Quick Answer: Hypothyroidism in elderly patients is a metabolic disorder caused by an underactive thyroid gland. In older adults, it frequently shows up as endocrine-induced pseudodementia rather than the classic weight gain seen in younger people. Seniors with this condition often experience memory loss, cognitive slowing, and depression, a pattern called apathetic hypothyroidism. Because these symptoms closely resemble Alzheimer’s disease and vascular dementia, misdiagnosis is common. A simple blood test measuring Serum Free T4 and TSH can identify the real cause, and in many cases, cognitive decline can be reversed with treatment.
Table of Contents
A Story That Changed How I Think About Dementia
I still remember Mrs. H. She was 82 years old, slumped in her wheelchair, staring at the floor of my office. Her daughter sat beside her in tears, clutching a brochure for a memory care facility.
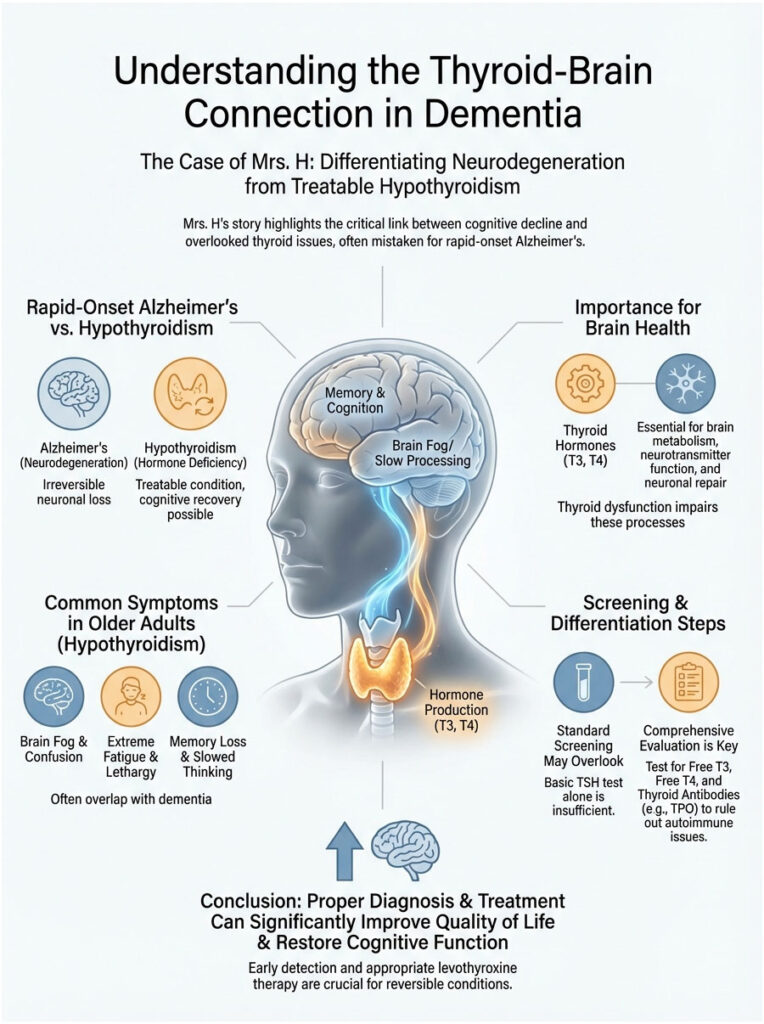
“She is just gone,” the daughter told me. “In six months, she went from doing crosswords to staring at walls. Her primary care doctor says it is rapid-onset Alzheimer’s.”
But something about the story did not add up. Alzheimer’s disease rarely sprints. It creeps. I looked closely at Mrs. H’s hands. They were puffy. Her skin was dry as parchment. I ordered a simple blood panel, and the results told a different story. Her Thyroid-Stimulating Hormone (TSH) was sky-high.
Mrs. H did not have Alzheimer’s. She had severe hypothyroidism, a condition often called the “great masquerader” of geriatric medicine.
Three months of Levothyroxine later, Mrs. H was back to complaining about the hospital food. She was herself again.
This article is not just about a small gland in your neck. It is about saving minds. We are going to break down the thyroid-brain connection, explain why standard screenings often fail older adults, and give you a clear roadmap for telling the difference between permanent neurodegeneration and a treatable metabolic problem.
Key Statistics You Should Know
- 10-15%: Estimated percentage of adults over 60 with some form of thyroid dysfunction.
- 5:1: The ratio of women to men affected by thyroid issues in the geriatric population.
- 20%: Percentage of hypothyroid seniors who present with purely psychiatric or cognitive symptoms, with no physical signs at all.
- 6 Weeks: Typical time for TSH levels to normalize after starting treatment.
- 3-6 Months: Time often required for full cognitive recovery once hormone levels are restored.
