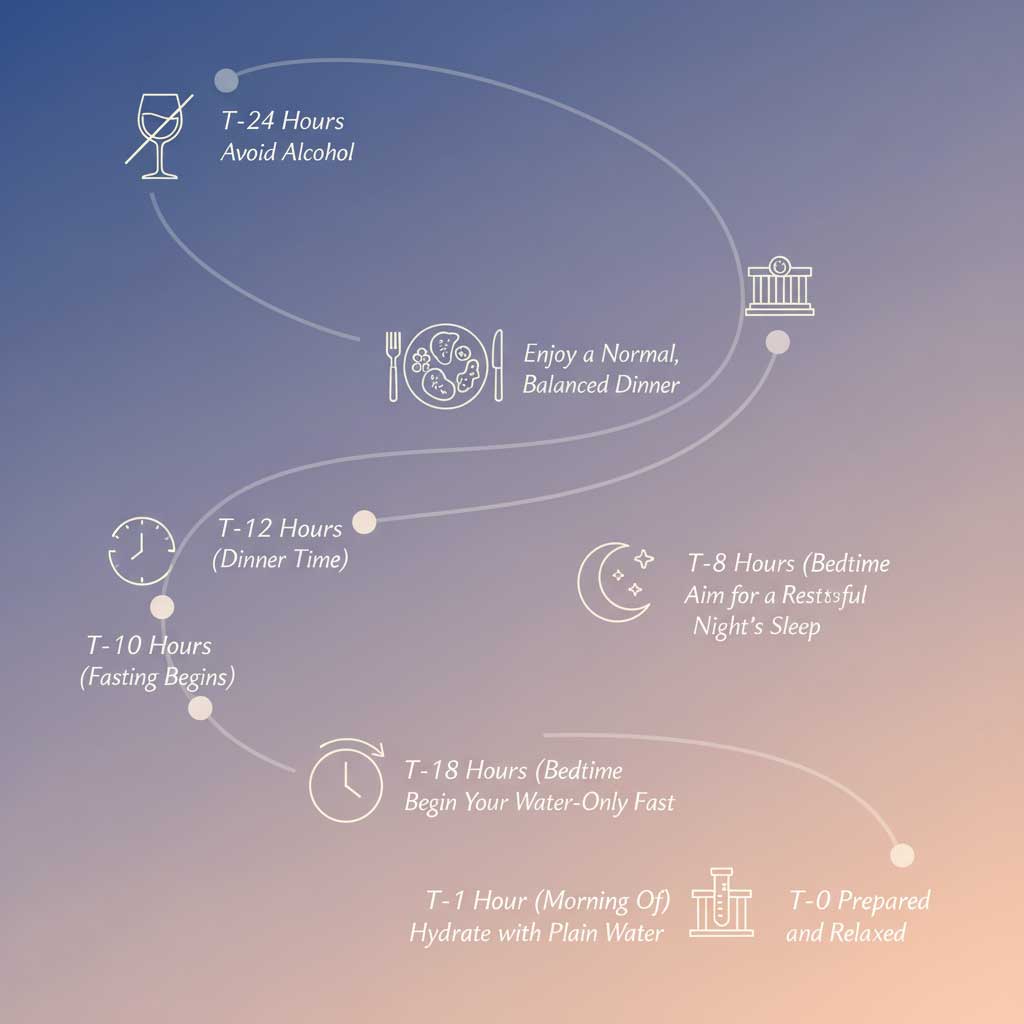
- Dos: Schedule a morning appointment to make fasting easier. Stay well-hydrated with water.
- Don’ts: Avoid alcohol for 24 hours and skip high-fat meals the night before. Do not drink coffee or tea, even if black.
- If You Accidentally Ate: Call the lab. If a nonfasting test was ordered, you can likely proceed. If a fasting test was required, they might still draw your blood and note the nonfasting status, but expect your doctor to order a repeat fasting test if your triglycerides are high.
Triglycerides-Focused Testing
Knowing how long to fast before a triglyceride test is crucial because this marker is the most volatile. TGs can skyrocket after a meal, making a nonfasting result difficult to interpret.
