Can Hypothyroidism Affect Fertility?
Hypothyroidism & Fertility are deeply connected through the metabolic regulation of the reproductive system. While standard medical guidelines consider a TSH level up to 4.5 mIU/L normal, clinical fertility guidelines from the American Thyroid Association (ATA) recommend a TSH level below 2.5 mIU/L for conception. Optimizing thyroid function is vital to ensure regular ovulation, support proper implantation, and reduce the risk of early miscarriage.
Table of Contents
You have likely sat in a doctor’s office, staring at a lab report that says “Normal,” yet you feel anything but normal. You are tired. Your cycles are slightly off. Your hands are cold. Despite months of trying, that second line on the pregnancy test refuses to appear.
This is a scenario I see constantly in my practice as a Reproductive Endocrinologist. The intersection of Hypothyroidism & Fertility is one of the most misunderstood areas of reproductive medicine. The definition of “normal” changes entirely when the goal shifts from general survival to creating a new life.
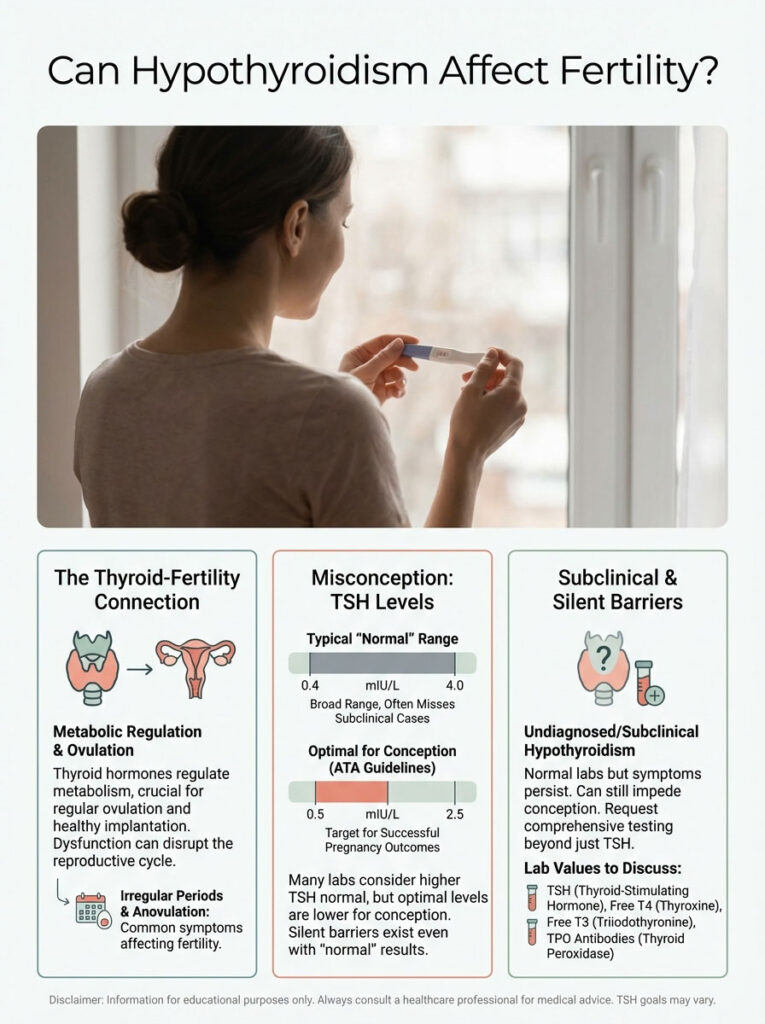
The thyroid is the metabolic thermostat of the body. When it runs low, every system slows down. This includes your reproductive system. For millions of women in the USA, undiagnosed or “subclinical” hypothyroidism is the silent barrier preventing conception.
The frustration is palpable. General practitioners are trained to treat thyroid disease only when it becomes severe. However, to get pregnant and stay pregnant, we need optimal levels. We do not just want acceptable ones.
In this comprehensive guide, we will examine the biological mechanisms at play. We will discuss the specific lab values you need to request. Finally, we will outline the exact protocols used in fertility clinics to help patients succeed in getting pregnant with hypothyroidism.
Key Statistics: Thyroid Health & Reproduction
- 2.5 mIU/L: The upper limit for TSH recommended by the American Thyroid Association for the first trimester.
- 2-3x Higher Risk: The increased likelihood of miscarriage in women with untreated thyroid antibodies (Hashimoto’s).
- 50% Increase: The dosage adjustment often required for levothyroxine immediately upon a positive pregnancy test.
- 2.3% to 10%: The estimated prevalence of hypothyroidism in women of reproductive age.
- 69%: The percentage of women with subclinical hypothyroidism who may have ovulatory dysfunction.
- 4-6 Weeks: The typical time required to stabilize TSH levels after starting medication.
The Biology: How the Thyroid Controls Your Ovaries
To understand why Hypothyroidism & Fertility are so tightly linked, we must look at the body’s control center: the brain. The thyroid does not operate in a vacuum. It is part of a complex feedback loop known as the Hypothalamic-Pituitary-Thyroid (HPT) axis.
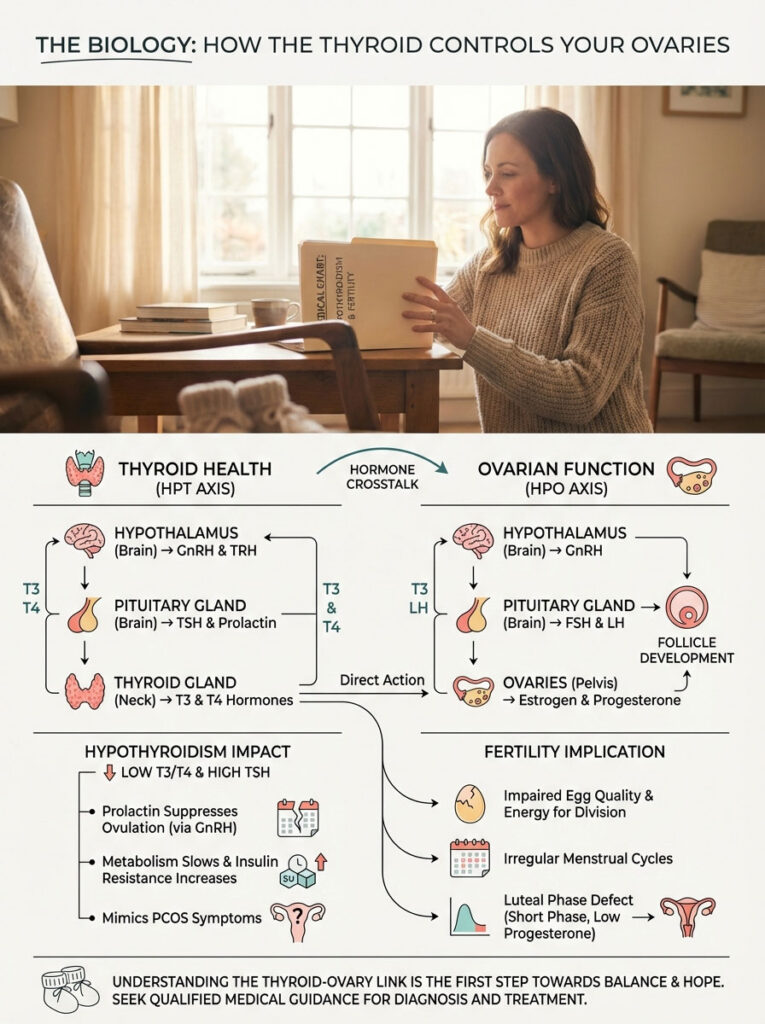
This system is in constant communication with the Hypothalamic-Pituitary-Ovarian (HPO) axis. They are like two different departments in the same company. If one department fails, the other cannot do its job.
