That persistent bloating, the unexplained fatigue, the nagging feeling that something is just not right after you eat. For millions of Americans, these symptoms are a daily reality, yet an estimated 80% of those with celiac disease remain undiagnosed. The path to answers begins with proper celiac disease screening, a process that is far more nuanced than a simple lab visit. It requires specific, crucial preparation to ensure the results are accurate and trustworthy.
Table of Contents
This comprehensive guide serves as your roadmap to understanding the entire celiac disease diagnosis pathway. We will explore everything from the first warning signs to the most advanced diagnostic tests. Most importantly, we will provide a clear, evidence-based explanation of how to prepare for a celiac blood test, demystifying the “gluten challenge” and empowering you to take the right steps toward a definitive diagnosis. Getting this first step right is the foundation for managing your health and reclaiming your well-being.
Understanding Celiac Disease: Why Screening is Crucial
Before diving into the testing process, it’s essential to grasp why an accurate celiac disease screening is so vital. This condition is not a food allergy or a simple intolerance; it is a serious autoimmune disorder with significant long-term health implications if left unmanaged.
What is Celiac Disease? A Primer
Celiac disease is a genetic autoimmune condition where consuming gluten, a protein found in wheat, barley, and rye, triggers an immune response. This response mistakenly attacks the small intestine, damaging the tiny, finger-like projections called villi. These villi are responsible for absorbing nutrients from food. When they are damaged, the body cannot absorb nutrients properly, leading to malnutrition and a host of other health problems.
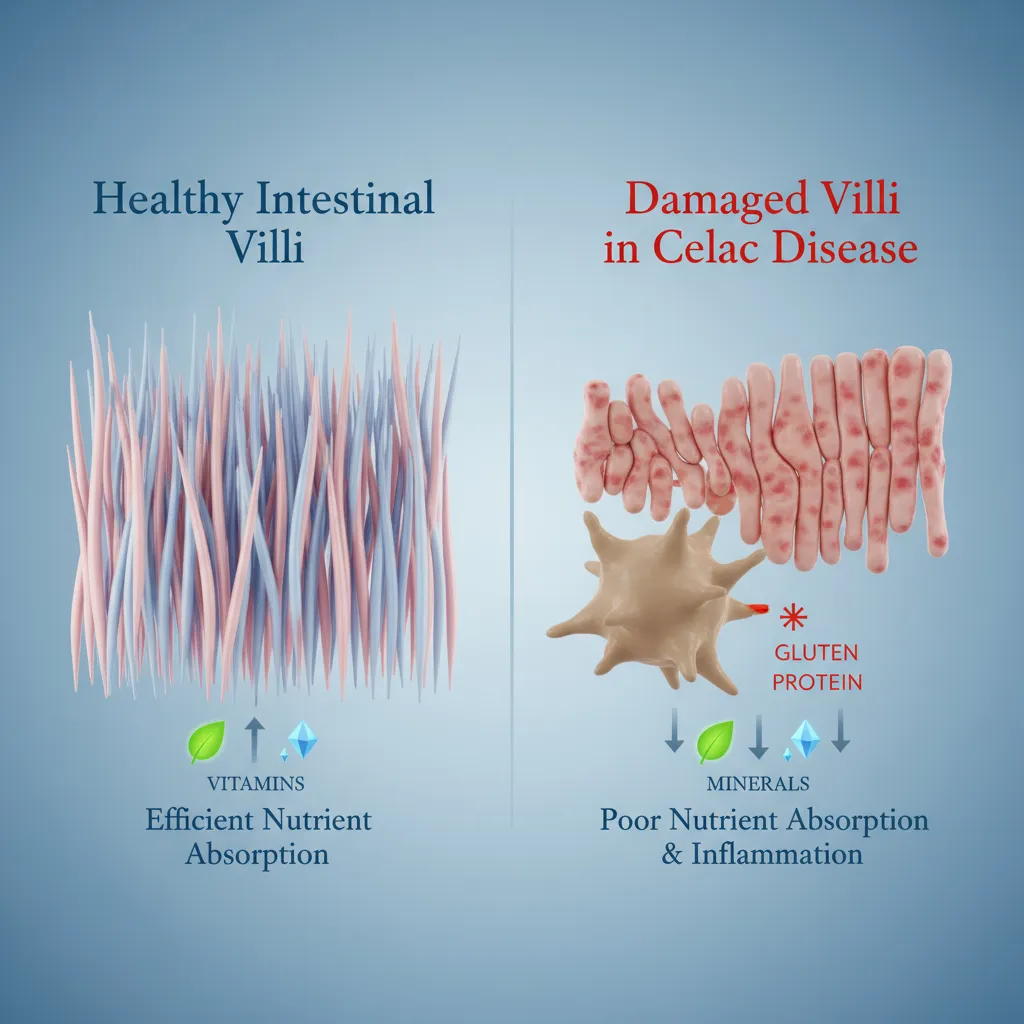
Undiagnosed and untreated, celiac disease can lead to severe complications, including:
- Chronic iron-deficiency anemia
- Early onset osteoporosis or osteopenia
- Infertility and miscarriage
- Neurological conditions like ataxia and neuropathy
- Increased risk of certain types of cancer, such as small bowel cancers and lymphomas
The Alarming Gap: Diagnosed vs. Undiagnosed Cases
Medical experts often refer to the “celiac iceberg” to illustrate the diagnostic gap. For every person with a confirmed celiac disease diagnosis, many more are living with the condition unknowingly. The symptoms can be vague or mimic other conditions, leading to years of misdiagnosis.
