Imagine eating nothing but kale and grilled chicken for months, only to have your doctor tell you your cholesterol is skyrocketing. I see this nightmare scenario play out constantly. You feel betrayed by your own body, wondering why the math doesn’t add up.
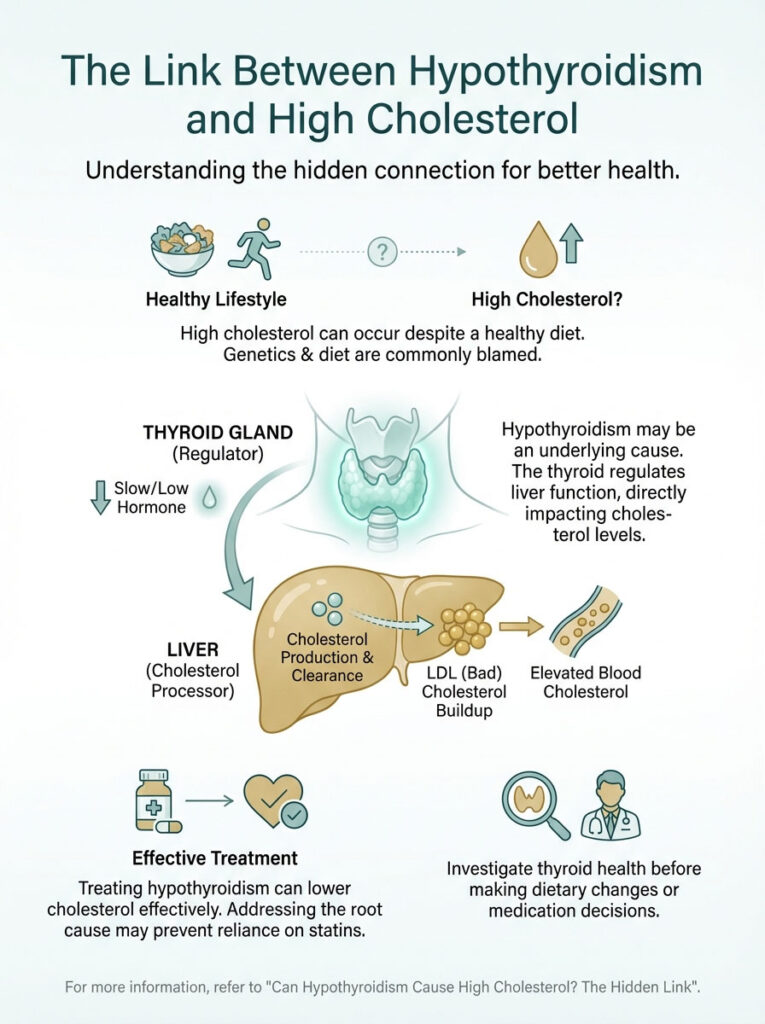
Most people immediately blame the eggs they ate for breakfast or their genetics. But in my experience, a massive percentage of these cases have nothing to do with food. There is a silent switch in your neck that controls your liver, and if it’s flipped off, no amount of salad will save you.
Before you accept a lifetime prescription for statins, you need to investigate the hypothyroidism connection. I found that treating the thyroid first doesn’t just lower cholesterol, it often fixes the problem entirely.
If this raised questions, the full guide answers them: Can Hypothyroidism Cause High Cholesterol? The Hidden Link
The Biological “Docking” Failure
Your liver acts as the primary filtration system for fat. Under normal circumstances, it produces tiny “docks” called LDL receptors. These receptors grab bad cholesterol from your blood and eliminate it.