The Thyroid-Brain Connection: Why It Matters More as You Age
How Thyroid Hormones Keep the Brain Running
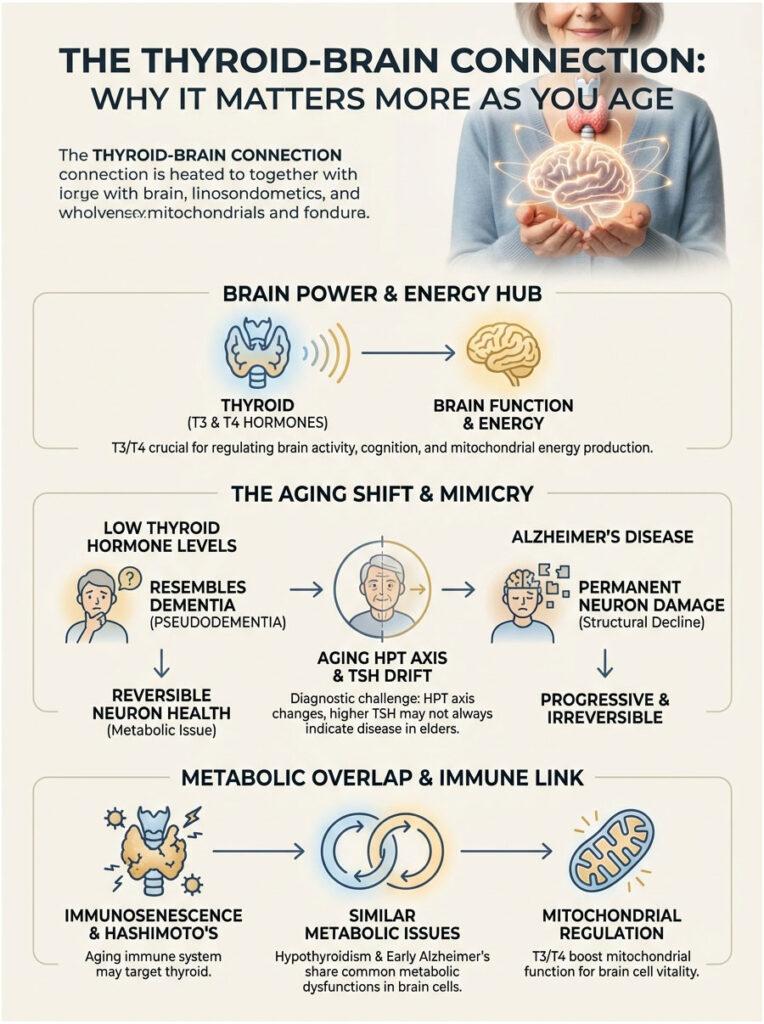
To understand why low thyroid hormone looks so much like dementia, you first need to appreciate what the brain demands. The brain is an energy-hungry organ. It burns through massive amounts of glucose and oxygen every day. Thyroid hormones, specifically Triiodothyronine (T3) and Thyroxine (T4), are what keep that engine running.
T3 crosses the blood-brain barrier and binds to nuclear receptors inside neurons. It controls the genes responsible for myelination (the insulation around nerve fibers) and neurotransmitter production. When T4 levels drop, the brain’s conversion to active T3 also drops. The effects are immediate: cerebral blood flow decreases and the production of serotonin and norepinephrine slows down.
This creates a state of “brain fog” that clinicians call endocrine-induced pseudodementia. Here is the critical distinction: unlike Alzheimer’s, where neurons actually die, the brain’s hardware remains intact in hypothyroidism. The power supply is simply too weak. Think of it this way: the lights are dim, but they are not broken.
What Happens to the Hypothalamic-Pituitary-Thyroid (HPT) Axis with Age
Aging changes the way our glands communicate with each other. In a healthy younger person, the pituitary gland sends a clear signal (TSH) telling the thyroid to produce hormones. If the thyroid is sluggish, the pituitary responds by raising TSH levels.
In older adults, this feedback loop shifts. We frequently see what is known as “TSH drift.” Research published in Nature Reviews Endocrinology suggests that TSH naturally rises with age, even in healthy centenarians. This creates a real diagnostic gray zone. Is a TSH of 5.5 mIU/L a sign of thyroid failure, or is it just normal aging?
On top of that, “immunosenescence,” the gradual decline of the immune system, can trigger late-onset autoimmune attacks on the thyroid. This can lead to Hashimoto’s Thyroiditis in people who never had thyroid problems before.
Mitochondria, Thyroid Hormone, and Neural Aging
Your brain cells are packed with mitochondria, the power plants of every cell. Thyroid hormone is the primary regulator of mitochondrial biogenesis. In elderly individuals with hypothyroidism, these cellular power plants begin to shut down.
This shutdown closely mimics the metabolic defects seen in early Alzheimer’s disease. In fact, some researchers refer to Alzheimer’s as “Type 3 Diabetes” because of the glucose handling problems it involves. Hypothyroidism causes a strikingly similar failure of glucose uptake.
That is why a PET scan of a severely hypothyroid brain can look frighteningly similar to an Alzheimer’s brain. Both show “cold” spots of low metabolic activity. The critical difference? One condition is reversible.
Apathetic Hypothyroidism: The Silent Symptoms Most Doctors Miss
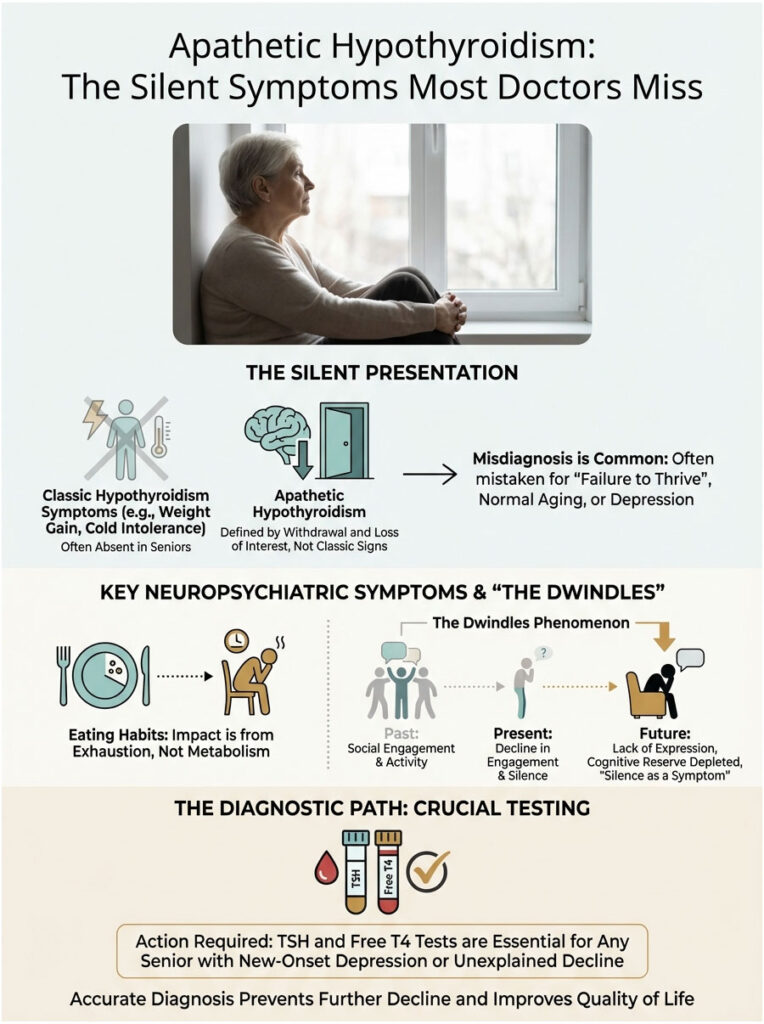
Why the Classic Signs Are Often Absent in Seniors
If you are looking for a goiter or major weight gain, you will likely miss the diagnosis in an older patient. Hypothyroidism in elderly patients rarely shows up with the textbook symptoms you might see in a 30-year-old.