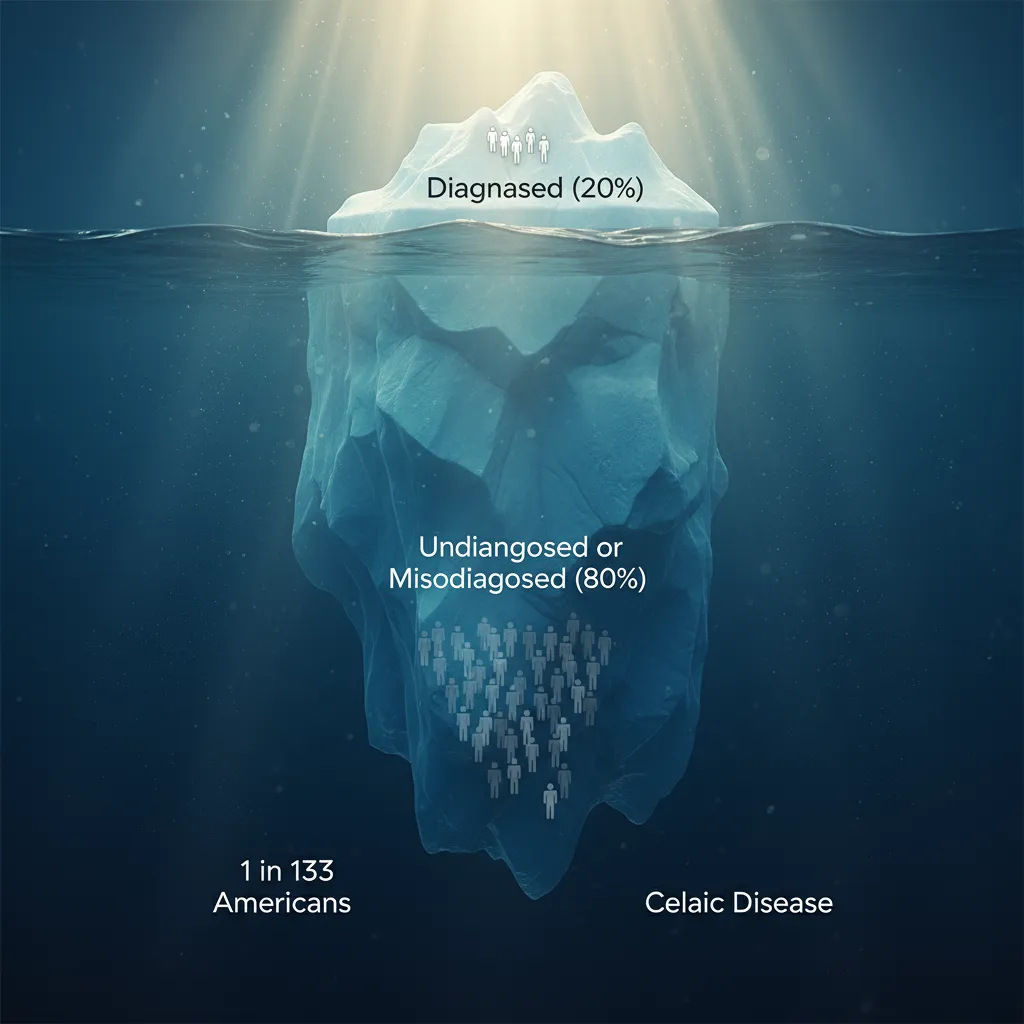
Effective celiac disease screening is the only way to close this gap. It allows for early intervention, which can prevent the long-term damage caused by the disease. An accurate diagnosis is the first and most critical step toward healing the intestine and improving overall health through the only available treatment: a strict, lifelong gluten-free diet.
Are You a Candidate? Key Symptoms and Risk Factors for Celiac Screening
Because the symptoms of celiac disease are so varied, knowing when to seek a celiac disease screening can be challenging. The signs can be gastrointestinal in nature, but often they appear in seemingly unrelated parts of the body. Understanding these symptoms and risk factors is key to knowing when to talk to your doctor about a celiac disease blood test.
Recognizing the Red Flags: Common Celiac Disease Symptoms in Adults
While classic symptoms involve the digestive system, many adults with celiac disease have few or no digestive complaints. It is crucial to be aware of the full spectrum of potential signs.