If your doctor’s primary goal is to assess your triglyceride level, a 10–12 hour fast is standard practice. You should follow this rule strictly if prior TG were high on a nonfasting test, as the follow-up fasting result is needed to confirm the diagnosis and guide treatment.
Fasting Blood Glucose (FBG)
The required fasting blood glucose test hours are a minimum of 8 hours. This ensures that the measured glucose level reflects your body’s baseline and not the sugar from your last meal.
For the most accurate results, schedule your FBG test in the morning. This aligns with your body’s natural overnight fast and reduces variability from daily hormonal cycles. Late-night snacks and alcohol can artificially raise your morning glucose, so avoid them the night before. Comparing fasting blood glucose vs HbA1c, the FBG is a snapshot, while the HbA1c is a long-term average that doesn’t require fasting.
Oral Glucose Tolerance Test (OGTT, 75 g)
The fasting for glucose tolerance test (OGTT) has the most rigid protocol. Adherence to the OGTT preparation rules and timing is not optional.
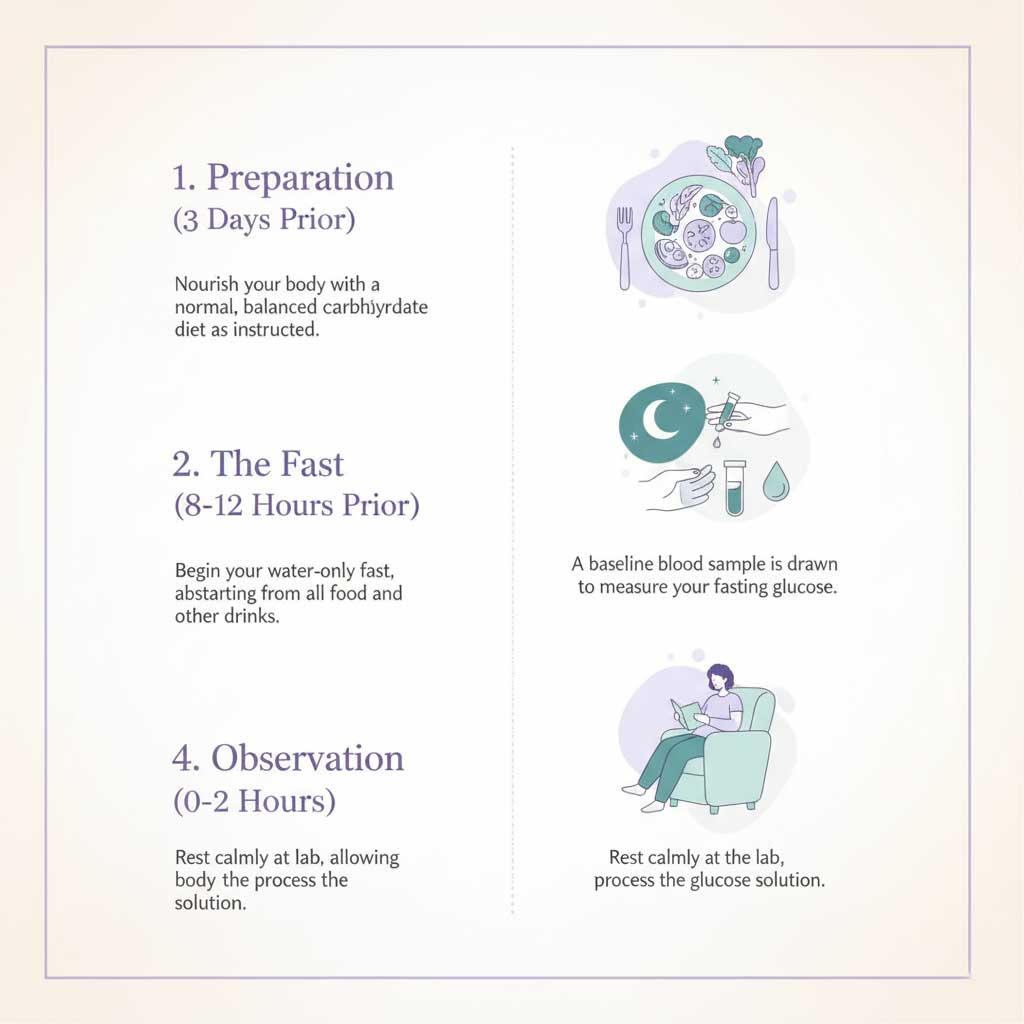
- Preparation: For three days leading up to the test, you must eat a normal diet containing at least 150 grams of carbohydrates per day to ensure your body is primed to process sugar correctly.
