Have you ever looked at a blood test report and felt a knot in your stomach? Seeing numbers marked in bold, falling outside the ‘normal’ range can be incredibly stressful. You might start imagining the worst, scheduling follow-up appointments, and worrying about your health. But what if one of the biggest reasons for these alarming numbers wasn’t a new illness, but something as simple as not drinking enough water? It might sound too simple to be true, but it’s a medical fact. The state of your hydration can dramatically alter your lab report, and understanding this is the first step toward gaining true control over your health insights.
Dehydration is a significant factor that can lead to inaccurate blood test results. In a country like India, with its diverse and often hot climate, staying adequately hydrated can be a daily challenge. This detailed guide will explore exactly how dehydration affects blood work. We will delve into the science, look at specific tests that are most impacted, and provide a clear, actionable plan to ensure your next blood test is as accurate as possible. This knowledge is crucial because an accurate diagnosis for conditions like diabetes, kidney issues, or even anemia depends on a reliable blood report.
What is Dehydration and Why is it a Concern in India?
At its core, dehydration is a simple state: your body loses more fluid than you take in. When this happens, your body doesn’t have enough water and other fluids to carry out its normal functions. While it sounds straightforward, the reasons it happens, especially in the Indian context, are numerous and often intertwined with our daily lives.
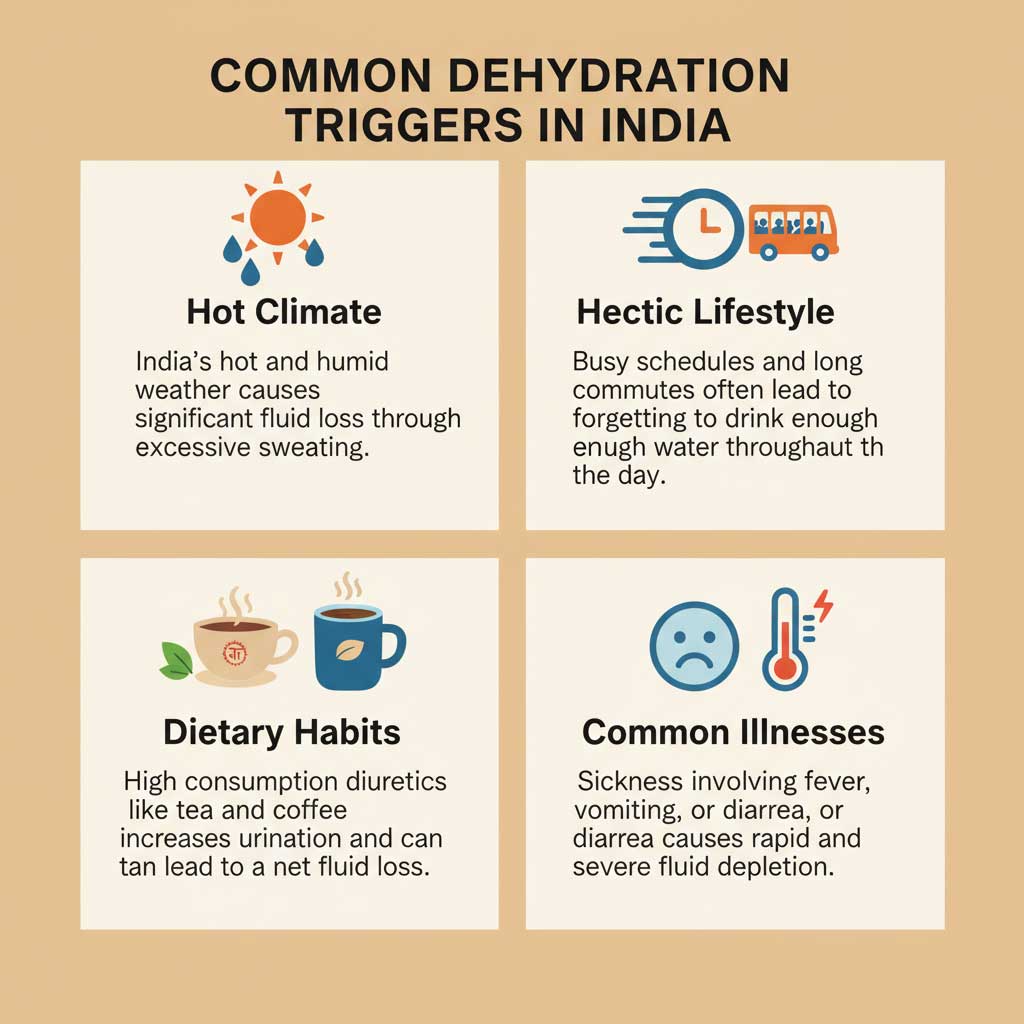
Common Causes of Dehydration in Our Daily Lives
- Climate and Environment: Much of India experiences hot and humid weather for a significant part of the year. This leads to increased sweating as the body tries to cool down, causing a rapid loss of fluids and salts.
- Hectic Lifestyles: From navigating crowded commutes to managing long work hours, remembering to drink water often takes a backseat. We might grab a quick cup of ‘chai’ or coffee, but these can actually contribute to fluid loss.
- Dietary Habits: Our love for tea and coffee is undeniable. However, both contain caffeine, which is a diuretic. This means it makes you urinate more frequently, leading to a net loss of body fluid if not balanced with enough water intake.
- Common Illnesses: A bout of food poisoning, gastroenteritis, or a simple fever—all common occurrences—can lead to significant fluid loss through vomiting, diarrhea, and sweating, causing acute dehydration.
The Science of Thirst
Your body is a finely tuned machine, composed of about 60% water. This water is vital for everything from regulating body temperature to transporting nutrients and flushing out waste. The body has a built-in alarm system for low fluid levels: the sensation of thirst. However, it’s a lagging indicator. By the time you feel thirsty, your body is already in a state of mild dehydration.
Symptoms of Dehydration to Watch For
It’s important to recognize the early signs of dehydration before it can impact your health or your blood tests. Think of this as a quick self-check you can do the day before your lab visit. The effects of dehydration can manifest in several ways:

- Dark Yellow or Amber-Coloured Urine: One of the most reliable signs. Well-hydrated urine is typically a pale, straw-like yellow.
