You have successfully completed a 24-hour, 48-hour, or even a longer fast. You feel mentally sharp. Your insulin levels have dropped. You are ready to refeed and nourish your body. You sit down for that first meal with excitement. But within twenty minutes, urgency strikes. Instead of digesting your nutrients, you are sprinting to the restroom with severe cramping. Diarrhea after fasting is a frustrating end to a disciplined health practice.
Table of Contents
This is a scenario I encounter constantly in my practice as a Registered Dietitian Nutritionist. Clients feel like they have failed or that their bodies are “rejecting” food. Here is the reality. This is not a personal failure. It does not mean fasting isn’t for you. This is a biological feedback loop.
It is a common gastrointestinal response. It is characterized by loose, watery stools caused by the rapid reactivation of the digestive tract. It is frequently triggered by bile acid malabsorption, osmotic shifts from carbohydrates, or an overactive gastrocolic reflex. Understanding these mechanisms is the key to preventing them.
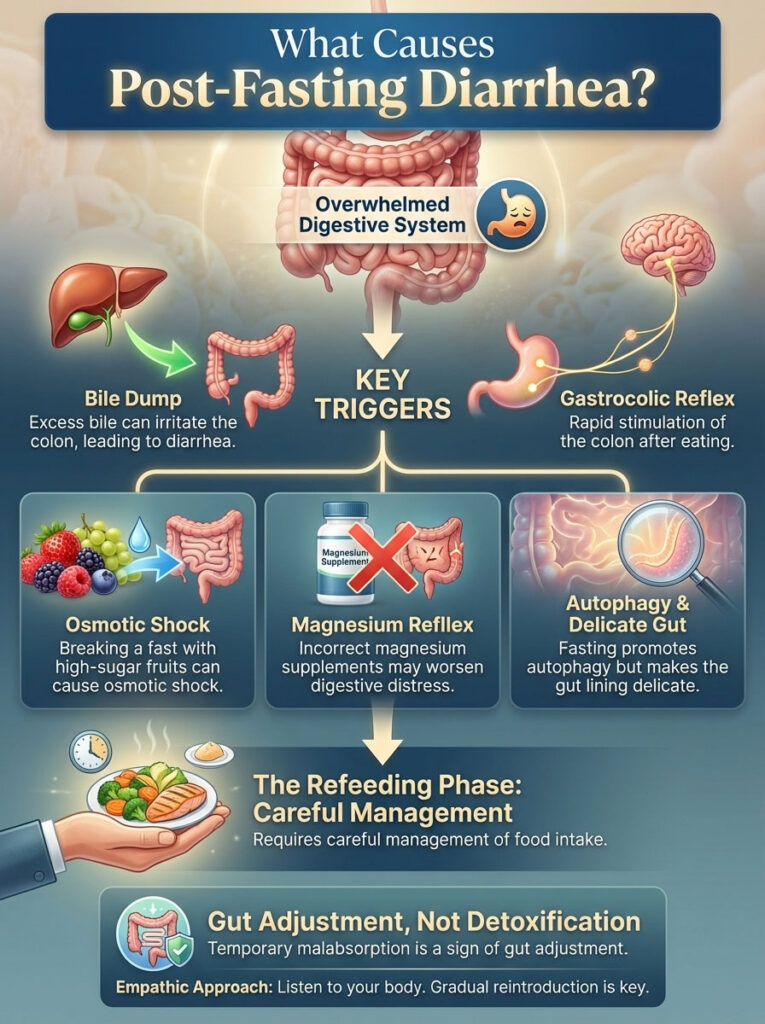
What Causes Post-Fasting Diarrhea?
Diarrhea after fasting occurs when a dormant digestive system is overwhelmed by food volume or type. The primary culprits are the “Bile Dump” (excess stored bile irritating the colon) and the “Gastrocolic Reflex” (stomach stretching signaling immediate evacuation). Other causes include osmotic shock from breaking a fast with high-sugar fruits or taking incorrect magnesium supplements. It is a sign of temporary malabsorption, not detoxification.
