Why am I hungry but have no appetite?
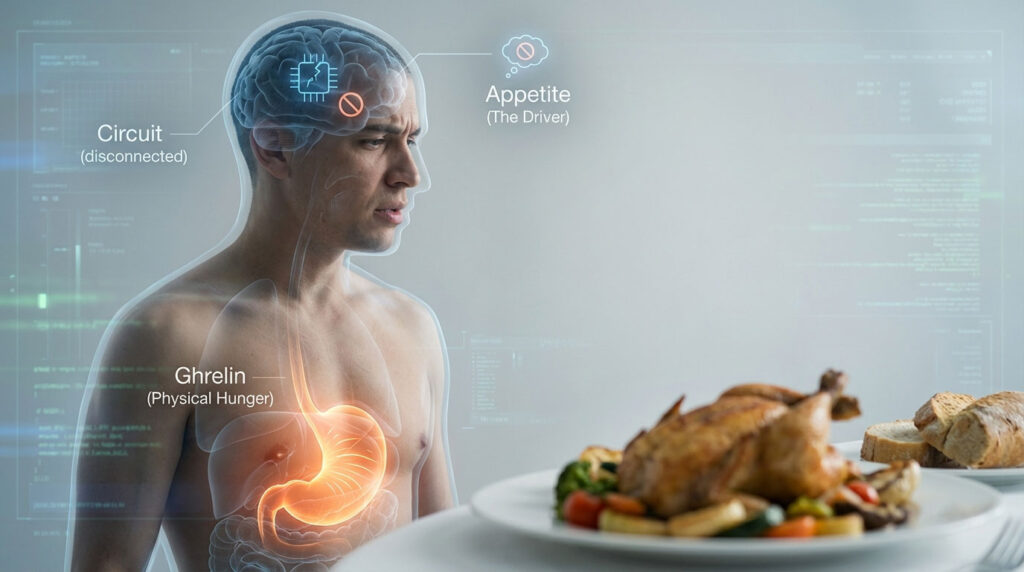
Hungry but no appetite, medically recognized as a distinct dissociation between physiological metabolic hunger and psychological hedonic appetite, occurs when the body generates intense physical hunger signals, such as stomach growling driven by ghrelin, while the brain’s desire to eat remains completely suppressed. This confusing and often distressing disconnect is frequently caused by first-trimester pregnancy hormones like rising hCG and estrogen, medication side effects specifically from ADHD stimulants or SSRIs, severe anxiety causing cortisol spikes, or chronic underlying conditions such as gastroparesis and cancer cachexia, where pro-inflammatory cytokines actively block the hypothalamus from receiving hunger cues.
Table of Contents
You are likely familiar with the specific, maddening sensation. You are staring at a plate of food. Your stomach is physically gnawing at you. It is growling loudly enough to be heard, signaling an empty, acidic hollow that desperately needs filling. Your body is screaming for fuel. Yet, the moment you pick up a fork or smell the aroma of the meal, a wave of nausea, exhaustion, or complete apathy washes over you. You physically need to eat. You psychologically cannot eat.
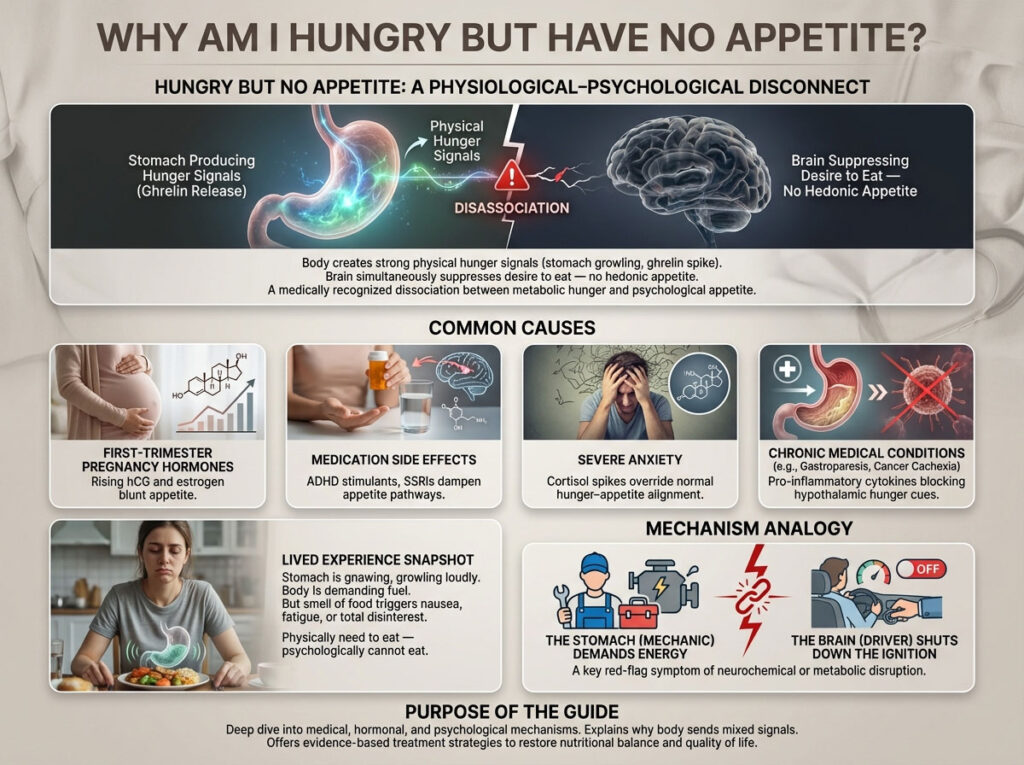
This is not simply a matter of being a picky eater. It is a complex physiological paradox where your “mechanic” (the stomach and metabolic system) is demanding energy, but the “driver” (the brain and reward pathways) has cut the ignition. For millions of patients, this symptom of feeling hungry but no appetite is the first tangible red flag of an underlying neurochemical or metabolic disruption.
This comprehensive, deep-dive guide analyzes the specific medical, hormonal, and psychological mechanisms behind this symptom. We will explore why your body is sending mixed signals and provide evidence-based treatment solutions to restore your nutritional balance and quality of life.
The Physiology of Appetitive Dissonance: Hunger Pangs Without Appetite
To treat this condition effectively, we must first dissect the biological machinery that creates the sensation of being hungry but having no appetite. Most people use the words “hunger” and “appetite” interchangeably, but medically, they are two distinct systems located in different parts of the body. In your case, these two systems are currently miscommunicating.
