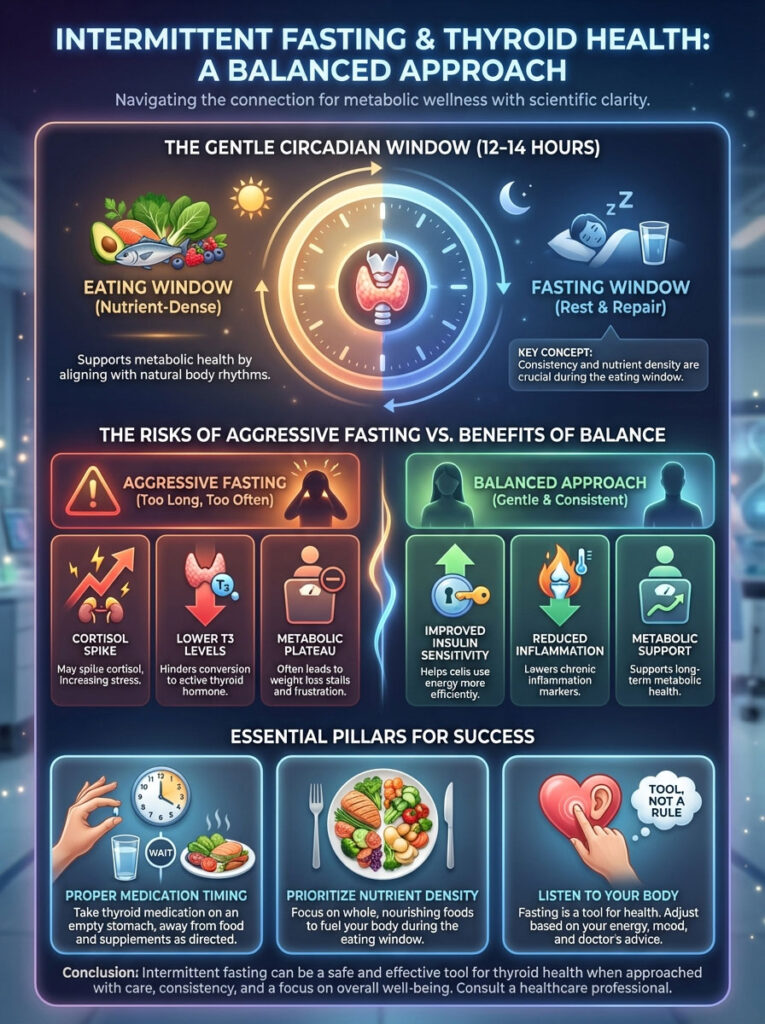
Quick Answer: Yes, intermittent fasting is generally safe for thyroid patients, but it requires a modified approach. While aggressive fasting can spike cortisol and lower T3 levels, a “Gentle Circadian” window of 12–14 hours typically supports insulin sensitivity and gut health without downregulating the metabolism. The key is consistency, nutrient density during the eating window, and proper timing of medication.
Table of Contents
You have likely experienced the specific, maddening frustration of the “hypothyroid weight loss plateau.” You restrict calories. You increase your exercise intensity. You do everything “right.” Yet, the scale remains frozen. For many of my patients, this is the breaking point where they begin looking for metabolic hacks. They often land on the concept of intermittent fasting and thyroid health as a potential solution.
The conflict is obvious. On one hand, fasting promises improved insulin sensitivity and cellular cleanup. On the other, you have been told that your thyroid is a delicate engine. You have been warned that it requires constant fuel to prevent a metabolic crash.
Here is the clinical reality. Fasting is a tool, not a religion. When applied with precision, it can reset the immune system and lower inflammation. When applied recklessly, it can force the body into a starvation response that halts weight loss entirely. This article explores the physiological nuances of intermittent fasting and thyroid health. We will ensure you can navigate this protocol without sacrificing your hormonal balance.
Key Statistics: Thyroid & Metabolism
- 20 Million: Estimated number of Americans with some form of thyroid disease (American Thyroid Association).
- 60%: Percentage of people with thyroid disease who are unaware of their condition.
- 14 Hours: The fasting duration threshold where autophagy (cellular cleanup) typically begins in humans.
- 20-30%: Potential reduction in T3 (active thyroid hormone) observed in aggressive caloric restriction studies.
- 5-7x: Women are five to eight times more likely than men to have thyroid problems.
The Metabolic Paradox: Why Thyroid Patients Struggle with Weight
Before we dive into fasting protocols, we must understand the landscape of the hypothyroid metabolism. The standard advice of “eat less, move more” often fails thyroid patients. This failure occurs because the thyroid controls the Basal Metabolic Rate (BMR). This is the number of calories you burn just by existing.
