Disclaimer: This content is for informational purposes only and does not constitute medical advice. Always consult your hepatologist or dietitian before making drastic dietary changes.
Can you eat red meat with fatty liver? Yes, patients with fatty liver disease (MASLD) can eat red meat, but strict moderation is required. While trimming the fat significantly reduces saturated fatty acids, which drive liver inflammation, it does not remove heme iron, a compound linked to oxidative stress. Current AASLD guidelines suggest limiting red meat to 1 serving (3 oz) per week, choosing lean beef cuts like sirloin or eye of round, and using moist-heat cooking methods like stewing to avoid toxic inflammatory spikes.
Table of Contents
The Meat-Eater’s Dilemma
You just left the doctor’s office with a diagnosis that feels heavy. Perhaps they used the term NAFLD or the newer, more accurate medical term MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease). The advice was likely standard and somewhat vague. Lose weight. Exercise more. Eat better. But for many people, “eating better” creates a specific, gnawing anxiety. Does this mean you can never enjoy a steak again?

It is a fair and difficult question. Beef is deeply ingrained in culinary culture. It is the centerpiece of summer barbecues, the star of holiday roasts, and the comfort food we turn to after a long week. The idea of a life committed solely to steamed broccoli and boiled chicken can feel discouraging enough to derail your diet before it even starts. When food loses its joy, compliance drops, and health suffers.
Here is the reality. The relationship between red meat and fatty liver disease risk is not black and white; it is nuanced. It depends entirely on what you eat, how much of it you eat, and exactly how you cook it. The liver is a resilient organ with an incredible capacity for regeneration, but it is also biologically sensitive to specific inflammatory triggers found in animal products.
We are going to dismantle the old “all-or-nothing” approach. Instead, we will look at the biochemistry of saturated fat and liver inflammation, explore the “Lean Cut Loophole,” and apply strategies from the longest-living populations on earth to help you manage your liver health without losing your mind. We will explore how to make informed choices that allow you to navigate social situations and family dinners without compromising your metabolic health.
The Core Concept: Why Is Red Meat a Risk Factor for MASLD?
To understand how to eat safely, you must first understand the mechanism of injury. Why exactly do hepatologists and dietitians worry about beef consumption MASLD? It is not just about calories, nor is it simply about “fat makes you fat.” The biological impact of red meat on the liver involves three distinct, interconnected pathways: lipotoxicity, oxidative stress, and the insulin response.
The Role of Saturated Fatty Acids (SFA)
The white marbling that makes a ribeye steak so tender and flavorful is primarily composed of saturated fatty acids. When you consume these fats in excess, they do not merely sit in your adipose tissue or expand your waistline. They travel directly to the liver via the portal vein.
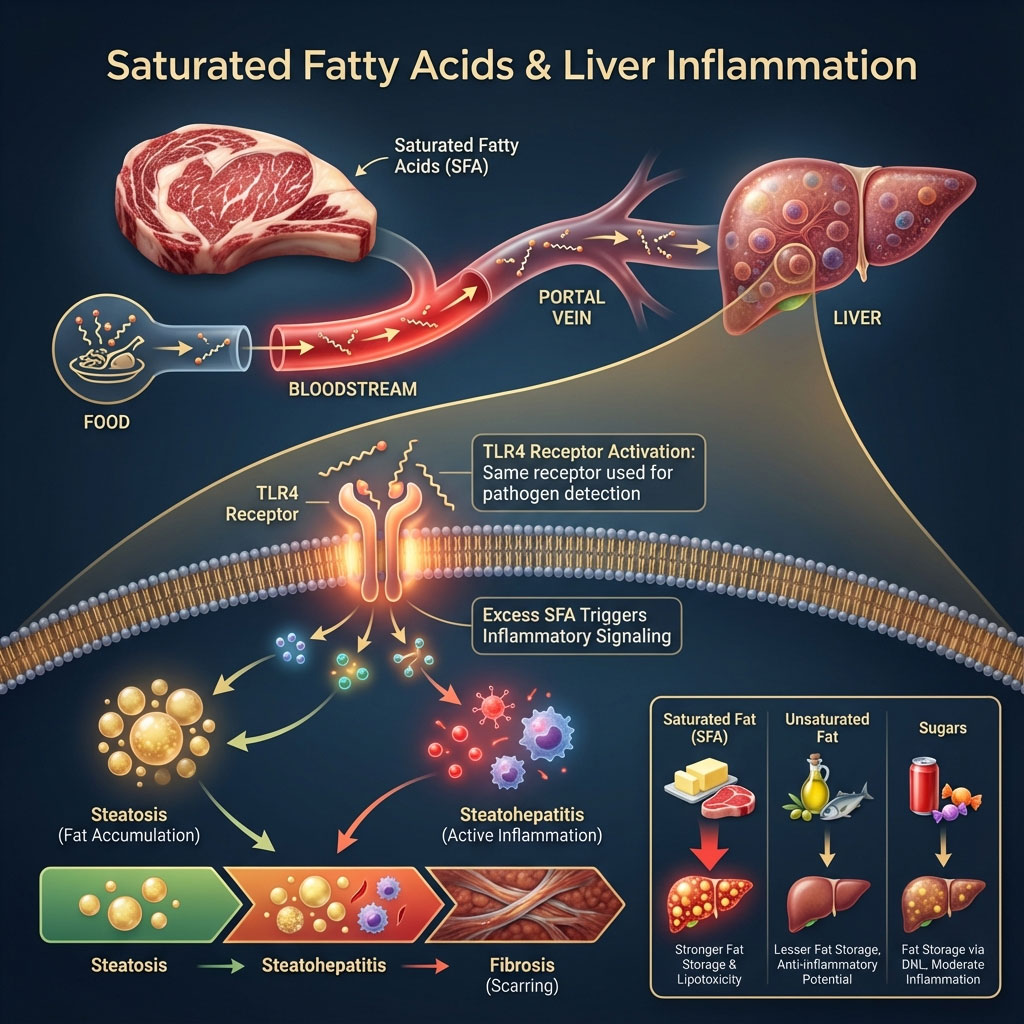
Once in the liver, these saturated fats act as potent signaling molecules. They are not biologically inert. They activate a specific receptor on the liver cells known as the TLR4 receptor (Toll-Like Receptor 4). This is the same receptor that the body uses to detect bacteria and pathogens. Essentially, high intake of saturated fat tricks your liver into thinking it is under attack by an infection.
