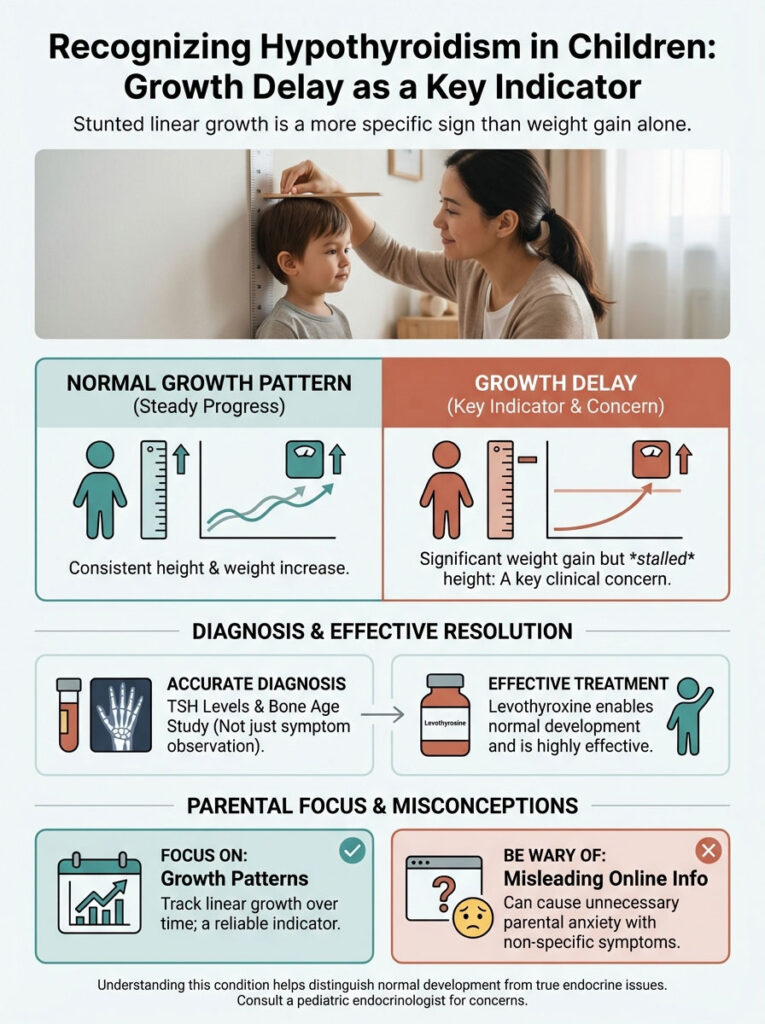
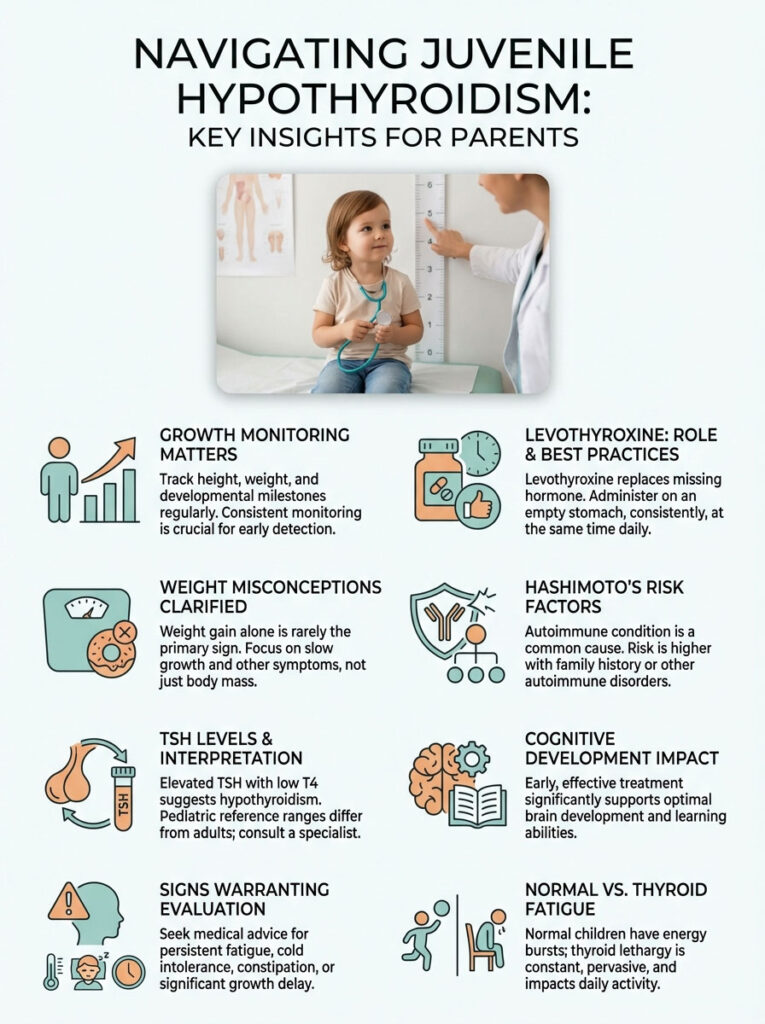
While parents often worry about fatigue or rapid weight gain, the most critical sign of hypothyroidism in children is actually a stalling of linear growth. If your child is gaining weight but not growing taller, this is a major clinical red flag. Most other symptoms are non-specific and often unrelated to the thyroid. Diagnosis relies on interpreting a TSH levels in children chart and a bone age study, not just symptom observation. Treatment with Levothyroxine for kids is highly effective and allows for a normal, healthy life.
Table of Contents
It is 2 AM. You are sitting in the glow of a smartphone screen watching your child sleep. Perhaps they have been more tired than usual lately. Maybe their grades have slipped. You type a few observations into a search bar and the results flood in. Suddenly you are convinced that every instance of dry skin or an afternoon nap is a sign of a hormonal crisis.