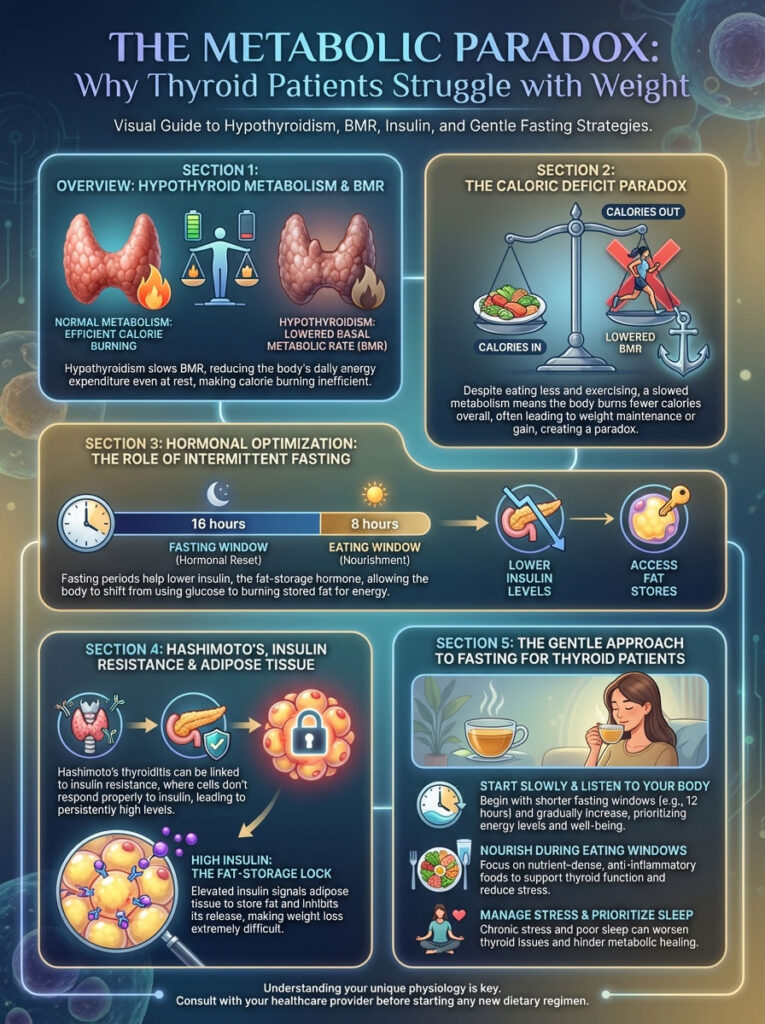
When you have hypothyroidism, your BMR is artificially suppressed. If you drastically cut calories, your body does not burn fat. Instead, it defends its energy stores. It perceives the calorie deficit as a famine.
This creates a paradox. You need a caloric deficit to lose weight. However, creating that deficit triggers your thyroid to slow down further. This is where intermittent fasting and thyroid health intersect. The goal of fasting is not just calorie restriction. The goal is hormonal optimization. We want to lower insulin levels to unlock fat stores without triggering the alarm bells in the thyroid gland.
The Insulin Connection
Many patients with Hashimoto’s or hypothyroidism also suffer from insulin resistance. Their cells do not hear the knock of insulin. As a result, the pancreas pumps out more insulin. High insulin levels block fat burning. They essentially lock the doors to your adipose tissue. Fasting lowers baseline insulin. This allows the body to access stored energy. But for a thyroid patient, we must do this gently.
The Physiology: How Fasting Affects the HPT Axis
To understand if this protocol is right for you, we must look beyond weight loss. We must examine the HPT axis (Hypothalamic-Pituitary-Thyroid axis). Think of the HPT axis as your body’s master thermostat. When you stop eating, your hypothalamus senses a drop in energy availability.
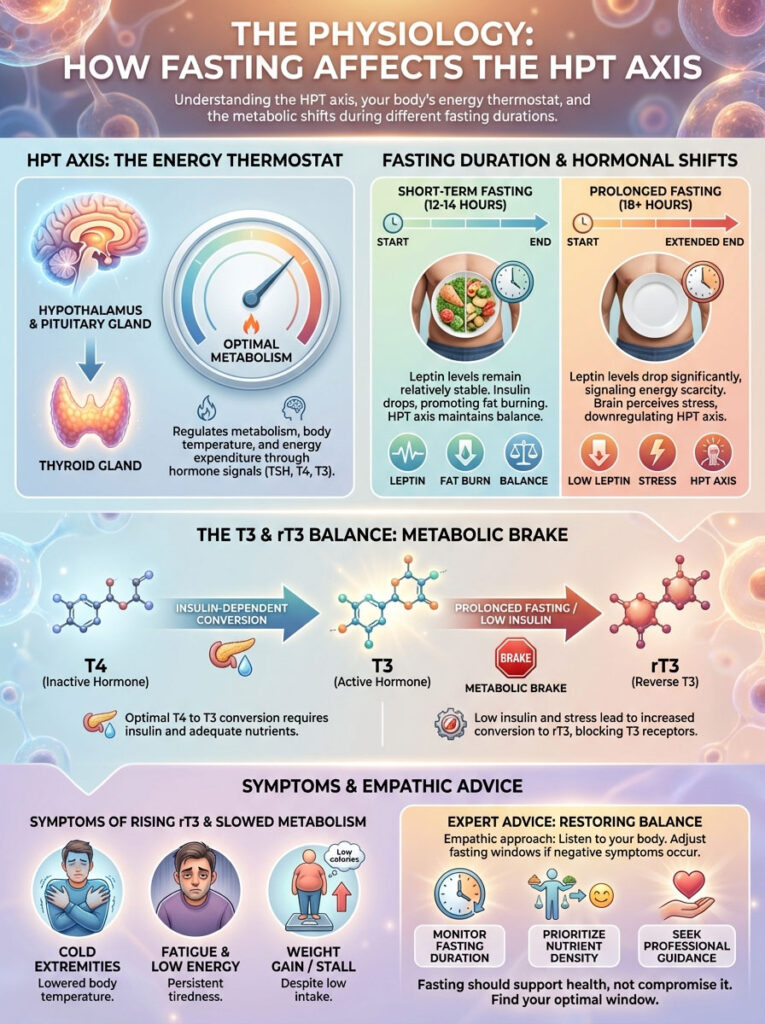
If this drop is perceived as a temporary break (12–14 hours), the body dips into fat stores. However, if the hypothalamus perceives “famine” (often 18+ hours or low-calorie intake), it signals the thyroid to slow down to ensure survival. This is where the nuance of intermittent fasting and thyroid health becomes critical.
