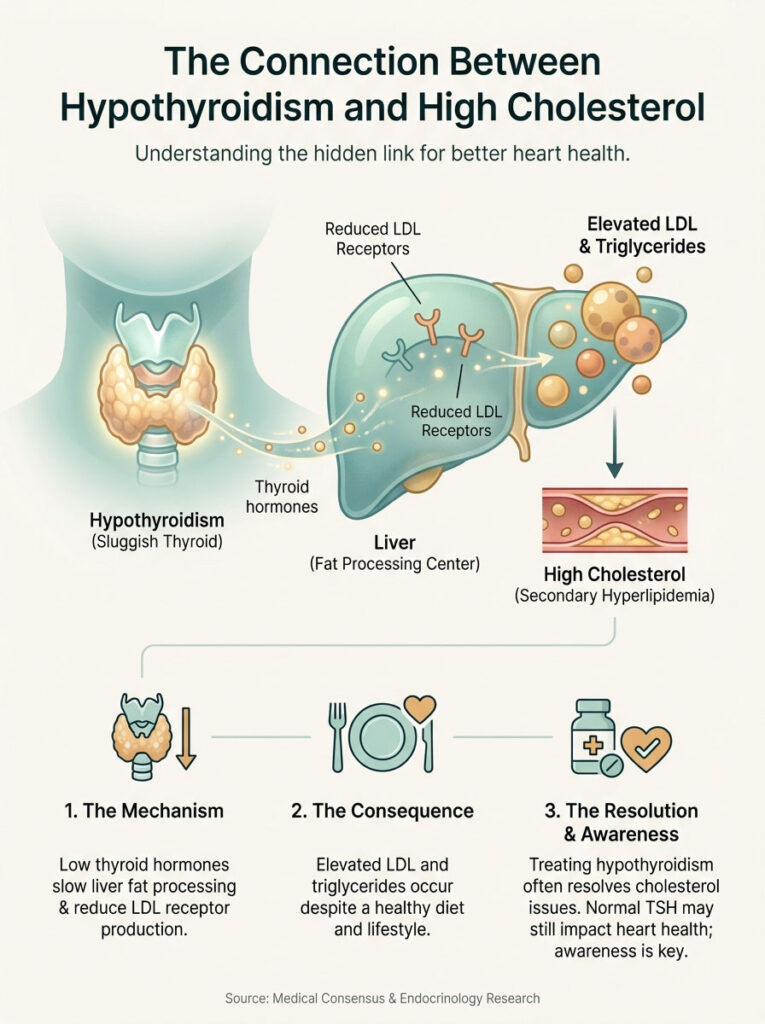
Yes, can hypothyroidism cause high cholesterol? Absolutely. It is a leading cause of secondary hyperlipidemia. Thyroid hormone regulates the liver’s ability to process fats. When thyroid levels are low, the liver produces fewer LDL receptors. This means it cannot clear “bad” cholesterol from the blood effectively. The result is elevated LDL and triglycerides, regardless of how healthy your diet is. Treating the thyroid usually resolves the cholesterol imbalance without the immediate need for statins.
Table of Contents
Picture a patient I see in my clinic almost every week. Let’s call her Sarah. She is thirty-four years old. She adheres to a strict Mediterranean diet. She exercises four times a week. Her BMI is a healthy 23. Yet, her primary care physician just referred her to endocrinology. Why? Because her LDL cholesterol is stubbornly sitting at 170 mg/dL.
She is frustrated. She is confused. She is worried about starting statin therapy at such a young age. The first question she asks is usually, “I’m doing everything right, so why are my numbers so wrong?”
The answer often lies not in what she is eating. It lies in how her body is metabolizing it. The critical question we must ask is: Can hypothyroidism cause high cholesterol? The answer is an emphatic yes. In fact, hypothyroidism is one of the most common causes of secondary hyperlipidemia. This is high cholesterol caused by an underlying medical condition rather than lifestyle alone.
Millions of Americans are currently managing high lipid profiles with statins. Many are unaware that the root cause might be a sluggish thyroid. In this comprehensive guide, we will examine the physiological mechanism connecting the thyroid gland to liver function. We will explain why “normal” TSH levels might still affect your heart health. We will also outline the medical protocols for treating the thyroid to resolve lipid imbalances.
The Biological Mechanism: How the Thyroid Governs Lipid Metabolism
To understand the link between your neck (thyroid) and your heart, we have to look at the liver. The liver is the engine room for cholesterol clearance. Specifically, we are looking at the hepatocytes, or liver cells. These cells are responsible for pulling Low-Density Lipoprotein (LDL) particles out of the bloodstream. They break them down and excrete them.
But the liver needs a signal to do this work. That signal comes from the thyroid.
The LDL Receptor Connection
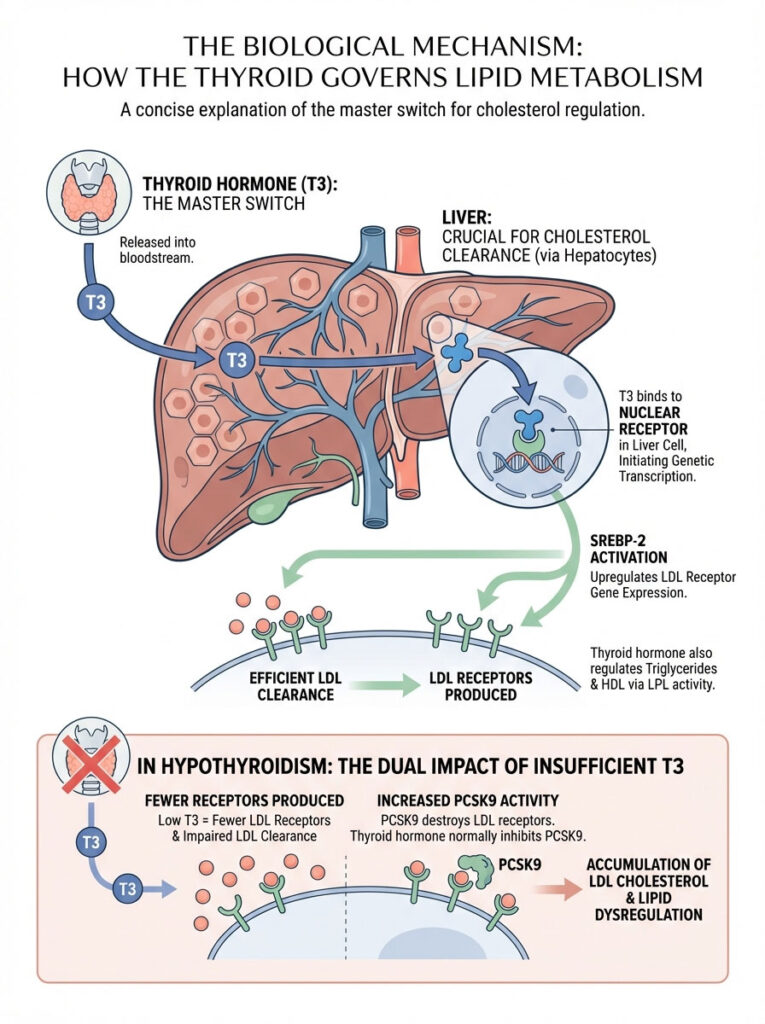
Thyroid hormone acts as a master switch for cholesterol regulation. We are specifically talking about the active form known as Triiodothyronine (T3). T3 binds to specific nuclear receptors on the surface of liver cells. This binding initiates a complex genetic transcription process.