Thyroid hormone receptors are not just found in the liver or heart. They are located directly on your oocytes (eggs). They are also found on the granulosa cells that surround the eggs. These cells require significant energy to mature an egg and prepare it for release.
When thyroid hormone levels are low, the mitochondria (power plants) within the egg cells cannot function efficiently. This leads to poor egg quality. It can also result in embryos that lack the energy to divide properly.
The Prolactin Connection (The TRH Mechanism)
One of the most direct ways hypothyroidism stops ovulation is through a hormone called Prolactin. Here is the mechanism:
- When your body detects low Thyroxine (T4), the hypothalamus releases Thyrotropin-Releasing Hormone (TRH).
- TRH screams at the pituitary gland to work harder.
- TRH stimulates the release of TSH (Thyroid Stimulating Hormone).
- However, TRH is a messy signal. It also stimulates the pituitary to release Prolactin.
High levels of prolactin (hyperprolactinemia) tell the body you are currently breastfeeding. This naturally suppresses GnRH (Gonadotropin-Releasing Hormone). Without GnRH, you do not ovulate.
This is why many women with untreated hypothyroidism have irregular periods. Some stop cycling altogether. Correcting the thyroid often fixes the prolactin issue without needing separate medication.
Impact on the Luteal Phase
Even if you are ovulating, Hypothyroidism & Fertility issues can manifest in the second half of your cycle. This is known as the luteal phase. We call this a Luteal Phase Defect (LPD).
After ovulation, the empty follicle becomes the corpus luteum. This structure must pump out progesterone to hold the uterine lining in place. Thyroid hormones are required for the corpus luteum to form correctly.
In hypothyroid patients, we often see the corpus luteum fail prematurely. This leads to a short luteal phase (less than 10 days). It can also cause low progesterone levels. The result? The embryo tries to implant, but the lining sheds too early. This appears as a “chemical pregnancy” or a very early miscarriage.
Expert Insight: The Metabolic Impact
Low thyroid function often travels with insulin resistance. Hypothyroidism decreases the production of Sex Hormone Binding Globulin (SHBG). Low SHBG can lead to higher levels of free testosterone and estrogen dominance. This creates a hormonal environment very similar to PCOS (Polycystic Ovary Syndrome).
Diagnosis: Beyond the Basic TSH
If you are struggling with Hypothyroidism & Fertility, a simple TSH test is insufficient. TSH is a pituitary hormone. It is not a thyroid hormone. It reflects the brain’s opinion of the thyroid environment.
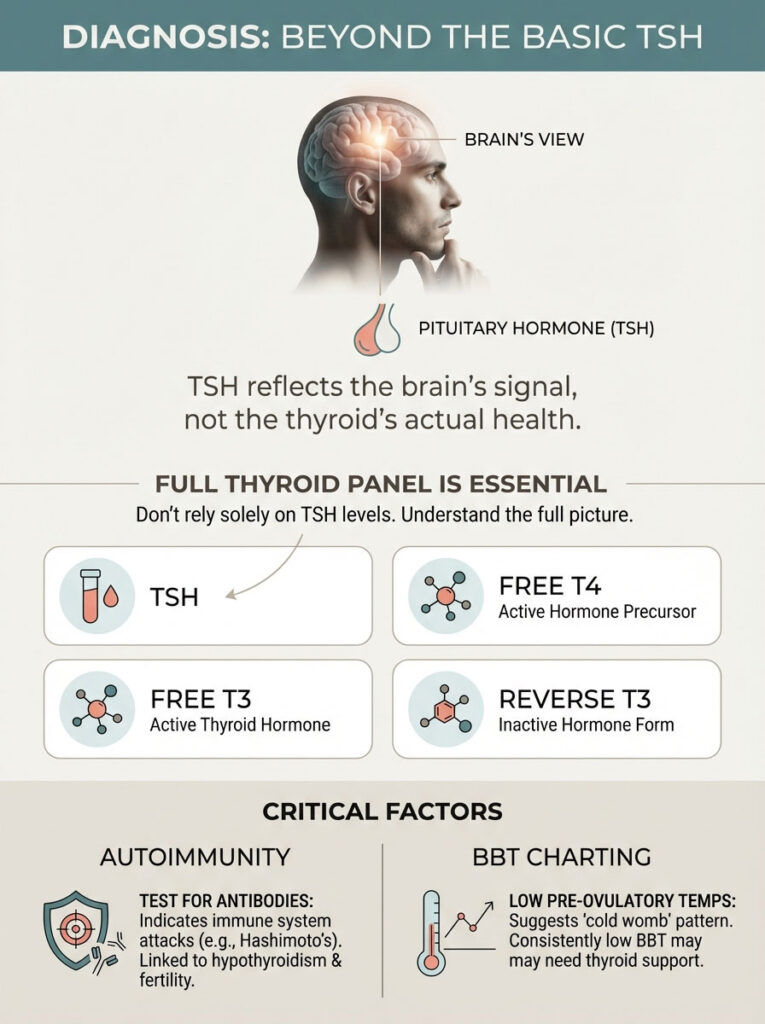
It does not tell us the whole story. In my practice, I see patients with a “normal” TSH of 3.5 mIU/L who are exhausted and infertile. Their actual thyroid hormones (T3 and T4) are often suboptimal.
To get a clear picture, you must advocate for a full thyroid panel. Do not settle for just TSH.
The Full Thyroid Panel (What to Ask For)
TSH (Thyroid Stimulating Hormone): The messenger. High levels mean your brain is screaming at your thyroid to work harder. In fertility, we want this quiet and calm.
Free T4 (Thyroxine): The storage hormone. This is what the gland produces. It must be converted into active hormone. We want this in the upper half of the range.
Free T3 (Triiodothyronine): The active hormone. This is what actually enters the cells and boosts metabolism. Low levels here indicate a conversion problem.
Reverse T3: The “brake” pedal. Sometimes the body converts T4 into Reverse T3 to conserve energy during stress. This blocks the active T3 from working. High stress often leads to high Reverse T3.
The Autoimmune Component
You cannot discuss Hypothyroidism and Fertility without addressing autoimmunity. The vast majority of hypothyroidism in the USA is caused by Hashimoto’s Thyroiditis. You need to test for:
- Anti-TPO (Thyroperoxidase Antibodies): The primary marker for Hashimoto’s.
- Anti-Tg (Thyroglobulin Antibodies): A secondary marker.