- Fasting: A strict 8–12 hour fast is required before your appointment.
- Test Day Protocol: After an initial fasting blood draw, you’ll drink a 75-gram glucose solution. You must then remain at the lab, seated, for the duration of the test (usually two hours). You cannot eat, smoke, or engage in any physical activity, as these can alter your results.
HbA1c (No Fasting)
The HbA1c test is the exception to the rule when it comes to glucose testing. Since it measures the average amount of glucose attached to your red blood cells over the past 2–3 months, a recent meal has no impact. This convenience is why the fasting blood sugar vs HbA1c: which test needs fasting debate is easily settled—only the FBG requires it.
Iron Studies / Metabolic Panels (CMP/BMP)
While not always mandatory, your clinician may still ask you to fast before a Comprehensive Metabolic Panel (CMP), Basic Metabolic Panel (BMP), or iron studies. This is because certain analytes on these panels, like glucose and iron, can shift after a meal. Fasting provides a standardized baseline, making results more consistent over time. Always ask your lab or clinician if fasting is required for your specific panel.
What You Can Drink (and Why It Matters)
One of the most frequent questions is what to drink before a fasting blood test. The answer is simple, but the reasons are important.
Water vs. Coffee/Tea/Flavored Drinks
Plain water is the only beverage universally allowed during a medical fast. In fact, it’s encouraged. Any other drink, even if it has zero calories, can potentially interfere with your results.
- Water Only: Water is essential for hydration and does not affect baseline measurements for glucose, lipids, or other common analytes.
- Coffee and Tea Are Not Allowed: The question of coffee before blood test fasting is a common pitfall. Even black, unsweetened coffee is not permitted. Caffeine can stimulate your adrenal glands, which may affect your glucose and insulin levels.
- Flavored Water and Gum: Avoid these completely. Artificial sweeteners, flavorings, and even the act of chewing gum can trigger digestive responses that technically break your fast. Does flavored water or chewing gum break a medical fast? Yes, it is safest to assume they do.
Hydration & Easier Blood Draws
Proper hydration and easier blood draw success go hand-in-hand. When you are well-hydrated, your veins are plumper and more accessible, making the phlebotomist’s job easier and the experience more comfortable for you.
Dehydration can cause veins to flatten or constrict, leading to a more difficult and potentially painful draw. Drinking a good amount of water the day before and a glass or two the morning of your test is a simple and effective preparation step.
Medications & Supplements: Safety and Accuracy
Navigating medications and fasting blood tests requires clear communication with your healthcare provider to ensure both your safety and the accuracy of your results.
Prescription Meds: Take or Hold?
Never stop taking a prescribed medication unless you are explicitly told to do so by your doctor. Most medications can and should be taken as scheduled with a small amount of plain water. However, you must confirm this for your specific situation.
- Diabetes Medications: This is the most critical category. Your provider will give you specific instructions on how to adjust insulin or oral medications to prevent hypoglycemia (low blood sugar) during your fast. These are crucial fasting rules for diabetics to avoid low blood sugar.
- Statins and Thyroid Meds: The question of whether to take thyroid, statins, and other meds timing before labs is common. Generally, these are taken as usual. Thyroid medication, for instance, is often taken first thing in the morning and is perfectly fine to take with water before a fasting test. However, always confirm.
