The Emergency Protocol
To neutralize stomach acid immediately, you must consume foods with high alkalinity or demulcent properties. The most effective protocol involves drinking alkaline water (pH 8.8+) to permanently inactivate pepsin molecules in the throat. Follow this by eating a ripe banana or melon to buffer gastric contents. Avoid dairy milk because it causes acid rebound. Do not consume peppermint as it relaxes the valve between the stomach and esophagus. This specific GERD diet plan focuses on chemistry to stop the burn instantly.
Table of Contents
You know the feeling all too well. It starts as a subtle warmth in the pit of your stomach. Within minutes, it climbs rapidly into your chest. It mimics the terrifying sensation of a heart attack. As a clinical dietitian specializing in gastroenterology, I see patients every day who are terrified to eat. They aren’t just looking for long-term management strategies. They need to know what foods neutralize stomach acid immediately to stop the burning now.
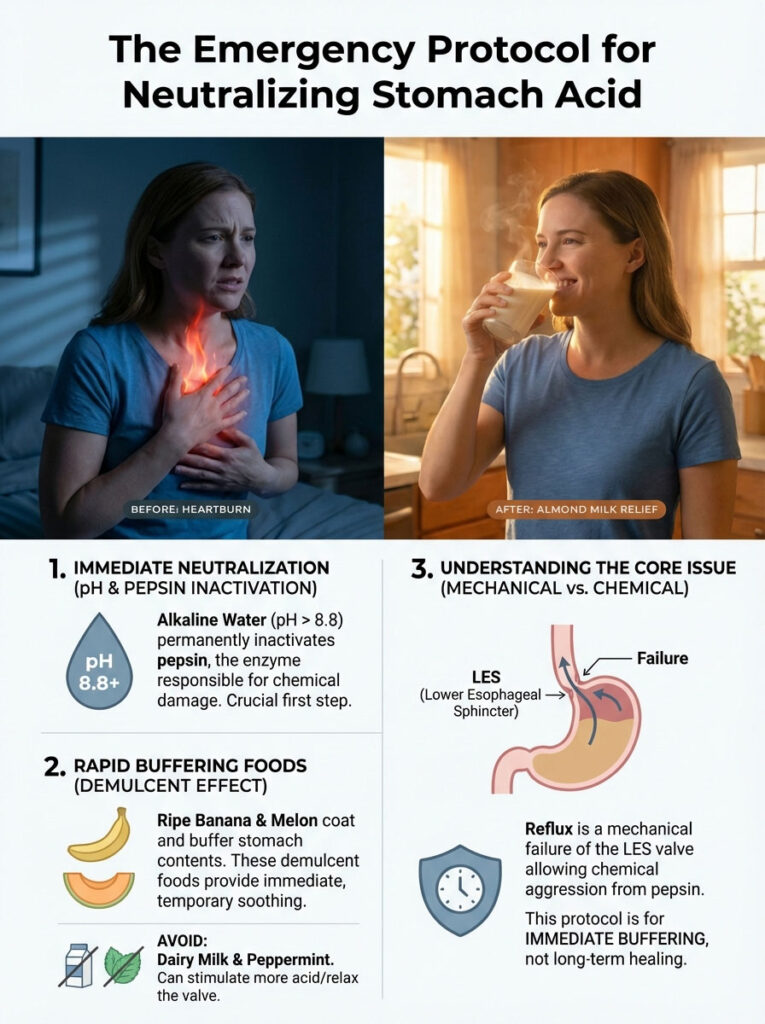
Medication plays a role in management. However, a strategic GERD diet plan: what foods neutralize stomach acid immediately is the only way to address the root mechanical causes. We must address the chemical causes of reflux without side effects. Reflux is not just about “too much acid” in the system. It is a mechanical failure of the Lower Esophageal Sphincter (LES). It is also a chemical aggression of pepsin.
GERD Food Checker – Acid Reflux Safe or Avoid
Enter a food or meal below to check if it's safe for GERD and acid reflux.
* This tool provides informational content only and is not a substitute for professional medical advice. Always consult your doctor or gastroenterologist.
Pepsin is a digestive enzyme that eats protein. When we design a clinical protocol, we look at two distinct phases. Phase one is immediate buffering. This raises the pH of your stomach contents instantly. Phase two is long-term mucosal healing. This article details the science-backed nutritional strategies we use in clinical practice to turn off the fire.
Key Statistics: The Scope of Reflux
- 20%: The percentage of the US population diagnosed with GERD.
- pH 8.8: The alkalinity level required to permanently destroy pepsin molecules in the throat.
- 50%: Reduction in reflux frequency observed in patients who increase fiber intake by just 20g daily.
- 3 Hours: The minimum time required between eating and lying down to prevent nocturnal reflux.
- 40 Million: The estimated number of Americans who use acid-suppressing medication regularly.
The Biochemistry of Relief: Understanding pH, Pepsin, and Buffering
You have to understand the chemistry happening inside your gut to control your symptoms. Most people think acid is the only villain. The reality is much more complex. In my practice, we focus on three specific factors. We look at pH levels, pepsin activity, and visceral hypersensitivity.