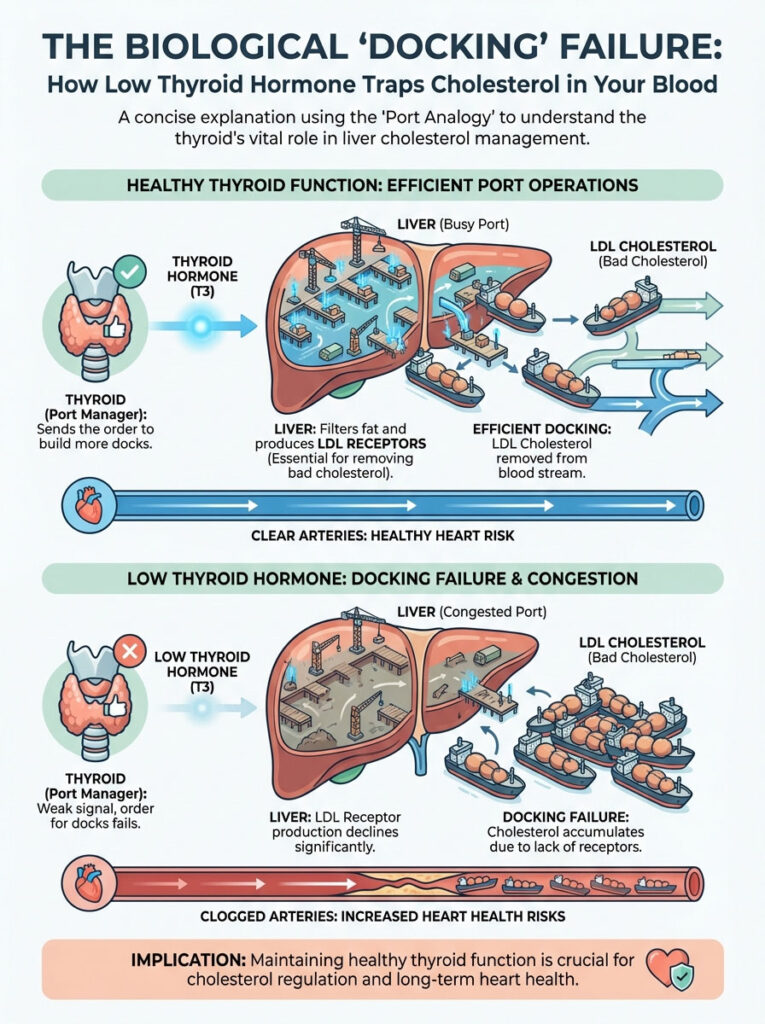
However, these docks require a specific fuel to be built: Thyroid Hormone (T3).
When I explain this to patients, I use a simple analogy. Imagine your liver is a busy port. If the port manager (the thyroid) goes on strike, the workers stop building docks. Ships full of cargo (cholesterol) pile up in the harbor (your arteries).
The Cellular Breakdown
- No Signal: Low T3 fails to trigger the SREBP-2 gene.
- No Docks: The liver stops making LDL receptors.
- Toxic Buildup: LDL particles oxidize and stick to artery walls.
Why Statins Can Be a Trap
Here is the terrifying truth about treating this condition backward. Statins work by forcing the liver to make more receptors. But remember, the liver needs thyroid hormone to build them.
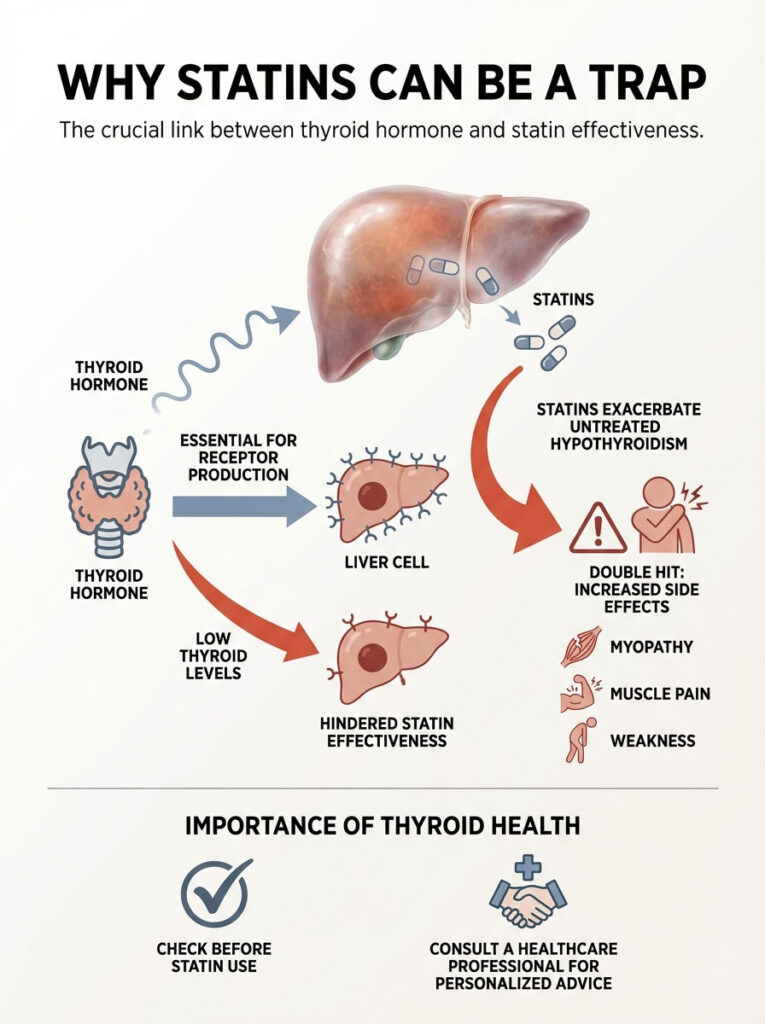
If you take a statin while your thyroid is tanked, you are whipping a starving horse. It can’t run faster.