The Role of Leptin and Signaling
Leptin is the satiety hormone produced by fat cells. In many hypothyroid patients, we see a condition called leptin resistance. Your brain does not “hear” the signal that you have enough energy. Consequently, it keeps your metabolism in low gear. Controlled fasting can help resensitize the body to leptin. When leptin sensitivity is restored, the HPT axis receives the “all clear” signal to upregulate metabolism. This theoretically aids in weight management.
T4 to T3 Conversion Mechanisms
The thyroid gland predominantly produces Thyroxine (T4). This hormone is metabolically inactive. It must be converted into Triiodothyronine (T3) to have any effect on your energy or weight. This T4 to T3 conversion happens largely in the liver and the gut.
Here is the catch. The enzyme required for this conversion (5′-deiodinase) is insulin-dependent and calorie-sensitive. Prolonged fasting can reduce the activity of this enzyme. If you fast too long, you may have plenty of T4 in your blood (normal TSH). But your cells are starving for T3. This explains why you might feel terrible even if your lab results look “normal” during a fast.
The Villain: Reverse T3 (rT3)
When the body is under stress, it diverts T4 down a different pathway. This stress can come from emotional trauma, sleep deprivation, or excessive fasting. Instead of creating active T3, the body creates Reverse T3 (rT3).
Reverse T3 acts as a metabolic brake. It binds to thyroid receptors but does not activate them. It effectively blocks active T3 from doing its job. In clinical practice, I often see patients who dive into aggressive 20-hour fasts develop high levels of Reverse T3. They feel colder. They feel more tired. They gain weight, even though they are barely eating. This is the primary risk of combining intermittent fasting and thyroid health incorrectly.
Expert Insight: If you are fasting and notice your hands and feet are becoming colder, or your resting heart rate drops significantly below your baseline, this is a sign of rising Reverse T3. It is a signal to shorten your fasting window immediately.
Intermittent Fasting and Hashimoto’s: The Autoimmune Connection
The majority of hypothyroidism cases in the United States are caused by Hashimoto’s Thyroiditis. This is an autoimmune condition. For these patients, the conversation shifts from simple weight loss to immune modulation. This is where Hashimoto’s and fasting can be a powerful therapeutic combination.
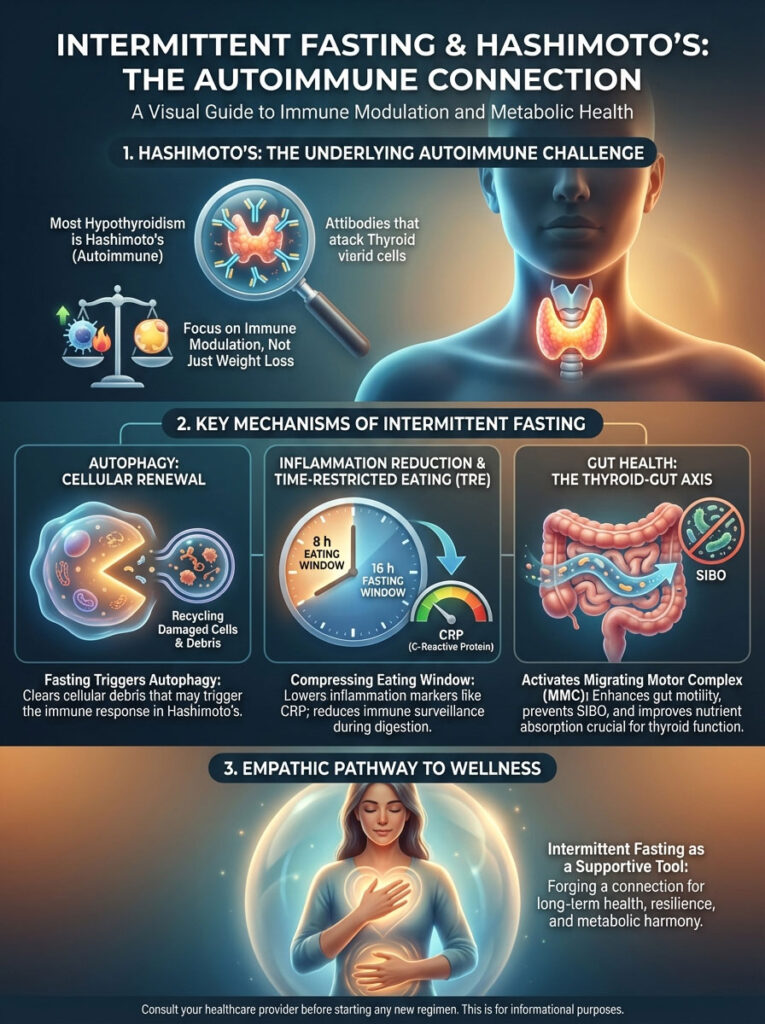
Autophagy Explained
Autophagy for autoimmune health is one of the most compelling arguments for fasting. Autophagy is the body’s cellular recycling process. During a fasted state, the body identifies damaged cells and misfolded proteins. It breaks them down. For a Hashimoto’s patient, this process helps clear out cellular debris. This debris may be triggering the immune system. Over time, this can potentially help to lower thyroid peroxidase (TPO) antibodies.
Inflammation Reduction
Chronic inflammation is the fuel for autoimmune disease. Time-restricted eating (TRE) has been shown to lower systemic inflammation markers such as C-Reactive Protein (CRP) and IL-6. By compressing your eating window, you give your digestive system a break. This reduces the constant immune surveillance that happens every time you ingest food.
Gut Health & The Microbiome
There is a strong link between gut health and thyroid function. Many Hashimoto’s patients suffer from SIBO (Small Intestinal Bacterial Overgrowth). The Migrating Motor Complex (MMC) is a wave of electrical activity. It sweeps bacteria out of the small intestine. But it only functions when you are in a fasted state.