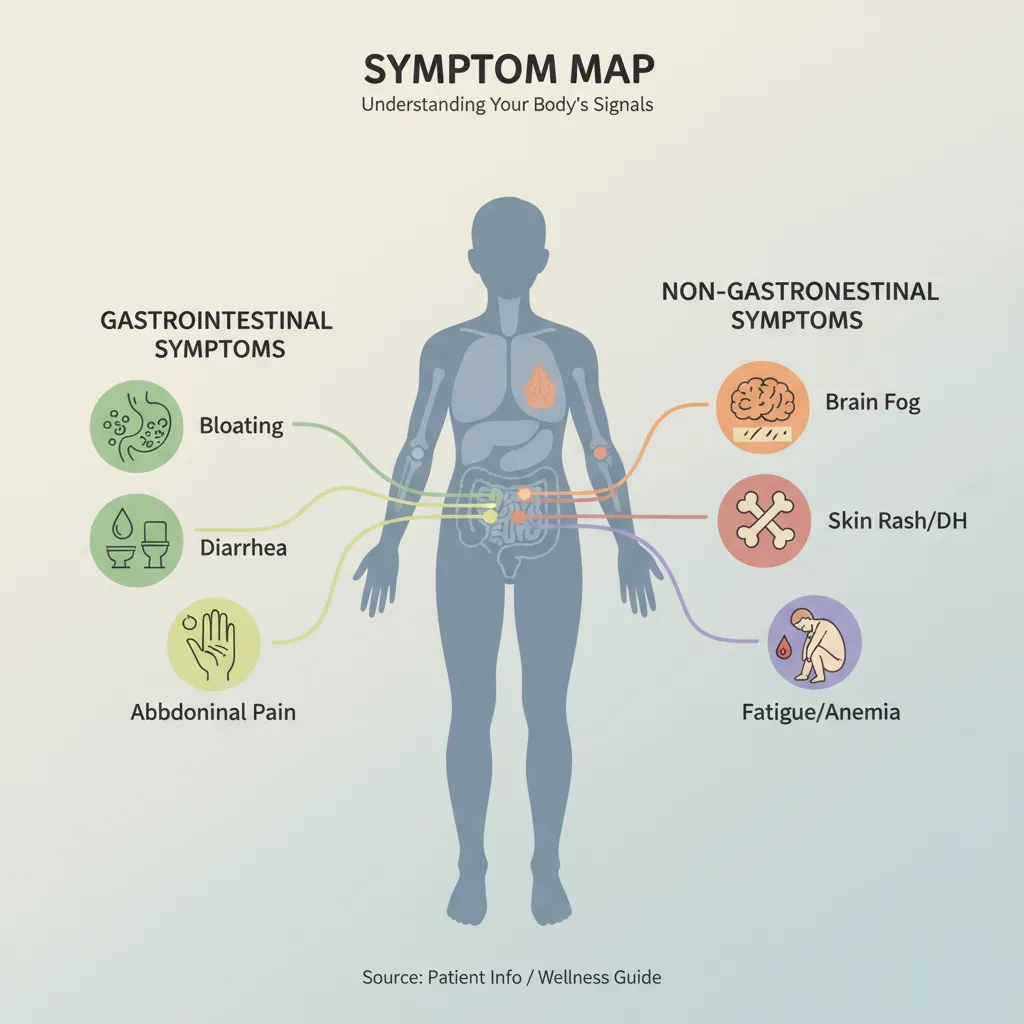
- Gastrointestinal Symptoms: These include chronic diarrhea, constipation, bloating, gas, abdominal pain, and nausea.
- Non-Gastrointestinal Symptoms: This is where diagnosis often gets tricky. These symptoms include persistent fatigue, unexplained iron-deficiency anemia, bone or joint pain, “brain fog” or difficulty concentrating, anxiety or depression, and severe or recurring mouth ulcers.
- Dermatitis Herpetiformis (DH): This is a chronic, intensely itchy skin rash with bumps and blisters. It is a direct manifestation of celiac disease and is sometimes referred to as the “celiac skin rash.”
Pediatric and Family History Screening Considerations
In children, the symptoms of celiac disease can present differently and may be mistaken for other childhood ailments. Key signs to watch for include poor growth or “failure to thrive,” delayed puberty, irritability or behavioral issues, and dental enamel defects.
