Is Gluten Killing Your Thyroid? Gluten and Hypothyroidism Truth is a complicated subject that demands a deeper look than a simple blood test provides. You take your Levothyroxine every single morning on an empty stomach. You wait an hour before your coffee just as prescribed. Yet by 2:00 PM the familiar fog rolls in and your energy crashes.
Table of Contents
Your hair is still thinning. The scale refuses to budge no matter how little you eat. Your joints ache with a dull and persistent throb. When you bring this up at your check-up you are likely told that your TSH is “within normal range.” You are told your symptoms are unrelated to your thyroid.
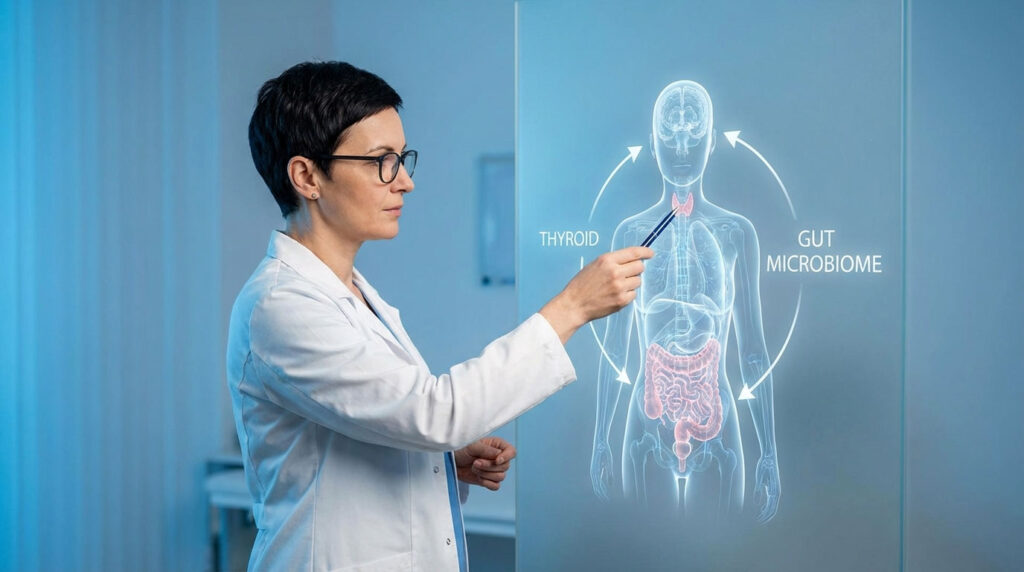
This is the clinical reality for millions of Americans. The standard TSH test fails to account for the complex interaction between your digestive system and your immune system. The thyroid does not operate in a vacuum. It is intrinsically linked to the gut. For the vast majority of patients with Hashimoto’s Thyroiditis what you eat acts as a biological instruction code for your immune system.
We are going to move beyond generic dietary advice. This is a deep examination of the biochemistry of the thyroid-gut axis. We will look at how specific proteins in wheat trigger autoimmune destruction. We will explain why “just a little bit” of bread can keep antibodies elevated for months. Finally we will provide the clinical blueprint required to put these conditions into remission.
