You are eating the “perfect” diet. You drink nearly a gallon of water a day. You take your medication faithfully every morning. Yet, you feel heavy, bloated, and toxic because your bowels simply will not move. In my clinical practice, Hypothyroidism Constipation is the most common and frustrating complaint I hear from patients managing thyroid conditions. It is not just a nuisance; it is a metabolic failure that perpetuates your disease.
Table of Contents
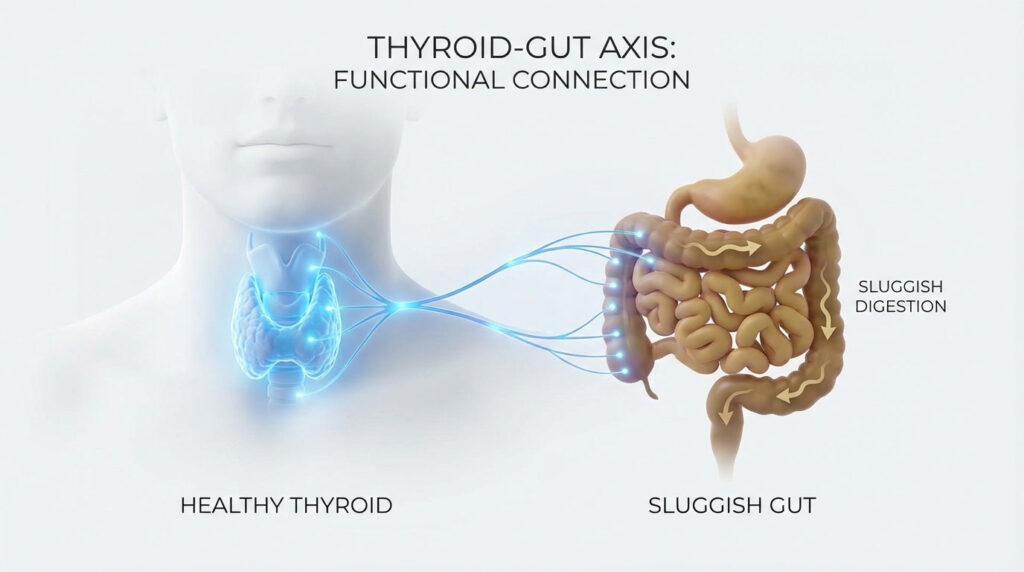
Hypothyroidism Constipation is not merely a lack of fiber. It is a systemic reduction in gastric motility caused by insufficient active thyroid hormone signaling to the gut’s nervous system. When your thyroid slows down, your digestion slows down. This creates a dangerous feedback loop where a slow gut impairs hormone conversion, which in turn further slows the gut. To break this cycle, we must look beyond laxatives and address the neurological and hormonal roots of the problem.

Why won’t my gut move?
Hypothyroidism Constipation occurs because a lack of T3 hormone signals the muscles in your intestines to relax. This prevents the wave-like contractions, known as peristalsis, needed to move waste. This leads to a halted Migrating Motor Complex (MMC). Consequently, bacteria overgrow (SIBO) and waste stagnates. Fixing it requires optimizing T3 levels, spacing meals to activate the MMC, and using specific prokinetics rather than just adding bulk fiber.
The Biology of a Slow Gut: Why Low Thyroid Stops Peristalsis
To understand why standard advice like “eat more bran” often fails patients with Hashimoto’s thyroiditis, we have to look at the cellular biology of digestion. Your thyroid is the master gear of your metabolism. It sets the pace for every process in the body. This includes how fast food travels through your gastrointestinal tract.
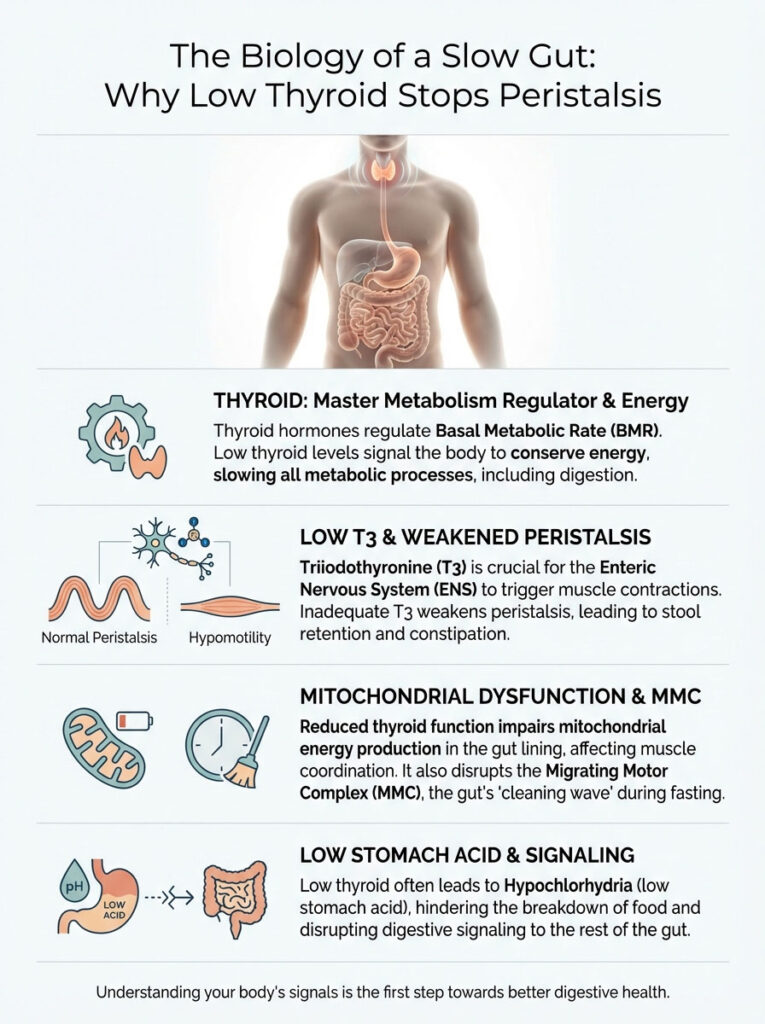
When the Basal Metabolic Rate (BMR) drops due to insufficient thyroid hormone, the body attempts to conserve energy. Digestion is an energy-intensive process. Consequently, the body applies a “metabolic brake” to the digestive system. This results in a condition clinically known as hypomotility.