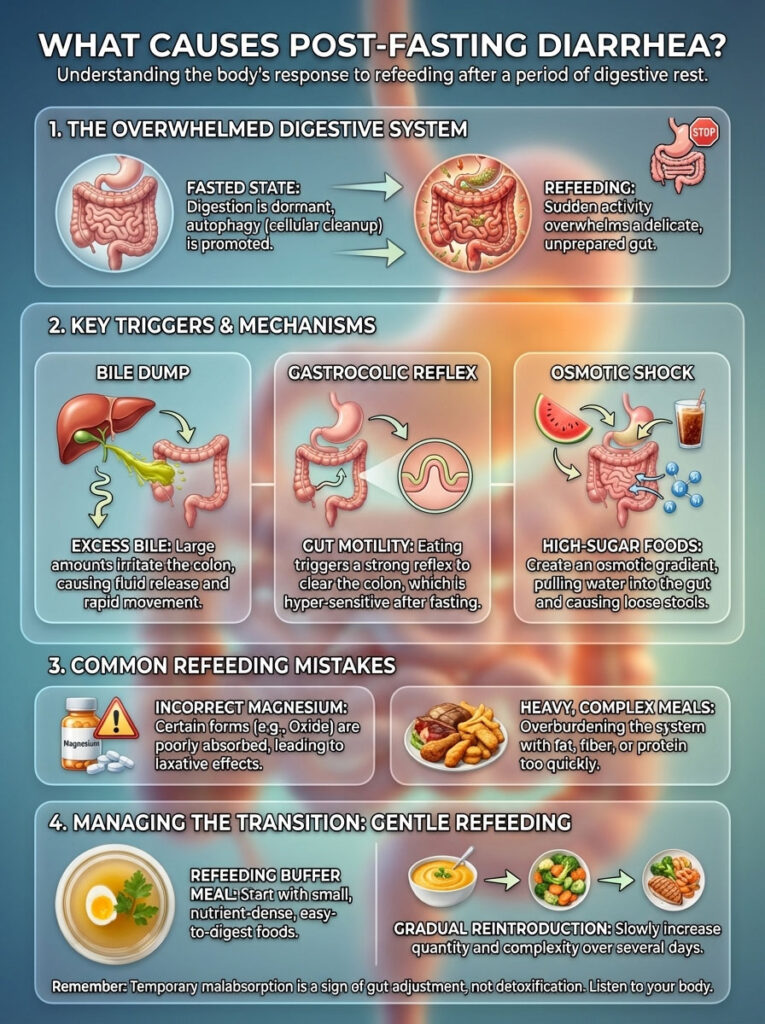
While fasting induces autophagy and improves metabolic flexibility, the “refeeding phase” is biologically delicate. Your gut lining thins during a fast. Enzyme production slows down. Throwing a heavy meal at a sleeping digestive system is like waking someone up with a bucket of ice water. Chaos ensues. The result is often urgent, liquid stool.
This comprehensive guide provides a deep examination of the pathophysiology of the gut during fasting. We will cover a clinically proven refeeding protocol to prevent this issue. We will also discuss emergency steps for immediate relief if you are already suffering.
Key Statistics on Fasting & Digestion
- 90-120 Minutes: The time it takes for the Migrating Motor Complex (MMC) to complete one cleaning cycle in a fasted state.
- 40-50%: The estimated reduction in digestive enzyme secretion after 24 hours of fasting.
- 30 Minutes: The critical window after refeeding where the gastrocolic reflex is most active.
- 1 in 3: Approximate number of intermittent fasters who report gastrointestinal distress when breaking a fast incorrectly.
- 95%: Percentage of bile acids that should be reabsorbed in the ileum; failure here causes diarrhea.
- 2000mg: The sodium intake threshold that can help stabilize fluid retention during refeeding.
The Physiology of Fasting: What Happens to Your Gut?
To prevent the issue, we must first understand the environment inside your stomach and intestines during a fast. When you stop eating, your body shifts resources away from digestion toward repair and maintenance. This shift is beneficial for cellular health. However, it creates a temporary vulnerability upon refeeding.
The Dormant Digestive System
During the fasting window, your digestive organs rest. This applies whether it is an intermittent 16 hours or a prolonged 48+ hours. The pancreas downregulates the production of key digestive enzymes. Specifically, it reduces amylase for carbs, protease for proteins, and lipase for fats.
Additionally, the mucosal lining of the gut can thin slightly due to lack of stimulation. This lining protects the intestinal wall. If you introduce complex foods immediately, your body lacks the chemical tools to break them down. Undigested food particles sitting in the intestine draw water in. They ferment rapidly. This leads to gas and liquid stool.
Think of your digestion like a factory line. When you fast, the workers go home and the lights turn off. Refeeding is the signal to restart production. If you dump a truckload of raw materials onto the conveyor belt before the workers have returned, the system jams. The emergency exit opens. That emergency exit is diarrhea.
The Migrating Motor Complex (MMC)
The MMC is essentially the “housekeeper” of the gut. It is an electromechanical wave of activity. It sweeps through the intestines between meals to clear out bacteria, debris, and undigested food. It creates that rumbling sound you hear when you are hungry.
Here is the conflict. Fasting ramps up MMC activity. Your gut is in deep cleaning mode. When you break a fast abruptly, you interrupt this powerful mechanical wave. This interruption can sometimes result in chaotic peristalsis. These are muscle contractions that are too fast and uncoordinated. They cause cramping and immediate urgency.
Microbiome Shifts and Mucosal Integrity
Your gut microbiome adapts rapidly to food scarcity. During a fast, bacteria that thrive on fiber and sugar go dormant or die off. Others flourish. This leads to a temporary reduction in Short-Chain Fatty Acids (SCFAs) like butyrate.
Butyrate is critical. It helps the cells of the colon absorb water. With lower SCFA levels, your colon is less efficient at drying out stool. This makes diarrhea after fasting more likely. Furthermore, the mucus layer that coats the intestinal tract can degrade slightly without the stimulation of fiber. This leaves the epithelial cells more exposed to irritants like bile acids or spicy foods.
The Vagus Nerve Connection
The gut and the brain are connected by the vagus nerve. Fasting increases cortisol and adrenaline initially as the body adapts to stress. These stress hormones can alter gut motility. When you eat, the vagus nerve signals the transition from “fight or flight” to “rest and digest.”
However, this switch isn’t instant. If you eat while your body is still in a sympathetic (stress) dominant state, digestion is impaired. The food moves through the system too quickly. This rapid transit time prevents proper water absorption in the colon.
