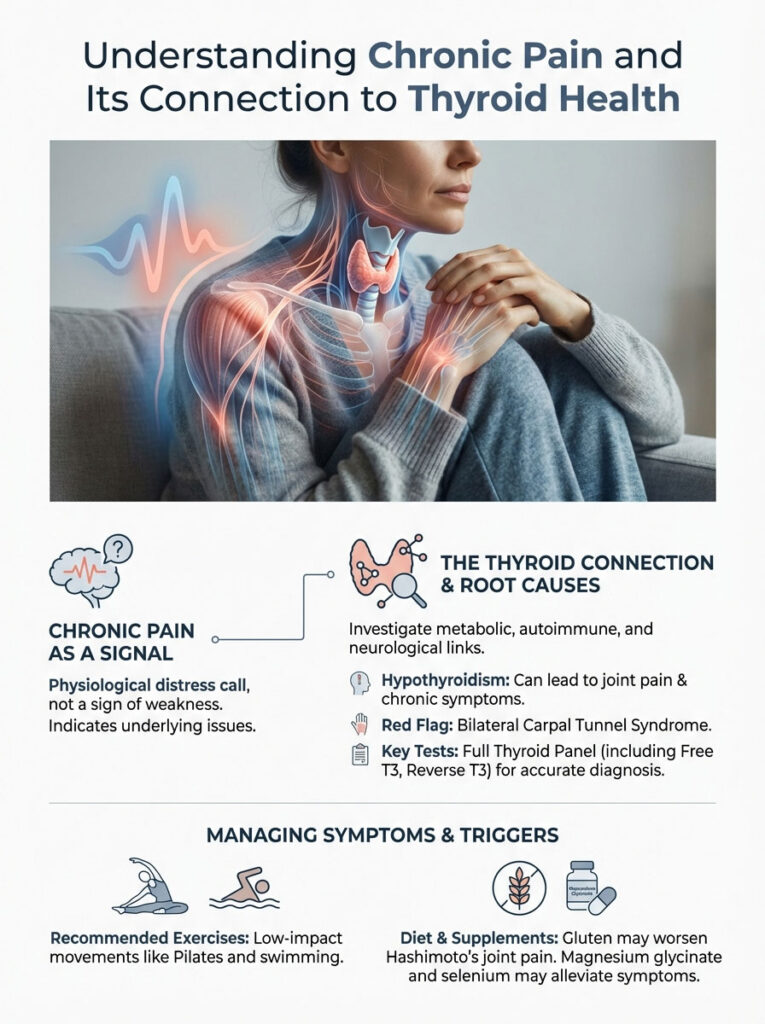
You wake up feeling like you have run a marathon in your sleep. Your muscles ache with a deep, bruising sensation. Your joints feel stiff and boggy. Your brain is struggling to push through a dense fog. For millions of patients, distinguishing between hypothyroidism joint pain and fibromyalgia is the first step toward reclaiming their lives. When you visit your doctor, you might be told your thyroid labs are “normal” based on a standard TSH test.
Table of Contents
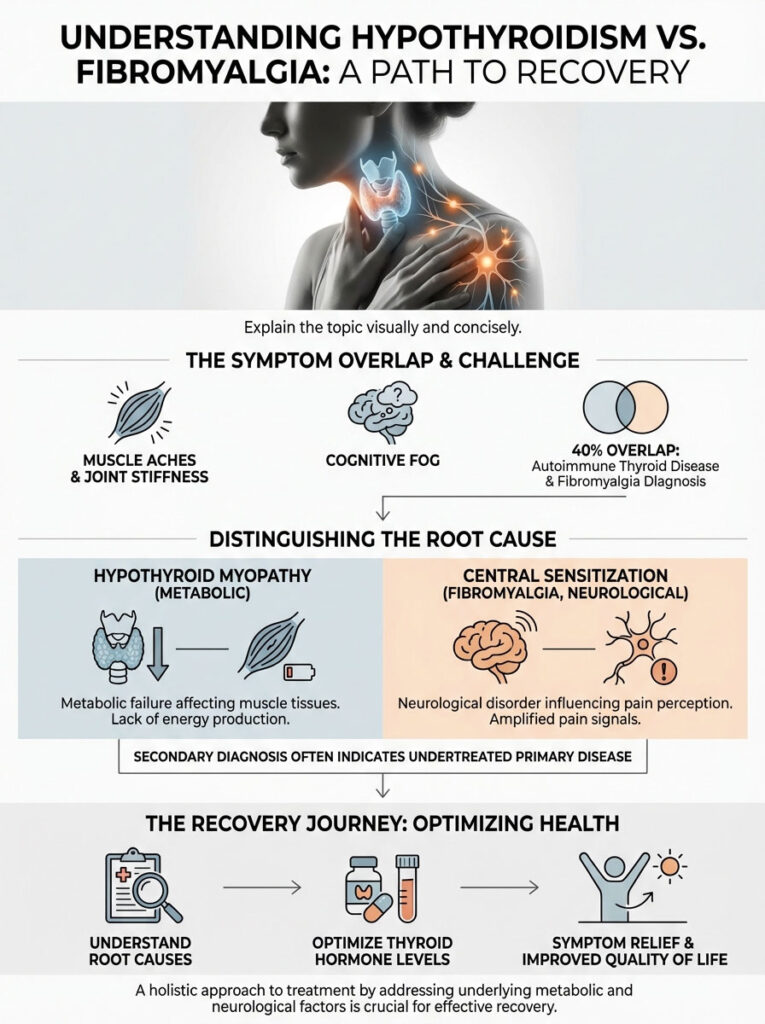
You might leave with a prescription for antidepressants and a diagnosis of fibromyalgia. But if the root cause is metabolic rather than neurological, that treatment plan will fail. Understanding the subtle physiological differences is the single most important factor in your recovery journey.
The Core Difference
Hypothyroid Myopathy is a metabolic failure. Muscle tissues physically clog with mucin-like substances called glycosaminoglycans due to a lack of thyroid hormone. This causes swelling, fluid retention, and objective weakness. Central Sensitization (Fibromyalgia) is a neurological disorder. The brain’s pain processing center turns the “volume” up too high. This causes non-painful stimuli to hurt. Treatment requires identifying if the issue is in the tissues or the nerves.
The overlap is statistically significant and clinically confusing. Research suggests that up to 40% of patients with autoimmune thyroid disease may eventually receive a secondary fibromyalgia diagnosis. However, a “secondary” diagnosis does not always mean you have two distinct diseases. It often means the primary disease is undertreated. If your thyroid hormone levels are not optimized for your unique physiology, you will experience systemic pain that mimics central sensitization perfectly.
Key Statistics: The Pain Landscape
- 40%: The percentage of Hashimoto’s patients who meet the criteria for Fibromyalgia.