Quick Answer: Is Gluten Harmful for the Thyroid?
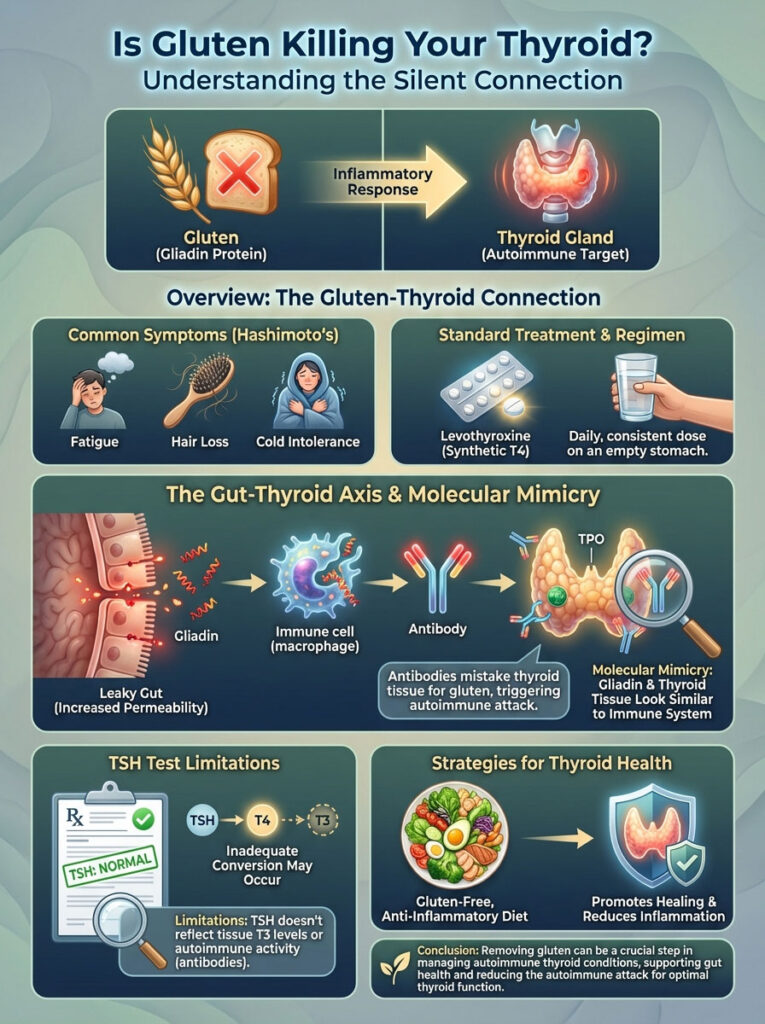
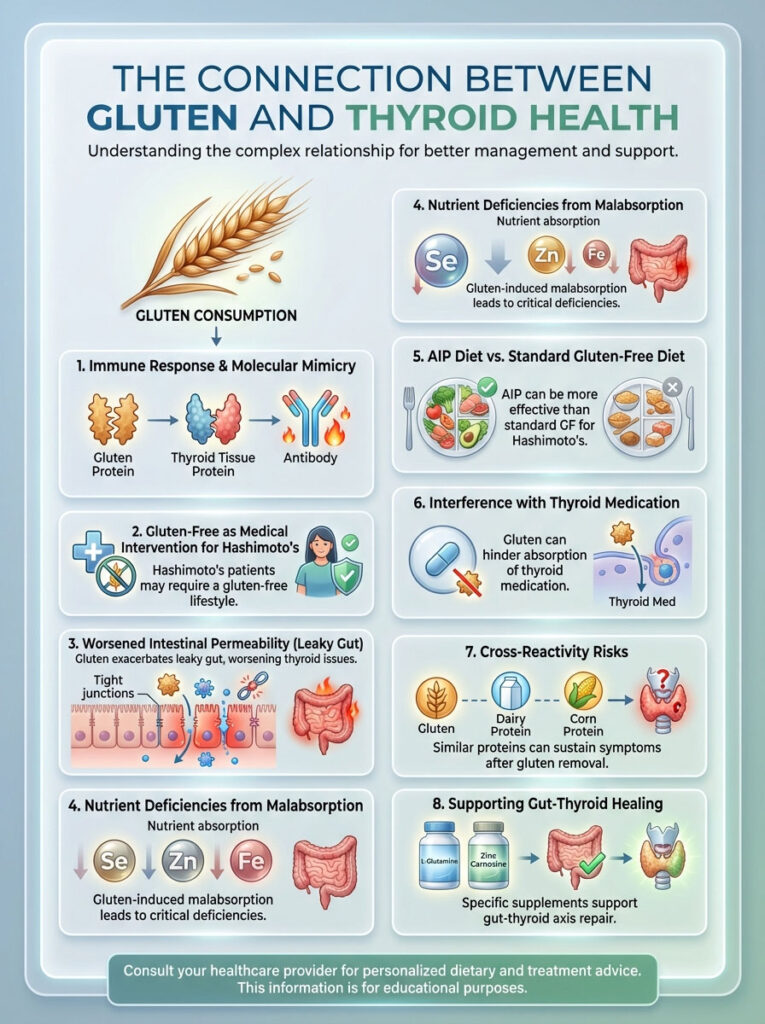
Yes. For patients with Hashimoto’s Thyroiditis gluten is a primary trigger for autoimmune attacks due to molecular mimicry. The protein structure of gluten (gliadin) closely resembles thyroid tissue. When the immune system attacks gluten it inadvertently targets the thyroid gland. This elevates TPO antibodies and perpetuates hypothyroidism.
Key Statistics: The Gluten-Thyroid Connection
- 90% of hypothyroidism cases in the USA are autoimmune (Hashimoto’s).
- 40-50% of adults with Celiac disease also have autoimmune thyroid disease.
- 3 to 6 months: The time it takes for TPO antibodies to significantly drop after full gluten elimination.
- 20% of T4 (inactive hormone) is converted to T3 (active hormone) in the gut bacteria.
- 1 in 3 Hashimoto’s patients suffer from Non-Celiac Gluten Sensitivity (NCGS).
The Biochemistry of Autoimmunity: Molecular Mimicry Explained
To understand why a bagel might be the enemy of your metabolism we have to look at the microscopic level. The immune system is a sophisticated defense force. It is designed to identify and neutralize foreign invaders like bacteria, viruses, and toxins. However in autoimmune thyroid disease this system loses its ability to distinguish self from non-self.