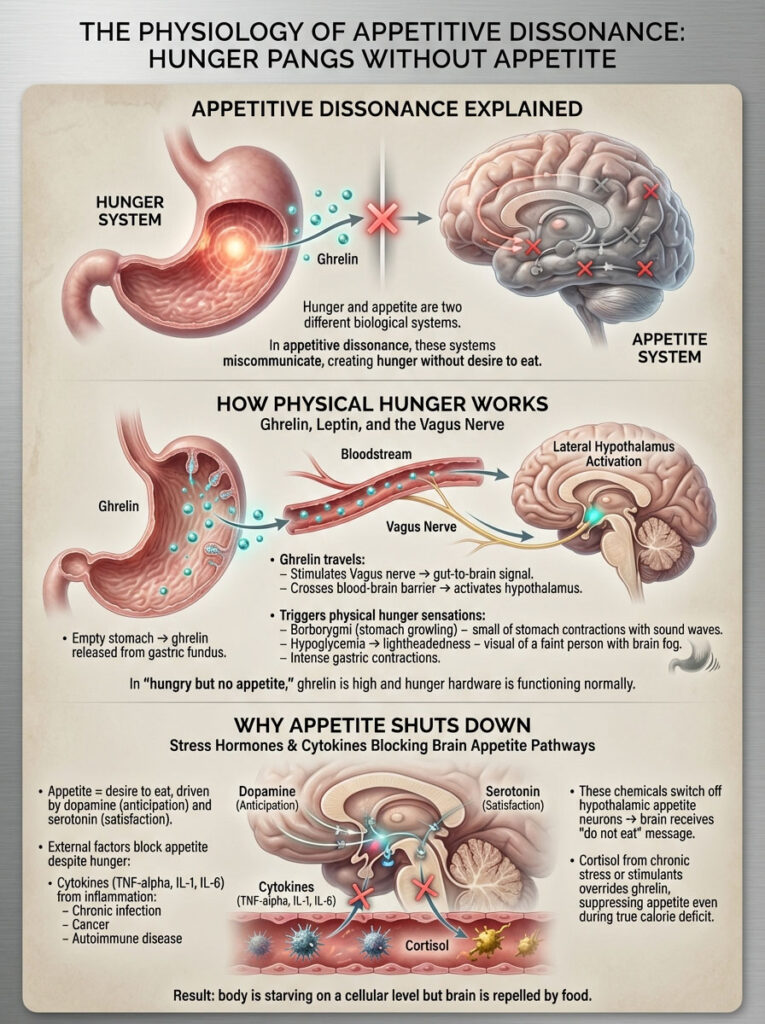
The Role of Ghrelin, Leptin, and the Vagus Nerve in Hunger Signals
Physical hunger is a survival reflex. It is not a mood or a choice. It is a hardwired metabolic alert system. When your stomach is empty, specialized cells in the gastric fundus (the upper part of the stomach) secrete a peptide hormone called ghrelin. This is often referred to by endocrinologists as the “hunger hormone.”
The mechanism is precise. Ghrelin enters the bloodstream and travels to two key locations. First, it stimulates the Vagus nerve, which creates a direct highway of information from the gut to the brainstem. Second, it crosses the blood-brain barrier to reach the hypothalamus.
This chemical signal triggers the lateral hypothalamus to initiate the physical sensations you recognize as hunger: stomach growling (medically termed borborygmi), lightheadedness from hypoglycemia (low blood sugar), and intense gastric contractions. In the state of being hungry but no appetite, your ghrelin levels are high. Your body is accurately detecting a calorie deficit. The “hardware” of hunger is working perfectly.
How Stress Hormones and Cytokines Block Hypothalamic Appetite Centers
If hunger is the need to eat, appetite is the desire to eat. Appetite is regulated by the brain’s reward pathways, specifically involving dopamine (anticipation of pleasure) and serotonin (mood and satisfaction). This is what makes food look appealing and motivates you to take a bite.
The blockade happens here. When you feel hungry but no appetite, an external factor is intercepting the hunger signal before it can create the desire to eat.
In conditions involving systemic inflammation, such as cancer, chronic infection, or autoimmune disease, the body releases inflammatory markers called cytokines, specifically TNF-alpha, IL-1, and IL-6. These chemicals serve a protective role in acute illness but have a devastating effect on nutrition. They cross the blood-brain barrier and chemically switch off the appetite neurons in the hypothalamus. Your brain literally receives a chemical message that says “do not eat,” even while the stomach is screaming “feed me.”
Similarly, stress hormones play a massive role. High levels of cortisol from chronic stress or synthetic drugs like stimulants can override the ghrelin signal. The result is a patient who is starving on a cellular level but feels mentally repelled by food.
8 Detailed Medical Causes of Feeling Hungry But Having No Appetite
This symptom is rarely idiopathic, meaning it almost always has a specific cause. It usually stems from one of eight specific medical, pharmaceutical, or lifestyle triggers.
1. Mental Health Factors: Anxiety-Induced Nausea and Depression Anhedonia
The gut-brain axis is the primary highway for emotional impact on digestion. The stomach is often called the “second brain” because of its sensitivity to emotion.
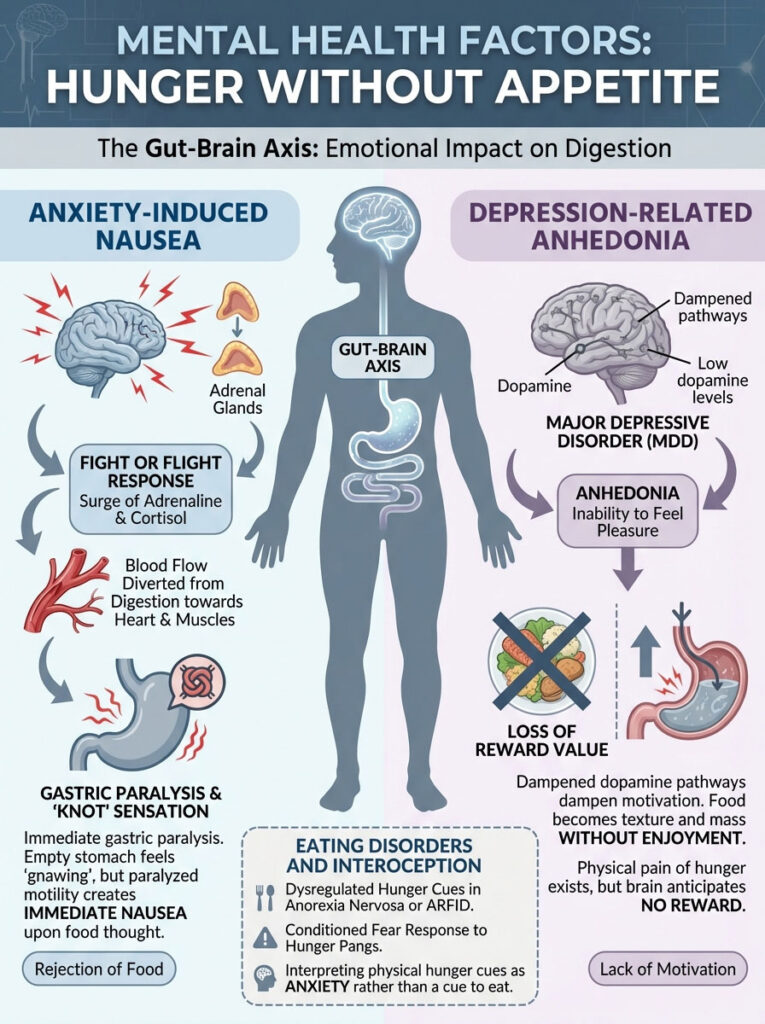
Anxiety-Driven Adrenaline:
When acute anxiety hits, the adrenal glands release a massive surge of adrenaline and cortisol. This triggers the ancient “fight or flight” response. To prepare you to run or fight, the body shunts blood flow away from non-essential systems like digestion and directs it toward the heart and skeletal muscles. The result is immediate gastric paralysis. You feel the “gnawing” emptiness of hunger because your stomach is empty, but because gastric motility has stopped, the idea of adding food to a “paralyzed” stomach creates immediate nausea. The physical sensation is often described as a “knot” in the stomach that mimics hunger but rejects food.