What we see instead is a pattern known as apathetic hypothyroidism. The patient is not necessarily gaining weight. They are losing interest. They become withdrawn, frail, and stop eating, not because their metabolism has slowed, but because they are simply too exhausted to lift a fork. This withdrawal frequently gets mislabeled as “failure to thrive” or just “getting old.”
Neuropsychiatric Symptoms vs. Physical Signs
In geriatric medicine, the symptoms that matter most are the ones affecting the mind and mood.
- Cognitive Symptoms: Short-term memory loss is common. More importantly, you will notice bradyphrenia, or slowed thinking. It takes the patient longer to process a question and form an answer. Executive function, the ability to plan and organize, often suffers early.
- Psychiatric Symptoms: Depression is the most common mimic. This depression, however, is often resistant to SSRIs. In severe cases, patients may develop paranoia or visual hallucinations, a condition historically called “myxedema madness.”
- Physical Red Flags: Watch for unexplained falls. Low thyroid hormone causes proximal muscle weakness, particularly in the legs and hips. If a senior is falling and also has severe constipation or worsening heart failure, check the thyroid.
Expert Insight: “If a patient presents with new-onset depression after age 65, do not prescribe an antidepressant without first seeing a TSH and Free T4 result. Geriatric hypothyroidism is a notorious cause of treatment-resistant depression.”
The “Dwindles” Phenomenon
Geriatricians often use the term “the dwindles” to describe a nonspecific decline. A senior who was previously active suddenly stops going to bridge club, stops calling the grandchildren, and spends hours sleeping in a recliner.
In younger patients, hypothyroidism tends to cause agitation or vocal complaints about fatigue. In the elderly, it causes silence. And that silence is dangerous. Family members often believe the patient is content or simply slowing down. In reality, the person is trapped in a low-energy state, lacking the cognitive reserve to even describe what they are going through.
Diagnostic Dilemmas: Is It Dementia, Depression, or the Thyroid?
The Challenge of Overlapping Symptoms
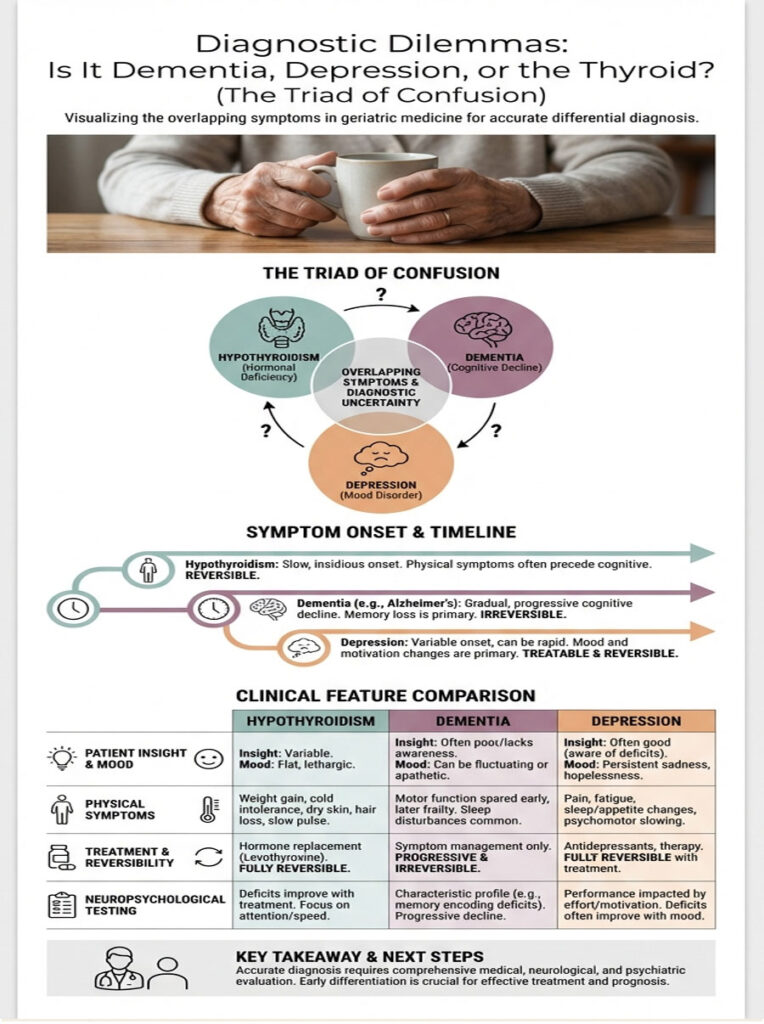
This is one of the hardest parts of geriatric medicine. We call it the “Triad of Confusion”: hypothyroidism in the elderly, major depressive disorder, and dementia (Alzheimer’s or vascular). All three can look almost identical from the outside.
We use screening tools like the Mini-Mental State Examination (MMSE), but a hypothyroid patient will fail this test just like an Alzheimer’s patient. The difference is why they fail. An Alzheimer’s patient fails because the memory is actually gone. A hypothyroid patient fails because they cannot gather the energy to focus on the question.