The Role of T3 in the Enteric Nervous System
The Enteric Nervous System (ENS) is often called the “second brain” of the gut. It lines the gastrointestinal tract. It controls the mechanical mixing and movement of food. Research published in the Journal of Clinical Endocrinology & Metabolism highlights a critical mechanism. The active thyroid hormone, Triiodothyronine (T3), binds directly to receptors on the smooth muscle cells of the intestines.
Without adequate T3, these muscles cannot contract with enough force. This weakens peristalsis. Peristalsis is the rhythmic squeezing action that pushes stool through the colon. The result is slow gut motility. Waste sits in the colon for days. It becomes dry, hard, and difficult to pass as the body reabsorbs water from the stool.
Mitochondrial Dysfunction in the Gut Lining
Every cell in your digestive tract requires energy to function. This energy comes in the form of ATP (Adenosine Triphosphate). The mitochondria, which are the power plants of your cells, require T3 to produce ATP. In a hypothyroid state, the mitochondria in the gut lining become sluggish.
This lack of cellular energy means the intestinal wall cannot repair itself efficiently. It also means the muscles lack the explosive power needed to move heavy waste matter. You might feel the urge to go, but the muscular coordination required to expel the stool is simply too weak. This is often why patients report feeling “incomplete evacuation” even after a bowel movement.
The Migrating Motor Complex (MMC)
Perhaps the most overlooked factor in thyroid gut health is the Migrating Motor Complex (MMC). Think of the MMC as the street sweeper of your intestines. It is an electromechanical wave. It sweeps through the small intestine every 90 to 120 minutes. But here is the catch: it only happens when you are in a fasted state.
In a healthy person, the MMC clears out residual food, bacteria, and cellular debris between meals. In patients with Hypothyroidism Constipation, the signaling to initiate the MMC is weak or absent. If you graze throughout the day or have low T3, this cleaning wave never happens. This stagnation is the primary driver for bacterial overgrowth and severe bloating.
Hypochlorhydria: The Acid Trigger
Digestion is a chain reaction. It starts in the stomach with the production of Hydrochloric Acid (HCL). HCL is necessary to break down proteins. More importantly, it triggers the pyloric sphincter to open and release food into the small intestine. Studies suggest a strong link between autoimmune thyroid disease and autoimmune gastritis. This leads to Hypochlorhydria, or low stomach acid.
If your stomach acid is low, the signal to move food forward is never sent. Food sits in the stomach. It ferments and causes reflux. Meanwhile, the lower bowel remains inactive because it never received the “incoming” signal. Addressing stomach acid is often step one in fixing slow gastric motility.
Key Statistics: The Thyroid-Gut Connection
- 54% of hypothyroid patients suffer from SIBO (Small Intestinal Bacterial Overgrowth), compared to low rates in healthy controls.
- 20% of your inactive T4 hormone is converted to active T3 in the gut by healthy bacteria.
- Gastric transit time can be prolonged by 50% or more in unmedicated hypothyroid patients.
- Up to 40% of Hashimoto’s patients exhibit signs of low stomach acid (Hypochlorhydria).
- Women are three times more likely to suffer from constipation-predominant IBS, which often overlaps with undiagnosed hypothyroidism.
The Vicious Cycle: How Constipation Worsens Thyroid Function
We often view constipation as a symptom of thyroid disease. In functional medicine, however, we recognize it as a cause of worsening thyroid function. This creates a self-perpetuating cycle that must be interrupted. If you do not fix the gut, you likely will not stabilize your thyroid labs.
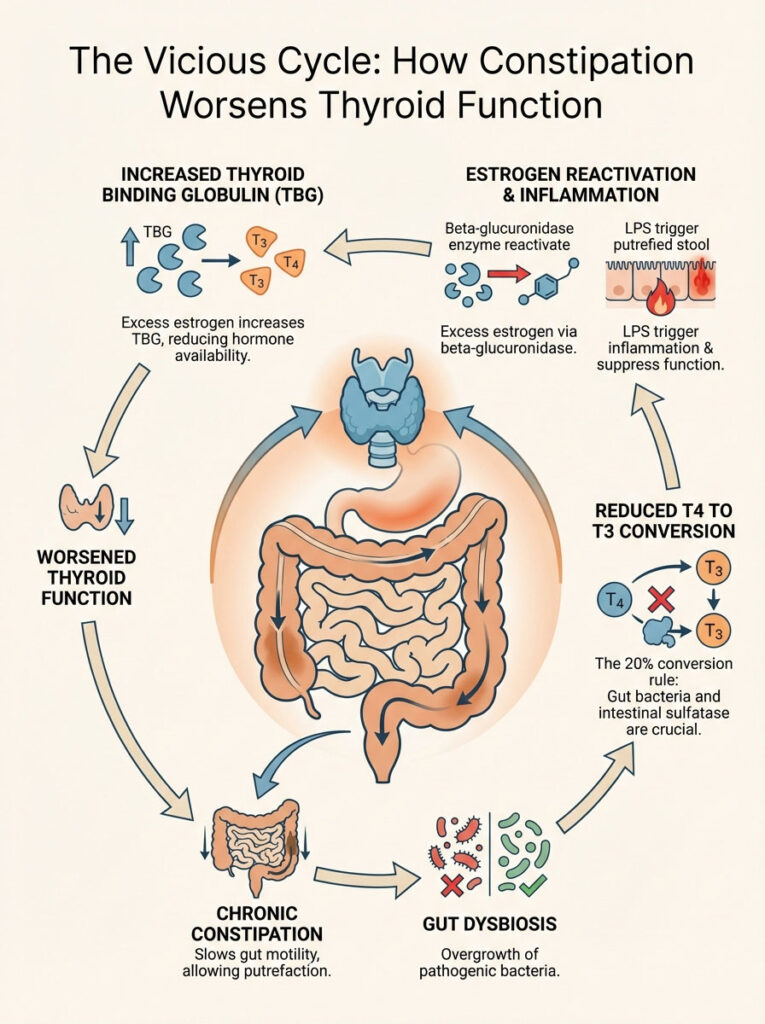
The 20% Conversion Rule
Your thyroid gland primarily produces T4 (Thyroxine). T4 is metabolically inactive. To feel energetic and have regular bowel movements, your body must convert T4 into T3. While the liver handles much of this, approximately 20% of this conversion takes place in the gut. This is facilitated by an enzyme called intestinal sulfatase.