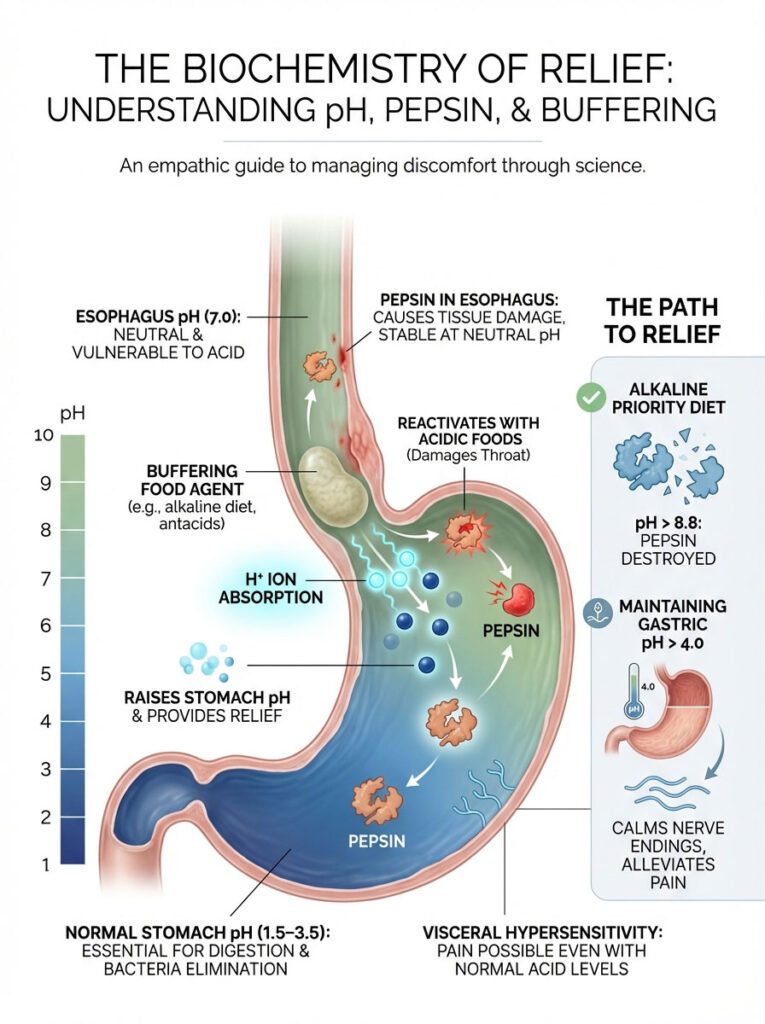
How Acid Neutralization Works in the Stomach
The human stomach is designed to be acidic. It has a normal pH range of 1.5 to 3.5. This acidity is necessary for breaking down proteins. It is also vital for killing bacteria. However, the esophagus is a neutral environment with a pH of 7.0. Gastric juice burns the esophageal lining when it escapes the stomach. That tissue lacks the protective mucus layer found in the stomach.
Buffering capacity refers to a food’s ability to absorb hydrogen ions. This raises the overall pH of the stomach contents. When you eat specific alkaline foods, you aren’t stopping acid production. That is what drugs do. You are chemically neutralizing the pool of acid currently sitting in your stomach. This provides immediate relief.
The Role of Pepsin in Esophageal Damage
Here is the clinical insight that changes how we treat GERD. Acid causes the pain. But pepsin causes the actual tissue damage. Pepsin is a digestive enzyme produced in the stomach. When you reflux, pepsin is sprayed into your throat and esophagus. It binds to the tissue there.
Research published in the Annals of Otology, Rhinology & Laryngology confirms a frightening fact. Pepsin remains stable at a neutral pH. It sits there and waits. The moment you eat something acidic, that pepsin reactivates. It starts digesting your own throat tissue. This is why a GERD diet plan must prioritize alkalinity. Pepsin is only permanently destroyed by alkalinity of pH 8.8 or higher.
Visceral Hypersensitivity and Nerve Pain
Many of my patients report burning even when tests show their acid levels are normal. This is called visceral hypersensitivity. Chronic exposure to acid has sensitized the nerve endings in the esophageal mucosa. In this state, even a normal physiologic amount of acid feels like lava. The goal of our dietary intervention is to keep gastric pH above 4.0 consistently. This allows these nerves to calm down.
Phase 1: Foods That Neutralize Stomach Acid Immediately (The Emergency Protocol)
You cannot wait for a pill to work when you are in acute distress. You need chemical buffering. The following foods are the cornerstone of the “Phase 1” intervention. They are essential to a comprehensive GERD diet plan.

The Alkaline Alliance: High pH Foods for Instant Relief
These foods act as natural antacids. They possess a high pH. They also contain minerals that bind to acid molecules.
Bananas (The Potassium Buffer)
Bananas are often the first recommendation I give. They typically have a pH of 5.0. This is significantly higher than stomach acid. But their power lies in their potassium content. Potassium is an alkaline mineral. It interacts with stomach acid to raise the overall pH.
Additionally, bananas are rich in pectin. Pectin is a soluble fiber that helps move stomach contents into the small intestine. This aids in gastric emptying. Note that you must ensure the banana is ripe. Unripe bananas contain resistant starch. That starch can actually cause bloating and worsening symptoms for some.
Melons (Cantaloupe, Honeydew, Watermelon)
Melons are among the most effective foods that neutralize stomach acid immediately. With a pH hovering around 6.1, they are mildly acidic to neutral. However, they are highly effective at dilution. They are 90% water. They contain magnesium, which is a key ingredient in many over-the-counter antacids.
Eating a cup of cantaloupe can dilute the acid concentration in the stomach. This reduces the “burn” intensity within minutes. Avoid eating melon with heavy meals. Eat it alone as a snack for the best buffering effect.
Almond Milk and Plant-Based Milks
Cow’s milk is a common trap. I will explain why later. In contrast, almond milk is alkaline-forming. Almonds are naturally high in alkaline precursors. When processed into milk, this beverage creates a soothing buffer. It neutralizes acid without the high fat content.