Depression-Related Anhedonia:
A defining, core symptom of Major Depressive Disorder (MDD) is anhedonia, which is the inability to feel pleasure or interest in things that were once enjoyable. Eating is biologically designed to be a dopamine-driven reward activity. When dopamine pathways are dampened by depression, food loses its reward value. It becomes texture and mass without enjoyment. You feel the physical pain of hunger, but you lack the motivation to resolve it because the brain anticipates no reward from the effort of eating.
Eating Disorders and Interoception:
In conditions like Anorexia Nervosa or ARFID (Avoidant/Restrictive Food Intake Disorder), the body’s hunger cues (interoception) become dysregulated. Over time, patients may feel the physical sensation of hunger but have conditioned a psychological fear response to it, interpreting the hunger pangs as anxiety rather than a cue to eat.
2. ADHD Medication Side Effects: Adderall and Ritalin Appetite Suppression
Prescription stimulants used for Attention Deficit Hyperactivity Disorder (ADHD) are perhaps the most common pharmaceutical cause of being hungry but no appetite in both children and adults.

Mechanism of Action:
Drugs like Adderall (amphetamine salts), Vyvanse (lisdexamfetamine), and Ritalin (methylphenidate) function by increasing synaptic concentrations of dopamine and norepinephrine in the prefrontal cortex. While this enhances focus and executive function, these neurotransmitters are potent appetite suppressants. They act on the hypothalamus to mimic satiety.
The “Hollow” Feeling:
Patients often describe a very specific, uncomfortable sensation. Their stomach feels “hollow,” “caved in,” or physically cramping from emptiness during the day while the medication is active. However, the thought of chewing or swallowing food feels impossible, almost like trying to eat cardboard. This creates a dangerous cycle of daytime starvation followed by “rebound hunger” late at night when the medication excretes from the system, often leading to binge eating at 9:00 PM or 10:00 PM.
3. SSRI Antidepressants and Serotonin-Related Nausea
Selective Serotonin Reuptake Inhibitors (SSRIs) like Lexapro (escitalopram), Zoloft (sertraline), and Prozac (fluoxetine) are the first-line treatments for anxiety and depression, yet they ironically worsen appetite issues during the initial phase of treatment.
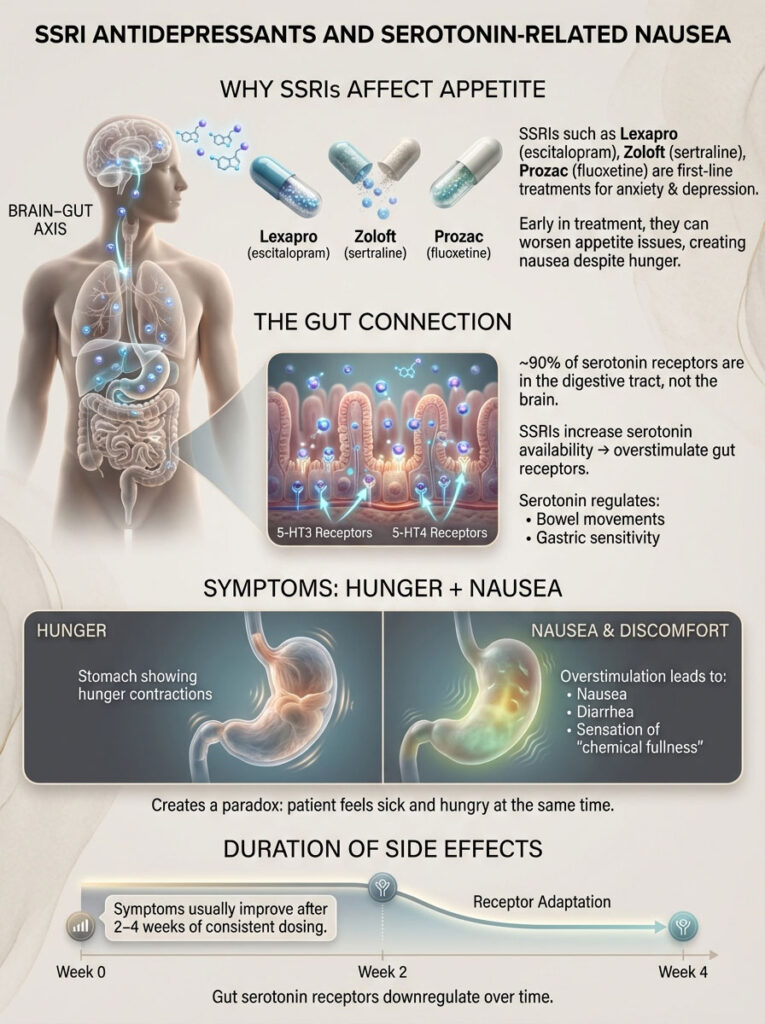
The Gut Connection:
It is a common misconception that serotonin is only in the brain. Approximately 90% of the body’s serotonin receptors (specifically 5-HT3 and 5-HT4 receptors) are located in the lining of the digestive tract. Serotonin regulates bowel movements and gastric sensitivity. By artificially boosting serotonin availability to help the brain, these medications also overstimulate the gut receptors.
This results in nausea, diarrhea, and a sensation of “chemical fullness” that clashes violently with physical hunger pangs. The patient feels sick and hungry simultaneously. Fortunately, this side effect is usually transient and typically resolves after 2 to 4 weeks of consistent dosing as the serotonin receptors downregulate.
4. Gastrointestinal Disorders: Gastroparesis and Acid Reflux Mimicking Hunger
Sometimes the disconnect is purely mechanical, originating within the digestive tract itself.
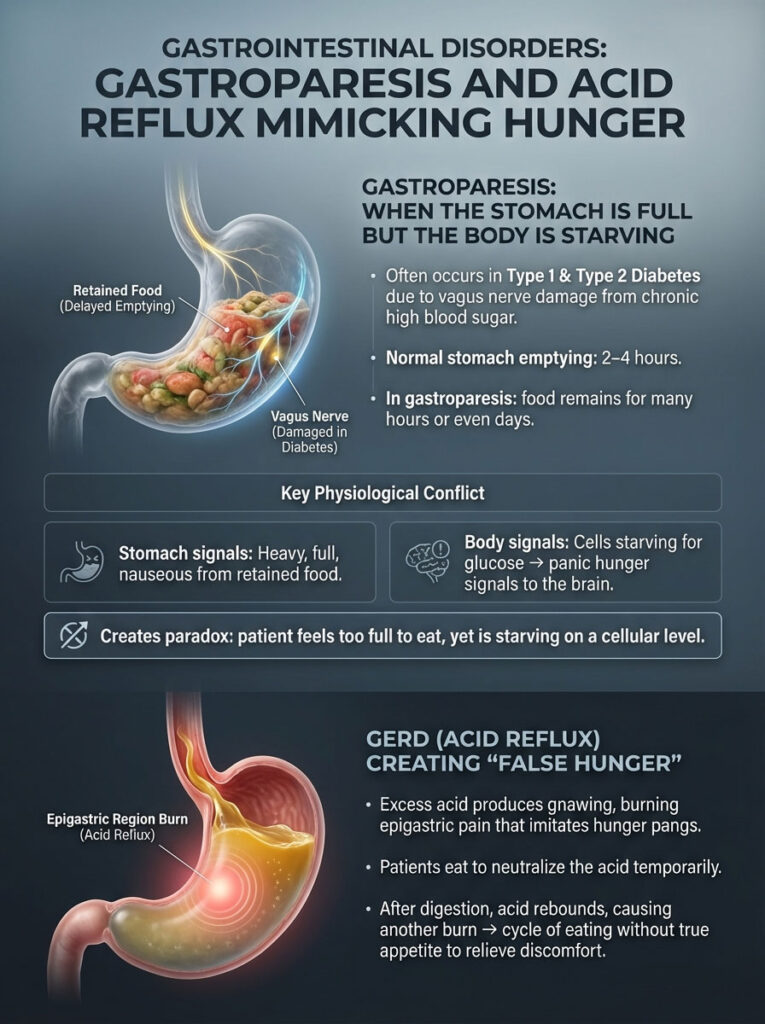
Diabetic Gastroparesis:
This is a serious condition involving partial paralysis of the stomach muscles, commonly seen in Type 1 and Type 2 Diabetes due to vagus nerve damage from high blood sugar. In a healthy stomach, food empties into the small intestine within 2 to 4 hours. In gastroparesis, food remains in the stomach for many hours or even days.