As a pediatric endocrinologist, I see this scenario play out in my clinic weekly. Parents arrive terrified. They clutch printouts of symptoms that could apply to almost any growing child. The fear is real. However, the focus is often wrong.
Hypothyroidism in children is a serious condition where the thyroid gland fails to produce enough hormone to meet the body’s metabolic and developmental demands. Yet the “symptoms” listed on general health websites often mislead parents. In pediatric medicine, we do not look for the same red flags as we do in adults. This article will help you distinguish between normal developmental phases and true endocrine pathology. We will focus specifically on growth delay in kids as the primary indicator you should never ignore.
Key Statistics & Facts
- Prevalence: Congenital hypothyroidism affects approximately 1 in 2,000 to 4,000 newborns in the USA.
- Gender Gap: Hashimoto’s thyroiditis is 4 to 10 times more common in girls than boys.
- Growth Impact: Over 90% of children with significant hypothyroidism will display a decrease in growth velocity before other symptoms appear.
- Screening Success: Newborn screening has virtually eliminated intellectual disability caused by congenital hypothyroidism in the developed world.
- Treatment: Levothyroxine is the 3rd most prescribed medication in the United States overall.
The “Dr. Google” Panic vs. Clinical Reality
The internet is a powerful tool. But it lacks context. When you search for child thyroid symptoms, you get a laundry list. Fatigue, constipation, cold intolerance, and weight gain appear at the top. The problem is that these are also symptoms of being a modern American child. School schedules are exhausting. Diets often lack fiber. Winters are cold.
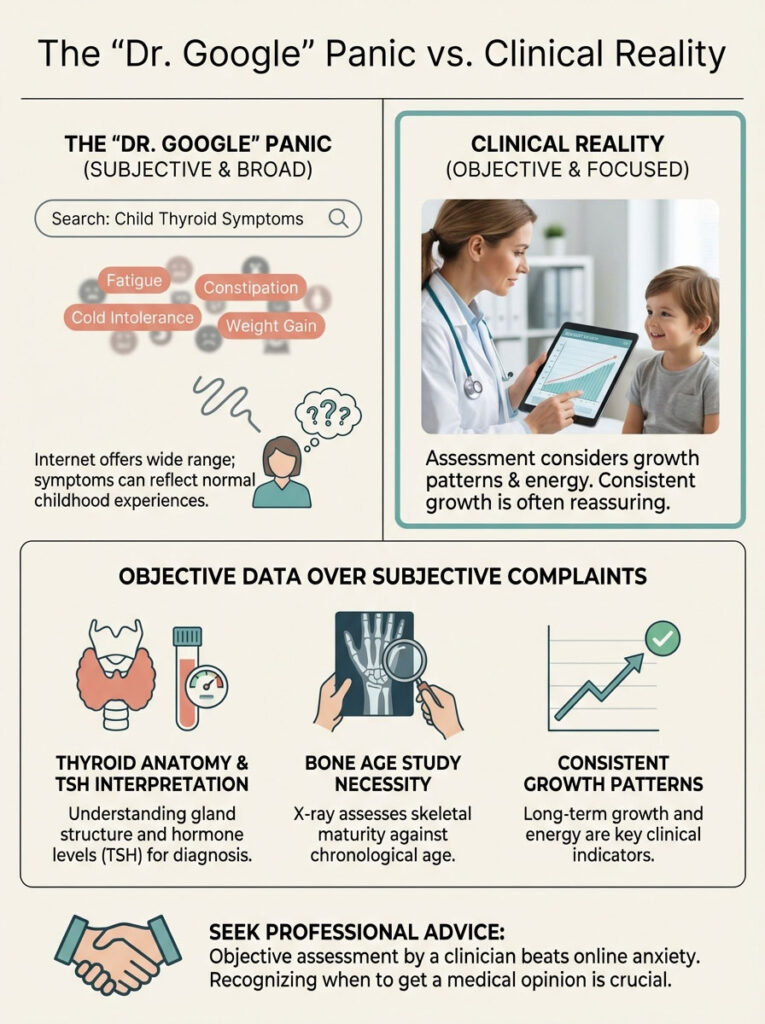
In my practice, the clinical reality is distinct from the online panic. A child who is tired but growing 2.5 inches a year likely does not have a thyroid problem. A child who is full of energy but has not bought new shoes in 18 months is a different story. That is the child I need to see immediately.
We must shift the focus from subjective complaints to objective data. This involves understanding the difference between a child who is “off” and a child with a pathological hormone deficiency. Throughout this guide, we will dissect the anatomy of the thyroid. We will explain the absolute necessity of a bone age study. We will also teach you how to properly interpret a TSH levels in children chart.
Anatomy 101: The Pediatric Thyroid and Growth
To understand why hypothyroidism in children presents differently than in adults, we must look at the Hypothalamus-Pituitary-Thyroid (HPT) axis. I often explain this to parents using a “Thermostat and Heater” analogy.
