Your blood test is a direct dialogue with your body. It provides a precise, quantitative look at your internal health, offering critical insights that guide medical decisions. For this dialogue to be clear and accurate, however, the line cannot have any static.
Table of Contents
The “static” in this case is the metabolic noise created by the foods, drinks, and activities you engage in during the 24 hours prior to your blood draw. Understanding the specific foods to avoid before a blood test is not merely a helpful tip—it is a clinical imperative for ensuring the integrity of your results.
Food Checker Before Blood Test
Enter the food item below to check if it can be consumed before blood tests.
* None of this is medical advice; users must follow their doctor/lab instructions.
This guide will move beyond the surface-level advice. We will perform a deep dive into the clinical reasoning behind what not to eat the night before a blood test, exploring the precise physiological mechanisms at play. By understanding why these rules exist, you become an empowered and informed participant in your own healthcare. We will demystify the fasting rules for blood work and provide an actionable, expert-level protocol to ensure your next blood test is as accurate as humanly possible.
The Clinical Imperative of the Fasting State
When a doctor requests a “fasting” sample, they are seeking a snapshot of your body in its purest metabolic state. This provides a stable, predictable baseline that allows for the accurate assessment of your body’s ability to manage its own chemistry without external influence.
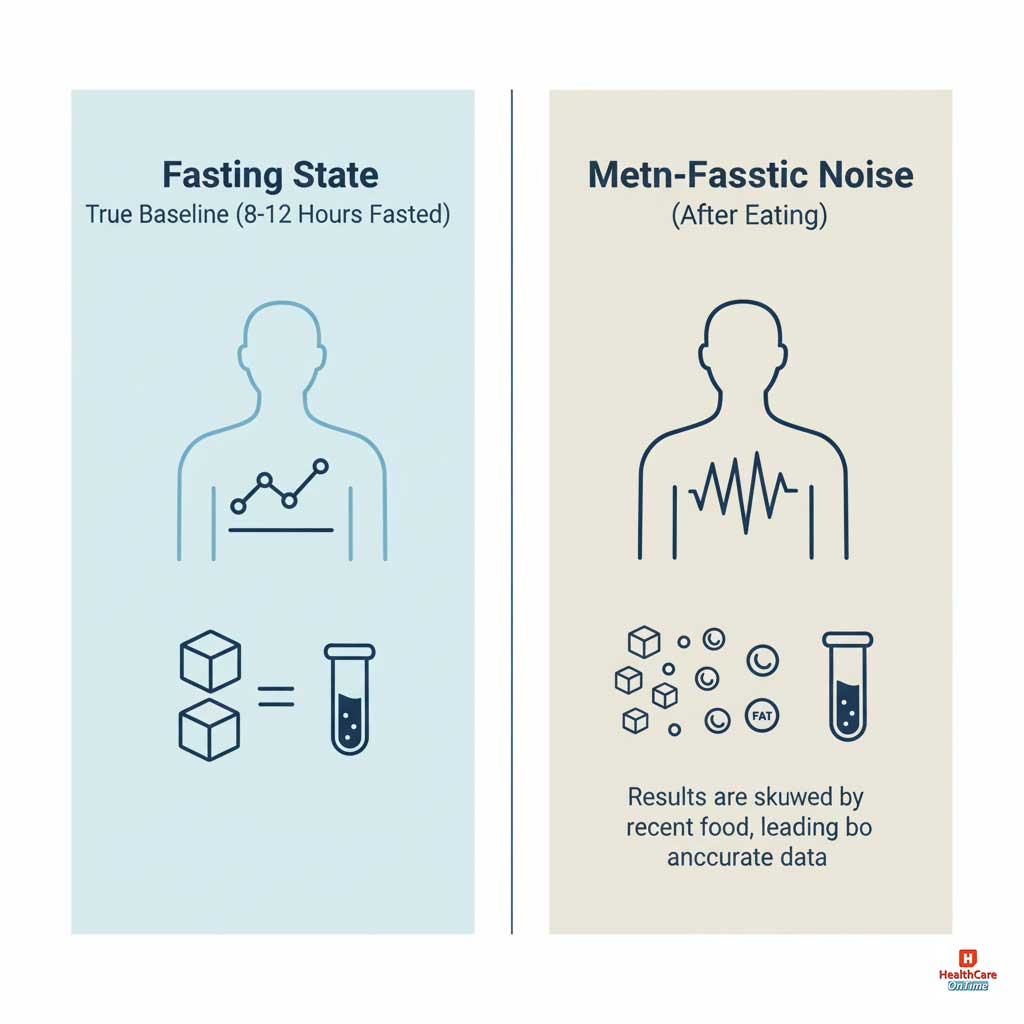
Achieving a True “Postabsorptive” Baseline
A true fasting state, known in clinical terms as the “postabsorptive state,” is achieved when the body has fully completed the digestion and absorption of your last meal. This metabolic equilibrium is typically reached after 8 to 12 hours without food.