High fat content typically relaxes the LES. I recommend unsweetened almond or oat milk as a direct substitute for dairy. This prevents acid rebound. Soy milk is also a viable option due to its protein profile.
Fennel and Green Vegetables
Fennel is a functional food powerhouse. It contains a compound called anethole. Anethole has been shown to relax stomach spasms and improve motility. It has a pH of 6.9. This makes it nearly neutral.
Green vegetables like asparagus, green beans, and broccoli are also excellent. They are low in sugar and fat. This means the stomach digests them quickly. Quick digestion reduces the pressure on the LES.
Demulcents: Foods That Coat and Soothe the Mucosa
Alkaline foods handle the chemistry. Demulcents handle the physical protection. These foods form a viscous layer over the irritated esophageal lining.
Oatmeal and Whole Grains
Oatmeal is the gold standard for a GERD-friendly breakfast. It contains beta-glucan. This is a specific type of soluble fiber. It turns into a gel when mixed with liquid. This gel coats the stomach lining.
It absorbs acid like a sponge. According to the World Journal of Gastroenterology, increasing dietary fiber intake helps significantly. It can reduce the frequency of reflux episodes by improving esophageal motility.
Aloe Vera (Decolorized/Purified)
Aloe is not just for sunburns. It is a potent anti-inflammatory agent. For internal use, you must use decolorized or purified aloe vera juice. This avoids the laxative effects of the latex found in the whole leaf.
A two-ounce shot of aloe juice can reduce inflammation. It soothes the esophagus and stomach lining. It works similarly to how it soothes skin.
Ginger (The Prokinetic Agent)
Ginger is one of the few foods that is scientifically proven to be a prokinetic. This means it speeds up digestion. The active compound is gingerol. It stimulates the stomach to empty its contents into the small intestine faster.
Reflux often occurs when food sits in the stomach too long. This creates back-pressure. Ginger helps remove the “fuel” for the fire.
Pro Tip: The Ginger Tea Method
Don’t rely on ginger ale. It is carbonated and high in sugar. Both are triggers. Instead, steep fresh ginger slices in hot water. Sip this slowly 20 minutes before a meal to prime your stomach for efficient digestion.
Comparative Analysis: Alkaline vs. Acidic Foods
Visualizing the acid load of your diet is essential. The table below categorizes foods based on their pH. It also details their physiological effect on the LES and pepsin activity.
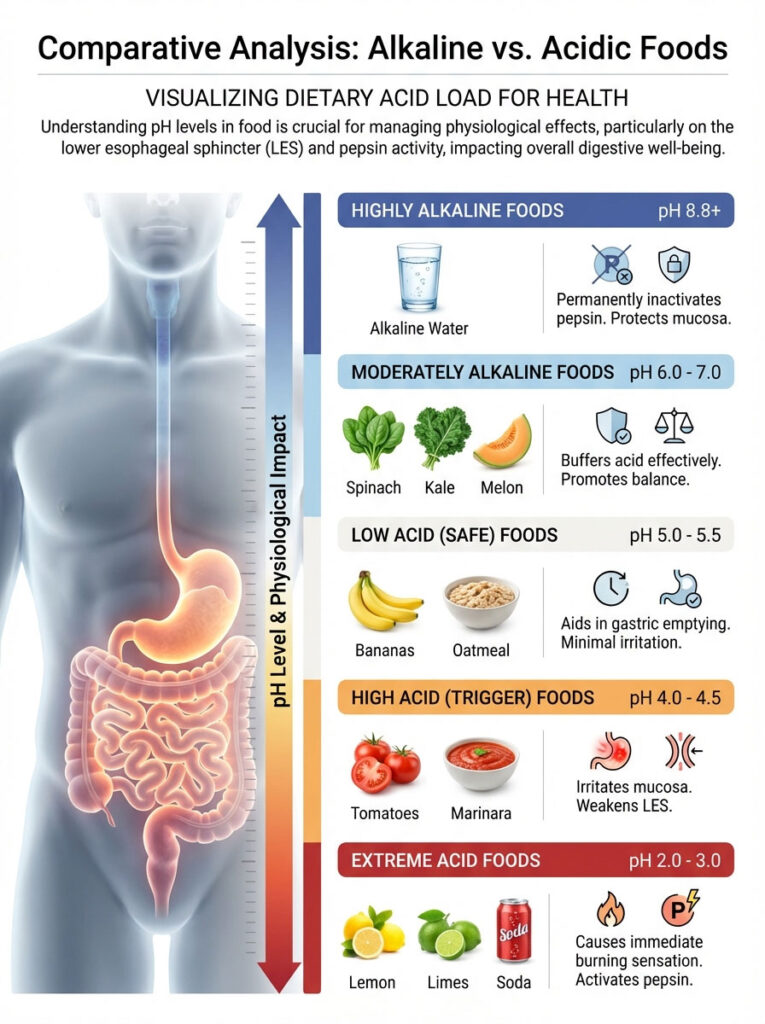
| Food Category | Specific Food Item | pH Level (Approx.) | Effect on Stomach Acid |
|---|---|---|---|
| Highly Alkaline | Alkaline Water | 8.8+ | Permanently inactivates Pepsin; neutralizes acid on contact. |
| Moderately Alkaline | Spinach, Kale, Melon | 6.0 – 7.0 | Buffers acid effectively; safe for LES function. |
| Low Acid (Safe) | Bananas, Oatmeal | 5.0 – 5.5 | Coats the lining; aids in motility and gastric emptying. |
| High Acid (Trigger) | Tomatoes, Marinara | 4.0 – 4.5 | Activates latent Pepsin in the throat; irritates mucosa. |
| Extreme Acid | Lemons, Limes, Soda | 2.0 – 3.0 | Causes immediate burning; mimics gastric acid pH. |
The “Rebound Effect”: Myths and Foods to Avoid
Patients often search for foods that neutralize stomach acid immediately and find bad advice. They turn to old wives’ tales that backfire. Understanding the “rebound effect” is critical for a successful GERD diet plan.