- Infrequent Urination: Going for many hours without needing to use the restroom.
- Persistent Fatigue: Feeling unusually tired or lethargic without a clear reason.
- Dizziness or Light-headedness: A feeling of being unsteady, especially when standing up quickly.
- Dry Mouth and Skin: A sticky feeling in the mouth and skin that doesn’t feel as elastic as usual.
- Headaches: Dehydration can often trigger tension headaches or even migraines.
Recognizing these dehydration symptoms is key. If you notice any of these the day before or the morning of your blood test, it’s a strong signal to focus on rehydration.
The Science of “Thick Blood”: Understanding Hemoconcentration
To truly understand how does dehydration affect blood test results, we need to talk about a scientific concept called hemoconcentration. While the term sounds complex, the idea behind it is quite simple and is the root cause of most dehydration-related testing errors.
Also Must Read:
Can Being Dehydrated Falsely Elevate Your Cholesterol Levels?
Can Dehydration Cause High Hemoglobin and RBC Count?
5 Key Blood Test Markers That Reveal Dehydration
Fasting for a Blood Test? Here’s What You Can Drink Safely
Can Dehydration Affect Your Urine Test Results?
Imagine you make a glass of ‘nimbu pani’ (lemon water) with the perfect balance of water, lemon juice, and sugar. Now, leave that glass out in the sun. As the water evaporates, the total amount of lemon and sugar remains the same, but the liquid becomes much more concentrated and potent. The same thing happens to your blood when you’re dehydrated.
Your blood is composed of two main parts:
- Formed Elements: These are the red blood cells, white blood cells, and platelets.
- Plasma: This is the liquid portion, which is about 92% water. It carries the formed elements, along with proteins, hormones, electrolytes, and nutrients.
When you’re dehydrated, you lose water from your plasma. The volume of the liquid part of your blood decreases. However, the number of red blood cells, proteins, and other substances remains the same. They are now simply suspended in less fluid. This creates a more concentrated, or “thicker,” blood sample. This state is hemoconcentration.
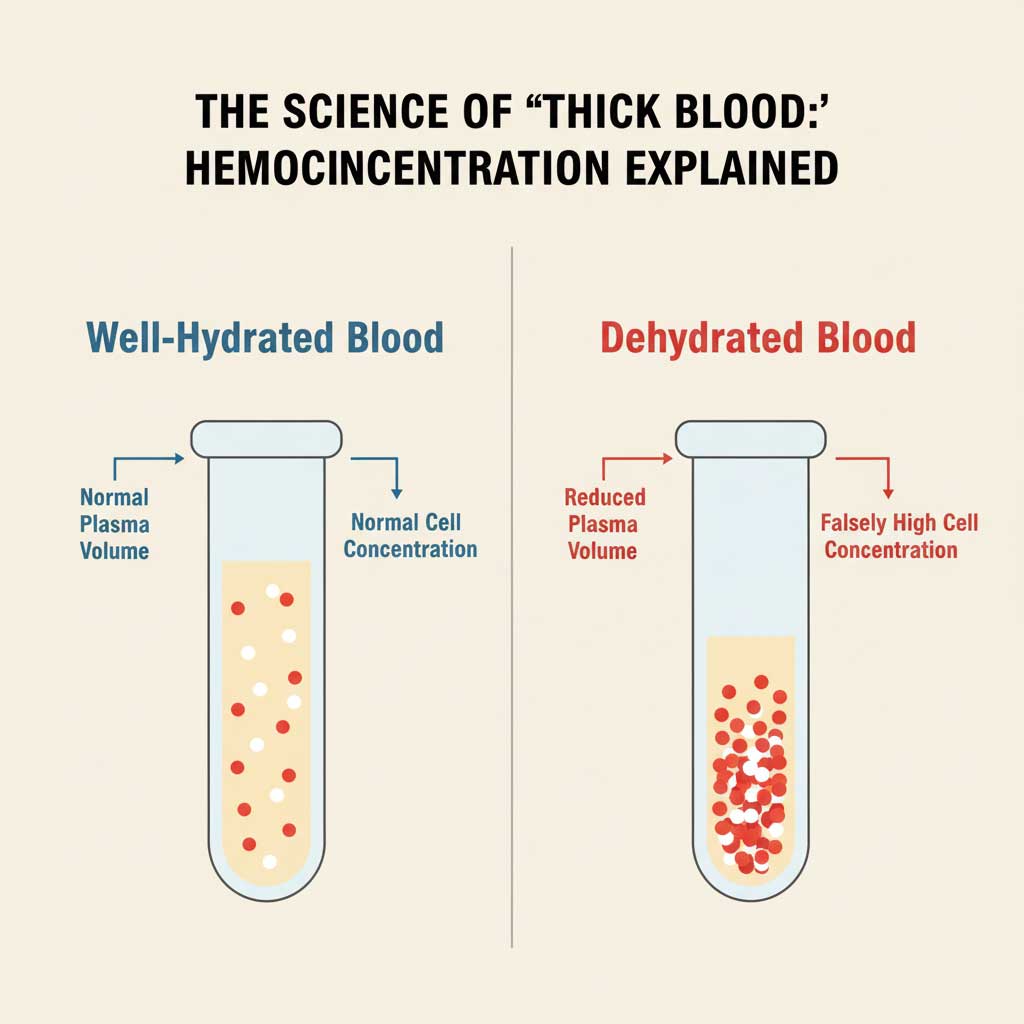
When this concentrated blood sample is run through a laboratory analyser, the machine reads the number of cells and substances per unit of volume. Because the volume of liquid is lower, the concentration of everything else appears artificially high. It’s a classic case of dehydration effects on labs. This doesn’t mean you’ve suddenly developed more red blood cells or your cholesterol has shot up overnight; it just means the components are more densely packed, leading to inaccurate blood test results. This is the fundamental mechanism that answers the question, “can dehydration affect blood test results?” Yes, it absolutely can, by creating a misleading picture of your health.