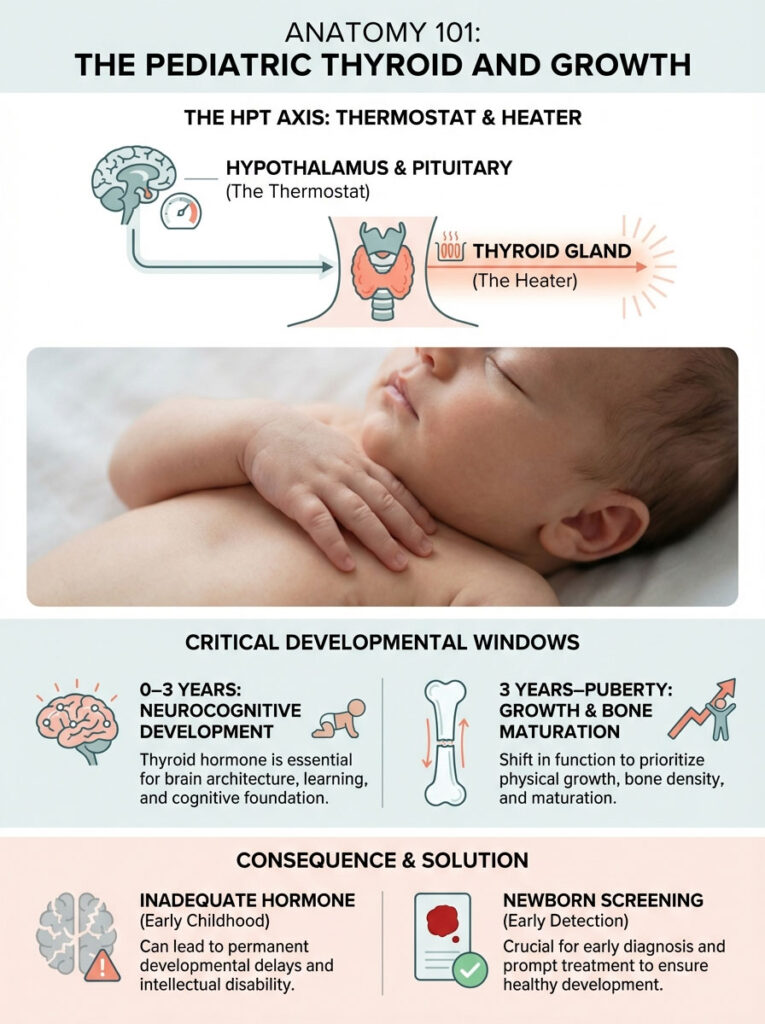
The Feedback Loop
The pituitary gland sits at the base of the brain. It acts as the thermostat. It constantly measures the level of thyroid hormone in the blood. If the level is too low, the pituitary screams for more heat. It does this by sending out Thyroid Stimulating Hormone (TSH).
The thyroid gland is a butterfly-shaped organ in the neck. It acts as the heater. Its job is to respond to the TSH by producing Thyroxine (T4) and Triiodothyronine (T3).
- High TSH: The thermostat is screaming because the house is cold (Hypothyroidism).
- Low TSH: The thermostat has shut off because the house is too hot (Hyperthyroidism).
Why Kids Are Not Small Adults
Here is where the distinction is vital. In adults, thyroid hormone primarily regulates metabolism. It controls how fast we burn calories. In children, thyroid hormone has two strictly defined “full-time jobs” depending on age.
1. Age 0 to 3 Years:
The primary job is neurocognitive development. Without adequate thyroid hormone during this window, permanent brain damage can occur. This is why newborn screening is non-negotiable.
2. Age 3 Years to Puberty:
The primary job shifts to linear growth and bone maturation. Because the biological priority is growth, a child’s body will sacrifice other functions to preserve the brain. This is why growth delay in kids is often the first sign. Sometimes it is the only sign of pediatric hypothyroidism. The metabolism slows down later.
The Two Faces of Diagnosis: Congenital vs. Acquired
When we discuss hypothyroidism in children, we are usually talking about two entirely different disease processes. Mixing these up causes significant confusion for parents.
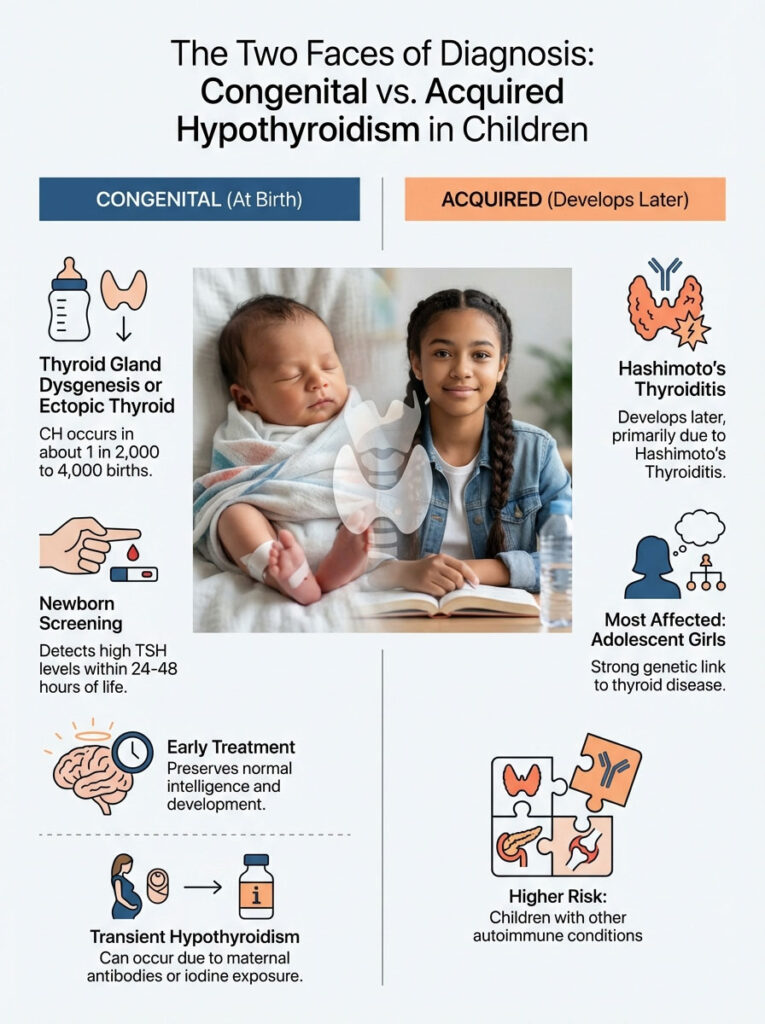
Congenital Hypothyroidism (CH)
Congenital Hypothyroidism refers to a baby born with an underactive thyroid. This occurs in about 1 in 2,000 to 4,000 births according to the American Thyroid Association. In most cases, the thyroid gland failed to form correctly. This is called dysgenesis. Sometimes the gland is in the wrong place. This is called ectopic thyroid.