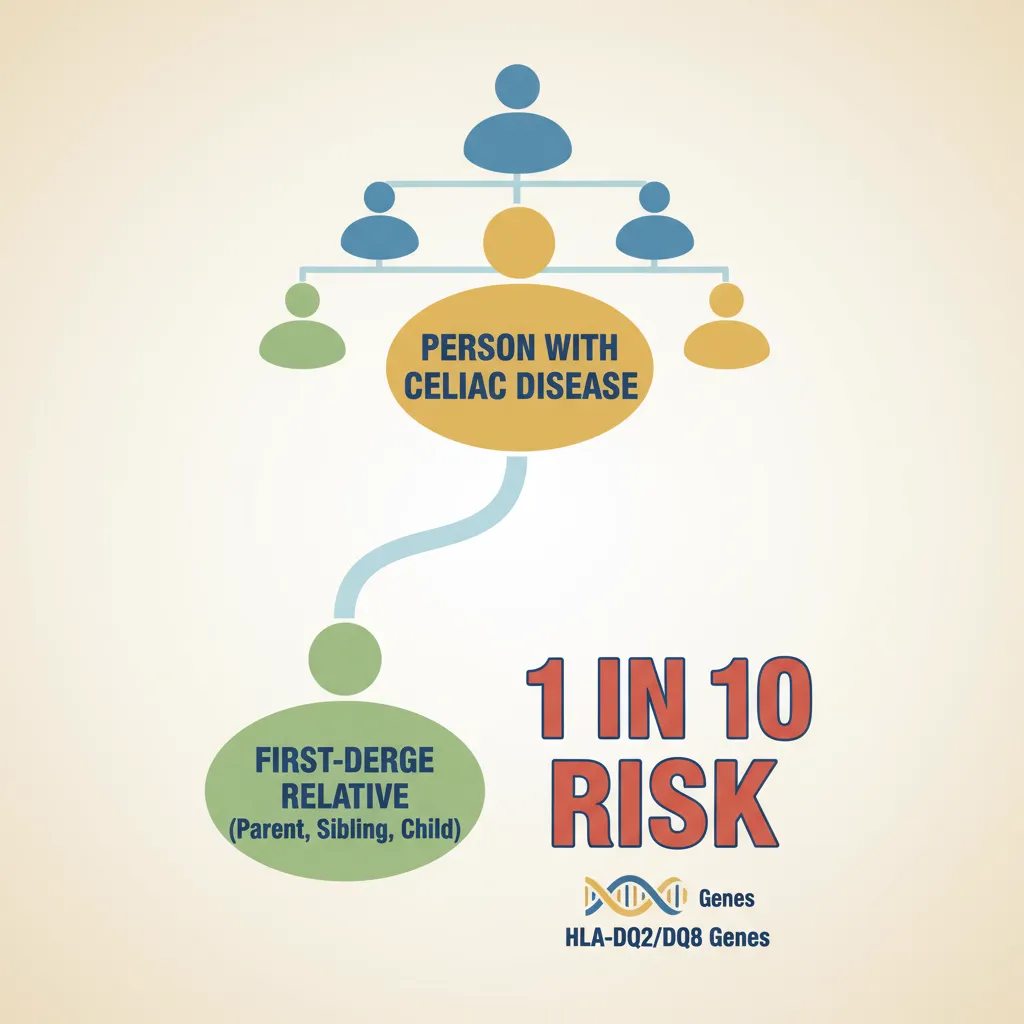
Family history is one of the strongest risk factors. First-degree relatives (a parent, child, or sibling) of someone with celiac disease have a 1 in 10 risk of developing the condition themselves. This makes proactive celiac disease screening a critical recommendation for these family members, even in the absence of obvious symptoms.
Associated Autoimmune Conditions
Celiac disease often co-occurs with other autoimmune disorders. Individuals with conditions like Type 1 diabetes, autoimmune thyroid disease (Hashimoto’s or Graves’ disease), Addison’s disease, or Sjögren’s syndrome have a significantly higher risk. Guidelines from the American College of Gastroenterology (ACG) recommend routine celiac disease screening for these patient populations.
The Core of Diagnosis: A Deep Dive into Celiac Disease Blood Tests
The journey to a celiac disease diagnosis almost always begins with a simple blood draw. This initial step involves a celiac panel blood test, also known as a celiac serology panel. These tests are designed to detect specific antibodies that the immune system produces in response to gluten.
The Celiac Serology Panel: What Are Doctors Looking For?
A serologic test for celiac disease is a highly effective screening tool. It measures the levels of certain antibodies in your bloodstream. Elevated levels of these antibodies are a strong indicator that your body is having an autoimmune reaction to gluten.
- Tissue Transglutaminase (tTG) Test (IgA): The Tissue Transglutaminase IgA or tTG-IgA test is the single most important and widely used celiac antibody test. It is highly sensitive and specific, making it the preferred initial screening test for adults and children over the age of two. Tissue transglutaminase is an enzyme in the intestine that is targeted by the immune system in people with celiac disease.
- Endomysial Antibody (EMA) Test (IgA): The Endomysial Antibody (EMA) test is another highly specific antibody test. While it is less commonly used as a first-line screening tool because it is more complex to perform, its near 100% specificity makes it an excellent confirmatory test for a positive tTG-IgA test result.
- Deamidated Gliadin Peptide (DGP) Test (IgA and IgG): The Deamidated Gliadin Peptide (DGP) test is particularly useful in two scenarios. First, it is often more reliable than the tTG-IgA test for screening children under two years old. Second, it is a key part of the celiac disease screening process for individuals with IgA deficiency, which we will discuss next.
The Critical Role of the Total IgA Test
A small percentage of the population, including a higher proportion of people with celiac disease, has a condition called selective Immunoglobulin A (IgA) deficiency. This means they do not produce enough IgA antibodies.