This enzyme is produced by healthy gut bacteria. When you have chronic constipation, the microbiome changes. Beneficial bacteria die off. Pathogenic bacteria overgrow, creating a state called dysbiosis. These pathogenic bacteria damage the intestinal lining and fail to perform this conversion. Therefore, a slow gut leads to less active T3. Less active T3 leads to an even slower gut.
Estrogen Dominance and Beta-Glucuronidase
Constipation prevents the excretion of toxins and excess hormones. One specific enzyme produced by overgrown bacteria in a stagnant gut is beta-glucuronidase. This enzyme is troublesome. It reactivates estrogen that was tagged for excretion by the liver. It sends this estrogen back into the bloodstream.
Excess estrogen increases Thyroid Binding Globulin (TBG). TBG is a protein that binds to thyroid hormones like a magnet. When bound, the hormones are unavailable to your cells. This means your blood tests might look “normal,” but your tissues are starving for hormone. This perpetuates Hypothyroidism Constipation despite normal TSH levels.
Lipopolysaccharides (LPS) and Inflammation
When stool sits in the colon for too long, it putrefies. This allows gram-negative bacteria to proliferate. These bacteria have a cell wall component called Lipopolysaccharides, or LPS. LPS is highly toxic. In a constipated gut, the intestinal wall becomes permeable (Leaky Gut). LPS leaks into the bloodstream.
Once in the bloodstream, LPS triggers a massive immune response. This systemic inflammation suppresses the thyroid gland directly. It also interferes with the thyroid hormone receptors on your cells. Essentially, the toxins from your constipation are jamming the lock so the thyroid key cannot work.
The SIBO-Thyroid Connection: When Fiber Makes It Worse
If you have increased your fiber intake and felt significantly worse, pay attention. If you experience more bloating, gas, and pain, you likely do not have simple constipation. You likely have SIBO (Small Intestinal Bacterial Overgrowth). This condition is rampant among those with Hashimoto’s thyroiditis.
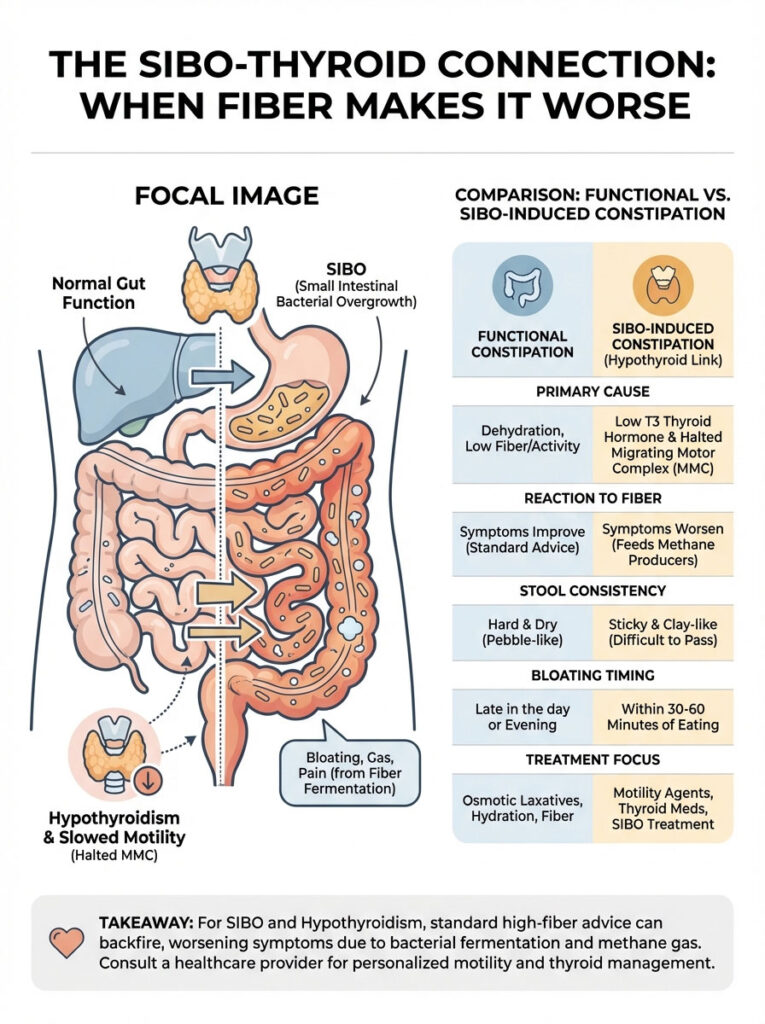
Because of the impaired Migrating Motor Complex (MMC) and low stomach acid, bacteria from the colon migrate upward. They move into the small intestine where they do not belong. When you eat fiber or prebiotics, you are feeding these misplaced bacteria. They ferment the fiber. This produces hydrogen and methane gas.
The Methane Factor
In hypothyroid patients, the overgrowth is often dominated by methanogens. These are archaea (single-celled organisms) that produce methane gas. Methane is not just an uncomfortable gas. It acts as a paralytic to the nerves of the gut. It freezes motility entirely.
This is why standard constipation advice fails. Fiber feeds the methane producers. The methane paralyzes the gut further. The constipation gets worse. Distinguishing between SIBO-induced constipation and functional constipation is vital for treatment.
