Recovering from a diverticulitis flare-up often leaves patients with a lingering sense of food fear. You might find yourself standing in the grocery aisle. Paralyzed by the thought that a single wrong ingredient could send you back to the emergency room. This anxiety is completely understandable. When you have spent days or weeks on a liquid diet to soothe an inflamed colon.
Table of Contents
The idea of eating roughage feels counterintuitive. However. The path to long-term health requires a complete mental shift. While a low-fiber diet is the correct treatment for an active infection. A diet rich in high fiber foods for diverticulitis is the only scientifically proven method to prevent that infection from coming back.
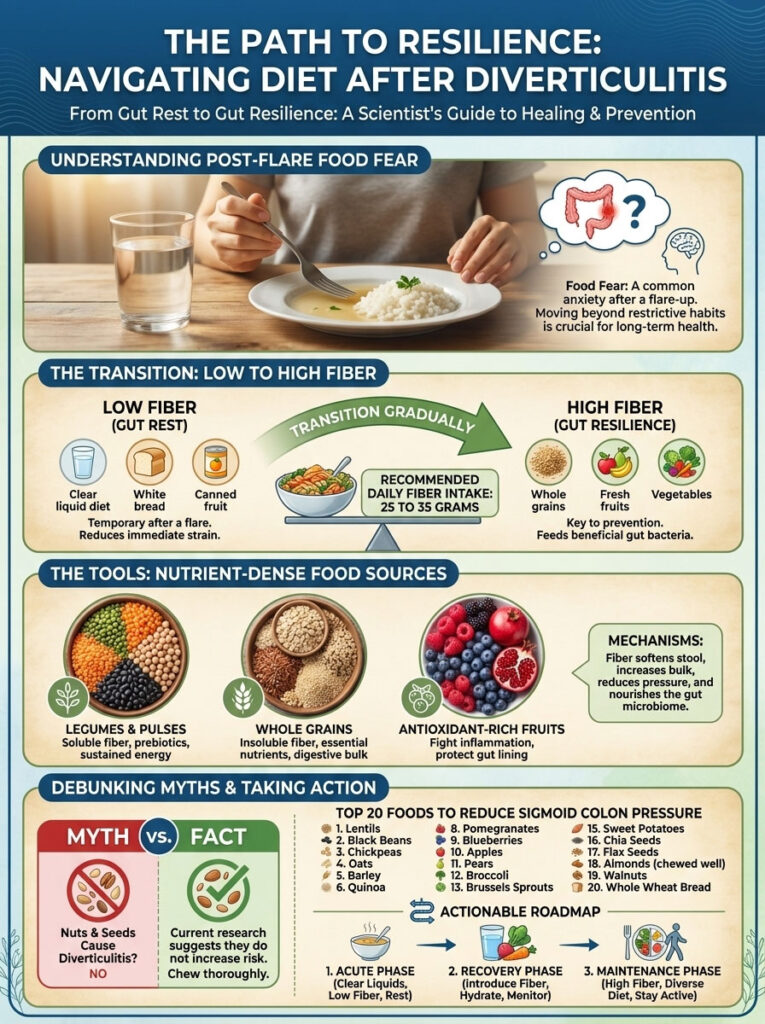
The best strategy for stopping future attacks involves a consistent. Daily intake of 25 to 35 grams of fiber. By focusing on nutrient-dense options like legumes. Whole grains. And antioxidant-rich fruits. You can mechanically strengthen the colonic wall. This guide will walk you through the top 20 foods that effectively reduce pressure in the sigmoid colon. We will be debunking outdated myths about nuts and seeds along the way. We will explore the specific mechanisms of the diverticulitis prevention diet and provide you with a safe. Actionable roadmap to transition from “gut rest” to “gut resilience.”
The Science of Prevention: How High Fiber Foods Reduce Intraluminal Pressure
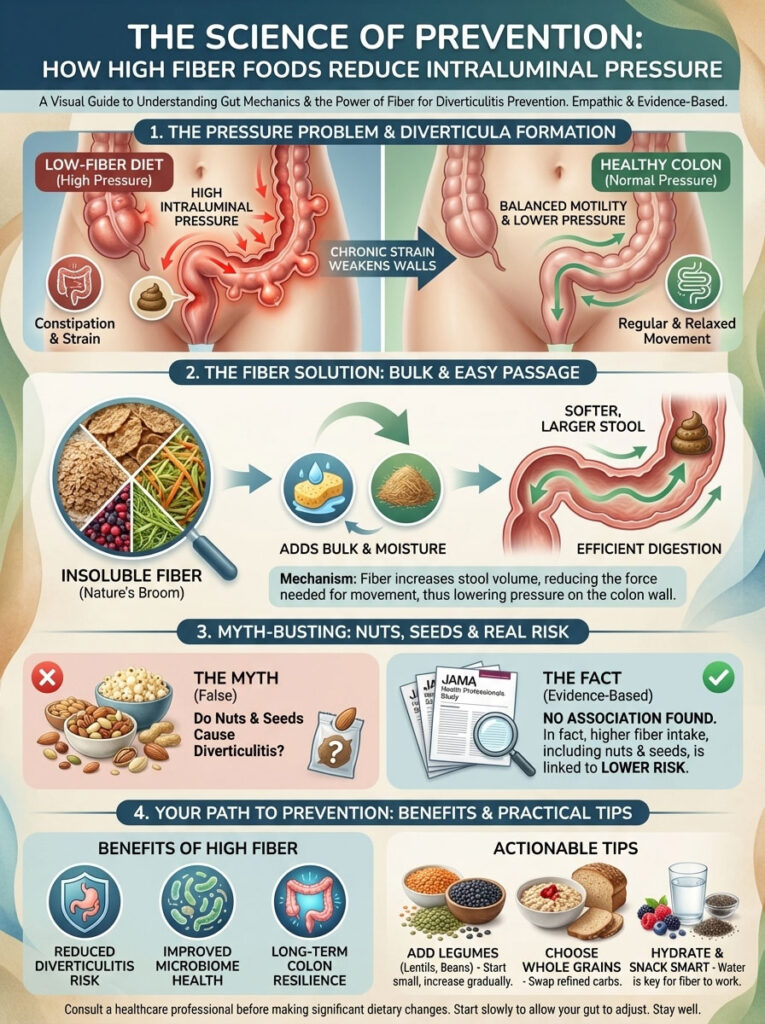
To commit to a diverticulitis prevention diet. You must first understand the mechanics of your own body. Diverticula do not form randomly. They are physical evidence of stress within the digestive tract. When the colon is forced to move small. Hard. And dry stools. It must generate immense force. This is known as high intraluminal pressure.