The Newborn Screen Triumph:
Decades ago, CH was a leading cause of preventable intellectual disability. Historically, this was termed cretinism. Today, every baby born in the USA undergoes a heel prick test within 24 to 48 hours of life. This screen detects high TSH levels immediately. Because of this, we can start treatment within the first two weeks of life. This preserves normal intelligence and development.
Transient vs. Permanent:
Not every positive screen means a lifetime of medication. Maternal antibodies or iodine exposure can cause “transient” hypothyroidism. In these cases, we treat the child until age three to protect the brain. We then run a trial off medication to see if the gland works on its own.
Acquired Hypothyroidism (Hashimoto’s Thyroiditis)
This is the form that develops later in childhood or adolescence. The most common cause in the United States is Hashimoto’s disease in childhood. This is an autoimmune condition. The body’s immune system mistakenly identifies the thyroid gland as a foreign invader and attacks it.
Demographics and Risk:
We see this most frequently in adolescent girls. There is a strong genetic link. If you or your spouse has thyroid disease, your child is at higher risk. Furthermore, children with other autoimmune conditions have a higher prevalence. This includes Type 1 Diabetes or Celiac disease. These children are significantly more likely to develop pediatric hypothyroidism.
The “Ignore” List: Deciphering Symptoms
This section addresses the core intent of this article. Parents often fixate on symptoms that are vague. They miss the clinical red flags. Below is what you need to know about child thyroid symptoms.
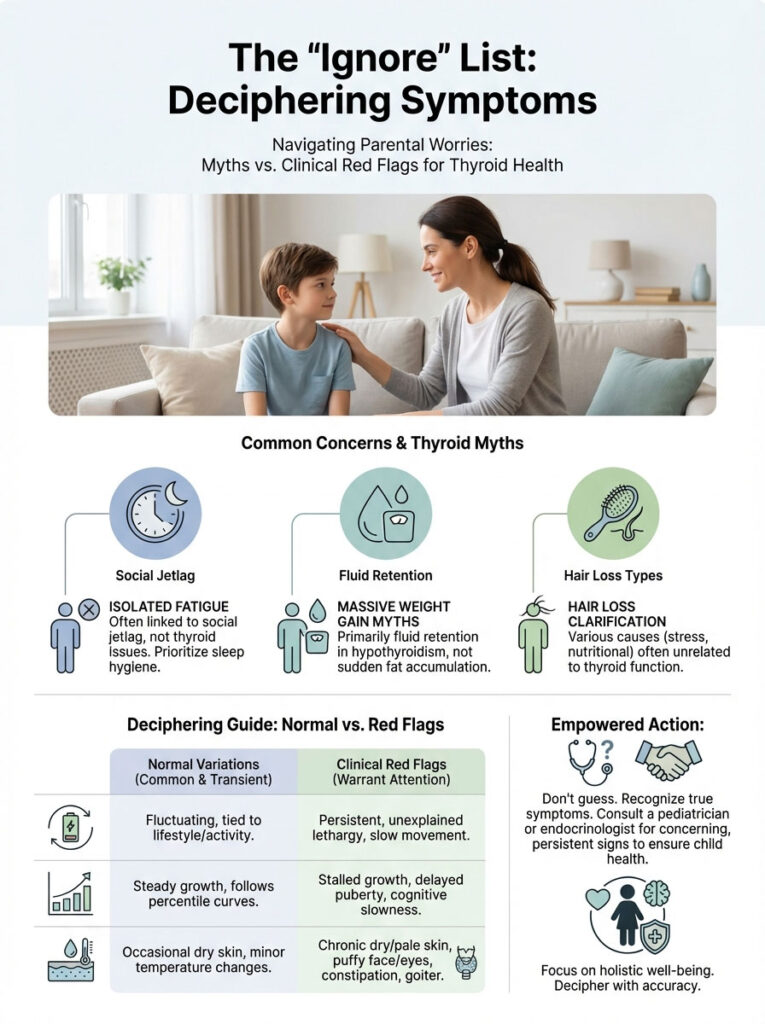
What Parents Often Worry About (But Shouldn’t)
1. Isolated Fatigue:
“My teenager sleeps until noon on Saturdays.” This is a common complaint. However, adolescents have a shifted circadian rhythm. If a child can play sports, attend school, and interact with friends but crashes on the weekend, this is likely social jetlag. It is not a thyroid coma. Pathological lethargy is profound. The child falls asleep at the dinner table. They lose interest in favorite activities.
2. Massive Weight Gain:
There is a pervasive myth that hypothyroidism causes obesity. While low thyroid function can lower basal metabolic rate, it typically accounts for only 5 to 10 pounds of weight gain. This is mostly due to fluid retention known as myxedema. If a child has gained 40 pounds in a year, hypothyroidism in children is rarely the sole cause. The thyroid may be a contributing factor. But it is almost never the primary driver of severe obesity.
3. Hair Loss:
Parents often find hair in the shower drain and panic. Hair loss, or telogen effluvium, is common after fevers, stress, or nutritional changes. Thyroid-related hair loss usually presents as general thinning. It has a dry, brittle texture rather than clumps falling out.