If these antibodies are present, your immune system is attacking the thyroid. This matters for fertility. A hyper-vigilant immune system may also attack a developing embryo.
Basal Body Temperature (BBT) Charting
Before advanced labs, we used temperature. BBT charting is a fantastic, low-cost diagnostic tool. Thyroid hormones regulate basal metabolic rate and heat generation.
In women with hypothyroidism, we often see a “cold womb” pattern. This presents as consistently low pre-ovulatory temperatures (below 97.0°F). You might also see a slow, sluggish rise after ovulation. If your chart looks rocky or consistently low, it is a strong bio-marker that your thyroid needs support.
The “Normal” vs. “Optimal” Debate: A Guide to TSH Levels
This is where the confusion lies for most patients. There is a massive difference between “reference range” and “functional range.” Understanding this distinction is key to success.
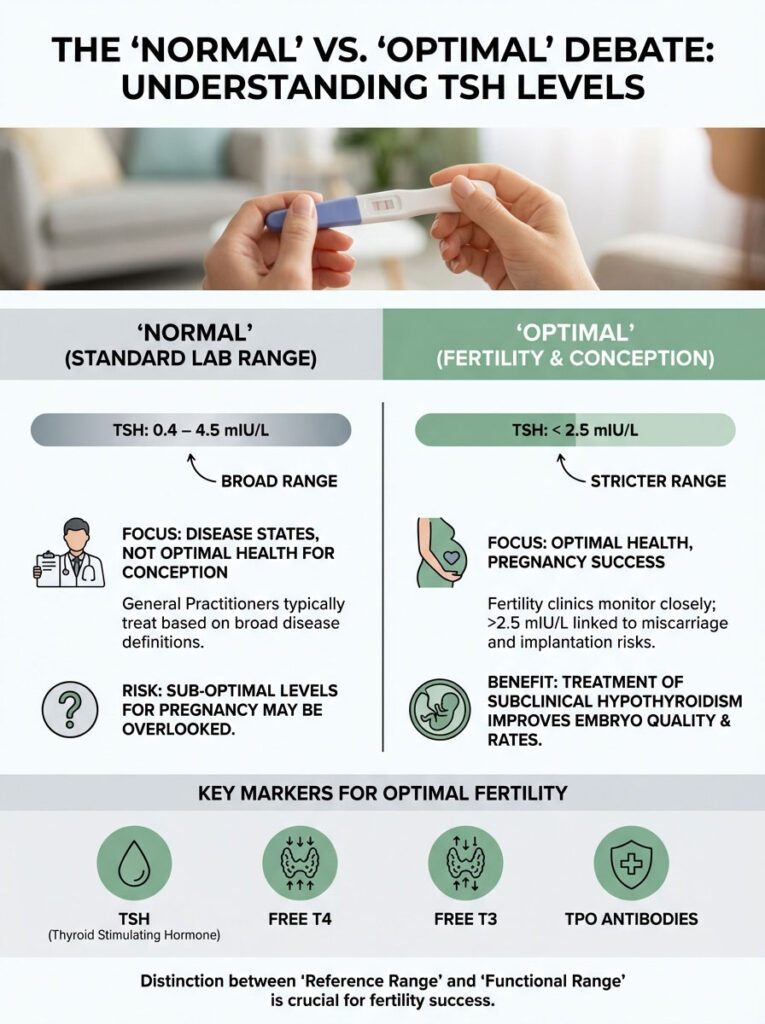
General Medicine vs. Reproductive Endocrinology
Standard lab reference ranges are based on a bell curve. They are derived from the population visiting that lab. Since many sick people visit labs, the “normal” range is quite wide. It is typically 0.4 to 4.5 mIU/L.
A General Practitioner will look at a TSH of 4.2 and say, “You are fine.” They are looking for disease states that threaten your life. They are not looking for optimal states that support new life.
However, TSH levels for pregnancy must be tighter. The American Society for Reproductive Medicine (ASRM) and the American Thyroid Association (ATA) have recognized the risks. TSH levels above 2.5 mIU/L are associated with lower implantation rates. They are also linked to higher miscarriage risks.
Subclinical Hypothyroidism (SCH)
Subclinical Hypothyroidism is defined as an elevated TSH with a normal Free T4. The TSH is usually > 2.5 or > 4.0 depending on the guideline. In a non-pregnant person, we might just watch this.
In a woman trying to conceive, we treat it. Studies have demonstrated clear benefits. When women with SCH are treated with levothyroxine to bring TSH below 2.5 mIU/L, embryo quality improves. Pregnancy rates increase.
This is why TSH levels for pregnancy are strictly monitored in fertility clinics. We do not take chances with sub-optimal levels.
| Marker | Standard Lab Reference Range | Optimal Fertility Target | Clinical Implication for Conception |
|---|---|---|---|
| TSH | 0.4 – 4.5 mIU/L | 0.5 – 2.5 mIU/L | TSH > 2.5 is linked to 2x miscarriage risk and implantation failure. |
| Free T4 | 0.8 – 1.8 ng/dL | 1.0 – 1.5 ng/dL | Must be in the upper half of the range to ensure adequate fetal supply. |
| Free T3 | 2.3 – 4.2 pg/mL | 3.2 – 4.0 pg/mL | Low T3 indicates poor conversion; leads to ovarian fatigue and poor egg quality. |
| TPO Antibodies | < 9 IU/mL (varies by lab) | 0 (Negative) | Presence indicates Hashimoto’s; increases risk of immune rejection of embryo. |
Hashimoto’s Thyroiditis: Autoimmunity and Implantation
Hashimoto’s thyroiditis fertility issues are distinct from simple hypothyroidism. Hashimoto’s is an immune disease. The thyroid destruction is just the symptom. The immune system is the cause.