Understanding the Mechanics of the Sigmoid Colon and Diverticula Formation
Think of your colon like a bicycle tire. If you pump too much air into a weak tire. It might bulge outward. In the human body. When the muscles of the sigmoid colon contract violently to push constipation through. The inner lining of the intestine herniates through weak spots in the outer muscle layer. These herniations are the diverticula.
A diet lacking in foods high in fiber for diverticulosis leads to low stool volume. The colon walls essentially collapse inward. And the muscular contractions become segmented and intense. According to data from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Sustaining a high-fiber diet increases stool bulk. This bulk acts like a stent. Keeping the colon slightly expanded and allowing waste to move through via gentle. Rhythmic waves rather than violent spasms.
The Bulking Effect of Insoluble Fiber on Colonic Motility
This is where insoluble fiber becomes your greatest ally. Unlike soluble fiber. Which dissolves in water. Insoluble fiber remains intact as it passes through the digestive system. It acts as a “skeleton” for the stool. Absorbing water and swelling in size. This increased volume stimulates the stretch receptors in the gut lining. Signaling the body to move waste forward efficiently. By reducing the transit time of waste. High fiber foods for diverticulitis minimize the window of opportunity for bacteria to become trapped in a diverticulum and trigger an infection.
Debunking the Nut and Seed Myth with the JAMA Health Professionals Study
For decades. Doctors advised patients to avoid nuts. Corn. Popcorn. And seeds. The logic was that these small. Hard particles would physically lodge inside a pouch and cause inflammation. We now know this was a medical myth based on assumptions rather than evidence.
The Health Professionals Follow-up Study. Published in the Journal of the American Medical Association (JAMA). Provided the definitive correction to this belief. Researchers followed over 47,000 men for 18 years and found no correlation between the consumption of nuts. Corn. Or popcorn and the risk of diverticulitis. In a surprising twist. The data revealed that men who ate the most popcorn actually had a lower risk of developing the disease compared to those who avoided it. The protective benefit of the fiber in these foods far outweighed any theoretical risk of physical irritation.
The Transition Phase: Implementing the 5-Gram Rule to Avoid Bloating
Switching immediately from white rice and toast to a bowl of three-bean chili is a recipe for disaster. This sudden influx of carbohydrates is often what causes patients to abandon their diverticulitis prevention diet before it even begins.
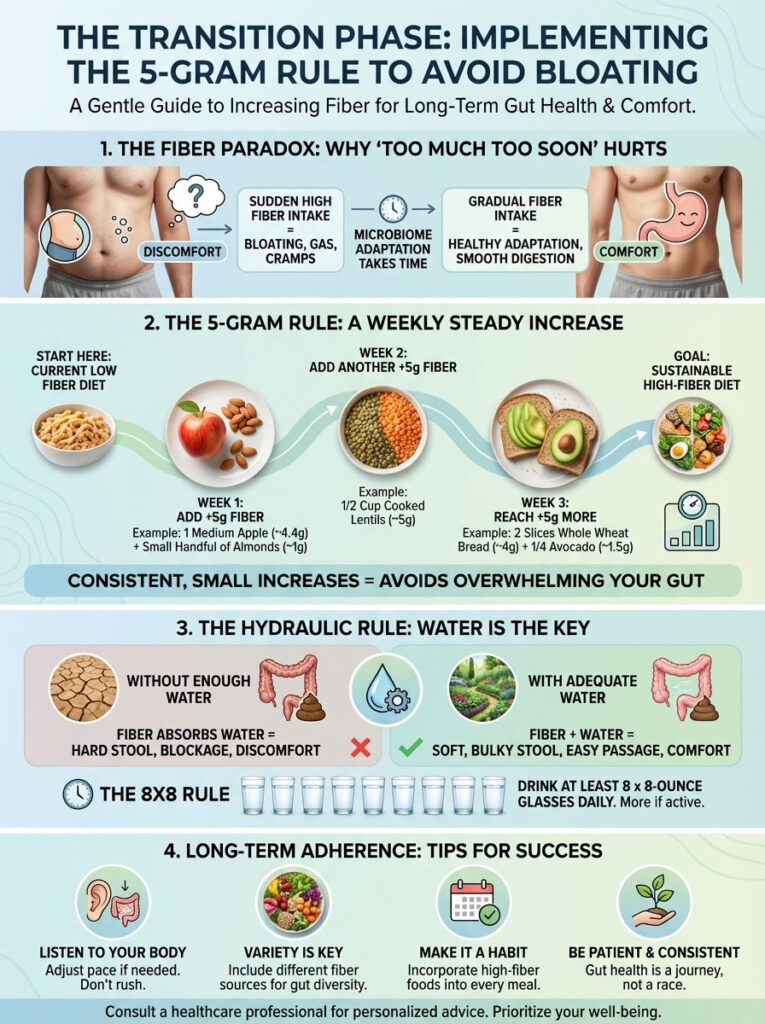
Navigating the Fiber Paradox and Microbiome Adaptation
The “Fiber Paradox” refers to the phenomenon where the very thing that heals you hurts you initially. Your gut microbiome is an ecosystem. If you have been eating low-fiber foods. The bacteria that digest fiber are low in numbers. When you suddenly introduce a massive amount of high fiber foods for diverticulitis. The existing bacteria become overwhelmed. They ferment the fiber rapidly. Producing excessive gas. Bloating. And abdominal distension.