This activation triggers a cascade of inflammation. It turns simple fat accumulation (steatosis), which is relatively benign, into active inflammation (steatohepatitis). This is the dangerous bridge between a reversible fatty liver and permanent liver fibrosis or scarring. Research consistently shows that saturated fat and liver inflammation are tightly linked. SFA increases liver fat storage significantly more than unsaturated fats or even sugars in some metabolic contexts because it induces this state of “lipotoxicity,” where the fat itself damages the cellular machinery.
The Hidden Danger: Heme Iron and Oxidative Stress
This is the factor most people miss, and it is crucial for understanding why lean meat is still a concern. You can trim every ounce of visible white fat off a steak, but the meat remains red. That red color comes from myoglobin, a protein that contains heme iron.
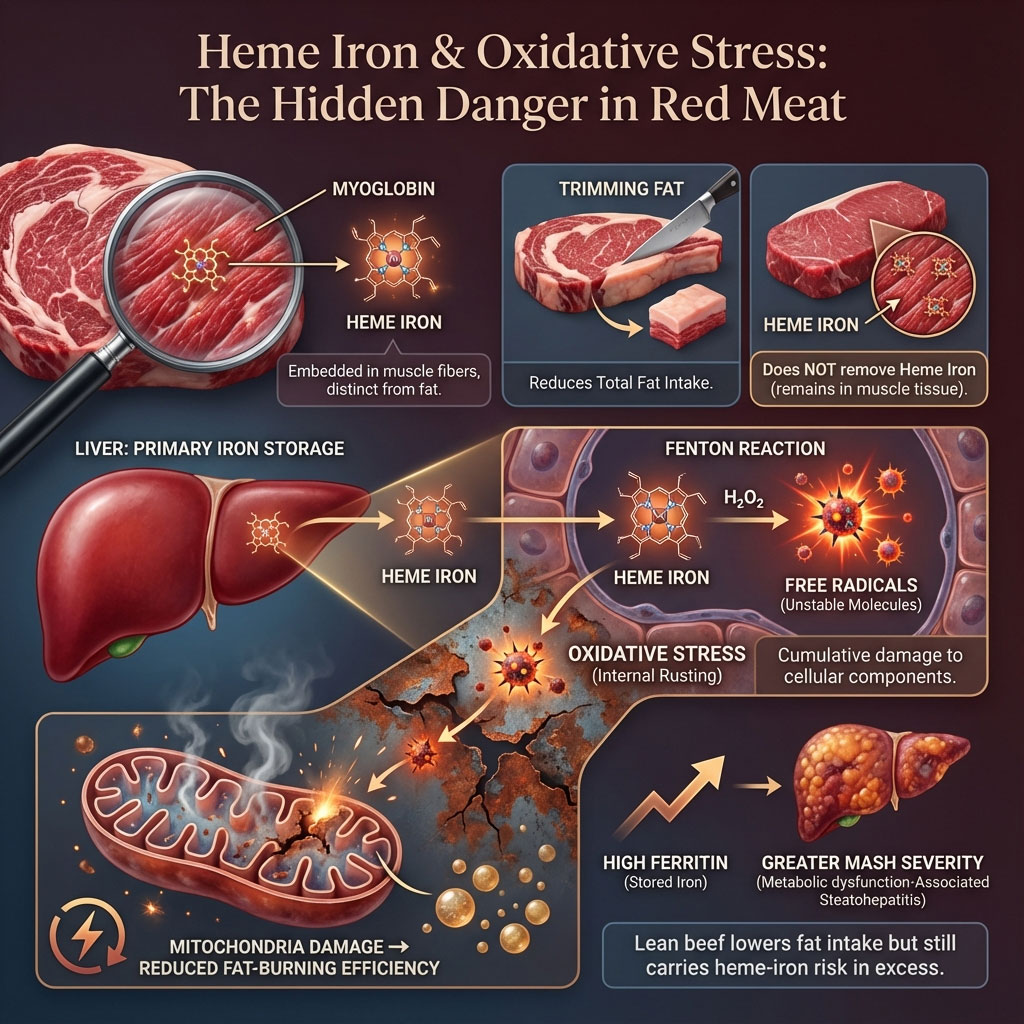
Iron is a heavy metal. While your body needs it for red blood cells to transport oxygen, the liver is the primary storage organ for excess iron. In the context of MASLD, excess iron is like pouring gasoline on a smoldering fire. It catalyzes a chemical reaction known as the Fenton reaction. This reaction produces free radicals, which are unstable molecules that strip electrons from healthy cells.
These free radicals cause oxidative stress, literally “rusting” the liver cells from the inside out. This damage injures the mitochondria, the power plants of your cells, making them less efficient at burning fat. High ferritin levels, a marker of iron storage, are frequently associated with greater severity of MASH (Metabolic Dysfunction-Associated Steatohepatitis). This is why lean beef for fatty liver is better than fatty beef, but it is still not perfectly safe in large quantities. The iron remains in the muscle fiber itself.
Insulin Resistance and Protein Source
MASLD is fundamentally a metabolic disorder. It is the liver manifestation of metabolic syndrome, often co-occurring with type 2 diabetes or pre-diabetes. The amino acid profile of red meat, particularly branched-chain amino acids, can stimulate insulin secretion more aggressively than plant-based proteins.