If you are grazing from 7:00 AM to 10:00 PM, the MMC never engages. By practicing intermittent fasting and thyroid health protocols, you allow the MMC to perform its “housekeeping” duties. This reduces bloating. It improves the absorption of nutrients necessary for thyroid function.
Gender Differences: Why Women Must Fast Differently
One of the biggest mistakes I see in the wellness world is treating women like “small men.” This is dangerous in the context of fasting. Women have a much more sensitive hormonal hierarchy. This hierarchy is designed to protect fertility.
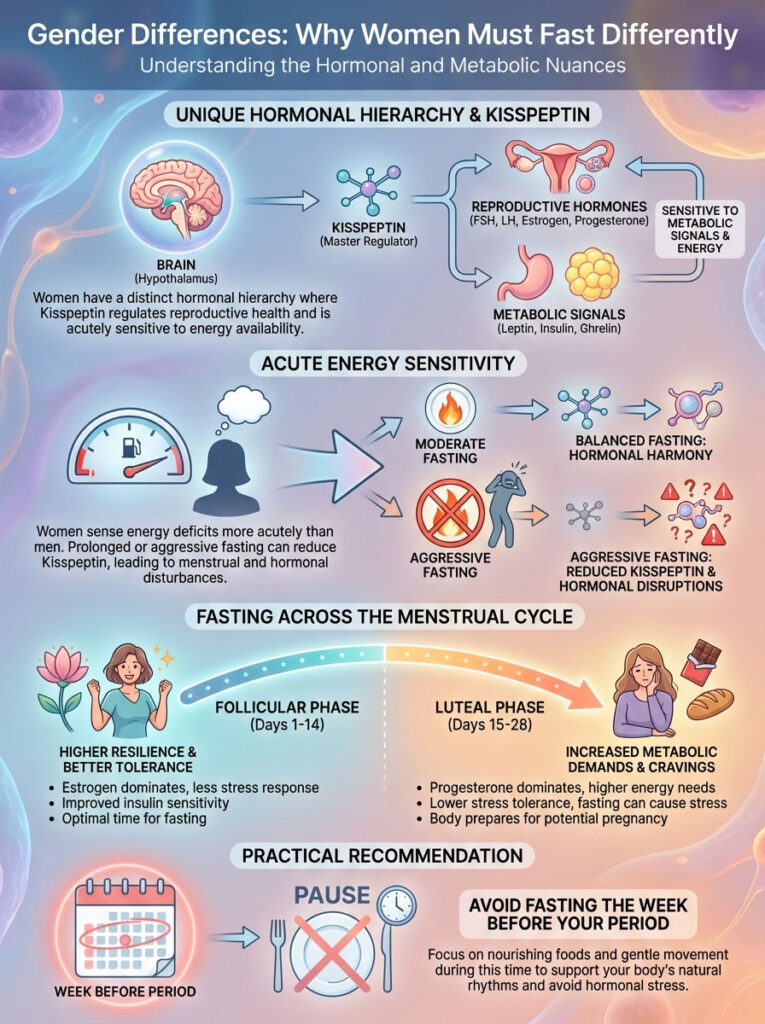
The Kisspeptin Connection
Kisspeptin is a neuropeptide in the brain. It governs the release of GnRH (Gonadotropin-Releasing Hormone). This hormone starts the chain reaction for ovulation and reproduction. Kisspeptin is highly sensitive to insulin, leptin, and ghrelin. In men, there are two main populations of kisspeptin neurons. In women, there are vastly more.
This means women are biologically wired to sense energy deficits more acutely than men. If a woman fasts too aggressively, kisspeptin production drops. This signals the ovaries to shut down. The thyroid, being the metabolic regulator, follows suit. This is why women often experience hair loss and cycle irregularities with aggressive fasting, while their husbands feel great.
Fasting and the Menstrual Cycle
Your fasting tolerance changes throughout the month.
Follicular Phase (Days 1-14): Estrogen is building. Estrogen is insulin-sensitizing. Women are generally more resilient to stress and fasting during the first two weeks of their cycle.
Luteal Phase (Days 15-28): Progesterone becomes dominant. Progesterone is a demanding hormone. It raises your metabolic rate and increases cravings. It requires stable blood sugar. Fasting during the week before your period creates a “double stress” on the body. This often leads to adrenal fatigue and thyroid suppression. I advise my female patients to stop fasting during this week.
Analyzing Fasting Protocols: Which is Best for Thyroid Health?
Not all fasting is created equal. In endocrinology, we look for the “Minimum Effective Dose.” This is the amount of stress required to trigger adaptation without causing a crash. Let’s analyze the popular methods.