This discomfort is not a sign that the diet is failing. It is a sign that your microbiome is waking up. The key is patience and a slow. Calculated increase in dosage.
The 5-Gram Rule for Safe Fiber Increases
To avoid the bloat. Follow the “5-Gram Rule.” Aim to increase your daily fiber intake by only 5 grams per week. This gradual ramp-up allows your bacterial colonies to multiply and adapt to the new fuel source.
- Week 1: Add 5g (e.g. one medium pear).
- Week 2: Add another 5g (e.g. switch to high-fiber cereal).
- Week 3: Add another 5g (e.g. add a serving of beans to dinner).
By the end of a month. You will be consuming an extra 20 grams of fiber daily with minimal side effects. This slow approach ensures you can sustain the daily fiber intake for diverticulitis required for long-term protection.
The Hydraulic Rule: Why Hydration is Critical for Diverticulitis Prevention
Fiber acts like a sponge. If you leave a dry sponge on the counter. It becomes hard and scratchy. If you soak it in water. It becomes soft and pliable. The fiber in your gut works the same way. Without adequate water. Fiber can harden and actually cause severe constipation.
For every 10 grams of fiber you add to your diet. You should add at least 8 to 10 ounces of water. A good baseline for diverticular disease diet management is the “8×8 rule.” Meaning eight 8-ounce glasses of water per day. But many high-fiber dieters need closer to 100 ounces daily to ensure everything moves smoothly.
Phase 1: High Fiber Legumes and Pulses for Diverticulitis Prevention
We have curated this list based on fiber density. Nutrient profile. And clinical efficacy. These are the heavy lifters of the diverticulitis prevention diet. Legumes are arguably the most important category for preventing attacks. They offer the highest fiber-to-volume ratio of any food group and are rich in protein. Which is vital for tissue repair.

1. Lentils: The Dense Source of Resistant Starch (15.5g per cup)
Lentils are the crown jewel of legumes and diverticulitis prevention. They are incredibly dense in both soluble and insoluble fiber. Because they are smaller than beans. They don’t require pre-soaking and cook quickly. The type of starch found in lentils is resistant starch. Which feeds the good bacteria in the colon. Producing short-chain fatty acids that heal the gut lining. A single cup provides over 50% of your daily needs. Making it the most efficient food for increasing stool bulk.
2. Black Beans: Anti-Inflammatory Anthocyanins (15g per cup)
Black beans are a powerhouse of nutrition. Beyond their massive fiber count. They are rich in anthocyanins. The antioxidants that give them their dark color. These compounds help reduce inflammation in the body. When incorporating black beans into a diverticular disease diet management plan. Rinse canned beans thoroughly to remove excess sodium and gas-producing oligosaccharides. Their soft texture makes them ideal for patients transitioning from a low-residue diet.
3. Chickpeas: Scrubbing the Colon Walls (12.5g per cup)
Chickpeas. Also known as garbanzo beans. Are versatile and can be used in salads. Soups. Or blended into hummus. They provide a significant amount of insoluble fiber. Which is crucial for bulking stool. Their rigid structure remains partially intact during digestion. Providing a “scrubbing” effect on the colon walls that helps remove debris. This mechanical cleaning action is vital for preventing the stagnation that leads to infection in the sigmoid colon.
4. Split Peas: High Soluble Fiber for Soft Stool (16g per cup)
Often overlooked. Split peas are one of the most concentrated fiber sources on the planet. A single bowl of split pea soup can provide nearly half of your daily fiber intake for diverticulitis. They are particularly high in soluble fiber. Which helps form a soft. Gel-like stool that passes easily past sensitive diverticula. Unlike whole peas. Split peas break down into a thick puree. Which is often better tolerated by those with sensitive stomachs.
5. Lima Beans: Potassium for Muscle Function (13g per cup)
Lima beans. Or butter beans. Are excellent for those who need a softer texture. They are exceptionally high in potassium. Potassium acts as an electrolyte that helps regulate the smooth muscle contractions of the digestive tract. Proper muscle function is essential for preventing the spasmodic contractions that lead to high colonic pressure. Including them in high fiber meals for diverticulitis ensures regular peristalsis without cramping.
Phase 2: Whole Grains to Power Gut Motility
Whole grains for diverticulitis provide the necessary insoluble fiber to keep waste moving. They are the engine that drives colonic motility. Unlike refined grains that turn to sugar. These complex carbohydrates provide sustained energy and gut protection.

6. Barley: Beta-Glucan for Mucosal Immunity (6g per cup)
Barley is a grain that deserves a comeback. It is one of the best sources of beta-glucan. A specific type of soluble fiber that has been shown to improve mucosal immunity. A strong mucosal barrier prevents bacteria from translocating through the colon wall. Which is a primary cause of diverticulitis complications. Adding barley to soups or salads is a simple way to fortify your diverticulitis prevention diet.