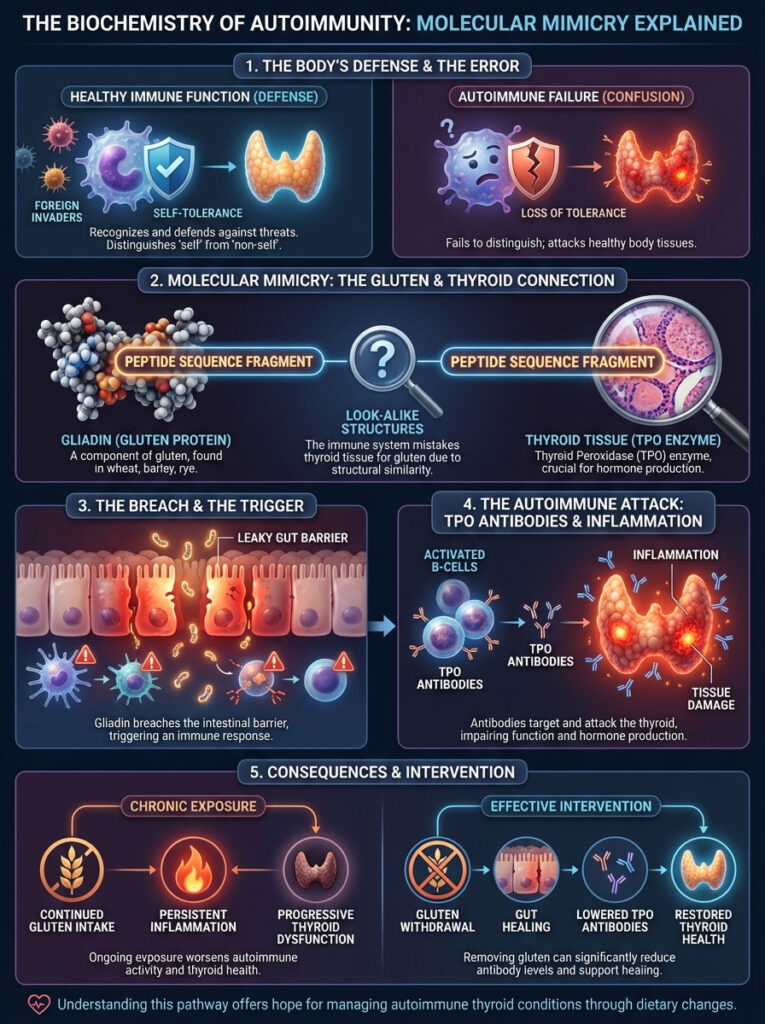
The Case of Mistaken Identity: How Gliadin Tricks the Immune System
The core mechanism driving the conflict between wheat and the thyroid is called Molecular Mimicry. Gluten is a composite protein made up of glutenin and gliadin. It is the gliadin portion that poses the most significant threat to thyroid patients.
Structurally the amino acid sequence of gliadin bears a striking resemblance to the protein structure of your thyroid tissue. When you consume gluten the gliadin protein breaches the intestinal barrier and enters the bloodstream. Your immune system tags this protein as a threat. It produces antibodies to destroy it.
Here is the problem. Because the thyroid tissue looks so similar to gliadin these antibodies do not just attack the gluten. They launch an assault on the thyroid gland itself. This is akin to a case of “friendly fire” in a war zone. Every time you consume gluten you are essentially restocking the ammunition for your immune system to attack your own gland.
Research published in Clinical and Experimental Immunology has documented this antibody cross-reactivity. The data shows that the immune response to gliadin can persist for up to six months after ingestion. This means a single cheat meal can derail months of progress.
TPO Antibodies and the Inflammatory Cascade
In clinical practice we measure this attack primarily through TPO Antibodies (Thyroid Peroxidase Antibodies) and Thyroglobulin antibodies. Thyroid Peroxidase is an enzyme responsible for iodinating tyrosine residues in the thyroglobulin molecule. This is a critical step in making thyroid hormones.
When the immune system attacks this enzyme via molecular mimicry TPO levels spike. This is not a silent process. It creates significant inflammation within the thyroid follicles. This leads to cell death and the gradual fibrosis of the gland.
Over years this destruction renders the thyroid incapable of producing enough hormone. This leads to permanent hypothyroidism. Data consistently shows that gluten withdrawal is one of the most effective non-pharmaceutical interventions for lowering these antibodies. We often see TPO titers in the thousands drop to the hundreds or even normal range within 3 to 6 months of a strict gluten-free diet.
The Gatekeeper: Intestinal Permeability and Zonulin
You cannot discuss autoimmune thyroid disease without discussing the gut. The two are physiological partners. The barrier that separates your bloodstream from the contents of your intestines is only one cell layer thick. This barrier is held together by structures called “tight junctions.”

The Zonulin Pathway: Breaking the Barrier
For decades the idea of “Leaky Gut” was dismissed by conventional medicine. However the discovery of Zonulin by Dr. Alessio Fasano changed everything. Zonulin is a protein that modulates the permeability of tight junctions between cells of the wall of the digestive tract.
When gliadin binds to the CXCR3 receptor on the intestinal cells it triggers an immediate release of Zonulin. This protein signals the tight junctions to open up. Under normal circumstances this opening is temporary and controlled.
However with chronic gluten exposure these junctions remain open. This condition is clinically known as increased intestinal permeability or Leaky Gut. Once the gate is open undigested food particles leak into the bloodstream. Bacterial toxins known as LPS (lipopolysaccharides) also enter circulation.
This constant influx of foreign material keeps the immune system in a state of chronic hyper-vigilance. It perpetuates the autoimmune cycle.
Expert Insight: You cannot heal the thyroid while the gut remains permeable. As long as the “gate” is open the immune system will remain overactive. Healing the gut lining is the prerequisite for lowering thyroid antibodies.
Systemic Inflammation and Thyroid Function
The breach of the gut barrier leads to systemic inflammation. The immune system releases inflammatory cytokines. These are chemical messengers that circulate throughout the body. These cytokines have a direct suppressive effect on thyroid function in two specific ways.
First they suppress the sensitivity of thyroid receptors on your cells. This means even if you have enough hormone in your blood your cells cannot “hear” the signal. You remain symptomatic despite normal blood levels.