A Test-by-Test Breakdown of Dehydration’s Effects on Your Blood Work
Dehydration isn’t selective; its effects can ripple across your entire blood test report, impacting various key health markers. Let’s break down which tests are most susceptible and how your results can be skewed. Understanding these specific effects of dehydration on blood test result can help you and your doctor interpret your report more accurately.
Does dehydration affect CBC results? The Complete Blood Count Explained
The Complete Blood Count (CBC) is one of the most common blood tests ordered. It provides a snapshot of the different types of cells in your blood. Dehydration can significantly throw off these numbers.
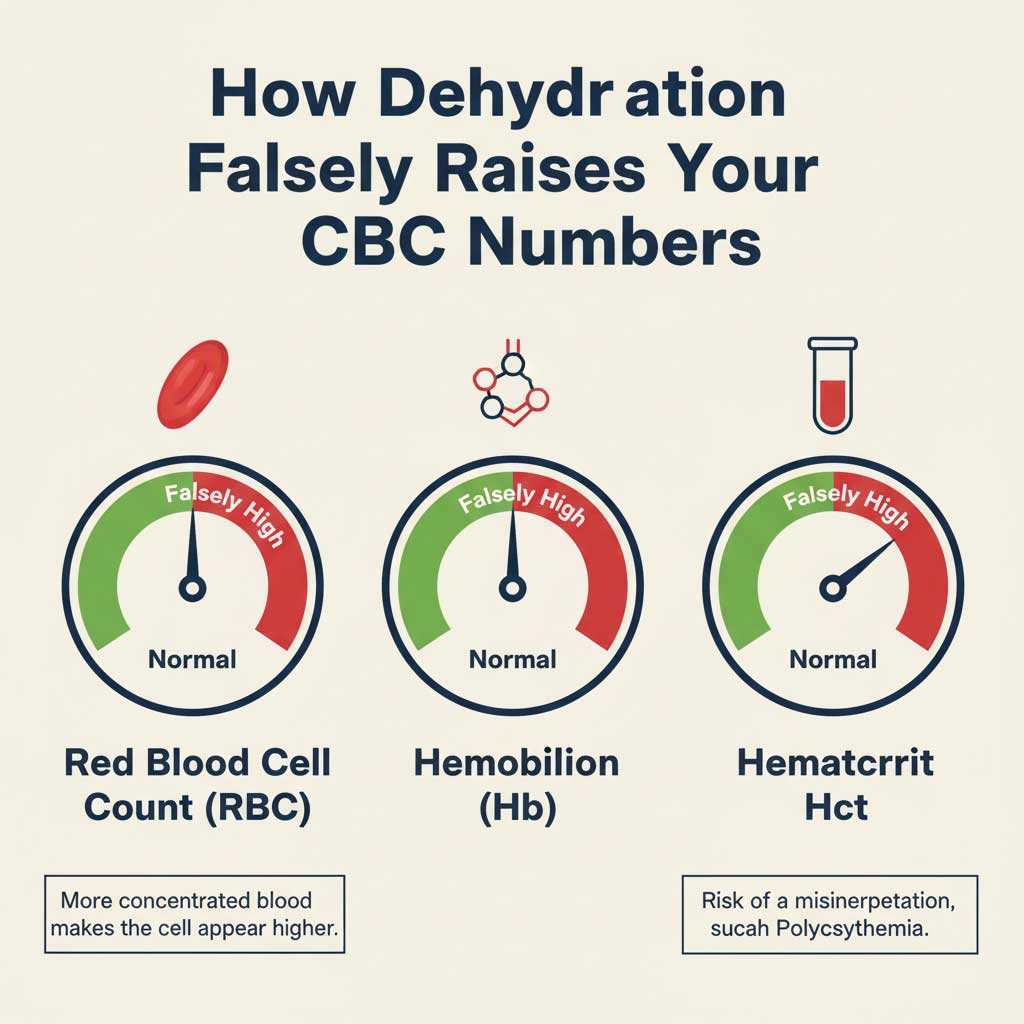
Red Blood Cells (RBC), Hemoglobin (Hb), and Hematocrit (Hct)
- How it’s affected: These three interconnected values measure the oxygen-carrying capacity of your blood. Hemoconcentration leads to a higher count of red blood cells in a smaller volume of plasma, which artificially inflates all three readings.
- Real-World Instance: Consider a 45-year-old man in Delhi preparing for an annual health check-up. He fasts overnight and skips his morning water bottle to avoid traffic delays. His blood report shows a hematocrit level of 51% (the normal range for men is typically 40-50%). This high level could prompt his doctor to investigate polycythemia, a serious condition where the body produces too many red blood cells. However, upon discussing his preparation, the doctor advises him to rehydrate properly for 24 hours and repeat the test. The new result comes back at a perfectly normal 45%. This is a classic example of how dehydration affects blood work, nearly leading to a stressful and unnecessary diagnostic path.
Kidney Function Tests (KFT): A False Alarm for Your Kidneys
Your kidneys are your body’s filtration system, and dehydration puts direct stress on them. This is clearly reflected in the Kidney Function Test (KFT).