In this state, your blood glucose has stabilized, insulin levels have returned to a resting baseline, and the transient fats (lipids) from your meal have been cleared from circulation. It is only from this pristine baseline that a physician can accurately diagnose or monitor conditions. Anything less is a measurement of your body’s reaction to a meal, not a measurement of your underlying health.
High-Sensitivity Tests: Which Biomarkers Demand a Fasting State?
While not all tests are affected by food, several of the most critical diagnostic panels are extremely sensitive to recent consumption. The fasting rules for blood work are therefore non-negotiable for:
- Glucose and Insulin Panels: These tests are the bedrock of diabetes and metabolic syndrome diagnosis. They are designed to measure your body’s endogenous (internal) glucose regulation. Any exogenous (external) source of sugar from food renders this measurement invalid.
- Lipid (Cholesterol) Panel: This panel assesses your risk for cardiovascular disease. The most variable and immediately affected component is triglycerides. Measuring “postprandial” (after-eating) triglycerides provides different information than the fasting baseline required for standard risk calculation.
- Comprehensive Metabolic Panel (CMP): This broad-spectrum test includes glucose, electrolytes, and markers of kidney and liver function. Fasting is required primarily for the glucose component, but severe dehydration or large meals can also subtly skew electrolyte results.
- Iron Panel: Your body’s iron absorption is directly influenced by the food you eat. Consuming an iron-rich meal can cause a temporary surge in serum iron levels, potentially masking an underlying iron deficiency.
The Definitive List of Foods to Avoid (and the Science Why)
This is the central pillar of your preparation. Each category below is avoided for a specific, scientific reason that directly impacts the technology and chemistry used in the laboratory to analyze your blood.
High-Fat, Fried, and Heavy Foods
This is arguably the most common cause of a rejected or invalidated blood sample, particularly for lipid and metabolic panels.
The Clinical Reason: Postprandial Lipemia and Spectrophotometric Interference
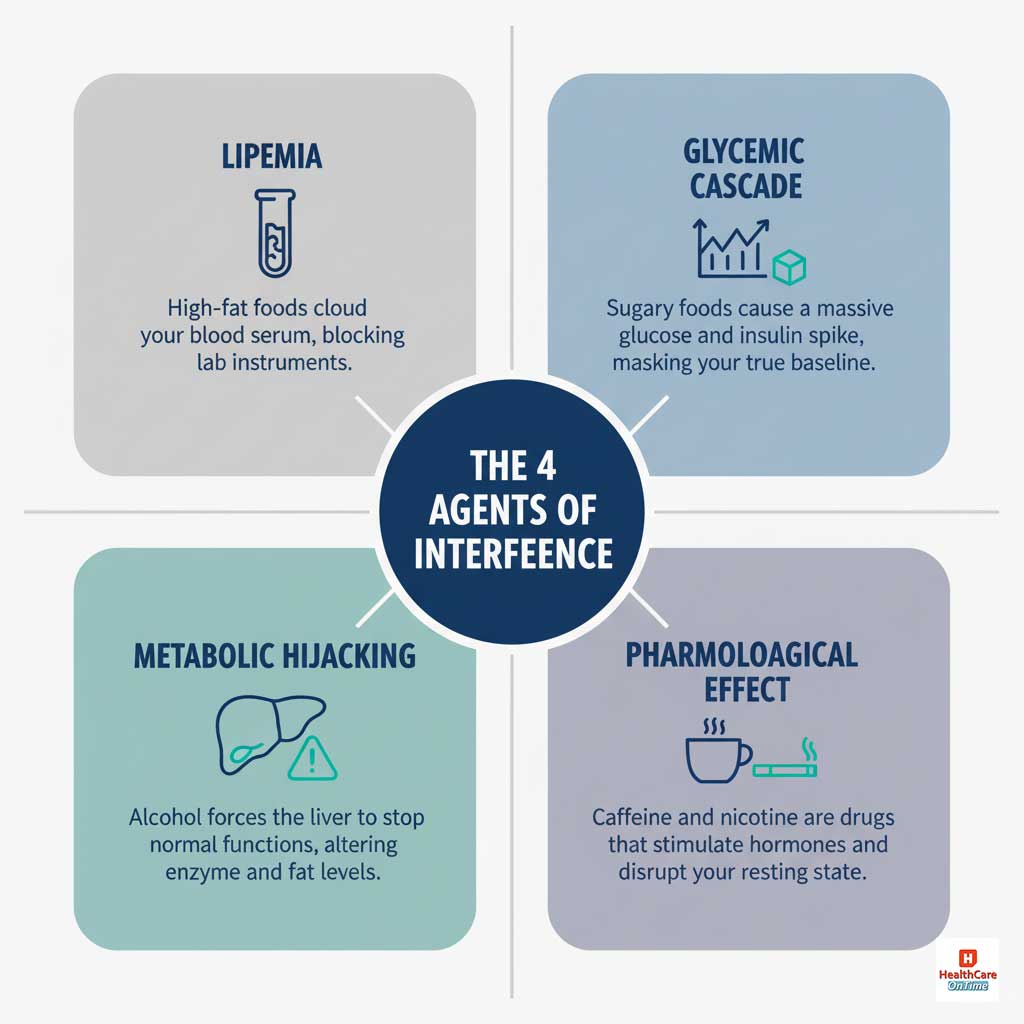
- Ingestion & Chylomicron Formation: When you eat a high-fat meal before a blood test, your digestive system packages the fats into large transport particles called chylomicrons.