Here is what happens at the cellular level:
When T3 binds effectively, it upregulates the expression of the LDL Receptor (LDL-R) gene. This is often mediated by a protein called SREBP-2 (Sterol Regulatory Element-Binding Protein 2). Simply put, thyroid hormone tells your liver to build more “docks” (receptors). These docks catch the floating LDL particles from your blood.
The Downregulation Effect
When you have hypothyroidism, T3 levels are insufficient. Without that signal, the SREBP-2 pathway is not activated. The liver produces significantly fewer LDL receptors. This is the core mechanism of the problem.
You might have a perfectly healthy diet. You might avoid all trans fats. But if your liver lacks the receptors to clear LDL, those particles remain circulating in the bloodstream. They oxidize and eventually form plaque in the arteries. This is why lifestyle changes often fail in hypothyroid patients.
Endocrinologist Insight: We often see patients whose cholesterol is “resistant” to diet changes. This is a classic sign of receptor downregulation. If the liver cannot physically grab the LDL due to low thyroid hormone, cutting dietary fat will have a negligible effect on serum levels.
Beyond LDL: Triglycerides and HDL
The impact of thyroid dysfunction extends beyond just LDL. Thyroid hormone also regulates the activity of an enzyme called Lipoprotein Lipase (LPL). LPL is responsible for clearing triglycerides from the blood. It breaks them down into free fatty acids for energy.
In a hypothyroid state, LPL activity is suppressed. This leads to higher triglyceride levels. This is dangerous because high triglycerides can thicken the blood and increase stroke risk.
Additionally, we see changes in CETP (Cholesteryl Ester Transfer Protein) activity. This can sometimes lead to artificially elevated HDL (the “good” cholesterol). However, do not be fooled. In hypothyroid patients, these HDL particles are often dysfunctional. They are less effective at reverse cholesterol transport, meaning they don’t clean the arteries as well as they should.
Deep Dive: The Role of PCSK9
Recent research has identified another culprit: PCSK9 (Proprotein Convertase Subtilisin/Kexin type 9). This protein destroys LDL receptors. Studies suggest that thyroid hormone naturally inhibits PCSK9.
Therefore, when thyroid levels drop, PCSK9 levels may rise. This leads to the destruction of the few LDL receptors the liver actually managed to produce. This creates a “double hit” on the liver’s ability to clear fats. It stops making new receptors, and the existing ones are destroyed.
The Evidence: Analyzing the Data
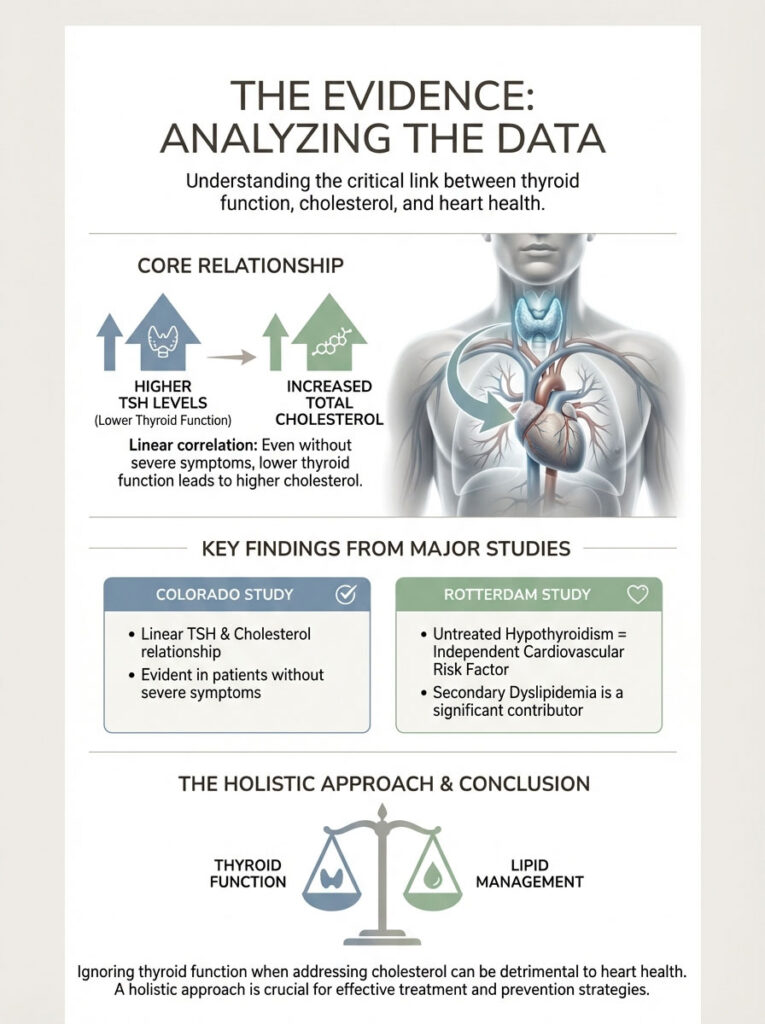
The correlation between thyroid function and lipid health is not merely theoretical. It is backed by decades of data. One of the most significant pieces of research in this field is the Colorado Thyroid Disease Prevalence Study.
Key Statistics: The Thyroid-Heart Connection
- 13% of patients with newly diagnosed high cholesterol have underlying thyroid pathology.
- TSH > 10 mIU/L is associated with a significantly higher prevalence of hypercholesterolemia.
- Treating hypothyroidism can reduce serum cholesterol levels by 20% to 30% without statins.
- Subclinical Hypothyroidism affects up to 10% of the adult female population.
- Hypothyroidism is more common in women, who are also more likely to be treated for high cholesterol later in life.
The Colorado study demonstrated a linear relationship. As TSH levels rose (indicating lower thyroid function), Total Cholesterol levels rose in tandem. This trend was visible even in patients who did not fit the classic picture of severe hypothyroidism.
Similarly, the Rotterdam Study analyzed the progression of atherosclerosis (hardening of the arteries) in hypothyroid subjects. The findings were stark. They indicated that untreated hypothyroidism is an independent risk factor for cardiovascular events. This risk is largely driven by this secondary dyslipidemia.
