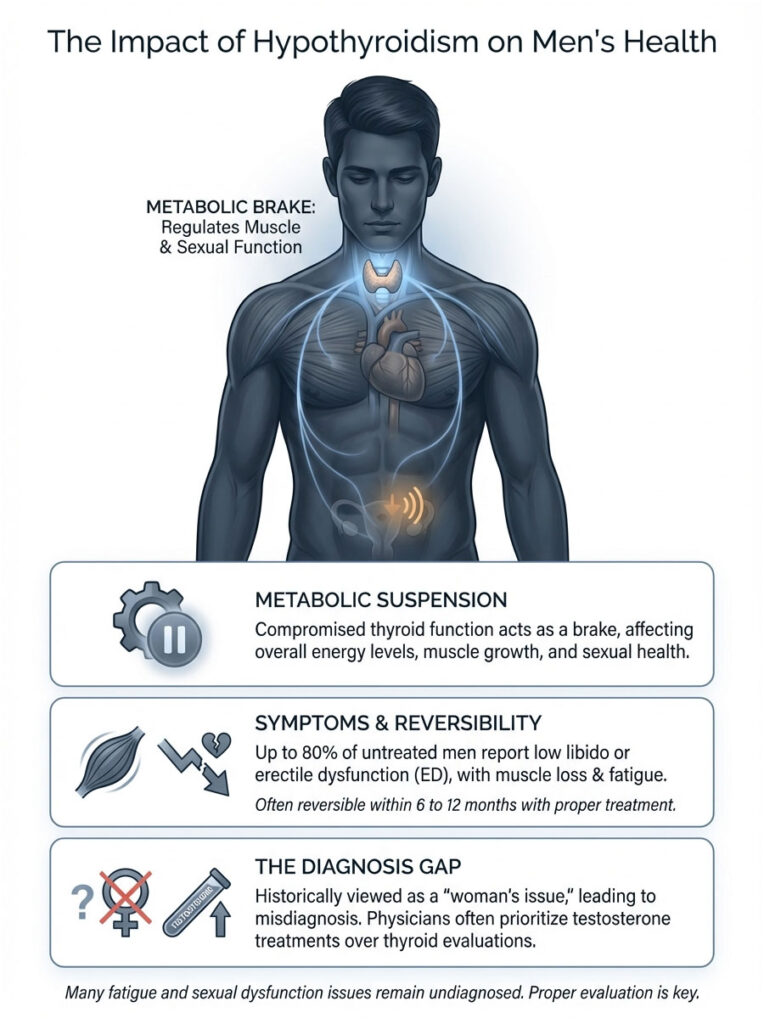
Quick Answer: Yes. Hypothyroidism acts as a metabolic brake that directly contributes to muscle atrophy and erectile dysfunction in men. Up to 80% of men with untreated thyroid disease experience low libido or ED. The good news? These symptoms are largely reversible within 6 to 12 months once thyroid levels are properly restored.
Table of Contents
You have been hitting the gym for months with nothing to show for it. Your libido has disappeared. Your doctor tells you your testosterone is “within range,” but you feel like a shell of who you used to be.
In my 18 years as an endocrinologist, I have watched this exact scenario play out hundreds of times. And the question patients keep coming back to is simple: Can hypothyroidism cause muscle loss and ED in men?
The answer is yes, and it happens far more often than most people realize.
The medical community has long treated thyroid health as a “woman’s issue.” That bias leads to delayed diagnosis in men. When a man walks into a clinic complaining of fatigue and erectile dysfunction, the typical response is a Viagra prescription or a Low T screening. Rarely does the physician think to check the thyroid first.
But here is the truth: your thyroid sets the metabolic pace for every cell in your body. When it underperforms, it does not just drain your energy. It physically reshapes your muscles and chemically disrupts your sexual function. Your body enters a state of metabolic suspension, prioritizing organ survival over muscle growth or reproduction.
Key Clinical Statistics
- 80% of hypothyroid men report some degree of sexual dysfunction (Journal of Clinical Endocrinology & Metabolism).
- 50% of hypothyroid patients show signs of myopathy (muscle disease) before diagnosis.
- 30-40% reduction in bioavailable testosterone is common due to SHBG changes.
- Elevated CPK (Creatine Phosphokinase) levels appear in up to 90% of symptomatic hypothyroid patients.
- 60% of hypothyroid men experience delayed ejaculation or anorgasmia due to slowed nerve transmission.
How Your Thyroid Controls Your Testes
To understand why you are losing both strength and drive, we need to look beyond the symptoms and into the biochemistry. The thyroid and the testes are tightly connected through the Hypothalamic-Pituitary-Thyroid (HPT) axis. This is not a simple on-off switch. It is a complex web of hormonal feedback loops.