Second they interfere with the HPT (Hypothalamus-Pituitary-Thyroid) axis. This interference often lowers TSH production artificially. This can make blood tests look “normal” even when the patient feels terrible.
Diagnosis: Celiac Disease vs. Non-Celiac Gluten Sensitivity
A common objection from patients is simple. “But my doctor tested me for Celiac and it was negative.” This is one of the most dangerous misconceptions in thyroid care. You do not need to have Celiac disease for gluten to destroy your thyroid health.
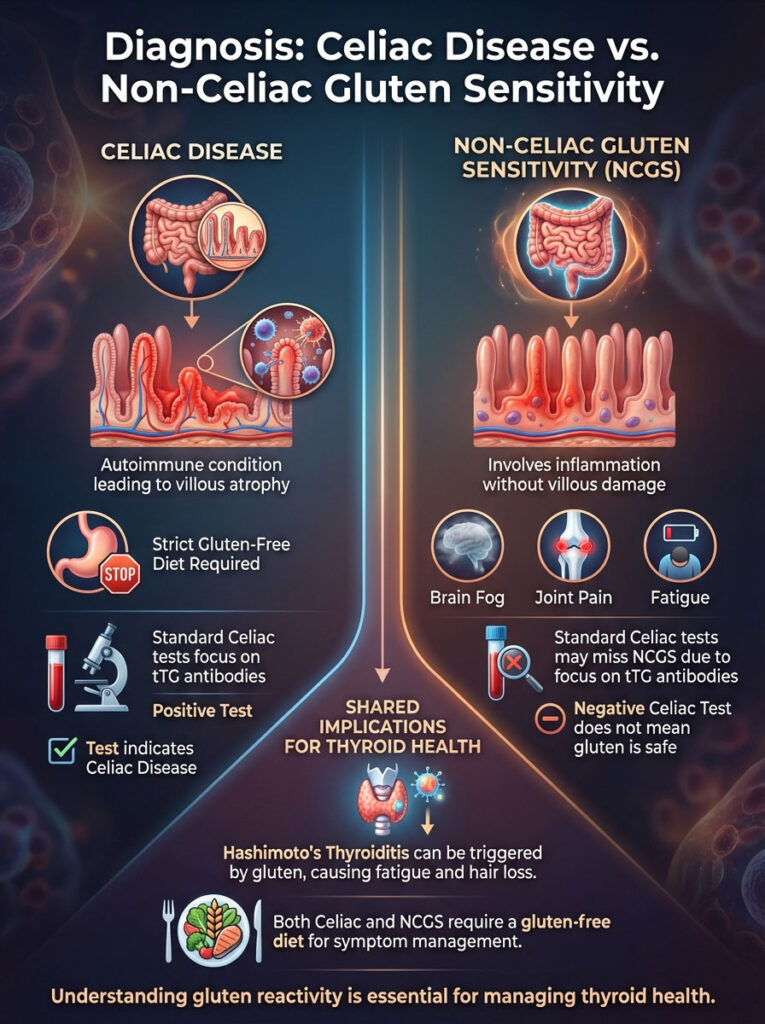
The Spectrum of Gluten Reactivity
Gluten reactivity exists on a spectrum. On one end you have Celiac Disease. This is an autoimmune condition where gluten causes total villous atrophy. The finger-like projections in the gut flatten completely. This results in severe malabsorption.
However a much larger segment of the Hashimoto’s population suffers from Non-Celiac Gluten Sensitivity (NCGS). In NCGS the immune system reacts to gluten with inflammation and antibody production. It does not result in the total destruction of the intestinal villi.
The symptoms are often extra-intestinal. Patients experience brain fog and joint pain. They report fatigue and critically thyroid suppression. These patients often feel just as sick as Celiac patients despite negative biopsies.
Why Standard Tests Fail Hashimoto’s Patients
Standard Celiac panels look for tissue Transglutaminase (tTG) antibodies and intestinal damage. If these are absent the patient is told they can eat bread. This ignores the IgG and IgA immune response to gliadin that drives NCGS.
A negative Celiac test is not a “green light” for a thyroid patient to consume gluten. It simply rules out one specific pathology. It ignores other equally damaging inflammatory pathways.
Comparison Table: Celiac vs. NCGS vs. Hashimoto’s Reactivity
| Feature | Celiac Disease | Non-Celiac Gluten Sensitivity (NCGS) | Hashimoto’s Thyroiditis (Gluten-Triggered) |
|---|---|---|---|
| Primary Biomarker | Tissue Transglutaminase (tTG-IgA) | No specific biomarker (Diagnosis of Exclusion) | TPO & Thyroglobulin Antibodies |
| Gut Pathology | Villous Atrophy (Flattened Villi) | Epithelial Inflammation (No Atrophy) | Increased Intestinal Permeability (Leaky Gut) |
| Reaction Time | Immediate to Delayed | Delayed (Hours to Days) | Delayed (Days to Weeks) |
| Systemic Impact | Malabsorption, Weight Loss | Brain Fog, Joint Pain, Bloating | Hypothyroidism, Fatigue, Hair Loss |
| Required Diet | Strict Gluten-Free (Medical Necessity) | Strict Gluten-Free (Symptom Management) | Gluten-Free/AIP (Autoimmune Management) |
The Medication Factor: Absorption and Conversion
Even if we set aside the autoimmune mechanism gluten presents a mechanical problem. This issue affects patients taking thyroid replacement hormone. This includes medications like Levothyroxine, Synthroid, Tirosint, and Armour.