The data tells us a clear story. Ignoring the thyroid when treating cholesterol is like ignoring a fire alarm while trying to fan away the smoke.
Subclinical Hypothyroidism: The “Grey Area” of Heart Health
Clinical hypothyroidism (overt disease) is easy to diagnose. TSH is very high, and T4 is very low. However, a more insidious issue is Subclinical Hypothyroidism (SCH). This condition is defined by an elevated TSH (typically 4.5–10 mIU/L) but with normal Free T4 levels.
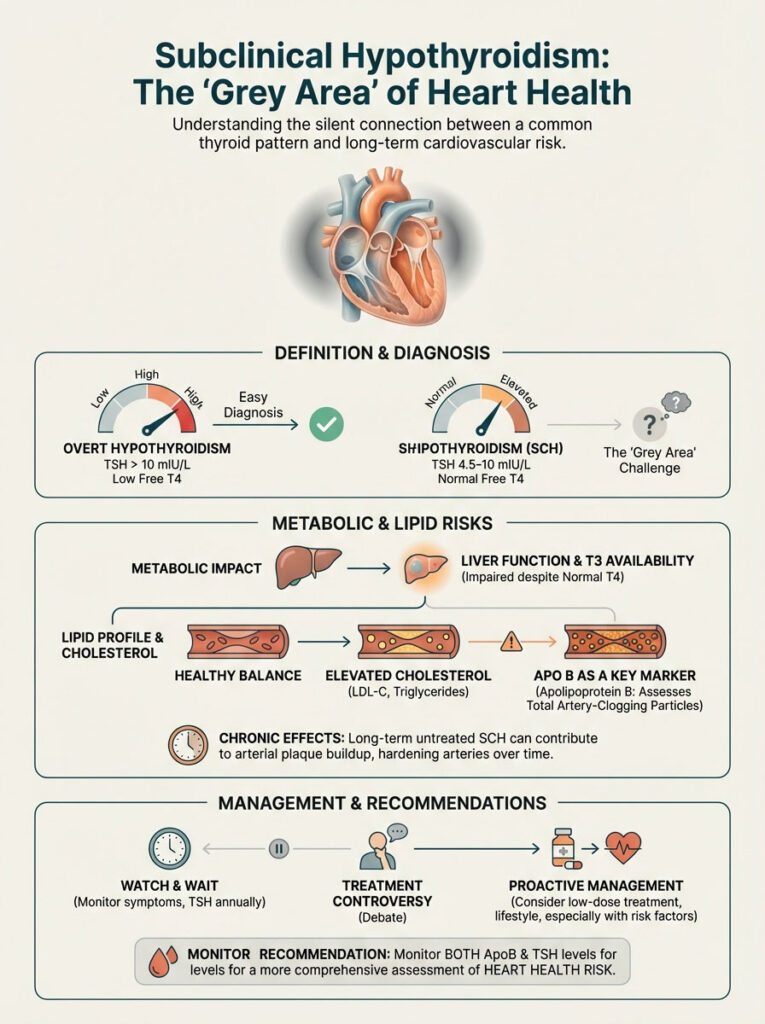
The Controversy
There is ongoing debate in the medical community regarding when to treat SCH. Some practitioners prefer a “watch and wait” approach. They argue that if the T4 is normal, the body is coping.
However, from a metabolic standpoint, waiting can be dangerous. The liver appears to be one of the most sensitive organs to slight drops in thyroid function. While the brain might be satisfied with the T4 levels, the liver might be starving for T3.
The Lipid Impact
Does subclinical hypothyroidism cause high cholesterol? The evidence suggests it does. Even when T4 levels appear normal on a lab report, the tissue-level availability of T3 in the liver may be compromised.
This leads to the same LDL receptor downregulation discussed earlier. It happens to a lesser degree than in overt disease, but it is chronic. Over 10 or 20 years, this slight elevation in cholesterol accumulates damage in the arteries.
Risk Stratification and ApoB
In my practice, I look beyond standard LDL when evaluating SCH patients. We look at ApoB (Apolipoprotein B). ApoB is a protein found on all atherogenic (plaque-causing) particles.
Subclinical hypothyroidism is specifically linked to higher ApoB levels. Many cardiologists now agree this is a more accurate predictor of heart disease than LDL cholesterol alone. If your TSH is 5.5 and your ApoB is high, “watching and waiting” is likely not the best strategy.
Comparison: Primary vs. Secondary Hyperlipidemia
Distinguishing between genetic high cholesterol (Familial Hypercholesterolemia or Primary) and thyroid-induced (Secondary) cholesterol is vital. It dictates the treatment plan. If we treat secondary hyperlipidemia with statins while ignoring the thyroid, we are merely putting a band-aid on a bullet wound.
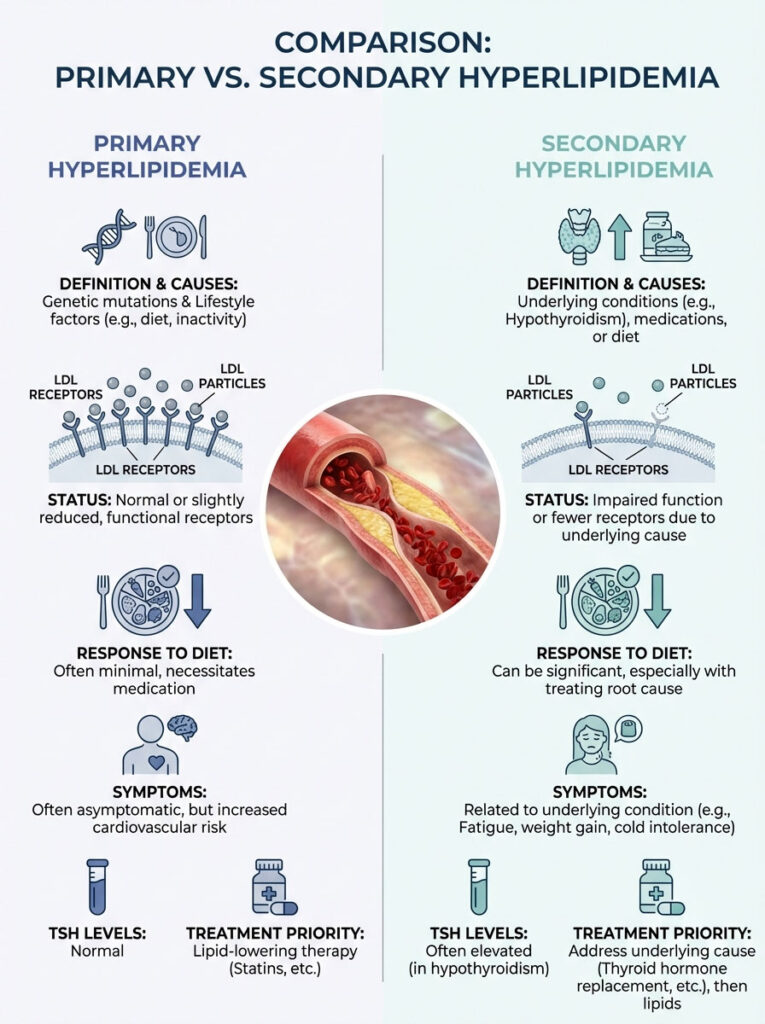
The table below outlines how we differentiate these conditions clinically.