- Serum Turbidity: These particles are released into your bloodstream, causing the liquid part of your blood (the serum or plasma) to become opaque, cloudy, and milky. This is a clinical condition called postprandial lipemia.
- Spectrophotometric Interference: Modern laboratory analyzers are highly sophisticated spectrophotometers. They work by passing a precise beam of light through the serum to measure the concentration of different biomarkers. When the serum is turbid, the chylomicron particles scatter the light beam, preventing the machine from getting a valid reading. This can throw off dozens of tests, rendering the entire sample useless.
Sugars, Juices, and Refined Carbohydrates
These substances trigger a rapid and significant hormonal response that directly conflicts with the purpose of fasting tests.
“If you have a pre-existing health condition like diabetes, CKD, heart disease, or thyroid issues, your test preparations require extra care. Read more in our special preparation blog.”
The Clinical Reason: The Exogenous Glycemic Excursion
The purpose of a fasting glucose test is to measure your body’s ability to maintain a stable blood sugar level on its own. When you consume sugar, juice, or refined carbs (which your body treats just like sugar), you are initiating a “glycemic excursion”—a rapid rise in blood glucose driven by an external source.
This forces your pancreas to release a surge of insulin to manage the sugar load. The resulting measurement would show extremely high glucose and insulin levels that have nothing to do with your baseline metabolic health and could easily be misinterpreted as a sign of severe diabetes. It is imperative to avoid sugary drinks and foods.
Alcoholic Beverages
Consuming alcohol before a blood test is problematic because the body treats it as a poison, prioritizing its metabolism above all other normal functions.
The Clinical Reason: Metabolic Prioritization and Hepatocyte Stress
- Disrupted Lipid Synthesis: As the liver works overtime to metabolize alcohol, its normal process of managing fats is disrupted. This can lead to an acute, temporary overproduction of triglycerides, which are then released into the bloodstream, falsely elevating your lipid panel results.
- Hepatocyte Enzyme Leakage: Alcohol metabolism is a stressful process for liver cells (hepatocytes). This stress can cause the cell membranes to become temporarily more permeable, allowing liver enzymes like GGT, AST, and ALT to leak into the bloodstream. An elevated reading could be mistaken for chronic liver inflammation or damage.
Coffee and Other Caffeinated Beverages
This is the most common point of confusion. “But it’s black, with no calories!” is a frequent refrain. However, the absence of calories does not mean an absence of physiological effect. The caffeine in coffee before a blood test has three distinct interfering actions.
The Clinical Reasons:
- The Glycemic/Insulin Effect: Caffeine is a stimulant that can promote the release of hormones like cortisol and epinephrine. These hormones can signal the liver to release some of its stored glucose into the bloodstream, potentially causing a mild but noticeable increase in blood sugar, even in a fasted state.
- The Hemodynamic Effect: Caffeine has well-documented hemodynamic effects, including increasing blood pressure and causing vasoconstriction (narrowing of blood vessels). This is not your body’s true resting state.
- The Hydration Effect: Caffeine is a diuretic, increasing urine output and potentially leading to mild dehydration. Dehydration concentrates the blood, which can falsely increase the measured values of cellular components (like red blood cells) and certain proteins. For this reason, any tea before a blood test containing caffeine must also be avoided.
Specific Food Items to Avoid: A Quick-Reference Table
For those who want a simple checklist, here are over 20 specific items to avoid in the 12-24 hours before your blood test, along with the primary reason for their exclusion.