Timing is your best clue. Cognitive symptoms caused by thyroid issues tend to develop over months, in what we call a sub-acute timeline. True Alzheimer’s is insidious, progressing slowly over years. If your mother was sharp at Christmas and confused by Easter, think thyroid. Think infection. Think medication interaction. Do not jump straight to Alzheimer’s.
Differential Diagnosis: A Side-by-Side Comparison
| Clinical Feature | Hypothyroidism (Pseudodementia) | Alzheimer’s Disease | Geriatric Depression |
| Onset Speed | Sub-acute (months) | Insidious/slow (years) | Variable (weeks to months) |
| Patient Insight | Complains of loss (“I can’t think”) | Denies loss (anosognosia) | Highlights failures (“I don’t know”) |
| Mood State | Apathetic, sluggish, “flat” affect | Fluctuating, anxious, or unconcerned | Sad, hopeless, negative rumination |
| Physical Symptoms | Cold intolerance, dry skin, constipation | Generally healthy in early stages | Sleep disturbances, weight change |
| Response to Treatment | Reversible with hormone replacement | Symptom management only; irreversible | Reversible with antidepressants |
Neuropsychological Testing: Subtle but Important Differences
When we look more closely with detailed cognitive testing, subtle differences emerge. In Alzheimer’s disease, the core deficit is in “encoding.” New information never makes it into the brain’s memory library. You can offer a hint, but it will not help.
In hypothyroidism, the problem is “retrieval.” The information is stored in the library, but the librarian is asleep. If you give a hypothyroid patient a cue or hint, they can often pull up the memory. This “cue-response” pattern is a critical differentiator. It tells us the neural pathways are intact, just sluggish.
Understanding TSH Reference Ranges in Older Adults
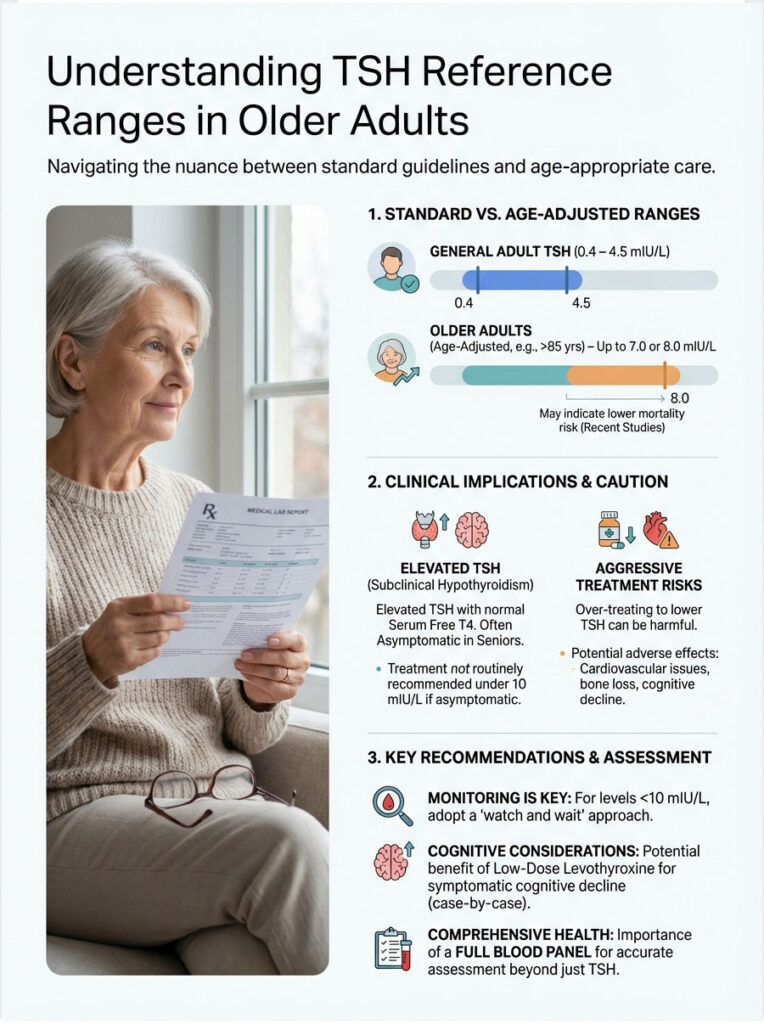
The Debate Over What Counts as “Normal”
This is where the medical community does not fully agree. The standard lab reference range for TSH is usually 0.4 to 4.5 mIU/L. If you are 30 and your TSH comes back at 6.0, you are hypothyroid. But what if you are 85?
There is growing evidence supporting age-adjusted TSH reference ranges. Data from the Leiden 85-plus Study suggests that in the oldest-old, a slightly elevated TSH may actually be protective. Levels up to 7.0 or even 8.0 mIU/L have been associated with lower mortality in this age group. The body may be intentionally slowing metabolism to conserve resources. Treating these patients aggressively to bring their TSH down to a “young” target of 2.0 can actually cause harm.
Subclinical Hypothyroidism: When to Treat and When to Wait
Subclinical hypothyroidism in seniors is defined as an elevated TSH paired with a normal Serum Free T4. The Endocrine Society guidelines generally recommend a “wait and see” approach for TSH levels under 10 mIU/L in patients over 75, as long as they are asymptomatic.
However, when cognitive decline enters the picture, the calculation shifts. If a patient has memory loss and a TSH of 8.0, many geriatricians will offer a trial of low-dose Levothyroxine to see if cognition improves. It comes down to a risk-benefit analysis: the risk of untreated endocrine-induced pseudodementia typically outweighs the risk of cautious treatment.
The Full Blood Panel Every Senior Needs
Do not settle for just a TSH test. You need the full picture to make an informed decision.
- TSH (High Sensitivity): The first line of defense.
- Serum Free T4: Essential for confirming how much active hormone is actually available to the brain.
- TPO Antibodies: Tests for Hashimoto’s Thyroiditis. Autoimmune thyroid disease is surprisingly common in late-onset cases.