| Feature | Primary Hyperlipidemia (Genetic/Lifestyle) | Secondary Hyperlipidemia (Hypothyroid-Induced) |
|---|---|---|
| Primary Cause | Genetics (PCSK9/LDL-R mutations), Diet, Sedentary Lifestyle | Low Thyroid Hormone (T3/T4) availability |
| LDL Receptor Status | Defective (Genetic) or Saturated | Downregulated due to lack of hormonal signal |
| Response to Diet | Moderate to High | Poor / Resistant |
| Associated Symptoms | Often Asymptomatic | Fatigue, Cold Intolerance, Weight Gain, Dry Skin, Hair Loss |
| TSH Level | Normal (0.4 – 4.0 mIU/L) | Elevated (> 4.5 mIU/L) |
| Treatment Priority | Statin Therapy / Lifestyle Modification | Thyroid Hormone Replacement (Levothyroxine) |
Understanding this distinction saves lives. It also prevents unnecessary medication side effects. Why take a drug for a genetic condition if your issue is hormonal?
The Diagnostic Protocol: What to Ask Your Doctor
If you are wondering, “Can hypothyroidism cause high cholesterol in my specific case?”, you need the right data. A standard annual physical often misses the connection. This is because the screening is too superficial.
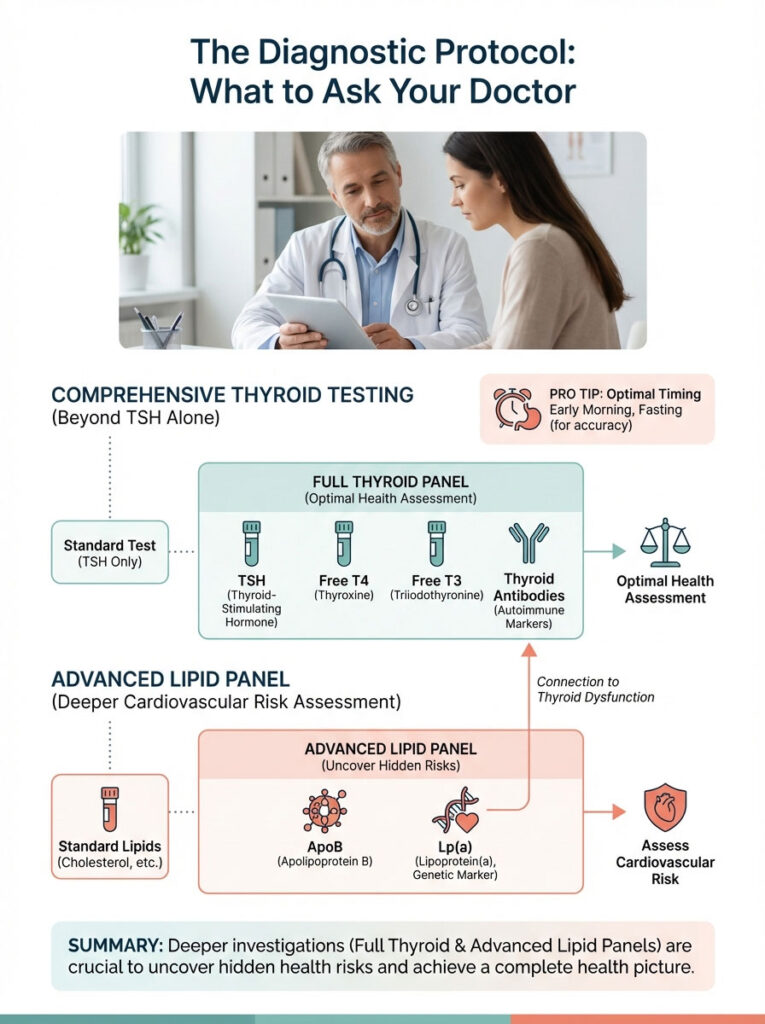
Doctors often only run a TSH test. If it comes back within the very wide “normal” range, they stop looking. But optimal health requires deeper investigation.
The Full Thyroid Panel
TSH alone is the screening tool, but it is insufficient for a full metabolic picture. A comprehensive panel should include:
- TSH: The brain’s signal to the thyroid. A high number means the brain is screaming for more hormone.
- Free T4: The storage hormone circulating in the blood.
- Free T3: The active hormone. This is crucial because T3 is what actually binds to the liver cells to clear cholesterol.
- Reverse T3: This is the “brake” pedal. Elevated levels can indicate metabolic stress blocking conversion.
- TPO & Tg Antibodies: Screening for Hashimoto’s Autoimmune Thyroiditis. This is the leading cause of hypothyroidism in the USA.
The Advanced Lipid Panel
Standard lipid panels give you the basics. I recommend digging deeper. Ask for testing for ApoB and Lp(a).
Lp(a) is a genetic marker. It is a very sticky, dangerous form of cholesterol. Its expression can be exacerbated by thyroid dysfunction. Knowing these numbers helps us assess true cardiovascular risk.
Pro Tip: Always test your thyroid hormones early in the morning. Aim for before 9:00 AM. Do this fasting. TSH levels follow a circadian rhythm and can drop falsely later in the day.
Treatment: Reversing the Damage
The good news is that secondary hyperlipidemia is reversible. When we address the question, “Can hypothyroidism cause high cholesterol to become permanent?”, the answer is generally no. Provided the thyroid is treated correctly, the lipids usually follow.