Comparison Table: Symptom Sorter
Use this table to help distinguish between normal variations and signs that warrant a juvenile hypothyroidism diagnosis.
| Feature | Likely “Normal” / Non-Thyroid | Clinical Red Flag for Hypothyroidism |
|---|---|---|
| Growth (Height) | Steady percentile curve (growing out of pants) | Growth velocity flattening (wearing same pants for 2 years) |
| Energy Levels | Tired after school or late nights | Lethargy despite adequate sleep; napping at unusual ages |
| Weight | Rapid gain with normal height growth | Mild gain with growth delay (getting “chubby” but not taller) |
| Digestion | Occasional constipation due to diet | Chronic, hard stools unresponsive to fiber/water |
| Neck Appearance | Normal contour | Visible goiter (fullness at base of neck) |
| Skin | Dry in winter or due to eczema | Cool, pale, yellow-tinted, and doughy to the touch |
The Gold Standard: Growth Velocity and Bone Age
If you take only one thing from this article, let it be this. Growth delay in kids is the most sensitive indicator of thyroid health.
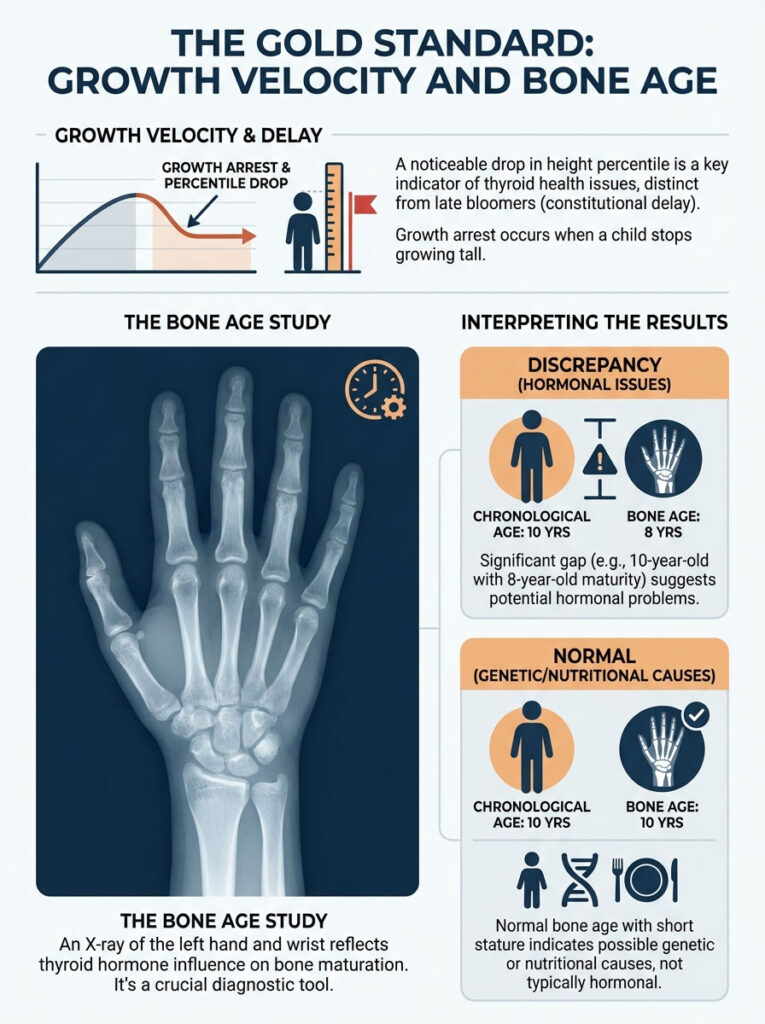
The Most Critical Sign
A child with a failing thyroid stops growing tall long before they show other symptoms. We call this “growth arrest.” In my clinic, when I plot a child’s height on a growth chart, I look for a “falling off the curve.”
Consider this example. A child has always tracked along the 50th percentile for height. Suddenly, they drop to the 25th percentile over a year. This is flashing a neon warning sign. This is distinct from “constitutional delay,” or late bloomers. Late bloomers stay on a lower curve but maintain velocity. In pediatric hypothyroidism, the velocity halts.
Bone Age Study: The Truth Serum
When we suspect a growth issue, we order a bone age study. This is a simple X-ray of the left hand and wrist. Radiologists compare the growth plates of the child’s hand to a standard atlas.
Thyroid hormone is essential for bone maturation. Therefore, a child with long-standing untreated hypothyroidism will have a “delayed” bone age.
Expert Insight: If your 10-year-old child has the bone maturity of an 8-year-old, this is a strong indicator of a hormonal issue. Conversely, if a child is short but their bone age matches their chronological age, the thyroid is likely functioning normally. In those cases, we look for genetic or nutritional causes.
Decoding the Labs: TSH and Free T4
Parents often bring me lab results ordered by general practitioners. They are confused by the numbers. Understanding these values is key to navigating a juvenile hypothyroidism diagnosis.