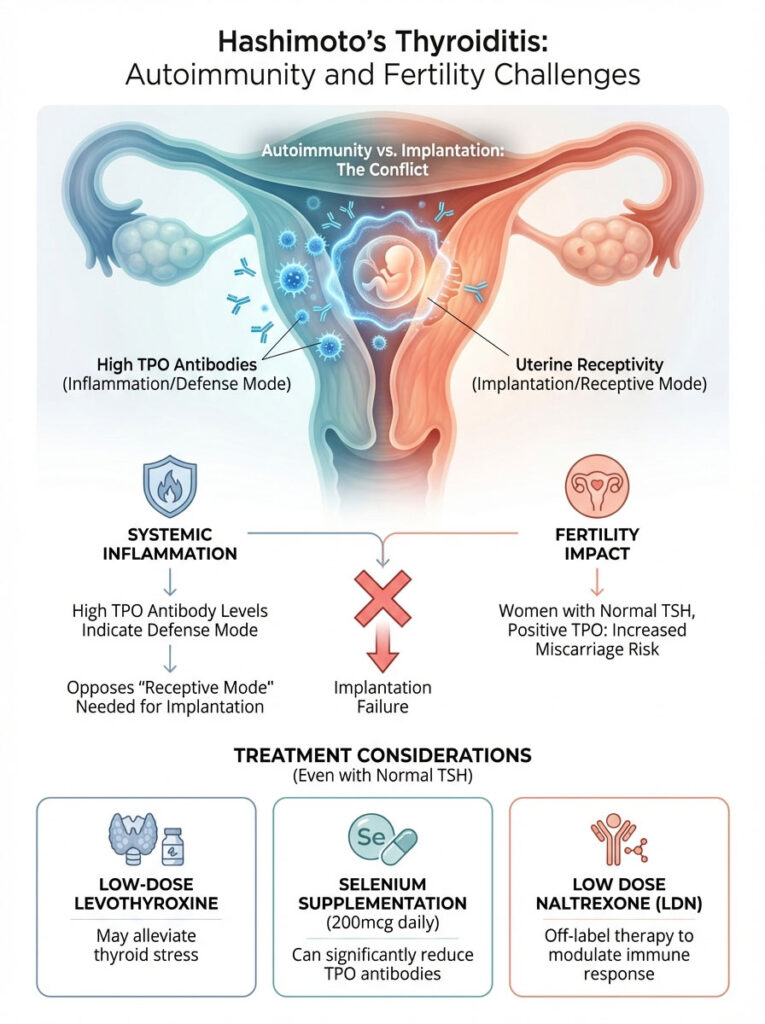
The Miscarriage Link
Reproductive Immunology is a growing field. It studies how the mother’s immune system tolerates the “foreign” DNA of the fetus. High levels of TPO antibodies indicate a systemic state of inflammation.
These antibodies create a pro-inflammatory cytokine environment in the uterus. Research indicates that women who are “euthyroid” (normal TSH) but test positive for TPO antibodies have a higher risk. They face a 2-3 times higher risk of miscarriage than antibody-negative women.
The body is essentially in “defense mode.” This is the opposite of the “receptive mode” required for implantation.
Treatment for Euthyroid Hashimoto’s
This is a controversial area. If your TSH is 1.5 (perfect) but your antibodies are 600 (high), should you be treated? Many Reproductive Endocrinologists, myself included, will consider treatment.
We may use low-dose levothyroxine treatment even if TSH is normal. This reduces the stress on the thyroid gland. It can lower the antigen presentation that drives the immune attack.
Additionally, we look at reducing antibody titers through supplementation. Selenium (200mcg daily) has been proven to reduce TPO antibodies significantly over 3-6 months. We also look at Low Dose Naltrexone (LDN). This is an off-label therapy used to modulate the immune system and lower inflammation in Hashimoto’s thyroiditis fertility patients.
Male Factor: The Overlooked Connection
We often focus entirely on the female partner. However, Hypothyroidism & Fertility affects men just as acutely. Thyroid hormones regulate the Sertoli and Leydig cells in the testes.
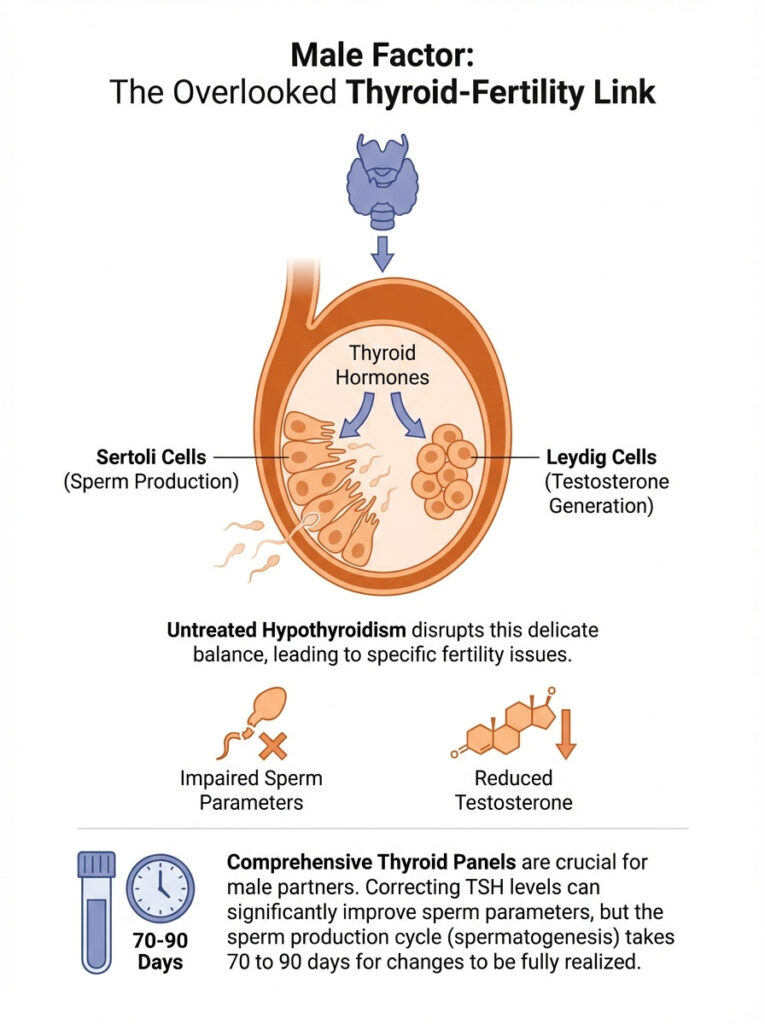
These cells are responsible for sperm production and testosterone generation. Men with untreated hypothyroidism often suffer from specific issues:
- Low Libido: A direct result of lowered testosterone.
- Erectile Dysfunction: Metabolic slowing affects blood flow and nerve response.
- Teratozoospermia: This refers to poor sperm morphology (shape). Thyroid hormone is needed for the final maturation of sperm.
If you are struggling to conceive, the male partner must also have a full thyroid panel. Correcting a man’s TSH can dramatically improve sperm parameters within 70 to 90 days. This is the length of the spermatogenesis cycle.
Clinical Management: Medication Protocols for Fertility
When it comes to Levothyroxine and pregnancy, there is a gold standard for treatment. Synthetic T4 (Levothyroxine) is the preferred medication for women trying to conceive.

Levothyroxine (T4) Therapy
Why T4 and not T3? While T3 makes you feel energetic, the developing fetus needs T4. The fetus converts the mother’s T4 into its own T3 within the brain. T3 does not cross the placenta as efficiently as T4.
Therefore, to protect the baby’s neurodevelopment, we prioritize T4 therapy. We need to ensure the maternal reservoir of T4 is high enough to share.
Brand vs. Generic: In fertility, consistency is vital. The FDA allows a variance in potency between generic batches. For most drugs, this doesn’t matter. For thyroid hormones, it is critical.
Thyroid meds have a “narrow therapeutic index.” A 5% difference can shift your TSH from 2.0 to 3.5. I strongly advise patients to stay on the same manufacturer. Ideally, choose brand-name Synthroid, Tirosint, or Unithroid during conception and pregnancy.
Natural Desiccated Thyroid (NDT)
Many patients feel better on Armour Thyroid or NP Thyroid. These are Natural Desiccated Thyroid (NDT) options. However, getting pregnant with hypothyroidism while on NDT requires caution.