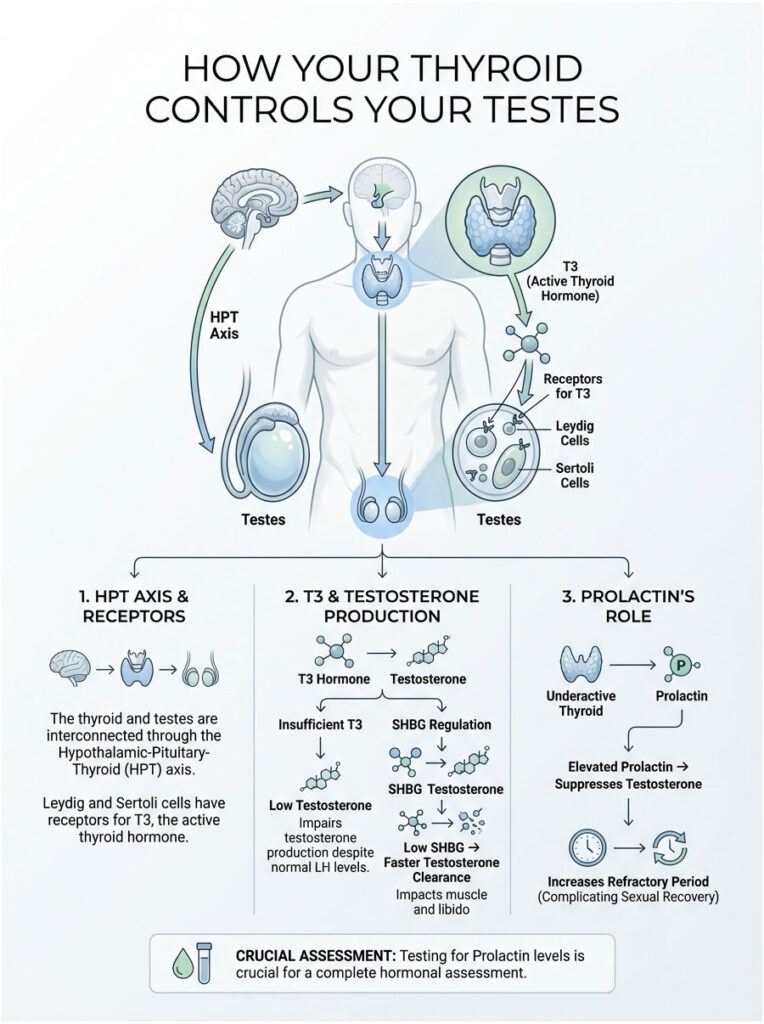
The Thyroid-Gonadal Axis
Your testes do not work in isolation. They receive signals from the pituitary gland through Luteinizing Hormone (LH). However, the Leydig cells (which produce testosterone) and the Sertoli cells (which support sperm production) both carry specific receptors for T3, the active thyroid hormone.
Without enough T3, the Leydig cells become sluggish. They cannot produce testosterone efficiently, no matter how much LH the pituitary sends. This is exactly why testosterone injections (TRT) often fail to fix the problem when an underlying thyroid issue remains untreated. The cellular machinery is still offline. The mitochondria inside your Leydig cells depend on T3 to generate the ATP needed for steroidogenesis, the process of creating testosterone from cholesterol.
The SHBG Paradox: Why “Normal” Testosterone Can Be Misleading
This is where most general practitioners get tripped up. They run a standard lab panel, see that your Total Testosterone reads 450 ng/dL (technically “normal”), and send you home telling you it is all in your head.
What they are missing is the Sex Hormone-Binding Globulin (SHBG) connection.
Thyroid hormone regulates SHBG production in the liver. In hypothyroid men, SHBG levels drop sharply. You might assume less binding protein is a good thing, but in this context, it backfires. Low SHBG means your testosterone gets metabolized and cleared from the bloodstream too quickly. It does not linger long enough to do its job.
The result? A man can have a “normal” Total Testosterone number while his bioavailable testosterone is critically low. The lab report looks fine on paper, but the tissues, your muscles and brain, are starved of androgenic stimulation. This mechanism is one of the silent culprits I point to when patients ask whether hypothyroidism can cause muscle loss and ED in men. Your metabolic drain is wide open, and testosterone is leaking out before it can build muscle or fuel an erection.
The Prolactin Connection: The Hidden Libido Killer
There is another hormonal domino that falls when your thyroid slows down. An underactive thyroid prompts the brain to push harder by releasing TRH (Thyrotropin-Releasing Hormone). TRH stimulates TSH, but it has an unwanted side effect: it also triggers the release of Prolactin.
Prolactin is the hormone that enables breastfeeding in women. In men, elevated prolactin functions almost like a chemical castration agent. It suppresses GnRH (Gonadotropin-Releasing Hormone), effectively shutting down your body’s natural testosterone production. This creates secondary hypogonadism, leading to severe ED and a near-complete loss of sexual desire.
On top of that, high prolactin increases the refractory period. Even if you can achieve an erection, recovering for another round becomes nearly impossible. If your doctor has not tested your Prolactin levels, the diagnostic picture is incomplete.
Hypothyroid Myopathy: Why It Is Not Just Fatigue
Many men describe a feeling of heaviness, as if they are moving through wet cement. This is not laziness. It is a distinct clinical condition called Hypothyroid Myopathy, and it changes the actual architecture of your skeletal muscle.
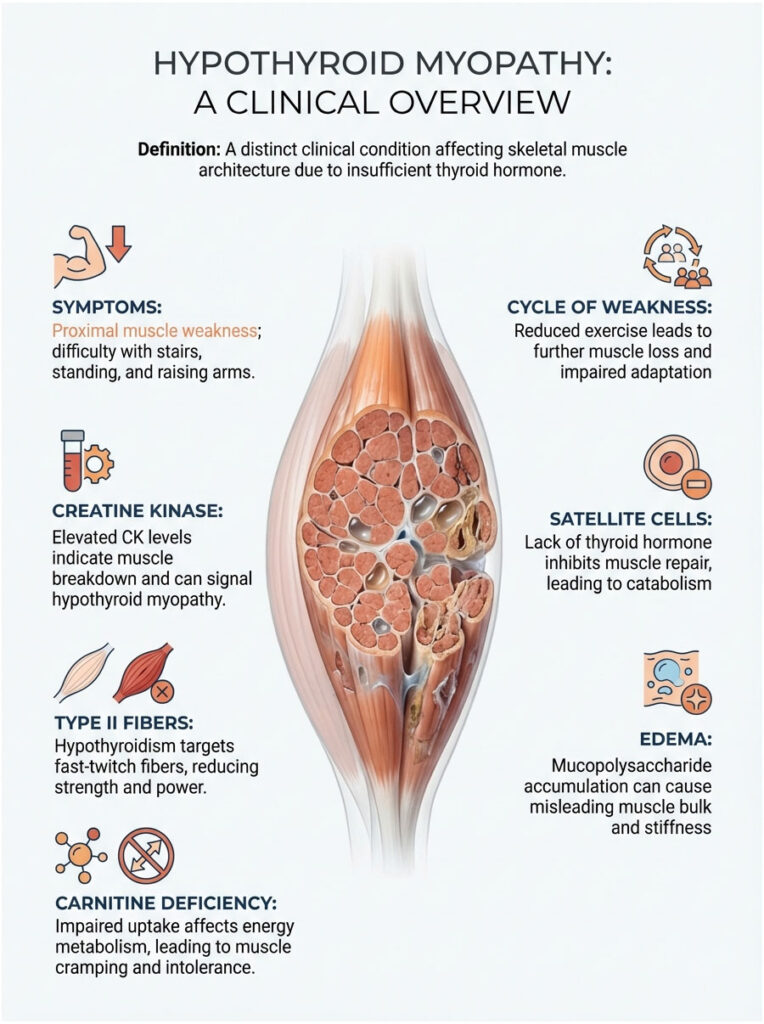
What Hypothyroid Myopathy Looks Like
This condition is fundamentally different from the tiredness you feel after a bad night of sleep. It shows up as proximal muscle weakness. You might struggle to climb stairs, stand up from a low chair, or lift your arms overhead to wash your hair. In severe cases, blood tests reveal elevated Creatine Kinase (CK) enzymes, which indicate active muscle tissue breakdown.