Is Gluten Blocking Your Levothyroxine?
Levothyroxine absorption occurs primarily in the jejunum and ileum of the small intestine. When a person with gluten sensitivity consumes gluten the resulting inflammation in the jejunum creates a malabsorptive environment. The villi become blunted or inflamed.
This reduces the surface area available to absorb the medication. We frequently observe patients whose TSH fluctuates wildly despite taking the same dose of medication at the same time every day. This instability is often due to variable absorption caused by dietary triggers.
Once Levothyroxine absorption and gluten are addressed by removing the irritant TSH levels often stabilize. Many patients actually require a reduction in their medication dosage. They are finally absorbing it efficiently for the first time.
The T4 to T3 Conversion Block
Your thyroid gland primarily produces T4 (Thyroxine). This hormone is metabolically inactive. It must be converted into T3 (Triiodothyronine) to give you energy. T3 is what burns fat and grows hair.
While the liver handles much of this conversion approximately 20% of T4 to T3 conversion happens in the gut. This is facilitated by healthy gut bacteria known as the microbiome. Gluten intake disrupts the microbiome.
This leads to dysbiosis which is an imbalance of good and bad bacteria. When the gut flora is compromised this critical conversion process stalls. You might have plenty of T4 in your blood satisfying your doctor’s lab sheet. However you likely have low Free T3 leaving you with all the symptoms of hypothyroidism.
Beyond Wheat: Cross-Reactivity and The Trap of “Gluten-Free” Junk
Going gluten-free is the first step. But it is rarely the final step for complex autoimmune cases. The immune system can begin to make mistakes with other proteins that look similar to gluten once it is hyper-sensitized.
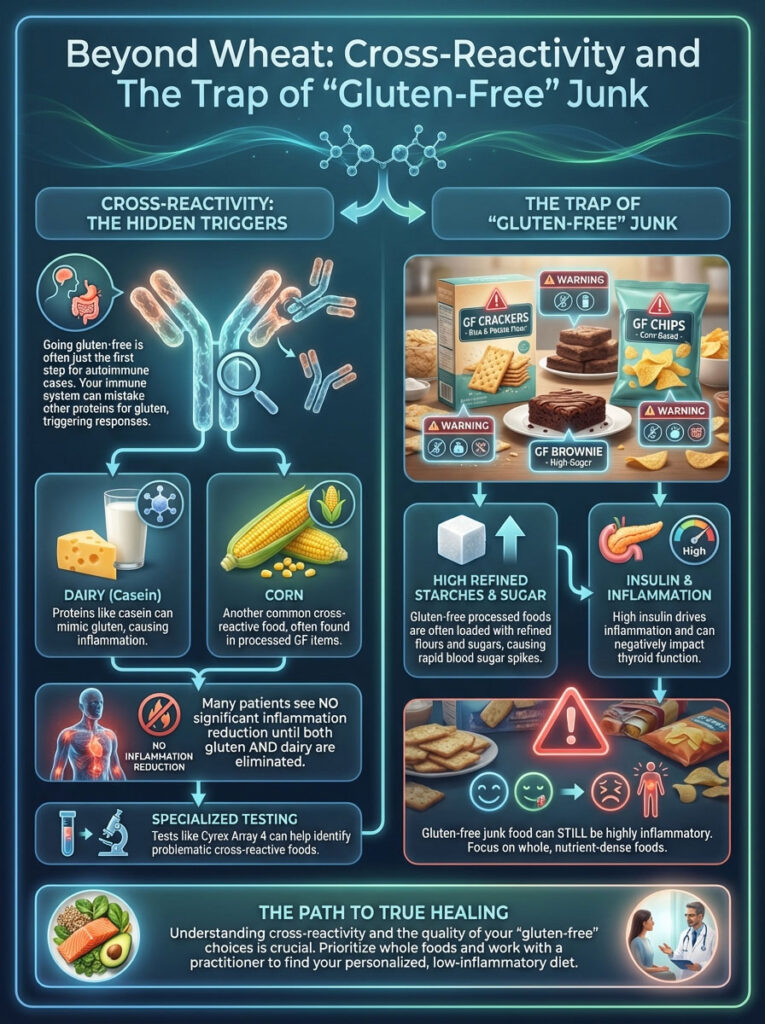
The Phenomenon of Cross-Reactivity
Cross-reactivity occurs when the amino acid sequence of a food protein is similar enough to gluten that the antibodies tag it for destruction. The most common offenders are dairy and corn. The protein structure of casein in dairy is very similar to gliadin.
Many patients see no reduction in inflammation until both gluten and dairy are removed. Corn is often used as a gluten substitute but it can trigger a similar inflammatory response in highly sensitive individuals. Even coffee can be an issue.
Certain instant coffees can mimic gluten proteins due to processing or contamination. We often recommend specialized testing like the Cyrex Array 4 to identify these cross-reactive foods for patients who see no improvement on a standard gluten-free diet.
Why “Gluten-Free” Processed Food is Not the Answer
A major pitfall is swapping whole wheat bread for “Gluten-Free” processed bread. These are often made from potato starch, tapioca starch, and rice flour. While these do not contain gliadin they are extremely high-glycemic.