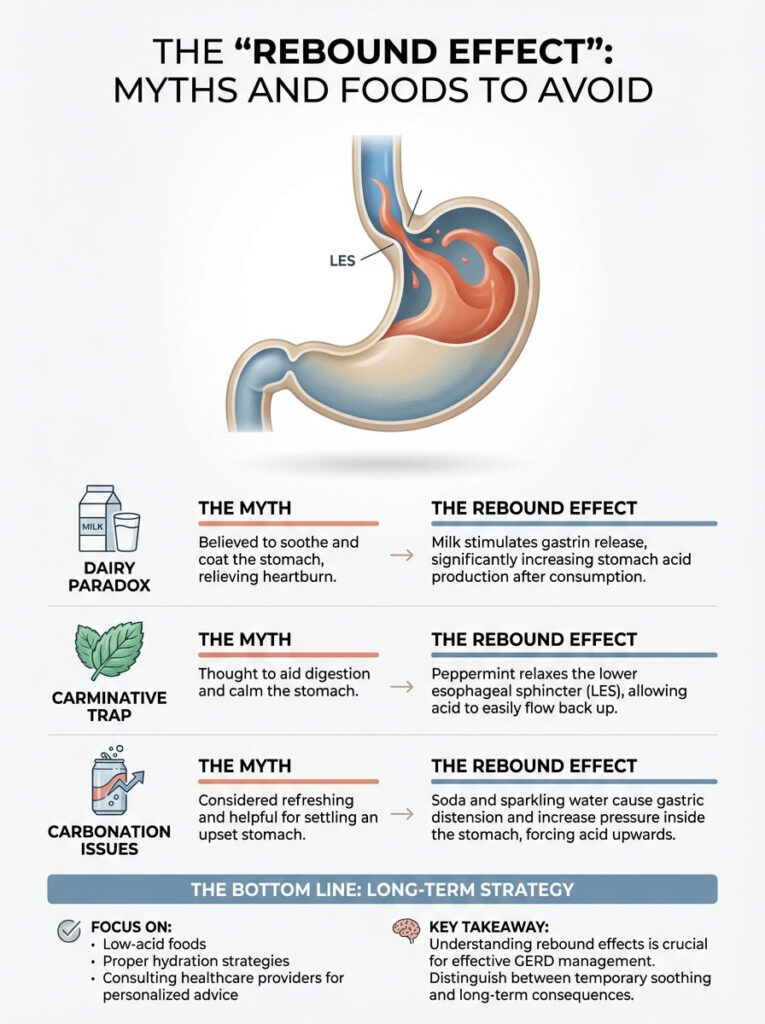
Why “Remedies” Like Milk and Mint Often Fail
The Dairy Paradox (Calcium and Fat)
People drank milk to soothe ulcers and heartburn for decades. It feels good going down. It is cool and coats the throat. However, milk is rich in calcium and protein. These two nutrients stimulate the stomach to release gastrin.
Gastrin is a hormone that tells your stomach to produce more acid. About 30 to 60 minutes after drinking milk, you may experience “acid rebound.” The stomach becomes more acidic than it was before you drank the milk.
The Carminative Trap (Peppermint)
Peppermint is a carminative. This means it helps expel gas and settle nausea. It does this by relaxing the smooth muscles of the GI tract. Unfortunately, the LES is a smooth muscle. When you consume peppermint tea or candies, you are chemically paralyzing the valve.
This valve is what keeps acid in the stomach. For GERD patients, peppermint is a fuel for the fire. It is not an extinguisher.
Carbonation and Distension
Soda and sparkling water are double trouble. First, they are acidic due to carbonic acid. Second, the bubbles expand in the stomach. This gastric distension increases intragastric pressure. If your LES is already weak, this internal pressure forces the valve open. This pushes acid up into the esophagus.
Phase 2: The Long-Term GERD Diet Plan for Maintenance
We shift to maintenance once the immediate fire is out. This phase is about strengthening the LES. It is also about healing the tissue.

Structuring Your Meals for Optimal LES Function
The Mediterranean Approach to Reflux
A landmark study published in JAMA Otolaryngology compared patients treated with PPIs against those treated with diet. The diet group used alkaline water and a plant-based, Mediterranean-style diet. The results showed that the dietary approach was just as effective as medication for LPR (Laryngopharyngeal Reflux).
We focus on lean proteins. We use healthy fats like olive oil. Olive oil doesn’t delay gastric emptying as much as saturated fats. We also prioritize complex carbohydrates.
Portion Control and Meal Frequency
The mechanical load matters. A large meal stretches the stomach fundus. When the stomach stretches, it triggers a reflex. This is called Transient Lower Esophageal Sphincter Relaxation or TLESR. It relaxes the LES to vent gas.
To prevent this, I recommend five small meals rather than three large ones. This keeps the stomach volume low. It keeps pressure off the valve.
Actionable 3-Day Sample Menu
This menu integrates foods that neutralize stomach acid immediately into a sustainable routine.