- 25%: The estimated prevalence of carpal tunnel syndrome in hypothyroid patients.
- 5-10 Years: The average time it takes to receive a correct diagnosis for autoimmune conditions.
- 30-80%: The percentage of hypothyroid patients who develop myopathy (muscle disease).
- 90%: The percentage of hypothyroid cases in the USA caused by Hashimoto’s Autoimmune Thyroiditis.
The Diagnostic Dilemma: Why Doctors Miss It
The journey to a correct diagnosis is often fraught with frustration. You know your body better than anyone else. You know that the pain you feel is not just “in your head.” Yet, standard medical training often compartmentalizes symptoms. An endocrinologist looks at your glands. A rheumatologist looks at your joints. A neurologist looks at your nerves. Rarely does one specialist look at how all three interact.
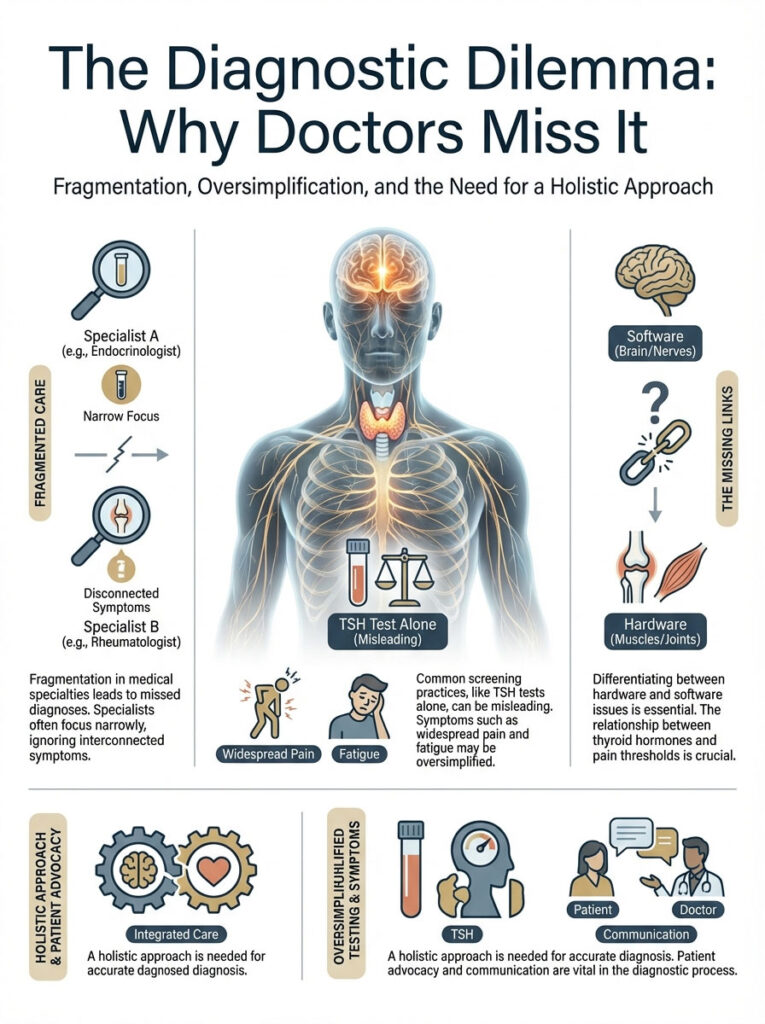
This fragmentation leads to missed opportunities. A patient presenting with widespread body aches and fatigue is often screened for thyroid issues using only a TSH test. If that number falls within the broad reference range, the thyroid is ruled out. The pain is then labeled “idiopathic” or “fibromyalgia.” This is a dangerous oversimplification. It ignores the cellular reality of how thyroid hormones dictate pain thresholds and tissue integrity.
We need to look deeper. We need to understand the biology of the pain itself. Is it a hardware problem (the muscles and joints)? Or is it a software problem (the brain and nerves)?
The Biological Mechanism: Why Hypothyroidism Hurts
To understand why hypothyroidism joint pain feels the way it does, we must look at the cellular environment. This is not simply “inflammation” in the way you might think of a sprained ankle. It is a fundamental change in the structural integrity of your tissues.
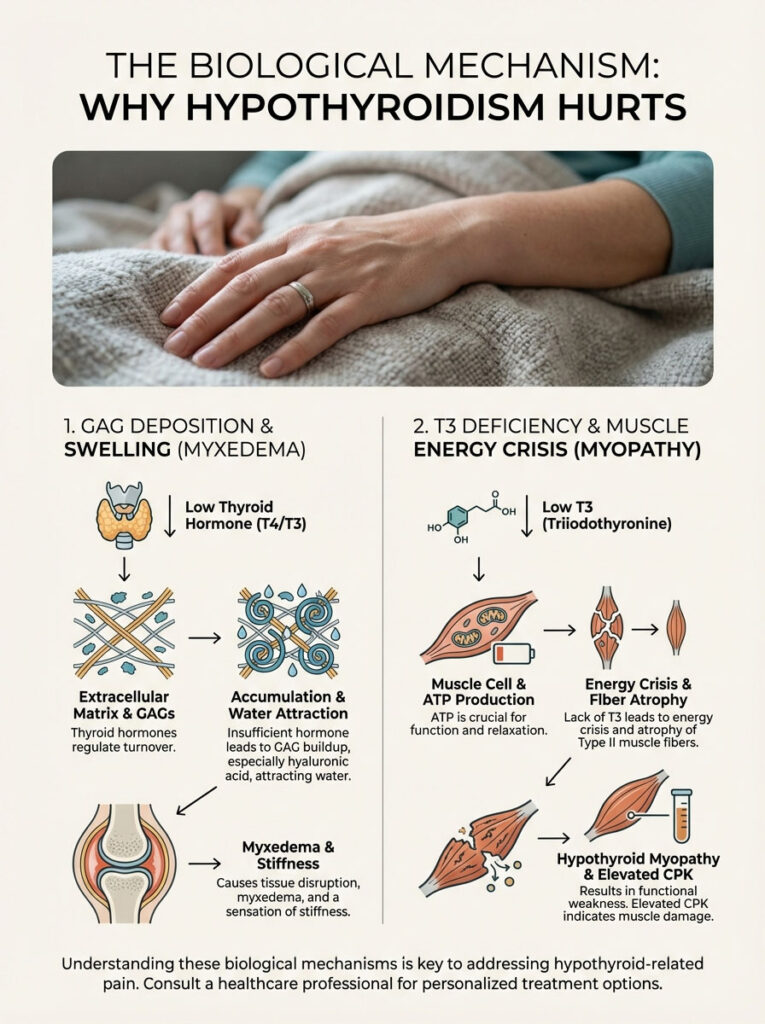
Glycosaminoglycan (GAG) Deposition
In a healthy body, thyroid hormones regulate the turnover of the extracellular matrix. This is the scaffolding that holds your cells together. When thyroid hormone is insufficient, your body loses the ability to break down specific sugar-protein complexes called glycosaminoglycans (GAGs). The most common of these is hyaluronic acid. These substances accumulate in the interstitial spaces between your muscle fibers and joints.