Comparison: Standard vs. Thyroid/SIBO Constipation
| Feature | Functional Constipation | Thyroid/SIBO Constipation |
|---|---|---|
| Primary Cause | Dehydration, low fiber, sedentary behavior | Low T3, halted MMC, Hypochlorhydria |
| Reaction to Fiber | Symptoms improve; stool softens | Worsens bloating, gas, and pain immediately |
| Stool Consistency | Hard, dry, pebble-like | Can be hard, or sticky/clay-like; often alternating |
| Bloating Timing | Late in the day; progressive | Within 30-60 minutes of eating or upon waking |
| Treatment Focus | Osmotic laxatives, hydration | Motility agents (prokinetics), gut repair, thyroid meds |
The Gallbladder Connection: The Missing Link
You cannot discuss Hypothyroidism Constipation without discussing the liver and gallbladder. The liver filters toxins and produces bile. The gallbladder stores this bile and releases it when you eat fat. Bile acts as a natural detergent for the gut.
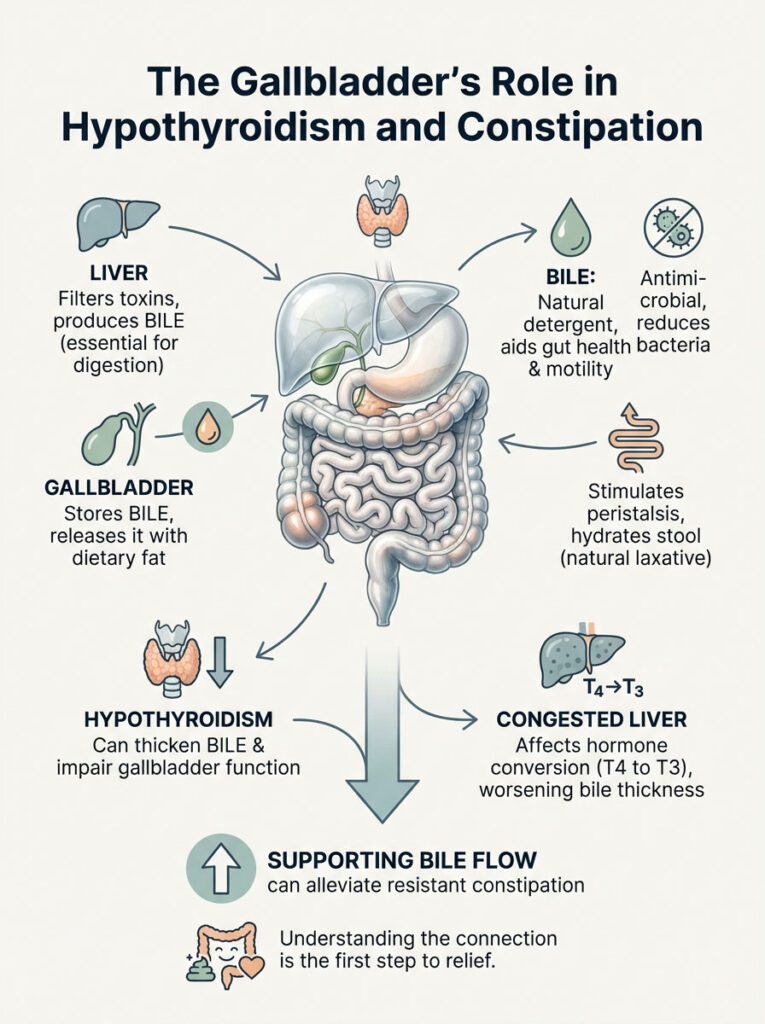
Bile serves two critical functions for motility. First, it is antimicrobial. It keeps bacteria levels in the small intestine low. Second, bile acids are a natural laxative. They irritate the lining of the colon slightly, which stimulates peristalsis and hydration of the stool.
Hypothyroidism thickens the bile. It makes the Sphincter of Oddi (the valve that releases bile) tight and sluggish. If bile does not flow, the gut does not move. Furthermore, the conversion of T4 to T3 is heavily dependent on liver function. A congested liver results in poor conversion, lowering T3, and thickening the bile further. Supporting bile flow is often the breakthrough for resistant constipation.
Strategic Dietary Interventions for the Hypothyroid Gut
Fixing slow gut motility requires a nuanced approach to diet. We cannot simply load up on roughage. We must respect the delicate state of the inflamed intestine. The goal is nourishment without irritation.

The “Right” Fiber Strategy
For patients with thyroid gut issues, insoluble fiber can be problematic. Sources like bran, raw kale, and seeds can act like sandpaper on an inflamed gut lining. They add bulk but do not soothe the inflammation. Instead, we focus on specific soluble fibers. These regulate stool without causing excessive fermentation.
Partially Hydrolyzed Guar Gum (PHGG) is a clinically validated fiber source. It is generally well-tolerated even by SIBO patients. It helps bulk the stool and feeds beneficial bacteria. It does this without the explosive gas production associated with inulin or chicory root. Cooked vegetables like carrots, squash, and zucchini are preferable to raw salads until motility is restored.
Hydration and Electrolytes
Water is not enough. For the smooth muscles of the colon to contract, they require electrolytes. Specifically, they need potassium, sodium, and magnesium. These minerals facilitate the electrical signals of the nervous system. Adrenal dysfunction often accompanies Hashimoto’s thyroiditis. This causes the body to dump minerals through urine.
I recommend adding sea salt or a clean electrolyte powder to your water. Cellular dehydration prevents the colon from remaining lubricated. This happens regardless of how much plain water you drink. If your urine is clear but you are still thirsty or constipated, you are likely electrolyte deficient.
Meal Spacing for MMC Activation
This is the most actionable tip you can start today. To fix Hypothyroidism Constipation, you must allow the Migrating Motor Complex (MMC) to run. This means stopping the habit of “grazing.” Do not eat six small meals a day.
Aim for a 4 to 5-hour gap between meals. During this gap, have zero caloric intake. Water or black tea is fine. This fasting window signals the gut that digestion is complete. It triggers the cleaning wave that pushes debris into the colon. If you snack two hours after lunch, you reset the clock. The sweeper never comes. The debris stays put.
The Problem with Goitrogens
There is much debate about goitrogens. These are compounds found in cruciferous vegetables like broccoli, cauliflower, and kale. They can interfere with iodine uptake in the thyroid. For most people, they are healthy. However, for a patient with a slow gut, raw cruciferous vegetables are hard to digest.