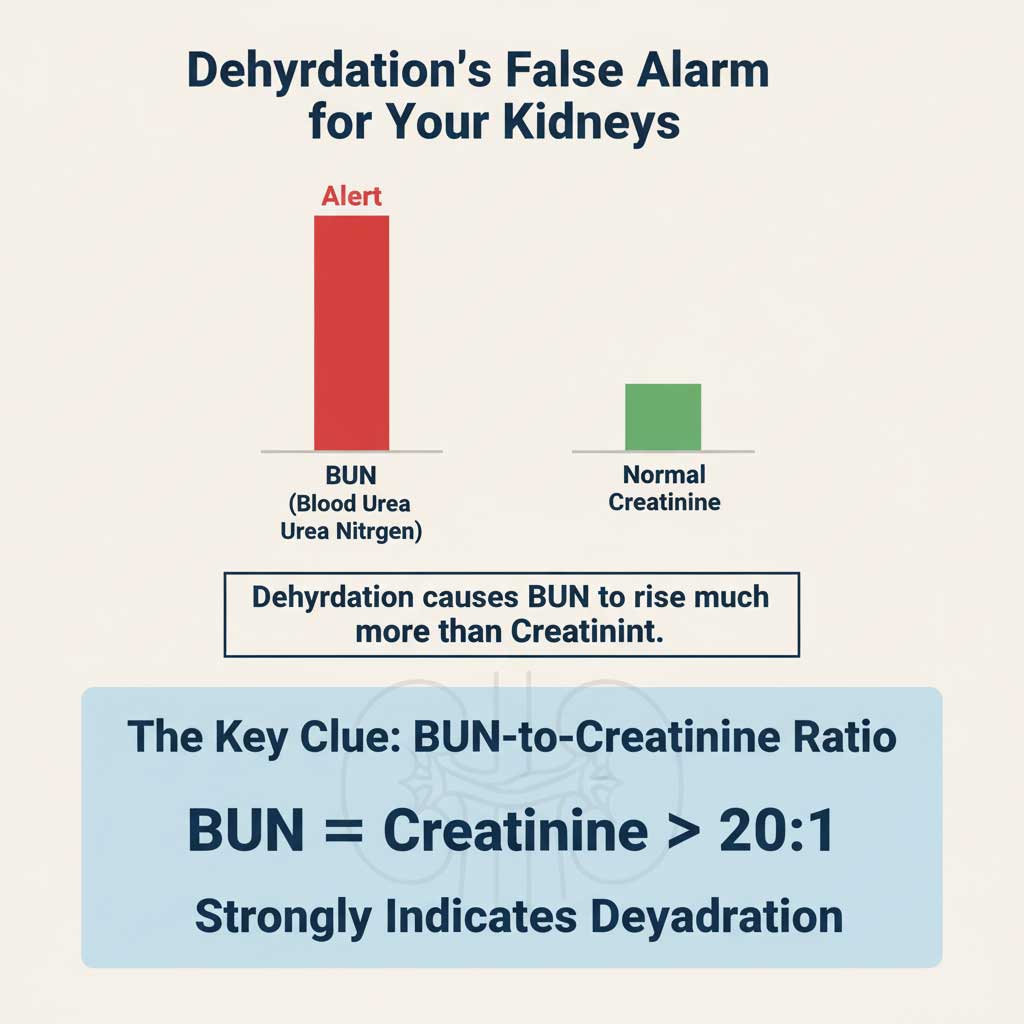
Blood Urea Nitrogen (BUN) and Creatinine
- How it’s affected: Urea is a waste product filtered by the kidneys. When you’re dehydrated, your kidneys try to conserve water by reabsorbing more urea back into the blood, causing BUN levels to rise. This connection is so strong that clinicians often look for elevated BUN and dehydration together.
- The Critical Clue: BUN-to-Creatinine Ratio: The most telling sign is the ratio between BUN and creatinine. Normally, this ratio is between 10:1 and 20:1. In dehydration, the ratio often shoots above 20:1.
- Real Data Example: Let’s say a patient’s report shows a BUN of 32 mg/dL (normal: 7-20 mg/dL) and a creatinine of 1.1 mg/dL (normal: 0.6-1.2 mg/dL). While the creatinine is normal, the BUN is high. The calculated BUN-to-Creatinine ratio is 29:1. This high ratio is a very strong indicator that the high BUN is due to dehydration (a “pre-renal” cause) and not an underlying kidney disease.
Dehydration and Electrolyte Imbalance: A Risky Fluctuation
Electrolytes are minerals in your body that have an electric charge. They are vital for balancing water levels, moving nutrients into cells, and ensuring your nerves, muscles, and heart work correctly.
Sodium (Na+), Potassium (K+), and Chloride (Cl-)
- How it’s affected: Dehydration is a primary cause of hypernatremia, or high sodium levels. As water volume in the blood decreases, the sodium concentration rises. While potassium and chloride levels can also be affected, sodium is the most sensitive indicator.
- Clinical Significance: A misdiagnosed electrolyte imbalance can be serious. Falsely elevated sodium might lead a doctor to look for hormonal disorders or other complex issues when the solution is simply to drink more water.
Cholesterol and Lipid Profile: A Deceptive Spike
Even your cholesterol levels are not immune to your hydration status. For the millions in India managing their heart health, an accurate lipid profile is essential.