This creates a confounding physiological state. The stomach feels heavy, full, and nauseous because of the retained food. However, because the food is not entering the small intestine to be absorbed, the body’s cells are starving for glucose. The brain receives panic signals of starvation (hunger), but the stomach sends signals of extreme fullness. The result is a patient who is starving on a cellular level but feels physically too stuffed to take a bite.
GERD (Acid Reflux):
Excess stomach acid can cause a gnawing, burning sensation in the epigastric region (the upper center of the abdomen) that closely mimics hunger pangs. This is often called “false hunger.” Patients often eat to soothe the burn, as food temporarily neutralizes the acid. However, once the food is digested, the acid rebounds, leading to a cycle of eating without true appetite to manage pain.
5. Cancer-Related Cachexia and Cytokine-Driven Appetite Loss
Cachexia is a complex metabolic wasting syndrome associated with advanced cancer, HIV/AIDS, and severe heart failure. It is distinct from simple starvation.
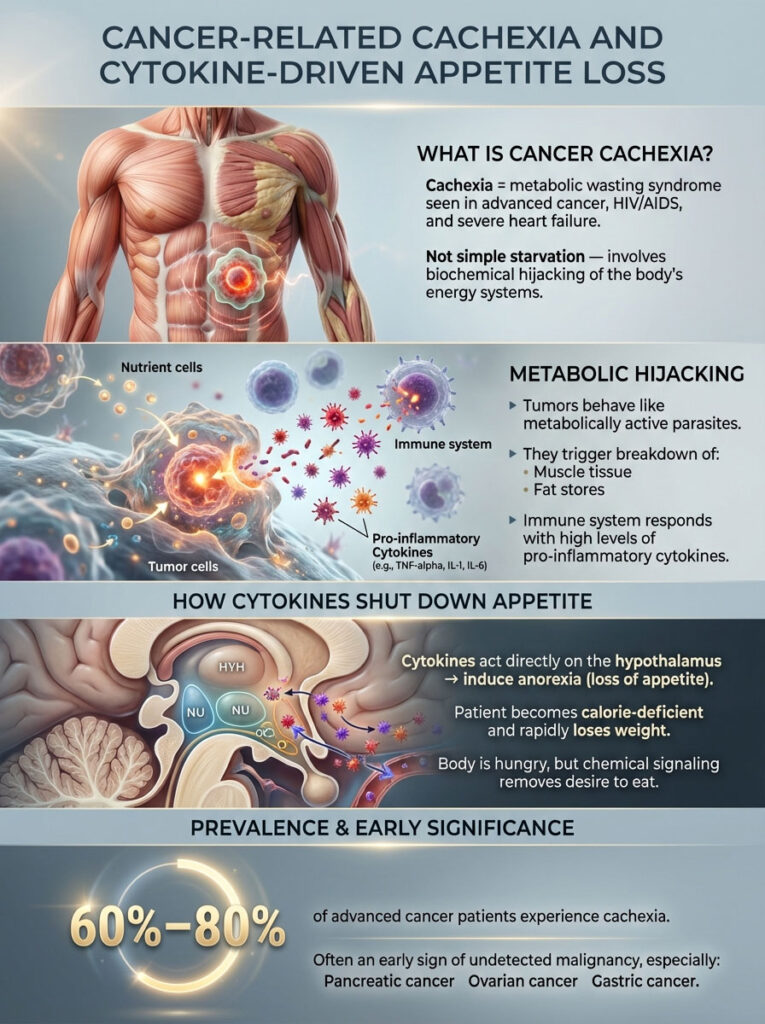
Metabolic Hijacking:
Tumors are metabolically active parasites. They produce chemical factors that actively break down the host’s muscle and fat tissue to use for their own fuel. Simultaneously, the immune system fights back by releasing massive amounts of pro-inflammatory cytokines.
The Outcome:
These cytokines act directly on the brain’s hypothalamus to induce anorexia (loss of appetite). The patient is in a severe calorie deficit (hungry) and losing weight rapidly, but they are chemically blocked from wanting food. Statistics indicate that 60% to 80% of advanced cancer patients experience this debilitating symptom. It is often one of the first signs of undetected malignancy, particularly in pancreatic, ovarian, and gastric cancers.
6. Thyroid Dysfunction: Hyperthyroidism Hunger vs. Hypothyroidism Slowing
The thyroid gland is the master regulator of metabolism, and its dysfunction can create confusing appetite signals.
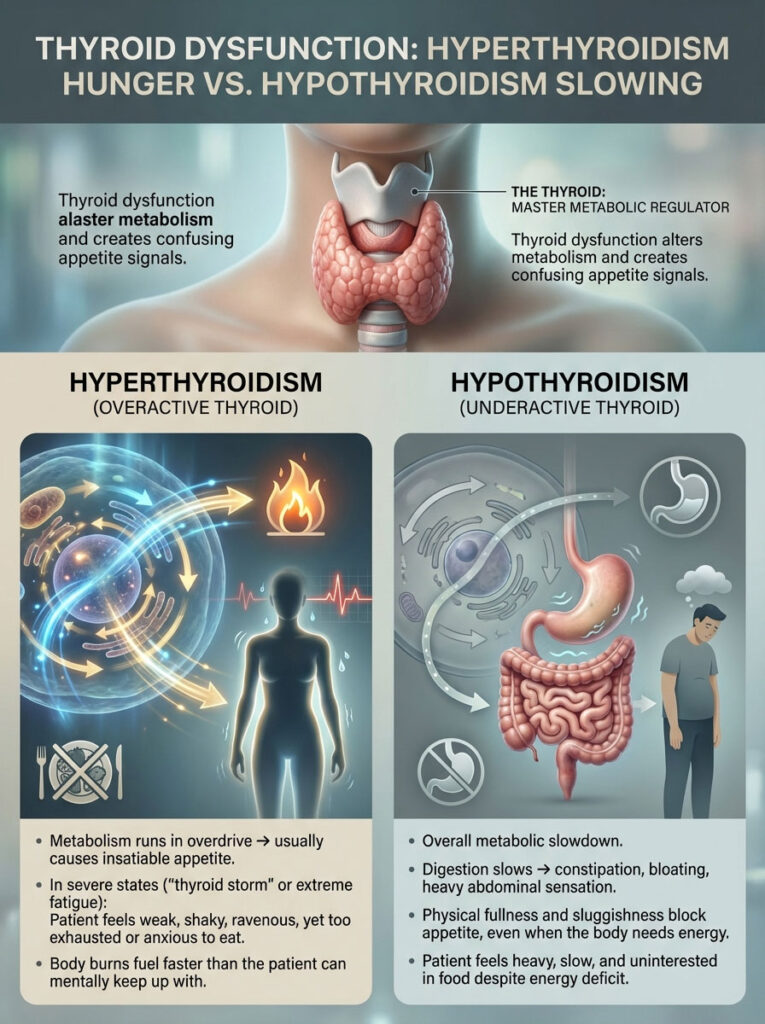
Hyperthyroidism (Overactive Thyroid):
An overactive thyroid sends the metabolism into overdrive. Typically, this causes an insatiable appetite. However, in states of “thyroid storm” or extreme fatigue, the metabolism runs so fast that the patient feels weak, shaky, and physically ravenous, yet they are too exhausted and anxious to physically consume food. The body is burning fuel faster than the patient can mentally keep up with.