They contain raffinose, a complex sugar that causes gas. If your motility is slow, that gas gets trapped. This leads to painful distension. Always cook your cruciferous vegetables. Steaming or roasting breaks down the goitrogens and the tough fibers. This makes them safer for your thyroid and your gut.
Medical and Supplement Protocols: Fixing the Flow
While diet is foundational, the hypothyroid gut often needs a “kickstart.” We use targeted supplementation and medication adjustments to restore the rhythm.
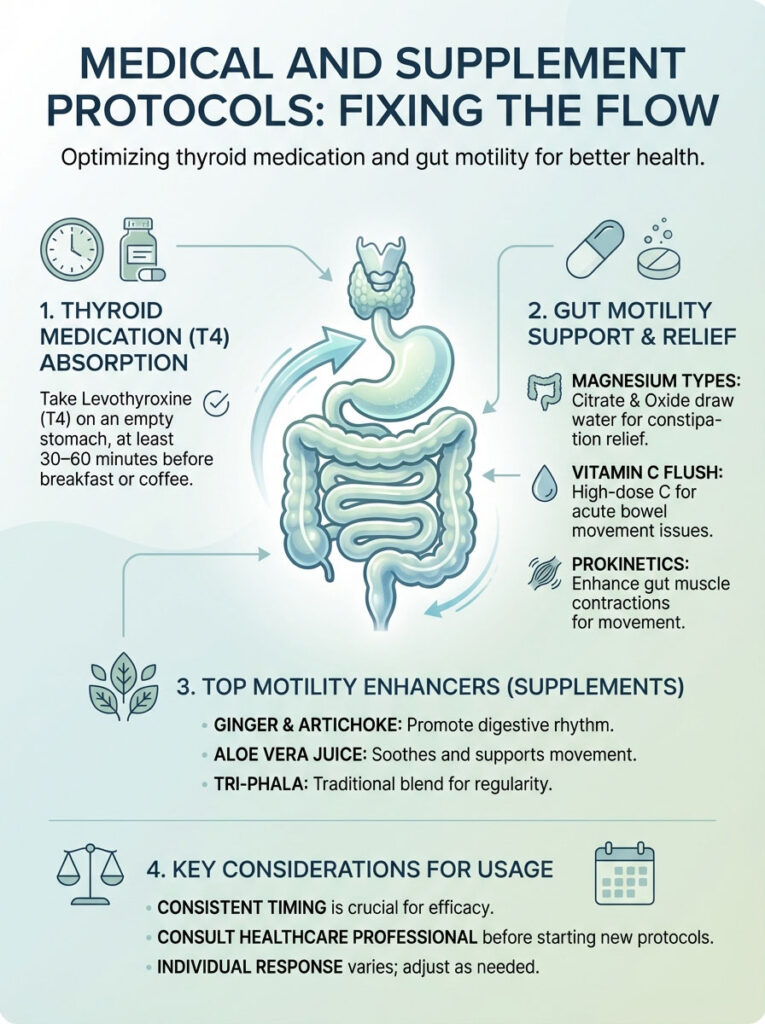
Optimizing Thyroid Medication
If you are taking Levothyroxine (T4), its absorption is highly dependent on gut acidity. Many patients take their medication with coffee. Or they take it too close to breakfast. The rule is strict. Take medication with water at least 60 minutes before food or coffee. Take it 4 hours away from calcium or iron supplements.
If gut issues persist, ask your doctor about soft gel capsules or liquid thyroxine formulations. These are easier to absorb for those with slow gastric motility. They contain fewer fillers like gluten or lactose that might trigger inflammation. If you are not absorbing your medication, you will never break the constipation cycle.
Magnesium: The Gold Standard
Magnesium is non-negotiable for thyroid patients. It serves a dual purpose. It is a cofactor for the enzymes that make thyroid hormone. It also relaxes the bowel to allow for easy passage of stool. However, the type matters significantly.
Magnesium Glycinate is excellent for sleep and anxiety. But it has a minimal laxative effect. For constipation, Magnesium Citrate or Magnesium Oxide are preferred. They are osmotic. They draw water into the bowel to soften the stool. I typically recommend dosing to “bowel tolerance.” Increase the dose nightly until a loose stool occurs. Then back off slightly.
Vitamin C Flush
For acute cases where the bowel has not moved in days, a Vitamin C flush can be effective. High doses of Vitamin C are not fully absorbed by the body. The excess remains in the gut and attracts water. This triggers a strong bowel movement. It is a safe, non-habit-forming way to clear the colon while providing antioxidant support.
Prokinetics (Motility Agents)
Prokinetics are substances that stimulate the Migrating Motor Complex (MMC). They are distinct from laxatives. They do not cause diarrhea. Instead, they coordinate the wave-like contractions in the small intestine.
- Ginger Root: A powerful natural prokinetic. High-dose ginger extract taken between meals can stimulate gastric emptying.
- Artichoke Extract: Works synergistically with ginger. It stimulates bile flow and motility in the small intestine.
- 5-HTP: A precursor to serotonin. Most serotonin is made in the gut and triggers motility.
- Prescription Options: Low Dose Naltrexone (LDN) or Low Dose Erythromycin are often used off-label in functional medicine. They help restore motility in resistant SIBO cases.
Top Supplements for Thyroid Motility
| Supplement | Mechanism of Action | Best Time to Take | Clinical Note |
|---|---|---|---|
| Magnesium Citrate | Osmotic; draws water into the colon | Before bed | Best for immediate relief of hard stool |
| Ginger Root | Prokinetic; stimulates gastric emptying | Between meals or with food | Helps reduce nausea and MMC stagnation |
| Betaine HCL | Acidifier; improves protein digestion | Middle of meal | Do not use if you have ulcers or gastritis |
| Vitamin C | Osmotic flush (high dose) | Morning | Can cause loose stools if tolerance exceeded |
| Spore Probiotics | Microbiome modulation | With food | Better tolerated in SIBO than Lactobacillus |
The Gut-Brain Axis: Vagus Nerve Stimulation
The connection between the brain and the gut is physical. It is called the Vagus nerve. This nerve travels from the brainstem down to the colon. It is responsible for the “Rest and Digest” state. This is the parasympathetic nervous system.