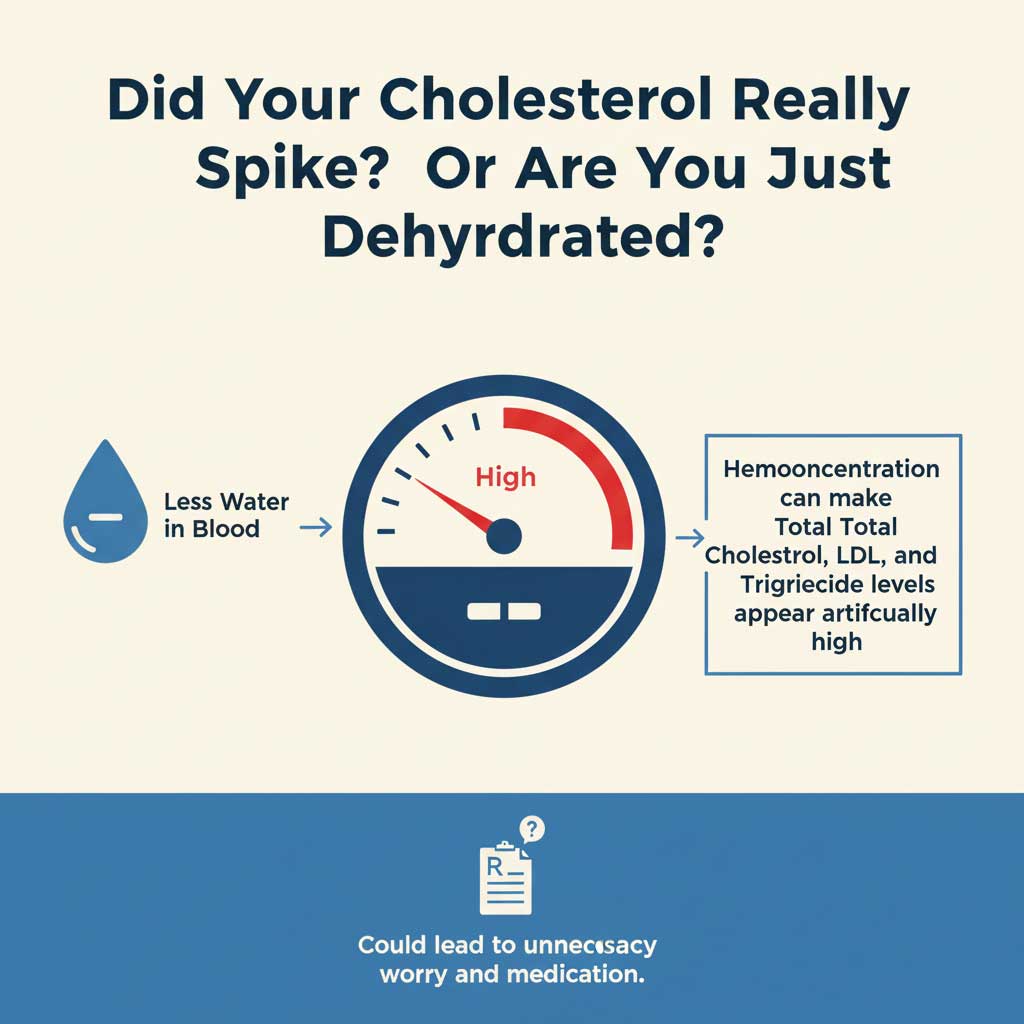
- How it’s affected: The principle of hemoconcentration applies here as well. The amount of cholesterol (Total Cholesterol, LDL, HDL) and triglycerides are measured relative to the volume of plasma. Less plasma means a higher concentration, which can make your lipid profile look worse than it actually is. This could lead to unnecessary anxiety or even the premature prescription of cholesterol-lowering medications like statins.
Blood Glucose Levels and Diabetes Monitoring
With India being the diabetes capital of the world, accurate blood glucose monitoring is a part of daily life for many.
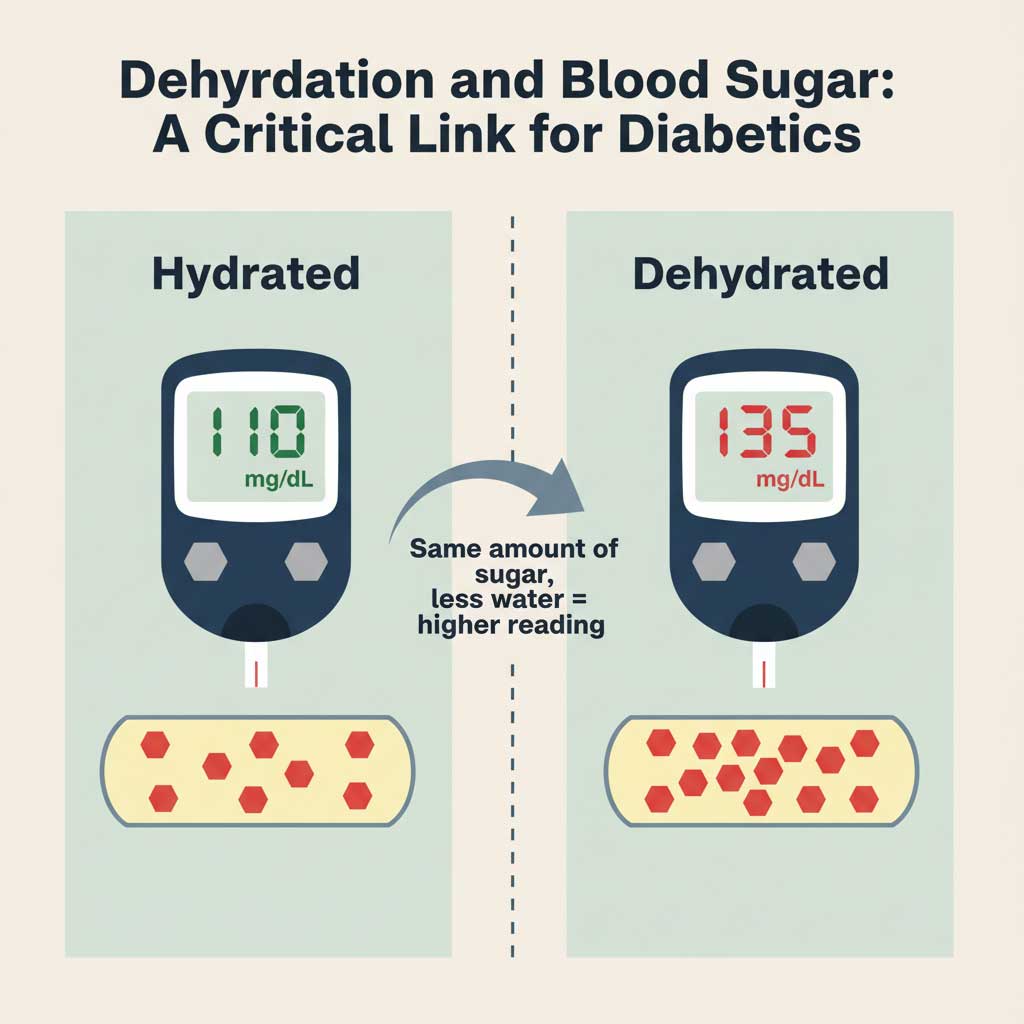
- How it’s affected: Dehydration concentrates the glucose in your bloodstream. This can lead to a falsely high blood sugar reading.
- Instance for Diabetics: An individual with well-managed Type 2 diabetes might wake up and test their fasting blood sugar. On a day they are dehydrated, the reading might be 135 mg/dL, causing alarm about their control. After rehydrating, a re-test an hour later might show a much more reassuring 110 mg/dL. For those managing their condition with insulin, acting on a falsely high reading could lead to a dangerous hypoglycemic event.