The 4 Clinical Causes of Post-Fasting Diarrhea
Based on clinical observation and gastrointestinal physiology, post-fasting urgency usually stems from specific mechanisms. It is rarely random. It is usually one (or a combination) of these four biological drivers.
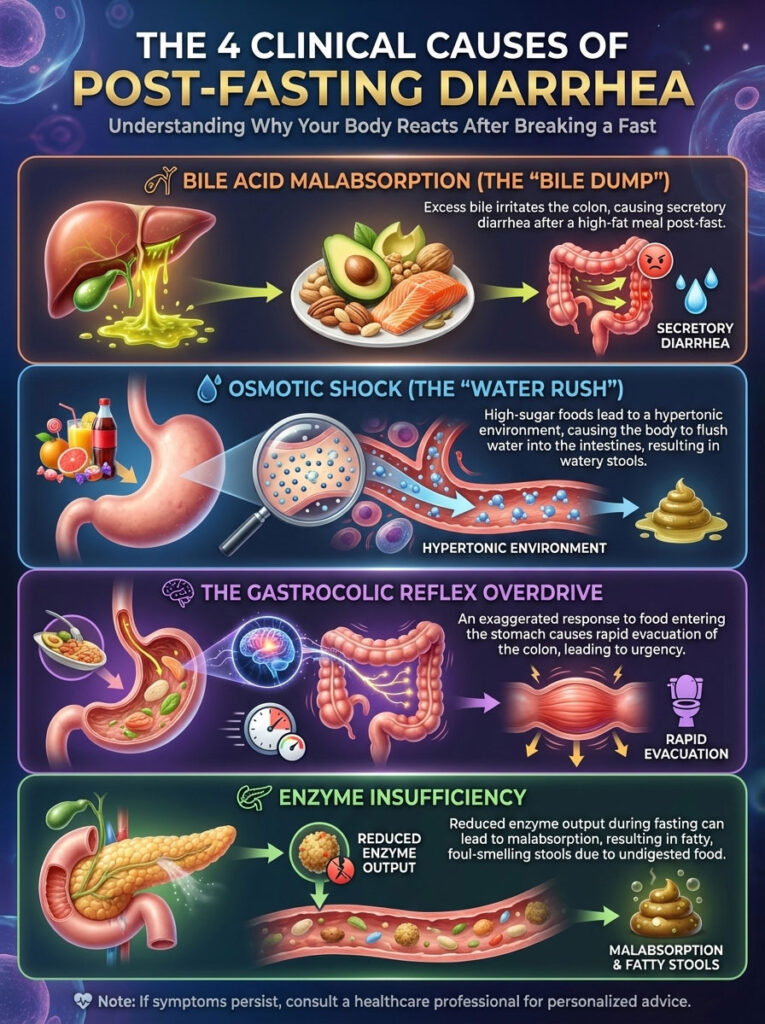
1. Bile Acid Malabsorption (The “Bile Dump”)
This is arguably the most common cause of refeeding diarrhea in high-fat or Keto dieters. The gallbladder stores and concentrates bile produced by the liver. Its job is to release this bile when fat enters the small intestine to emulsify it.
During a fast, no fat is coming in. The gallbladder fills up. It becomes distended with highly concentrated bile. When you finally eat, the hormone Cholecystokinin (CCK) signals a release. If that meal contains significant fat, the release is massive. This is the “Bile Dump.”
Under normal conditions, your small intestine reabsorbs 95% of this bile. But after a fast, the transporters in the terminal ileum may be sluggish. They cannot reabsorb this sudden flood of bile salts. The salts spill over into the colon.
Bile salts are extremely irritating to the colon lining. They draw water into the bowel through osmosis. This results in secretory diarrhea. It is often yellow in color and burning in sensation. Research indicates that bile acid diarrhea is frequently misdiagnosed but is a primary driver of urgency after periods of dietary restriction.
2. Osmotic Shock (The “Water Rush”)
Osmolarity refers to the concentration of particles in a solution. The contents of your gut should be isotonic with your blood. This means they should have a similar concentration. Breaking a fast with high-sugar fruits or simple carbs creates a hypertonic environment.
Imagine eating a large bowl of watermelon or grapes. These are high in fructose. If the gut cannot transport that fructose into the blood fast enough, it sits in the lumen. Nature hates imbalance. To dilute the sugar, the body flushes water from the bloodstream into the intestines.
This massive influx of fluid leads to immediate, watery bowel movements. This is why the common advice to have a “fruit feast” often leads to disaster. The sugar load is simply too high for the dormant transporters to handle.
3. The Gastrocolic Reflex Overdrive
The gastrocolic reflex is a normal physiological reaction. When food enters the stomach, a signal is sent to the colon to evacuate to make room. After a fast, this reflex is hypersensitive. The stomach has been empty for a long time.
Suddenly, it stretches. The vagus nerve fires a strong signal to the colon. Because the gut has been dormant, the response can be exaggerated. This leads to propulsive contractions. These contractions force contents through the system before water can be absorbed. The result is urgency within 15 to 30 minutes of the first bite.
4. Enzyme Insufficiency
This follows the “use it or lose it” principle. As mentioned, the pancreas temporarily reduces enzyme output during fasting. If you eat a steak or cheese before enzymes are upregulated, the food passes through undigested.