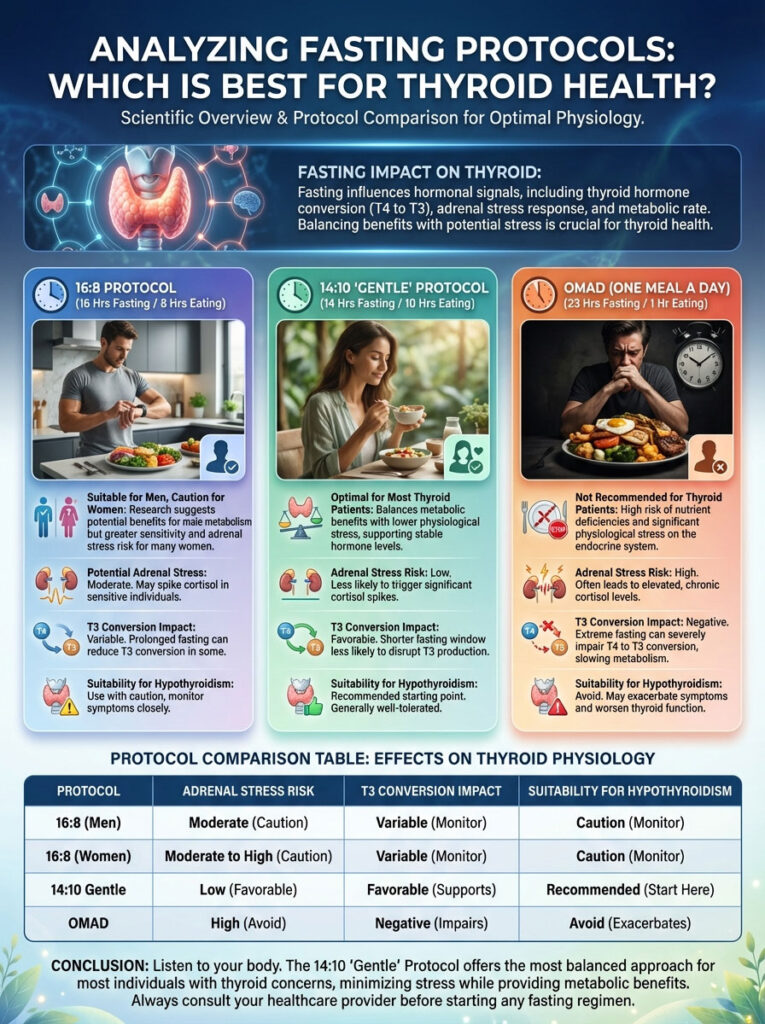
The 16:8 Protocol
This involves 16 hours of fasting and an 8-hour eating window. While popular, 16 hours can be metabolically expensive for women with advanced adrenal fatigue or severe hypothyroidism and intermittent fasting intolerance. It often works well for men. However, women need to monitor their cycle and energy levels closely.
The 14:10 “Gentle” Protocol
I consider this the “Goldilocks” zone for most thyroid patients. Fasting for 14 hours (e.g., 7:00 PM to 9:00 AM) provides the benefits of gut rest and insulin sensitivity. It does this without triggering the starvation response in the hypothalamus. It is sustainable. It is less likely to spike cortisol.
OMAD (One Meal a Day)
I explicitly advise against OMAD for thyroid patients. Trying to cram all your protein, selenium, zinc, and tyrosine into a one-hour window is nearly impossible. Furthermore, the sheer volume of food in one sitting can spike insulin. Meanwhile, the 23-hour fast spikes cortisol. This “push-pull” dynamic is a recipe for Reverse T3 dominance.
Below is a comparison of how these protocols impact thyroid physiology.
| Protocol | Window (Fast/Eat) | Adrenal Stress Risk | T3 Conversion Impact | Suitability for Hypothyroidism |
|---|---|---|---|---|
| Gentle Circadian | 12:12 | Very Low | Neutral/Positive | High (Best Starting Point) |
| Moderate IF | 14:10 | Low | Neutral | High (Optimal for Women) |
| Standard IF | 16:8 | Moderate | Variable (Monitor Temp) | Moderate (Proceed with Caution) |
| OMAD | 23:1 | Very High | Negative (Lowers T3) | Low (Not Recommended) |
| Alternate Day | 24+ Hours | Extreme | Negative (Increases rT3) | Low (Medical Supervision Only) |
The Critical Logistics: Medication and Nutrient Timing
One of the most common logistical hurdles in intermittent fasting and thyroid health is medication timing. Levothyroxine (Synthroid) and Liothyronine (Cytomel) are notoriously fussy drugs. They require an acidic environment for absorption. They are easily blocked by calcium, iron, and coffee.

The Absorption Problem
If you take your medication and then immediately drink coffee with cream, you may be absorbing as little as 60% of your dose. Over time, this mimics a worsening of your condition. This leads your doctor to unnecessarily increase your dosage. This cycle can cause hyperthyroid symptoms like anxiety and palpitations.
Scenario A: Morning Fasting
If you prefer to skip breakfast, you must still wake up to take your medication.
Protocol: Take medication at 6:00 AM with 4oz of water. Wait at least 60 minutes before drinking black coffee. Wait until 11:00 AM or 12:00 PM to eat your first meal. This ensures maximum thyroid medication absorption.
Scenario B: Evening Fasting
Some patients find morning dosing inconvenient with fasting.
Protocol: Stop eating at 7:00 PM. Take your medication at 11:00 PM (bedtime dosing). Studies suggest bedtime dosing can actually result in better absorption levels. This is because stomach acid production is naturally higher at night, and the gut is slower.
Scenario C: Split Dosing
For patients taking T3 (Cytomel) or Natural Desiccated Thyroid (Armour/NP Thyroid), you often need a second dose in the afternoon. This is tricky with fasting windows. I recommend taking the second dose at least 2 hours after your lunch and 1 hour before your dinner. This ensures the stomach is relatively empty.
Coffee and The Thyroid
A frequent question is, “Can I have cream in my coffee?” The answer for thyroid patients is a strict no during the fasting window. Dairy proteins and calcium bind to thyroid medication. Furthermore, calories from cream break the fast. This halts the MMC gut cleaning process. Stick to black coffee, tea, or water.
Breaking the Fast: Nutrient Density Over Caloric Restriction
The most important meal of the day is the one that breaks your fast. This meal signals to the HPT axis that the “famine” is over. It must be nutrient-dense. If you break your fast with a bagel or high-sugar cereal, you spike insulin while inflammation is high. This is counterproductive.

Key Nutrients Required
To support T4 to T3 conversion, your first meal should be rich in specific micronutrients.
- Selenium: Brazil nuts, sardines, halibut. Selenium is the cofactor for the deiodinase enzyme. It protects the thyroid gland from oxidative damage.