Visualizing the Impact: A Comparative Table
Words and instances are powerful, but sometimes a visual comparison makes the impact crystal clear. The following table breaks down how blood test results for a single individual can vary dramatically based on their hydration status. This highlights the potential for misinterpretation and underscores the importance of proper preparation.
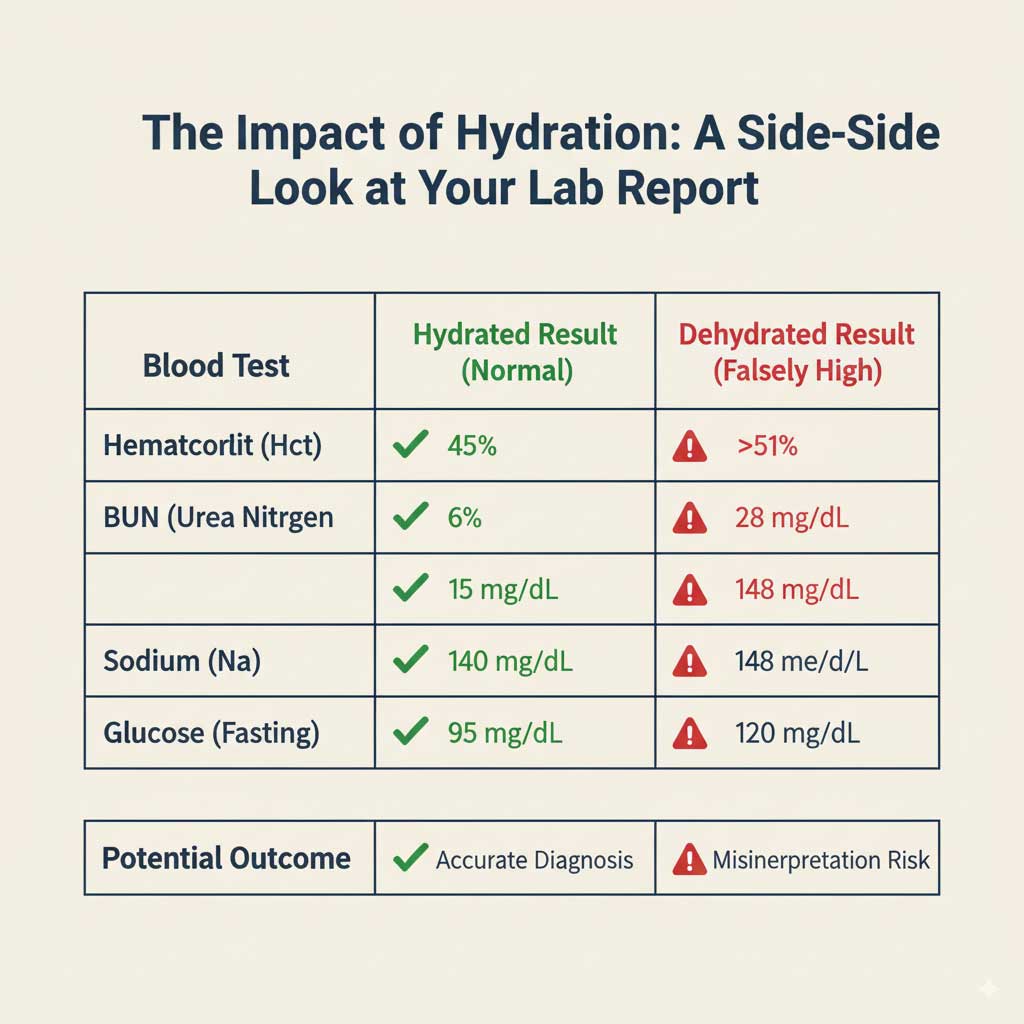
| Blood Test Parameter | Component Measured | Typical Result (Well-Hydrated) | Likely Result (Dehydrated) | Potential Clinical Misinterpretation |
| Complete Blood Count (CBC) | Hematocrit (Hct) | Male: 40-50%<br>Female: 36-44% | Elevated (e.g., >52% in males) | Misdiagnosis of Polycythemia Vera (a blood cancer) instead of simple dehydration. |
| Kidney Function Test (KFT) | Blood Urea Nitrogen (BUN) | 7-20 mg/dL | Significantly Elevated (>25 mg/dL) | Unnecessary investigation for chronic kidney disease or kidney failure. |
| Kidney Function Test (KFT) | BUN:Creatinine Ratio | 10:1 to 20:1 | Elevated (>20:1) | The key indicator of pre-renal azotemia (high nitrogen levels due to poor kidney blood flow, often from dehydration). |
| Electrolyte Panel | Sodium (Na+) | 135-145 mEq/L | Elevated (>145 mEq/L) | Misdiagnosis of hypernatremia-related disorders, potentially leading to incorrect fluid management plans. |
| Lipid Profile | Total Cholesterol | <200 mg/dL | Falsely Elevated | Unnecessary prescription of cholesterol-lowering medication (statins) and undue dietary restrictions. |
| Blood Glucose | Fasting Glucose | 70-99 mg/dL | Falsely Elevated (e.g., >110 mg/dL) | Incorrect adjustment of diabetes medication or misdiagnosis of prediabetes, causing significant patient anxiety. |
| Liver Function Test (LFT) | Albumin | 3.4-5.4 g/dL | Elevated | Can mask underlying conditions that cause low albumin (like liver or kidney disease), delaying a correct diagnosis. |
Your Proactive Guide: How to Prepare for a Blood Test Correctly
Now that you understand the profound effects of dehydration on blood test result, the good news is that preventing it is simple and entirely within your control. Following a few easy steps can make the difference between an accurate report and one that is misleading. Here is your ultimate checklist for how to prepare for a blood test.