Because the most common celiac screening tests (tTG-IgA and EMA-IgA) measure IgA antibodies, someone with IgA deficiency and celiac testing could receive a false negative celiac test result. To prevent this, labs almost always run a Total Serum IgA test alongside the celiac panel blood test. If a deficiency is detected, the doctor will rely on IgG-based tests, such as the DGP-IgG and tTG-IgG tests, for an accurate screening.
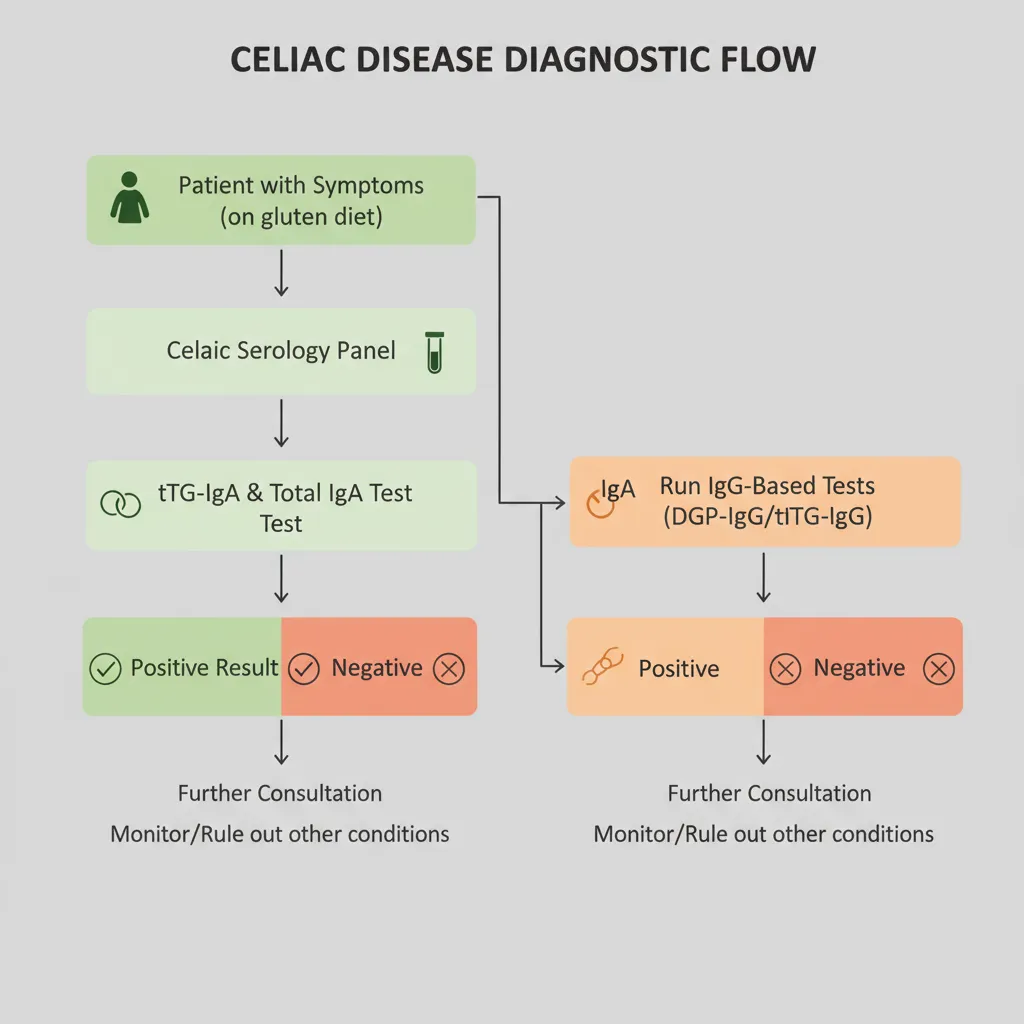
Interpreting Your Celiac Panel Blood Test Results
Receiving your celiac disease blood test results can be confusing. A positive result means that one or more of the antibodies were detected at a level above the normal range, indicating a high probability of celiac disease. A negative result means no antibodies were detected. It is important to remember that this celiac disease screening is just that, a screening. A definitive celiac disease diagnosis requires further steps.
Comparison of Key Serologic Tests for Celiac Disease
To clarify the roles of these different blood tests, here is a comparison of the primary serologic tests used in celiac disease screening.