Here is the problem: GAGs are highly hydrophilic. This means they attract water. As they build up in your tissues, they pull fluid with them. This results in myxedema, a specific type of non-pitting edema. Imagine your muscle fibers being soaked in a thick, gel-like substance. This substance expands and compresses everything around it. This creates a sensation of stiffness that feels like you are wearing a heavy, wet wetsuit. The pain is mechanical. It comes from pressure and fluid retention within the muscle compartments themselves.
Hypothyroid Myopathy and Muscle Energetics
Beyond the structural clogging, there is an energy crisis. Thyroid hormone (specifically T3) is required for mitochondria to produce ATP. ATP is the energy currency of your cells. In a state of hypothyroid myopathy, your muscles literally run out of fuel. This leads to a shift in muscle fiber composition.
We see a preferential atrophy of Type II (fast-twitch) muscle fibers. These are the fibers responsible for explosive movement and strength. When these atrophy, you experience specific functional weaknesses. You might have difficulty climbing stairs. You might struggle to lift your arms to wash your hair. This is distinct from the generalized “pain” of fibromyalgia. It is objective, measurable weakness. Furthermore, the muscle membranes become unstable. Enzymes like Creatine Phosphokinase (CPK or CK) leak into the bloodstream. Elevated CPK is a hallmark of hypothyroid muscle damage that is rarely seen in pure fibromyalgia.
The Calcium Connection
There is another layer to this metabolic failure. Muscle relaxation requires energy. It is an active process. Calcium must be pumped out of the muscle cells for them to relax after a contraction. This pump is driven by ATP. When you are hypothyroid, you lack ATP. The calcium stays stuck inside the cell. This causes the muscle fibers to remain in a semi-contracted state. This manifests as chronic cramps, “charley horses,” and a relentless, deep ache that massage rarely fixes.
The Neurological Mechanism: Understanding Fibromyalgia
While hypothyroidism is a tissue issue, fibromyalgia is a processing issue. Understanding fibromyalgia vs hypothyroidism requires accepting that pain can exist without tissue damage.
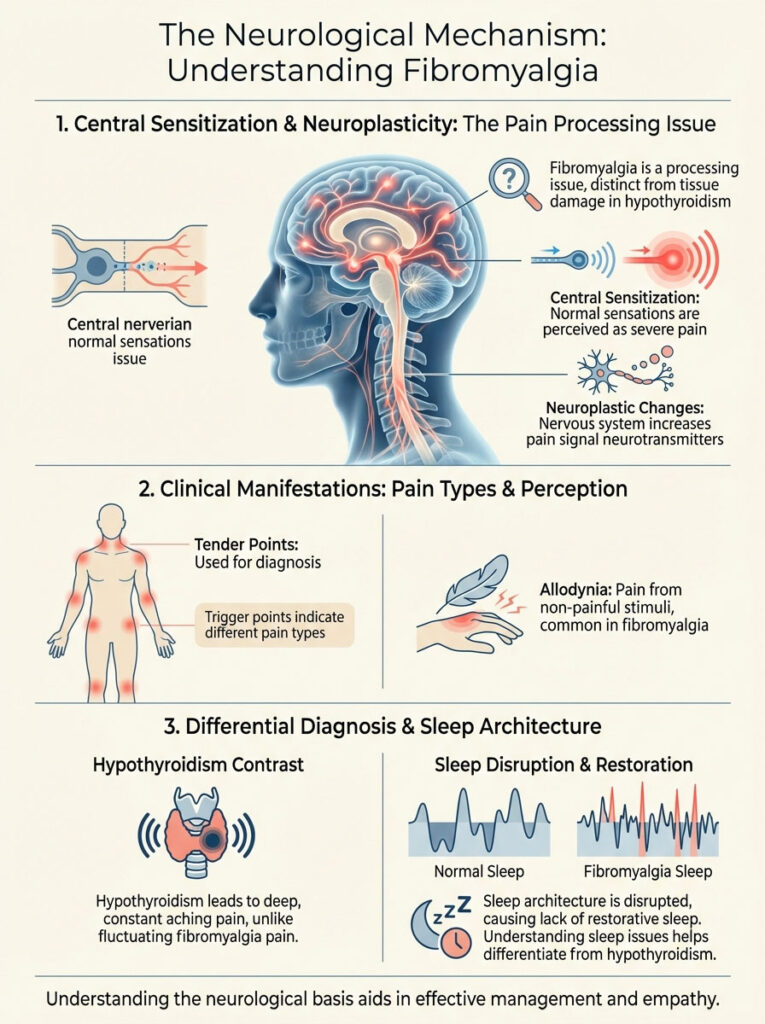
Central Sensitization Explained
In fibromyalgia, the hardware (your muscles and joints) is often structurally sound. But the software (the nervous system) is glitching. This is known as central sensitization. Imagine a radio where the volume knob is stuck on maximum. A gentle breeze, a light touch, or a minor temperature change sends a signal to the brain. The brain interprets this signal as severe pain.
This occurs due to neuroplastic changes in the dorsal horn of the spinal cord and the brain. Neurotransmitters that signal pain, such as Substance P and Glutamate, are present in higher concentrations in the spinal fluid of fibromyalgia patients. The brain loses its ability to inhibit these signals. Therefore, the pain is real. But the origin is not in the knee or the elbow. The origin is in the neural pathway reporting on the knee and elbow.
The “Tender Point” vs. “Trigger Point” Distinction
Historically, doctors used 18 “tender points” to diagnose fibromyalgia. While the American College of Rheumatology has updated these criteria to focus on widespread pain indices, the concept remains relevant. Fibromyalgia pain is often accompanied by allodynia. This is pain from stimuli that should not be painful. The pressure of a bra strap or a waistband can feel like a knife.
In contrast, hypothyroidism joint pain is usually a deep, constant ache. It does not fluctuate wildly with a light touch. It feels like it is coming from the bone or the deep muscle belly. It feels heavy. It feels like gravity is pulling on you twice as hard as everyone else.
Sleep Architecture and Pain
Sleep plays a massive role here. Fibromyalgia patients suffer from “alpha-delta intrusion.” This means their deep sleep is constantly interrupted by awake-brain waves. They never get physically restorative sleep. This lack of sleep lowers the pain threshold even further. Hypothyroid patients also sleep poorly. But their issue is often related to sleep apnea (due to swollen throat tissues) or temperature dysregulation. Understanding *why* you are tired can help pinpoint the diagnosis.