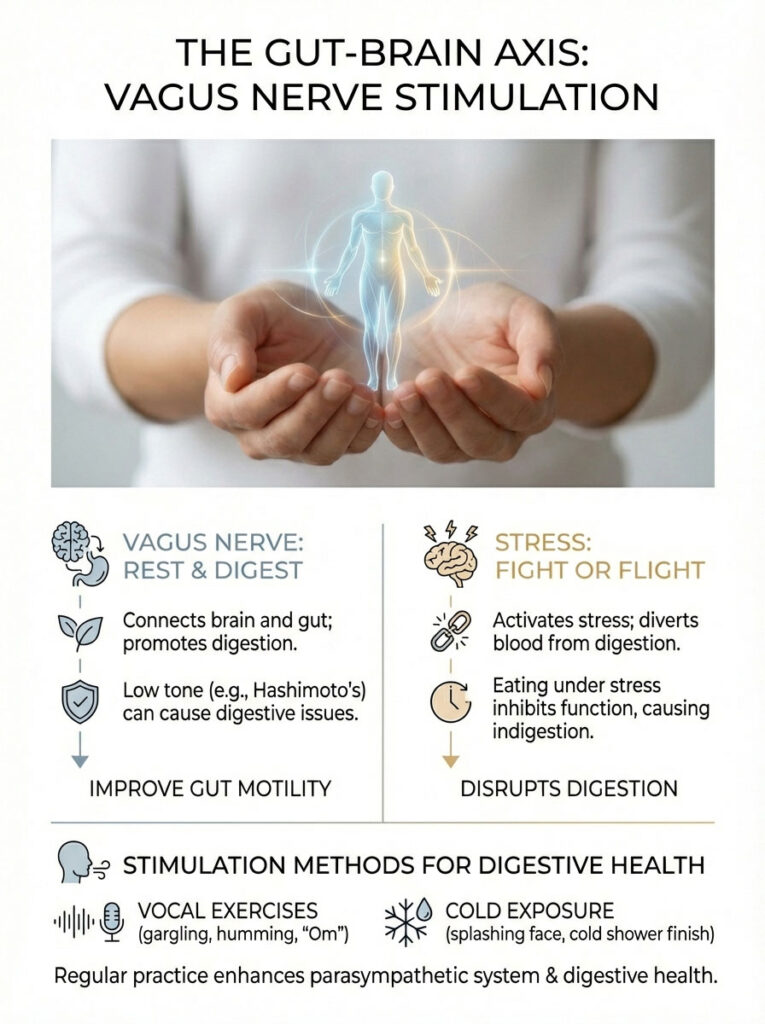
In patients with Hashimoto’s thyroiditis, chronic inflammation and stress often result in low vagal tone. When the Vagus nerve is dormant, the signals to produce stomach acid are blocked. The release of enzymes is halted. The contraction of the colon stops. You can take all the supplements in the world. But if the Vagus nerve is not firing, the gut will remain sluggish.
Stress and Peristalsis
When you are stressed, your body enters “Fight or Flight” mode. Blood is shunted away from the digestive organs and toward the limbs. Digestion effectively shuts down. Many patients eat while driving, working, or watching stressful news. This guarantees that the Vagus nerve remains inactive. Eating in a state of stress is a primary cause of indigestion and stagnation.
Expert Insight: Toning the Vagus Nerve
You can physically stimulate the Vagus nerve to improve slow gut motility. Since the nerve passes through the vocal cords, exercises involving vibration work well. Loud gargling with water, humming, or chanting “Om” create vibrations that stimulate the nerve. I prescribe my patients to gargle water aggressively for 2 minutes twice a day. It sounds simple, but it activates the parasympathetic nervous system needed for digestion.
Cold Exposure
Another way to stimulate the Vagus nerve is through acute cold exposure. Splashing freezing cold water on your face for 30 seconds can reset the nervous system. Ending your shower with 30 seconds of cold water also works. This shock triggers a parasympathetic rebound, which can help stimulate bowel activity.
Testing: Don’t Guess, Check
If you are struggling with Hypothyroidism Constipation, relying solely on TSH tests is insufficient. You need a comprehensive picture of what is happening inside the gut and the thyroid.
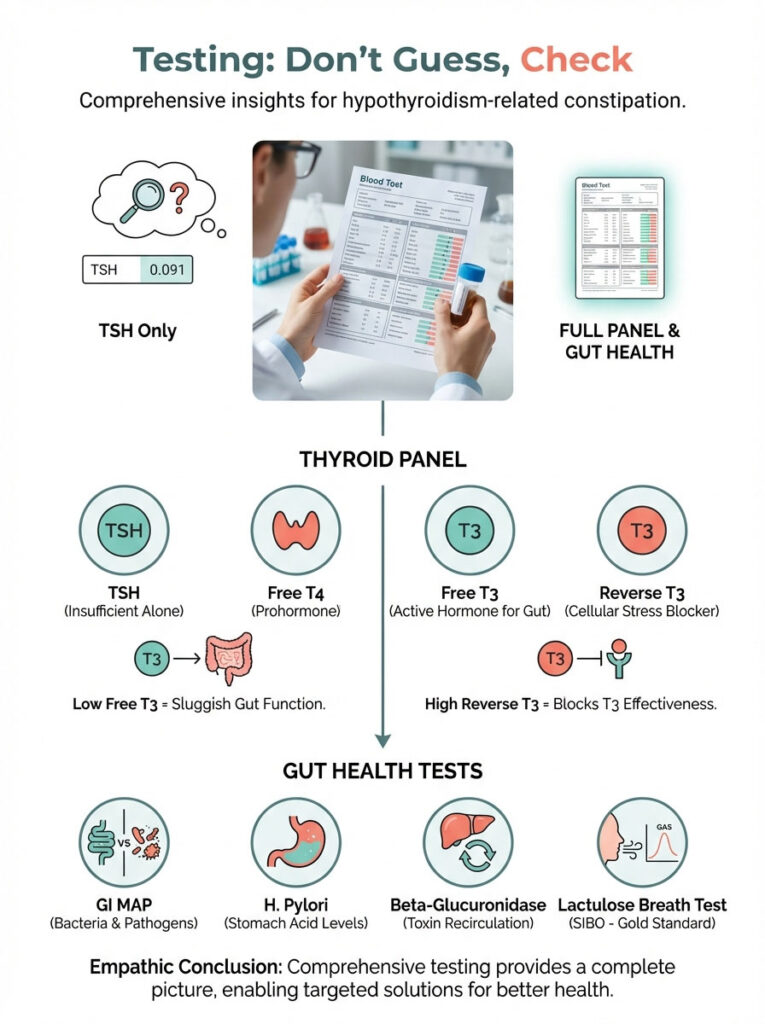
The Complete Thyroid Panel
You must request a full panel. This includes Free T3, Free T4, and Reverse T3. If your Free T3 is in the bottom 25% of the reference range, you do not have enough active hormone to move the gut. If Reverse T3 is high, you are in a state of cellular stress. Your body is actively blocking T3 from working.