Proteins require protease. Fats require lipase. Without lipase, fat is not broken down. This results in steatorrhea. These are fatty, floating, foul-smelling stools. They are often loose and pale. This is a clear sign of malabsorption. The food is exiting your body before you have harvested the nutrients.
Common Triggers and Mistakes to Avoid
Many health-conscious individuals inadvertently trigger gastrointestinal distress. They follow popular but misguided advice. Here are the specific behaviors that lead to the bathroom sprint.

The “Magnesium Mistake”
Electrolytes are vital during a fast. However, the formulation matters immensely. Many fasters take Magnesium Citrate or Magnesium Oxide to prevent headaches or muscle cramps. These forms of magnesium are osmotic laxatives.
Doctors prescribe Magnesium Citrate to clear the bowels before a colonoscopy. Taking this on an empty stomach right before food draws water into the intestines. When combined with the natural refeeding response, it guarantees a run to the bathroom. Stick to Magnesium Glycinate or Malate instead.
High-Fat “Keto” Breaking
A common error in the Keto community is breaking a fast with “Fat Bombs.” People drink butter coffee or pure MCT Oil. They do this to keep insulin low. However, pure liquid fat is the single hardest macronutrient for a dormant gut to process.
Without a food matrix like fiber or protein to slow it down, liquid fat triggers the most aggressive CCK spike. This leads to the massive bile dump we discussed earlier. MCT oil is particularly risky because it bypasses normal digestion and hits the system rapidly.
The Volume Problem (OMAD Pitfalls)
For the One Meal A Day (OMAD) community, the pressure is high. You must consume 1,500 to 2,000 calories in a one-hour window. Consuming this volume in 30 minutes overwhelms gastric emptying rates.
The stomach cannot churn and acidify the food fast enough. It dumps semi-solid food into the small intestine. This triggers the emergency evacuation reflex. The body senses it cannot process this volume, so it ejects it.
Artificial Sweeteners and Gums
Many people break their fast with a “health” bar or a protein shake. These often contain sugar alcohols like Erythritol, Xylitol, or Maltitol. They may also contain gums like Xanthan or Guar gum.
These ingredients are fermentable. In a fasted gut with an altered microbiome, they ferment explosively. This draws gas and fluid into the bowel. The result is bloating followed by loose stool. Always read the label before that first bite.
Caffeine Sensitivity
Coffee is a staple for many fasters. However, caffeine is a stimulant that increases gut motility. It makes your colon contract. Drinking a strong cup of coffee right before or with your first meal adds fuel to the fire.
The caffeine stimulates peristalsis. The food stimulates the gastrocolic reflex. The combination creates a “perfect storm” for diarrhea. It is wise to separate your last coffee and your first meal by at least two hours.
Comparison: Fasting Duration vs. Digestive Risk
Not all fasts carry the same risk. A 16-hour fast rarely requires a specific protocol. A 3-day fast requires a strategic approach. See the table below to assess your risk level and necessary precautions.
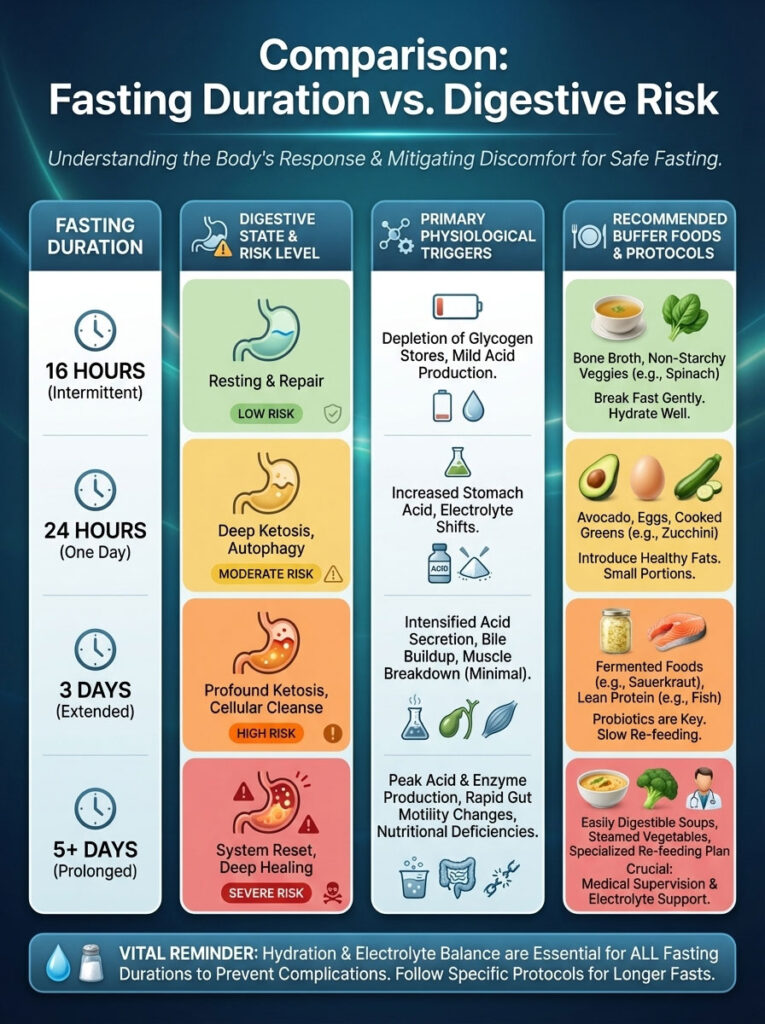
| Fasting Duration | Digestive State | Risk Level | Primary Physiological Trigger | Recommended “Buffer” Food |
|---|---|---|---|---|
| Intermittent (16-20 hrs) | Active/Resting | Low | Electrolyte imbalance (Magnesium) or Caffeine | Small handful of nuts or bone broth |
| OMAD (23-24 hrs) | Mildly Dormant | Moderate | Gastrocolic Reflex (Volume overload) | Lean protein (Egg/Fish) 30 mins before main meal |
| Extended (48-72 hrs) | Dormant | High | Bile Acid Malabsorption (Bile Dump) | Bone broth + Collagen (Liquid only first) |
| Prolonged (5+ Days) | Atrophied | Severe | Refeeding Syndrome & Osmotic Shock | Diluted broth only (Medical supervision advised) |
The RDN-Approved Refeeding Protocol
To stop diarrhea after fasting, you must treat the first intake of calories not as a meal, but as a primer. We call this the “Buffer Method.” The goal is to wake up the gut gently without overwhelming it.