This creates a vicious cycle. You feel weak, so you exercise less. You exercise less, so you lose more muscle. But even if you push through and train, the lack of thyroid hormone prevents the normal adaptation response. You are digging a hole you cannot fill.
Expert Tip: If you have unexplained muscle soreness after mild exercise that lingers for days, ask for a CK (Creatine Kinase) test alongside your thyroid panel. Elevated CK without heavy trauma is a hallmark of hypothyroid myopathy.
Satellite Cell Deactivation and Muscle Wasting
So why does muscle waste away? The answer comes down to satellite cells, the stem cells of your muscle tissue. When you lift weights, you create micro-tears in the fibers. Satellite cells then activate, fuse with the damaged fiber, and repair it, making it larger and stronger.
T3 is essential for activating these satellite cells. Without enough thyroid hormone, muscle repair stalls. You break muscle down in the gym, but the repair phase never completes. The result is a net loss of muscle mass (catabolism) despite your best efforts.
What makes this worse is that hypothyroidism preferentially targets Type II fast-twitch fibers, the very fibers responsible for strength, power, and muscle size. This selective atrophy explains why hypothyroid men lose their explosiveness first. You can still manage a slow walk, but sprinting or lifting a heavy box feels impossible. The fast-twitch fibers have essentially gone dormant.
The Carnitine Deficiency Factor
Low thyroid function also impairs carnitine uptake in muscle tissue. Carnitine is the shuttle that transports fatty acids into the mitochondria to be burned for energy. When that shuttle stalls, your muscles cannot use fat as fuel efficiently.
This leads to metabolic buildup, cramping, and severe exercise intolerance. Your muscles are not just shrinking; they are starving for energy. You may notice a burning sensation with very little exertion, caused by lactic acid accumulation because your aerobic energy systems are failing.
Glycosaminoglycan Deposition: The “False” Bulk
Sometimes men with hypothyroidism actually appear bulkier, even though they are weaker. This happens because mucopolysaccharides (glycosaminoglycans) accumulate inside the muscle tissue. These substances attract water, making the muscle swell.
This is not functional muscle. It is edema (water retention) trapped within the muscle belly. It creates stiffness and pain, a condition called Hoffman’s Syndrome in severe cases. You might look big, but the tissue is boggy, weak, and painful. It is the puffy appearance that often accompanies profound hypothyroidism.
How Hypothyroidism Causes Erectile Dysfunction
Erections are hydraulic events driven by chemical signals. Hypothyroidism disrupts the key chemical messenger required for penile blood flow: Nitric Oxide.
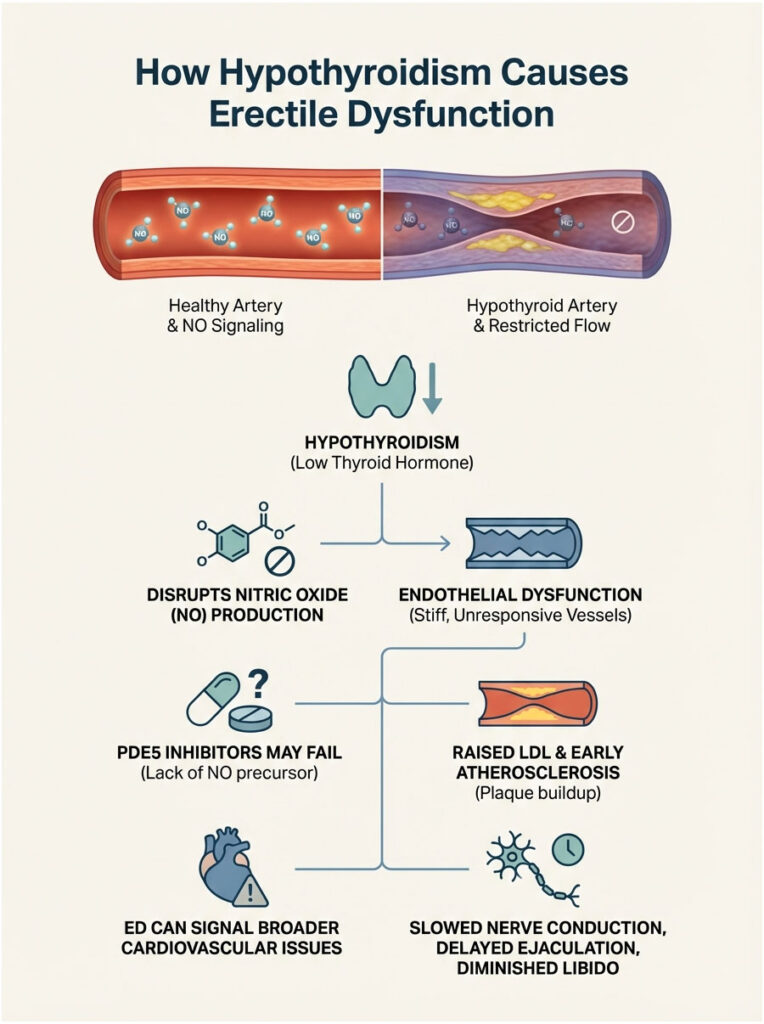
Nitric Oxide Depletion and Vascular Stiffness
The endothelium (the inner lining of your blood vessels) depends on thyroid hormones to produce Nitric Oxide synthase. Nitric Oxide (NO) is the gas molecule that signals blood vessels to relax and dilate. Without it, the vessels stay constricted.