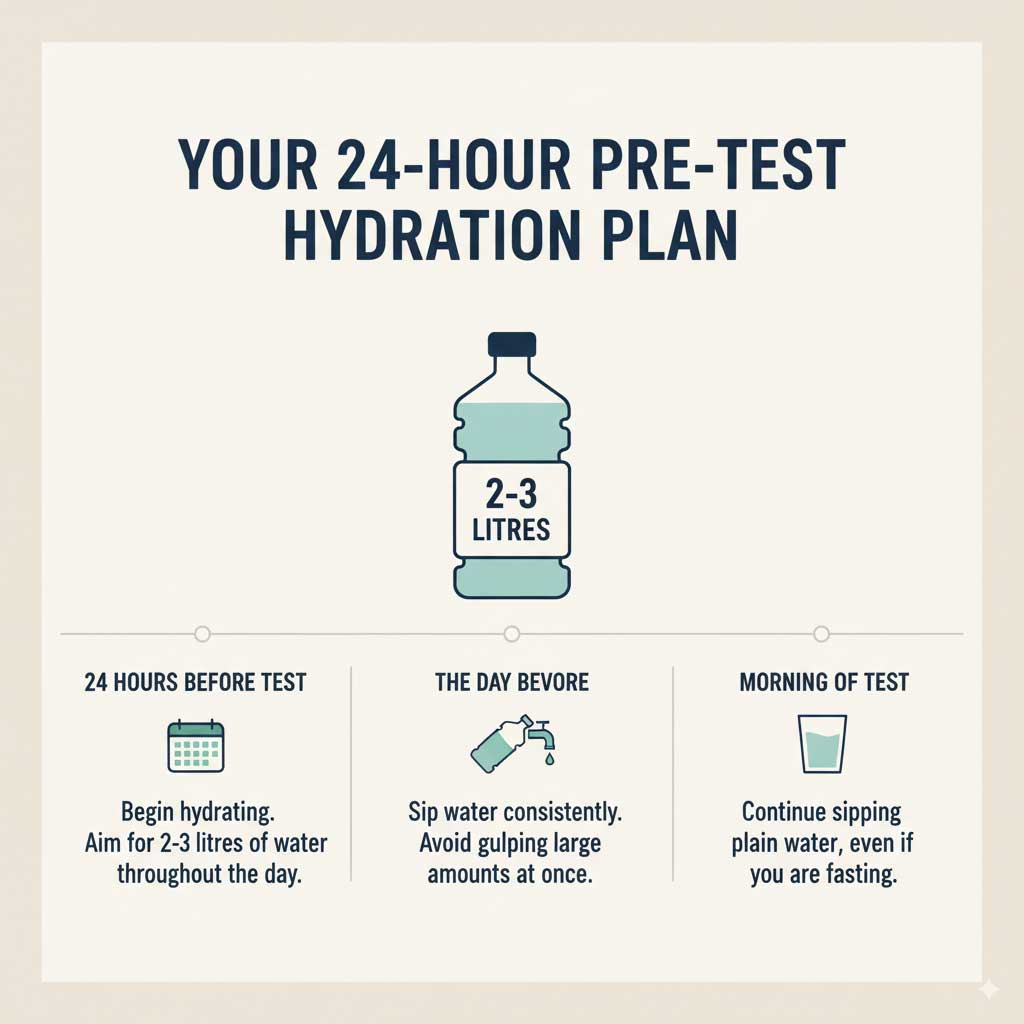
The 24-Hour Hydration Rule
Preparation for your blood test doesn’t start the morning of the test; it begins a full day before.
- Your Goal: Aim to drink at least 2-3 litres of plain water in the 24 hours leading up to your appointment. This is roughly equivalent to 8-12 glasses.
- Sip, Don’t Gulp: Instead of chugging large amounts of water at once, which can cause your body to just flush it out, sip water consistently throughout the day. Keep a water bottle with you at your desk, during your commute, and at home as a constant reminder.
Busting the Myth: Fasting Blood Test and Water Intake
This is perhaps the most common point of confusion for patients. The instruction “fasting” often creates fear of consuming anything at all, including water. Let’s clear this up once and for all.

- The Golden Rule: A fasting blood test and water are not enemies. Fasting means no food and no beverages other than plain water.
- Why Water is an Exception: Plain water contains no calories, proteins, fats, or sugars. It will not interfere with the results of tests that require fasting, such as blood glucose or a lipid profile. In fact, drinking water is highly encouraged.
- The Necessity of Water: As we’ve established, avoiding water will lead to dehydration and hemoconcentration, skewing the very results your fasting test is trying to measure accurately. So, please, drink water.
Beverages to Avoid Before Your Blood Draw
While hydrating with water is crucial, hydrating with the wrong liquids can be counterproductive. In the 12-24 hours before your test, it’s best to avoid:

- Coffee and Caffeinated Tea: Caffeine is a natural diuretic, which increases urine production and can contribute to dehydration.
- Alcohol: Alcohol is also a potent diuretic and should be avoided for at least 24 hours before your blood test.
- Sugary Drinks and Juices: These are not allowed during a fasting period and can directly impact your blood glucose and triglyceride levels. Stick to plain water.