Biotin & Supplement Interference (Hidden Pitfalls)
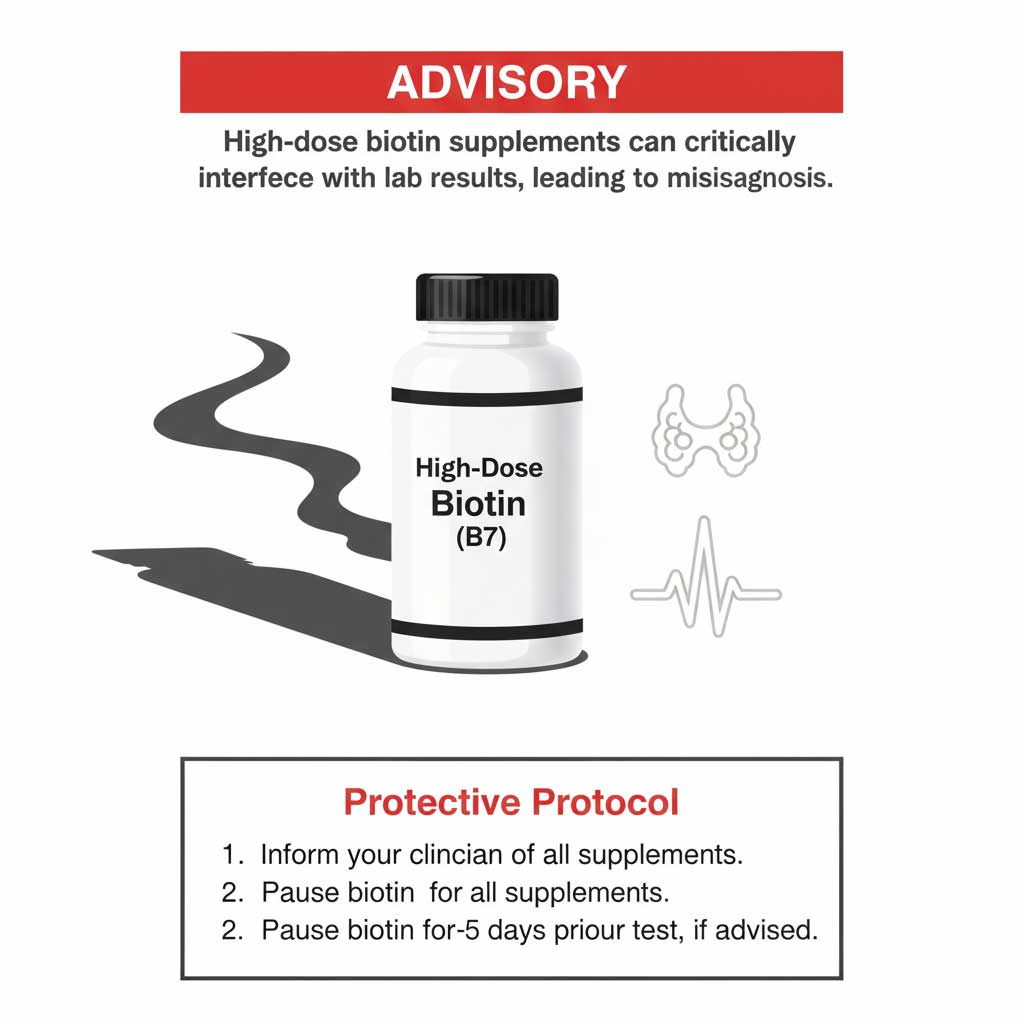
A significant and often overlooked issue is biotin/supplement interference with lab assays. High-dose biotin (Vitamin B7), commonly found in supplements for hair, skin, and nail health, can cause profoundly inaccurate results for numerous tests.
It can create falsely low results for troponin (a heart attack marker) and falsely high or low results for thyroid hormone tests (TSH, T3, T4). If you take a supplement with biotin, especially in doses over 1,000 mcg, you must inform your doctor. They will likely advise you to stop taking it for 3 to 5 days before your blood draw.
Behavior Factors That Skew Results
Your actions in the 24 hours leading up to a blood test can influence the outcome. Understanding the effects of exercise, alcohol, smoking effects on lab values helps ensure your results reflect your true baseline health.