Hypothyroidism causes endothelial dysfunction. Blood vessels become stiff and unresponsive. Even when you are mentally aroused, the physical signal cannot get through because the vascular pathways are chemically blocked.
This is also why PDE5 inhibitors like Cialis or Viagra sometimes fail in hypothyroid men. Those drugs work by amplifying Nitric Oxide, but if your body is not producing NO in the first place, there is nothing to amplify.
Additionally, hypothyroidism is well-known to raise LDL cholesterol, which promotes plaque buildup in the arteries. Because the penile arteries are among the smallest in the body, they are often the first to be affected by this accelerated atherosclerosis. ED is frequently the first warning sign of broader cardiovascular disease driven by thyroid dysfunction.
Neural Dampening and Ejaculatory Disorders
Thyroid hormone also governs the speed of nerve impulse transmission. In a hypothyroid state, nerve conduction velocity slows down, directly affecting the autonomic nervous system that controls arousal and ejaculation.
This is why delayed ejaculation is so common among these patients. While hyperthyroidism (overactive thyroid) is linked to premature ejaculation, hypothyroidism slows the neural reflexes, making it difficult or even impossible to reach climax. Combine that with the brain fog and depressive symptoms that typically accompany the condition, and libido can vanish entirely. The connection between the brain and the genitals is literally running slower.
Hypothyroidism vs. Low Testosterone: How to Tell Them Apart
Because the symptoms of hypothyroidism and primary Low T overlap so much, distinguishing between them can be tricky. This comparison should help you identify the more likely root cause.
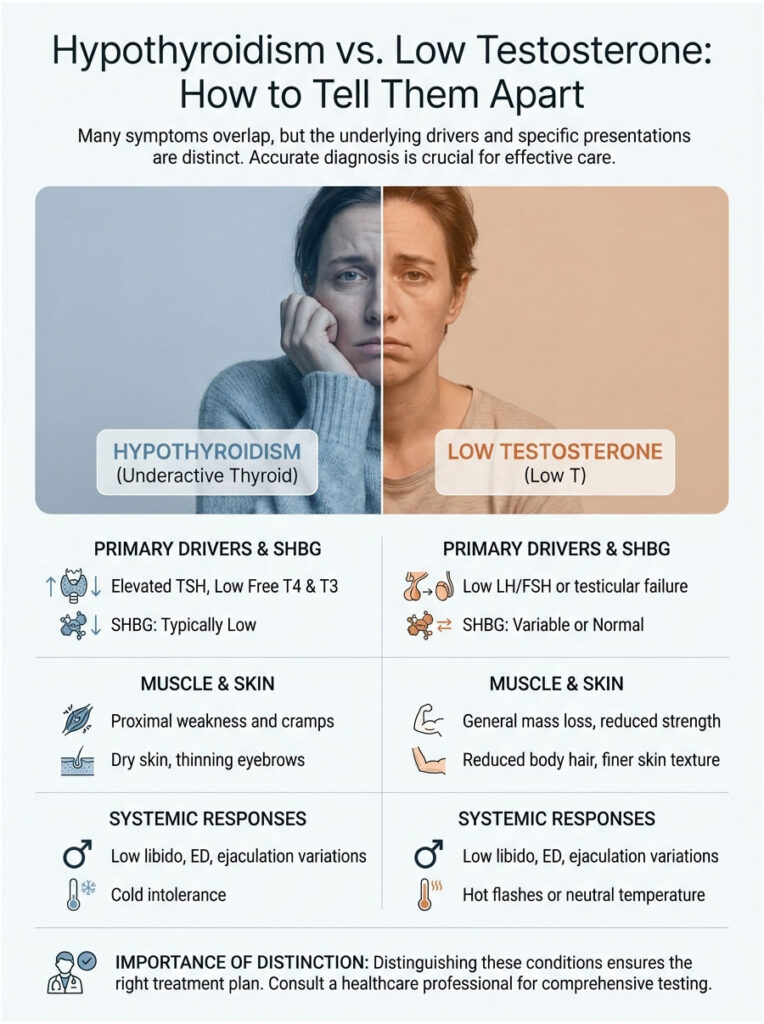
| Symptom / Feature | Hypothyroidism | Primary Low T |
| Primary Driver | High TSH, Low Free T4/T3 | Low LH/FSH or Testicular Failure |
| Muscle Symptoms | Proximal weakness, cramps, high CK | General mass loss, reduced strength |
| Sexual Function | Low libido, ED, often delayed ejaculation | Low libido, ED, loss of morning erections |
| Body Temperature | Cold intolerance (always freezing) | Hot flashes or temperature neutral |
| Skin/Hair | Dry skin, thinning outer eyebrows | Reduced body hair, finer skin texture |
| SHBG Levels | Typically Low | Variable or Normal |
Diagnosis: The Complete Male Thyroid Panel
The standard of care in many clinics is a simple TSH test. If the result falls between 0.4 and 4.0 mIU/L, you are told you are fine. For men experiencing muscle loss and ED, this approach is not good enough.