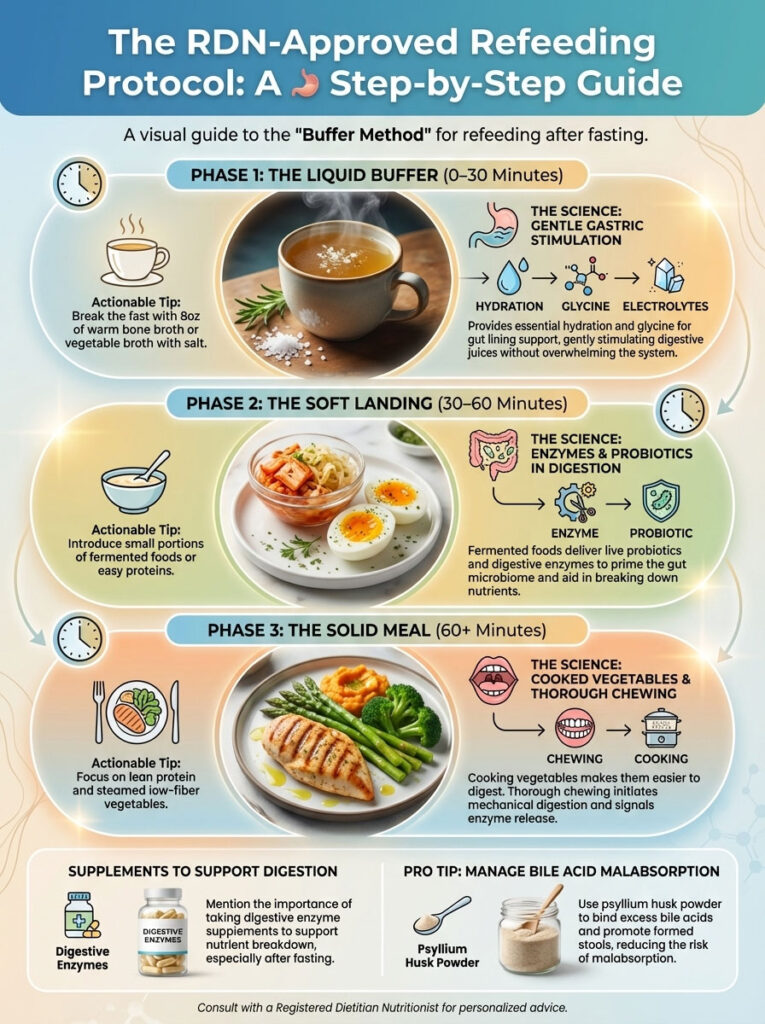
Phase 1: The Liquid Buffer (0–30 Minutes)
Actionable Tip: Break the fast with 8oz of warm bone broth or vegetable broth. Add a pinch of high-quality salt.
The Science: Bone broth is rich in glycine. Glycine is an amino acid that supports the integrity of the gut lining. The broth provides electrolytes like sodium to hydrate cells without requiring heavy digestion. The warmth soothes the stomach. It gently wakes up the gastric juices without triggering a massive bile release. It tells the pancreas, “Get ready, food is coming soon.”
Phase 2: The Soft Landing (30–60 Minutes)
Actionable Tip: Introduce a small portion of fermented food. A shot of sauerkraut juice or a tablespoon of kimchi is excellent. Alternatively, eat a very easy protein, such as a soft-boiled egg.
The Science: Fermented foods provide enzymes and probiotics. They pre-digest the food for you. Eggs contain choline and are highly bioavailable. This phase stimulates the pancreas to begin producing enzymes (amylase, protease, lipase) gently. We are “revving the engine” before driving the car. We are ensuring the bile duct opens slowly, not explosively.
Phase 3: The Solid Meal (60+ Minutes)
Actionable Tip: Eat your main meal. Focus on lean protein like chicken breast or white fish. Pair it with steamed low-fiber vegetables like zucchini or spinach.