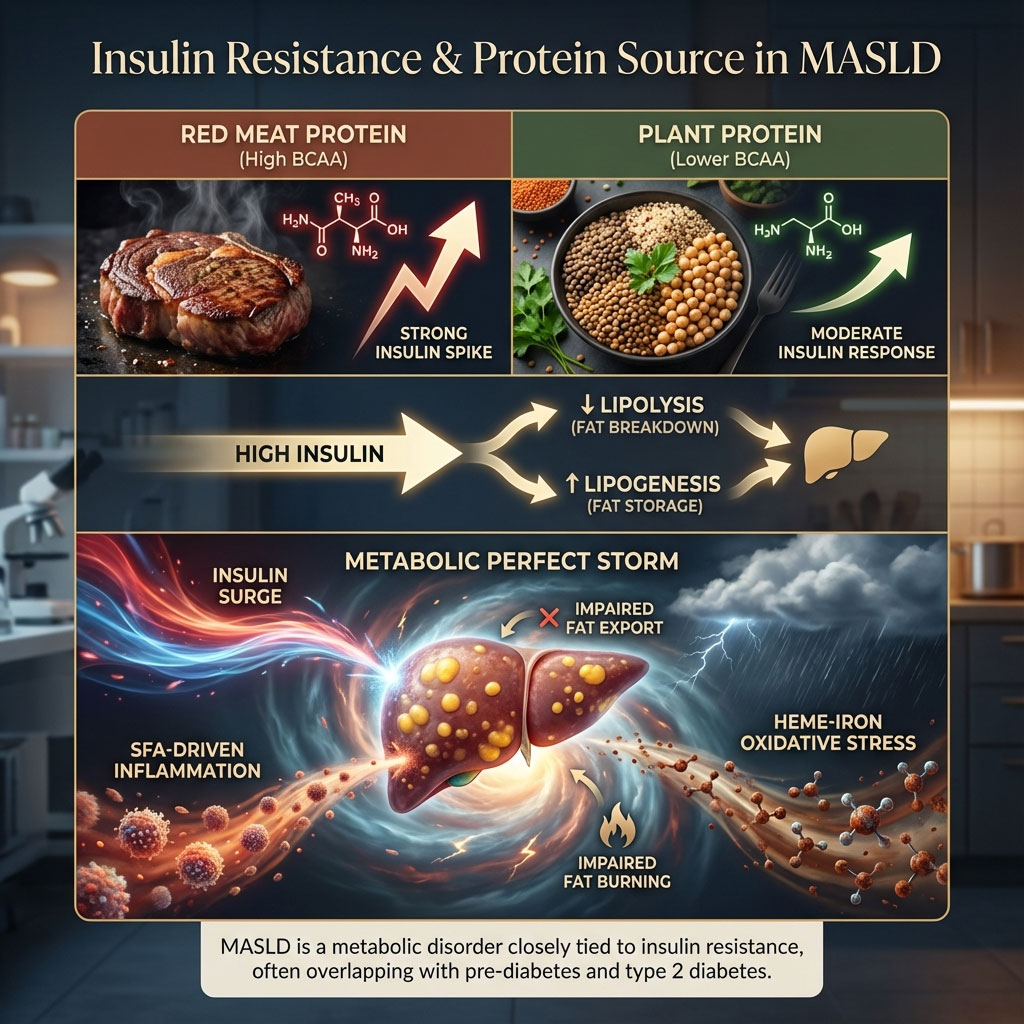
Chronic spikes in insulin prevent the liver from breaking down fat (lipolysis) and encourage it to store new fat (lipogenesis). When you combine the insulin spike from a heavy meal with the inflammatory hit from saturated fat and the oxidative stress from heme iron, you create the perfect storm for liver injury. The liver becomes overwhelmed, unable to export fat or burn it for energy, leading to further accumulation and inflammation.
The Big Question: Is Steak Safe If You Trim the Fat?
This is one of the most common questions asked in the hepatology clinic. Patients want to negotiate. Is steak safe if you trim the fat? The answer requires us to look at the anatomy of the meat itself and the limitations of kitchen surgery.
The Benefit of Trimming
Does trimming fat from steak reduce fatty liver risk? Yes, absolutely. By surgically removing the visible rim of white fat (subcutaneous fat) from a steak, you are directly removing a concentrated source of inflammatory saturated lipids. You are also reducing the total caloric load of the meal. Since weight loss is the primary treatment for MASLD, any reduction in caloric density is a therapeutic win.

For example, trimming the fat off a standard sirloin steak can save upwards of 10 to 15 grams of fat and over 100 calories. Over the course of a year, these small reductions add up significantly. If you are going to eat steak and MASLD (fatty liver) is part of your medical history, trimming is non-negotiable. It is the first line of defense and the easiest variable to control.
The Limitation (What Trimming Doesn’t Do)
However, trimming has limits. You can remove the subcutaneous fat, which is the strip on the outside of the steak. You cannot easily remove the intramuscular fat, the marbling inside the muscle fibers that gives high-quality beef its texture. In cuts like Ribeye, T-Bone, or Wagyu beef, this internal marbling is substantial and inextricable. Even a “trimmed” ribeye is still a high-fat food.

Furthermore, as discussed, trimming fat does nothing to reduce heme iron oxidative stress. The muscle tissue itself carries the iron load. Therefore, while trimming makes the meat safer, it does not turn a steak into a “free food” like a chicken breast or a fillet of white fish. The metabolic impact is lessened, but the inflammatory potential remains.
The Verdict
Trimming fat transforms a “high-risk” food into a “moderate-risk” food. It allows you to fit red meat fatty liver protocols occasionally, but it does not grant permission for daily consumption. It is a harm-reduction strategy, not a cure. It allows you to participate in the meal, but the portion size and frequency must still be strictly managed to prevent the accumulation of liver fat.
Strategic Selection: The “Lean Cut Loophole”
If you are going to eat beef, you must become a strategic shopper. Not all cows are created equal, and not all cuts carry the same metabolic penalty. The USDA defines “lean” cuts specifically, and adhering to this list is your best bet for navigating red meat and fatty liver disease risk. Learning to identify these cuts at the butcher counter is a critical skill for managing your health.
Defining “Lean” for Liver Health
According to USDA standards, a “lean” cut of beef must contain less than 10 grams of total fat, 4.5 grams or less of saturated fat, and less than 95 milligrams of cholesterol per 3.5-ounce serving. For a patient with MASLD, you want to aim even lower than that if possible. You are looking for cuts that look red and firm, not white and speckled.
The “Safe List” (Best Cuts)
These are the cuts that fit into a liver-conscious diet when eaten in moderation.

- Eye of Round: This is often called the “gold standard” for leanness. It comes from the leg of the cow, a muscle that does a lot of work, meaning it stores very little fat. It is lean, but it can be tough. It requires slow cooking, thin slicing, or marinating to break down the muscle fibers.
- Sirloin Tip Side Steak: This cut offers robust beef flavor with significantly less fat than the loin cuts. It is versatile and works well in stir-fries where you can stretch a small amount of meat with a large amount of vegetables.
- Top Round: This is a budget-friendly cut that is incredibly lean. It is the ideal candidate for lean beef for fatty liver recipes involving stewing or braising, as moist heat helps tenderize it without adding fat.
- Top Sirloin: If you are at a steakhouse, this is your safest order. It is tender enough to grill gently but lacks the heavy fat load of a ribeye or porterhouse.
- Flank Steak: While lean, flank steak is long and flat with a distinct grain. It is best marinated to prevent charring and sliced against the grain. It is a favorite for fajitas or salads where portion control is easier to maintain.