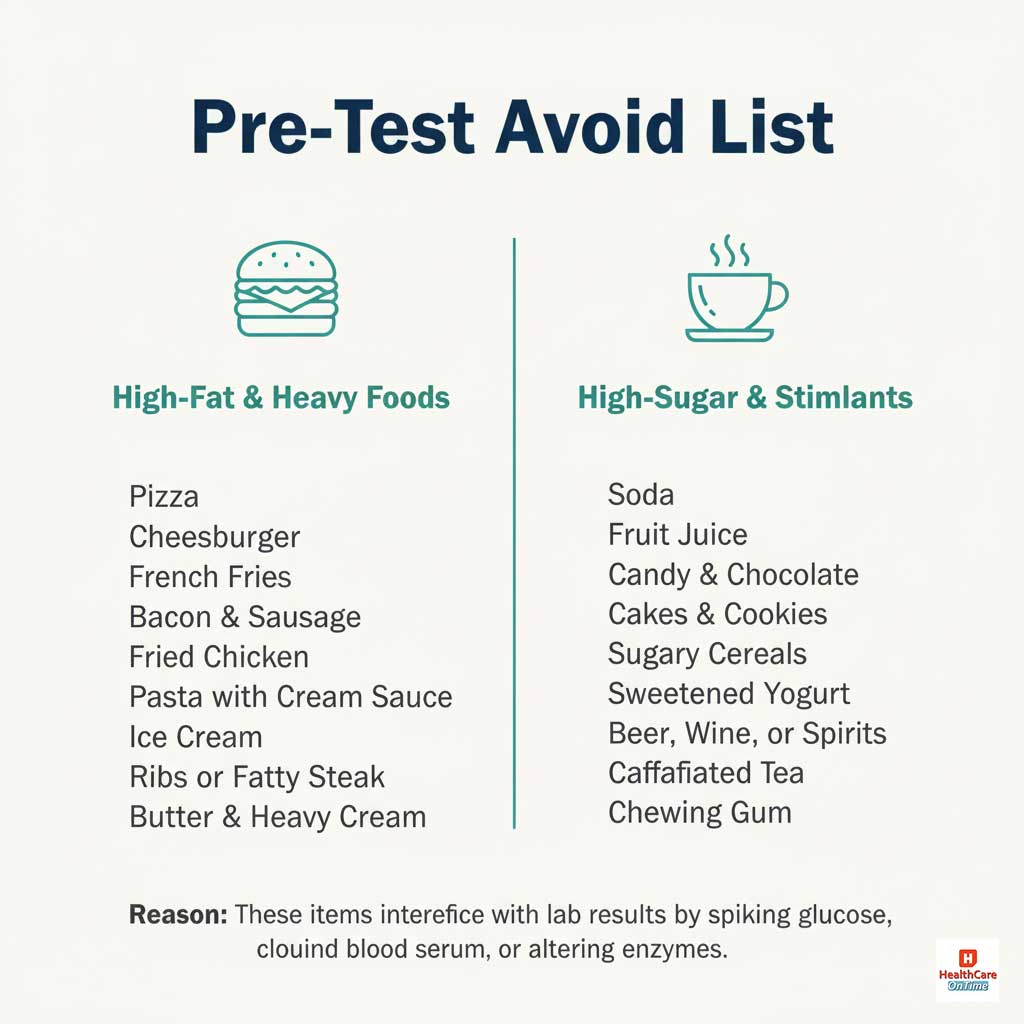
| Food/Drink Item | Primary Reason for Avoidance |
| Pizza | High fat and refined carbs cause lipemia and spike glucose. |
| Cheeseburger | High in saturated fat, leading to cloudy serum (lipemia). |
| French Fries | High in fat from frying and are a simple carbohydrate. |
| Bacon & Sausage | Extremely high in fat, a primary cause of lipemia. |
| Fried Chicken | High fat content from the frying process interferes with lab machines. |
| Pasta with Cream Sauce | High in both fat and refined carbohydrates. |
| Ice Cream | High in both fat and sugar, impacting lipids and glucose. |
| Doughnuts & Pastries | High in sugar, refined flour, and fat. |
| Ribs or Fatty Steak | High saturated fat content can significantly raise triglycerides. |
| Butter & Heavy Cream | Concentrated sources of fat that directly cause lipemia. |
| Soda (e.g., Coke, Pepsi) | Extremely high in sugar, causing a severe blood glucose spike. |
| Fruit Juice (any kind) | A concentrated source of sugar without fiber; spikes glucose rapidly. |
| Energy Drinks | High in sugar and caffeine, which interferes with multiple tests. |
| Candy & Chocolate Bars | Pure sugar and fat, disrupting glucose and lipid readings. |
| Cakes, Cookies, & Pies | High in sugar, refined flour, and fat. |
| Sugary Breakfast Cereals | Refined carbs that act like sugar, causing a glucose surge. |
| Sweetened Yogurt | High sugar content disrupts a true fasting glucose baseline. |
| Beer, Wine, or Spirits | Alcohol raises triglycerides and stresses the liver, elevating enzymes. |
| Coffee (any kind) | Caffeine stimulates hormone release and can alter glucose levels. |
| Caffeinated Tea | Contains caffeine, which acts as a stimulant and diuretic. |
| Chewing Gum (any kind) | Stimulates the digestive system, disrupting a true fasting state. |
Beyond Diet: Crucial Non-Food Factors That Alter Your Blood Chemistry
Your pre-blood test diet and hydration are paramount, but they are not the only factors. Physical activity and supplements can introduce equally significant variables.