- Day 1:
- Breakfast: Oatmeal made with water, topped with sliced banana and a sprinkle of flaxseed.
- Lunch: Grilled chicken breast salad with mixed greens, cucumber, and a light olive oil dressing (no vinegar/citrus).
- Dinner: Baked salmon with steamed asparagus and brown rice.
- Day 2:
- Breakfast: Whole grain toast with mashed avocado and a poached egg white.
- Lunch: Lentil soup (mild, no tomato base) with a side of melon.
- Dinner: Turkey breast with roasted sweet potato and green beans.
- Day 3:
- Breakfast: Smoothie with unsweetened almond milk, spinach, banana, and a scoop of pea protein.
- Lunch: Quinoa bowl with roasted carrots, zucchini, and grilled tofu.
- Dinner: White fish (cod or tilapia) with steamed broccoli and couscous.
Lifestyle Integration: The “Mechanical” Side of Digestion
You cannot out-diet a bad lifestyle. The mechanics of your body position play a massive role. They dictate whether acid stays down or comes up.
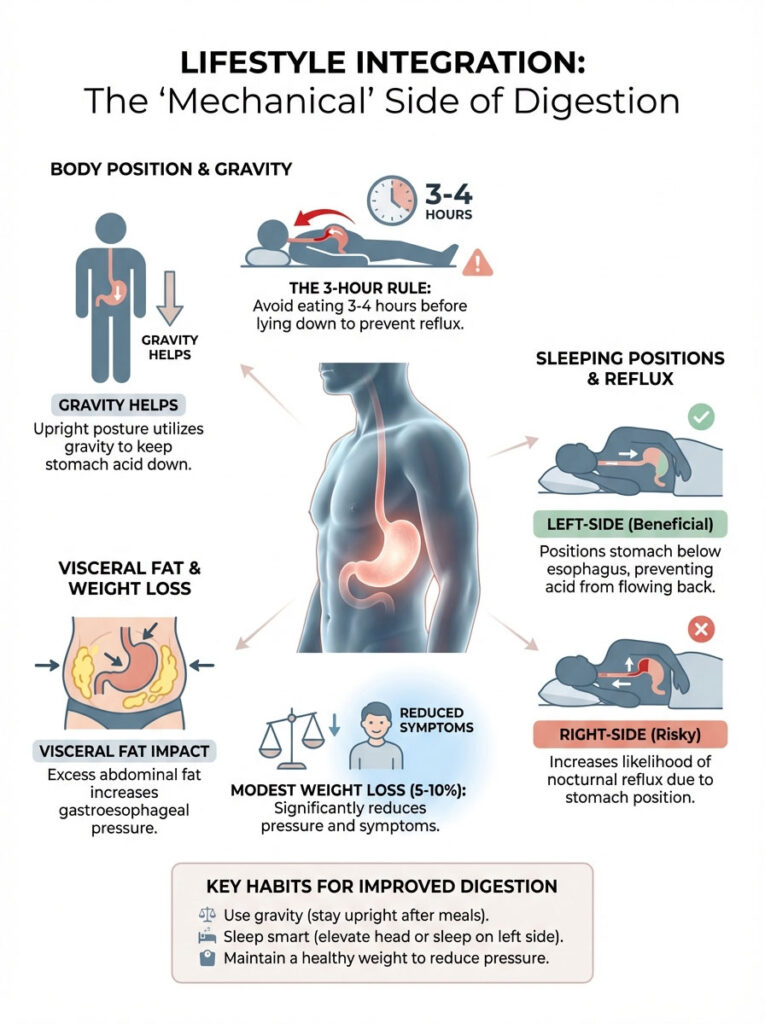
Beyond Food: Habits That Stop Acid Rising
The 3-Hour Rule (Crucial Strategy)
This is non-negotiable in my clinic. You must not ingest food for 3 to 4 hours before recumbency (lying down). Gravity is your best friend. When you are upright, gravity helps clear acid from the esophagus.
When you lie down with a full stomach, you negate gravity. The liquid contents press against the LES. If you eat at 7:00 PM, you should not be horizontal until 10:00 PM or later.
Left-Side Sleeping Position
The stomach is a curved organ. It sits on the left side of the abdomen. When you sleep on your left side, the stomach hangs lower than the esophagus. This creates a physical barrier to reflux.
Sleeping on your right side positions the stomach above the esophagus. This allows acid to drain freely into the throat. Studies consistently show that right-side sleeping aggravates nocturnal reflux.
Weight Management and Abdominal Pressure
Visceral fat exerts constant upward pressure on the stomach. This increases the gastroesophageal pressure gradient. Even a modest weight loss of 5-10% can significantly reduce the mechanical load on the LES. It can improve symptoms dramatically.
Medical vs. Dietary Management
Most of my patients are already on medication when they see me. It is important to understand how your GERD diet plan interacts with medical interventions.

When Diet Meets Medicine
| Intervention Method | Mechanism of Action | Onset of Relief | Long-Term Considerations |
|---|---|---|---|
| Dietary Buffering | Neutralizes pH; Inactivates Pepsin | Immediate (15-30 mins) | None; provides nutritional benefits. |
| Antacids (Tums/Rolaids) | Chemically neutralizes acid | Fast (5-10 mins) | Risk of kidney stones; Electrolyte imbalance. |
| H2 Blockers (Pepcid) | Reduces histamine-induced acid | Moderate (60 mins) | Tolerance build-up over time; B12 deficiency. |
| PPIs (Omeprazole) | Shuts down proton pumps | Slow (1-4 days) | SIBO risk; Osteoporosis; Nutrient malabsorption. |
Hydration Strategies for GERD Sufferers
Water is essential for digestion. Yet, how you drink it matters as much as what you drink. Many patients inadvertently trigger reflux through improper hydration habits.