| Test Name | Abbreviation | Primary Use | Key Advantage |
| Tissue Transglutaminase Antibody | tTG-IgA | The single preferred screening test for patients over 2. | High sensitivity and specificity; widely available. |
| Endomysial Antibody | EMA-IgA | Often used to confirm a positive tTG-IgA result. | Extremely high specificity (virtually 100%). |
| Deamidated Gliadin Peptide | DGP-IgG/IgA | Screening for children under 2; screening for IgA-deficient individuals. | More sensitive than tTG in very young children. |
| Total Serum Immunoglobulin A | Total IgA | Performed alongside other tests to check for IgA deficiency. | Prevents false negative celiac test results from tTG-IgA/EMA-IgA tests. |
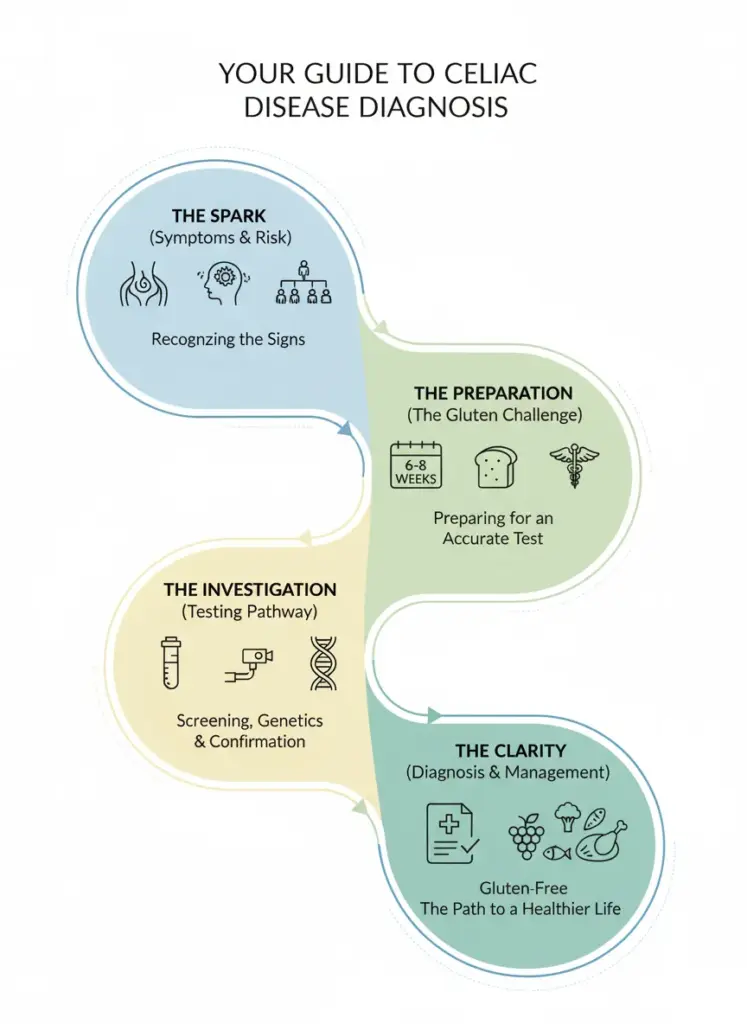
How to Prepare for a Celiac Blood Test: The Gluten Challenge Explained
This is arguably the most critical and often misunderstood part of the entire celiac disease screening process. The accuracy of your celiac disease blood test depends entirely on one factor: you must be actively eating gluten. This preparatory phase is known as the gluten challenge.
Why You MUST Eat Gluten for an Accurate Celiac Test
Let’s be perfectly clear: starting a gluten-free diet before you are tested for celiac disease is the single biggest reason for a false negative celiac test. The logic is simple. The celiac antibody test works by detecting the antibodies your immune system produces to fight what it perceives as the “threat” of gluten.
If you remove gluten from your diet, you remove the trigger. Your immune system calms down, stops producing those antibodies, and your intestinal lining can even begin to heal. While this is the goal of treatment after a diagnosis, it makes the disease invisible to the blood tests. To get an accurate result, you must continue a gluten-containing diet before testing.
The Gluten Challenge: How Long and How Much?
For those who have already started a gluten-free diet on their own, a medically supervised “gluten challenge” is necessary. This involves reintroducing a specific amount of gluten into your diet for a set period before your celiac disease blood test.
So, how long should I eat gluten before celiac blood test? According to guidelines from leading organizations like the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN), the recommendation for an accurate celiac disease screening is to consume gluten daily for 6 to 8 weeks. The amount should be equivalent to about two slices of wheat bread per day (approximately 10 grams of gluten). For a follow-up endoscopy, some gastroenterologists may advise a shorter challenge, but this should be determined by your doctor.

Practical Tips for a Medically Supervised Gluten Challenge
Embarking on a gluten challenge for celiac testing can be daunting, especially if gluten causes you significant discomfort. It is absolutely essential that this process is supervised by your healthcare provider.
- Communicate with Your Doctor: Before you start, discuss a plan with your doctor. They can advise you on how to manage symptoms and what to look out for.
- Incorporate Gluten-Containing Foods: The goal is to consume foods with wheat, barley, or rye. Good sources include pasta, bread, crackers, cereals, and baked goods.
- Track Your Symptoms: Keep a journal of your symptoms during the challenge. This information can be very helpful for your doctor during the celiac disease diagnosis process.
- Do Not Go It Alone: This is not something to be done without medical guidance. If symptoms become severe, contact your doctor immediately.
Understanding how to prepare for a celiac blood test is the key to avoiding the frustration and delay of a misdiagnosis. Following the principles of the gluten challenge ensures that your body will provide the clearest possible answer during the celiac disease screening.