Clinical Showdown: Distinguishing the Symptoms
Both conditions cause fatigue, brain fog, and depression. This is where the diagnostic waters get murky. However, the quality of the physical symptoms differs significantly if you know what to look for. You have to be a detective in your own health journey.
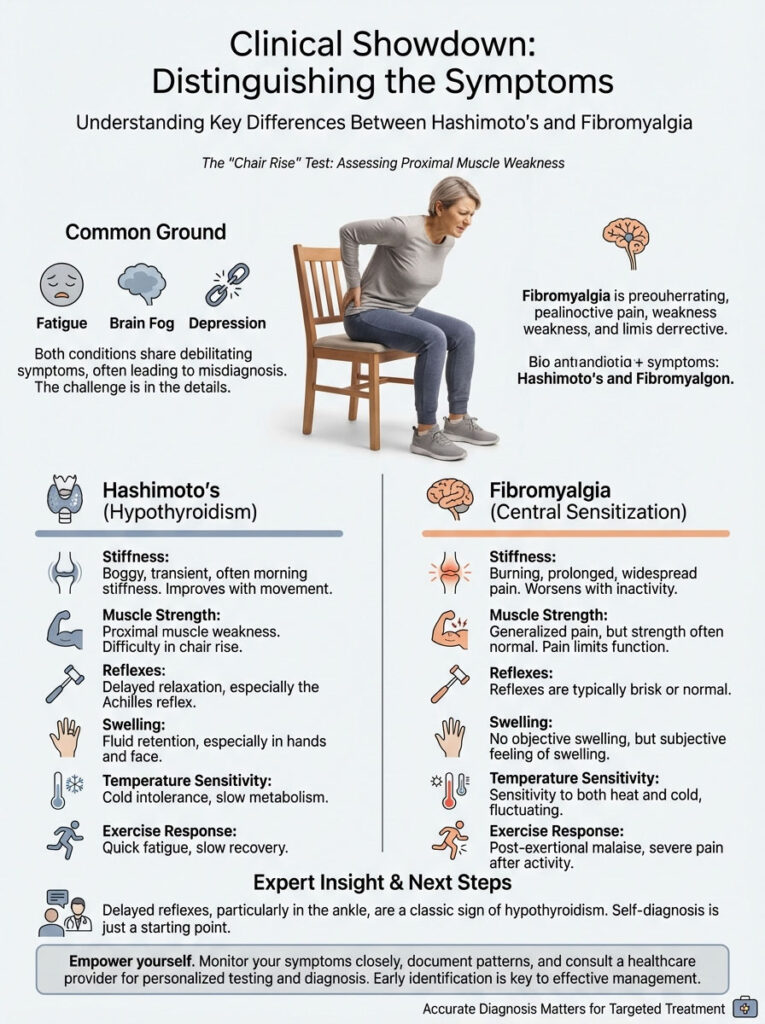
The Nature of the Stiffness
Morning stiffness is common in both. But the duration and sensation vary. In Hashimoto’s joint pain, the stiffness is often described as “boggy.” It improves slightly as you move and fluid is pumped out of the tissues. But it returns immediately if you sit still or become fatigued. It is a heavy sensation.
In fibromyalgia, the stiffness is often prolonged. It can last more than an hour in the morning. It is highly reactive to external factors like barometric pressure changes, stress, or lack of sleep. Patients often describe it as a “burning” stiffness rather than a “swollen” stiffness. It feels electrical.
The “Chair Rise” Test (Proximal Muscle Weakness)
Here is a practical way to test yourself at home. Proximal muscle weakness is a classic sign of hypothyroid disease. The proximal muscles are those closest to the center of your body. These are your hips, thighs, and shoulders. Hypothyroid patients often struggle to rise from a squatting position without using their hands for support. They may find it exhausting to hold a hairdryer up for five minutes.
Fibromyalgia patients will feel pain while doing these tasks. But their actual muscle strength usually remains intact. If you have objective weakness—meaning your muscles physically fail to perform the task—you should look closely at your thyroid. Can you climb a flight of stairs without your legs feeling like lead? If not, check your T3 levels.
Expert Insight: The Reflex Test
Ask your doctor to check your reflexes. Specifically, ask for the Achilles tendon reflex test. In hypothyroidism, we look for “delayed relaxation.” The foot kicks out normally. But it returns to the resting position in slow motion. This delayed relaxation of deep tendon reflexes is almost pathognomonic for hypothyroidism. It is rarely seen in pure fibromyalgia.
Comparison Table 1: Hypothyroidism vs. Fibromyalgia Symptoms
| Symptom | Hypothyroidism (Endocrine) | Fibromyalgia (Neurological) | Clinical Note |
|---|---|---|---|
| Pain Type | Deep, aching, heavy; feels like “growing pains” or bruising. | Burning, shooting, electrical, or prickly; skin sensitivity. | Hypo pain is deep tissue; Fibro pain is often superficial/nerve-based. |
| Muscle Strength | Objective weakness (proximal); difficulty climbing stairs. | Pain-limited effort, but strength is usually normal. | “I can’t lift it” vs. “It hurts to lift it.” |
| Swelling | Visible Myxedema; hands/feet look puffy; rings don’t fit. | Subjective sensation of swelling, but usually no visible fluid. | Look for indentations from socks (hypo). |
| Reflexes | Delayed relaxation phase (slow return). | Normal or Hyperactive (jumpy). | Reflexes are a window into metabolic speed. |
| Temp Sensitivity | Severe cold intolerance; inability to warm up. | Sensitivity to temperature fluctuations (hot or cold). | Hypo patients have low basal body temperature. |
| Exercise Response | Cramping, fatigue, long recovery needed. | Post-exertional malaise; flare-up of widespread pain. | Both struggle with HIIT; both need gentle movement. |
The Critical Red Flag: Bilateral Carpal Tunnel Syndrome
If there is one symptom that should make you demand a full thyroid panel immediately, it is bilateral carpal tunnel syndrome. Carpal tunnel is common in the general population. It usually affects the dominant hand due to repetitive strain from typing or manual labor. However, when it appears in both hands simultaneously, especially without a history of repetitive injury, it is a metabolic red flag.