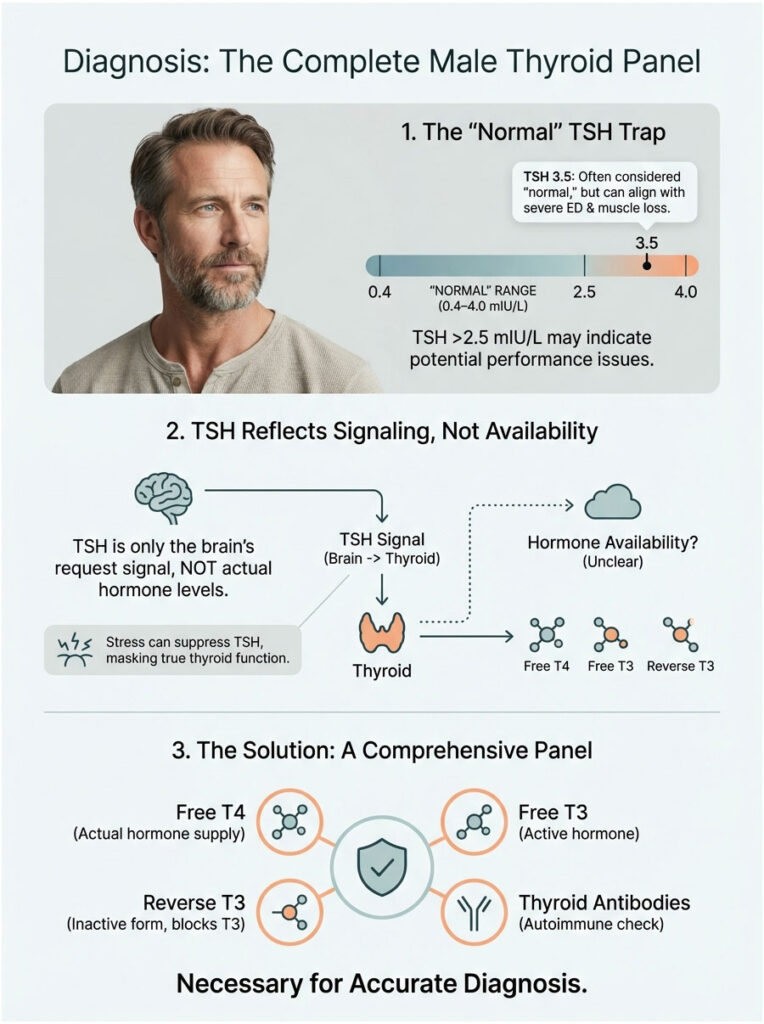
Why TSH Alone Falls Short
TSH (Thyroid Stimulating Hormone) is a pituitary hormone, not a thyroid hormone. It reflects the brain’s request for more thyroid activity, not the actual fuel available to your cells. I frequently see men with a TSH of 3.5 mIU/L, technically “normal,” who are dealing with severe ED and an inability to build muscle.
In functional endocrinology, a TSH above 2.5 can already be problematic for optimal male performance. On top of that, stress and cortisol can suppress TSH, making the number appear normal even when thyroid output is genuinely low. Relying solely on TSH is like checking your fuel gauge to see if the engine is running. It tells you about the tank, not the combustion.
The Gold Standard Blood Panel
To properly determine whether hypothyroidism is behind your muscle loss and ED, you need a comprehensive set of tests. Here is what to request from your provider:
- TSH – Baseline screening. Optimal is typically between 0.5 and 2.0.
- Free T4 – The storage hormone. Low levels suggest low thyroid production.
- Free T3 – The unbound, active hormone available to your cells. The most critical marker for muscle and libido.
- Reverse T3 – The “anti-thyroid” hormone that blocks T3 receptors. High stress or chronic dieting can elevate it.
- TPO Antibodies (TPOAb) – Rules out Hashimoto’s autoimmune disease, the leading cause of hypothyroidism.
- Thyroglobulin Antibodies (TgAb) – Another marker for autoimmune thyroid attack.
- Total and Free Testosterone – To assess the hormonal interplay and rule out primary hypogonadism.
- SHBG – Determines bioavailable testosterone status.
- Prolactin – Checks whether the pituitary is suppressing your testes.
- Creatine Kinase (CK) – Detects active muscle damage (myopathy).
- Ferritin – Iron is essential for thyroid function. Low levels can mimic hypothyroidism.
Treatment and Recovery Protocols
The encouraging news is that this condition is highly treatable. Once the metabolic brake is lifted, the body is eager to repair itself. Recovery involves medication, lifestyle adjustments, and patience.
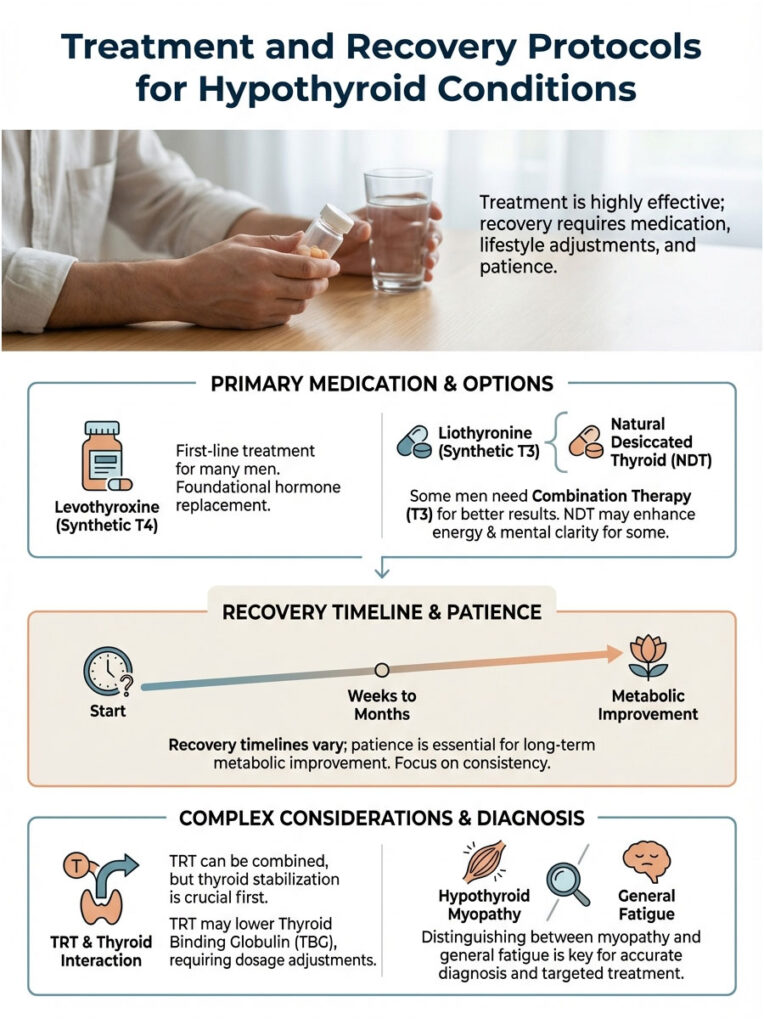
Restoring Euthyroid Status with Medication
The first line of treatment is usually Levothyroxine (Synthetic T4). For many men, this is sufficient. The body converts T4 into active T3, and symptoms resolve. However, some men carry a genetic difficulty converting T4 to T3 (polymorphisms in the DIO2 gene).