Beyond Blood Work: Genetic Testing and Endoscopy
While the celiac disease blood test is the cornerstone of screening, it is not the final word. A complete celiac disease diagnosis often involves two other important procedures: genetic testing and an endoscopy with a biopsy.
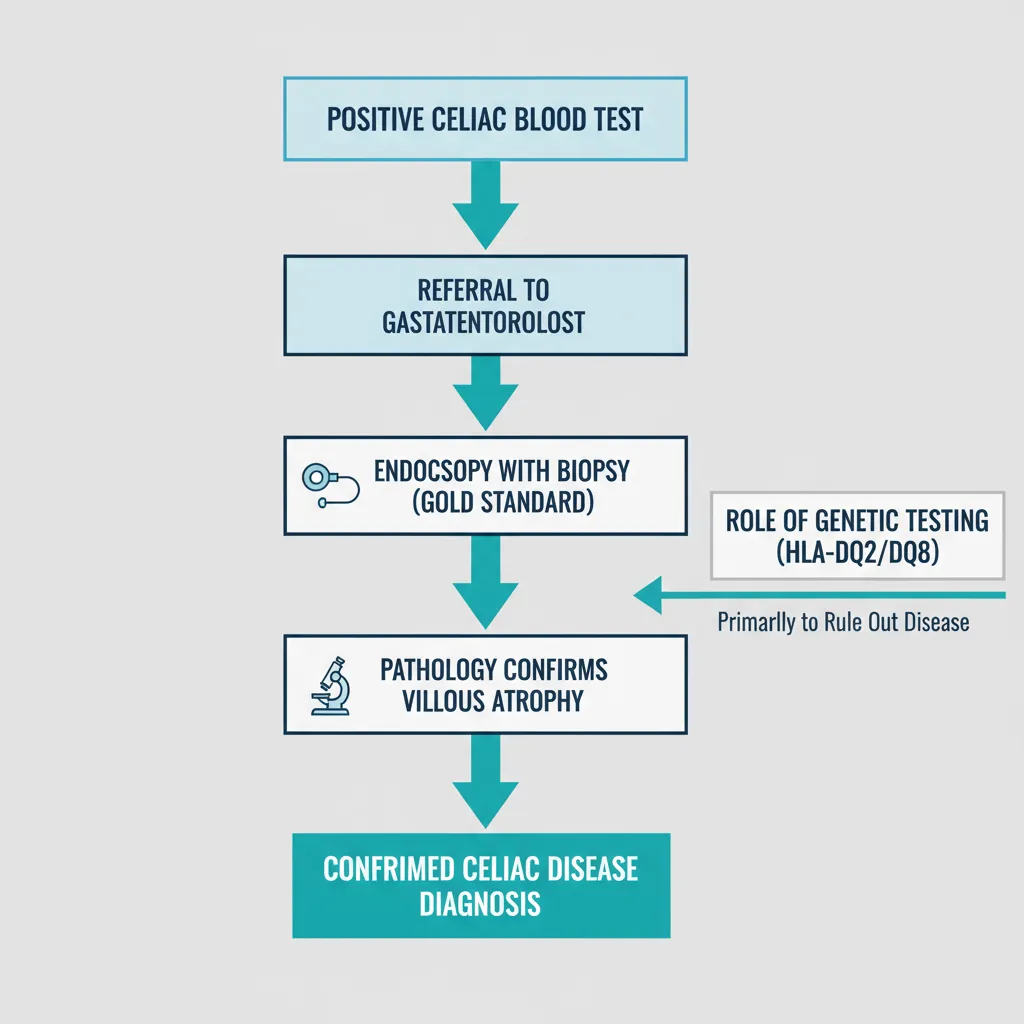
Genetic Testing for Celiac Disease: HLA-DQ2 and HLA-DQ8
Genetic testing for celiac disease looks for two specific human leukocyte antigen (HLA) genes: HLA-DQ2 and HLA-DQ8. Nearly all people with celiac disease have one or both of these genes.
However, this test is not used to diagnose celiac disease. Why? Because about 30% of the general population carries these genes, but only a small fraction of them will ever develop the condition. The true power of genetic testing for celiac disease lies in its ability to rule out the condition. If you test negative for both HLA-DQ2 and HLA-DQ8, your chances of ever developing celiac disease are extremely low (a greater than 99% negative predictive value). This can be invaluable for at-risk family members or in cases where blood test results are ambiguous.
The Gold Standard: Endoscopy for Celiac Disease Confirmation
If your celiac panel blood test comes back positive, your doctor will likely refer you to a gastroenterologist for an upper endoscopy with a biopsy. This procedure is considered the “gold standard” for confirming a celiac disease diagnosis.
During an endoscopy for celiac disease, a thin, flexible tube with a camera is passed through the mouth and into the small intestine. The doctor can visually inspect the lining for damage and will take several tiny tissue samples (a biopsy). These samples are then examined under a microscope by a pathologist to look for the characteristic flattening of the villi, known as villous atrophy, which is the hallmark of celiac disease. Just like with the blood test, you must be on a gluten-containing diet before testing for the biopsy to show accurate results.