7. Quinoa: The Complete Protein for Sensitive Stomachs (5g per cup)
Quinoa is technically a seed. But it is prepared like a grain. It is a complete protein. Containing all nine essential amino acids. For patients with foods high in fiber for diverticulosis on their menu. Quinoa is often better tolerated than wheat because it is gluten-free and less likely to cause bloating in sensitive individuals. It provides a light. Fluffy texture that adds bulk without heaviness.
8. Oats: The Gold Standard for Soothing Soluble Fiber (4g per cup)
Oats are the gold standard for soothing soluble fiber. Starting your day with oatmeal coats the stomach and intestines with a protective gel. This is often the first “high fiber” food introduced during the transition phase because it is so gentle. It helps normalize bowel movements. Addressing both constipation and loose stools. For best high fiber breakfast for diverticulitis recovery. Choose steel-cut oats over instant varieties for a lower glycemic index.
9. Brown Rice: Reliable Insoluble Bulk (3.5g per cup)
While lower in fiber than other grains. Brown rice is a reliable staple. It provides consistent insoluble fiber. Unlike white rice. Which is stripped of its nutrients. Brown rice retains the bran layer. This bran acts as a mild laxative. Helping to maintain regularity without the need for harsh over-the-counter medications. It serves as an excellent base for fiber-rich stir-fries and bowls.
10. Whole Wheat Pasta: Easy Volume Eating (6g per cup)
For many Americans. Pasta is a comfort food. Switching from white to whole wheat is an easy volume win. A standard dinner serving can provide nearly 20% of your daily goal. The dense structure of whole wheat pasta means it digests slowly. Providing sustained energy and preventing blood sugar spikes that can increase systemic inflammation. It pairs perfectly with high-fiber vegetables for a complete diverticulitis safe meal.
Phase 3: High Antioxidant Berries and Fruits for Gut Health
Fruits are essential high fiber snacks for diverticulitis. The key is to eat the skin and seeds. Where the majority of the fiber resides. Berries. In particular. Are unique because their tiny seeds provide extra insoluble fiber and antioxidants.
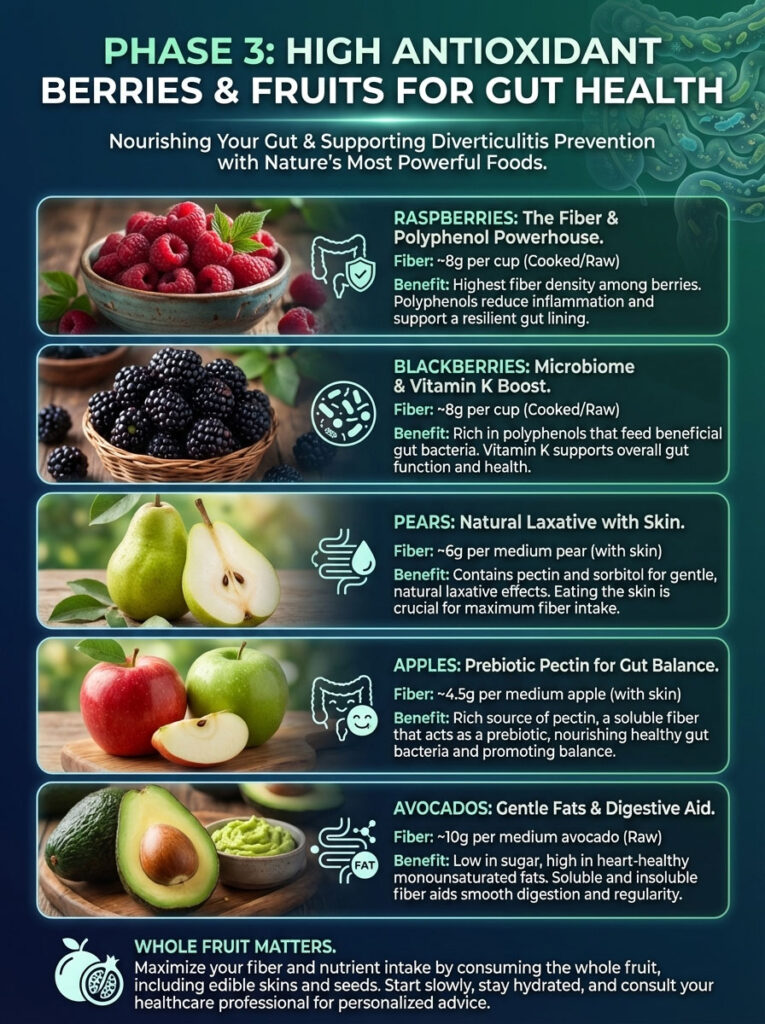
11. Raspberries: The Highest Fiber Density Fruit (8g per cup)
Raspberries offer the most fiber per calorie of any fruit. Their aggregate structure means they are made up of tiny drupelets. Each containing a seed. These seeds are safe and provide excellent insoluble fiber. They act as tiny scrubbers in the digestive tract. Ensuring that nothing stagnates in the sigmoid colon. They are low in sugar and high in polyphenols. Making them ideal for daily consumption.
12. Blackberries: Vitamin K and Polyphenols (7.5g per cup)
Similar to raspberries. Blackberries are incredibly fiber-dense. They are also high in Vitamin K. Which is important for blood clotting and bone health. Their dark pigment indicates a high level of polyphenols. Which have been shown to modify the gut microbiome composition favorably. Reducing the growth of pathogenic bacteria that could infect a diverticulum.