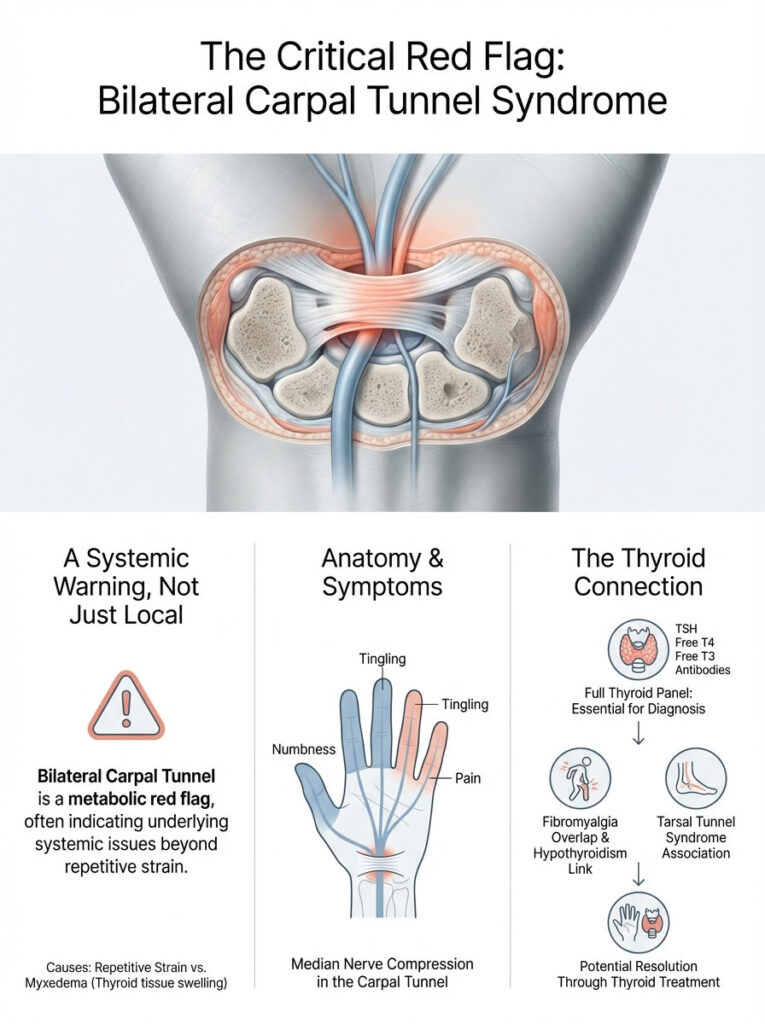
The carpal tunnel is a narrow passageway in your wrist housing the median nerve. Remember the glycosaminoglycan deposition we discussed earlier? When those mucin-like substances build up in the connective tissues of the wrist, they compress the median nerve. This causes numbness, tingling, and pain in the thumb, index, and middle fingers.
This is not a structural injury from overuse. It is a space-occupying lesion caused by myxedema. Treating the thyroid often resolves the carpal tunnel without the need for surgery. If you have been diagnosed with Fibromyalgia but also have numbness in both hands, you must investigate hypothyroidism joint pain as the primary culprit. The same applies to Tarsal Tunnel Syndrome in the feet. If you have plantar fasciitis that never heals, look at your thyroid.
The Diagnostic Roadmap: Labs You Need
The standard of care often fails pain patients because it relies too heavily on the TSH (Thyroid Stimulating Hormone) test alone. TSH is a pituitary hormone. It is not a thyroid hormone. It reflects what the brain is asking for, not necessarily what the tissues are receiving. You can have a “normal” TSH and still have severe hypothyroid myopathy.

Beyond the TSH: The Complete Thyroid Panel
To differentiate Fibromyalgia vs hypothyroidism, you need a granular view of your hormonal status. You must advocate for a full panel.
- TSH: The lab range is usually 0.5 to 5.0 mIU/L. However, the American Association of Clinical Endocrinologists has suggested that a TSH above 2.5 or 3.0 may be abnormal. Many patients report normal TSH but still in pain until their levels are closer to 1.0.
- Free T3 and Free T4: These measure the actual circulating hormones available to your cells. Free T3 is the active hormone that enters the muscle cells to power the mitochondria. Low Free T3 is strongly correlated with chronic pain and muscle stiffness.
- Reverse T3: This is the metabolic “brake.” If your body is stressed or inflamed, it may convert T4 into Reverse T3 instead of Free T3. This blocks the thyroid receptors. You can have normal TSH and T4, but if Reverse T3 is high, you are functionally hypothyroid at the cellular level.
- TPO and Tg Antibodies: These markers diagnose Hashimoto’s. High antibodies indicate an active autoimmune attack. This systemic inflammation can cause joint pain (cytokine storms) even if your TSH and T4 levels look perfect on paper. This is often where Hashimoto’s joint pain originates—from the immune attack itself, not just the hormone deficiency.
Markers for Muscle and Inflammation
If your doctor is unsure, ask for a Creatine Kinase (CK) test. As mentioned, CK enzymes leak from damaged muscle tissue. Elevated CK levels are a sign of myopathy and are common in uncontrolled hypothyroidism but typically normal in fibromyalgia. This is a crucial differentiator.
Additionally, check ESR (Erythrocyte Sedimentation Rate) and CRP (C-Reactive Protein). These inflammatory markers are usually normal in fibromyalgia. However, they may be mildly elevated in Hashimoto’s due to the autoimmune process. Ferritin (iron storage) is also vital. Low iron mimics hypothyroidism symptoms perfectly and prevents thyroid hormone from working.
Excluding Other Mimics
Before accepting a diagnosis of exclusion like fibromyalgia, ensure you have ruled out other mimics. Vitamin D deficiency is rampant in the USA. It causes deep bone pain and muscle weakness that feels identical to hypothyroidism. Polymyalgia Rheumatica (PMR) is another inflammatory condition causing stiffness in the hips and shoulders. Rheumatoid Arthritis must also be excluded by checking for RF factor and CCP antibodies. Lupus is another autoimmune condition that presents with joint pain and fatigue.
Comparison Table 2: Diagnostic Markers & Interpretation
| Marker | Hypothyroid Indication | Fibromyalgia Indication | “Gray Zone” Interpretation |
|---|---|---|---|
| TSH | Elevated (> 4.5) or High-Normal (> 2.5) | Normal | If TSH is > 2.5 and pain exists, trial treatment may be warranted. |
| Creatine Kinase | Often Elevated | Normal | Creatine kinase levels define muscle damage vs. pain processing. |
| Tender Points | Absent or few; generalized ache. | 11+ Positive points; Allodynia. | High antibodies can cause tender points via systemic inflammation. |
| Reflexes | Delayed relaxation. | Normal. | The most objective physical sign available. |
| NSAID Response | Minimal relief (metabolic issue). | Minimal relief (central nerve issue). | Neither responds well to standard painkillers like Ibuprofen. |
| Levothyroxine | Significant improvement over months. | No change in pain levels. | Response to therapy confirms the diagnosis. |
The “Double Diagnosis”: When You Have Both
It is entirely possible, and unfortunately common, to suffer from both conditions. This is the concept of Polyautoimmunity. If you have Hashimoto’s, your risk of developing other autoimmune or chronic conditions increases. Furthermore, chronic untreated hypothyroidism joint pain can actually cause fibromyalgia.