- Reverse T3: Elevated levels can indicate “Euthyroid Sick Syndrome,” a state where the body poorly clears thyroid hormone due to other illnesses.
- Vitamin B12 and Folate: Low thyroid function often impairs B12 absorption. Since B12 deficiency also mimics dementia, this must be ruled out.
Treating Hypothyroidism in the Elderly: The “Start Low, Go Slow” Approach
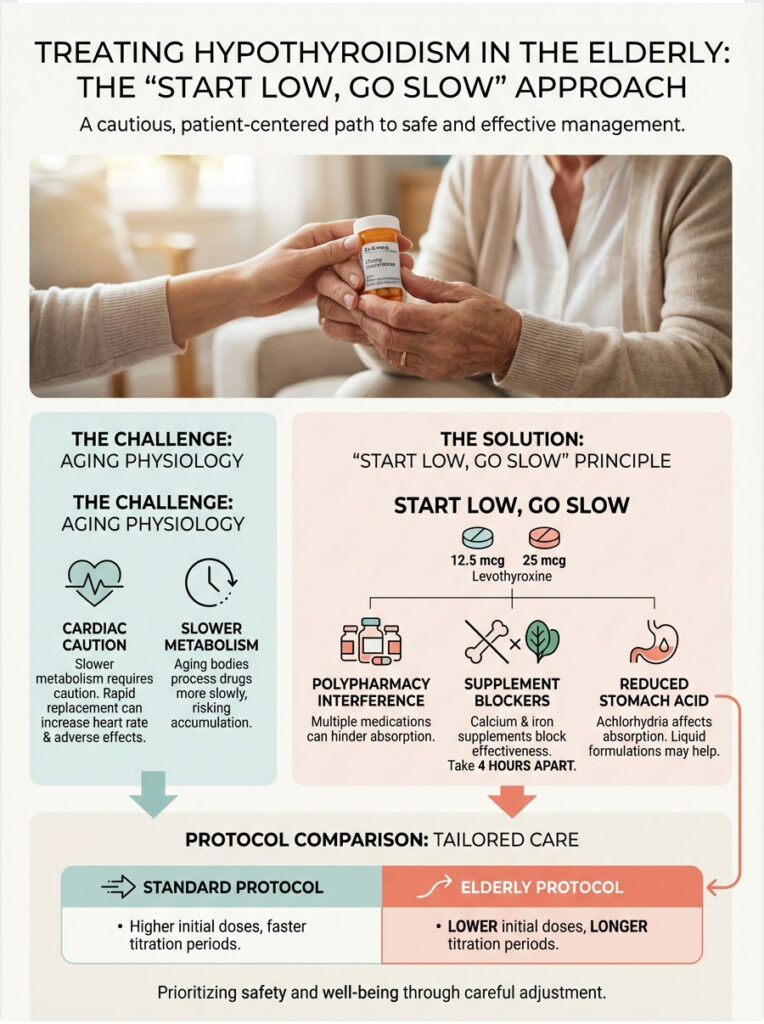
Why the Aging Heart Requires Extra Caution
Treating geriatric hypothyroidism is not the same as treating a 40-year-old. Seniors metabolize drugs more slowly, and their hearts are stiffer. Thyroid hormone replacement increases metabolic demand and heart rate, so rushing in with a full replacement dose risks triggering angina or, even worse, iatrogenic atrial fibrillation, an irregular heartbeat that can cause strokes.
The golden rule is “Start Low, Go Slow.” We typically begin with 12.5 mcg or 25 mcg of Levothyroxine, a fraction of the standard adult dose. The goal is to wake the body up gently, not shock it.
Absorption Problems in Elderly Patients
Even if the dose is correct, it may not be reaching the bloodstream effectively. Polypharmacy interactions are a major challenge in geriatrics. Calcium carbonate, iron supplements, proton pump inhibitors (PPIs) for acid reflux, and cholesterol binders can all block thyroid medication absorption.
On top of that, stomach acid production decreases with age, a condition called achlorhydria. Levothyroxine tablets need acid to dissolve properly. For some seniors, switching to a liquid gel capsule or liquid formulation can help bypass this absorption issue. We also advise patients to take their thyroid medication at least 4 hours apart from other supplements.
Treatment Protocol Comparison: Standard vs. Geriatric
| Treatment Parameter | Standard Adult (Under 60) | Geriatric Protocol (Over 70) |
| Initial Dosage | Full dose (1.6 mcg/kg body weight) | Low dose initiation (12.5 mcg – 25 mcg) |
| Titration Schedule | Adjust every 4-6 weeks | Adjust every 6-8 weeks (slower equilibration) |
| Target TSH Goal | 0.4 – 2.5 mIU/L | 3.0 – 6.0 mIU/L (age-dependent) |
| Primary Risk Concern | Under-treatment (lingering symptoms) | Over-treatment (atrial fibrillation, bone loss) |