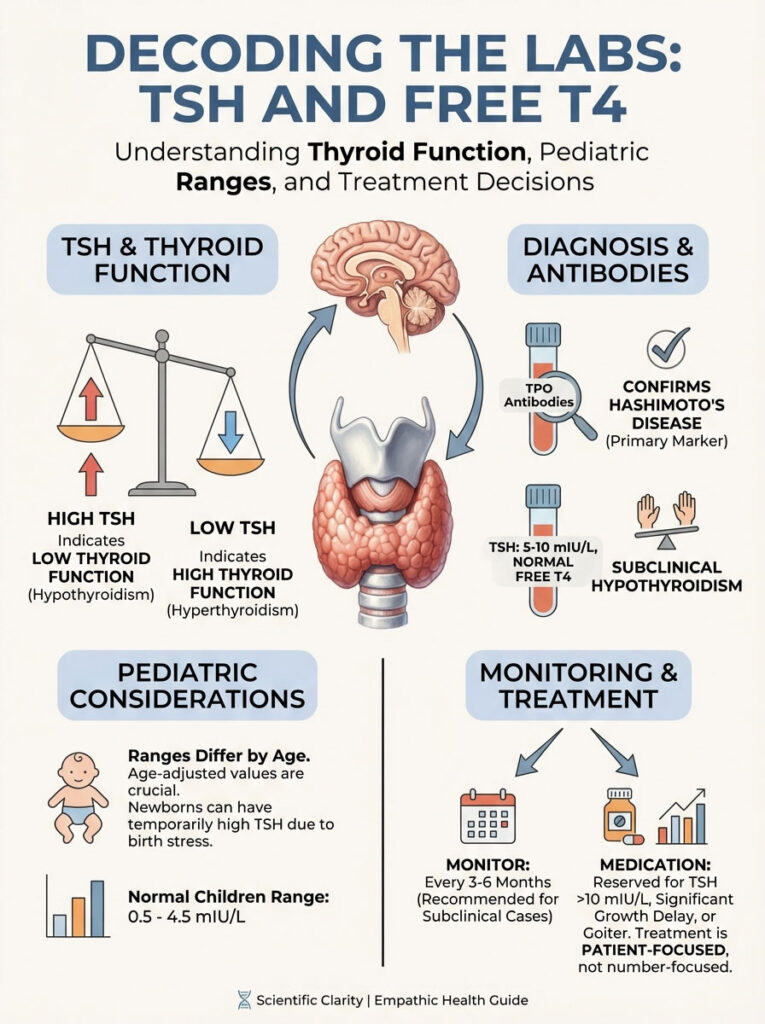
The “Inverse” Relationship
Remember the thermostat analogy? High TSH equals Low Thyroid Function. This is counterintuitive for many people. They see “High” and think “Hyper.” It is the opposite. The pituitary is working overtime to stimulate a lazy thyroid.
Pediatric Reference Ranges
You cannot use the reference ranges printed on the lab report if they are not age-adjusted. A TSH levels in children chart looks very different from an adult chart.
For newborns, TSH can surge to 20 mIU/L shortly after birth and be normal. This is due to the stress of birth and the cold environment. For children and adolescents, a TSH between 0.5 and 4.5 mIU/L is generally considered normal.
Labs often flag a TSH of 5.5 as “High.” While technically elevated, this does not always require medication. We treat the patient, not the number.
Antibody Testing
To confirm Hashimoto’s disease in childhood, we test for antibodies. Thyroid Peroxidase Antibodies (TPO) are the primary marker. A positive result means the immune system is attacking the thyroid. Thyroglobulin Antibodies are a secondary marker often checked alongside TPO.
Subclinical Hypothyroidism
We frequently see children with TSH levels between 5 and 10 mIU/L. However, they have normal Free T4 levels. This is called “Subclinical Hypothyroidism.” It is a grey area. The thyroid is struggling. But it is compensating enough to keep hormone levels normal in the blood.
Current consensus from the Pediatric Endocrine Society suggests “watchful waiting” for these cases. We monitor labs every 3 to 6 months. Often, levels return to normal without intervention. We typically do not medicate unless TSH rises above 10 mIU/L. We also medicate if there is significant growth delay in kids or a goiter present.
Treatment Protocols: Levothyroxine Management
Once a diagnosis of hypothyroidism in children is confirmed, treatment is straightforward. It is also highly effective. The goal is to replace exactly what the body is missing.

The Medication: Levothyroxine
The standard of care is Levothyroxine for kids (T4). It is a synthetic version of the hormone the thyroid naturally makes.
In adults, some alternative practitioners use T3 (Cytomel) or desiccated pig thyroid (Armour). In pediatrics, we avoid these. T3 has a very short half-life. It can cause cardiac side effects like palpitations. It can also cause behavioral issues. The human body is perfectly capable of converting T4 into T3 as needed. This provides a smoother, more stable hormone level for a growing child.
Brand vs. Generic
Thyroid hormone has a “narrow therapeutic index.” This means small changes in the pill formulation can affect blood levels. I advise parents to try to stay on the same manufacturer. If you start on brand name (Synthroid, Tirosint) or a specific generic, try not to switch back and forth every month. This can cause TSH fluctuations.
Administration Rules
Levothyroxine for kids is a fussy medication. For it to work, you must follow the rules. First, give it on an empty stomach. Give it at the same time every day. Ideally, this is 30 to 60 minutes before breakfast.
Second, avoid interactions. Do not give calcium, iron, or soy products within 4 hours of the medication. These bind to the hormone in the gut. They prevent absorption. Third, be consistent. Missed doses lead to unstable levels.
Comparison Table: Congenital vs. Acquired Management
The journey differs depending on when the diagnosis occurs.
| Parameter | Congenital Hypothyroidism | Acquired (Hashimoto’s) |
|---|---|---|
| Age of Onset | Birth (detected by screen) | Childhood / Adolescence |
| Primary Risk | Neurocognitive damage | Growth delay in kids, puberty issues |
| Dosing Needs | High dose per weight (rapid growth demand) | Lower dose per weight |
| Monitoring Freq. | Monthly in infancy | Every 3-6 months |
| Permanency | Usually permanent (trial off at age 3) | Usually lifelong |
Lifestyle, Diet, and “Natural” Cures
Parents naturally want to know if they can fix hypothyroidism in children with diet. The answer requires nuance.