Genetic vs. Serologic Testing for Celiac Disease
It is important to understand how these different tests fit together in the diagnostic puzzle. Each serves a distinct and complementary purpose in the celiac disease screening and diagnosis process.
| Feature | Serologic (Blood) Testing | Genetic (HLA) Testing |
| Purpose | Detects active disease by measuring gluten-response antibodies. | Determines genetic predisposition; primarily used to rule out celiac disease. |
| Requires Gluten? | Yes, gluten consumption is mandatory for accuracy. | No, genes are permanent and unaffected by diet. |
| Can it Diagnose? | No, it’s a screening tool that indicates high probability. | No, it only indicates risk (approx. 30% of people have the genes). |
| Best Use Case | Initial screening for symptomatic individuals. | Ruling out celiac in at-risk family members or ambiguous cases. |
Navigating the Future: Latest Diagnostic Innovations (2025 and Beyond)
The field of celiac disease diagnosis is constantly advancing. In 2025, several exciting innovations are improving the speed, accuracy, and accessibility of celiac disease screening. The diagnostics market growth in the USA continues to be strong, with an approximate 8.1% compound annual growth rate driven by these advancements and increased awareness.
FDA clearance of fully automated testing platforms has significantly enhanced the efficiency and reliability of the celiac panel blood test. Furthermore, emerging AI-based risk scoring tools are being developed to analyze patient data and even pathology slides, helping clinicians make faster and more precise decisions. While still in development for wider use, point-of-care and multiplex assays promise to bring rapid celiac disease screening even closer to the patient in the coming years.

Summary & Key Takeaways: Your Path to an Accurate Diagnosis
Navigating the path to a potential celiac disease diagnosis can feel overwhelming, but it begins with a few clear, actionable steps. An accurate celiac disease screening is the foundation of this journey, and its success hinges on proper preparation.
The most critical takeaway is this: do not remove gluten from your diet before you have completed your celiac disease blood test. A medically supervised gluten challenge for celiac testing is essential for an accurate result and prevents the common pitfall of a false negative celiac test. By understanding the different types of tests available and working closely with your healthcare provider, you can confidently move toward a definitive answer and take control of your health.
Frequently Asked Questions (FAQs)
What is the first test for celiac disease?
The first test is typically a celiac disease blood test, specifically a serology panel that includes the Tissue Transglutaminase IgA (tTG-IgA) test. This is the primary celiac disease screening tool.
Can I drink water before a celiac blood test?
Yes, you can and should stay hydrated by drinking water. Fasting is generally not required for a celiac panel blood test, but it is always best to confirm with your doctor or the laboratory providing the test.
What happens if I test positive on a celiac blood test?
A positive result from a celiac antibody test indicates a high likelihood of celiac disease. The next step is usually a referral to a gastroenterologist, who will likely recommend an upper endoscopy for celiac disease confirmation via biopsy.
How quickly do celiac antibodies disappear on a gluten-free diet?
After starting a strict gluten-free diet, antibody levels can decline significantly within a few weeks to several months. This is why following a gluten-containing diet before testing is so crucial for an accurate initial celiac disease screening.
Can stress cause a false positive celiac test?
No, emotional or physical stress does not cause a false positive on a serologic test for celiac disease. These tests are very specific to the autoimmune antibodies produced in response to gluten.
Is there a cure for celiac disease?
Currently, there is no cure for celiac disease. The only effective and lifelong treatment is strict adherence to a 100% gluten-free diet, which allows the small intestine to heal and prevents further damage.
What is the difference between a gluten intolerance test and a celiac disease test?
A celiac disease test is a validated medical diagnostic tool, like the tTG-IgA test, that looks for specific autoimmune markers. In contrast, most commercial “gluten intolerance” or “food sensitivity” tests are not scientifically validated for diagnosing celiac disease and are not recommended by medical experts for this purpose.
Can I develop celiac disease as an adult?
Absolutely. Celiac disease can be diagnosed at any age, from infancy to late adulthood. It is possible for a person to eat gluten for decades without issue before the disease is “triggered” and becomes active.
Why is genetic testing for celiac disease useful if it can’t diagnose it?
The main value of genetic testing for celiac disease is its ability to rule out the condition. A negative result for the HLA-DQ2 and HLA-DQ8 genes makes a future celiac disease diagnosis extremely unlikely, providing peace of mind for at-risk family members.
What should my next steps be if I suspect I have celiac disease?
The most important first step is to schedule an appointment with your doctor to discuss your symptoms. Do not start a gluten-free diet on your own. Your doctor can order the correct celiac disease screening tests to begin the formal diagnostic process.
Which blood test is most reliable for celiac disease?
The Tissue Transglutaminase IgA (tTG-IgA) test is considered the most reliable single screening blood test for celiac disease due to its high sensitivity and specificity in people who are consuming gluten.
Does gluten-free diet affect celiac blood test results?
Yes, profoundly. A gluten-free diet will almost certainly cause a celiac disease blood test to be falsely negative. This is because the test measures the immune response to gluten; without gluten, there is no response to measure.