Hypothyroidism (Underactive Thyroid):
Conversely, an underactive thyroid causes a general slowdown of all bodily functions, including digestion. Gastric motility slows down, leading to severe constipation and bloating. This physical blockage creates a barrier to eating, even when the body signals a need for energy. The patient feels sluggish and heavy, killing the appetite despite the need for nutrients.
7. Viral Infections and Sickness Behavior: Flu and COVID-19
When you catch a viral load like Influenza or COVID-19, your body enters a specific physiological mode known as “sickness behavior.”
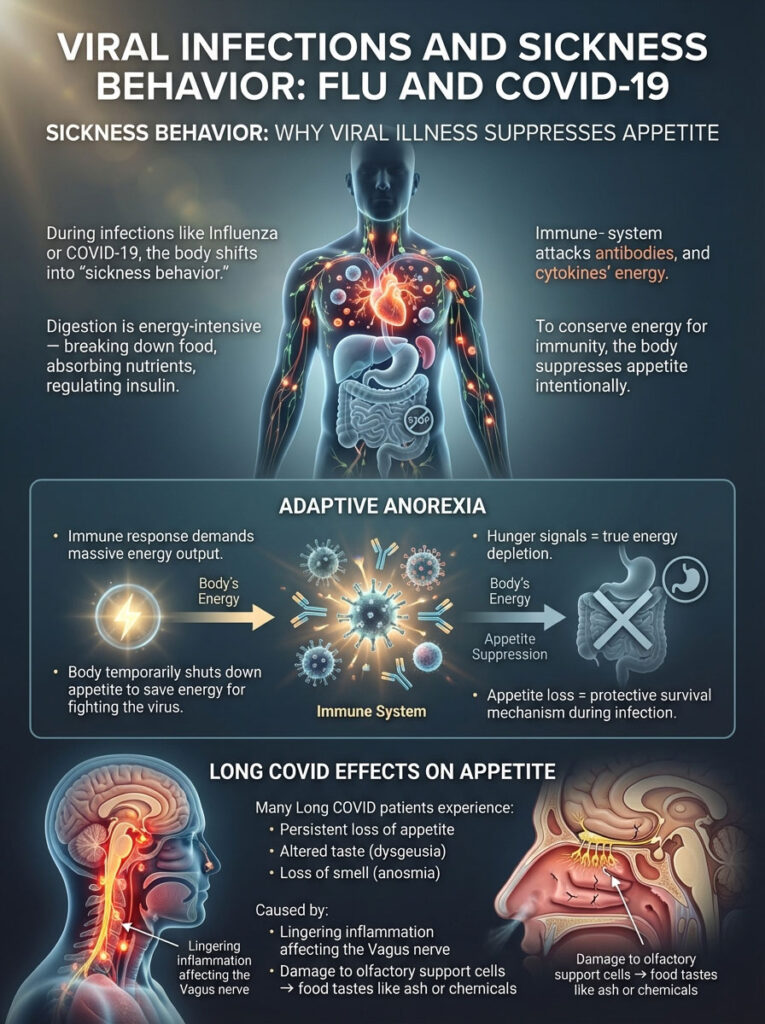
Adaptive Anorexia:
Digestion is an energy-intensive process. It requires significant caloric output to break down food, absorb nutrients, and manage insulin levels. When the immune system is under attack, the body decides it cannot spare the energy for digestion. It suppresses appetite to conserve resources for the immune response. The “hunger” you feel is a valid signal of energy depletion, but the loss of appetite is a protective mechanism preventing you from spending limited energy on digestion.
Long COVID Implications:
In the wake of the pandemic, many patients with “Long COVID” report persistent loss of appetite or altered taste and smell (anosmia or dysgeusia) for months after the initial infection. This is believed to be caused by lingering inflammation affecting the Vagus nerve or the destruction of olfactory support cells, making food taste like ash or chemicals.
8. Nutritional Deficiencies: Zinc and Vitamin B12
Sometimes the lack of appetite is caused by the absence of the very nutrients you need to eat.
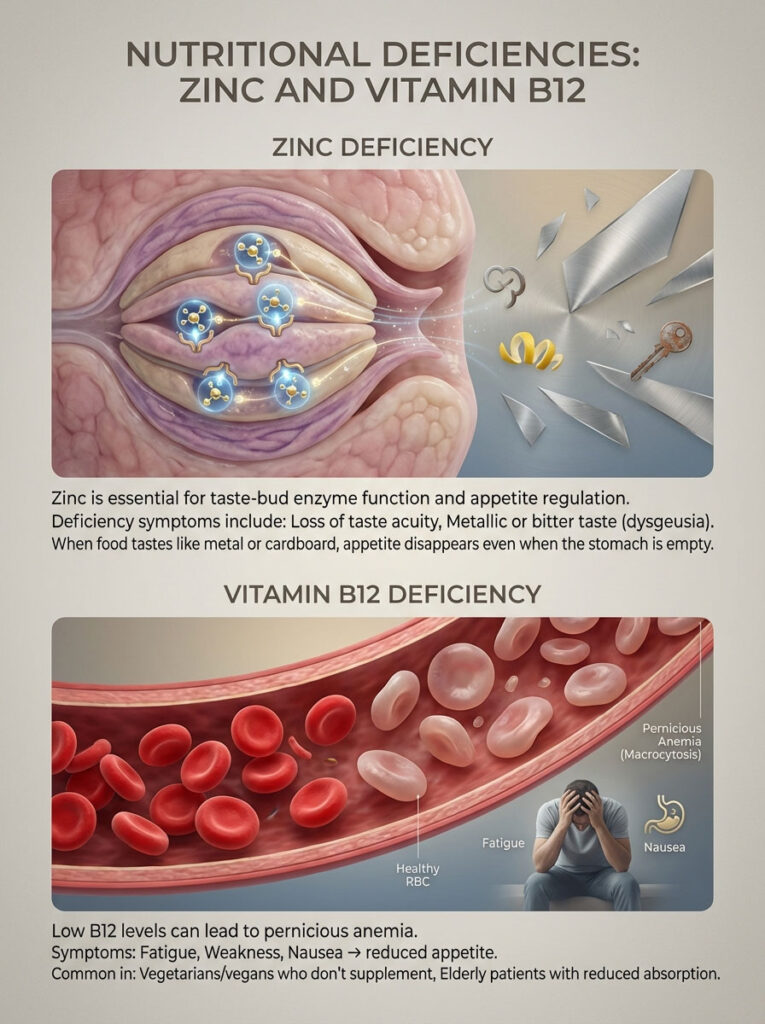
Zinc Deficiency:
Zinc is a trace mineral that is crucial for the enzymatic function of taste buds and appetite regulation. A deficiency often manifests as a loss of taste acuity or a persistent metallic/bitter taste in the mouth (dysgeusia). If food tastes like metal or cardboard, the psychological desire to eat vanishes, even if the stomach is empty.