- Zinc: Oysters, beef, pumpkin seeds. Zinc is essential for TSH synthesis. It also aids in the nuclear receptor binding of T3.
- Tyrosine: Poultry, dairy, avocados. This amino acid is the backbone of thyroid hormone structure.
- Iron: Red meat, spinach, lentils. Low ferritin (stored iron) is a common cause of poor conversion.
Carbohydrates and Conversion
There is a misconception that “Zero Carb” is best for thyroid weight loss. However, insulin is actually a signal required for the conversion of T4 to T3. Very low-carb diets (Keto) can sometimes lower T3 levels. We recommend “Smart Carbs” like root vegetables, berries, and quinoa during your eating window to keep the conversion pathways open. The goal is an insulin “pulse,” not a chronic spike.
Goitrogens: Fact vs. Fiction
Many patients fear broccoli and kale due to goitrogens. The clinical reality is that cooking cruciferous vegetables deactivates the goitrogenic compounds. You can safely include cooked spinach, broccoli, and cauliflower in your feeding window without harming your thyroid. The benefits of the sulforaphane in these veggies for liver detox far outweigh the theoretical risks.
| Substance | Fasting Window | Eating Window | Reason |
|---|---|---|---|
| Water/Electrolytes | YES | YES | Hydration supports liver detox pathways. |
| Black Coffee/Tea | YES (In moderation) | YES | Caffeine can stress adrenals; keep away from meds. |
| MCT Oil/Cream | NO | YES | Breaks the fast; interferes with medication absorption. |
| Supplements (Zinc/Sel) | NO | YES | Require stomach acid and food for absorption. |
| Thyroid Meds | YES (Empty stomach) | NO | Must be taken away from food, iron, and calcium. |
Troubleshooting: When to Stop Fasting
Even with the best planning, intermittent fasting and thyroid health may not align for everyone. You must listen to your body’s biofeedback. The goal is health, not adhering to a clock. There are specific warning signs that your body is entering a “danger zone.”
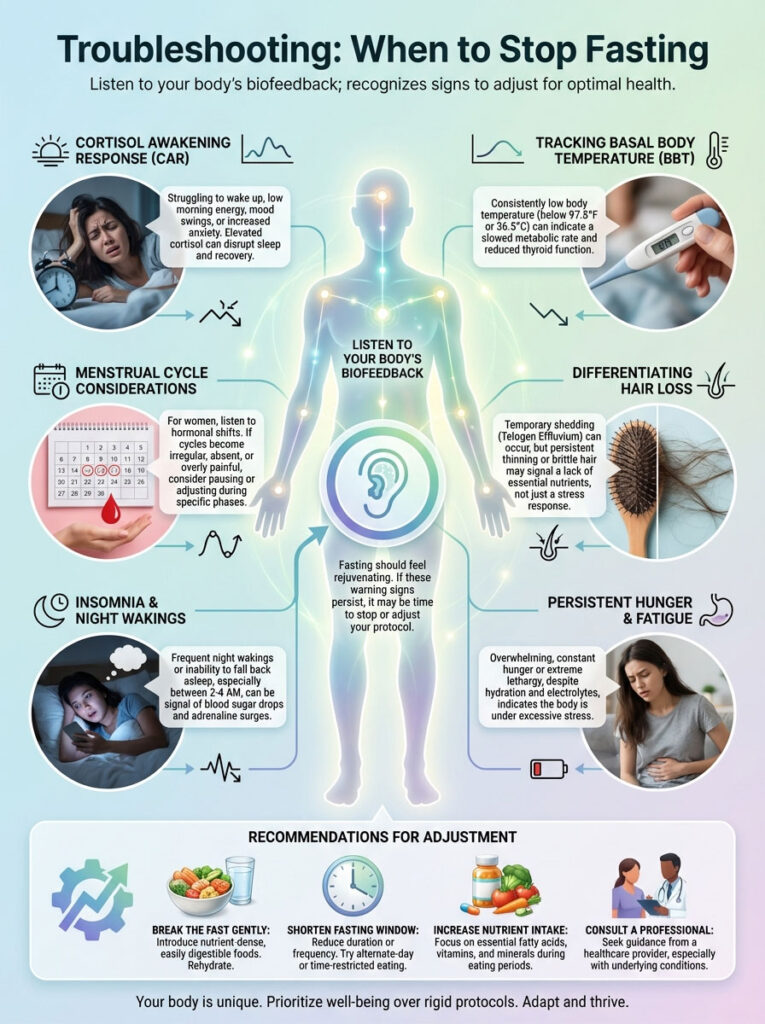
The Cortisol Awakening Response (CAR)
If you start waking up with a racing heart, anxiety, or a feeling of “tired but wired,” your fasting window is likely too long. This indicates that your cortisol is spiking to maintain blood sugar. High cortisol suppresses TSH. It also blocks the conversion of T4 to T3. If this happens, eat breakfast immediately upon waking for a week to reset your adrenals.
Basal Body Temperature (BBT)
A practical strategy I use with patients is tracking morning temperature. Before you get out of bed, take your temperature. If you see a consistent drop below 97.8°F (36.5°C) over several days of fasting, your metabolic rate is slowing down. Your body is trying to conserve energy. You should widen your eating window immediately.
Menstrual Cycle Considerations
As mentioned earlier, women are not small men. During the luteal phase (the week before menstruation), your body requires more energy to produce progesterone. Fasting during this week can cause severe PMS and hormonal disruption. I advise my female patients to stop fasting or switch to a simple 12:12 schedule during the week before their period.
Hair Loss
Distinguish between “telogen effluvium” (temporary shedding due to stress/weight loss) and thyroid hair loss. If hair loss accelerates significantly after starting IF, check your iron (Ferritin) and T3 levels. You may be under-eating protein. Hair follicles are very sensitive to energy deficits. They are often the first thing the body sacrifices when it perceives a famine.