The “Danger List” (Cuts to Avoid)
These cuts contain levels of saturated fat that can trigger immediate inflammation in a compromised liver. They should be viewed as “red light” foods.
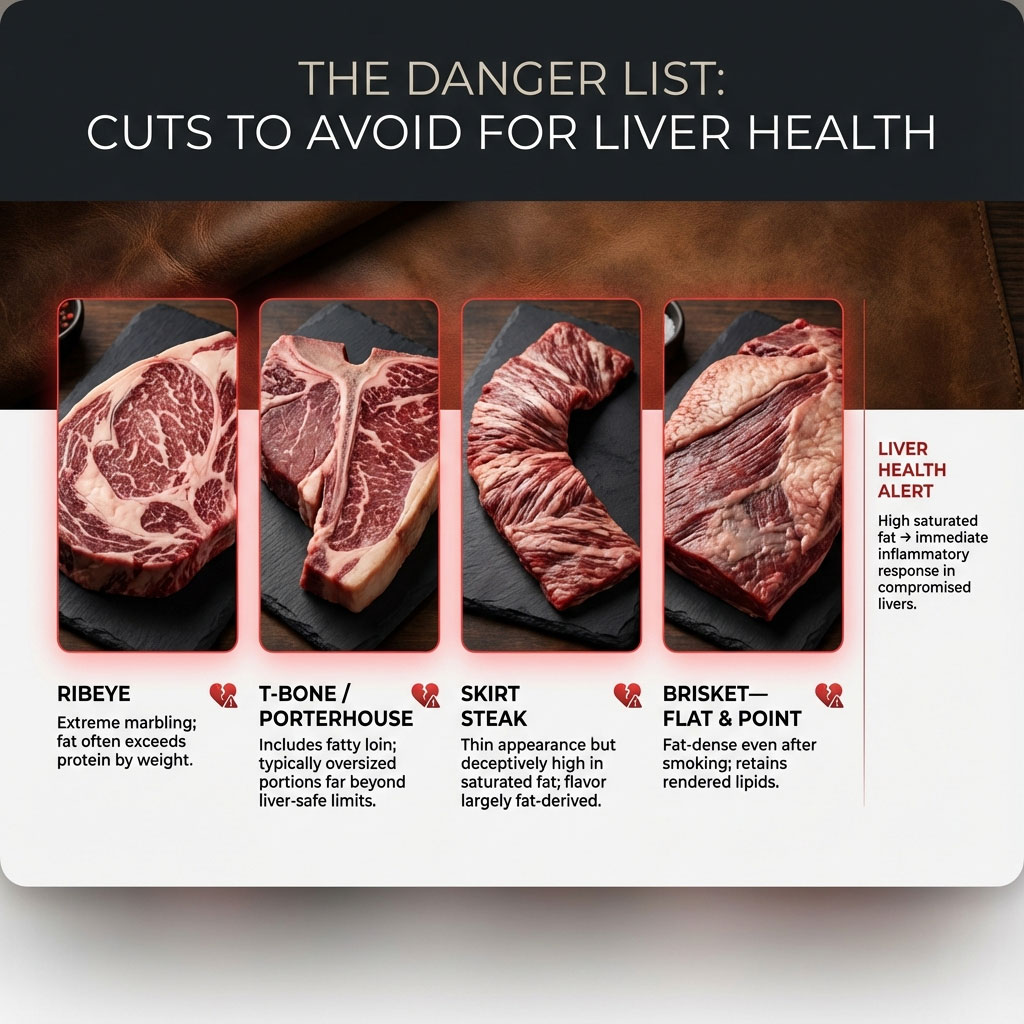
- Ribeye: This is arguably the most dangerous cut for a fatty liver patient due to heavy marbling. The fat content is often higher than the protein content by weight in premium cuts.
- T-Bone and Porterhouse: These cuts include the fatty loin section and are typically served in enormous portions that far exceed liver-safe limits.
- Skirt Steak: Often deceptively fatty despite looking thin. It is known for its rich flavor, which is derived almost entirely from its high fat content.
- Brisket (Flat and Point): While delicious when smoked, brisket is an inherently fatty cut that retains a significant amount of rendered lipids even after cooking.
Processed vs. Unprocessed Red Meat: A Critical Distinction
We must draw a hard line here. The difference between processed vs unprocessed red meat is not a matter of degree; it is a difference in kind. They behave differently in the body.

Processed meats include bacon, sausage, pepperoni, salami, hot dogs, beef jerky, and deli ham. These products are preserved with nitrates, nitrites, and massive amounts of sodium. Nitrates can be converted in the body into nitrosamines, compounds that are directly toxic to the liver and are linked to insulin resistance and increased liver stiffness. Sodium causes fluid retention and hypertension, which worsens the metabolic profile of MASLD patients.
Unprocessed red meat fatty liver risks are manageable with portion control. Processed meat risks are not. If you have fatty liver, processed meats should be eliminated entirely from your diet. There is no “safe” amount of bacon for an inflamed liver.
Comparative Analysis: Meat Types & Liver Impact
To visualize why your choice of protein matters, consider this comparison of how different meats interact with liver pathology. This table breaks down the risks associated with common protein choices.
| Meat Type | Saturated Fat Content | Heme Iron Level | Additives/Toxins | Risk Level for MASLD |
| Processed (Bacon/Sausage) | High | High | Nitrates & Sodium (Very High) | 🔴 Critical Risk |
| Fatty Beef (Ribeye) | High | High | HCAs (if grilled) | 🔴 High Risk |
| Lean Beef (Sirloin) | Low-Medium | High | None (if fresh) | 🟡 Moderate Risk |
| Lean Pork (Tenderloin) | Low | Medium | None (if fresh) | 🟡 Moderate Risk |
| White Meat (Chicken) | Low | Low | None | 🟢 Safe / Low Risk |
| Plant Protein (Lentils) | None | Non-Heme (Safe) | Fiber (Beneficial) | 🟢 Beneficial |
It is clear from this comparison that moving down the chart correlates with better liver outcomes. Plant proteins not only lack the harmful elements (saturated fat and heme iron) but actively contribute beneficial elements (fiber and phytonutrients).
Advanced Toxicology: Cooking Methods Matter
You can buy the most expensive grass-fed Eye of Round, but if you cook it wrong, you can still damage your liver. The method of preparation is just as critical as the cut itself. This brings us to healthy cooking methods for red meat.