Vitamin B12 Deficiency:
Low B12 levels can cause pernicious anemia. Symptoms include fatigue, weakness, and significant nausea, which leads to a reduction in appetite. This is common in vegetarians or vegans who do not supplement, as well as in elderly patients with poor absorption.
Hungry But No Appetite During Pregnancy: Trimester-Specific Causes
Pregnancy is one of the leading causes of this phenomenon in women of childbearing age, but the underlying mechanism shifts dramatically from the beginning to the end of gestation.
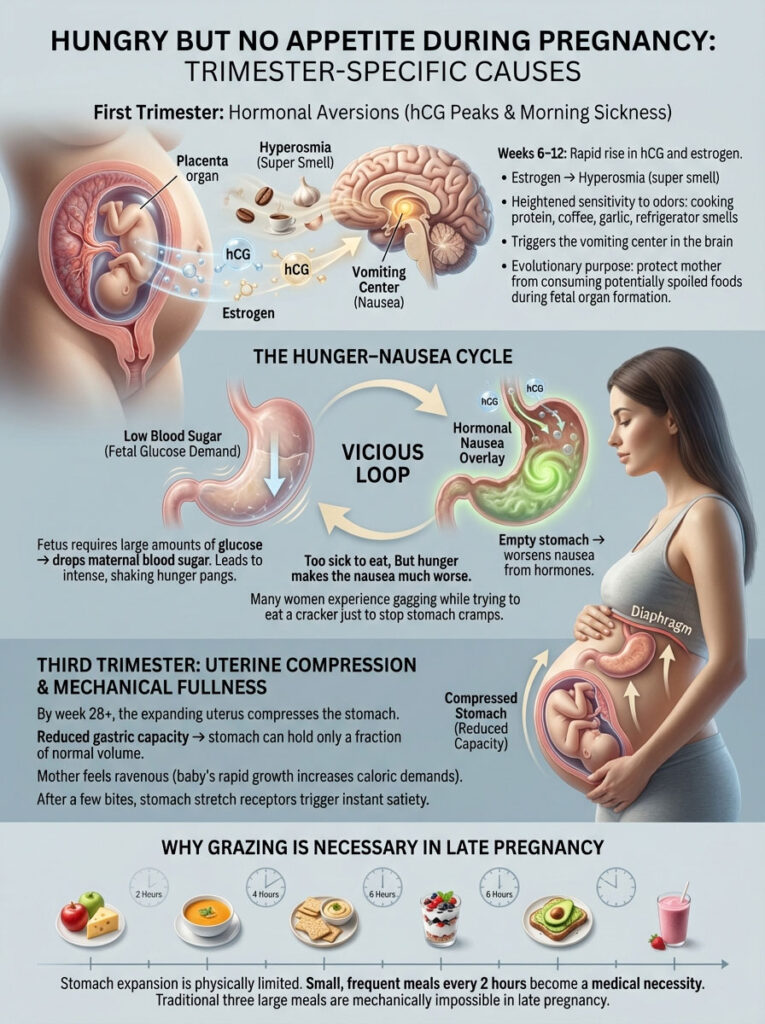
First Trimester Hormonal Aversions: hCG Peaks and Morning Sickness
Between weeks 6 and 12, the placenta produces rapidly increasing levels of hCG (Human Chorionic Gonadotropin) and estrogen.
Hyperosmia (Super Smell):
Estrogen heightens olfactory sensitivity to a superhuman degree. The smell of cooking protein, coffee, garlic, or even a refrigerator being opened can trigger the vomiting center in the brain. This is an evolutionary protection mechanism to prevent the mother from ingesting potentially spoiled food during the critical period of organ formation.
The Hunger-Nausea Cycle:
Simultaneously, the developing fetus has high glucose demands, which drops the mother’s blood sugar rapidly. This triggers intense, shaking physical hunger pangs. However, the empty stomach worsens the nausea caused by hormones. This creates a vicious cycle: you are too sick to eat, but being hungry makes you sicker. This is why many women find themselves gagging while trying to eat a cracker to stop their stomach from cramping.
Third Trimester Uterine Compression and Mechanical Fullness
By week 28 and beyond, the uterus has expanded significantly to accommodate the growing baby, physically pushing the stomach upward against the diaphragm and squashing it.
Reduced Gastric Capacity:
The stomach physically has less room to expand. Its capacity is reduced to a fraction of its normal size. You may feel ravenous due to the baby’s rapid growth spurts and high caloric needs, but after just a few bites, the stomach wall stretches to its limit. This triggers immediate satiety signals via the stretch receptors.
Solution:
This is why the “grazing” method (eating small amounts every 2 hours) is not just a tip but a medical necessity in late pregnancy. Three large meals are mechanically impossible.
Diagnostic Comparison: Distinguishing Hunger Pangs from Gastritis and Nausea
It is crucial to determine if your sensation is true metabolic hunger or a “false alarm” caused by gastric irritation. This distinction helps in choosing the right treatment.
| Feature | True Metabolic Hunger | False Hunger (Gastritis/Acid) | Appetite Loss (Anhedonia) |
| Sensation Origin | Deep pit of stomach, throat, or general weakness. | Upper abdomen (burning), chest, or back of throat. | Brain / Emotional State. |
| Onset Pattern | Gradual build-up (3-4 hours post-meal). | Sudden onset, constant, or waking you at night. | Constant lack of interest, unrelated to meal timing. |
| Response to Food | Sensation resolves immediately upon eating. | Sensation often worsens or changes to nausea after eating. | Eating feels like a forced chore; no satisfaction. |
| Associated Symptoms | Stomach growling, lightheadedness, shakiness. | Acidic taste, bloating, sharp pain. | Fatigue, sadness, social withdrawal, numbness. |
| Relief Mechanism | Eating carbohydrates or protein. | Antacids or proton pump inhibitors. | Exercise, therapy, medication adjustment. |
Medical Treatments and Dietary Solutions for Appetite Loss
When the brain refuses to cooperate with the stomach, relying on “willpower” rarely works. You cannot simply force yourself to enjoy food. You must use clinical strategies to bypass the psychological and physiological barriers to eating.

Nutritional Strategies: Liquid Calories, Cold Foods, and Micro-Dosing Meals
Liquid Bio-Hacking:
The mechanical act of chewing and swallowing can feel insurmountable when appetite is low. It requires effort and prolongs the sensory experience of food. Liquids bypass the “chewing fatigue” and move through the stomach faster.
- Tactics: Utilize high-calorie oral nutritional supplements (ONS) like Ensure Plus, Boost VHC, or clinical peptide formulas. Alternatively, make homemade calorie-dense smoothies using full-fat Greek yogurt, nut butters, heavy cream, and whey protein isolate. Sipping a 500-calorie shake over an hour is easier than eating a 500-calorie meal in 20 minutes.
The “Cold Food” Protocol:
Hot foods release volatile organic compounds (aromas) that float into the air, trigger the olfactory nerve, and can induce immediate nausea. Cold foods are chemically more stable and emit significantly less smell.
- Tactics: Switch to a “cold diet” when symptoms are bad. Rely on chilled chicken salad, cottage cheese, hard-boiled eggs, chilled fruit (grapes/melon), cold sandwiches, and gelatin. Avoid heating food in the microwave, which disperses odors.