Worse, I have seen patients suffer severe side effects. Combining statins with untreated hypothyroidism creates a “double hit” on your muscles. This significantly raises the risk of myopathy, severe muscle pain and weakness.
Danger Zones
- Muscle destruction: Increased risk of rhabdomyolysis.
- Brain fog: Statins may worsen cognitive fatigue.
- Liver stress: Enzymes can spike dangerously high.
The “Normal” Range Lie
Your doctor might say your thyroid is “fine” because your TSH is 4.5. Do not accept this answer. In the functional medical world, we know the liver is incredibly sensitive.
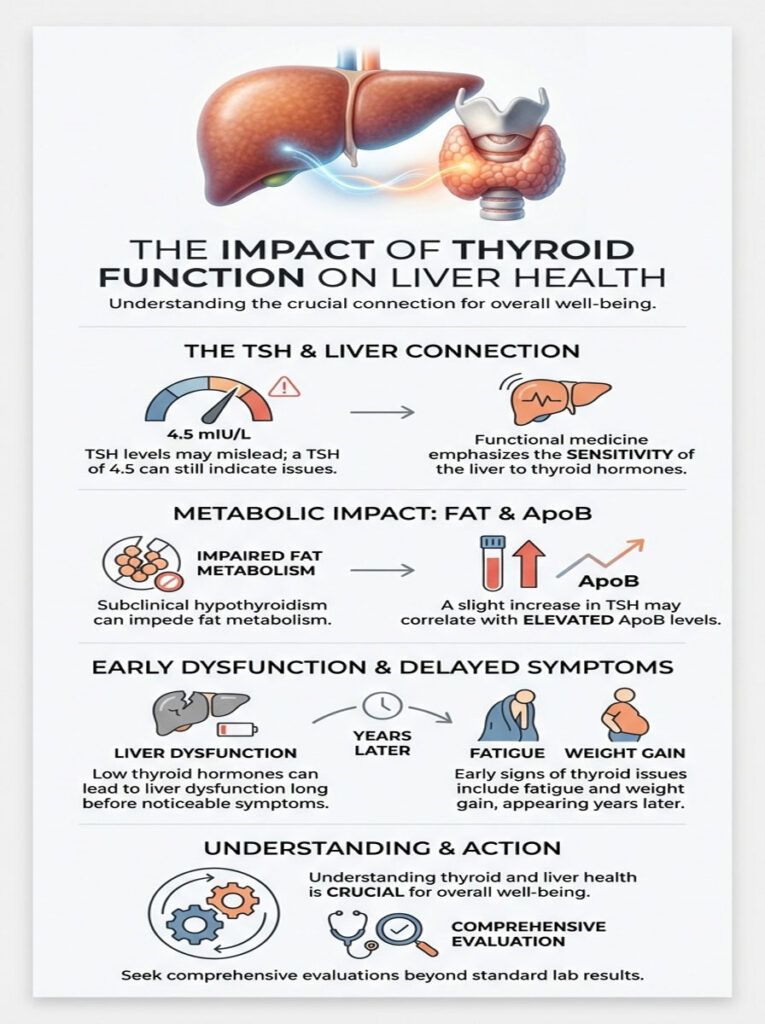
Even “subclinical” hypothyroidism, where labs look mostly normal can stall fat burning. I have reviewed charts where a slight TSH elevation correlated perfectly with a massive spike in ApoB (a deadly heart disease marker).