The Grill Trap (HCAs and PAHs)
When meat muscle is subjected to high temperatures, such as direct flame grilling or pan-frying, a chemical reaction occurs. Amino acids, sugars, and creatine in the meat react to form Heterocyclic Amines (HCAs). When fat drips onto hot coals and smokes up, it coats the meat in Polycyclic Aromatic Hydrocarbons (PAHs).
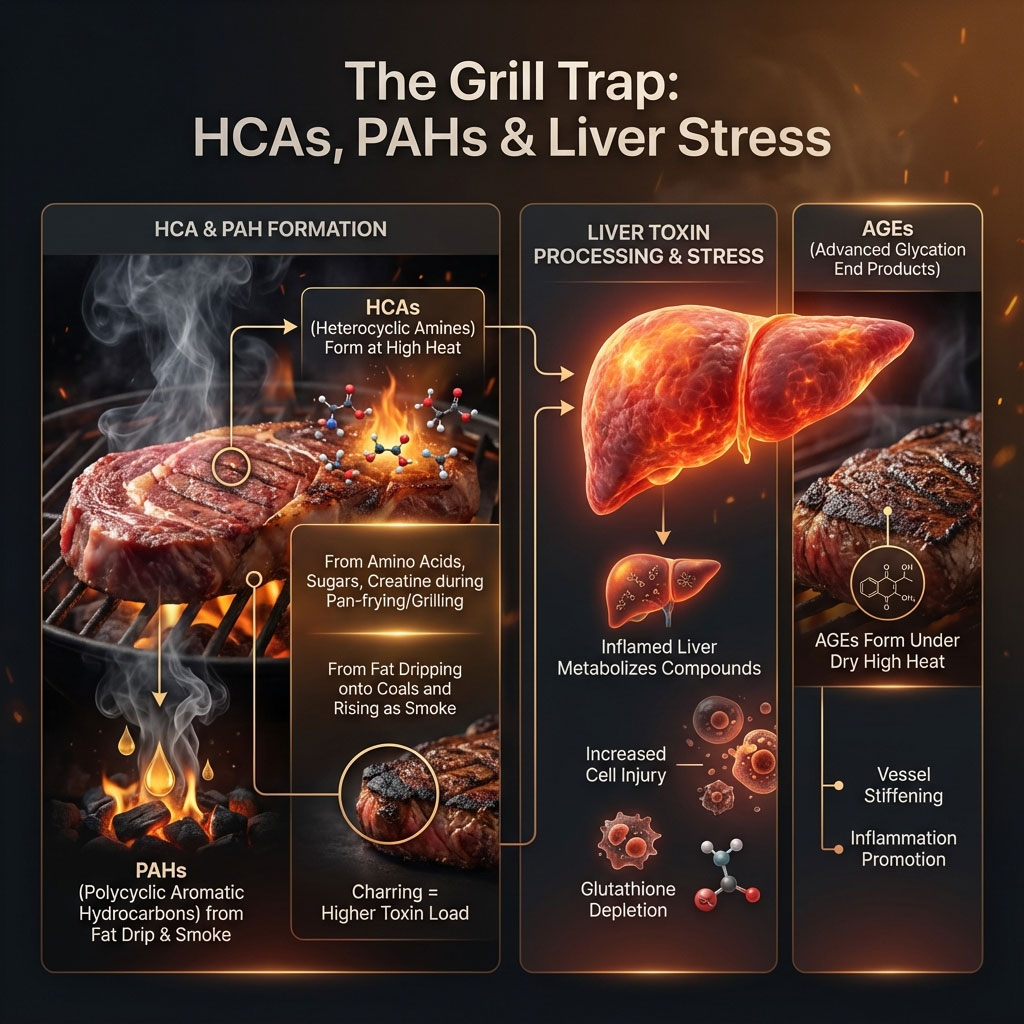
These are toxins. Your liver is the organ responsible for filtering toxins from the blood. When you eat charred meat, you force an already inflamed liver to work overtime to metabolize these difficult compounds. This added stress can exacerbate cell injury and depletion of glutathione, the liver’s master antioxidant. Furthermore, high dry heat creates Advanced Glycation End Products (AGEs), which are sticky compounds that can stiffen blood vessels and promote inflammation in the liver tissue.
Safe Cooking Techniques
To minimize red meat fatty liver complications, you need to use moist heat and lower temperatures. This prevents the formation of these toxins.

- Stewing and Braising: Submerging meat in liquid prevents the temperature from exceeding the boiling point of water (212°F). This virtually eliminates HCA formation. The long cooking time breaks down the collagen in lean cuts like round steak, making them tender without the need for fat.
- Boiling and Poaching: While less flavorful for beef, these are the safest methods toxicologically. They are traditional in many cultures (such as Pot-au-Feu in France) and are extremely liver-friendly.
- Slow Cooking (Crockpot): This renders out the fat over several hours. The fat floats to the top of the cooking liquid and can be skimmed off and discarded before serving. This further reduces the saturated fat and liver inflammation load of the final dish.
- Sous Vide: Cooking meat in a water bath at precise, low temperatures ensures tenderness in lean cuts without any risk of charring or oxidation.
Case Study Evidence: Clinical observations have noted that populations consuming mostly boiled or stewed meats have lower elevations in liver enzymes compared to those consuming mostly fried or grilled meats, even when total meat intake is similar. The “Western” diet is characterized not just by high meat intake, but by high dry-heat cooking.
The “Green Med” Protocol: A Modern Diet Strategy
The conversation around liver health is shifting. We are moving away from simple “low fat” advice toward a more sophisticated “Green Mediterranean” approach. This is the gold standard for MASLD nutritional therapy.

The Mankai Duckweed & Green Tea Connection
Recent high-profile research, specifically the DIRECT-PLUS trial, has illuminated a new path. Researchers found that a “Green Mediterranean” diet—which restricts red meat and adds specific green plants—was superior for liver health compared to standard healthy diets.
Participants who replaced red meat fatty liver dietary patterns with Mankai duckweed shakes (a tiny aquatic plant rich in protein and polyphenols), green tea (3-4 cups daily), and walnuts saw the most significant reduction in intra-hepatic fat. This suggests that it is not just about removing the bad (meat) but adding the good (polyphenols). Polyphenols act as fuel for beneficial gut bacteria and directly reduce oxidative stress in the liver.
Substitution Strategy (The “Plus” Approach)
You do not have to become a vegan overnight. The goal is to crowd out the meat. If you usually eat an 8oz steak, try eating a 3oz steak and filling the rest of the hunger gap with lentils, chickpeas, or walnuts.