Insomnia and Night Wakings
If you fall asleep fine but wake up at 2:00 AM or 3:00 AM, this is often a blood sugar issue. Your liver runs out of glycogen during the night. The body spikes adrenaline to release stored sugar. This adrenaline wakes you up. If this happens, try eating a small amount of slow-burning carbs (like half a sweet potato) with dinner.
Case Studies & Expert Protocol
How do we implement this safely? We use the “Slow Starter” approach. Do not jump from a standard American diet to a 16-hour fast overnight. The thyroid hates sudden changes.
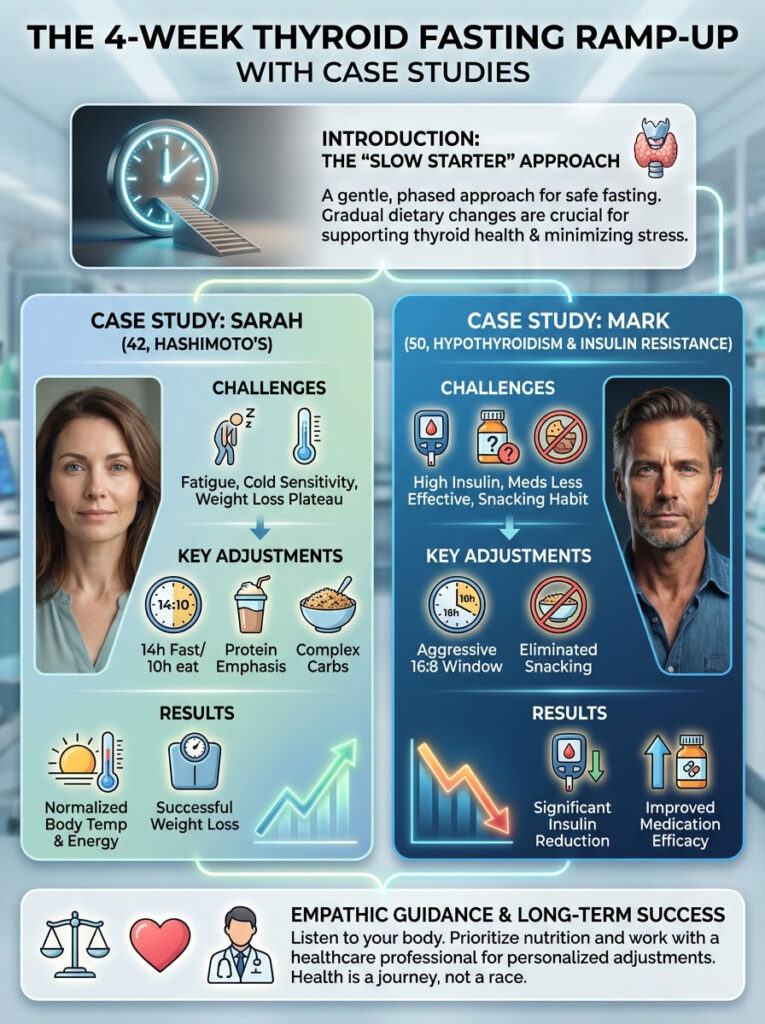
The 4-Week Thyroid Fasting Ramp-Up
- Week 1: 12:12 Schedule. Simply stop snacking after dinner. Establish a 12-hour gut rest. Focus on hydration.
- Week 2: 13:11 Schedule. Push breakfast back by one hour. Ensure you are taking meds correctly.
- Week 3: 14:10 Schedule. This is the goal for most. Assess how you feel. Check your temperature.
- Week 4: Evaluation. Check energy, temperature, and sleep. If all are good, maintain. If not, revert to Week 2.
Case Study: Sarah’s Plateau
Consider “Sarah,” a 42-year-old with Hashimoto’s and fatigue. She was doing 16:8 fasting. She was drinking coffee with almond milk during the fast. She was breaking her fast with low-calorie salads. Her weight was stuck. She was freezing all the time.
The Fix: We shifted her to a 14:10 window. We removed the almond milk from the fasting window to ensure true gut rest and MMC activation. Most importantly, we prioritized 30g of protein at her first meal (Break-Fast). We added a complex carb to dinner to help her sleep. Within three weeks, her body temperature normalized. Her energy returned. The thyroid weight loss plateau finally broke.
Case Study: Mark’s Insulin Resistance
“Mark,” a 50-year-old male with hypothyroidism, had high fasting insulin. He could handle more aggressive fasting. We put him on a 16:8 schedule. We focused heavily on eliminating snacking between meals. Because men have more robust kisspeptin neurons, he did not experience the adrenal crash. His insulin levels dropped by 50% in two months. This allowed his thyroid medication to work more effectively.
Summary & Key Takeaways
The relationship between intermittent fasting and thyroid health is nuanced. It is not inherently dangerous. But it requires respect for your biology. Fasting is a stressor; the dose matters. You cannot force a healed metabolism through starvation.
The Golden Rule: Consistency trumps intensity. A 12-hour fast done every day for a year does more for your mitochondrial health than a 24-hour fast done once a month that leaves you exhausted.
Final Actionable Steps:
- Start with a 12-hour window. Only increase if your energy remains stable and your sleep is good.
- Separate thyroid medication from food and coffee by at least 60 minutes. This is non-negotiable.
- Prioritize protein, selenium, and zinc in your eating window. These nutrients support the conversion of T4 to T3.
- Listen to your body. If your temperature drops, your hair falls out, or you stop sleeping, stop fasting.
- For women, respect your cycle. Ease up on fasting during the week before your period.