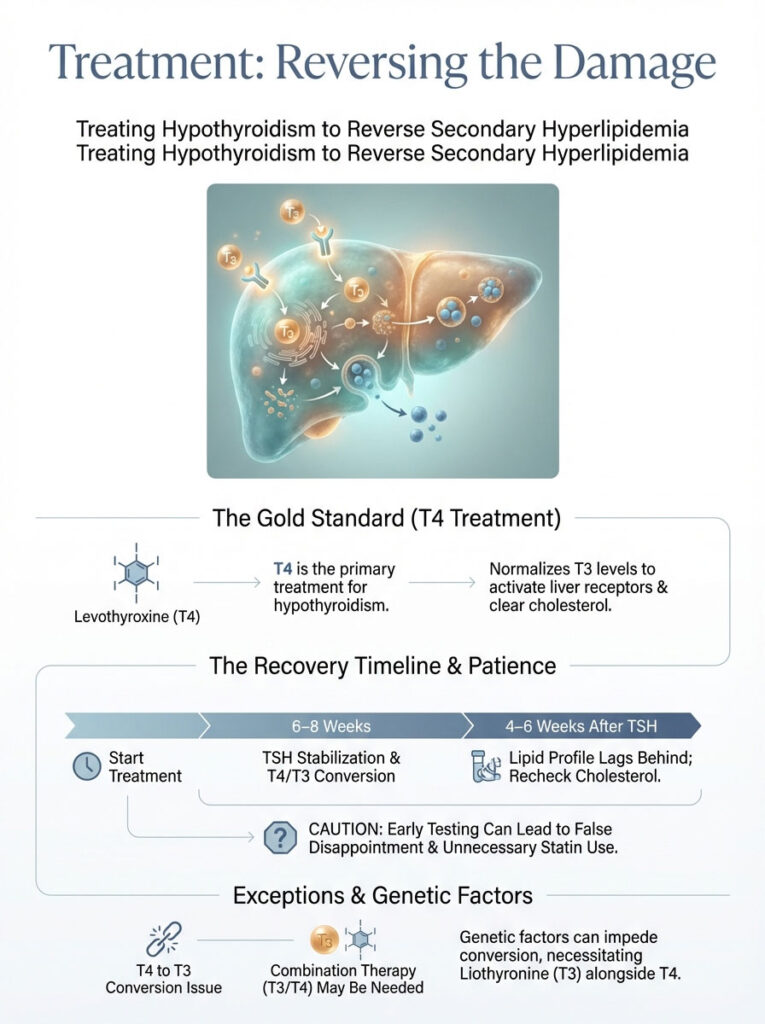
Levothyroxine (T4) Monotherapy
The gold standard treatment is Levothyroxine. This is synthetic T4. By replacing the missing T4, we provide the body with the raw material to convert to T3.
Once T3 levels normalize, the hormone re-engages the nuclear receptors in the liver. The SREBP-2 gene is activated. The liver starts building LDL receptors again. The backlog of cholesterol is cleared.
Timeframe for Recovery
Patience is required here. It takes approximately 6 to 8 weeks for TSH levels to stabilize after starting medication or changing a dose. However, the lipid profile may lag behind.
We typically do not re-check cholesterol until the patient has been euthyroid (normal thyroid levels) for at least 4 to 6 weeks. Checking too early leads to false disappointment. It may also lead to unnecessary statin prescriptions.
Combination Therapy (T3/T4)
For some patients, T4 alone is not enough. Some people have a genetic inability to convert T4 to T3 efficiently. This is due to polymorphisms in the DIO2 gene.
In these cases, their liver may still be starved of T3 even if their TSH looks normal. Adding Liothyronine (synthetic T3) can offer additional lipid-lowering benefits. This ensures the liver gets the direct signal it needs to clear the blood.
The Statin Dilemma: Risks and Interactions
A common scenario involves a patient being placed on a statin while their hypothyroidism remains undiagnosed. Or perhaps it is undertreated. This presents two major problems: statin resistance and myopathy.
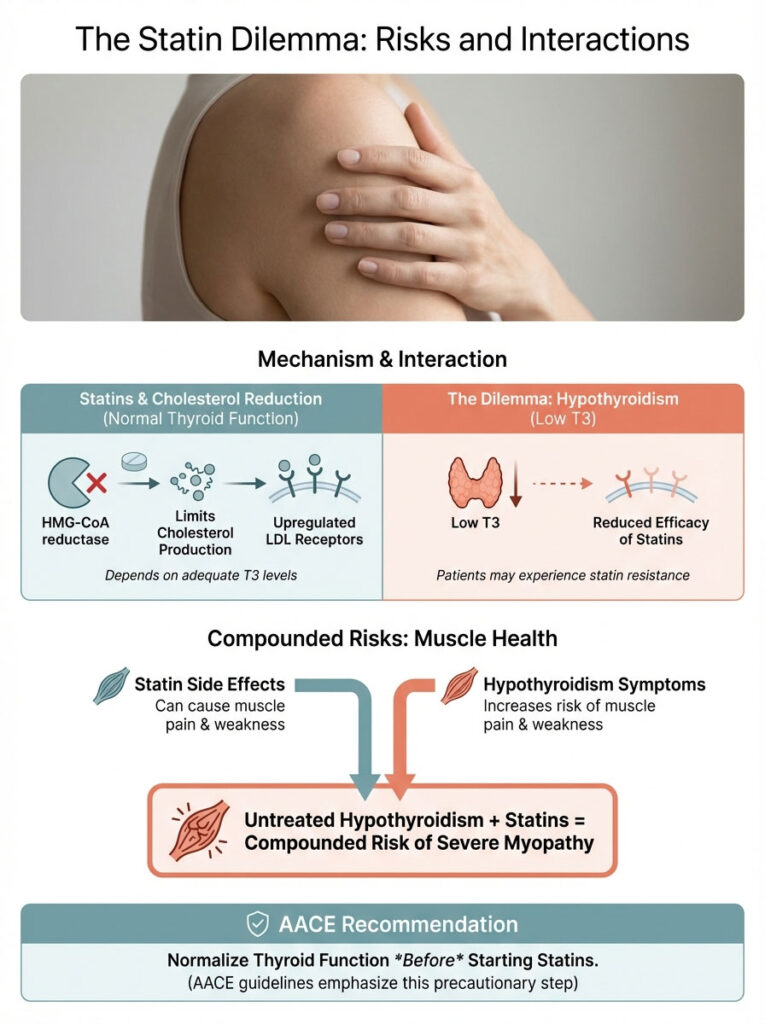
Statin Resistance
Statins work by inhibiting the HMG-CoA reductase enzyme. This limits cholesterol production. They also work by upregulating LDL receptors. However, as we have established, the upregulation of LDL receptors is dependent on thyroid hormone.
If T3 is low, the statin cannot work to its full potential. The mechanism it relies on is broken. You may find yourself on increasing doses of statins with diminishing returns. The numbers just won’t budge.
The Danger of Myopathy
This is a critical safety warning. Hypothyroidism predisposes patients to muscle pain and weakness. Statins also carry a risk of muscle-related side effects.
When you combine untreated hypothyroidism with statin therapy, the risk of severe myopathy increases exponentially. The muscles are hit from both sides. They lack the energy from thyroid hormone, and the statin affects their structure.
In rare cases, this can lead to rhabdomyolysis. This is a serious condition involving rapid muscle breakdown. It can damage the kidneys and be life-threatening. The American Association of Clinical Endocrinologists (AACE) guidelines are clear. They recommend normalizing thyroid function before committing a patient to long-term lipid-lowering pharmacotherapy.