The Science: Cooked vegetables are easier to break down than raw ones. The cellulose structure is softened by heat. Lean protein provides amino acids for repair without the heavy fat load that triggers bile dumping. Chew your food thoroughly. Digestion begins in the mouth. The more you chew, the less work your stomach has to do.
Supplements to Support Digestion
Pro Tip: The Psyllium Sponge
If you consistently suffer from bile acid malabsorption, take 1 teaspoon of psyllium husk powder mixed in water 15 minutes before your first meal. Psyllium is a soluble fiber. It acts as a “sponge” that binds to excess bile salts. This prevents them from irritating the colon. It adds bulk to the stool, preventing the liquid rush. Start with a small amount to avoid bloating.
Additionally, a broad-spectrum digestive enzyme can be helpful. Look for one containing ox bile and lipase. Take it with your first meal to assist the pancreas. This acts as “outsourced” digestion while your body gets back up to speed.
Foods to Eat vs. Foods to Avoid
Choosing the right ingredients is the difference between a satisfied stomach and stomach pain after breaking a fast. Some “healthy” foods are terrible for refeeding. Refer to the detailed table below for the “Green Light” and “Red Light” foods.
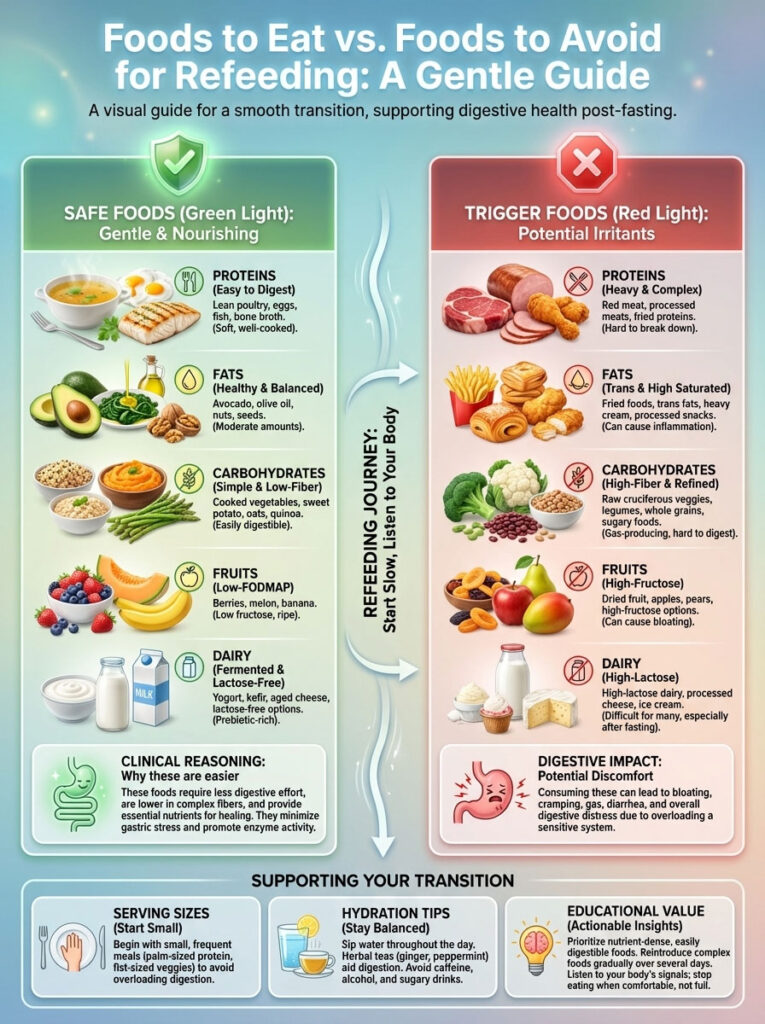
| Food Category | ✅ Safe Foods (The “Green Light”) | ❌ Trigger Foods (The “Red Light”) | The Clinical Reason |
|---|---|---|---|
| Proteins | White fish, eggs, collagen peptides, chicken breast, turkey | Red meat, fried chicken, protein shakes with whey concentrate, pork | High fat and lactose content are difficult to digest without upregulated enzymes. Red meat is dense and slow to digest. |
| Fats | Avocado (small amount), olive oil drizzle, coconut oil (small amount) | MCT oil, heavy cream, handfuls of nuts, butter sticks, cheese | Pure fats trigger massive bile release (CCK spike). Nuts contain inhibitors that are hard on a fasted gut. |
| Carbohydrates | Steamed zucchini, pumpkin, cooked carrots, sweet potato (boiled) | Raw kale, beans, lentils, popcorn, raw broccoli, cauliflower | Insoluble fiber acts like sandpaper on a sensitive gut lining. Legumes cause massive gas production. |
| Fruits | Berries (small quantity), papaya, pineapple (contains enzymes) | Watermelon, grapes, dried fruit (dates/raisins), mango | High fructose load causes osmotic fluid shifts (“water rush”). Dried fruit is too sugar-dense. |
| Dairy | Ghee (clarified butter), yogurt (fermented) | Milk, soft cheese, ice cream, cream | Lactase enzyme is the first to downregulate. Milk sugar (lactose) will cause instant diarrhea. |
Immediate Relief: How to Stop the Diarrhea
If you are reading this while already experiencing diarrhea after fasting, you need damage control. The goal is to stabilize electrolytes and soothe the inflammation. Do not panic. This is usually self-limiting.