NDT contains a fixed ratio of T4 to T3 (4:1). This is higher in T3 than humans naturally produce. During pregnancy, the demand for T4 skyrockets. If you are on NDT, your doctor must monitor your Free T4 closely.
We need to ensure it doesn’t drop too low for the baby. This can happen even if your TSH looks suppressed due to the T3 in the medication. Often, we add a small amount of synthetic T4 to the NDT regimen during pregnancy.
Timing and Absorption
You can have the perfect prescription and still fail to absorb it. Levothyroxine and pregnancy success depends on strict rules:
- Take on an empty stomach with water only.
- Wait 60 minutes before eating or drinking coffee. Coffee reduces absorption by up to 30%.
- Critical: Separate thyroid meds from prenatal vitamins by at least 4 hours. The calcium and iron in prenatals bind to the thyroid hormone in the gut. This renders the medication useless.
The “First 48 Hours” Protocol: Managing a Positive Pregnancy Test
The moment you see a positive pregnancy test, the clock starts ticking. This is the most critical juncture for Hypothyroidism & Fertility patients.
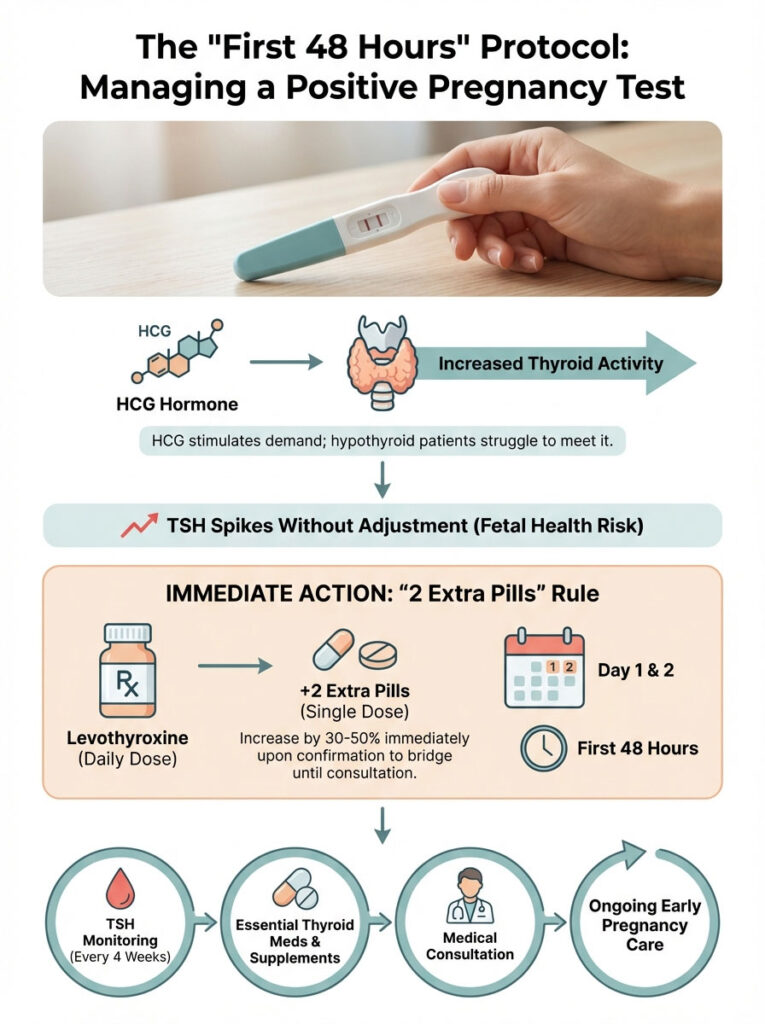
The Physiology of Early Pregnancy
For the first 12 weeks of gestation (the first trimester), the fetus does not have a functioning thyroid gland. It relies 100% on the mother for thyroid hormone. This is a massive physiological demand.
Simultaneously, the pregnancy hormone HCG (Human Chorionic Gonadotropin) stimulates the thyroid gland. In a healthy person, the thyroid ramps up production by 50%. In a hypothyroid person, the gland cannot ramp up. The tank is empty.
If you do not increase your medication externally, your TSH will spike. The fetus may not get enough T4. This increases the risk of miscarriage or developmental delays.
The Critical Action Step
The ATA guidelines recommend increasing the dosage of levothyroxine by approximately 30-50% immediately upon confirmation of pregnancy. Do not wait for a doctor’s appointment.
The “2 Extra Pills” Rule: A safe, immediate bridge protocol used by many specialists is the “2 Extra Pills” rule. You simply take two extra pills per week of your current dosage.
If you take one pill daily (7 pills a week), you immediately start taking 9 pills a week. You might double up on Monday and Thursday. This provides a roughly 29% increase instantly. You then call your clinic to schedule blood work within the week.
Monitoring Schedule
Once pregnant, the monitoring schedule tightens. We check TSH every 4 weeks during the first half of pregnancy. The goals shift slightly by trimester:
- First Trimester Goal: TSH < 2.5 mIU/L
- Second Trimester Goal: TSH < 3.0 mIU/L
- Third Trimester Goal: TSH < 3.0 mIU/L
| Medication / Supplement | Safety Class | Purpose | Special Instructions for Pregnancy |
|---|---|---|---|
| Levothyroxine (Synthroid) | Safe (Category A) | Replaces T4 hormone. | MUST INCREASE DOSE by 30-50% immediately upon positive test. |
| Liothyronine (Cytomel) | Safe | Replaces T3 hormone. | Does not cross placenta well. Usually combined with T4, rarely used alone for pregnancy. |
| Iodine | Safe (in moderation) | Fuel for thyroid hormone. | RDA is 220-250mcg. Do not exceed 500mcg if you have Hashimoto’s to avoid inflammation. |
| Selenium | Safe | Lowers antibodies. | 200mcg daily is safe and protective against postpartum thyroiditis. |
| Biotin | Safe (but tricky) | Hair/Nail health. | STOP 3 DAYS BEFORE LABS. Biotin falsely lowers TSH results, hiding hypothyroidism. |
Special Considerations: IVF and Assisted Reproductive Technology
Patients undergoing IVF face unique challenges regarding Hypothyroidism & Fertility. The process is intense. Ovarian stimulation involves injecting gonadotropins to grow multiple eggs.