13. Pears: Pectin and Sorbitol for Natural Laxative Effects (5.5g per medium)
You must eat the skin. A peeled pear loses most of its gut-health benefits. Pears contain pectin. A soluble fiber that binds to fatty substances and toxins in the digestive tract and helps eliminate them. They are naturally high in sorbitol and fructose. Which pull water into the colon. Keeping stools soft. This natural laxative effect is crucial for preventing the straining associated with diverticular formation.
14. Apples: Prebiotic Pectin for Microbiome Diversity (4.5g per medium)
“An apple a day” holds true for diverticulitis. Apples are a primary source of pectin. As a prebiotic. Pectin feeds the beneficial bacteria in the colon. A healthy bacterial population prevents the overgrowth of pathogenic bacteria that could infect a diverticulum. Eating apples with the peel ensures you get the insoluble cellulose needed for bulk.
15. Avocados: Monounsaturated Fats and Fiber (10g per cup)
Avocados are unique among fruits because they are low in sugar and high in healthy monounsaturated fats. Fat is essential for the absorption of fat-soluble vitamins (A, D, E, K). The combination of fat and fiber in avocados stimulates the gastrocolic reflex gently. Encouraging a bowel movement without cramping. They are easily digestible and soothing for the gut lining.
Phase 4: Root and Cruciferous Vegetables to Heal the Colon
These vegetables are functional foods. Cruciferous vegetables for gut motility are unmatched in their ability to detoxify and repair the gut.
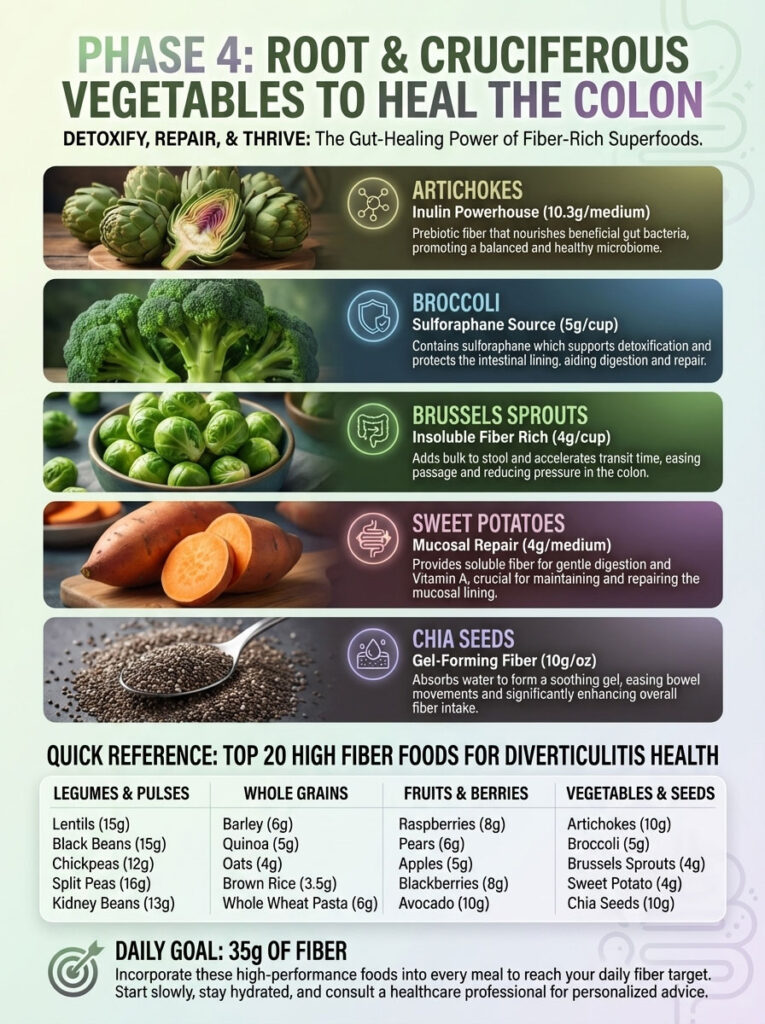
16. Artichokes: The Prebiotic Powerhouse (10.3g per medium)
Artichokes are one of the highest natural sources of inulin. A powerful prebiotic fiber. Inulin travels to the large intestine unchanged. Where it becomes a feast for Bifidobacteria. Increasing the population of these bacteria is linked to reduced inflammation and better immune function in the gut. Steaming whole artichokes allows you to eat the tender leaves and heart. Both rich in fiber.
17. Broccoli: Sulforaphane for Cellular Protection (5g per cup)
Broccoli contains sulforaphane. A compound that protects the lining of the stomach and intestine from bacterial overgrowth. It provides a good balance of fibers. During the early stages of a diverticulitis prevention diet. Cook broccoli thoroughly to break down the tough cellulose. Making it easier to tolerate. It is a staple for maintaining colonic health.
18. Brussels Sprouts: Increasing Stool Weight (4g per cup)
These mini cabbages are dense with insoluble fiber. They are particularly effective at increasing stool weight. Heavier stool moves faster through the colon. By reducing the time waste sits in the colon. Brussels sprouts minimize the exposure of the colon wall to toxins. Roasting them makes them palatable and easier to digest than boiling.
19. Sweet Potatoes: Vitamin A for Mucosal Repair (4g per medium)
Sweet potatoes are soothing and anti-inflammatory. They provide soluble fiber which is gentle on the digestive tract. They are also rich in Vitamin A. Which is crucial for maintaining the integrity of the mucosal lining of the intestines. Always eat the skin for maximum benefit. As it contains the insoluble fiber necessary for bulk.
20. Chia Seeds: The Gel-Forming Lubricant (10g per ounce)
Chia seeds are a modern superfood for gut health. When exposed to liquid. They form a mucilaginous gel. This gel lubricates the passage of stool. Making bowel movements effortless. They are effortless to add to yogurt. Oatmeal. Or smoothies. Making them an easy way to boost your daily fiber intake for diverticulitis.