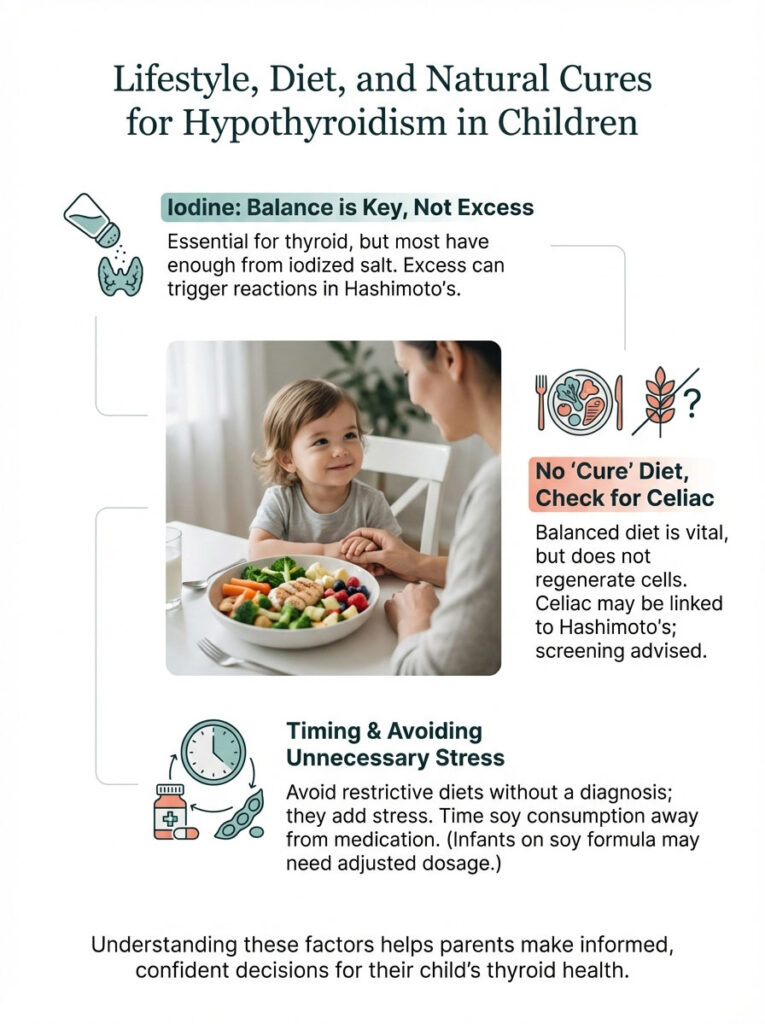
The Iodine Connection
Iodine is the building block of thyroid hormone. In developing countries, iodine deficiency is a major cause of hypothyroidism. However, in the USA, our salt is iodized. Most American children get sufficient iodine. Supplementing extra iodine is rarely necessary. In fact, it can actually trigger autoimmune attacks in children with Hashimoto’s disease in childhood.
The “Thyroid Diet” Myth
There is no specific diet that cures hypothyroidism. While a balanced diet is vital for growth, removing gluten or dairy will not make the thyroid gland start working again. If the cells have been destroyed by antibodies, diet cannot regenerate them.
However, there is a connection between Celiac disease and Hashimoto’s. If your child has child thyroid symptoms despite normal labs, screening for Celiac is reasonable. Stomach pain is another indicator. But putting a child on a restrictive diet without a diagnosis adds unnecessary stress.
Soy Caution
You do not need to ban soy. But you must time it. Soy protein can interfere with the absorption of Levothyroxine for kids. If your infant is on soy formula and thyroid medication, we may need to increase the medication dose. This helps to overcome the absorption issue.
Long-Term Prognosis: Puberty and Beyond
The outlook for children with treated hypothyroidism is excellent. These children live full, normal lives.
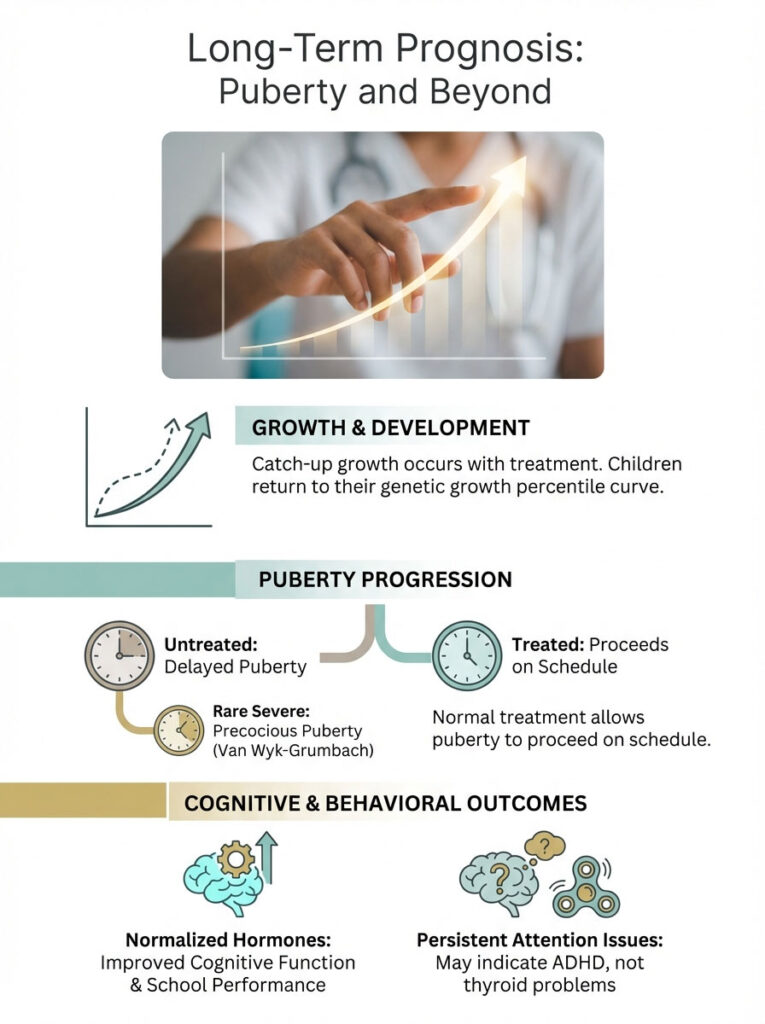
Catch-Up Growth
When treatment begins, we often see a phenomenon called “catch-up growth.” A child who had stopped growing will suddenly sprout up. They return to their genetic percentile curve. It is a rewarding phase for parents and doctors alike.