Consuming these refined starches causes rapid spikes in blood sugar and insulin. High insulin levels drive inflammation. They can also increase the conversion of testosterone to estrogen which further complicates thyroid function.
The goal is not just to avoid gluten but to nourish the body. A diet of gluten-free brownies and crackers is still an inflammatory diet. It will not heal a compromised thyroid.
Nutrient Malabsorption: The Hidden Cost of Gluten
Beyond inflammation gluten causes direct nutrient deficiencies. When the gut lining is inflamed it cannot absorb micronutrients effectively. The thyroid requires specific minerals to function.
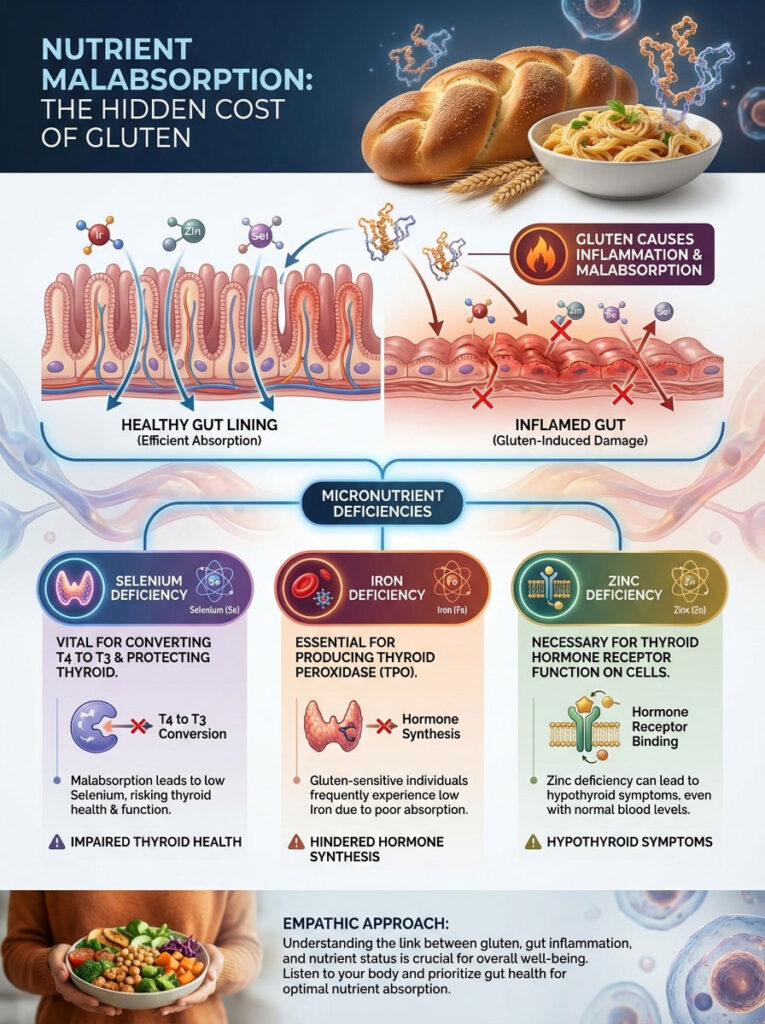
The Selenium Deficit
Selenium is crucial for the enzyme that converts T4 to T3. It also protects the thyroid gland from oxidative stress. Malabsorption in the small intestine often leads to low selenium levels. This leaves the gland vulnerable to damage.
Iron and Ferritin
Iron is required for the production of thyroid peroxidase. Low iron levels are rampant in the gluten-sensitive population due to poor absorption. Without adequate iron the thyroid cannot synthesize hormones efficiently.
Zinc Deficiency
Zinc is necessary for the receptor sites on your cells to accept thyroid hormone. If you are zinc deficient your hormones cannot “dock” onto your cells. This creates hypothyroid symptoms even with normal blood levels.
The Clinical Solution: The Autoimmune Protocol (AIP)
If the standard gluten-free diet is not enough what is the solution? In functional medicine we use the Autoimmune Protocol (AIP). This is a rigorous approach designed to halt the immune attack.