Quick Reference Table: Top 20 High Fiber Foods for Diverticulitis
Use this data to audit your grocery list. Aim to include at least one of these high-performance foods in every meal to reach your 35-gram goal.
| Food Item | Fiber Per Serving (Approx) | Primary Benefit for Colon |
| Lentils (1 cup) | 15.5g | Maximum stool bulk & rapid transit |
| Black Beans (1 cup) | 15.0g | Anti-inflammatory anthocyanins |
| Split Peas (1 cup) | 16.0g | High soluble fiber for softness |
| Chickpeas (1 cup) | 12.5g | Scrubbing effect on colon walls |
| Artichoke (1 medium) | 10.3g | Prebiotic fuel for microbiome |
| Chia Seeds (1 oz) | 10.0g | Gel-forming hydration & lubrication |
| Avocado (1 cup) | 10.0g | Healthy fats for motility |
| Raspberries (1 cup) | 8.0g | Highest fruit fiber density |
| Blackberries (1 cup) | 7.5g | Polyphenols for gut flora balance |
| Barley (1 cup) | 6.0g | Beta-glucan for mucosal immunity |
| Whole Wheat Pasta (1 cup) | 6.0g | Sustainable energy & volume |
| Pears (1 medium) | 5.5g | Natural laxative properties (Sorbitol) |
| Quinoa (1 cup) | 5.0g | Complete protein, gluten-free option |
| Broccoli (1 cup) | 5.0g | Sulforaphane for cell protection |
| Apples (1 medium) | 4.5g | Pectin for microbiome diversity |
| Oats (1 cup) | 4.0g | Soothing gel for sensitive stomachs |
| Brussels Sprouts (1 cup) | 4.0g | Increases stool weight significantly |
| Sweet Potato (1 medium) | 4.0g | Vitamin A for mucosal repair |
| Brown Rice (1 cup) | 3.5g | Consistent insoluble fiber source |
| Lima Beans (1 cup) | 13.0g | Potassium for smooth muscle function |
Strategic Meal Planning for Long-Term Gut Health
Knowing which foods to eat is only half the battle. Integrating them into your lifestyle requires strategy. A successful diverticulitis prevention diet spreads fiber intake throughout the day to avoid overwhelming the gut. You cannot simply eat 35 grams of fiber at dinner and expect your stomach to handle it well.

The “Front-Load” Breakfast Strategy for Fiber Intake
The best high fiber breakfast for diverticulitis recovery sets the tone for the day. Aim to consume at least 10 grams of fiber before 9:00 AM. This gets your digestive system moving early and prevents the need to “catch up” later in the day.
Actionable Strategy: “Pro-Oats”
Do not just eat plain oatmeal. Create a fiber-dense power bowl. Combine 1/2 cup of dry oats (4g) with 1 tablespoon of chia seeds (5g) and a half-cup of raspberries (4g). This single bowl provides 13 grams of fiber. Which is nearly half of the daily requirement for some people. It combines soluble fiber from oats with insoluble fiber from seeds and berries. Creating the perfect balance.
Snacking Smart: The Anti-Chip Protocol
Snacking is where most diets fail. Processed snacks are typically devoid of fiber and high in inflammatory oils. To maintain a foods high in fiber for diverticulosis regimen. You must replace empty calories with functional foods.
Actionable Strategy: Popcorn and Nuts
Replace potato chips with air-popped popcorn. Three cups of popcorn provide nearly 4 grams of fiber. Combined with a handful of almonds or walnuts. You have a safe. Crunchy snack that actively contributes to your goals. The JAMA study explicitly states that popcorn does not cause diverticulitis. So enjoy it without fear.
Navigating Restaurants and Social Events on a Diverticulitis Diet
Dining out does not have to be dangerous. You simply need to know how to modify the menu. Many patients avoid restaurants for fear of low-fiber options. But most kitchens are stocked with the ingredients you need.
Actionable Strategy: The “Double Veg” Swap
Most restaurants serve sides of steamed broccoli or baked potatoes. Swap the french fries for a baked potato and eat the skin. If ordering a salad. Ask for extra beans or chickpeas to be added. Avoid white pasta dishes and opt for grilled proteins with double vegetables. This ensures you maintain your diverticulitis prevention diet even while socializing.
The Ecosystem: Prebiotics and Fiber Supplements
A diverticulitis prevention diet works best when supported by a healthy ecosystem. This involves feeding the good bacteria and knowing when to use supplements as an insurance policy.