Comparative Analysis: Statin vs. Thyroid Hormone
Choosing the right path requires understanding the mechanism of action. We need to know what we are treating. Are we treating the symptom (cholesterol) or the cause (thyroid)?
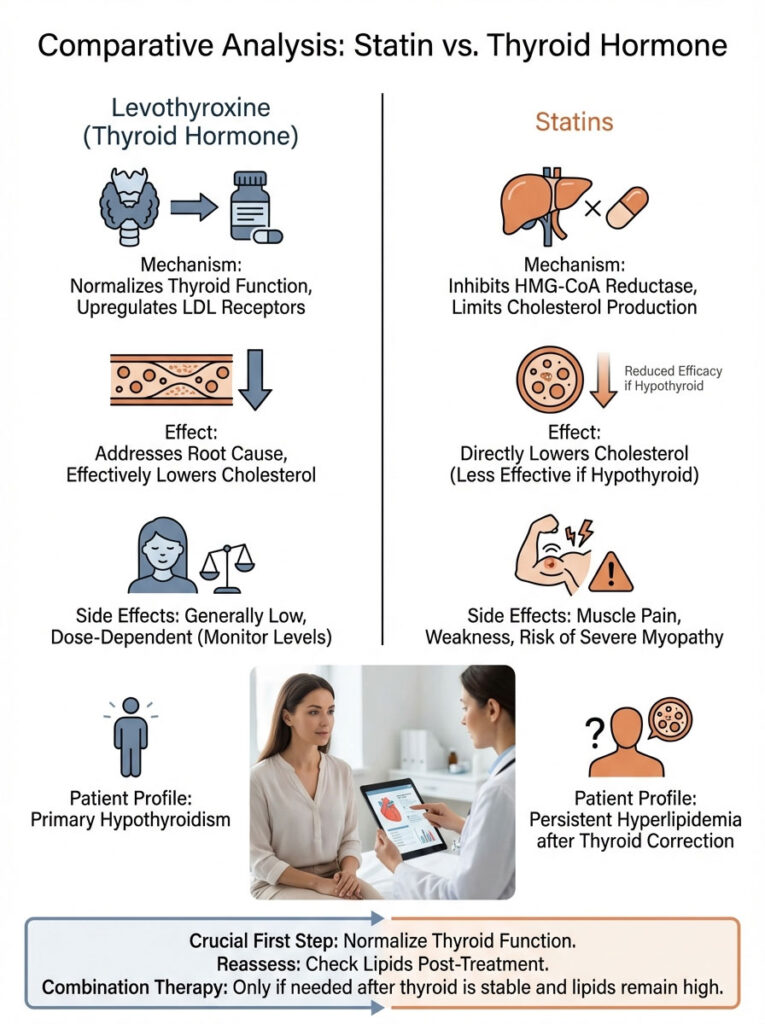
The table below compares the two approaches for a patient with thyroid-induced hyperlipidemia.
| Treatment Approach | Mechanism of Action | Effect on Cholesterol | Side Effect Profile | Best For… |
|---|---|---|---|---|
| Levothyroxine Only | Restores LDL receptor gene expression via T3 | Can lower LDL by 20–30% | Minimal (if dosed correctly to euthyroid state) | Hypothyroid patients with secondary high cholesterol |
| Statin Only | Inhibits HMG-CoA reductase enzyme | Lowers LDL by 30–50% | Muscle pain, liver enzyme elevation, blood sugar rise | Primary hyperlipidemia or genetic high cholesterol |
| Combination Therapy | Dual mechanism (Receptor + Enzyme inhibition) | Synergistic effect (Maximum reduction) | Increased risk of myopathy if thyroid not stable first | Patients with both thyroid disease and genetic lipid issues |
This comparison highlights why order matters. First, fix the thyroid. Then, reassess the lipids. If they are still high, then consider the statin.
Diet and Lifestyle: Why It Still Matters
We have established that hypothyroidism cause high cholesterol through a metabolic mechanism. However, diet remains the fuel for that mechanism. A synergistic approach yields the best results. You cannot medicate your way out of a bad diet.
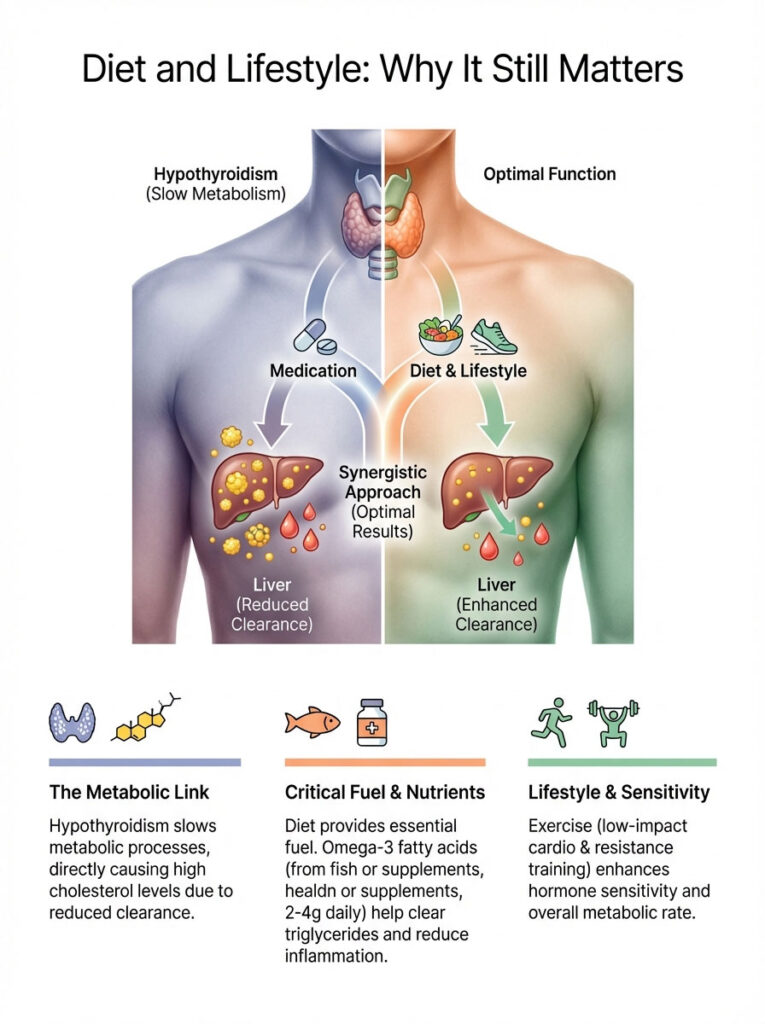
Nutrients for Thyroid & Heart
To support the liver’s ability to clear lipids, we need to support the thyroid’s ability to convert hormones. Several key nutrients bridge this gap.