Puberty and School
Untreated pediatric hypothyroidism can cause delayed puberty. Paradoxically, severe long-standing cases can cause a type of precocious puberty. This is known as Van Wyk-Grumbach syndrome. With treatment, puberty typically proceeds normally.
Regarding school performance, once hormone levels are normalized, the “brain fog” lifts. If attention issues persist after TSH is normal, we look for other causes. We consider ADHD rather than continuing to blame the thyroid.
Summary & Key Takeaways
Navigating a medical diagnosis for your child is daunting. But knowledge is the antidote to fear. When it comes to hypothyroidism in children, the internet often amplifies the wrong symptoms.
Here is the reality:
- Ignore isolated fatigue or mild weight gain if linear growth is normal.
- Focus on growth delay in kids. If the height velocity stalls, seek a specialist.
- Trust the bone age study and the TSH levels in children chart over subjective observations.
- Treat with Levothyroxine for kids consistently to ensure full cognitive and physical potential.
With proper juvenile hypothyroidism diagnosis and management, your child will not just survive. They will thrive, grow, and reach every milestone just like their peers. If you suspect your child is falling off their growth curve, put down the phone. Make an appointment with a pediatrician.
Frequently Asked Questions
What is the most reliable clinical indicator of hypothyroidism in children?
The most sensitive red flag is a stalling of linear growth velocity, often called growth arrest. While adults often present with metabolic shifts, a child who stops growing taller or “falls off” their growth curve requires an immediate endocrine evaluation.
Does hypothyroidism in children cause significant weight gain or obesity?
Contrary to popular belief, hypothyroidism typically only accounts for 5 to 10 pounds of weight gain, largely due to fluid retention known as myxedema. If a child is experiencing rapid, massive weight gain while still growing normally in height, the thyroid is rarely the primary cause.
How should parents interpret a TSH levels in children chart compared to adult ranges?
Pediatric reference ranges are age-specific and much broader than adult standards, particularly in newborns where a TSH of 20 mIU/L can be normal. For older children, we often monitor “subclinical” elevations between 5 and 10 mIU/L without medication unless growth delay or a goiter is present.
Why do pediatric endocrinologists order a bone age study for suspected thyroid issues?
Thyroid hormone is essential for skeletal maturation; therefore, an X-ray of the left hand helps us determine if the child’s bone maturity lags behind their chronological age. A delayed bone age is a hallmark sign of long-standing, untreated juvenile hypothyroidism.
How can I distinguish between normal adolescent fatigue and pathological thyroid lethargy?
Normal fatigue is usually situational, such as “social jetlag” where a teen sleeps late on weekends but functions well during activities. Pathological lethargy is profound, often manifesting as a child falling asleep at the dinner table or losing interest in favorite hobbies despite adequate rest.
What are the specific rules for administering Levothyroxine for kids to ensure absorption?
Levothyroxine must be taken on an empty stomach, ideally 30 to 60 minutes before breakfast, with water only. Consistency is vital, as the medication has a narrow therapeutic index and missed doses or varying administration times can cause TSH fluctuations.
What are the primary risk factors for Hashimoto’s disease in childhood?
Hashimoto’s is an autoimmune condition that is significantly more common in girls and has a strong genetic component. Children with existing autoimmune disorders, such as Type 1 Diabetes or Celiac disease, are at a much higher risk for developing acquired hypothyroidism.
What does a positive newborn screen for congenital hypothyroidism mean for my baby?
A positive screen indicates that the infant’s thyroid gland is not producing enough hormone, which is critical for neurocognitive development. Starting Levothyroxine within the first two weeks of life is essential to prevent permanent intellectual disabilities and ensure normal brain growth.
When is medication necessary for subclinical hypothyroidism in children?
We typically adopt a “watchful waiting” approach for TSH levels between 5 and 10 mIU/L if Free T4 levels remain normal. Treatment is generally reserved for cases where the TSH exceeds 10 mIU/L, or if the child displays a visible goiter or a declining growth velocity.
Can dietary changes or iodine supplements cure pediatric hypothyroidism?
In the United States, iodine deficiency is rare due to iodized salt, and excessive iodine can actually trigger autoimmune attacks in children with Hashimoto’s. While a balanced diet supports general health, it cannot regenerate thyroid tissue that has been destroyed by antibodies.
Which foods or supplements interfere with pediatric thyroid medication?
Calcium, iron, and soy products are known to bind to thyroid hormone in the gut, significantly reducing its absorption. These should be spaced at least four hours away from the morning dose of Levothyroxine to ensure the child receives the full therapeutic benefit.
Will my child experience catch-up growth once they start thyroid treatment?
Yes, once thyroid hormone levels are normalized, most children experience a “catch-up growth” phase where they sprout up rapidly. This allows them to return to their original genetic percentile curve and reach their full adult height potential.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Pediatric thyroid conditions require complex clinical management. Always consult a qualified healthcare professional or a pediatric endocrinologist before making decisions regarding your child’s health or medication.
References
- American Thyroid Association (ATA) – thyroid.org – Comprehensive clinical guidelines on congenital and acquired hypothyroidism in pediatric populations.
- Pediatric Endocrine Society (PES) – pedsendo.org – Consensus statements regarding the management of subclinical hypothyroidism and growth velocity in children.
- Journal of Clinical Endocrinology & Metabolism – “Growth and Bone Age in Pediatric Thyroid Disorders” – Peer-reviewed research on the correlation between T4 levels and linear growth.
- American Academy of Pediatrics (AAP) – aap.org – Official recommendations for universal newborn screening and early intervention for thyroid dysgenesis.
- National Institutes of Health (NIH) – niddk.nih.gov – Statistical data on the prevalence of Hashimoto’s thyroiditis and autoimmune markers in adolescents.