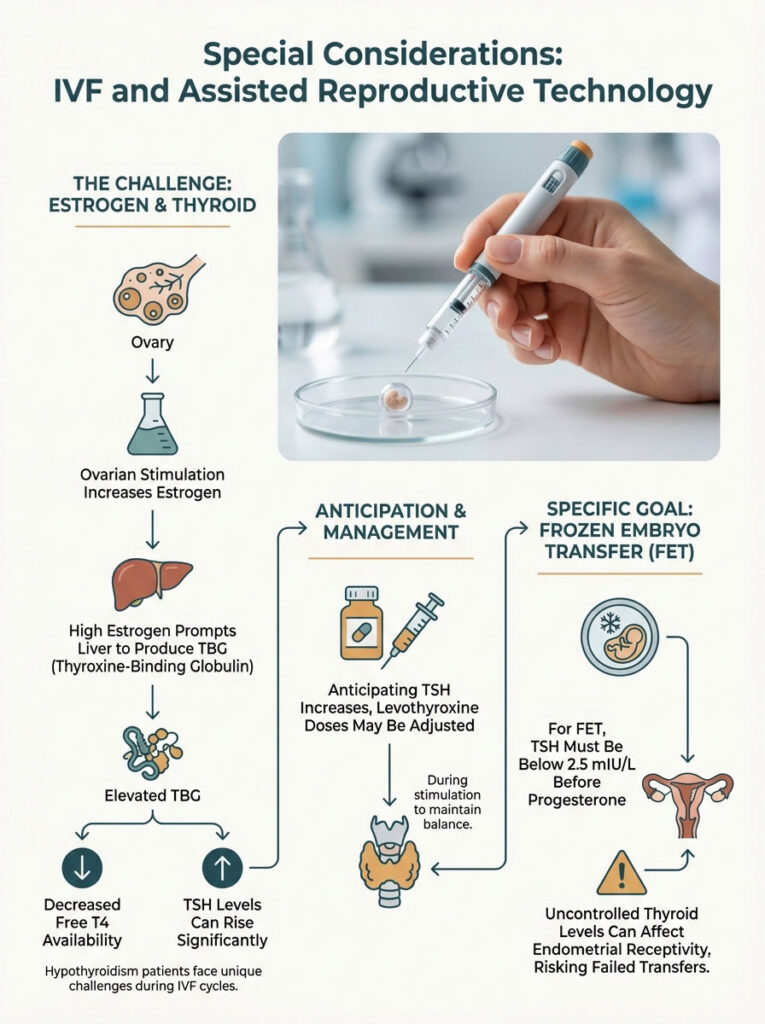
This causes estrogen levels to soar. They can go 10 times higher than a natural cycle. This has a profound effect on thyroid function.
Ovarian Stimulation Impact
High estrogen stimulates the liver to produce Thyroxine-Binding Globulin (TBG). Think of TBG as a sponge. It soaks up your Free T4.
This makes the T4 unavailable to your body. Because the Free T4 drops, the pituitary panics. It releases more TSH. It is very common for a woman to start an IVF cycle with a TSH of 1.5.
By the time of egg retrieval, her TSH may have spiked to 4.0. We anticipate this. We often increase the levothyroxine dose during stimulation. This counteracts the estrogen surge and ensures optimal levels for the embryo transfer.
Frozen Embryo Transfer (FET) Prep
Before a Frozen Embryo Transfer, we are strict. We want TSH below 2.5 mIU/L before starting progesterone injections. Thyroid status can influence the window of implantation.
If the thyroid is uncontrolled, the endometrial receptivity may be altered. This could lead to a failed transfer of a genetically normal embryo. It is a heartbreaking outcome that is largely preventable.
Diet, Lifestyle, and Supplements: Supporting the Thyroid
While medication is the heavy lifter, lifestyle changes create the foundation. You cannot medicate your way out of a poor diet. This is especially true for getting pregnant with hypothyroidism.

The “Thyroid Diet” for Fertility
The most significant dietary intervention for Hashimoto’s thyroiditis fertility patients is often gluten elimination. There is a phenomenon called “molecular mimicry.”
The protein structure of gluten (gliadin) looks very similar to thyroid tissue. When you eat gluten, your immune system attacks it. In the confusion, it attacks your thyroid gland too.
I recommend a 3-month trial of a strict gluten-free diet. Many patients report reduced bloating. They have better energy. Most importantly, they see lower antibody levels.
What about goitrogens? You may have heard to avoid broccoli and kale. The fear is largely overstated. You would need to eat truckloads of raw kale to hurt your thyroid.
Steaming these vegetables deactivates the goitrogenic compounds. It preserves the nutrients vital for fertility. Do not avoid greens; just cook them.
Essential Nutrients
- Selenium: As mentioned, 200mcg is the sweet spot. Brazil nuts are a potent source. However, soil quality varies, so a supplement is often more reliable.
- Iodine: This is a delicate balance. The fetus needs iodine for brain development. However, excessive iodine can trigger a Hashimoto’s flare. A prenatal vitamin usually contains 150mcg, which is generally safe. Avoid high-dose iodine supplements like Lugol’s solution unless supervised.
- Zinc and Iron: These are co-factors required to convert T4 into T3. Iron deficiency is common in hypothyroid women due to heavy periods. Ensure your Ferritin levels are above 50 ng/mL for hair growth and thyroid function.
- Myo-Inositol: While famous for PCOS, inositol also helps sensitization of TSH receptors. It can aid in lowering TSH levels naturally alongside medication.
The Gut-Thyroid Axis
There is a saying in functional medicine: “Heal the gut, heal the thyroid.” Approximately 20% of your T4 is converted to T3 in the gut. This requires healthy gut bacteria.
If you have dysbiosis or inflammation in the intestines, this conversion slows down. Probiotics and fermented foods can be helpful. Reducing processed sugars is also essential to feed the good bacteria.
Stress, Adrenals, and the “Cortisol Steal”
You cannot talk about the thyroid without talking about stress. The thyroid and the adrenal glands are best friends. They work together.
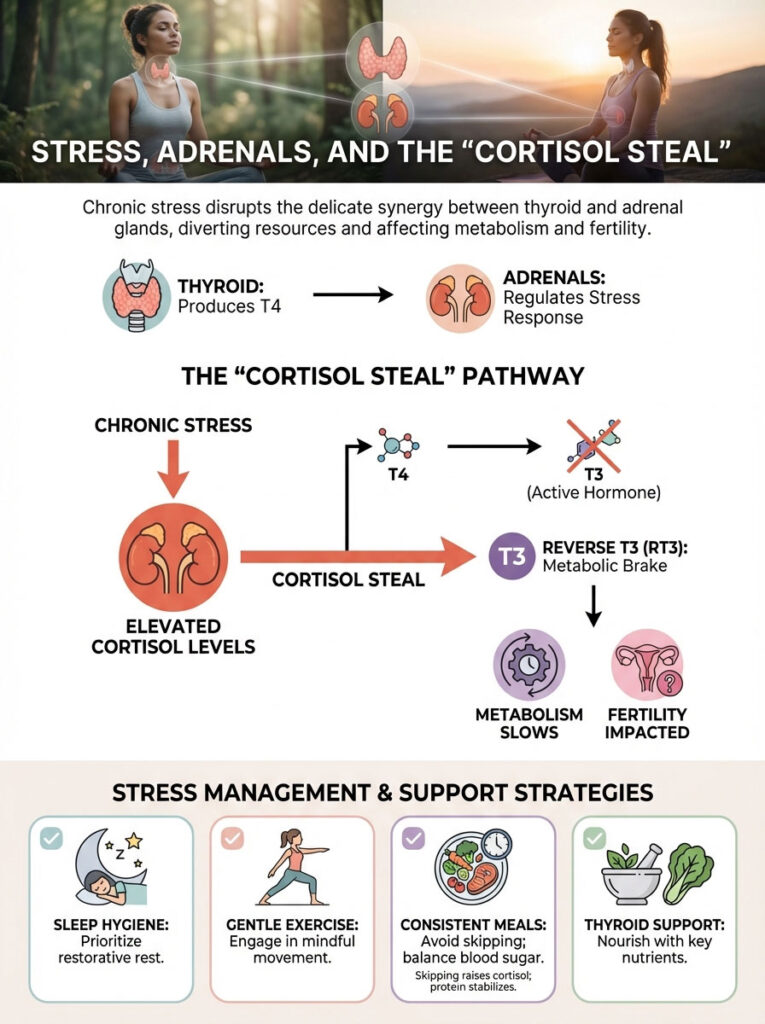
When you are chronically stressed, your body produces cortisol. High cortisol inhibits the enzyme that converts T4 to T3. Instead, it encourages the conversion of T4 to Reverse T3.