Strenuous Exercise and the “Enzyme Leakage” Phenomenon
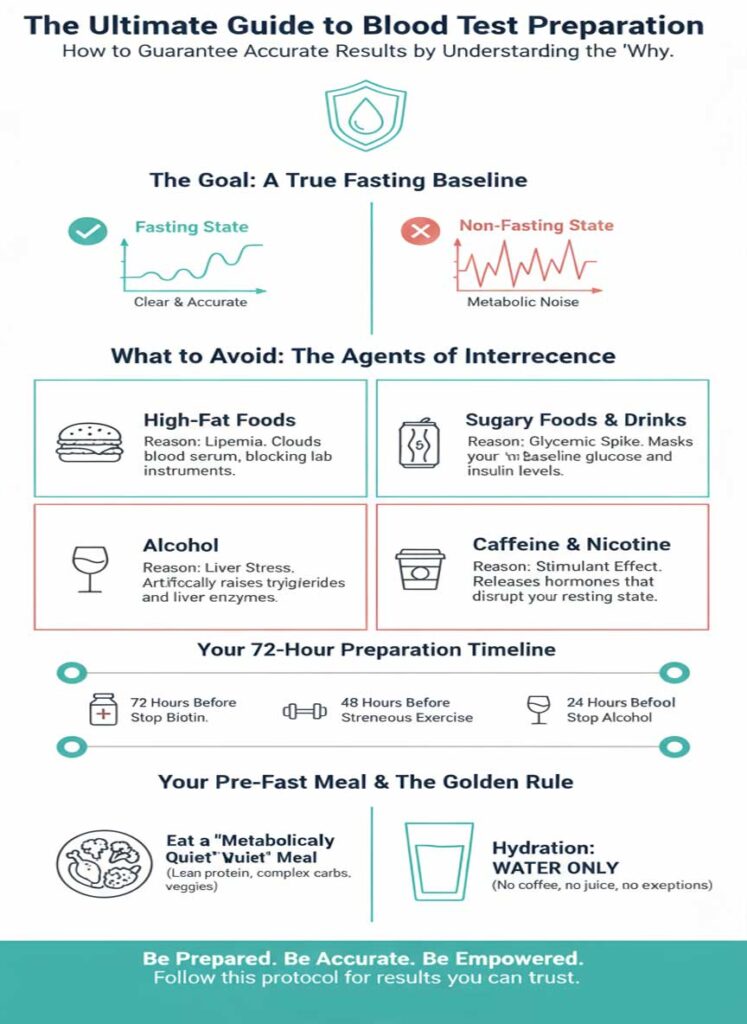
A common error among health-conscious individuals is maintaining their intense workout schedule right up until their test. However, a hard exercise before a blood test can produce results that mimic serious disease. The intense exertion causes a release of intracellular enzymes from muscle tissue, most notably Creatine Kinase (CK). Levels can be elevated by thousands of units, which could trigger an investigation for rhabdomyolysis or other myopathies. Since AST and ALT are also present in muscle, their elevation can falsely suggest liver damage. A minimum 48-hour rest period from strenuous activity is advised.
The Critical Alert on Biotin: Understanding a Direct Lab Interference
The warning on biotin/supplements before a blood test cannot be overstated. High-dose biotin, found in “hair, skin, and nails” formulas, does not just subtly alter a biomarker—it directly sabotages the testing machinery itself. Many lab tests use a “Streptavidin-Biotin” bond as a core part of their mechanism. Excess biotin from your blood physically blocks this mechanism, leading to catastrophic and unpredictable errors. The FDA has issued a formal safety communication on this, as biotin interference has been linked to misdiagnoses of Graves’ disease and missed diagnoses of heart attacks. This is non-negotiable: stop all high-dose biotin for a minimum of 72 hours.
Your Action Plan: The Ideal Pre-Test Meal and Hydration
So, with a long list of what to avoid, what to eat the night before a fasting blood test? The answer is to aim for a meal that is metabolically “quiet.”