Reversing Cognitive Decline: What Families Should Expect
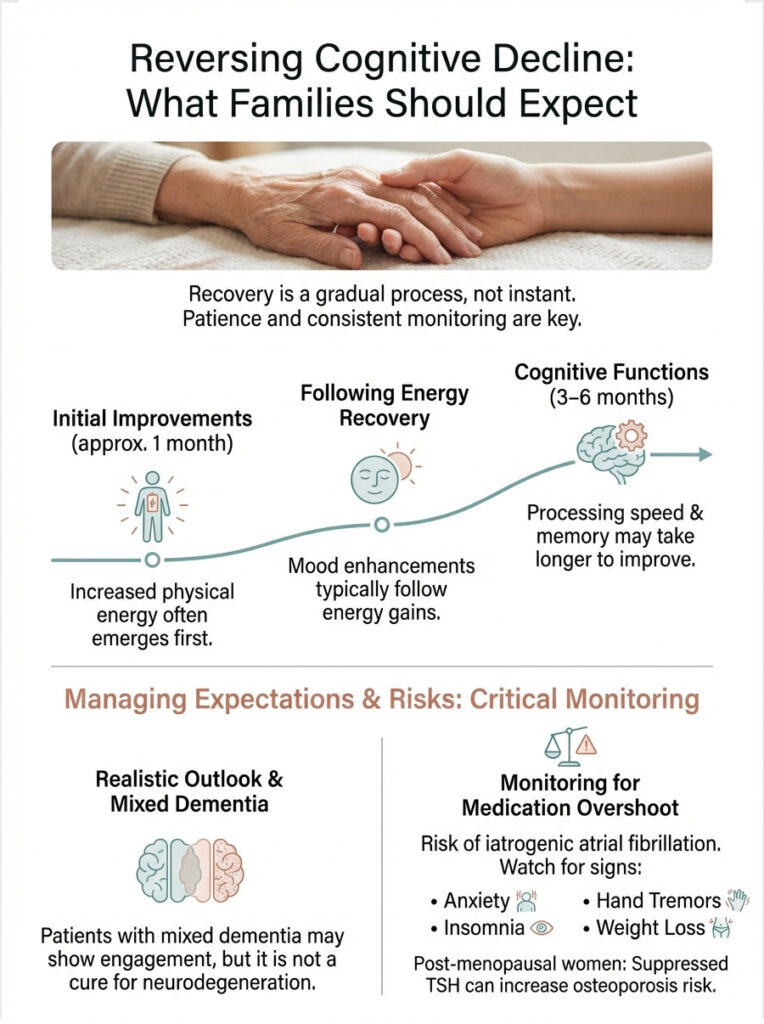
The Realistic Timeline for Recovery
Families often hope for a “Lazarus moment,” expecting Mom to wake up three days after taking the first pill. Realistically, reversing cognitive decline from hypothyroidism takes time. Blood levels of TSH may look better within 6 weeks, but the brain takes much longer to repair the metabolic damage.
Most patients and families notice physical energy returning first, usually within a month. Mood tends to improve next. Cognitive processing speed and memory are the last functions to bounce back, often requiring 3 to 6 months of stable euthyroid (normal thyroid) status.
It is important to manage expectations here. If the patient has mixed dementia, meaning Alzheimer’s plus a thyroid problem, the medication will improve alertness and engagement but will not cure the underlying neurodegeneration.
Monitoring for Overshoot
Because iatrogenic atrial fibrillation is a serious risk, we monitor patients closely during treatment. Signs that the medication dose has overshot the mark include new anxiety, hand tremors, insomnia, and sudden weight loss. In post-menopausal women, a suppressed TSH can also accelerate osteoporosis risk. Clinicians are constantly balancing the need for cognitive clarity against the health of the heart and bones.
Myxedema Coma: The Worst-Case Scenario
When hypothyroidism in elderly patients goes untreated for years, the consequences can be severe. A patient with depleted thyroid reserves who faces a sudden stressor, such as a urinary tract infection, pneumonia, or a fall in cold weather, can be pushed into myxedema coma.
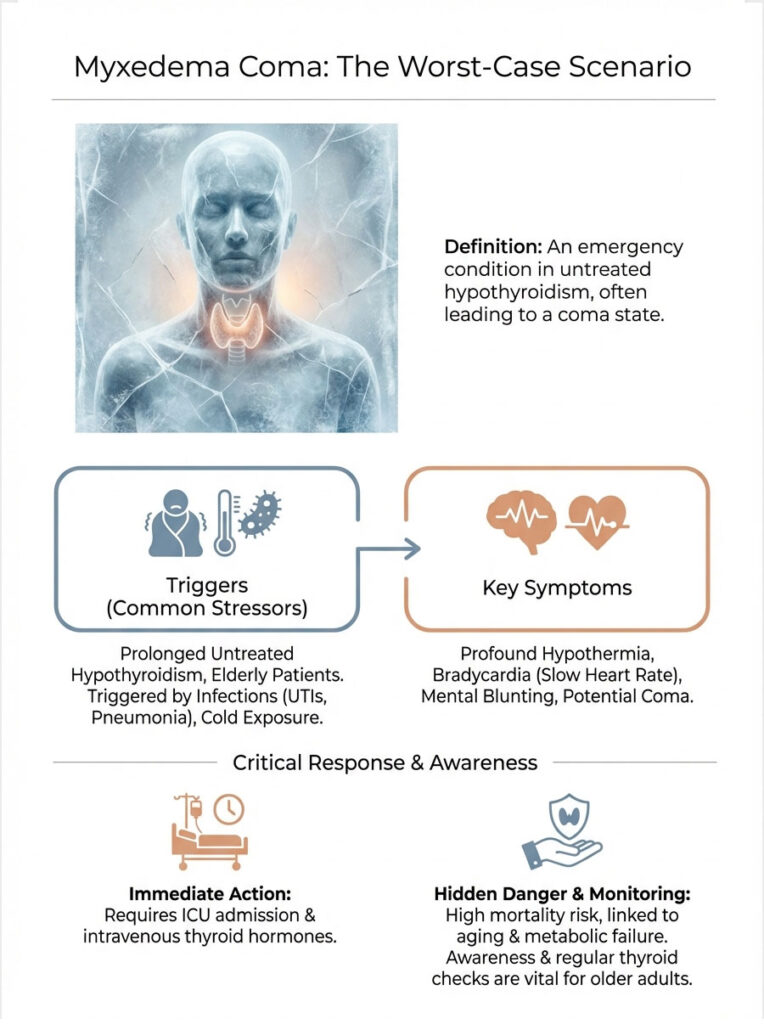
This is a medical emergency and represents the end stage of the disease. Symptoms include profound hypothermia (dangerously low body temperature), bradycardia (slow heart rate), and mental blunting that can progress to actual coma. Mortality rates are high, and it requires immediate ICU admission with intravenous thyroid hormones.
It is a rare complication, but it underscores why “just getting old” is a dangerous diagnosis when metabolic failure may be the real culprit.