Plant-based protein fatty liver benefits are well documented. Legumes contain soluble fiber that binds to bile acids in the gut. Since bile is made from cholesterol in the liver, forcing the body to make new bile helps pull cholesterol out of the liver, directly easing the organ’s burden. This is a mechanical “detox” that supplements cannot replicate.
Bio-Hacking Your Steak Dinner
If you are going to eat red meat fatty liver conscious meals, use biochemistry to your advantage. Eating spinach with steak or drinking a cup of coffee or tea with your meal can actually help mitigate the damage.
Spinach is rich in calcium and specific polyphenols. Tea and coffee contain tannins. Both calcium and tannins inhibit the absorption of heme iron in the gut. By pairing these foods with your beef, you reduce the amount of oxidative iron that actually reaches your liver circulation. It is a practical “hack” to lower the biological impact of a treat meal. Think of it as an internal shield.
Action Plan: How Often to Eat Meat with Fatty Liver
Patients often demand a number. They want clarity in a confusing landscape. “Just tell me what I can do.” How often should someone with fatty liver eat red meat?
The Frequency Pyramid
Based on the synthesis of AASLD guidance and nutritional data, here is a safe frequency pyramid for MASLD management.
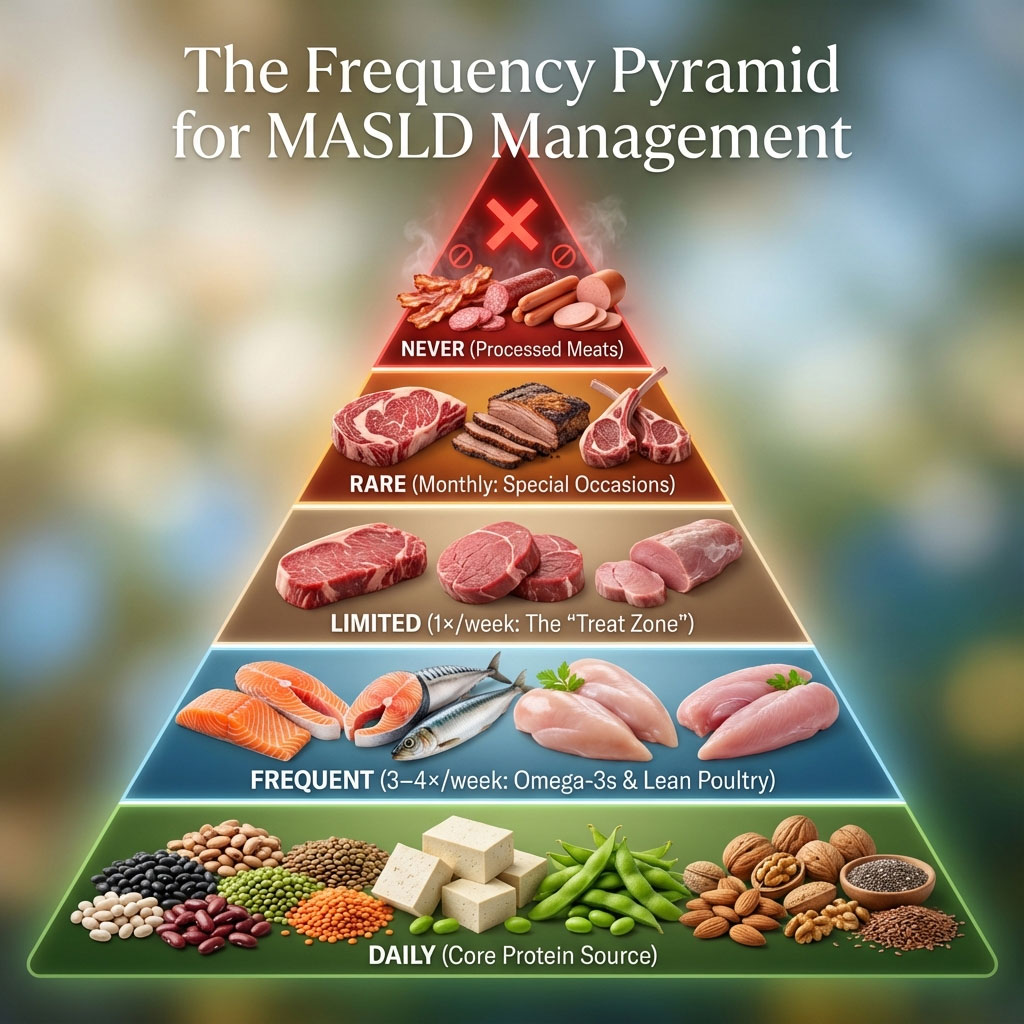
- Daily Base: Plant proteins (beans, lentils, tofu, edamame), nuts, seeds. These should form the foundation of your protein intake.
- Frequent (3-4x week): Fatty fish (Salmon, Mackerel, Sardines for Omega-3s), lean poultry (Chicken breast, Turkey). Omega-3s are actively anti-inflammatory and help resolve liver fat.
- Limited (1x week): Lean beef for fatty liver (Sirloin, round), pork tenderloin. This is the “treat” zone.
- Rare (Monthly/Special Occasion): Fatty cuts (Ribeye, brisket), lamb. These are reserved for weddings, anniversaries, or rare celebrations.
- Never: Processed meats (bacon, salami, hot dogs, bologna). These have no place in a liver-healing diet.
Portion Control Visualization
Portion distortion is a major issue in the United States. A standard restaurant steak is often 12 to 16 ounces, which is four to five times the recommended serving size. A liver-safe portion is 3 ounces.