If you are on T4 medication and your labs look good but you still feel weak and have ED, you may need Combination Therapy. This means adding Liothyronine (Synthetic T3) to your regimen. Direct T3 supplementation can be transformative for hypothyroid myopathy and libido because it bypasses the conversion bottleneck. The rule is always “start low, go slow.” Rushing thyroid medication can trigger heart palpitations and anxiety, which are counterproductive.
Another option is Natural Desiccated Thyroid (NDT), such as Armour Thyroid or NP Thyroid. These are derived from porcine thyroid glands and contain T4, T3, T2, and T1. Many patients report feeling subjectively better on NDT, particularly when it comes to energy and mental clarity.
What the Recovery Timeline Looks Like
Patience is essential. You cannot undo years of metabolic slowing in a week. Here is what men typically experience:
- Weeks 1-4: Fluid retention drops. The puffy look in the face fades. Energy levels begin to stabilize.
- Months 3-6: This is when sexual function typically turns around. Libido returns, erectile quality improves as Nitric Oxide levels restore, and cholesterol starts to normalize.
- Months 6-12: Full muscle protein synthesis comes back online. If you are training properly, you will see hypertrophy (growth) again. The satellite cells wake up and begin repairing the damage.
Can You Combine TRT with Thyroid Medication?
I am frequently asked whether TRT (Testosterone Replacement Therapy) can be used alongside thyroid meds. The answer is yes, and they often work well together. However, you must stabilize the thyroid first. Adding testosterone to a system with a broken metabolism is like putting premium fuel in a car with a flat tire. The engine revs, but you do not go anywhere.
Also worth noting: TRT can slightly lower TBG (Thyroid Binding Globulin), which means your thyroid dosage may need tweaking once you start testosterone. It is a careful balancing act that requires an experienced physician. Do not attempt to self-medicate with testosterone while managing a thyroid condition.
Hypothyroid Myopathy vs. General Fatigue
Telling apart general tiredness from actual muscle disease is critical for accurate diagnosis. This guide can help you communicate your symptoms more clearly.
| Feature | Hypothyroid Myopathy | General Fatigue |
| Sensation | Physical heaviness, pain, stiffness | Mental exhaustion, low motivation |
| Exercise Response | Severe soreness, inability to recover, cramps | Tiredness, but muscles recover normally |
| Enzyme Markers | Elevated Creatine Kinase (CK) | Normal CK levels |
| Location | Proximal (thighs, shoulders) | Generalized, whole body |
| Resolution | Requires hormone replacement | Resolves with rest, sleep, caffeine |
Lifestyle Support for Muscle Recovery and Sexual Health
Medication is the foundation, but lifestyle is the structure you build on top of it. You cannot out-medicate a bad lifestyle, and supporting your body during recovery makes a real difference.

Nutritional Priorities for Thyroid Health
Your thyroid needs specific micronutrients to convert T4 into T3. Selenium and zinc are non-negotiable. Zinc is especially important because it also drives testosterone production. A zinc deficiency hits you twice: it slows your thyroid and starves your Leydig cells. Good sources include oysters, red meat, and pumpkin seeds.
Selenium is found in high concentrations in Brazil nuts. Just two Brazil nuts a day can cover your daily requirement. This mineral protects the thyroid gland from oxidative damage during hormone production.
As for protein, hypothyroidism is a catabolic (muscle-wasting) state. To counteract this, you need to increase your protein intake. Aim for 1.6 to 2.0 grams of protein per kilogram of body weight. This ensures your body has enough amino acids to repair tissue even against the hormonal headwinds.
A Word of Caution on Iodine
Many men read online that iodine supports the thyroid and jump straight to high-dose kelp or iodine supplements. This can be dangerous. While iodine is a building block of thyroid hormone, too much of it can actually trigger Hashimoto’s disease or shut down the thyroid entirely (the Wolff-Chaikoff effect). Stick to food sources like fish and dairy, and avoid mega-dose supplements unless prescribed by your doctor.
How to Train During Thyroid Recovery
If you have active hypothyroid myopathy, training like a bodybuilder is going to backfire. Your muscles simply cannot repair the damage you are inflicting. You need to adjust your approach:
- Prioritize intensity over volume. Do fewer sets, but make each one count.
- Cut back on chronic cardio. Excessive steady-state cardio (like long-distance running) raises cortisol, which suppresses T4-to-T3 conversion. It works against the hypothyroid man.
- Extend rest periods between sets. Your mitochondria are sluggish, so give them time to replenish ATP.
- Listen to your body. If soreness lingers more than 48 hours after a workout, you are training too hard for your current hormonal status. Scale it back.
Sleep and Stress: Two Overlooked Factors
Sleep is when the pituitary gland releases the majority of its hormones. Poor sleep crushes both TSH and testosterone output. For hypothyroid men, sleep apnea is a common co-occurring condition. The weight gain and muscle relaxation that come with hypothyroidism can cause the airway to collapse at night.
If you snore heavily and wake up feeling unrefreshed, get a sleep study. Treating sleep apnea alone can sometimes dramatically improve thyroid function and ED.
The Psychological Impact You Should Not Ignore
We cannot overlook the mental toll of this condition. Hypothyroidism causes neuroinflammation, which leads to brain fog, anxiety, and depression. When you feel depressed, your libido drops. When you experience ED, performance anxiety kicks in. This creates a psychological loop that reinforces the physical problem.