Alcohol, Exercise, Smoking, and Sleep
- Alcohol: Avoid alcohol for at least 24 hours before your test. It can significantly raise triglyceride levels and may also impact glucose and liver function tests.
- Exercise: Postpone any vigorous morning exercise. Strenuous physical activity can temporarily increase cholesterol levels, inflammatory markers, and certain enzymes.
- Smoking: Nicotine can affect blood sugar levels and other markers. It is strictly forbidden before and during an OGTT and best avoided before any blood test.
- Sleep: Lack of quality sleep can impact hormones that regulate glucose, potentially affecting FBG results. Aim for a normal night’s rest.
Morning Scheduling & Logistics
Choosing a morning appointment for fasting labs is a simple but effective strategy. It capitalizes on your natural overnight fast, making adherence much easier.
- Bring a Post-Draw Snack: Pack a healthy snack (like nuts, a protein bar, or fruit) and a beverage to have immediately after your test to stabilize your blood sugar.
- Arrange Transportation if Needed: If you are prone to feeling lightheaded or dizzy while fasting, especially for longer tests like the OGTT, consider having someone drive you.
- Best Time of Day: The best time of day for fasting blood work for accurate results is as early in the morning as your schedule allows, minimizing the fasting duration while you’re awake.
If You Broke the Fast: Exactly What to Do
Knowing what to do if I ate before my fasting blood test can save you a trip to the lab. The correct action depends entirely on the test you were scheduled for.
Decision Flow by Test
- Fasting Blood Glucose (FBG) or OGTT: You must call and reschedule your appointment. The results would be invalid, and proceeding is a waste of your time and resources.
- Lipid Panel / Cholesterol Test: Call the lab or your doctor’s office. If your order allows for a nonfasting panel, you may be able to proceed. However, be prepared for a potential follow-up fasting test if your triglycerides are very high.
- Other Fasting Tests (Iron, etc.): Call the lab for guidance. They will advise you based on the specific markers being measured and their sensitivity to food intake. Do not simply show up and hope for the best.

Special Populations & Edge Cases
Standard fasting rules apply to most people, but certain conditions and lifestyles require special considerations to ensure safety and accuracy.
Diabetics (Insulin or Sulfonylureas)
For individuals with diabetes, safety is paramount. Diabetic fasting protocols must be carefully managed with a healthcare provider to prevent hypoglycemia.
Your doctor will provide specific instructions on adjusting your insulin or oral medication doses. Schedule the earliest possible morning appointment to minimize the fasting period. Always carry a source of fast-acting glucose to consume immediately after your blood draw.
Children & Teens (Pediatric Lipids)
Pediatric/teen lipid screening fasting guidance has shifted significantly. To improve compliance, major health organizations now recommend nonfasting lipid panels for routine cholesterol screening in youth. A fasting test is typically reserved as a follow-up if the nonfasting results show elevated triglycerides or other abnormalities.
Shift Workers, Athletes, and Intermittent Fasters
If your schedule is not a typical 9-to-5, you can still follow fasting rules effectively.
- Shift Workers: Align the 8–12 hour fast with your main sleep period. If you work overnight and sleep during the day, you would fast during your sleep and schedule an evening blood draw before your first “meal.”
- Athletes: Avoid intense training sessions during the fasting window and on the morning of your test.
- Intermittent Fasters: Schedule your blood draw to coincide with the end of your usual fasting window for maximum convenience.