- Selenium: This is essential for the conversion of T4 to T3. Without it, the medication works poorly. Brazil nuts are a great source.
- Zinc: Another co-factor for thyroid conversion. It also supports immune health.
- Fiber: This is the cleanup crew. Once the liver pulls cholesterol from the blood, it dumps it into the bile. Soluble fiber binds to this bile in the intestines. It ensures it is excreted rather than reabsorbed. Aim for 30 grams of fiber daily. Good sources include oats, legumes, and flaxseeds.
Omega-3 Fatty Acids
Hypothyroidism specifically impairs the clearance of triglycerides. High-dose Omega-3 fatty acids can be a powerful adjunct therapy. A dose of 2 to 4 grams daily is often recommended.
Omega-3s help combat the sluggishness of the Lipoprotein Lipase enzyme. They help “grease the wheels” of your metabolism. They also lower inflammation, which protects the arteries.
The Role of Exercise
Exercise is not just about burning calories. It sensitizes the body to hormones. Resistance training, in particular, can help improve receptor sensitivity.
For hypothyroid patients, low-impact steady-state cardio combined with weight lifting is ideal. It boosts metabolism without spiking cortisol. High cortisol can further suppress thyroid function, so balance is key.
Special Considerations: The “Thin” Hypothyroid Patient
There is a dangerous myth that only overweight people have high cholesterol or hypothyroidism. This leads to missed diagnoses. I see many thin patients with sky-high LDL.
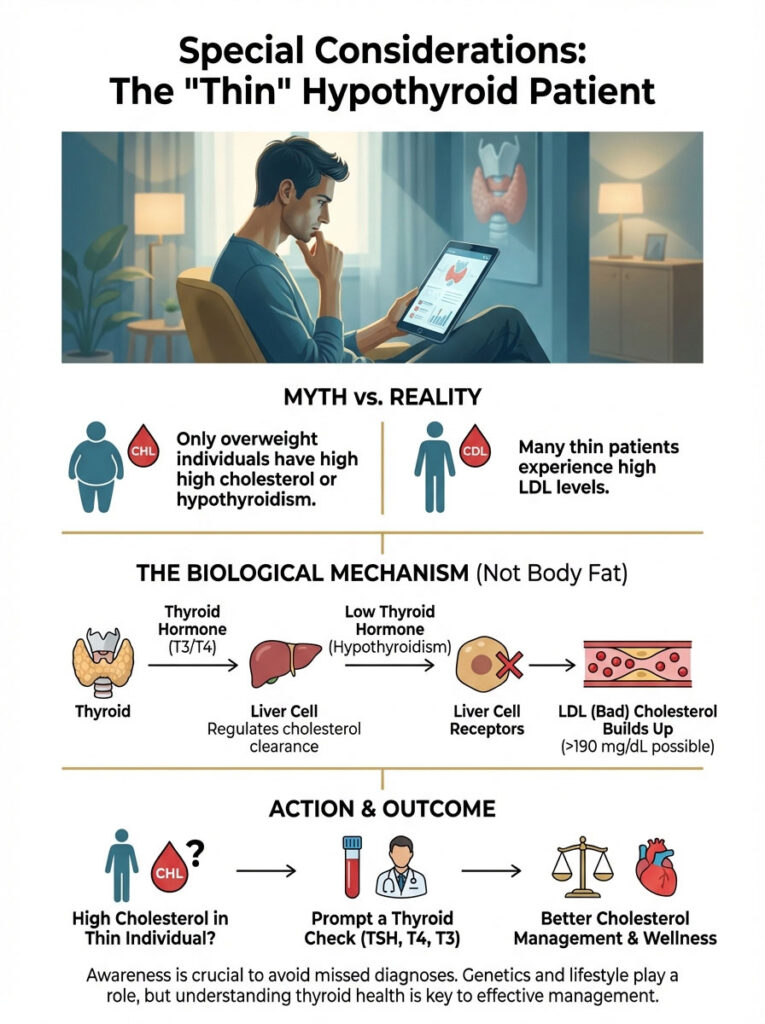
Remember, the mechanism is cellular. It is about receptors on the liver cells. It is not about body fat percentage. A thin person with a failing thyroid can easily have an LDL over 190 mg/dL.
If you are thin, eat well, and have high cholesterol, do not assume it is just “bad genetics.” Demand a thyroid check. It is often the missing piece of the puzzle.
Conclusion: Key Takeaways for Heart Health
The connection is undeniable: Can hypothyroidism cause high cholesterol? Yes. It is likely one of the most underdiagnosed causes of heart disease risk in the United States. The thyroid controls the liver’s ability to process fat. When that control signal fades, cholesterol rises.
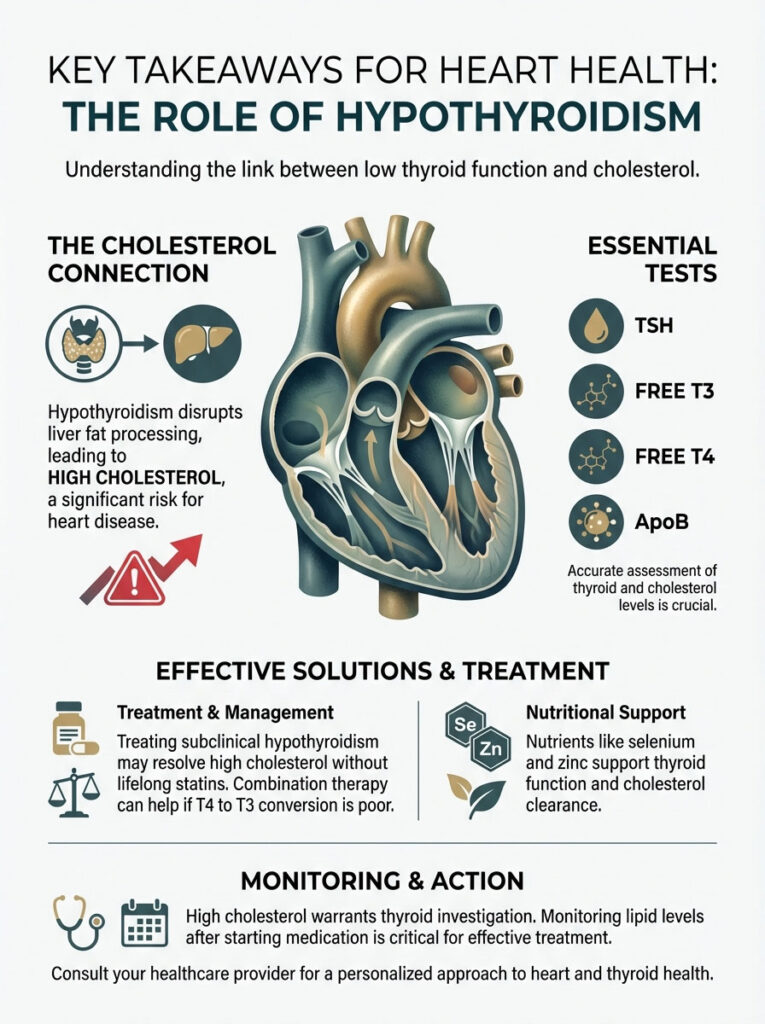
Think of high cholesterol not just as a dietary failure. Think of it as a potential “check engine” light for your thyroid. If you are struggling with lipid levels despite a healthy lifestyle, do not accept a lifetime of statins without asking “why.”