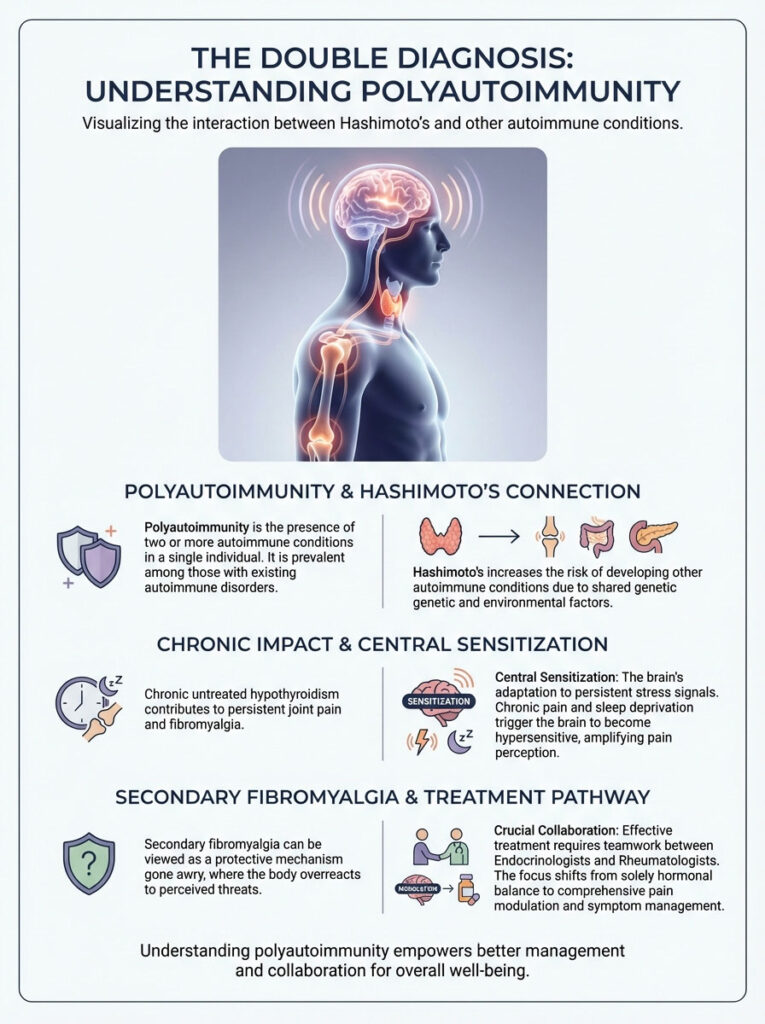
The Autoimmune Connection
How does one lead to the other? Chronic pain and sleep deprivation are the two biggest triggers for central sensitization. If your thyroid condition goes undiagnosed for years, the persistent muscle pain and poor sleep quality bombard your nervous system with stress signals. The brain is under siege.
Eventually, the central nervous system adapts by becoming hypersensitive. It lowers the threshold for what it considers “dangerous.” Even after you fix the thyroid levels and clear the glycosaminoglycan deposition, the brain may remain stuck in a “high alert” pain state. This is secondary fibromyalgia. It is a protective mechanism gone wrong.
Managing Comorbidities
When a patient has normalized TSH, Free T3, and Free T4 but still experiences widespread pain, we must pivot. This is where the Endocrinologist and Rheumatologist must collaborate. The goal shifts from hormonal replacement to pain modulation. You cannot treat the remaining pain with more thyroid hormone. Doing so will only cause thyrotoxicosis (heart palpitations, anxiety, bone loss) without fixing the central sensitization. You have to treat the brain separately from the gland.
Treatment Protocols: From Hormones to Neurons
Effective treatment depends on targeting the correct mechanism. We do not use a hammer to turn a screw. Similarly, we do not use antidepressants to treat myxedema. We need a precision approach.
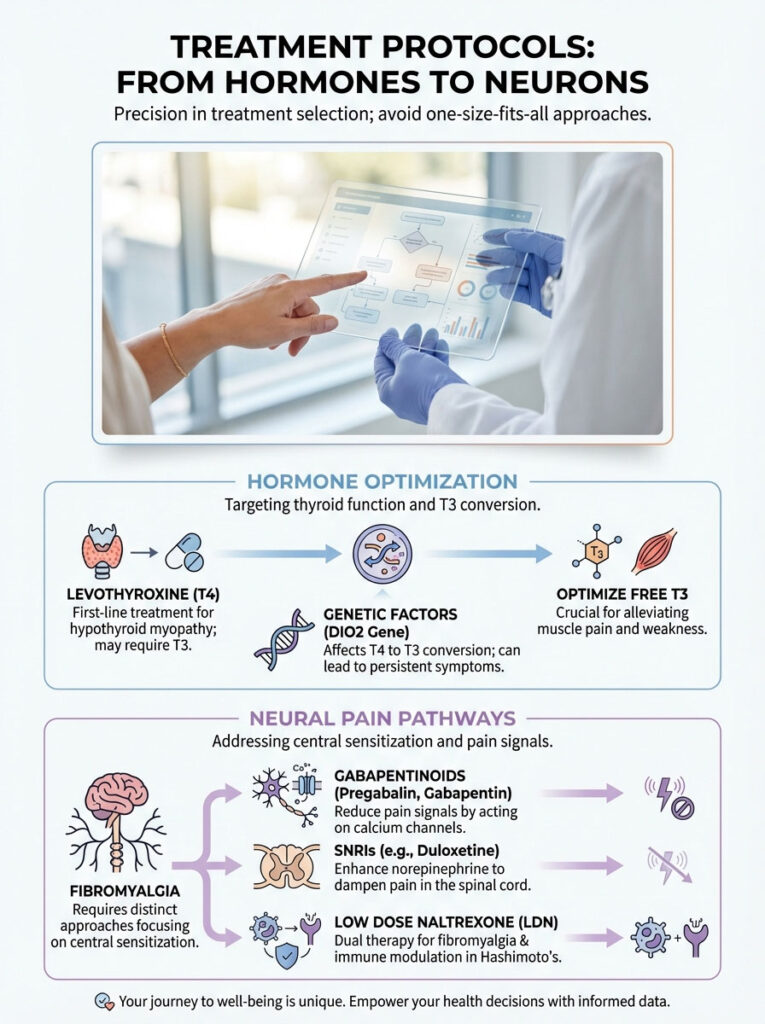
Optimizing Thyroid Hormone Replacement
For hypothyroid myopathy, the first line of defense is Levothyroxine (T4). However, T4 is a pro-hormone. It must be converted into T3 by the liver and kidneys to be active. Some patients have a genetic polymorphism (DIO2 gene) that impairs this conversion. For these individuals, T4 monotherapy may normalize TSH, but their muscle tissues remain starved of T3.