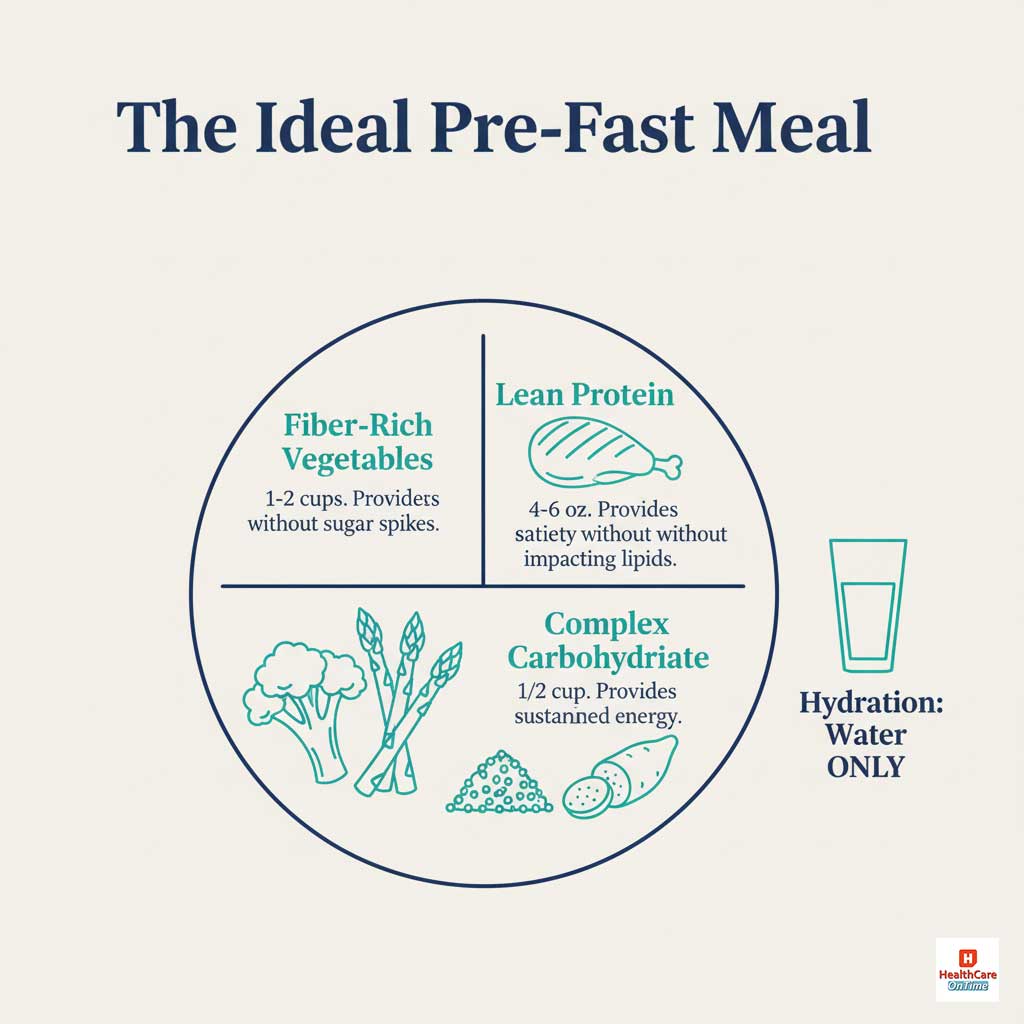
The Blueprint for the Ideal Pre-Test Meal
- Component 1: Lean Protein (4-6 oz): Provides satiety without a lipid spike. Examples: Baked chicken breast, grilled cod or tilapia, tofu.
- Component 2: Complex Carbohydrate (1/2 cup): Provides sustained energy without a sugar rush. Examples: Quinoa, brown rice, sweet potato.
- Component 3: Fiber-Rich Vegetables (1-2 cups): Provides nutrients and aids digestion. Examples: Steamed broccoli, asparagus, green beans, or a simple salad with vinaigrette.
Hydration: The “Water ONLY” Rule
The common question, “water only or is lemon water allowed,” has a definitive answer: ONLY plain, unflavored water is permitted. Lemon juice contains citric acid and sugars that can stimulate the digestive system. The same is true for the artificial sweeteners and acids in seltzers and diet sodas. Stay well-hydrated with plain water to ensure your veins are plump and your blood is not artificially concentrated.
The Definitive Pre-Test Protocol: A Timeline for Success
This clinical table provides the ultimate reference for your preparation. It is your step-by-step guide to guaranteeing data integrity.
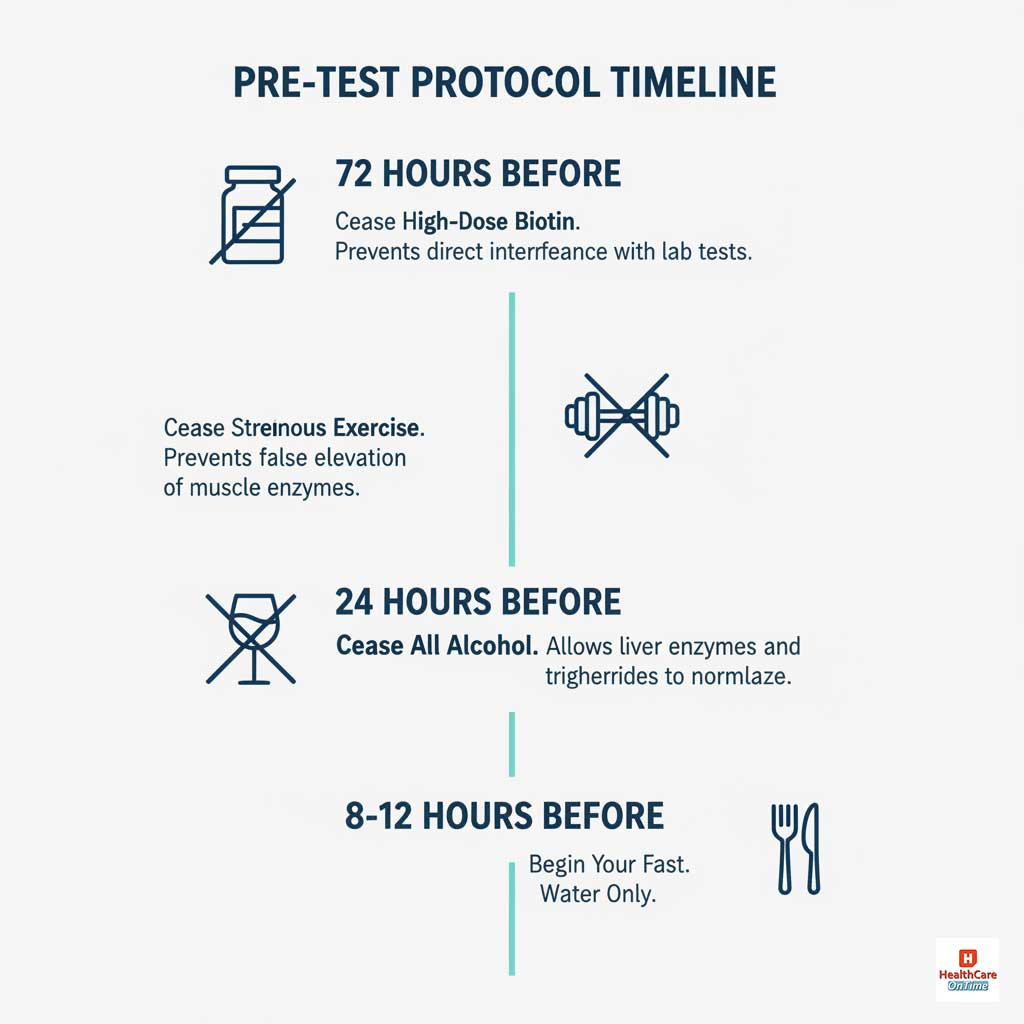
| Timeframe | Action | The Clinical Rationale for This Action |
| 72 Hours Before | CEASE HIGH-DOSE BIOTIN | To prevent direct, structural interference with lab testing mechanisms, avoiding potentially catastrophic misdiagnoses. |
| 48 Hours Before | CEASE STRENUOUS EXERCISE | To prevent the release of muscle enzymes (CK, AST) that could be misinterpreted as signs of cardiac or liver pathology. |
| 24 Hours Before | CEASE ALL ALCOHOL | To allow liver enzymes and triglycerides to return to a true baseline. |
| 12 Hours Before | CONSUME FINAL MEAL | Eat a “metabolically quiet” meal. The fasting period begins now. |
| During the Fast | WATER ONLY. ZERO EXCEPTIONS. | To maintain a true postabsorptive state, free from any external metabolic stimulation. Avoid all food, coffee, tea, gum, etc. |
| Morning of Test | HYDRATE & TAKE PRESCRIBED MEDS | Continue drinking plain water. Take doctor-prescribed medications as scheduled with a small amount of water. |