By treating fasting as a dial rather than a switch, you can harness its benefits for inflammation and insulin sensitivity. You can do this while keeping your thyroid happy and healthy.
Frequently Asked Questions
Is intermittent fasting safe for people with hypothyroidism?
Yes, intermittent fasting is generally safe but requires a modified, gentle approach to avoid metabolic downregulation. While short fasting windows can improve insulin sensitivity, aggressive fasting may spike cortisol and lower active T3 levels. We typically recommend a 12 to 14-hour window to balance cellular cleanup with hormonal stability.
Why is my weight loss stalled on intermittent fasting with a thyroid condition?
This “hypothyroid weight loss plateau” occurs because the body perceives a severe calorie deficit as a famine, triggering the thyroid to further lower your Basal Metabolic Rate (BMR). Instead of burning fat, your body defends its energy stores to ensure survival. To break the plateau, you must focus on hormonal optimization and nutrient density rather than just restricting calories.
How does prolonged fasting impact T4 to T3 conversion?
Prolonged fasting can reduce the activity of the 5\’-deiodinase enzyme, which is responsible for converting inactive T4 into active T3. Studies have shown that aggressive restriction can lead to a 20-30% reduction in T3 levels. This explains why some patients feel colder and more fatigued even if their TSH levels remain within the standard reference range.
Can intermittent fasting help reduce Hashimoto’s thyroid antibodies?
Fasting can potentially lower TPO antibodies by triggering autophagy, the body\’s natural cellular recycling process that clears out damaged proteins and debris. By reducing systemic inflammation and giving the digestive system a rest, you lower the immune surveillance that often drives autoimmune flares. However, this must be balanced with a nutrient-dense diet to avoid stressing the HPT axis.
What is the ideal intermittent fasting window for thyroid health?
The “Goldilocks” zone for most thyroid patients is the 14:10 gentle protocol, involving 14 hours of fasting and a 10-hour eating window. This duration is long enough to engage the Migrating Motor Complex for gut health but short enough to avoid signaling a “starvation response” to the hypothalamus. It is particularly effective for women who are more sensitive to energy deficits.
How should women adjust their fasting schedule for thyroid and hormonal balance?
Women have highly sensitive kisspeptin neurons that can shut down the thyroid and reproductive axis if energy is too low. I advise female patients to use a 12:12 or 14:10 schedule and to stop fasting entirely during the luteal phase (the week before menstruation). This prevents the “double stress” of fasting and high progesterone demands that often leads to adrenal fatigue.
When is the best time to take thyroid medication while intermittent fasting?
Thyroid medication must be taken on an empty stomach, at least 60 minutes before consuming food or coffee. If you fast in the morning, take your dose upon waking with water only; alternatively, bedtime dosing can be highly effective as stomach acid is higher and gut motility is slower. Ensure you stay consistent with your choice to maintain stable blood levels of the hormone.
Can aggressive fasting cause a spike in Reverse T3 levels?
Yes, excessive fasting acts as a physiological stressor that can divert T4 into Reverse T3 (rT3) instead of active T3. Reverse T3 acts as a metabolic brake by blocking thyroid receptors, which leads to symptoms like cold intolerance and weight gain. Monitoring your basal body temperature is a practical way to see if your rT3 is rising and slowing your metabolism.
Is black coffee allowed during a fast if I have thyroid issues?
Black coffee is permitted, but you must avoid adding cream, MCT oil, or milk, as these contain calories that break the fast and dairy proteins that bind to thyroid medication. Furthermore, excessive caffeine can overstimulate the adrenals in hypothyroid patients. Always keep your coffee consumption at least one hour away from your medication dose to ensure proper absorption.
What are the signs of adrenal stress while fasting with hypothyroidism?
Warning signs include waking up with a racing heart, experiencing “tired but wired” energy, or having trouble staying asleep through the night. These symptoms suggest a heightened Cortisol Awakening Response, where the body spikes adrenaline to maintain blood sugar levels. If these occur, you should immediately shorten your fasting window and prioritize adrenal support.
Which nutrients are essential when breaking a fast to support thyroid function?
Your first meal should be rich in protein and cofactors like selenium, zinc, and tyrosine to support the deiodinase enzymes. Including “smart carbs” like sweet potatoes or berries is also critical, as a small insulin pulse is required to signal the liver to convert T4 into active T3. Avoid breaking your fast with high-sugar or processed foods that spike systemic inflammation.
Is the One Meal a Day (OMAD) protocol recommended for thyroid patients?
I explicitly advise against OMAD for those with thyroid disease because it creates an extreme stress response that often leads to T3 suppression. It is nearly impossible to absorb the necessary amounts of selenium, zinc, and protein required for thyroid health in a single sitting. This protocol frequently results in hair loss and a crashed metabolism due to elevated Reverse T3 levels.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Intermittent fasting and thyroid health protocols involve complex hormonal interactions; therefore, you should always consult a qualified healthcare professional or endocrinologist before making significant changes to your diet or medication schedule.
References
- American Thyroid Association – thyroid.org – Statistics on thyroid disease prevalence and the impact of caloric restriction on BMR.
- The Journal of Clinical Endocrinology & Metabolism – Oxford Academic – Research on the effects of fasting on the HPT axis and T3/T4 conversion enzymes.
- Endocrine Reviews – Endocrine Society – Peer-reviewed data on the role of leptin and kisspeptin in female hormonal signaling and energy deficits.
- Frontiers in Immunology – frontiersin.org – Studies regarding autophagy, time-restricted eating, and the reduction of systemic inflammation markers.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – NIH – Official guidance on insulin resistance and its relationship with metabolic disorders.
- Journal of Thyroid Research – Hindawi – Clinical insights into the absorption of levothyroxine and the interference of food/calcium.