Remember Reverse T3? It is the brake pedal. Stress literally puts the brakes on your metabolism. It puts the brakes on your fertility.
For women trying to conceive, “just relax” is the most annoying advice in the world. However, physiological stress management is medical advice. This includes sleep hygiene, gentle exercise (like yoga), and blood sugar balancing.
Skipping meals spikes cortisol. Eating protein with every meal stabilizes it. This simple change can help support thyroid function.
Environmental Toxins and Thyroid Health
Our environment is filled with endocrine-disrupting chemicals (EDCs). The thyroid is particularly sensitive to these. Two of the biggest offenders are halides: Fluoride and Bromide.
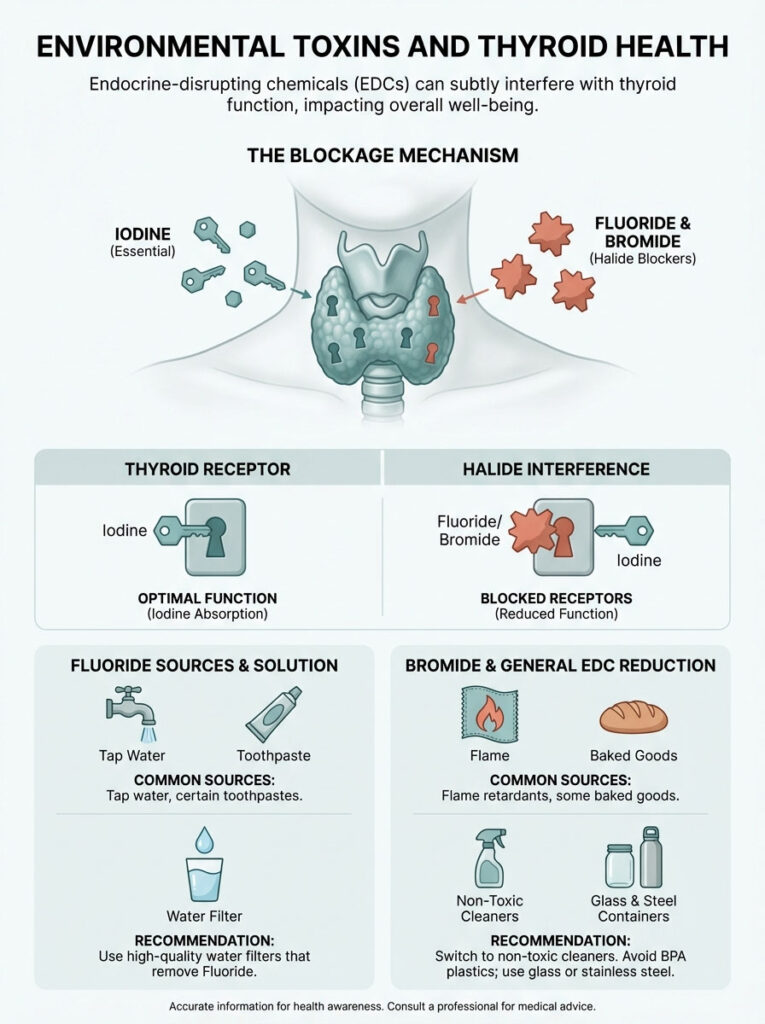
These elements are in the same chemical family as Iodine. Because they look like Iodine, the thyroid gland sucks them up. They block the receptors, preventing real Iodine from getting in.
Fluoride is found in tap water and toothpaste. Bromide is found in flame retardants and some baked goods. To support your thyroid fertility journey, consider a high-quality water filter. Look for one that removes fluoride. Switch to non-toxic household cleaners.
Plastics are another concern. Bisphenol A (BPA) can interfere with thyroid receptor function. Switch to glass or stainless steel food containers. Never heat plastic in the microwave.
Postpartum Thyroiditis: The Fourth Trimester
The journey does not end with birth. There is a condition called Postpartum Thyroiditis (PPT). It affects up to 10% of all women, but higher in those with antibodies.
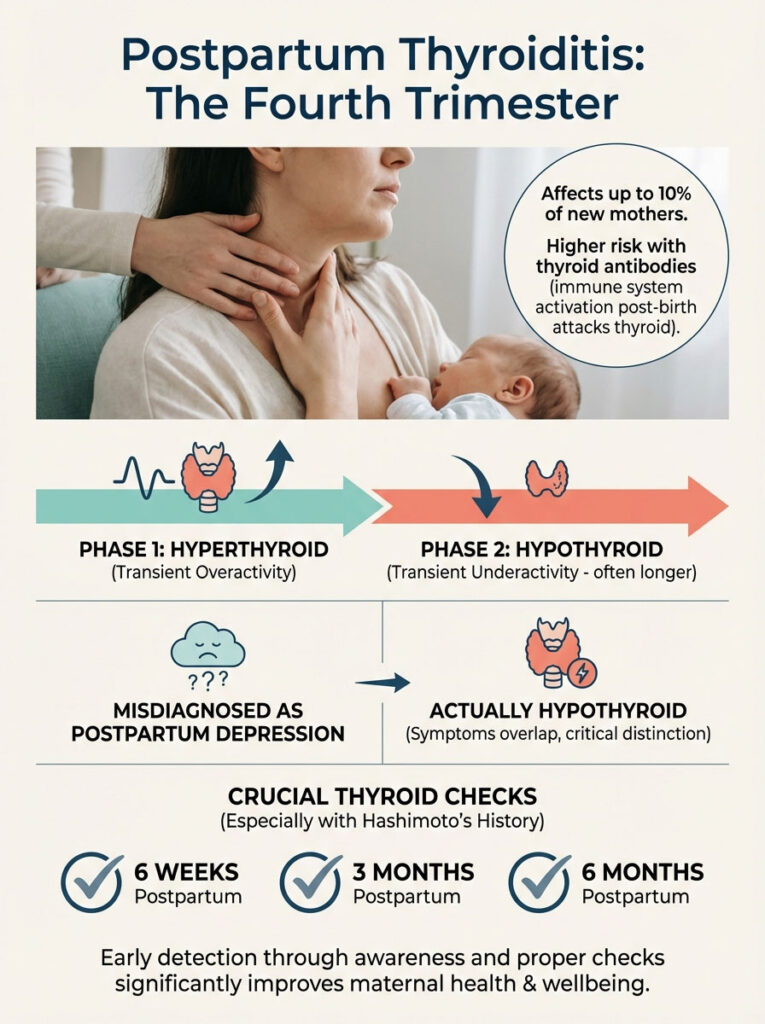
After the baby is born, the immune system “wakes up” from its pregnancy suppression. It can launch a rebound attack on the thyroid. This often presents in two phases:
- Hyperthyroid Phase (1-4 months postpartum): Anxiety, rapid weight loss, palpitations.