Hydration Strategy: The Sodium Priority
Do not just drink plain water. When you have diarrhea, you lose water and salts. Drinking plain water can dilute your remaining electrolytes further. This leads to dizziness and fatigue. You need an electrolyte solution.
Follow the World Health Organization (WHO) principle for rehydration. You need water, sodium, potassium, and a small amount of glucose. The glucose helps transport the sodium across the gut barrier. A diluted sports drink is better than plain water in this acute moment. Alternatively, use a high-quality electrolyte powder like LMNT or Liquid I.V., but sip it slowly.
Should You Use Anti-Diarrheals?
My expert opinion is to avoid Loperamide (Imodium) initially. Here is why. Breaking a fast often triggers a purge of bile or bacteria. Your body is trying to expel an irritant. It is a cleaning mechanism.
Locking that irritant inside your colon by paralyzing the muscles can lead to severe cramping and toxicity. That is how Loperamide works. It stops the movement. Let your body flush the irritant out. Use anti-diarrheals only if the symptoms persist for more than 6 hours or if you are at risk of severe dehydration.
The “MEAT” vs. “BRAT” Protocol
You may have heard of the BRAT diet (Bananas, Rice, Applesauce, Toast) for diarrhea. While effective for stomach bugs, it is suboptimal for metabolic fasters or those on Keto. The massive insulin spike from these carbs can make you feel groggy and bloated.
Instead, use the “MEAT” protocol. This stands for Meat, Eggs, Avocado (in moderation), and Tea. Lean poultry and eggs provide the protein needed for gut repair without the sugar crash. Bone broth is superior to applesauce for electrolyte replenishment. Peppermint or ginger tea can soothe the smooth muscle of the intestines.
Natural Binders
If the urgency is severe, consider natural binders. Activated charcoal or bentonite clay can help bind toxins and excess gas. However, be careful. They also bind nutrients and medications. Take them away from other supplements. They can help firm up the stool without paralyzing the gut like pharmaceutical drugs do.
When to Worry: Red Flags and Refeeding Syndrome
While liquid stool is uncomfortable, it is rarely dangerous unless it persists. However, there is a serious medical condition called Refeeding Syndrome. This can occur after prolonged fasting, usually 5 days or more.

Distinguishing Discomfort from Danger
Refeeding Syndrome is potentially fatal. It involves dangerous shifts in fluids and electrolytes. The hallmark signs are not just diarrhea. They include edema (swelling in ankles), rapid heart rate (tachycardia), extreme fatigue, and confusion.
This happens because insulin causes cells to pull phosphate, potassium, and magnesium out of the blood rapidly. If you have been fasting for less than 72 hours, Refeeding Syndrome is highly unlikely. However, you should still be aware of the electrolyte crash.
When to Seek Medical Attention
You should seek medical help if you experience specific severe symptoms. Watch for bloody or black, tarry stool. This indicates bleeding in the digestive tract. Severe abdominal pain that radiates to the back can be a sign of pancreatitis.
Dizziness or fainting that does not resolve with electrolyte intake is a red flag. Finally, if diarrhea lasts longer than 24 hours, you risk severe dehydration and should see a doctor. Listen to your body. Fasting should heal you, not hurt you.
Long-Term Gut Health and Adaptation
If you experience diarrhea every time you fast, your gut may need training. The gut is adaptable. It is like a muscle. You can train it to handle fasting better over time.

Gradual Progression
Do not jump from eating six times a day to a 48-hour fast. Start with 12 hours. Then move to 14, then 16. Allow your gallbladder and pancreas to adapt to the new rhythm. This trains the bile concentration and release mechanisms.
Gut Healing Protocols
Between fasts, focus on gut integrity. Consume collagen, bone broth, and L-Glutamine regularly. These nutrients strengthen the tight junctions of the gut lining. A stronger lining is less susceptible to irritation from bile acids.
Also, diversify your fiber intake during your eating window. A diverse microbiome is a resilient microbiome. The more robust your bacterial colonies, the better they can handle the stress of a fast. They will produce more butyrate, protecting you from future episodes of diarrhea.
Summary & Key Takeaways
Diarrhea after fasting is a mechanical and chemical mismatch. It is a clash between the food you ate and your gut’s current functional capacity. It is not a mystery; it is physiology. The dormant gut cannot handle high volume, high fat, or high sugar immediately.

To prevent this, remember that the fast isn’t over when you stop eating. It is over when you have successfully digested your first meal. Preparation is the ultimate prevention. Treat your refeeding window with as much discipline as your fasting window.
Takeaway Checklist:
- Buffer: Always start with bone broth 30 minutes before food to prime the system.
- Avoid: No MCT oil, raw nuts, huge salads, or dairy in the first hour.
- Bind: Use psyllium husk if you are prone to the “bile dump” effect.
- Hydrate: Use electrolytes with sodium, not just plain water, if urgency strikes.
- Pace: Eat slowly. Chew thoroughly. Give your body time to catch up.