Fasting vs. Nonfasting by Test: A Detailed Comparison
This table provides a clear breakdown of fasting requirements for common blood tests, helping you understand the “why” behind each rule.
| Test/Panel | Typical Requirement | Why Fasting Matters | When Nonfasting Is Acceptable | If You Ate By Mistake |
| Lipid Panel (LDL, HDL, TG) | Often nonfasting; fasting if TG high | Meals raise TG, can alter LDL-C calculation. | Routine screening without known TG concerns. | Proceed; expect repeat fasting if TG is high. |
| Triglycerides (focus) | Fasting preferred (10–12 hours) | Post-meal TG spikes are significant and can mask the true baseline. | Rarely acceptable unless specified by a clinician. | Reschedule or expect a fasting repeat order. |
| Fasting Blood Glucose (FBG) | ≥8 hours fasting | Meals directly raise glucose, invalidating the baseline measurement. | Not applicable for this test. | Reschedule the test. |
| OGTT (75 g) | Strict 8–12 hour fast | Meals or exertion before or during the test will alter the glucose curve. | Not applicable for this test. | Reschedule the test. |
| HbA1c | No fasting | Measures a 2–3 month average, unaffected by recent food intake. | Always acceptable. | Proceed with the test. |
| Iron Studies / CMP/BMP | Often fasting, per lab/provider | Some analytes (glucose, iron) shift post-meal, affecting consistency. | Case-dependent; many panels can be nonfasting. | Call the lab/clinician for instructions. |
Summary & Key Takeaways
Adhering to the correct blood test fasting rules is a simple yet powerful way to ensure the quality and accuracy of your health data. For most tests, this means an 8–12 hour fast with water only. However, the modern approach is nuanced, with non-fasting lipid panels becoming more common for routine screening.
Always prioritize the specific instructions from your healthcare provider. When in doubt, a quick phone call to the lab can prevent confusion and the need for a repeat visit.
- DO confirm the specific fasting window required for your test (e.g., 8, 10, or 12 hours).
- DON’T consume anything other than plain water, including black coffee, tea, or gum.
- DO ask your provider for precise instructions on taking or holding your medications.
- DON’T perform strenuous exercise or drink alcohol in the 24 hours before your test.
- DO reschedule immediately if you accidentally break your fast for a glucose-related test.
Frequently Asked Questions (FAQ)
How many hours should I fast before a cholesterol test in the USA?
For routine cholesterol screening, many labs no longer require fasting. However, if your doctor is specifically monitoring high triglycerides or performing a diagnostic workup, a fast of 8 to 12 hours is standard. Always follow the instructions on your lab order.
What is the difference between a fasting blood sugar test and an HbA1c test?

A fasting blood sugar (FBG) test measures your glucose level at a single point in time after an 8-hour fast. An HbA1c test requires no fasting and measures your average blood sugar control over the last 2 to 3 months. Both are used to screen for and manage diabetes.
What are the specific OGTT fasting time and what should I expect step by step?

You must fast for 8 to 12 hours before your OGTT appointment. Step 1: A baseline blood sample is drawn. Step 2: You drink a 75-gram glucose beverage. Step 3: You must remain seated at the lab for 2 hours, with additional blood draws typically at the 1-hour and 2-hour marks.
Is black coffee okay during fasting for blood work?
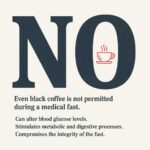
No, black coffee is not okay. Caffeine can affect your blood glucose levels and stimulate your metabolism, which technically breaks the fast and can interfere with the accuracy of your results. Stick to plain water only.
Should I take my thyroid or statin meds before fasting labs?

Generally, yes. You should take your usual medications with a small amount of plain water unless your doctor explicitly instructs you otherwise. Always confirm with your provider to be certain.
I accidentally ate before my fasting blood test—what should I do?

If the test was for fasting glucose (FBG) or an OGTT, you must call and reschedule. If it was for a lipid panel, call the lab. They may advise you to proceed and will note it on the report, but you may need a repeat fasting test later if triglycerides are high.
Do fasting rules for diabetics differ to avoid low blood sugar?

Yes, and safety is the top priority. Your doctor will give you specific instructions on how to adjust your insulin or other diabetes medications on the morning of the fast to prevent hypoglycemia. Schedule the earliest possible appointment.
Why does my lab still require fasting for cholesterol if many guidelines say it’s not needed?

Many labs maintain fasting as a default policy to ensure standardization. A fasting sample provides a cleaner, more consistent baseline, which is especially useful for comparing results over time. It eliminates the variable of what a patient may have eaten right before the test.