In these cases, adding Liothyronine (synthetic T3) or using Natural Desiccated Thyroid (NDT) can be a game-changer. Anecdotal evidence and emerging clinical data suggest that raising Free T3 levels to the upper quadrant of the reference range can help resolve residual muscle pain and proximal muscle weakness. Patience is required here. While energy may improve in days, it takes weeks or even months for the mucin and fluid to clear from the joint spaces. Muscles heal slowly.
Addressing Central Pain (Fibro-Specific)
If the component of pain is identified as fibromyalgia (central sensitization), we use different tools. Gabapentinoids like Pregabalin and Gabapentin work by binding to calcium channels on nerves. This effectively turns down the volume of pain signals. SNRIs like Duloxetine help by increasing norepinephrine. This acts as a natural pain-dampener in the spinal cord.
An emerging therapy gaining traction in the integrative medicine community is Low Dose Naltrexone (LDN). LDN acts as a glial cell modulator. Glial cells are the immune cells of the central nervous system. By calming these cells, LDN can reduce the neuro-inflammation driving fibromyalgia. Interestingly, LDN is also used to modulate the immune system in Hashimoto’s. This makes it a potentially powerful “bridge” therapy for patients with both Hashimoto’s joint pain and fibro.
The Role of Supplements
Supplements should be targeted, not random. You are not just taking vitamins; you are providing co-factors for enzymatic reactions.
- Selenium: Essential for the conversion of T4 to T3. It also helps reduce TPO antibodies.
- Magnesium Glycinate: Highly absorbable and crucial for muscle relaxation. It helps combat the cramping associated with myopathy. It also aids sleep quality.
- Thiamine (Vitamin B1): High-dose thiamine has shown promise in addressing the fatigue associated with autoimmune diseases. It helps with mitochondrial function.
- Curcumin: A potent anti-inflammatory that can help with the joint pain component of Hashimoto’s.
Dietary and Lifestyle Interventions
You cannot medicate your way out of a bad environment. Lifestyle changes are the bedrock of managing both conditions. The food you eat and the way you move dictate your inflammation levels.
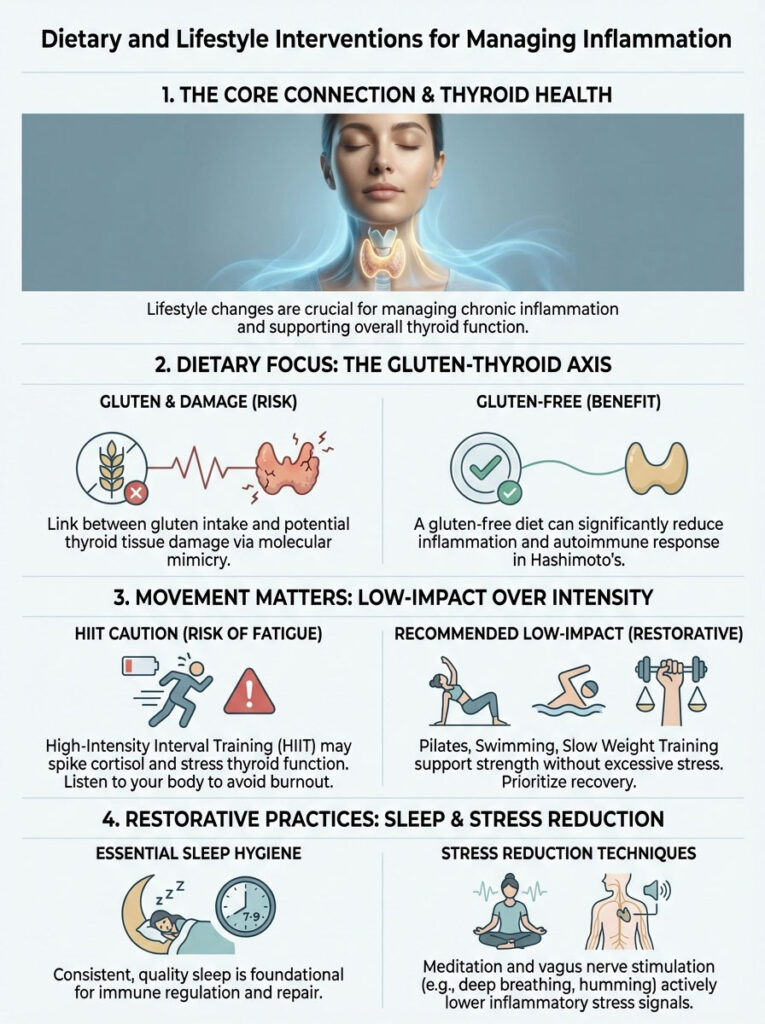
The Gluten-Thyroid Axis
There is a strong molecular mimicry between gliadin (the protein in gluten) and thyroid tissue. When you eat gluten, your immune system attacks the gliadin. But due to the structural similarity, it may also attack your thyroid gland. Many patients with Hashimoto’s joint pain report a significant reduction in inflammation and stiffness after adopting a strict gluten-free diet. It is worth a 90-day trial to see if your pain scores drop. Dairy is another common trigger due to the protein casein.
Anti-Inflammatory Movements
Exercise is a double-edged sword. While movement is necessary to pump fluid out of boggy tissues, High-Intensity Interval Training (HIIT) can be disastrous. HIIT spikes cortisol. Cortisol can suppress thyroid function and trigger a fibromyalgia flare. It tells your body it is in danger.
Instead, focus on low-impact, resistance-based movements. Pilates, swimming, and slow weight training help rebuild the atrophied Type II muscle fibers without overwhelming your adrenal system. Walking is excellent, but do not push to the point of exhaustion. Listen to your body’s signals. If you crash the next day, you did too much.
Sleep Hygiene and Stress Reduction
Since both conditions are exacerbated by poor sleep, hygiene is non-negotiable. Keep your room cool. Block out all blue light. Consider a sleep study to rule out apnea. Stress reduction techniques like meditation or vagus nerve stimulation can help shift your body from a sympathetic (fight or flight) state to a parasympathetic (rest and digest) state. This is crucial for healing.
Summary & Key Takeaways
The journey to resolve chronic pain is rarely a straight line. But understanding the source is the compass you need. Pain is not “in your head,” nor is it a sign of weakness. It is a physiological signal that something is wrong. It is either in the metabolic engine of your cells or the wiring of your nervous system.
Remember these critical points:
- Hypothyroidism joint pain is caused by tissue swelling (GAGs) and energy failure (mitochondria). It leads to deep aches and objective weakness.
- Fibromyalgia is a neurological amplification of pain signals (Central Sensitization) without tissue damage.
- Bilateral carpal tunnel syndrome and delayed relaxation of deep tendon reflexes are strong indicators of thyroid dysfunction.
- A “Normal TSH” does not guarantee your muscles have enough T3. Advocate for a full panel including Free T3 and CK.