The Added Benefit: Making the Blood Draw Smoother
Proper hydration before blood draw has another immediate, practical advantage. When you are well-hydrated, your veins are plumper, more elastic, and easier for the phlebotomist (the technician drawing your blood) to locate. This often leads to:
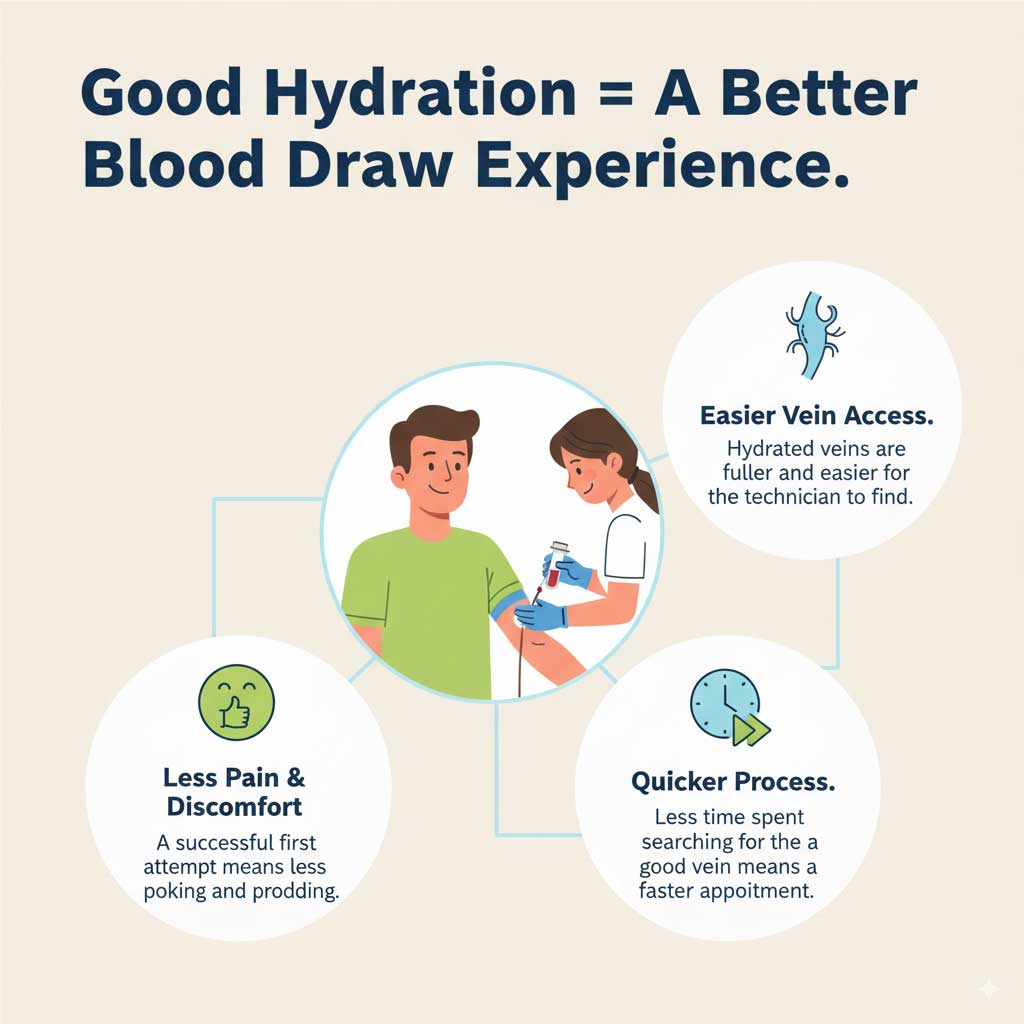
- A quicker, one-prick blood draw.
- Less pain and discomfort for you.
- A reduced chance of bruising at the site of the needle prick.
Your Health is in Your Hands
Your journey to understanding your health through blood tests should be built on a foundation of accuracy. The data in your report is not just numbers on a page; it guides critical medical decisions, shapes your lifestyle choices, and impacts your peace of mind. As we have seen, dehydration can affect blood test results in a profound and misleading way.
However, the power to prevent this distortion is entirely yours. It doesn’t require expensive medication or complicated procedures. It simply requires a conscious effort to hydrate. By drinking plenty of water the day before your test, continuing to drink water even when fasting, and avoiding diuretics like coffee and alcohol, you are taking a simple yet powerful step to ensure the integrity of your results.
By following this guide, you are empowering both yourself and your doctor with the most accurate data possible. This collaboration is the key to better health outcomes and a more confident approach to managing your well-being.
10 Commonly Asked Questions About Dehydration and Blood Tests
- How much water should I drink before a blood test?
Aim for 2-3 litres (about 8-12 glasses) of water in the 24 hours before your test. Continue to sip water on the morning of the test as well, even if you are fasting. - Can I drink coffee before a fasting blood test?
No. Coffee, even black coffee without sugar, contains caffeine which is a diuretic and can cause dehydration. It can also sometimes affect blood sugar and blood pressure readings. Stick to plain water. - Can dehydration make my red blood cell count high?
Yes. Dehydration reduces the plasma (liquid) volume in your blood, making the red blood cells more concentrated. This can lead to an artificially high red blood cell count, hemoglobin, and hematocrit, a condition known as hemoconcentration. - Will being dehydrated affect my thyroid test results?
While the direct impact on thyroid hormones (TSH, T3, T4) is less pronounced than on a CBC or kidney tests, severe dehydration can put stress on the entire endocrine system. For the most accurate results, it is always best to be well-hydrated. - How can I tell if my blood test was affected by dehydration?
A key indicator is a high BUN-to-creatinine ratio (often above 20:1). Other signs can include simultaneously elevated hematocrit, albumin, and sodium levels. The best course of action is to discuss your hydration status with your doctor when reviewing the results. - Can drinking too much water affect my blood test results?
While it’s theoretically possible, causing hemodilution (the opposite of hemoconcentration), it’s very difficult to achieve for a healthy individual. You would need to drink an excessive and unsafe amount of water in a short period. Following the standard advice of 2-3 litres over 24 hours will not negatively impact your results. - Does dehydration affect urine test results as well?
Absolutely. Dehydration makes your urine more concentrated, which will affect results for specific gravity, ketones, and the concentration of various substances. Accurate urine tests also depend on normal hydration. - How soon before a blood test should I stop drinking alcohol?
It is best to avoid alcohol for at least 24 hours before your blood test. Alcohol is a diuretic that causes dehydration and can also directly affect liver function tests and triglyceride levels. - Can dehydration cause high creatinine levels?
While BUN is more sensitive to hydration, severe or prolonged dehydration can reduce blood flow to the kidneys enough to cause a temporary, mild increase in creatinine levels. However, a significantly elevated creatinine level usually points to an underlying kidney issue. - What should I do if I think my results were inaccurate due to dehydration?
Be open with your doctor. Inform them that you may have been dehydrated at the time of the test. They can then interpret the results in that context and may recommend a repeat test after ensuring you are properly hydrated to confirm the findings.