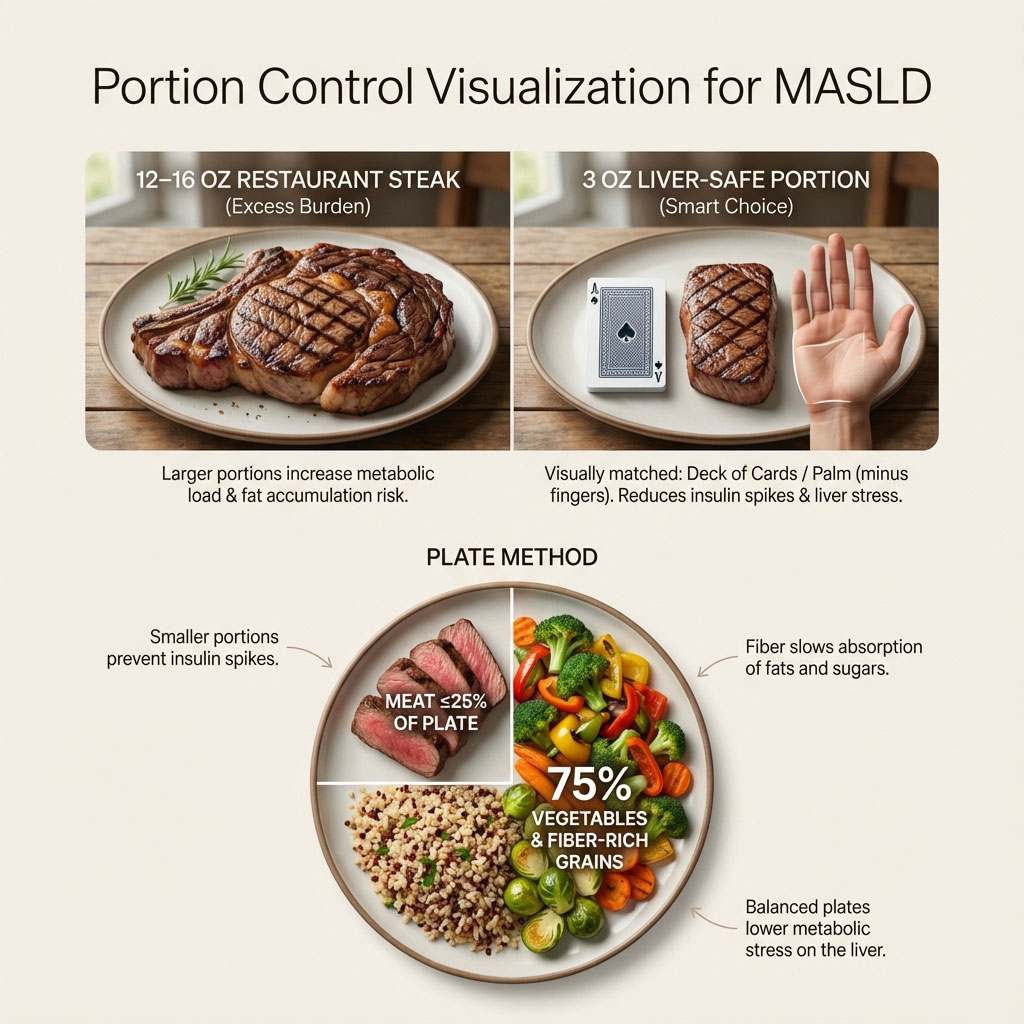
Use the “Deck of Cards” rule. A serving of meat should be roughly the size and thickness of a standard deck of playing cards or the palm of your hand (minus the fingers).
Adopt the “Plate Method.” Meat should be the garnish, occupying no more than one-quarter of the plate. Vegetables and fiber-rich grains should occupy the other three-quarters. This ensures that the glycemic load of the meal remains low, preventing the insulin spikes that drive MASLD progression. The fiber from the vegetables also creates a physical mesh in the stomach that slows the absorption of fats and sugars.
Feature Comparison: The Old Way vs. The New Way
Medical advice evolves as our understanding of biology deepens. Ten years ago, the advice for NAFLD was simply “lose weight.” Today, for MASLD, the advice is far more specific and targeted.
| Feature | Old “NAFLD” Advice | New “MASLD” Authority Approach |
| Diet Focus | “Low Fat” / “Low Calorie” | “Anti-Inflammatory” / “Quality of Fat” |
| Red Meat | “Just eat less.” | “Choose Lean, Limit Iron, Cook Gently.” |
| Cooking | Ignored cooking methods. | Prioritizes stewing/boiling over grilling to avoid toxins. |
| Substitution | Chicken or Fish. | Plant-forward (Legumes) + Green Polyphenols (Tea/Walnuts). |
| Terminology | Passive “Fatty Liver.” | Metabolic Dysfunction (emphasizes insulin/metabolism). |
This shift empowers patients. It moves away from the vague goal of weight loss and toward specific, actionable daily choices that improve liver mechanics regardless of the number on the scale.
The Consultant’s Monday Morning Checklist
Living with MASLD does not require a life of deprivation; it requires a life of intention. Can you eat red meat with fatty liver? Yes. But you must respect the biology of your liver. You must understand that every meal is a signal to your body—either a signal to heal or a signal to inflame.
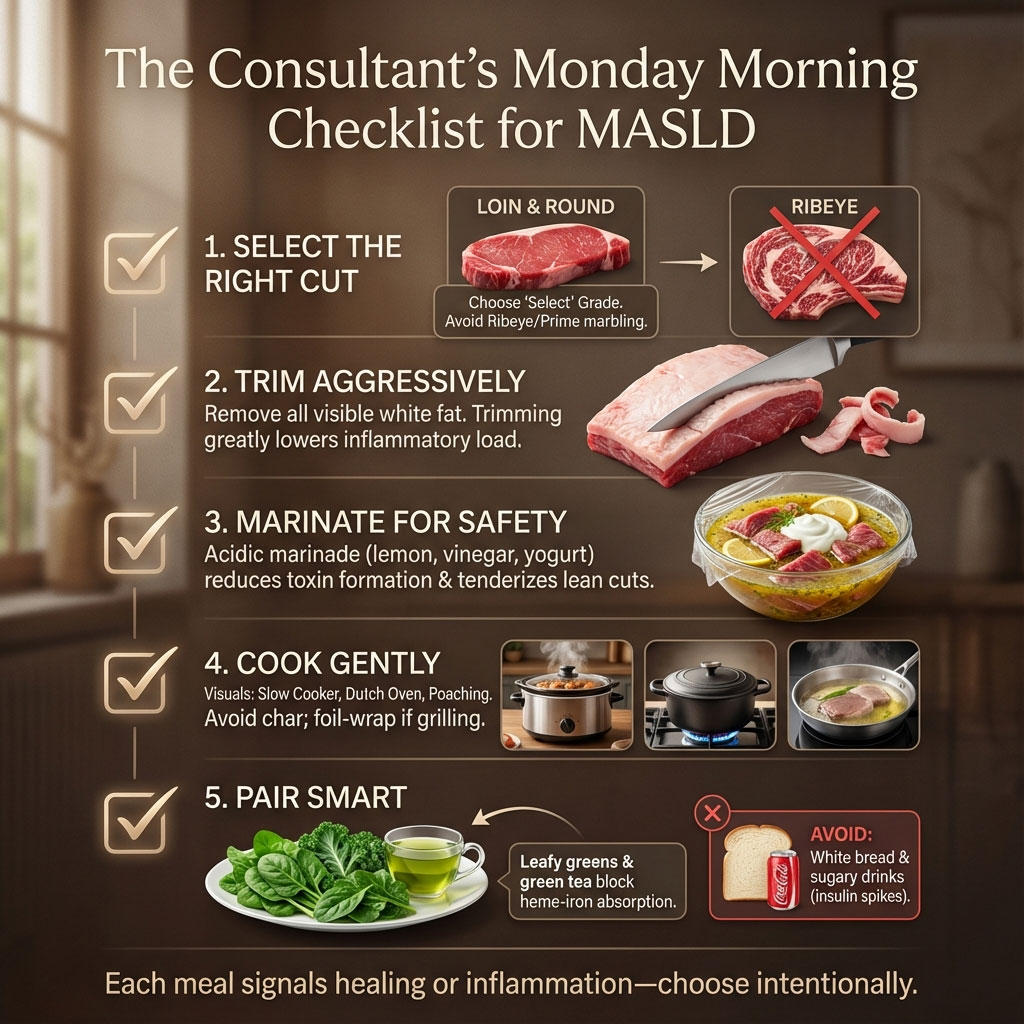
Here is your checklist for the next time you are at the grocery store or planning a meal:
- Select the Right Cut: Buy “Loin” or “Round” cuts only. Leave the Ribeye for the history books. Check the label for “Select” grade rather than “Prime,” as “Select” has less marbling.