- Hypothyroid Phase (4-8 months postpartum): Depression, fatigue, low milk supply, weight retention.
Many women are misdiagnosed with Postpartum Depression. In reality, they are hypothyroid. If you have Hashimoto’s thyroiditis fertility history, you must have your thyroid checked at 6 weeks, 3 months, and 6 months postpartum.
Summary & Key Takeaways
Navigating Hypothyroidism & Fertility requires you to be the CEO of your own health. The standard of care in general medicine is simply not aggressive enough for the delicate process of reproduction.

You must advocate for yourself. You must understand the numbers. You must be proactive.
Here are your Golden Rules:
- Target TSH < 2.5 mIU/L: Do not accept “normal” if it is above this number while trying to conceive. Fight for the optimal range.
- Check Antibodies: Know if you have Hashimoto’s thyroiditis fertility issues. If positive, consider Selenium and gluten elimination to manage the immune risk.
- The Positive Test Plan: Have a plan with your doctor to increase your Levothyroxine and pregnancy dosage immediately. Usually, this is a 30-50% increase the moment you see a positive test.
- Monitor Frequently: Check TSH every 4 weeks in early pregnancy. The baby depends on you.
- Don’t Forget Him: Check the male partner’s thyroid if sperm parameters are off.
Thyroid dysfunction is one of the most treatable causes of infertility. It is not a permanent sentence. With the right diagnosis, the correct medication, and precise monitoring, your odds of a healthy pregnancy are excellent.
If your TSH is above 2.5 and you have been trying for six months without success, it is time to consult a Reproductive Endocrinologist. Find someone who understands these nuances. Your future family is worth the effort.
Frequently Asked Questions
What is the ideal TSH level for getting pregnant?
While general labs consider a TSH up to 4.5 mIU/L normal, clinical fertility guidelines recommend a TSH between 0.5 and 2.5 mIU/L for conception. Maintaining this tighter range is essential for ensuring regular ovulation and reducing the risk of early pregnancy loss.
Can subclinical hypothyroidism cause infertility even if my labs are normal?
Yes, subclinical hypothyroidism, where TSH is slightly elevated but Free T4 is normal, is a common barrier to conception. It can lead to ovulatory dysfunction and a shortened luteal phase, making it difficult for an embryo to implant properly in the uterine lining.
How do TPO antibodies affect my chances of staying pregnant?
The presence of thyroid peroxidase (TPO) antibodies, indicative of Hashimoto’s, creates a pro-inflammatory environment that can double or triple the risk of miscarriage. Even if your TSH is normal, high antibody titers may signal an overactive immune response that interferes with fetal tolerance.
How much should I increase my thyroid medication after a positive pregnancy test?
Standard protocol suggests increasing your levothyroxine dosage by 30% to 50% the moment pregnancy is confirmed. Many specialists recommend the “two extra pills per week” rule as an immediate bridge until your TSH can be formally retested by your physician.
Why must I separate my thyroid medication from my prenatal vitamins?
Calcium and iron found in prenatal vitamins significantly interfere with the absorption of thyroid hormones in the digestive tract. To ensure you receive the full dose, you should wait at least four hours between taking your thyroid medication and your prenatal supplement.
Can hypothyroidism in men cause male factor infertility?
Absolutely, as thyroid hormones regulate the cells in the testes responsible for sperm production and testosterone. Untreated hypothyroidism in men can lead to low libido, erectile dysfunction, and poor sperm morphology, which often resolves after 90 days of thyroid hormone replacement.
Why does TSH often spike during an IVF stimulation cycle?
The high levels of estrogen produced during ovarian stimulation increase Thyroxine-Binding Globulin (TBG), which acts like a sponge and soaks up free thyroid hormone. This often causes TSH to rise rapidly, requiring a proactive dosage adjustment to keep levels optimal for the upcoming embryo transfer.
Is it safe to take T3 or desiccated thyroid medication while pregnant?
While some patients feel better on T3 or NDT, the developing fetus relies exclusively on the mother’s T4 for brain development during the first trimester. If you remain on these medications, we must monitor your Free T4 levels very closely to ensure the reservoir is sufficient for the baby’s needs.
Should I go gluten-free if I have Hashimoto’s and am trying to conceive?
Many patients benefit from a gluten-free diet because the protein structure of gluten mimics thyroid tissue, potentially triggering immune attacks. Eliminating gluten can lower systemic inflammation and antibody titers, creating a more receptive environment for pregnancy.
How does hypothyroidism cause high prolactin and stop ovulation?
When thyroid levels are low, the brain releases Thyrotropin-Releasing Hormone (TRH) to compensate, which inadvertently stimulates the production of prolactin. Elevated prolactin signals the body to suppress ovulation, similar to what happens during breastfeeding, leading to irregular cycles and infertility.
What are the symptoms of a “cold womb” on a BBT chart?
In hypothyroid patients, basal body temperatures (BBT) are often consistently below 97.0°F during the follicular phase. You may also observe a slow, sluggish temperature rise after ovulation, indicating that the metabolism is too low to support optimal progesterone production and implantation.
What is postpartum thyroiditis and how does it affect new mothers?
Postpartum thyroiditis is an immune rebound that occurs after birth, causing the thyroid to become temporarily hyperactive followed by a period of hypothyroidism. It affects up to 10% of women and is often misdiagnosed as postpartum depression or simple fatigue.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The intersection of thyroid health and reproduction is complex and requires individualized clinical care. Always consult a qualified Reproductive Endocrinologist or healthcare professional before starting new medications, changing dosages, or making significant lifestyle changes, especially when trying to conceive or during pregnancy.
References
- American Thyroid Association (ATA) – thyroid.org – Guidelines for the diagnosis and management of thyroid disease during pregnancy and the postpartum period.
- American Society for Reproductive Medicine (ASRM) – asrm.org – Clinical practice committee opinions on subclinical hypothyroidism and its impact on infertility and IVF outcomes.
- The Endocrine Society – endocrine.org – Research and clinical guidelines regarding the Hypothalamic-Pituitary-Thyroid (HPT) axis and reproductive health.
- Journal of Clinical Endocrinology & Metabolism (JCEM) – academic.oup.com/jcem – Peer-reviewed studies on the correlation between TPO antibodies and recurrent pregnancy loss.
- Thyroid Journal – liebertpub.com/thy – Official journal of the ATA, providing data on levothyroxine dosage adjustments in the first trimester.
- National Institutes of Health (NIH) – nichd.nih.gov – Statistical data on the prevalence of thyroid dysfunction in women of reproductive age.