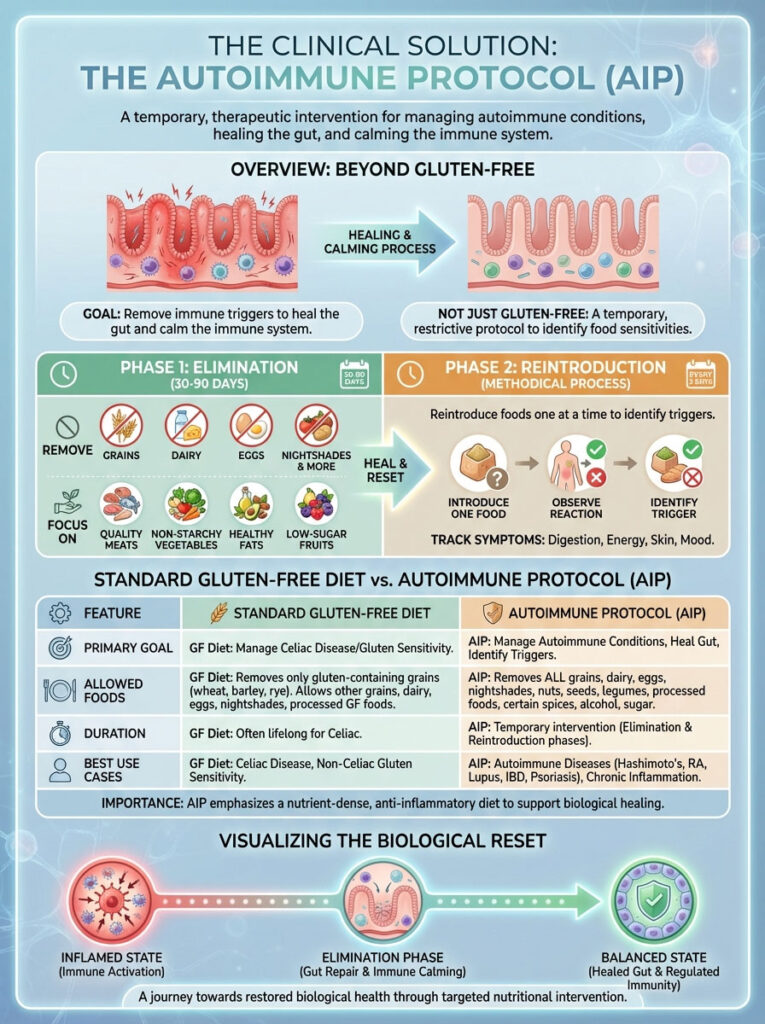
Moving Beyond “Just Gluten-Free”
The AIP is not a lifestyle diet intended for forever. It is a temporary medical intervention. The goal is to strip away all potential immune triggers. This allows the gut lining to heal and the immune system to calm down.
Think of it as hitting the “reset” button on your biology. It reduces antibody production by removing the stimulus. It is the gold standard for Hashimoto’s remission.
Phase 1: Elimination (The Healing Phase)
For a period of 30 to 90 days the patient eliminates several food groups. This includes grains like rice and corn. Dairy is removed completely.
- Eggs are removed because the whites can be inflammatory.
- Nuts and seeds are paused due to phytic acid and potential irritation.
- Nightshades such as tomatoes, potatoes, peppers, and eggplant are avoided.
- Alcohol and processed sugars are strictly forbidden.
This leaves a diet rich in organic meats and fish. It includes massive amounts of vegetables and healthy fats like avocado and olive oil. It is nutrient-dense and anti-inflammatory.
Phase 2: Reintroduction
Once symptoms improve and antibodies drop foods are reintroduced one at a time. We typically reintroduce one food every 3 days. This allows the patient to monitor for reactions.
This process allows the patient to create a personalized diet. The goal is a diet that is as broad as possible without triggering autoimmunity.
Comparison Table: Standard Gluten-Free Diet vs. Autoimmune Protocol (AIP)
| Aspect | Standard Gluten-Free Diet (GFD) | Autoimmune Protocol (AIP) |
|---|---|---|
| Primary Goal | Avoid Gliadin/Gluten | Heal Gut Lining & Lower Inflammation |
| Allowed Grains | Corn, Rice, Oats, Quinoa | None (Grain-Free) |
| Dairy | Allowed | Prohibited (Casein triggers) |
| Nightshades | Allowed (Tomatoes, Potatoes, Peppers) | Prohibited (Solanine triggers) |
| Best For | Maintenance / NCGS | Active Autoimmune Flare / High Antibodies |
| Duration | Lifelong | Temporary (30-90 Days) then Reintroduction |
Supplements to Repair the Thyroid-Gut Axis
While diet is the foundation targeted supplementation can accelerate the repair. We need to support the intestinal lining and thyroid biochemistry simultaneously.

Accelerating Gut Repair
To fix Leaky Gut we need to provide the fuel for the enterocytes to regenerate. The enterocytes are the cells lining the small intestine.
- L-Glutamine: This amino acid is the primary fuel source for the cells lining the small intestine. It helps seal the tight junctions.
- Zinc Carnosine: Research shows this specific form of zinc stabilizes the gut mucosa. It supports epithelial integrity better than standard zinc.
Supporting Thyroid Conversion
To assist the thyroid while the gut heals we use specific nutrients.
- Selenium: This mineral is non-negotiable for Hashimoto’s patients. It acts as an antioxidant. It neutralizes hydrogen peroxide produced during thyroid hormone synthesis. It is proven to lower TPO antibodies.
- Spore-Based Probiotics: Unlike conventional probiotics that often die in stomach acid spore-based strains survive the transit. They help recondition the gut microbiome and fight dysbiosis.
Summary & Key Takeaways
The connection between your plate and your thyroid is undeniable. The question “Is Gluten Killing Your Thyroid? Gluten and Hypothyroidism Truth” is answered by the clear biological pathways of molecular mimicry. It is confirmed by the mechanics of intestinal permeability. When you consume gluten you are not just eating a food.
You are triggering an immune cascade that targets your own tissue. This creates a cycle of inflammation that medication alone cannot fix. The standard of care often ignores this critical piece of the puzzle.
The Final Verdict: For the Hashimoto’s patient a gluten-free lifestyle is not a fad. It is a medical intervention necessary to stop the destruction of the thyroid gland. By removing the trigger and repairing the barrier remission is possible.
If you are still suffering despite medication it is time to look at your diet. Test your TPO antibodies. Consider a 90-day trial of the AIP diet and watch the numbers. Your body has the capacity to heal but you must first stop the attack.