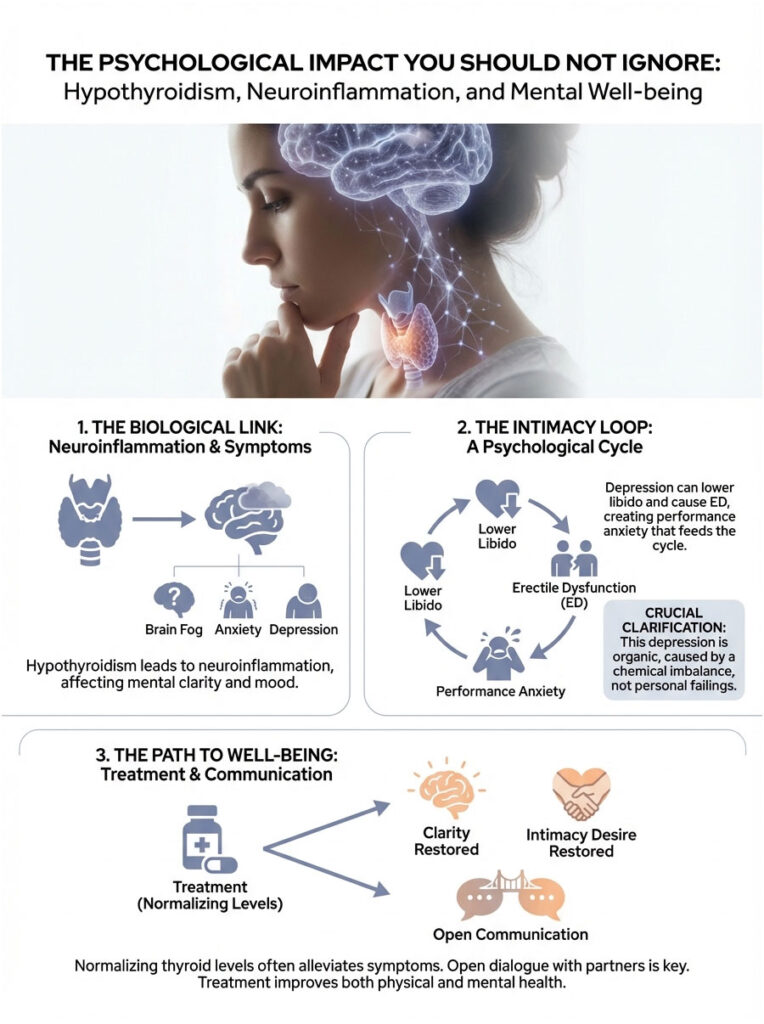
It is important to recognize that this depression is organic. It is driven by a chemical imbalance, not a personal failing. As thyroid levels normalize, the brain fog lifts, and the mental desire for intimacy typically returns.
If you are struggling, communicate openly with your partner. Let them know this is a medical condition you are actively treating, not a loss of attraction.
Key Takeaways
So, can hypothyroidism cause muscle loss and ED in men? Absolutely. It is a systemic issue that goes far beyond feeling tired. It is a metabolic crisis that touches every system involved in male performance.
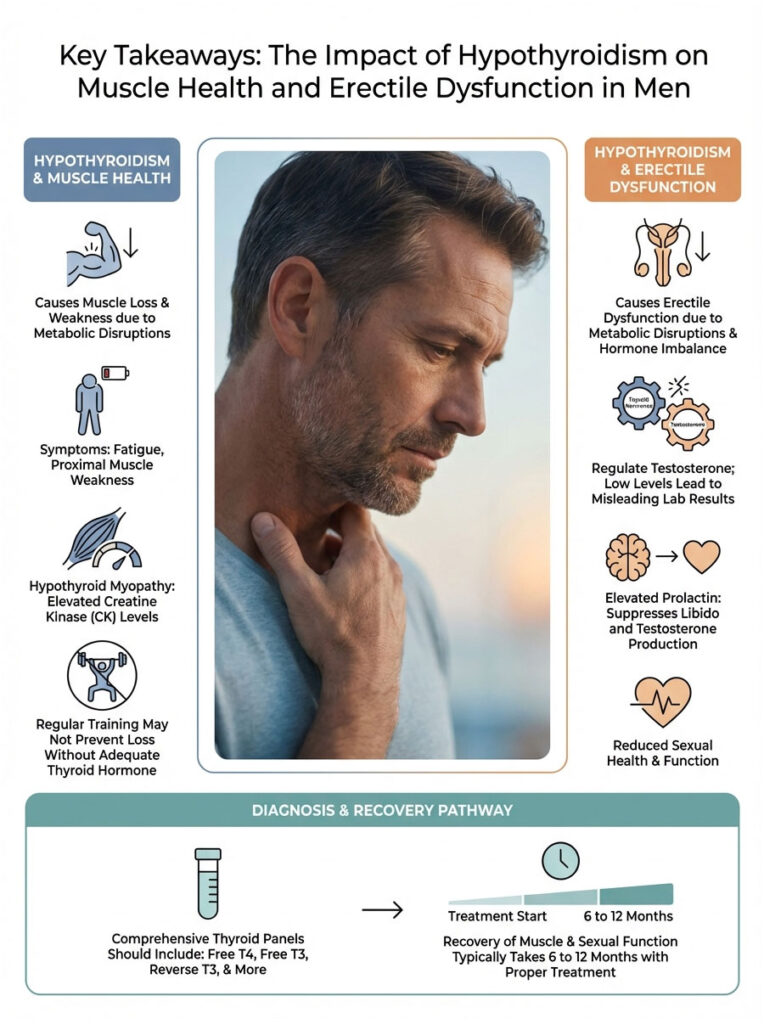
- Hormonal Disruption: Hypothyroidism lowers SHBG (reducing bioavailable testosterone) and elevates Prolactin (suppressing natural testosterone production).
- Muscle Wasting: It causes Hypothyroid Myopathy by deactivating satellite cells and preferentially atrophying Type II strength fibers.
- Vascular ED: It depletes Nitric Oxide and stiffens blood vessels, making erections mechanically difficult even when desire is present.
- Diagnostic Gap: Standard TSH tests frequently miss the severity. A full panel including Free T3, Free T4, and Reverse T3 is necessary.
- The Solution: Proper hormone replacement (T4 and potentially T3) combined with a high-protein diet and adjusted training can reverse these symptoms within 6 to 12 months.