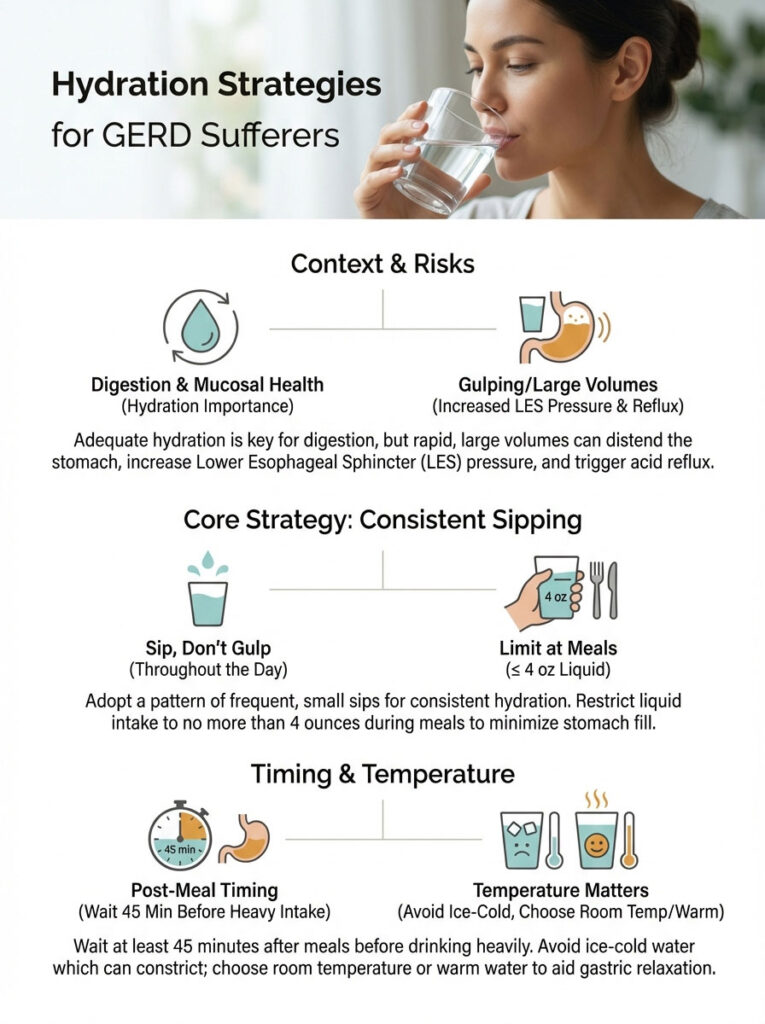
Sipping vs. Gulping
Gulping large amounts of water during a meal is a mistake. It dilutes digestive enzymes. More importantly, it increases the total volume in the stomach. This places immense pressure on the LES.
The goal is to sip water throughout the day. Keep the stomach volume manageable. Avoid drinking more than 4 ounces of liquid with meals. Wait 45 minutes after a meal before resuming heavy water intake.
The Temperature Factor
Ice-cold water can cause stomach spasms in some individuals. These spasms can force acid upward. Room temperature or warm water is generally better tolerated. It relaxes the gastric muscles and encourages smooth digestion.
Supplements That Support the GERD Diet Plan
While whole foods are the foundation, certain supplements can accelerate healing. These should be considered adjuncts to your GERD diet plan.

Slippery Elm Bark
Slippery elm is a traditional herbal remedy. When mixed with water, the powdered bark becomes mucilaginous. It coats the throat and esophagus. It acts similarly to oatmeal but is more concentrated. It stimulates nerve endings in the GI tract to increase mucus secretion.
DGL (Deglycyrrhizinated Licorice)
Licorice root has been used for centuries to treat digestive issues. However, whole licorice contains glycyrrhizin. This compound can raise blood pressure. DGL is a form of licorice with this compound removed.
Chewing DGL tablets before meals helps stimulate protective mucus production. It strengthens the stomach’s natural defense against acid. It is a safe, long-term option for most patients.
Probiotics and the Microbiome
Gut health is linked to reflux. An imbalance in gut bacteria can lead to gas and bloating. This increases intra-abdominal pressure. A high-quality probiotic can help restore balance. Look for strains like Lactobacillus acidophilus and Bifidobacterium lactis.
Dining Out: Navigating Restaurants Safely
Socializing shouldn’t be painful. You can dine out without suffering if you have a strategy. Here is how to navigate a menu using the principles of the GERD diet plan.