The Role of Nutrition and Lifestyle in Supporting Thyroid Health
While medication is the cornerstone of treatment, lifestyle and nutrition play an important supporting role. The elderly brain needs specific nutrients to convert T4 into active T3. Selenium and zinc are critical co-factors in this conversion process. A diet lacking in these minerals can make thyroid medication less effective.
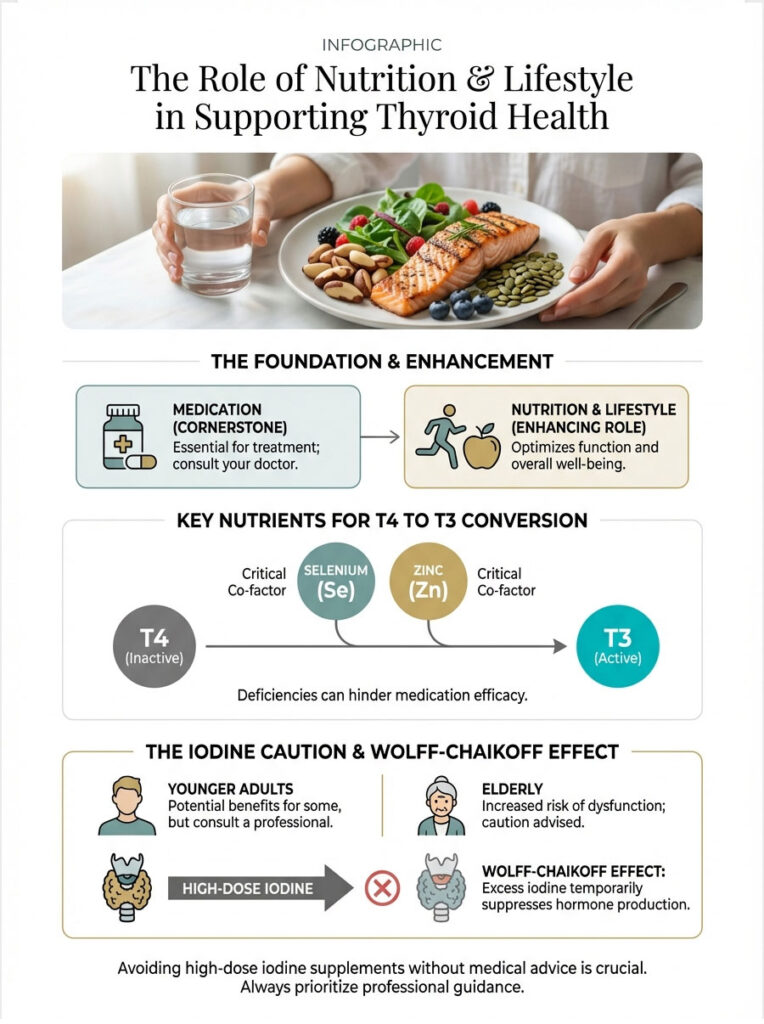
A word of caution about iodine: in younger people, iodine fuels the thyroid gland. In the elderly, especially those with underlying autoimmune thyroid disease, excess iodine can actually be toxic. High doses from supplements can further shut down the thyroid gland, a reaction known as the Wolff-Chaikoff effect. Seniors should avoid high-dose iodine supplements unless specifically prescribed by their doctor.
Key Takeaways: Protecting Elderly Loved Ones from Misdiagnosis
Hypothyroidism in elderly populations is a reversible cause of suffering that hides in plain sight. It mimics the very conditions we fear most: dementia and depression. But unlike Alzheimer’s, this is a problem we can fix.
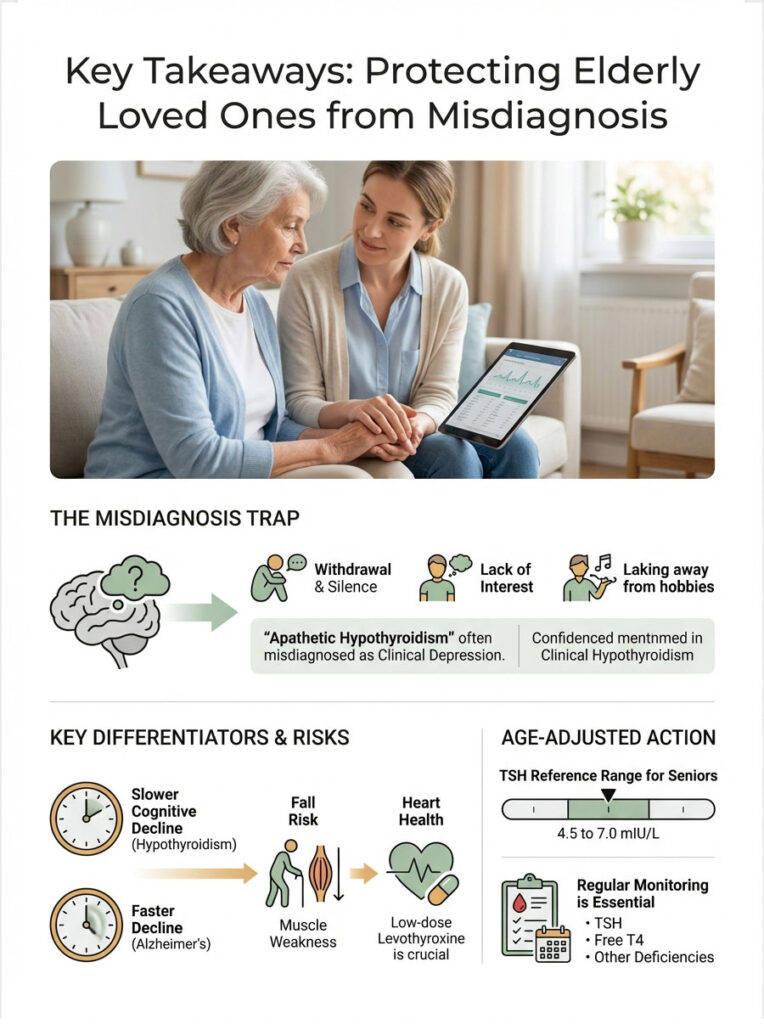
The apathetic nature of the symptoms, including withdrawal, silence, and slowness, means the quiet patient is the one who gets overlooked. The grandmother who stops talking gets ignored while the one who complains gets attention. As caregivers and clinicians, we have to stay vigilant.