Micro-Dosing Calories:
A full dinner plate creates visual anxiety. It looks like a mountain that you have to climb.
- Tactics: Adopt a strict “grazing” schedule. Eat 6 to 8 micro-meals per day. Redefine what a “meal” is. Five crackers and a slice of cheese count as a meal. Half a banana with a spoonful of peanut butter counts as a meal. The goal is to keep blood sugar stable without ever overfilling the sensitive stomach.
Pharmacological Interventions: Appetite Stimulants and Anti-Nausea Medications
If dietary changes are insufficient, medical intervention is required. Doctors have several tools to help reset the appetite.
Appetite Stimulants (Orexigenics):
- Megestrol Acetate: A progesterone derivative often used in cancer, AIDS, and geriatric patients. It significantly boosts appetite and promotes weight gain, though it is hormonal and used with caution.
- Mirtazapine (Remeron): An atypical antidepressant utilized in geriatrics and depression cases. Unlike SSRIs that kill appetite, Mirtazapine’s primary side effect is significant appetite stimulation and sedation. It is excellent for patients who are anxious, can’t sleep, and can’t eat.
- Corticosteroids: Drugs like Dexamethasone are used for short-term appetite boosting, primarily in palliative care or chemotherapy settings. They reduce inflammation (cytokines) and induce a feeling of well-being and hunger.
Anti-Emetics (Anti-Nausea):
- If nausea is the primary barrier, treating the hunger is useless until the nausea is gone. Medications like Zofran (Ondansetron) work by blocking serotonin receptors in the gut and brain that trigger the vomiting reflex. Taking this 30 minutes before a planned meal can open the “eating window” and allow natural hunger cues to surface.
Clinical Case Studies and Data on Appetite Dysregulation
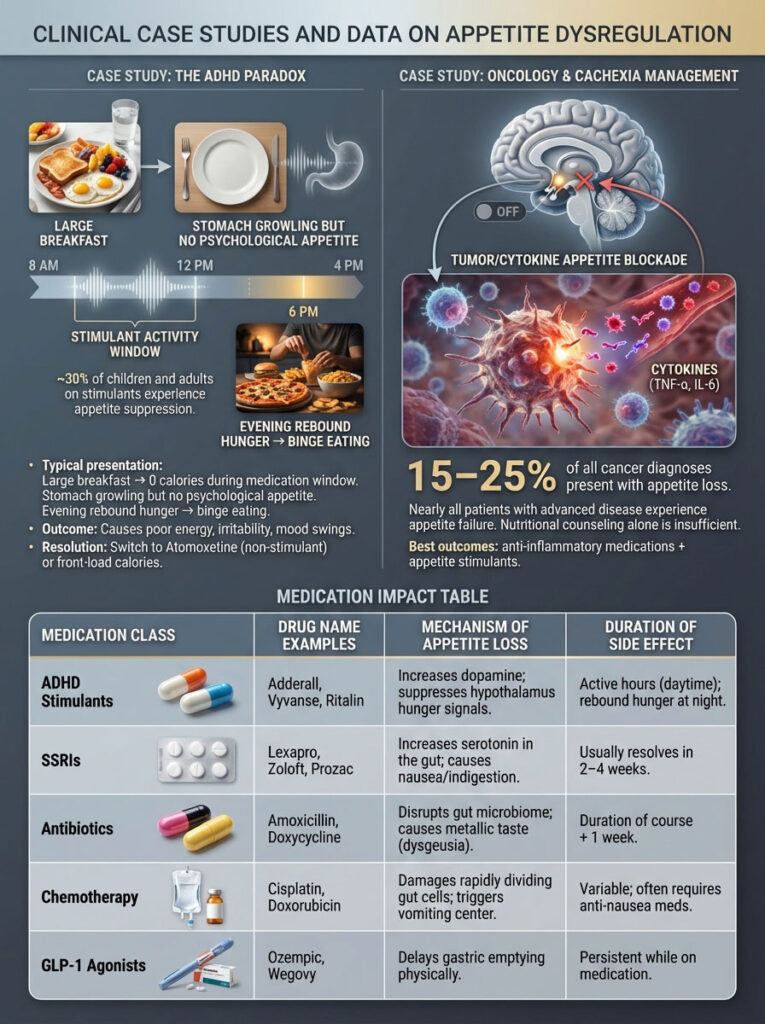
Case Study: The ADHD Paradox
Clinical data suggests that up to 30% of children and adults on stimulant medications experience appetite suppression as a primary side effect. A typical clinical presentation involves a patient who eats a large breakfast before dosing, consumes zero calories during the active medication window (8:00 AM – 4:00 PM) despite having a growling stomach, and then experiences extreme “rebound hunger” in the evening.
- Outcome: This binge-restrict cycle often leads to poor energy, irritability, and mood swings. Switching to non-stimulant medications (like Atomoxetine) or adjusting meal timing to “front-load” calories often resolves the issue.
Case Study: Oncology and Cachexia Management
According to the National Cancer Institute, loss of appetite is one of the presenting symptoms in 15% to 25% of all cancer diagnoses and is present in nearly all patients with advanced disease.
- Insight: In a study of advanced cancer patients, nutritional counseling alone was found to be insufficient. The biological drive to not eat was too strong. The combination of anti-inflammatory medication (to lower cytokines) plus appetite stimulants showed the highest success rate in restoring the drive to eat.
Medication Impact Table
This table outlines common medications that cause the “hungry but no appetite” phenomenon and how long the effect typically lasts.
| Medication Class | Drug Name Examples | Mechanism of Appetite Loss | Duration of Side Effect |
| ADHD Stimulants | Adderall, Vyvanse, Ritalin | Increases dopamine; suppresses hypothalamus hunger signals. | Active hours (daytime); rebound hunger at night. |
| SSRIs | Lexapro, Zoloft, Prozac | Increases serotonin in the gut; causes nausea/indigestion. | Usually resolves in 2–4 weeks. |
| Antibiotics | Amoxicillin, Doxycycline | Disrupts gut microbiome; causes metallic taste (dysgeusia). | Duration of course + 1 week. |
| Chemotherapy | Cisplatin, Doxorubicin | Damages rapidly dividing gut cells; triggers vomiting center. | Variable; often requires anti-nausea meds. |
| GLP-1 Agonists | Ozempic, Wegovy | Delays gastric emptying physically. | Persistent while on medication. |
Summary & Key Takeaways: Managing Appetitive Dissonance
Before addressing common questions, let’s consolidate the critical points regarding why you feel hungry but no appetite and how to manage it.