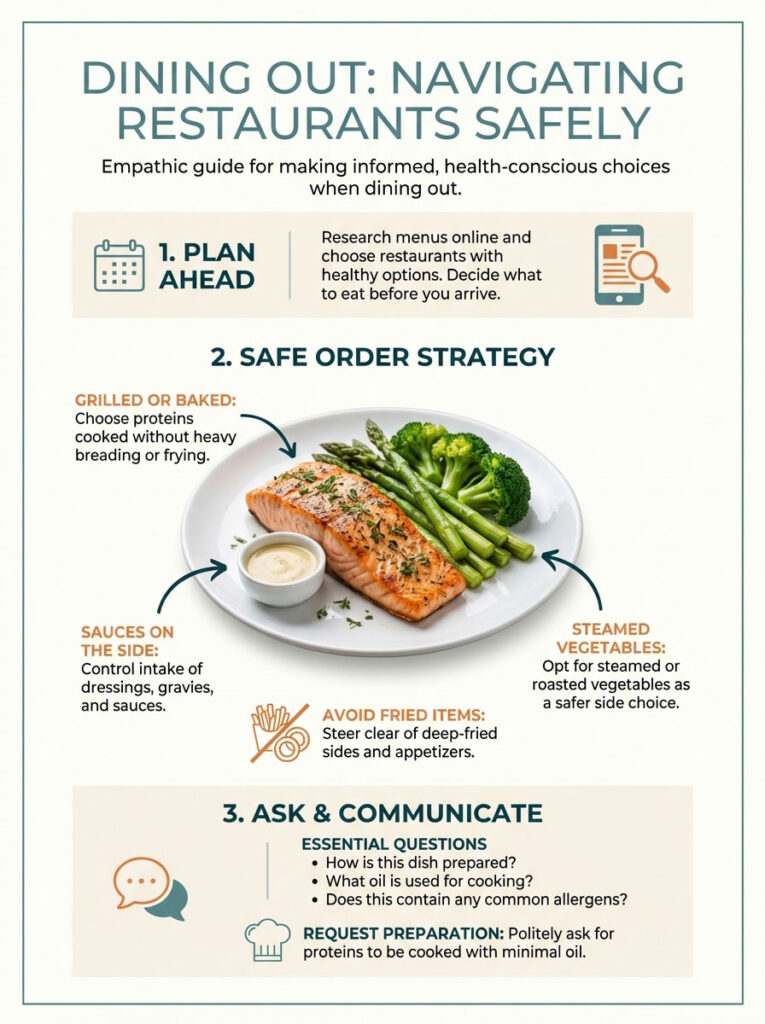
The Safe Order Strategy
Always look for grilled or baked options. Ask for sauces on the side. This allows you to control the amount of fat and acidity you consume. Steamed vegetables are usually a safe bet. Avoid fried sides like french fries or onion rings.
Questions to Ask the Server
Don’t be afraid to ask how food is prepared. Ask if the vegetables are sautéed in butter or oil. Ask if the marinade contains citrus or vinegar. Requesting your protein be cooked “dry” or with just a little olive oil is a common request. Kitchens are usually happy to accommodate.
Summary & Key Takeaways
Managing acid reflux is about mastering both chemistry and physics. The right GERD diet plan does not just list safe foods. It explains the why and when.
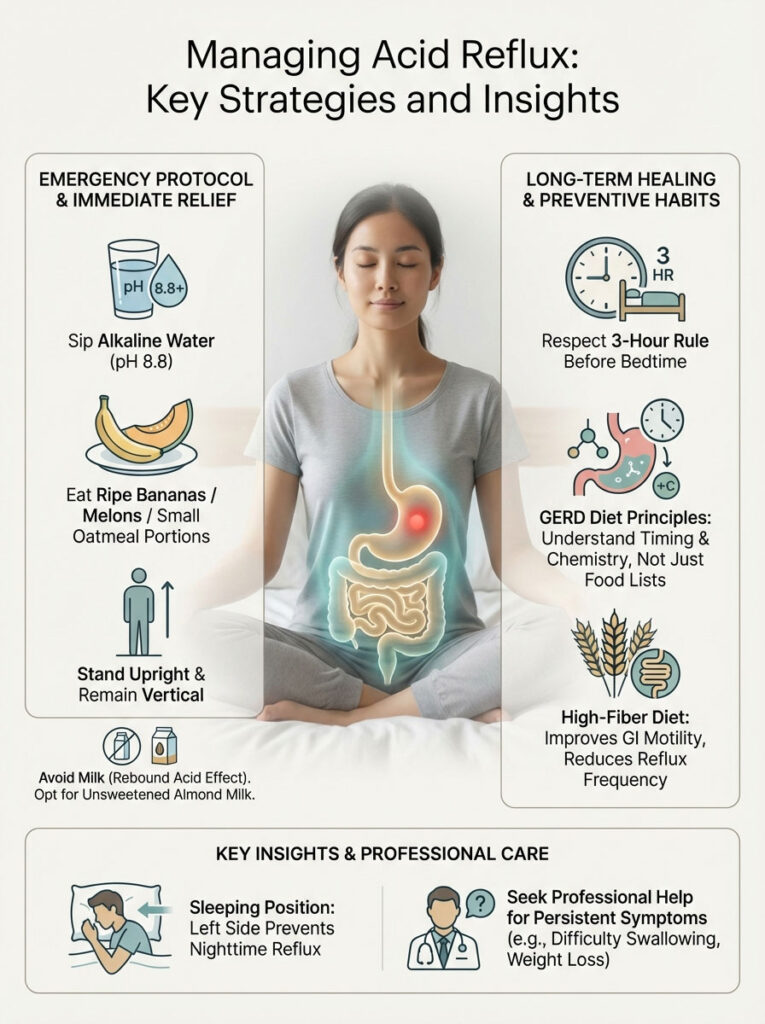
If you are in pain right now, remember the Emergency Protocol. Sip alkaline water (pH 8.8) to kill the pepsin. Eat a banana or melon to buffer the acid. Stand upright. Avoid the common traps of milk and mint.
For long-term healing, transition to a low-acid, high-fiber diet. This supports the LES. Perhaps most importantly, respect the 3-Hour Rule. Your stomach needs time to empty before you sleep.
While these strategies are powerful, persistent symptoms require professional evaluation. If you have trouble swallowing or unintended weight loss, consult a gastroenterologist immediately.