Frequently Asked Questions
How does gluten cause the immune system to attack the thyroid gland?
This occurs through a process called molecular mimicry, where the protein structure of gliadin in gluten closely resembles thyroid tissue. When the immune system identifies gluten as a foreign invader, it produces antibodies that mistakenly attack the thyroid, leading to the cellular destruction seen in Hashimoto’s Thyroiditis.
Can I have gluten-related thyroid issues if my Celiac disease test was negative?
Yes, many patients suffer from Non-Celiac Gluten Sensitivity (NCGS), which does not cause the total villous atrophy required for a Celiac diagnosis but still triggers significant systemic inflammation. In Hashimoto’s patients, the immune response to gluten can suppress thyroid function and elevate antibodies regardless of a Celiac test result.
How long does it take for thyroid antibodies to drop after going gluten-free?
Clinical observations typically show a significant reduction in TPO and Thyroglobulin antibodies within 3 to 6 months of strict gluten elimination. However, because the immune response to gliadin can persist in the body for months, even a single exposure can delay this progress and keep antibody titers elevated.
Does gluten interference affect the absorption of Levothyroxine or Synthroid?
Absolutely. Gluten-induced inflammation in the small intestine, specifically in the jejunum, creates a malabsorptive environment that prevents thyroid medication from entering the bloodstream efficiently. Many patients find their TSH levels stabilize and their required dosage decreases once they remove gluten and heal the gut lining.
What is the role of Zonulin in Hashimoto’s and leaky gut?
Zonulin is a protein that modulates the “tight junctions” of the intestinal wall; gluten triggers its release, leading to increased intestinal permeability or “leaky gut.” This allows undigested proteins and toxins to enter the circulation, which keeps the immune system in a state of chronic hyper-vigilance and perpetuates the attack on the thyroid.
Why do I still have hypothyroid symptoms after removing gluten from my diet?
You may be experiencing cross-reactivity, where your immune system mistakes other proteins—like casein in dairy or proteins in corn—for gluten. Additionally, if you are consuming processed “gluten-free” junk foods, the high-glycemic starches can drive insulin-related inflammation that continues to suppress thyroid hormone conversion.
How does gut health impact the conversion of T4 to T3 thyroid hormones?
While much of the conversion happens in the liver, approximately 20% of inactive T4 is converted into active T3 by healthy gut bacteria. When gluten disrupts the microbiome and causes dysbiosis, this conversion process stalls, often resulting in low Free T3 levels and persistent fatigue despite normal TSH readings.
What are the most common nutrient deficiencies caused by gluten in thyroid patients?
Gluten-driven malabsorption frequently leads to deficiencies in Selenium, Zinc, and Iron (ferritin), all of which are critical for thyroid health. Selenium protects the gland from oxidative stress, while Iron and Zinc are required for hormone synthesis and the cellular receptors that allow the body to use thyroid hormone.
Is the Autoimmune Protocol (AIP) better than a standard gluten-free diet for Hashimoto’s?
For patients in an active autoimmune flare or those with high antibodies, the AIP is superior because it removes additional inflammatory triggers like nightshades, dairy, and eggs. It serves as a powerful short-term medical intervention to “reset” the immune system and allow the intestinal barrier to repair fully.
Can a single “cheat meal” with gluten really damage my thyroid for months?
Yes, research in immunology suggests that the antibody response to gliadin can stay active for up to six months following ingestion. For someone with an autoimmune thyroid condition, a single exposure can re-ignite the inflammatory cascade and stall the healing of the thyroid-gut axis.
What supplements help repair the gut-thyroid axis after stopping gluten?
I frequently recommend L-Glutamine and Zinc Carnosine to help seal the intestinal tight junctions and repair the mucosal lining. Additionally, Selenium is vital for lowering TPO antibodies, while spore-based probiotics can help restore the microbiome balance necessary for proper hormone conversion.
Why does my doctor say my thyroid is fine even though I feel terrible?
Standard TSH tests often fail to account for cellular resistance caused by systemic inflammation or poor T4 to T3 conversion in the gut. Even if your blood levels look “normal,” the underlying autoimmune attack triggered by dietary proteins like gluten can leave your cells unable to utilize the hormone effectively.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Hashimoto’s Thyroiditis and hypothyroidism are complex medical conditions that require professional management. Always consult a qualified healthcare professional or endocrinologist before making significant changes to your diet, supplements, or medication regimen.
References
- Physiological Reviews – Zonulin and its regulation of intestinal barrier function – Dr. Alessio Fasano’s landmark study on how gluten triggers leaky gut via the zonulin pathway.
- Clinical and Experimental Immunology – Celiac disease and autoimmune thyroid disease – Research documenting the high prevalence of thyroid disorders in patients with gluten reactivity.
- Journal of Clinical Endocrinology & Metabolism – The impact of gastrointestinal disorders on thyroxine absorption – A study detailing how gut inflammation interferes with Levothyroxine efficacy.
- Dr. Datis Kharrazian – Why Do I Still Have Thyroid Symptoms? – Expert clinical insights into the thyroid-gut axis and the mechanisms of molecular mimicry.
- World Journal of Gastroenterology – Non-Celiac Gluten Sensitivity: The New Frontier – Statistical data on the prevalence of NCGS and its systemic inflammatory effects beyond the digestive tract.