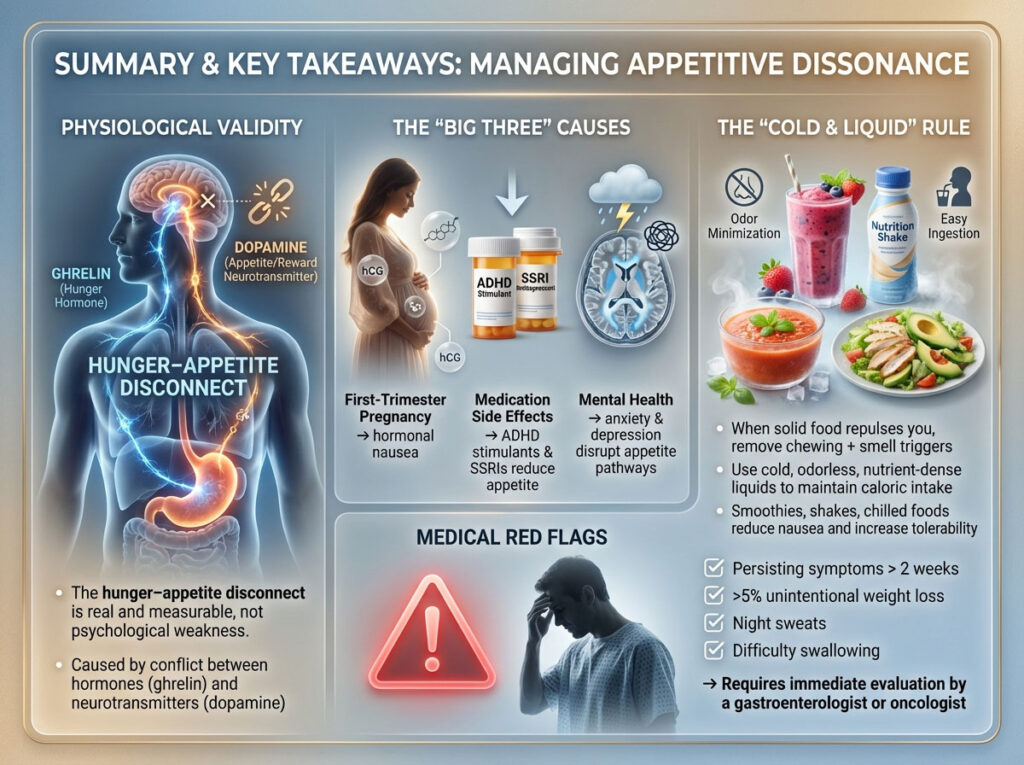
- Physiological Validity: The disconnect between physical hunger (stomach) and psychological appetite (brain) is a real, measurable medical phenomenon, not a behavioral flaw. It is driven by a clash between hormones like ghrelin and neurotransmitters like dopamine.
- The “Big Three” Causes: The most frequent drivers of this symptom are First-Trimester Pregnancy (hormonal nausea), Medication Side Effects (specifically ADHD stimulants and SSRIs), and Mental Health (anxiety and depression).
- The “Cold & Liquid” Rule: When solid food repulses you, bypass the chewing mechanism and olfactory triggers. Rely on cold, odorless, nutrient-dense liquids (smoothies, shakes) to maintain caloric intake without triggering nausea.
- Medical Red Flags: While often temporary, if this symptom persists for more than two weeks, or is accompanied by unintentional weight loss of more than 5% of your body weight, night sweats, or difficulty swallowing, it requires immediate evaluation by a gastroenterologist or oncologist.
Frequently Asked Questions About Hunger Without Appetite
Why do I feel hungry but nauseous when I look at food?
This specific symptom profile—physical hunger mixed with nausea—is the classic hallmark of gastritis, early pregnancy, or severe anxiety. The hunger stems from an empty stomach releasing ghrelin, while the nausea is caused by irritation of the gastric lining or stress hormones triggering the chemoreceptor trigger zone (CTZ) in the brain. The two signals collide, leaving you feeling sick and starving simultaneously.
Can chronic stress make you hungry but have no appetite?
Yes. Chronic stress elevates cortisol and adrenaline. These hormones prepare the body for “fight or flight” by shutting down non-essential systems like digestion. You may feel the physical emptiness of the stomach, but your brain has chemically suppressed the appetite center to prioritize survival and alertness. This is often called “stress anorexia.”
How do I force myself to eat when I have no appetite?
Do not force large meals, as this can trigger a gag reflex or vomiting, creating a stronger psychological aversion to food. Instead, treat eating as a medical necessity, like taking medicine. Set an alarm for every 3 hours. Consume nutrient-dense, low-volume foods like nut butters, cheese, or liquid nutrition shakes. Distracted eating (eating while watching TV or scrolling on a phone) can also help bypass the psychological block by keeping the conscious brain occupied.
Is feeling hungry but no appetite a sign of diabetes?
It can be. Specifically, it is a symptom of diabetic gastroparesis. High blood sugar over time damages the Vagus nerve, causing the stomach to empty too slowly. This leaves you feeling full and nauseous because food is sitting in the stomach, yet your body’s cells are starving for glucose, sending out urgent hunger signals.
Why does my stomach growl if I don’t want to eat?
Stomach growling (borborygmi) is a mechanical event caused by the movement of gas and fluid in the intestines. It is intensified by the hormone ghrelin when the stomach is empty. Your stomach is simply performing its mechanical duty to signal emptiness, even if your brain is suppressing the desire to eat due to medication, mood, or illness.
How long does appetite loss from antibiotics last?
Appetite loss from antibiotics typically persists for the duration of the medication course plus 2 to 3 days. Antibiotics can disrupt the gut microbiome and cause dysgeusia (metallic taste), both of which suppress appetite. Taking a high-quality probiotic during and after the course may help accelerate recovery.
Can dehydration cause false hunger pangs?
Yes. The hypothalamus regulates both hunger and thirst signals, and they are located very close to each other in the brain. Mild dehydration often presents as a hollow feeling or “hunger.” If you are hungry but no appetite, sip an electrolyte drink first; if the hunger subsides, it was likely thirst.
Why am I hungry but can’t eat in the morning?
Morning appetite loss is often due to the “Cortisol Awakening Response,” a natural spike in stress hormones upon waking that mobilizes energy but suppresses digestion. Additionally, post-nasal drip settling in the stomach overnight can cause morning nausea that masks hunger. Eating a plain cracker before getting out of bed can sometimes help neutralize the acid.
Is it safe to skip meals if I have no appetite?
Occasional skipping is acceptable during acute illness, but chronic skipping worsens the problem. An empty stomach accumulates acid, which leads to more nausea and a stronger aversion to food. This creates a “starvation-nausea loop.” Small, frequent snacks are much safer and more effective than skipping meals entirely.
What are the best foods for appetite loss in the elderly?
Elderly patients often lose appetite due to diminished taste and smell known as “anorexia of aging.” The best foods are flavor-enhanced and soft in texture. Good options include cream soups, puddings, scrambled eggs with cheese, mashed avocado, and protein-fortified shakes (like Boost VHC). Adding spices and herbs can help stimulate the numbed taste buds.
Does COVID-19 cause long-term appetite loss?
Yes. “Long COVID” can cause persistent loss of appetite or altered taste/smell for months. This is believed to be caused by lingering inflammation affecting the Vagus nerve or olfactory neurons. Olfactory training (smell therapy) has shown some success in helping these patients recover.
Can low blood sugar occur without feeling hungry?
Yes, this is called hypoglycemia unawareness. It is dangerous. However, more commonly, the body screams for sugar (physical hunger, shaking, sweating) even if the person has no appetite or desire for food due to nausea or illness. In this case, fast-acting glucose (like juice or honey) is medically necessary regardless of appetite.
Disclaimer: This content is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The symptom of feeling hungry but having no appetite can indicate serious underlying medical conditions ranging from thyroid disorders to cancer. Always consult a qualified healthcare provider for diagnosis and treatment.
References
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Gastroparesis and Diabetic Complications.
- American Cancer Society. Managing Cancer-Related Appetite Loss.
- National Institute of Mental Health (NIMH). The Neurobiology of Anhedonia in Depression.
- Journal of Clinical Psychopharmacology. Stimulant Medication and Appetite Suppression in ADHD.
- American College of Obstetricians and Gynecologists (ACOG). Morning Sickness: Nausea and Vomiting of Pregnancy.