GI MAP Stool Test
A functional stool test, like the GI MAP, looks for DNA markers of specific bacteria. It can reveal if you have low levels of beneficial bacteria. It checks for pathogens like H. Pylori, which lowers stomach acid. It also measures Beta-Glucuronidase levels, confirming if you are recirculating estrogen and toxins.
SIBO Breath Test
If you have the bloating symptoms described earlier, a lactulose breath test is the gold standard. It measures hydrogen and methane gases over a 3-hour period. If methane is elevated, we know that methanogens are paralyzing your gut. The treatment plan then shifts to targeting these specific organisms.
A Daily Routine for Regularity (The “Perfect Day” Protocol)
Overcoming Hypothyroidism Constipation requires consistency. Random interventions yield random results. Here is a sample protocol designed to optimize hormones, acid, and motility.

- 7:00 AM: Wake up. Take thyroid medication with a full glass of water. Wait 60 minutes before eating or drinking coffee.
- 7:30 AM: Vagus nerve exercises. Gargle water aggressively. Splash cold water on your face.
- 8:00 AM: Breakfast. High protein (eggs or collagen smoothie). Moderate healthy fat. Take Betaine HCL (if prescribed) in the middle of the meal.
- 12:30 PM: Lunch. Cooked vegetables, lean protein. No snacking since breakfast. This allows the Migrating Motor Complex (MMC) to run.
- 1:00 PM: Ginger tea or Ginger supplement to stimulate digestion.
- 4:00 PM: Hydration check. Drink electrolyte water. Do not snack.
- 6:30 PM: Dinner. Smaller meal. Soups or stews are best as they are pre-digested. Avoid raw salads at night.
- 9:00 PM: Magnesium Citrate powder in warm water. This relaxes the nervous system. It draws water into the bowel for the next morning.
Summary & Key Takeaways
Resolving Hypothyroidism Constipation is rarely as simple as drinking more water. It is a complex interplay of hormonal signaling, neurological health, and microbiome balance. The “slow gut” is a direct result of low T3 affecting the Enteric Nervous System. This is compounded by a dormant Migrating Motor Complex (MMC) and low stomach acid.
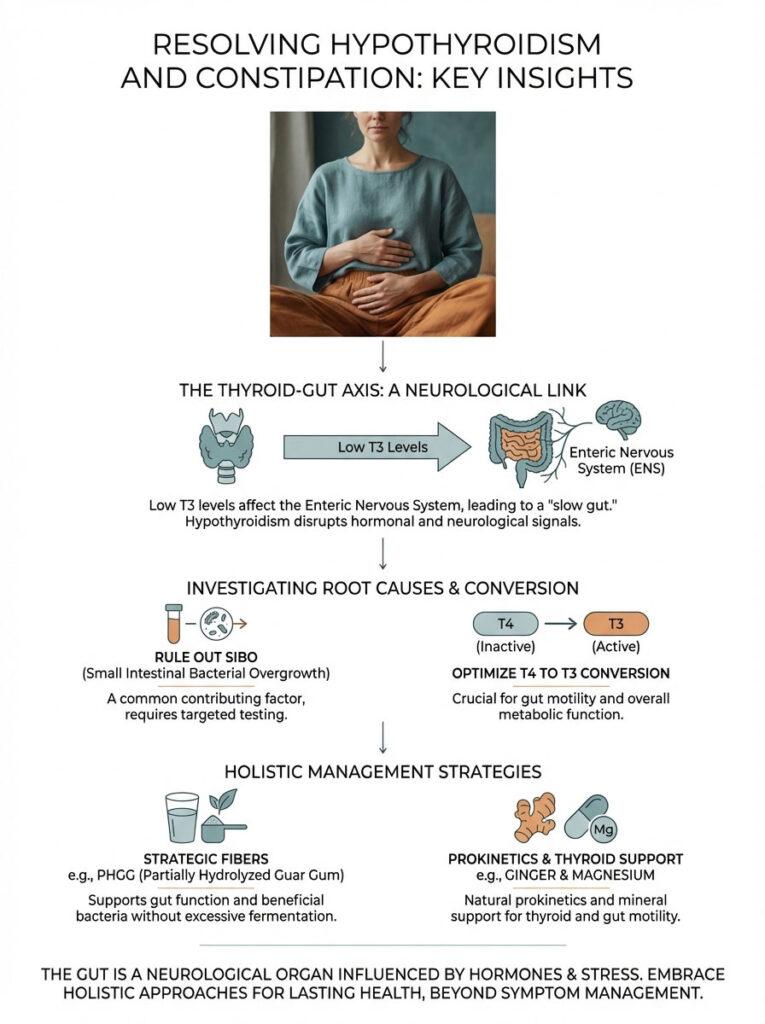
To heal, we must move beyond symptom management. We must optimize T4 to T3 conversion. We must rule out SIBO. We must use strategic fibers like PHGG. We must employ prokinetics like ginger and Magnesium for thyroid support. By addressing these root causes, you not only restore regularity but also improve the absorption of your thyroid medication. This creates a positive spiral toward better health.
Remember, your gut is not just a plumbing system. It is a neurological organ that responds to hormones, stress, and timing. Treat it with the respect it deserves, and it will begin to move again.
Frequently Asked Questions
What is the main difference between a PET scan and a standard CT scan?