Post-Draw Protocol: How to Safely Break Your Fast
The moment the blood draw is complete, your fast is over. It is important to break it promptly and safely to avoid any lightheadedness or discomfort.
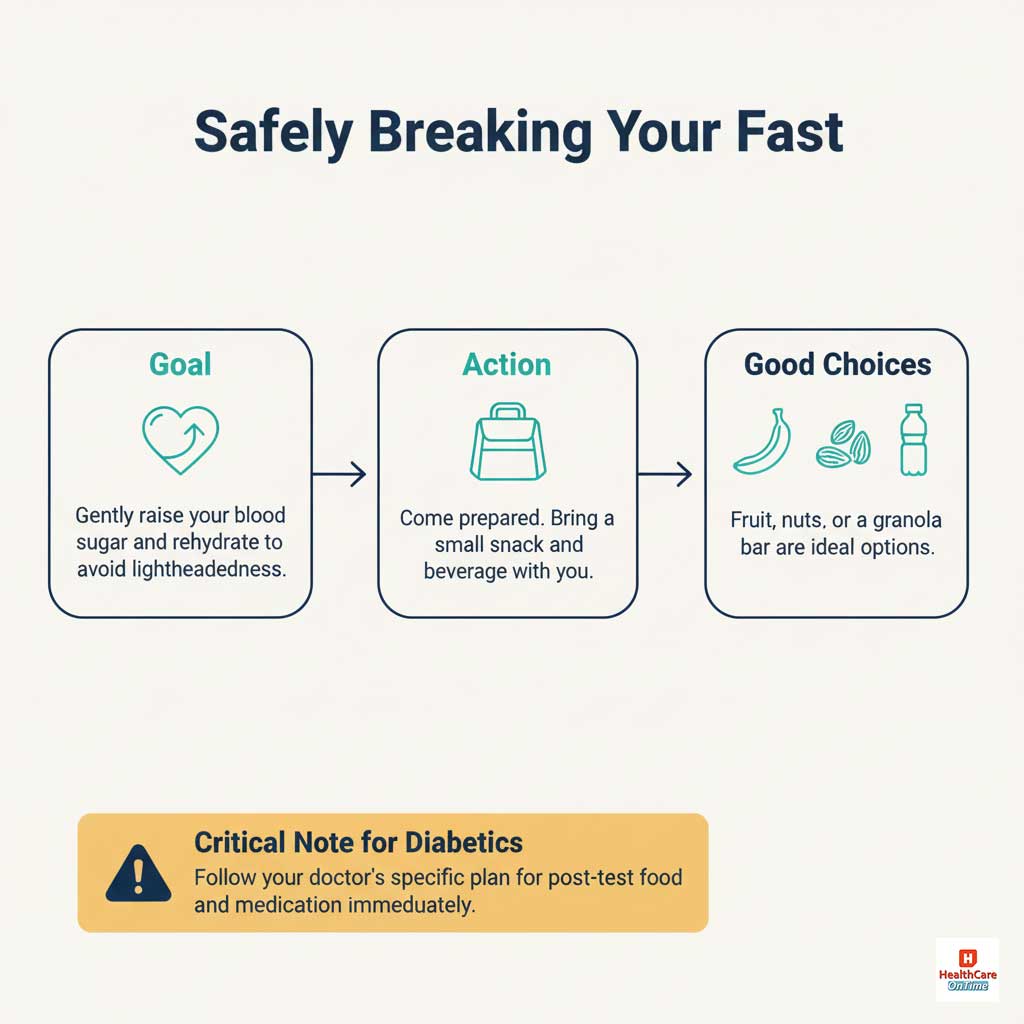
- The Immediate Goal: Gently raise your blood sugar and rehydrate your body.
- What to Have Ready: It is highly recommended to bring a small, prepared snack and a beverage with you to your appointment.
- Good Choices: A piece of fruit (like a banana or an apple), a handful of nuts, a simple granola bar, or some crackers are all excellent options. Pair it with a bottle of water or juice.
- A Critical Note for Diabetics: It is absolutely essential to follow your doctor’s specific instructions. This typically involves testing your blood sugar immediately after the draw and consuming your planned snack and medication to prevent a dangerous hypoglycemic (low blood sugar) event.
By following this expert protocol, you are ensuring the dialogue with your body is crystal clear and providing your healthcare team with the most accurate, reliable data possible. Preparing for a blood test doesn’t have to be a source of anxiety. With this knowledge, you are in complete control, ensuring the conversation with your body is as clear and accurate as possible.
Frequently Asked Questions (FAQs)
Do I really need to fast for a full 12 hours, or is 8 hours enough?

While 8 hours is the minimum threshold, fasting closer to the 12-hour mark is considered the gold standard. This provides the maximal clearance time for triglycerides from your last meal, ensuring the truest possible baseline for your lipid panel.
Let’s be unequivocally clear: can I have black decaf coffee?

No. While decaf removes most of the caffeine, it still contains other compounds that can stimulate the gut and potentially have minor metabolic effects. For a test of this importance, the clinical consensus is firm: to eliminate every variable, stick to plain water only.
I had one glass of wine with dinner before I remembered my test. What should I do?