Summary of Action Steps:
- Test, Don’t Guess: Get a full thyroid panel (TSH, Free T3, Free T4, Antibodies) alongside your lipid panel.
- Check ApoB: This gives a clearer picture of heart risk than LDL alone, especially in subclinical cases.
- Treat the Root: If you are hypothyroid, prioritize normalizing thyroid hormones before starting statins.
- Monitor for Safety: Be aware of the increased risk of muscle pain if taking statins while hypothyroid.
- Support Metabolism: Use diet and fiber to help your liver flush out the cholesterol your thyroid medication helps it catch.
Advocate for your health. Ensure your TSH, Free T3, and Free T4 are optimal, not just “in range.” By treating the root cause, the thyroid, you may find that your heart health resolves itself naturally.
Frequently Asked Questions
Can hypothyroidism cause high cholesterol even if I follow a strict diet?
Yes, hypothyroidism is a primary cause of secondary hyperlipidemia. When thyroid hormone levels are low, the liver lacks the hormonal signal to produce enough LDL receptors, preventing the clearance of “bad” cholesterol from your blood regardless of how many healthy fats or vegetables you consume.
How does thyroid hormone specifically regulate cholesterol levels in the liver?
Active thyroid hormone, specifically Triiodothyronine (T3), activates the SREBP-2 pathway in liver cells. This genetic switch tells the liver to build LDL receptors, which act as “docks” to catch and clear LDL particles from the bloodstream; without sufficient T3, these receptors are downregulated, causing cholesterol to accumulate.
Does subclinical hypothyroidism require treatment if my cholesterol is elevated?
Many endocrinologists recommend treating subclinical hypothyroidism—where TSH is high but T4 is normal—if lipid imbalances are present. The liver is highly sensitive to minor thyroid deficiencies, and correcting the TSH can often resolve “resistant” high cholesterol without the need for lifelong statin therapy.
Why is it important to check thyroid function before starting a statin?
It is vital to rule out a sluggish thyroid because statins rely on the very LDL receptors that are downregulated in hypothyroid patients. Furthermore, taking statins while hypothyroid significantly increases the risk of statin-associated muscle symptoms and severe myopathy, as the muscles are already metabolically compromised.
What is the significance of ApoB testing for someone with thyroid issues?
ApoB measures the total number of atherogenic (plaque-causing) particles in the blood, providing a more accurate cardiovascular risk profile than standard LDL-C. Hypothyroidism is specifically linked to an increase in these dangerous particles, making ApoB a critical metric for assessing how much your thyroid is impacting your heart health.
How long does it take for cholesterol levels to improve after starting thyroid medication?
While TSH levels typically begin to stabilize within 6 to 8 weeks, the lipid profile may lag behind. We generally recommend re-testing cholesterol only after a patient has maintained a euthyroid (normal) state for at least 4 to 6 weeks to ensure the liver has had sufficient time to clear the circulating fats.
Can an inability to convert T4 to T3 affect my lipid profile?
Yes, because T3 is the active hormone that binds to liver receptors, poor conversion of T4 to T3 can leave the liver “starved” for the signal it needs to process cholesterol. In these cases, patients may benefit from combination T3/T4 therapy to effectively lower lipid markers and restore metabolic efficiency.
Why do triglycerides often rise in patients with low thyroid function?
Thyroid hormone regulates the activity of Lipoprotein Lipase (LPL), the enzyme responsible for breaking down and clearing triglycerides from the blood. When thyroid function is low, LPL activity is suppressed, leading to elevated triglycerides which can thicken the blood and increase the risk of cardiovascular events.
Is it possible for hypothyroidism to cause high cholesterol in thin individuals?
Absolutely. The link between thyroid function and cholesterol is a cellular metabolic process involving liver receptors, not a result of body fat percentage. Even a patient with a healthy BMI can experience dangerously high LDL levels if their thyroid is not providing the necessary signals for lipid clearance.
What role does the protein PCSK9 play in thyroid-related high cholesterol?
Research indicates that thyroid hormone naturally helps inhibit PCSK9, a protein that destroys LDL receptors on the liver. In a hypothyroid state, PCSK9 levels may rise, leading to the destruction of the few receptors the liver manages to produce, creating a “double hit” on your body’s ability to manage fats.
Which thyroid lab tests are essential for a complete metabolic assessment?
A standard TSH screening is often insufficient for patients with high cholesterol; you should request a full panel including Free T4, Free T3, and TPO antibodies. Additionally, testing Reverse T3 can help determine if metabolic stress is preventing the active hormone from reaching the liver cells.
Can specific nutrients help the thyroid improve cholesterol clearance?
While they do not replace hormone therapy, selenium and zinc are vital co-factors for the conversion of T4 to the active T3 needed by the liver. Furthermore, increasing soluble fiber intake helps the body excrete the cholesterol-rich bile that the liver clears once thyroid levels are optimized.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Hypothyroidism and hyperlipidemia are complex medical conditions that require professional diagnosis and management. Always consult a qualified healthcare professional or endocrinologist before making changes to your medication or treatment plan.
References
- The Colorado Thyroid Disease Prevalence Study – Archives of Internal Medicine – A landmark study establishing the linear relationship between TSH levels and elevated serum cholesterol.
- American Association of Clinical Endocrinologists (AACE) – Clinical Practice Guidelines – Official medical protocols recommending thyroid screening for all patients with hyperlipidemia.
- The Rotterdam Study – Journal of Clinical Endocrinology & Metabolism – Longitudinal research identifying subclinical hypothyroidism as an independent risk factor for atherosclerosis.
- Journal of Lipid Research – “Thyroid Hormone Regulation of LDL Receptor Gene” – A deep dive into the molecular mechanism of how T3 influences SREBP-2 and hepatic cholesterol clearance.
- Thyroid Federation International – Patient Education Resources – Statistical data regarding the prevalence of thyroid-induced secondary hyperlipidemia in women.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Official Health Information – Data regarding the impact of thyroid function on liver enzyme activity and triglyceride clearance.