- You can have both conditions. Treating the thyroid may not fully resolve pain if central sensitization has set in. This requires a multi-modal approach.
Do not settle for a life of unexplained pain. Do not accept a label without investigating the cause. By methodically addressing the metabolic, autoimmune, and neurological aspects of your health, you can turn down the volume on pain. You can reclaim your vitality.
Frequently Asked Questions
How can I tell if my joint pain is caused by hypothyroidism or fibromyalgia?
Hypothyroidism joint pain is typically a metabolic issue caused by glycosaminoglycan (GAG) buildup in tissues, leading to a “boggy” or heavy sensation. Fibromyalgia, conversely, is a neurological condition involving central sensitization where the brain over-processes pain signals. A key clinical differentiator is objective proximal muscle weakness, which is common in hypothyroid patients but rare in those with pure fibromyalgia.
Why is my TSH normal if I am still experiencing chronic muscle and joint pain?
A “normal” TSH only reflects the pituitary gland’s response, not necessarily the amount of active Free T3 available to your muscle tissues. Many patients suffer from cellular hypothyroidism or poor T4-to-T3 conversion, which leaves muscles starved for energy despite standard lab results. We recommend a full thyroid panel, including Free T3 and Reverse T3, to assess metabolic function at the tissue level.
What is the significance of bilateral carpal tunnel syndrome in thyroid patients?
Developing carpal tunnel symptoms in both hands simultaneously is a major clinical red flag for hypothyroidism rather than repetitive strain. This occurs because mucin-like substances called glycosaminoglycans accumulate in the wrist’s connective tissues, physically compressing the median nerve. Optimizing thyroid hormone levels often resolves this “space-occupying lesion” without the need for surgical intervention.
Can Hashimoto’s cause joint pain even if my thyroid levels are within range?
Yes, Hashimoto’s joint pain can occur independently of hormone levels due to the systemic inflammation and cytokine storms associated with an active autoimmune attack. High TPO or Tg antibodies indicate that the immune system is targeting the gland, which can trigger widespread inflammation throughout the body’s connective tissues. In these cases, managing the autoimmune response through diet and lifestyle is as important as hormone replacement.
What is the “delayed relaxation” reflex test for hypothyroidism?
During a physical exam, a clinician may check your Achilles tendon reflex to look for a slow return to the resting position after the initial kick. This delayed relaxation phase is a classic sign of hypothyroid myopathy and reflects the slow metabolic rate of muscle fibers. This phenomenon is rarely observed in fibromyalgia, making it a highly specific tool for identifying thyroid-driven physical dysfunction.
Is there a specific lab test that can differentiate muscle damage from nerve pain?
The Creatine Kinase (CK) test is an excellent diagnostic tool for distinguishing between these two conditions. Elevated CK levels indicate that muscle membranes are unstable and leaking enzymes into the blood, which is a hallmark of hypothyroid myopathy. In contrast, fibromyalgia patients typically have normal CK levels because their pain originates in the nervous system rather than from structural muscle damage.
Can chronic hypothyroidism eventually lead to a fibromyalgia diagnosis?
Untreated hypothyroidism can indeed trigger secondary fibromyalgia through a process called central sensitization. Years of persistent muscle pain, metabolic energy deficits, and sleep disturbances can overtax the nervous system, causing the brain to become hypersensitive to pain signals. Even after thyroid levels are corrected, the “software” of the brain may remain in a high-alert state, requiring separate neurological treatment.
Why do hypothyroid patients experience “boggy” swelling and morning stiffness?
This sensation is caused by myxedema, where hydrophilic sugar-protein complexes (GAGs) trap fluid within the interstitial spaces of the muscles and joints. This creates a mechanical pressure that feels like a heavy, wet wetsuit, often peaking in the morning after hours of inactivity. Movement helps pump some of this fluid out, which is why the stiffness may slightly improve as the day progresses.
Does Levothyroxine (T4) always resolve the joint pain associated with hypothyroidism?
While Levothyroxine is the standard treatment, some patients struggle to convert T4 into the active T3 hormone required by muscle mitochondria. If muscle aches and proximal weakness persist on T4-only therapy, a clinician might consider adding Liothyronine (T3) or transitioning to Natural Desiccated Thyroid (NDT). Reaching the upper quadrant of the Free T3 reference range is often necessary to fully clear tissue-level myxedema.
How does gluten consumption affect joint pain in Hashimoto’s patients?
Gluten can exacerbate Hashimoto’s joint pain due to molecular mimicry, where the immune system confuses the protein gliadin with thyroid tissue. This cross-reactivity fuels the autoimmune attack and systemic inflammation, leading to increased stiffness and discomfort. Many patients find that a strict 90-day gluten-free trial significantly reduces their overall pain scores and inflammatory markers.
What type of exercise is best for managing both hypothyroidism and fibromyalgia?
Low-impact, resistance-based movements like Pilates, swimming, or slow weight training are ideal for rebuilding atrophied muscle fibers without triggering a flare. High-Intensity Interval Training (HIIT) should be avoided, as it can spike cortisol and suppress thyroid function, leading to post-exertional malaise. The goal is to encourage circulation and fluid drainage while respecting the body’s limited metabolic energy reserves.
Are there specific supplements that help with hypothyroid muscle cramps?
Magnesium glycinate is highly recommended as it is easily absorbed and aids in the active process of muscle relaxation, which is often impaired in hypothyroid states. Additionally, Selenium supports the conversion of T4 to T3, while high-dose Thiamine (B1) has shown clinical promise in reducing the profound fatigue and muscle heaviness associated with autoimmune thyroid disease.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The distinction between endocrine and neurological conditions is complex and requires professional evaluation. Always consult a qualified healthcare professional, such as an endocrinologist or rheumatologist, before making health decisions or changing your medication protocol.
References
- American Thyroid Association (ATA) – thyroid.org – Provides clinical guidelines for the diagnosis and management of hypothyroidism and its systemic effects.
- Journal of Clinical Endocrinology & Metabolism – “Musculoskeletal Manifestations of Hypothyroidism” – A peer-reviewed study detailing the biological impact of T3 deficiency on muscle tissue.
- American College of Rheumatology – rheumatology.org – Official source for the diagnostic criteria of fibromyalgia and central sensitization syndromes.
- Mayo Clinic Proceedings – “The Overlap of Fibromyalgia and Autoimmune Thyroid Disease” – Research exploring the high prevalence of secondary fibromyalgia in Hashimoto’s patients.
- Frontiers in Endocrinology – “The Role of T3 in Mitochondrial Function” – A scientific review of how thyroid hormones regulate ATP production and muscle energetics.
- National Institutes of Health (NIH) – niddk.nih.gov – Statistical data on Hashimoto’s Thyroiditis and its prevalence in the United States.