Frequently Asked Questions
Why do I experience urgent diarrhea immediately after breaking a fast?
This is typically a mechanical and chemical mismatch where a dormant digestive system is overwhelmed by the sudden introduction of food. Common physiological drivers include a hyperactive gastrocolic reflex, which signals the colon to empty prematurely, or a “bile dump” where concentrated bile irritates the intestinal lining.
What is a bile dump and how does it affect post-fasting digestion?
During a fast, the gallbladder stores and concentrates bile since no fats are present to trigger its release. When you finally eat, a massive amount of this concentrated bile is secreted; if the ileum cannot reabsorb it quickly enough, the excess bile salts enter the colon and cause secretory diarrhea.
Can taking magnesium supplements during a fast cause loose stools?
Yes, especially if you are using Magnesium Citrate or Magnesium Oxide, which act as osmotic laxatives by drawing water into the intestines. To prevent gastrointestinal distress, I recommend switching to Magnesium Glycinate or Malate, which are better absorbed and less likely to trigger urgency when you refeed.
Why is bone broth considered the best food to break a long fast?
Bone broth acts as a “liquid buffer” that gently wakes up the digestive tract by providing electrolytes and the amino acid glycine to support gut lining integrity. It stimulates the production of gastric juices and enzymes without the heavy caloric load that often triggers a rapid evacuation reflex.
Is it safe to break a fast with high-sugar fruits like watermelon?
Breaking a fast with high-fructose fruits can lead to osmotic shock, where the concentrated sugar pulls a massive influx of water from the bloodstream into the gut lumen. This results in immediate watery diarrhea, making it much safer to start with lean proteins or cooked, low-fiber vegetables instead.
How does the gastrocolic reflex contribute to refeeding urgency?
The gastrocolic reflex is a neural signal that triggers colonic contractions when the stomach stretches. After fasting, this reflex is often hypersensitive, causing the body to “make room” for new food by forcefully ejecting current contents before the colon has time to absorb excess water.
Why does MCT oil or butter coffee often cause diarrhea after fasting?
Pure liquid fats trigger an aggressive release of Cholecystokinin (CCK), which causes the gallbladder to contract and dump bile. Without a solid food matrix to slow down transit time, these fats hit the system too fast for the dormant pancreas to produce enough lipase, leading to malabsorptive stool.
What is the psyllium sponge method for preventing bile acid diarrhea?
Taking one teaspoon of psyllium husk in water 15 minutes before your first meal acts as a “sponge” that binds to excess bile salts. This prevents the bile from irritating the colon wall and adds necessary bulk to the stool, effectively neutralizing the most common cause of refeeding urgency.
Which foods should I avoid in the first hour after ending a fast?
You should avoid “Red Light” foods such as dairy (due to temporary lactase deficiency), raw cruciferous vegetables, nuts, and artificial sweeteners like erythritol. These ingredients are highly fermentable or mechanically irritating, which can lead to severe bloating and liquid bowel movements in a sensitive gut.
How can I distinguish between normal post-fasting diarrhea and Refeeding Syndrome?
Standard post-fasting diarrhea is localized to the gut and usually self-limiting within a few hours. Refeeding Syndrome is a medical emergency involving dangerous electrolyte shifts and is characterized by systemic symptoms like swelling (edema), rapid heart rate, confusion, and extreme muscle weakness.
Should I use anti-diarrheal medications like Imodium after fasting?
As an RDN, I generally advise against using Loperamide (Imodium) immediately, as your body is often trying to flush out irritants like excess bile. It is better to allow the “purge” to happen naturally while focusing on aggressive electrolyte rehydration using sodium and potassium to prevent dehydration.
Why is enzyme insufficiency a problem when breaking an extended fast?
During extended fasts, the pancreas reduces the secretion of amylase, protease, and lipase to conserve resources. If you consume a large meal before these enzymes are upregulated, the undigested macronutrients ferment in the colon, drawing in water and causing foul-smelling, fatty, or loose stools.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Diarrhea after fasting can lead to dehydration or signify underlying conditions like Refeeding Syndrome. Always consult a qualified healthcare professional or a Registered Dietitian before starting a fasting regimen or if symptoms persist for more than 24 hours.
References
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – https://www.niddk.nih.gov – Provides clinical data on the Migrating Motor Complex (MMC) and gastrointestinal motility during periods of food scarcity.
- American Journal of Clinical Nutrition – “Physiological adaptations to caloric restriction and fasting” – A peer-reviewed study examining the downregulation of pancreatic enzymes during prolonged fasts.
- Journal of Clinical Gastroenterology – “Bile Acid Malabsorption: The Forgotten Cause of Chronic Diarrhea” – Research supporting the mechanism of “bile dumps” after gallbladder inactivity.
- World Health Organization (WHO) – https://www.who.int – Official guidelines on Oral Rehydration Salts (ORS) and the use of glucose-sodium cotransport for treating acute diarrhea.
- Academy of Nutrition and Dietetics – “Practice Paper: Nutritive and Nonnutritive Sweeteners” – Evidence regarding the fermentation of sugar alcohols in the gut and their osmotic effects.
- Frontiers in Nutrition – “The impact of intermittent fasting on the gut microbiome and mucosal integrity” – A study detailing the thinning of the mucosal lining and shifts in SCFA production.