If you have been suffering in silence, relying on caffeine to drag yourself through the day and ED medication to get through the night, it is time to look at your thyroid. This is not a permanent sentence. With the right treatment, your strength, muscle mass, and sexual health can return. Do not accept “normal” lab results if you do not feel normal. Advocate for yourself and get the comprehensive care you deserve.
Frequently Asked Questions
Can hypothyroidism cause muscle loss and erectile dysfunction in men?
Yes, hypothyroidism acts as a systemic metabolic brake that directly inhibits muscle satellite cell activation and reduces Nitric Oxide availability. This hormonal deficiency leads to a state of metabolic suspension where the body prioritizes organ survival over muscle hypertrophy and reproductive function, clinically manifesting as muscle atrophy and erectile dysfunction.
Why are my testosterone levels normal on lab tests if I have symptoms of ED and hypothyroidism?
Thyroid hormones regulate the production of Sex Hormone-Binding Globulin (SHBG) in the liver. When thyroid levels are low, SHBG drops, causing testosterone to be metabolized and cleared from the bloodstream too quickly; this results in a “normal” Total Testosterone lab result while your Bioavailable Testosterone is critically low and unable to stimulate your tissues.
How does an underactive thyroid contribute to high prolactin and low libido?
In a hypothyroid state, the brain releases excess Thyrotropin-Releasing Hormone (TRH) to stimulate the thyroid, which has the “dirty” side effect of triggering the pituitary to release Prolactin. Elevated Prolactin acts as a chemical castration agent in men, suppressing Gonadotropin-Releasing Hormone (GnRH) and effectively shutting down natural testosterone production and sexual desire.
What are the specific signs of hypothyroid myopathy in men?
Hypothyroid myopathy typically presents as proximal muscle weakness, making it physically difficult to climb stairs, stand from a low chair, or lift your arms above your head. You may also experience elevated Creatine Kinase (CK) levels in your blood, which is a hallmark indicator of active muscle tissue breakdown and metabolic damage.
Why am I losing muscle mass even though I am training regularly in the gym?
Sufficient T3 levels are required to activate muscle satellite cells, which are the stem cells responsible for repairing micro-tears after a workout. Without enough thyroid hormone, the repair phase never happens, leading to a net loss of Type II fast-twitch fibers and a catabolic state where you are effectively breaking down muscle without the ability to rebuild it.
What is the best thyroid blood panel for men experiencing ED and muscle weakness?
A comprehensive male thyroid panel must go beyond TSH and include Free T4, Free T3, and Reverse T3 to assess cellular fuel availability. Additionally, I recommend testing for TPO antibodies to rule out Hashimoto’s, as well as checking SHBG, Prolactin, and Creatine Kinase (CK) to understand the full impact on your hormonal and muscular systems.
Can I take testosterone replacement therapy (TRT) while on thyroid medication?
Yes, TRT and thyroid medications can be used synergistically, but the thyroid must be stabilized first to ensure the cellular machinery is “online” to utilize the testosterone. It is important to note that starting TRT can lower thyroid-binding proteins, so your endocrinologist will likely need to adjust your thyroid dosage once testosterone therapy begins.
Why does hypothyroidism cause delayed ejaculation or difficulty reaching orgasm?
Thyroid hormone dictates the speed of nerve impulse transmission throughout the body. In a hypothyroid state, nerve conduction velocity slows down, which affects the autonomic nervous system and often leads to delayed ejaculation or anorgasmia because the neural reflexes required for climax are significantly dampened.
What is the typical recovery timeline for regaining muscle and sexual function?
Initial energy improvements and reduced water retention often occur within the first month of treatment. However, it typically takes 3 to 6 months for libido and erectile quality to normalize as Nitric Oxide levels restore, and 6 to 12 months for full muscle protein synthesis and hypertrophy to return to their optimal states.
Why do ED medications like Cialis or Viagra often fail in hypothyroid patients?
These medications work by amplifying Nitric Oxide (NO) signals, but hypothyroidism causes endothelial dysfunction that prevents the blood vessels from producing NO in the first place. If your body is not generating the baseline chemical messenger, PDE5 inhibitors have nothing to amplify, making thyroid restoration a prerequisite for successful ED treatment.
Is it possible for hypothyroidism to make my muscles look bigger but feel weaker?
Yes, this phenomenon is often caused by the accumulation of glycosaminoglycans in the muscle tissue, which attracts water and creates a “puffy” or “boggy” appearance. This is not functional muscle but rather intramuscular edema—sometimes called Hoffman’s Syndrome—which causes the muscle to feel stiff, painful, and significantly weaker despite the increased size.
Which dietary supplements help support thyroid function and muscle repair in men?
Selenium and Zinc are the most critical micronutrients for converting T4 into the active T3 hormone and supporting Leydig cell function in the testes. I also recommend increasing protein intake to 1.6–2.0 grams per kilogram of body weight to provide the necessary amino acids for tissue repair while the body recovers from a catabolic hypothyroid state.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The content is based on clinical observations and endocrine research but should not replace the diagnosis or treatment plan of a qualified healthcare professional. Always consult with your doctor before starting new medications or supplements, especially regarding hormonal health.
References
- Journal of Clinical Endocrinology & Metabolism – https://academic.oup.com/jcem – Research on the prevalence of sexual dysfunction in men with thyroid disorders.
- American Thyroid Association (ATA) – https://www.thyroid.org – Clinical guidelines for the diagnosis and management of hypothyroidism.
- Endocrine Society – https://www.endocrine.org – Expert insights into the Hypothalamic-Pituitary-Thyroid (HPT) axis and male reproductive health.
- Mayo Clinic Proceedings – https://www.mayoclinicproceedings.org – Clinical review of hypothyroid myopathy and its effect on skeletal muscle enzymes.
- The Journal of Sexual Medicine – https://www.jsm.jsexmed.org – Studies linking thyroid hormone levels to Nitric Oxide production and erectile quality.
- National Institutes of Health (NIH) – https://www.ncbi.nlm.nih.gov/pmc/ – Research papers on the role of T3 in satellite cell activation and muscle fiber repair.
- Cleveland Clinic – https://my.clevelandclinic.org – Data regarding the impact of high Prolactin and low SHBG on bioavailable testosterone.