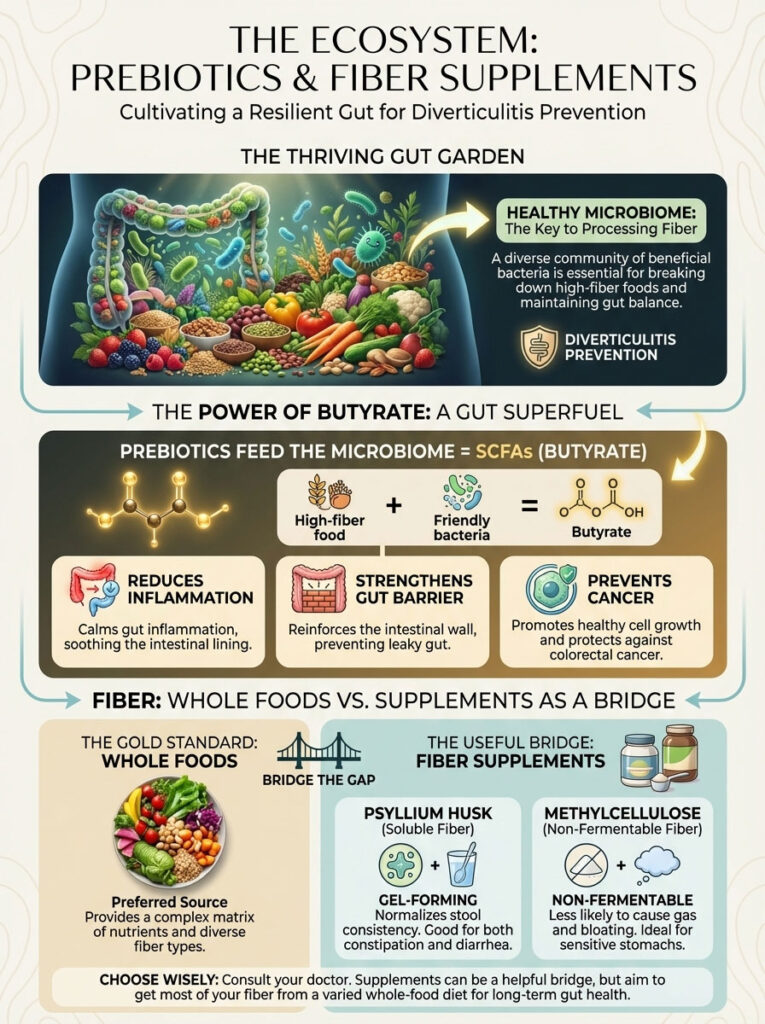
The Microbiome Connection: Feeding the Good Bacteria
When you eat high fiber foods for diverticulitis. You are not just feeding yourself. You are feeding your microbiome. Bacteria ferment this fiber to produce Short-Chain Fatty Acids (SCFAs). Specifically butyrate. Butyrate is a miracle molecule for the colon. It serves as the primary fuel source for the colonocytes (cells lining the colon). High levels of butyrate reduce inflammation. Strengthen the gut barrier. And even prevent the development of cancer cells.
When to Use Psyllium Husk and Methylcellulose
Ideally. You should get your fiber from whole foods. However. Consistency is key. If you cannot eat perfectly every day. Supplements act as a bridge.
Psyllium Husk (Metamucil): This is mostly soluble fiber. It absorbs water and forms a gel. It is excellent for normalizing stool consistency and is often used for psyllium husk for diverticular disease. It is particularly good for those who alternate between constipation and diarrhea.
Methylcellulose (Citrucel): This is a non-fermentable fiber. It creates bulk but does not ferment. Meaning it produces less gas. This is often a better choice for patients who experience severe bloating with natural fiber.
Comparative Analysis: Soluble vs. Insoluble Fiber for Gut Health
Understanding the balance between soluble and insoluble fiber is the difference between a comfortable gut and a bloated one. You need both. But they serve different masters.

Soluble fiber is the soother. It absorbs water to form a gel-like consistency. Slowing down digestion and softening stool to prevent straining. It is found in oats. Apples. Beans. And Psyllium husk. It is the best starting point for preventing the “hard stool” that requires straining.
Insoluble fiber is the mover. It adds bulk and structure to the stool. Speeding up transit time and scrubbing the colon walls. It is found in wheat bran. Nut skins. Cauliflower. And brown rice. It prevents the “stagnant stool” that breeds infection.
For a diverticular disease diet management plan. The synergy is what matters. The insoluble fiber pushes the waste. While the soluble fiber ensures the waste is soft enough to slide without injuring the diverticula. You should aim for a ratio of about 25% soluble fiber to 75% insoluble fiber.
| Feature | Soluble Fiber | Insoluble Fiber |
| Primary Function | Absorbs water to form gel | Adds bulk and structure |
| Action in Colon | Softens stool prevents straining | Speeds transit time scrubs walls |
| Best Food Sources | Oats Apples Beans Psyllium | Wheat Bran Nut Skins Brown Rice |
| Diverticulitis Benefit | Prevents hard stool complications | Prevents stagnation and infection |
| Target Ratio | Aim for ~25% of total intake | Aim for ~75% of total intake |
Summary & Key Takeaways
Preventing the recurrence of diverticulitis is an active process. It requires a commitment to fueling your body with the high fiber foods for diverticulitis that keep the sigmoid colon functioning optimally. It is not about avoiding food. It is about choosing the right food.