- Trim Aggressively: Remove all visible white fat before the meat hits the heat. Is steak safe if you trim the fat? It is much safer than if you don’t. Be your own surgeon in the kitchen.
- Marinate for Safety: Soaking meat in an acidic marinade (lemon juice, vinegar, yogurt) for 30 minutes before cooking can reduce toxin formation and tenderize lean cuts.
- Cook Gently: Use a slow cooker, Dutch oven, or poaching liquid. Avoid the char. If you must grill, wrap the meat in foil to protect it from direct flame.
- Pair Smart: Always eat meat with a massive side of leafy greens or a cup of green tea to block iron absorption. Never eat meat with white bread or sugary drinks, which spike insulin.
Your liver is resilient. It has an incredible capacity to regenerate. It can handle a small amount of lean beef for fatty liver management occasionally. What it cannot handle is a lifestyle of chronic inflammation. Choose your fuel wisely, and your liver will thank you.
Frequently Asked Questions (FAQ)
Can I eat hamburger with fatty liver disease?
Generally, no. Most hamburgers, especially fast-food varieties, are high in saturated fat (often 20-30% fat content) and are cooked at extremely high heat, which creates toxins. If you must have a burger, choose 90% lean ground beef or ground sirloin, grill it gently without charring, and eat it without a white flour bun to avoid the double hit of fat and an insulin spike.
Is pork better than beef for fatty liver?
Lean pork, like tenderloin or loin chops, is comparable to lean beef for fatty liver. It is lower in saturated fat than fatty beef cuts but still contains heme iron and inflammatory potential. It should be treated with the same moderation as beef—limited to once a week. Avoid fatty cuts like pork belly or ribs.
Does grass-fed beef have less fat for liver health?
Yes, grass-fed beef typically has a better fatty acid profile than grain-fed beef. It contains more Omega-3 fatty acids and often less total saturated fat. Omega-3s are beneficial for liver inflammation. However, grass-fed beef still contains heme iron, so it must still be consumed in moderation. It is a better choice, but not a cure-all.
How many ounces of meat per week is safe for MASLD?
Current guidance suggests limiting red meat intake to roughly 3 to 6 ounces per week maximum. This means one or two small servings, prioritizing days with zero meat consumption to lower red meat and fatty liver disease risk. The majority of your protein should come from plants, fish, or poultry.
What is the best lean beef cut for fatty liver?
The Eye of Round is widely considered the best option. It is extremely lean and fits well into MASLD dietary protocols when cooked with moist heat to keep it tender. Top Sirloin is the best option for grilling or pan-searing.
Can trimming fat from steak reverse liver damage?
No, trimming fat cannot reverse existing damage or fibrosis. It acts as a preventative measure to stop further fat accumulation and inflammation. Reversal of liver fibrosis or steatosis usually requires significant weight loss (7-10% of body weight) and a holistic dietary change toward a Mediterranean-style eating pattern.
Are processed meats (bacon) worse than steak?
Yes, absolutely. Processed meats contain nitrates and high sodium that cause oxidative stress and insulin resistance. The risk profile for processed vs unprocessed red meat is vastly different; processed meats are considered critical risks and should be completely avoided by anyone with liver concerns.
Can replacing red meat with legumes reduce fatty liver risk?
Yes. Studies, including the Green Med trials, show that swapping animal proteins for plant proteins like lentils, beans, and chickpeas significantly reduces liver fat and inflammation markers. Legumes provide protein without the inflammatory fat and iron, plus they add fiber which helps detoxify the liver.
Is organ meat (liver) safe for fatty liver patients?
It is generally advised to avoid organ meats like beef liver. While nutrient-dense, they are extremely high in cholesterol and purines, which can exacerbate metabolic issues and uric acid levels often found alongside MASLD. They also contain very high concentrations of iron.
Does coffee help if I eat red meat?
Yes. Coffee is hepatoprotective (liver-protecting). Drinking black coffee can help lower liver enzymes and may inhibit the absorption of iron from the red meat if consumed during or shortly after the meal. It is one of the few beverages actively recommended for liver health.
Why is it called MASLD now?
The name changed from NAFLD (Non-Alcoholic Fatty Liver Disease) to MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) to better reflect that the condition is driven by metabolic factors like insulin resistance and obesity, rather than just defining it by what it is not (alcohol). It reduces stigma and points directly to the cause: metabolism.
Is the Carnivore Diet safe for fatty liver?
The Carnivore Diet is generally considered high-risk for MASLD patients. It is devoid of fiber, which is crucial for gut health and cholesterol excretion, and is extremely high in saturated fat and liver inflammation triggers. While some people lose weight on it initially due to calorie restriction, the long-term impact of such high saturated fat and iron intake on an already compromised liver is medically concerning.