Social Currency Fact: The liver is the first organ to suffer from low thyroid hormones, often years before you feel tired or gain weight.
Strategic Testing Protocol
You cannot fix what you do not measure. A standard physical is useless here. You must demand a deeper look at your metabolic engine.
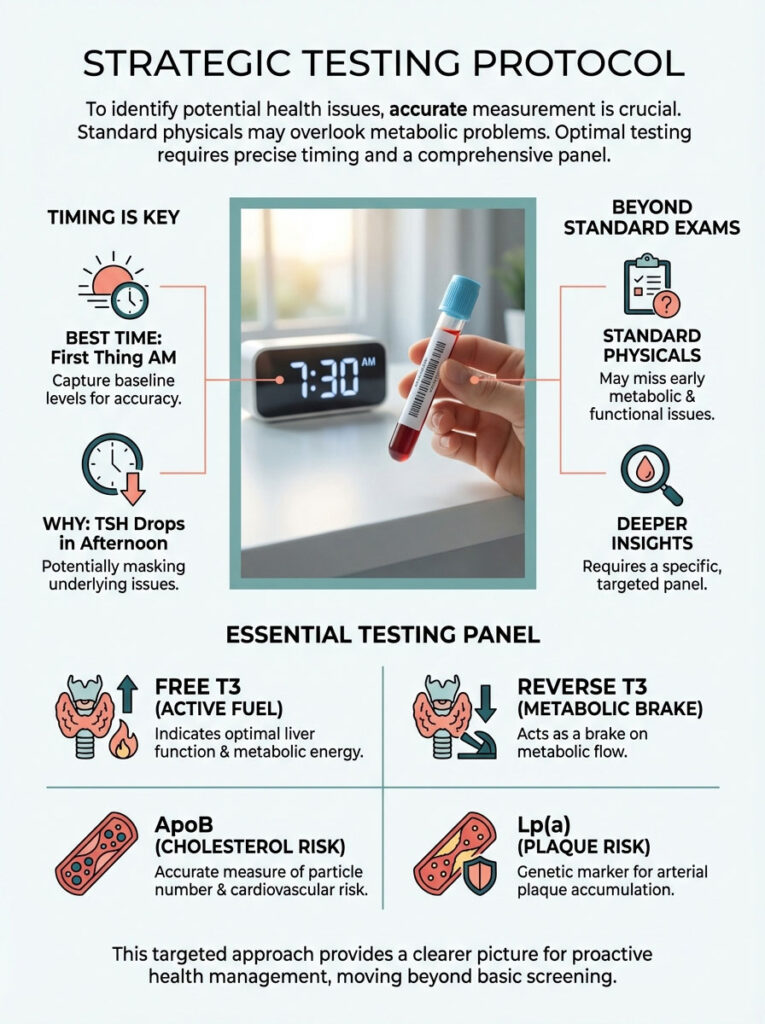
I always advise my clients to test first thing in the morning. TSH levels drop naturally in the afternoon, which can mask the problem entirely.
The Essential Panel
| Test Name | What It Reveals | optimal Target |
|---|---|---|
| Free T3 | The active fuel your liver needs | Top 50% of range |
| Reverse T3 | The “brake pedal” blocking flow | Bottom of range |
| ApoB | The true count of plaque particles | < 80 mg/dL |
| Lp(a) | Genetic sticky cholesterol risk | < 30 mg/dL |
Reversing the Damage
The most amazing part of this diagnosis is that it is reversible. You aren’t doomed to have heart disease. Once we introduce the right thyroid medication, the magic happens.

The T3 hormone enters the liver cells. It flips the genetic switch. Suddenly, the liver builds millions of new receptors. I have watched LDL levels drop 50 points in six weeks just by optimizing thyroid medication.
My 3-Step Recovery Plan
- Stabilize TSH: Use Levothyroxine or NDT to reach euthyroid status.
- Wait 6 Weeks: Give the liver time to clear the backlog.
- Re-test Lipids: Only then should you consider if statins are needed.
Key Takeaway: If your cholesterol is high, look at your neck before you look at your heart. The solution might be hormonal, not dietary.