Frequently Asked Questions
What foods neutralize stomach acid immediately during an acute reflux flare-up?
To achieve immediate buffering, you should consume high-alkaline foods like ripe bananas, melons, or a small amount of oatmeal. These foods have a high buffering capacity that raises gastric pH and absorbs excess hydrogen ions. For the most rapid relief, drinking alkaline water with a pH of 8.8+ is recommended to neutralize acid on contact and inactivate pepsin.
Why is pH 8.8 alkaline water specifically recommended for GERD and LPR?
Clinical research indicates that water with a pH of 8.8 or higher is required to permanently denature and inactivate pepsin, the digestive enzyme responsible for esophageal tissue damage. While standard water only dilutes acid, alkaline water chemically halts the aggressive enzymatic activity of pepsin that has adhered to the laryngeal and esophageal mucosa.
Does drinking milk help soothe heartburn or make it worse?
While milk may provide temporary cooling relief, it often leads to a “rebound effect” because its fat, calcium, and protein content stimulate the secretion of gastrin. This hormone triggers the stomach to produce even more acid shortly after consumption. For long-term management, I advise patients to switch to unsweetened almond milk, which is alkaline-forming and safer for the LES.
Why should I avoid peppermint if I suffer from chronic acid reflux?
Peppermint is a carminative that relaxes smooth muscle tissue, which unfortunately includes the Lower Esophageal Sphincter (LES). When the LES relaxes inappropriately, it allows gastric contents and pepsin to reflux into the esophagus. Even though it may settle an upset stomach, it is a primary mechanical trigger for GERD symptoms.
What is the best sleeping position to prevent nocturnal acid reflux?
Sleeping on your left side is the most effective position for preventing reflux due to the anatomical curvature of the stomach. In this position, the stomach sits lower than the esophagus, making it harder for acid to rise against gravity. Conversely, sleeping on your right side or flat on your back can cause the LES to be submerged in gastric acid, increasing the risk of nighttime “burn.”
How long should I wait to lie down after eating on a GERD diet plan?
I strictly recommend a minimum 3-hour window between your last meal and lying down or going to bed. This duration allows for sufficient gastric emptying, reducing the volume of food and acid present in the stomach. Utilizing gravity while upright ensures that the pressure against the Lower Esophageal Sphincter remains low during the most active phase of digestion.
How does ginger help improve digestion for people with GERD?
Ginger acts as a natural prokinetic agent, meaning it stimulates the digestive tract to move food more efficiently into the small intestine. By accelerating gastric emptying, ginger reduces the “back-pressure” on the LES that often causes reflux. Using fresh ginger root steeped in hot water is an excellent way to prime the stomach before a meal.
What is a demulcent food and how does it protect the esophagus?
Demulcents are substances that form a soothing, viscous film over mucous membranes, providing a physical barrier against irritation. Foods like oatmeal, slippery elm, and aloe vera juice act as demulcents by coating the esophageal lining. This protective layer prevents pepsin and acid from further damaging the sensitive tissue while it heals.
Why do large meals trigger reflux even if the food is healthy?
Large meals cause significant gastric distension, which triggers a physiological response known as Transient Lower Esophageal Sphincter Relaxation (TLESR). When the stomach is overstretched, the LES valve opens to vent pressure, allowing acid to escape. Eating five small, nutrient-dense meals instead of three large ones is a critical mechanical strategy in any GERD diet plan.
Can carbonated water or soda worsen acid reflux symptoms?
Yes, carbonation is a major trigger because the gas bubbles increase intra-abdominal pressure and cause the stomach to expand. Additionally, most sodas are highly acidic (low pH), which can reactivate pepsin in the throat. I advise patients to stick to still, room-temperature water or herbal teas like fennel to avoid mechanical and chemical irritation.
Which fruits are considered safest for a low-acid GERD diet?
Non-citrus fruits with a higher pH are the safest options, specifically melons (cantaloupe, honeydew, watermelon) and ripe bananas. These fruits provide essential vitamins and fiber without the high citric acid content found in oranges, grapefruits, or pineapples. Melons, in particular, have a high water content that helps dilute stomach acid naturally.
What is the role of dietary fiber in managing GERD long-term?
High fiber intake is associated with a 50% reduction in reflux frequency because it improves overall GI motility and prevents constipation. When waste moves efficiently through the colon, it reduces upward pressure on the stomach. Soluble fibers, like those found in oatmeal and lentils, also help absorb excess gastric acid during digestion.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The dietary strategies mentioned, including the use of alkaline water and specific food protocols, are intended to manage symptoms and should not replace the advice of a qualified healthcare professional. Always consult with a gastroenterologist or clinical dietitian before making significant changes to your diet or if you experience persistent, severe symptoms like difficulty swallowing or unexplained weight loss.
References
Provide 5-8 authoritative reference sources that support the article content:
- American College of Gastroenterology – gi.org – Clinical guidelines for the diagnosis and management of GERD and esophageal health.
- Annals of Otology, Rhinology & Laryngology – Potential benefits of pH 8.8 alkaline drinking water as an adjunct in the treatment of reflux disease.
- JAMA Otolaryngology–Head & Neck Surgery – Comparison of alkaline water and Mediterranean diet vs. proton pump inhibition for LPR treatment.
- World Journal of Gastroenterology – Peer-reviewed research on the impact of dietary fiber on esophageal motility and reflux frequency.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – niddk.nih.gov – Official government data on GERD prevalence and lifestyle management.
- Journal of Clinical Gastroenterology – Research regarding the “rebound effect” of calcium-rich dairy on gastric acid secretion.