The most responsible action is to call the lab or your doctor’s office before you go. A single drink can still noticeably elevate triglycerides and GGT. It is better to reschedule and get an accurate result than to proceed with a potentially flawed one.
I take a daily low-dose aspirin and a multivitamin. Should I stop them?

You should never stop a prescribed medication like aspirin without your doctor’s consent. For a general multivitamin, it is wise to skip it on the morning of your test to be safe, especially to avoid any low-dose biotin it may contain.
If I accidentally break my fast with a piece of toast, is the whole test ruined?

Yes, for the fasting-dependent components, the results will be invalid. You must inform the phlebotomist. They will likely not draw the blood for fasting tests and will advise you to reschedule. Proceeding without disclosing this information will lead to inaccurate results.
Does being sick with a cold or flu affect blood test results?

Yes, significantly. An acute illness triggers a powerful inflammatory response in your body, which can elevate your white blood cell count, inflammatory markers like C-Reactive Protein (CRP), and can affect other biomarkers. If it’s a routine test, it’s often best to reschedule until you have fully recovered.
Why is chewing gum, even sugar-free, not allowed?

The act of chewing initiates the first phase of digestion (the “cephalic phase”). It signals your stomach to produce acid and your pancreas to potentially release small amounts of insulin, which disrupts your true fasting baseline.
My doctor ordered a “non-fasting” lipid panel. Does that mean I can eat a bacon cheeseburger right before?

While you are not required to fast, the goal is still to get a representative look at your health. A “non-fasting” test is meant to reflect your body’s state after a typical meal. Eating an unusually large or high-fat meal can still cause an extreme triglyceride spike that may not be representative of your normal diet, potentially triggering an unnecessary follow-up fasting test. It is best to eat your normal, average diet on the day of a non-fasting test.