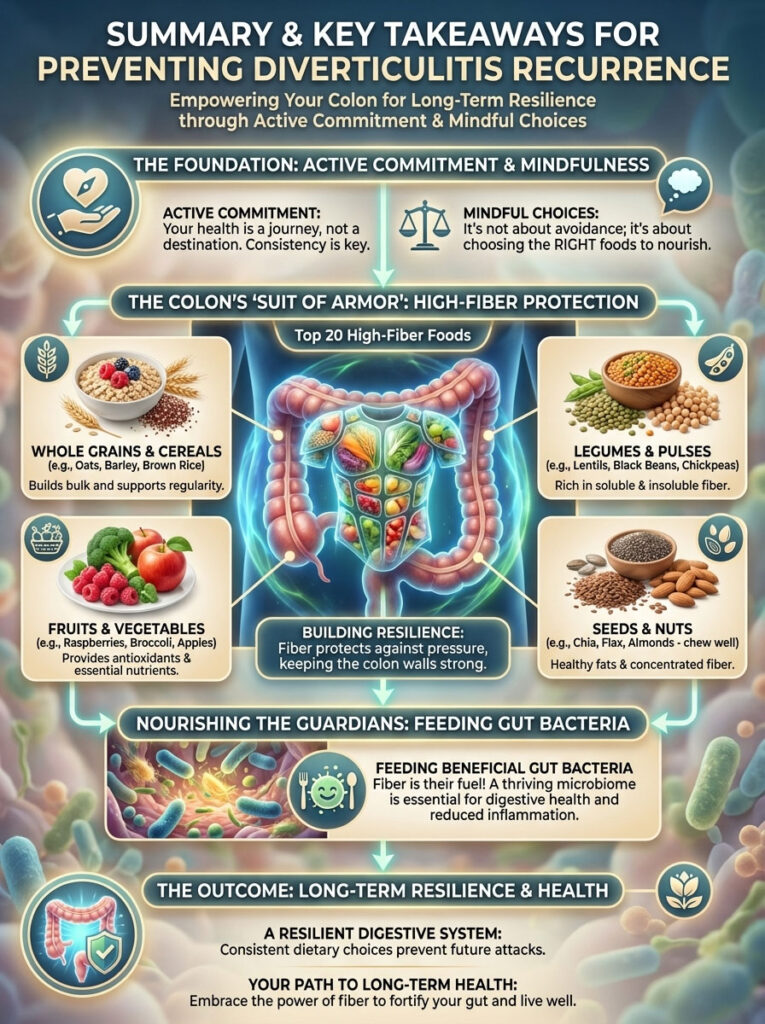
- The Goal is 35g: Aim for a daily fiber intake for diverticulitis of 25 to 35 grams.
- Embrace the Bean: Legumes are the most efficient way to reach your goals. Providing massive bulk and anti-inflammatory benefits.
- Fear No Seed: The science is clear. Nuts. Seeds. And corn are safe and beneficial. Do not let outdated advice limit your nutrition.
- Hydrate to Move: Fiber without water is a traffic jam. Drink at least 64 ounces of water daily to keep everything moving.
- Start Slow: Respect the 5-gram rule to avoid the discomfort of the fiber paradox.
By prioritizing the top 20 foods listed above. You are essentially building a suit of armor for your colon. You are reducing pressure. Feeding beneficial bacteria. And ensuring that your digestive system remains resilient against future attacks.
Frequently Asked Questions
Can I eat high fiber foods during a diverticulitis flare-up?
No. Absolutely not. During an active flare-up. Your colon is infected and needs rest. High fiber foods will irritate the inflamed tissue. You must stick to a clear liquid diet or low-residue diet until your doctor confirms the infection has cleared.
How much fiber should I eat to prevent diverticulitis?
Gastroenterologists generally recommend a daily fiber intake for diverticulitis of 25 to 35 grams. Data suggests that consistently hitting the higher end of this range (30g+) offers the strongest protection against recurrence.
Are seeds and nuts safe for diverticulitis?
Yes. They are safe. The JAMA study definitively proved that seeds. Nuts. And popcorn do not increase the risk of diverticulitis. In fact. They are excellent sources of insoluble fiber that help prevent constipation.
What is the best high fiber food for diverticulitis?
Legumes. Specifically lentils and split peas. Are widely considered the best options. They provide the highest density of fiber per serving and offer a perfect blend of soluble and insoluble fibers.
Why does fiber make me bloated?
Bloating occurs when your gut bacteria ferment fiber too rapidly. This usually happens when you increase your fiber intake too quickly. By adding fiber slowly (5 grams per week) and drinking more water. You can minimize this side effect.
Is oatmeal good for diverticulitis?
Yes. Oatmeal is excellent. It is a rich source of soluble fiber. Which is very soothing to the digestive tract. It is often the best first step when transitioning from a low-fiber recovery diet to a high-fiber maintenance diet.
Can I use fiber supplements like Psyllium husk?
Yes. Psyllium husk for diverticular disease is a great tool if you cannot reach your fiber goals through food alone. It is particularly helpful for regulating bowel movements and ensuring stool is soft and easy to pass.
Are beans safe for diverticulosis?
Beans are highly recommended for foods high in fiber for diverticulosis. They promote regular bowel movements and significantly reduce the colonic pressure that leads to the formation of new diverticula.
How does fiber “stop” diverticulitis attacks?
Fiber absorbs water and creates bulk. This allows the muscles of the colon to move waste gently. Without bulk. The colon must contract violently. Creating high pressure that can blow out the colon wall and cause infection.
What fruit has the most fiber for diverticulitis?
Raspberries are the top choice. Providing about 8 grams of fiber per cup. Other excellent high fiber snacks for diverticulitis include blackberries. Pears with the skin on. And apples.
Should I eat raw or cooked vegetables?
When first starting a high-fiber diet. Cooked vegetables are easier to tolerate because the heat breaks down some of the cellulose. Once your body adjusts. Raw vegetables are excellent for providing maximum insoluble fiber.
Can a high fiber diet heal diverticula?
A high fiber diet cannot make existing diverticula (pouches) disappear. Only surgery can remove them. However. A high fiber diet is the most effective way to prevent them from becoming inflamed and causing an attack.
Disclaimer
This article is for educational purposes only and does not constitute medical advice. Diverticulitis is a complex medical condition. Always consult your Gastroenterologist or primary care physician before making significant changes to your diet. Especially if you have recently experienced a flare-up or have a history of complications.
References
- Journal of the American Medical Association (JAMA). “Nut. Corn. And Popcorn Consumption and the Incidence of Diverticular Disease.”
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Eating. Diet. & Nutrition for Diverticular Disease.”
- Mayo Clinic. “Diverticulitis diet: List of foods to avoid.”
- American Gastroenterological Association. “Management of Acute Diverticulitis.”