- Advocate: If memory declines suddenly, demand a full thyroid panel (TSH + Free T4). Do not accept “it is just aging” as an answer.
- Contextualize: Understand that TSH ranges change with age. What is normal for a 30-year-old is not normal for an 80-year-old.
- Be Patient: Treatment follows the “Start Low, Go Slow” rule to protect the heart. Reversible dementia takes months to fully clear.
- Watch the Heart: Monitor for signs of over-treatment, including rapid heartbeat, anxiety, and unexplained weight loss.
Frequently Asked Questions
How can I tell if a senior has dementia or a thyroid issue?
The primary differentiator is the speed of onset; hypothyroidism-induced cognitive decline usually develops over months, whereas Alzheimer’s is typically an insidious process spanning years. Additionally, hypothyroid patients often exhibit “retrieval” issues where they can remember facts with a cue, unlike the “encoding” failure seen in true neurodegeneration.
What is apathetic hypothyroidism in elderly patients?
Unlike younger patients who present with weight gain and agitation, seniors often display “apathetic hypothyroidism,” characterized by extreme withdrawal, silence, and a lack of interest in daily activities. This clinical phenotype is frequently misdiagnosed as “failure to thrive” or clinical depression because the classic physical symptoms are often absent.
What is the recommended TSH reference range for someone over age 70?
In geriatric medicine, we utilize an age-adjusted TSH reference range because a slightly elevated TSH (between 4.5 and 7.0 mIU/L) may actually be protective in the oldest-old. We generally avoid aggressive treatment for subclinical levels unless the patient is symptomatic, as forcing a “young” TSH level can increase the risk of cardiac events.
Why is Levothyroxine started at such a low dose for seniors?
We follow the “start low, go slow” protocol to protect the aging heart, which is highly sensitive to sudden increases in metabolic demand. Starting at a full replacement dose risks inducing iatrogenic atrial fibrillation or angina, so we typically begin with 12.5 to 25 mcg and titrate every 6 to 8 weeks based on serum Free T4 levels.
Can hypothyroidism cause frequent falls in older adults?
Yes, low thyroid hormone levels lead to proximal muscle weakness, particularly in the legs and hips, which significantly increases the risk of unexplained falls. When combined with the slowed cognitive processing, or bradyphrenia, associated with the condition, a senior’s balance and reaction time are severely compromised.
How long does it take for memory to improve after starting thyroid treatment?
While blood chemistry may normalize within six weeks, full cognitive restoration of memory and processing speed often takes three to six months of stable hormone levels. It is a gradual metabolic repair process, and families should look for improvements in physical energy and mood before expecting a full reversal of cognitive slowing.
What is endocrine-induced pseudodementia?
This is a reversible cognitive impairment caused by metabolic failure, where the brain’s “hardware” is intact but the “power supply” provided by thyroid hormones is insufficient. Unlike permanent neurodegenerative diseases, this condition can often be fully reversed once the patient achieves a euthyroid state through proper hormone replacement therapy.
What medications interfere with thyroid hormone absorption in seniors?
Many common geriatric medications, including calcium carbonate, iron supplements, and proton pump inhibitors (PPIs) for acid reflux, can significantly block the absorption of Levothyroxine. To ensure efficacy, these supplements and medications should be taken at least four hours apart from the thyroid hormone dose to prevent pharmacological interaction.
What are the signs of over-treatment with thyroid medication in the elderly?
Clinicians must watch for “overshoot” symptoms such as new-onset anxiety, hand tremors, insomnia, or a rapid, irregular heartbeat. In post-menopausal women, excessive thyroid hormone replacement also carries the long-term risk of accelerating bone mineral density loss and increasing the likelihood of osteoporosis.
Why isn’t a TSH test alone enough for a geriatric thyroid screening?
A comprehensive panel including Serum Free T4 and TPO antibodies is necessary because the HPT axis shifts with age, making TSH alone potentially misleading. We also screen for Vitamin B12 and folate deficiencies simultaneously, as these frequently co-occur with thyroid issues and independently mimic dementia symptoms in seniors.
Is subclinical hypothyroidism in seniors always treated?
Treatment for subclinical hypothyroidism—elevated TSH with normal Free T4—is controversial and usually reserved for patients with clear symptoms or TSH levels above 10 mIU/L. However, if a senior shows signs of cognitive decline or treatment-resistant depression, a trial of low-dose Levothyroxine may be indicated to see if cognition improves.
What is myxedema coma and how does it affect the elderly?
Myxedema coma is a life-threatening medical emergency representing the extreme end-stage of untreated hypothyroidism, often triggered by a secondary stressor like an infection or cold exposure. It manifests as profound hypothermia, a dangerously slow heart rate, and progression into a coma, requiring immediate intensive care intervention.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
References
- Nature Reviews Endocrinology – “Thyroid function and the aging mind” – Detailed analysis of the HPT axis shifts and TSH drift in geriatric populations.
- The Lancet Diabetes & Endocrinology – “Subclinical thyroid dysfunction in older adults” – Comprehensive study on treatment thresholds for seniors over age 75.
- Journal of the American Geriatrics Society (JAGS) – “Apathetic Hypothyroidism in the Elderly” – Research on the neuropsychiatric presentation of thyroid disease in seniors.
- The Leiden 85-plus Study – “Thyroid status at age 85 and beyond” – Longitudinal data showing the protective nature of slightly elevated TSH in the oldest-old.
- Endocrine Society – “Clinical Practice Guidelines: Hypothyroidism” – Official protocols for Levothyroxine initiation and the “start low, go slow” approach.
- American Thyroid Association (ATA) – “Thyroid Disease in the Older Patient” – Clinical resource for identifying the “great masquerader” in geriatric medicine.