A standard CT scan focuses on anatomical structures like bones and organs, while a PET scan evaluates cellular metabolism and function. By fusing these modalities, PET CT provides a dual-layer map that shows both where a lesion is located and whether it is biologically active. This allows us to distinguish between active disease and benign scar tissue that might look identical on a regular CT.
Why do I need to fast for six hours before my PET CT imaging?
Fasting is essential to lower your blood insulin levels, ensuring the 18F-FDG radiotracer is absorbed by glucose-hungry cancer cells rather than your muscles. If you eat before the scan, insulin will drive the tracer into your skeletal muscles, creating “background noise” that can hide tumors. Maintaining a fasting state for at least 6 hours ensures the highest diagnostic sensitivity.
What does a high Standardized Uptake Value (SUV) mean on a PET report?
The Standardized Uptake Value (SUV) is a semi-quantitative metric used to measure the intensity of radiotracer accumulation in a specific area. While a higher SUV often correlates with more aggressive metabolic activity, it must be interpreted in context, as inflammation or infection can also cause elevated values. We compare these numbers against background activity in the liver or blood pool to determine the clinical significance of a “hot spot.”
How does the Warburg Effect explain why cancer shows up on a PET scan?
The Warburg Effect refers to the phenomenon where cancer cells consume glucose at a significantly higher rate than normal cells to fuel rapid division. Since our primary radiotracer, 18F-FDG, is a sugar analog, these hypermetabolic cells “greedily” take up the radioactive tracer. This allows the PET scanner to detect biochemical changes in the body long before structural changes appear on an X-ray or CT.
Can I exercise the day before my PET CT scan?
Physical activity must be avoided for 24 hours prior to your scan because muscle repair requires significant glucose consumption. Strenuous exercise can cause “muscle uptake,” where the radiotracer accumulates in the legs, arms, or torso instead of the areas we need to evaluate. This metabolic distraction can obscure small tumors and lead to a non-diagnostic or misinterpreted study.
How should diabetic patients prepare for a PET CT scan?
Diabetic patients require careful management because high blood glucose levels compete with the 18F-FDG tracer for entry into cells. Generally, we aim for a blood sugar level below 200 mg/dL and advise against taking short-acting insulin within four hours of the injection. We typically schedule these appointments for early morning to better manage fasting requirements and medication timing.
What is the purpose of the 60-minute uptake phase after the radiotracer injection?
The 60-minute uptake phase allows the 18F-FDG radiotracer to circulate through your bloodstream and be fully absorbed by tissues with high metabolic activity. During this hour, you must remain perfectly still and quiet to prevent the tracer from accumulating in active muscles or brain regions used for talking or reading. This resting period is critical for ensuring that the final images are sharp and free of physiological artifacts.
How is PET CT used to determine if chemotherapy is actually working?
PET CT imaging is superior to standard CT for monitoring treatment because it detects “metabolic shutdown” before a tumor actually shrinks in size. Using PERCIST criteria, we can see if a tumor has stopped consuming sugar after just a few cycles of chemotherapy. This real-time feedback allows oncologists to either proceed with effective treatment or pivot to a different drug if the cancer remains metabolically active.
What are the specific benefits of PSMA PET scans for prostate cancer patients?
PSMA PET imaging uses specialized tracers that bind to the Prostate-Specific Membrane Antigen protein found on the surface of prostate cancer cells. This technology is far more sensitive than traditional bone scans or CTs, allowing us to detect microscopic recurrences at very low PSA levels. It is a game-changer for staging and localized treatment planning in patients with biochemical recurrence.
Is the radiation exposure from a PET CT scan dangerous?
The effective radiation dose from a PET CT scan typically ranges from 10 to 25 mSv, which combines the exposure from the radiotracer and the CT component. While this is higher than a standard X-ray, we follow the ALARA (As Low As Reasonably Achievable) principle to minimize exposure while ensuring diagnostic quality. In most oncologic cases, the life-saving information gained from accurate staging far outweighs the theoretical risks of the radiation dose.
How does PET imaging help differentiate between types of dementia like Alzheimer’s?
In neurology, PET scans identify specific patterns of “hypometabolism,” or reduced sugar usage, in different regions of the brain. Alzheimer’s disease typically shows low activity in the temporal and parietal lobes, whereas Frontotemporal Dementia affects the frontal lobes. These metabolic signatures help clinicians provide an accurate diagnosis when clinical symptoms and MRI findings are inconclusive.
What is Theranostics and how does it relate to nuclear medicine imaging?
Theranostics is an emerging field that combines “therapy” and “diagnostics” by using the same molecular target for both imaging and treatment. We first use a diagnostic radiotracer to “see” the tumor, and if it lights up, we switch the isotope to a therapeutic one that delivers targeted radiation directly to the cancer cells. This “search and destroy” approach represents the pinnacle of personalized nuclear medicine.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Hypothyroidism and digestive disorders are complex conditions that require professional diagnosis and management. Always consult a qualified healthcare professional or endocrinologist before starting new supplements, changing medications, or making significant dietary changes.
References
- The Journal of Clinical Endocrinology & Metabolism – “Thyroid Hormone Action on the Gut” – Research detailing how T3 binds to smooth muscle receptors in the intestines to regulate motility.
- American Thyroid Association (ATA) – official thyroid guidelines – Documentation on the systemic effects of hypothyroidism on the Basal Metabolic Rate and digestion.
- Frontiers in Endocrinology – “The Thyroid-Gut Axis” – A comprehensive review of the bidirectional relationship between the microbiome and thyroid hormone conversion.
- World Journal of Gastroenterology – “Small Intestinal Bacterial Overgrowth in Hypothyroidism” – Statistical data showing the 54% prevalence of SIBO in hypothyroid patients.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – “Your Digestive System and How it Works” – Background information on the Migrating Motor Complex and peristalsis.
- Journal of Clinical Medicine – “The Role of Magnesium in Thyroid Function” – Clinical insights into magnesium as a cofactor for thyroid enzymes and its osmotic effect on the bowel.
- British Journal of Pharmacology – “Prokinetics and Gut Motility” – Study on the mechanisms of ginger and artichoke extracts in stimulating the MMC.