You sit in the doctor’s office. You are tired of feeling cold and tired of the hair coming out in the shower. You are tired of the scale not budging despite your best efforts. You have heard the success stories. Neighbors are dropping thirty pounds in two months. Colleagues are bragging about their boundless energy. Naturally, you wonder if the Keto Diet for Hypothyroidism is the missing piece of your metabolic puzzle.
Table of Contents
It is a scenario I see in my functional medicine practice almost daily. A patient adopts a strict ketogenic lifestyle to manage their weight. They see incredible results for the first six weeks. Then they hit a wall. Suddenly, the fatigue returns with a vengeance. The weight starts creeping back up.
This is the metabolic paradox of the thyroid patient. We exist in a medical landscape where standard advice often ignores nutrition. Yet functional endocrinology tells us that what you eat directly signals your hormones. The conflict here is biological. Suppressing insulin is fantastic for weight loss. But your thyroid hormones rely on insulin for activation. This is not about whether keto is “good” or “bad.” It is about understanding how to modify a powerful metabolic therapy. We want it to support, rather than suppress, your thyroid function.
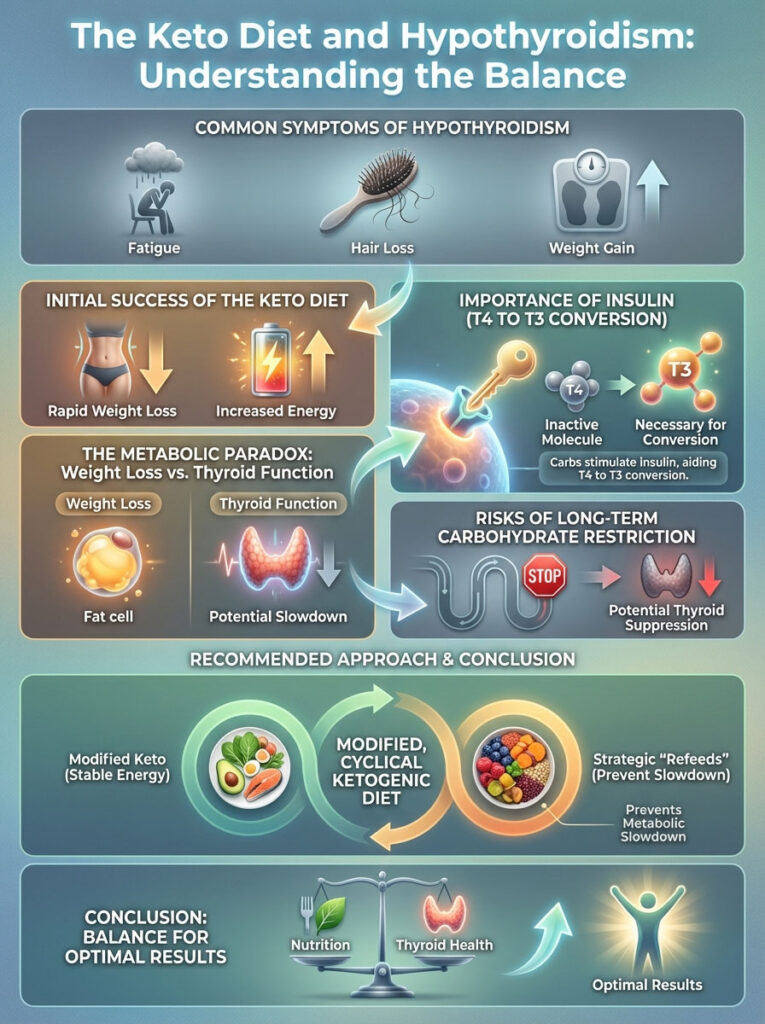
The Keto Diet for Hypothyroidism is a double-edged sword. While the reduction in gluten and sugar lowers the inflammation driving Hashimoto’s, chronic long-term carbohydrate restriction can inhibit the conversion of T4 (inactive hormone) to T3 (active hormone). The most effective approach is not strict, perpetual ketosis. Instead, you should use a modified, cyclical ketogenic diet. This incorporates strategic carbohydrate “refeeds” to prevent metabolic slowdown.
Understanding the Physiology: How Low Carb Impacts the HPT Axis
To understand why a diet might stop working, we have to look under the hood of your metabolism. The thyroid does not operate in a vacuum. It is part of the Hypothalamic-Pituitary-Thyroid (HPT) axis. This is a feedback loop that constantly scans your environment. It decides if it is safe to burn energy.
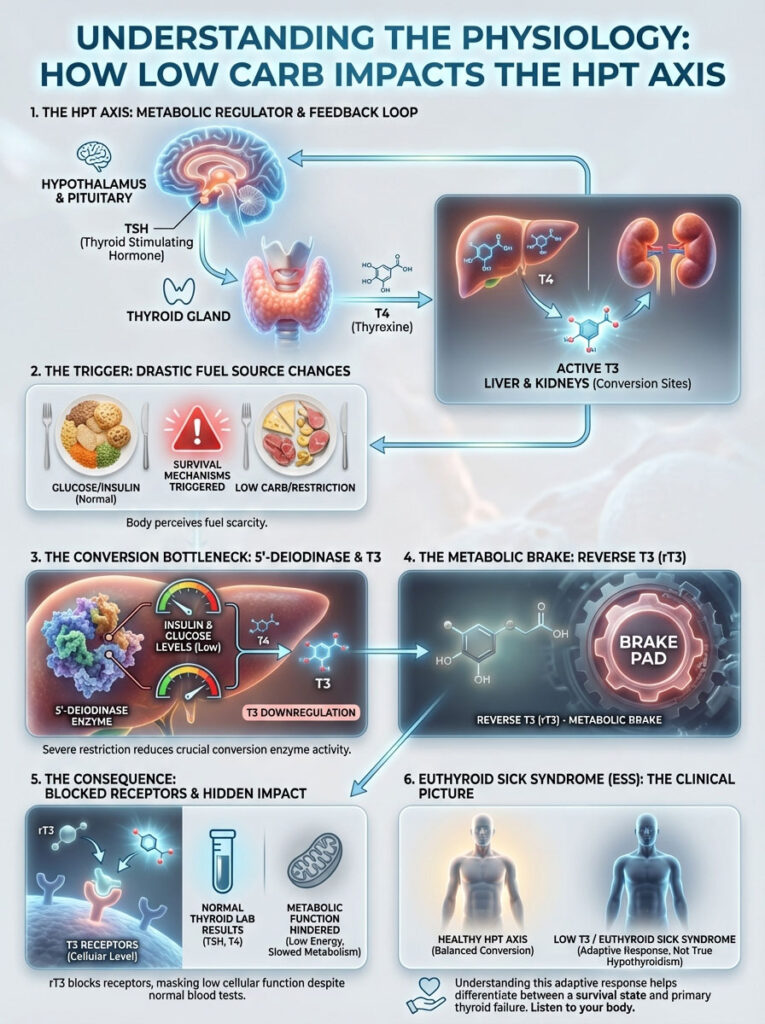
Your body is hardwired for survival. It prioritizes safety over vanity metrics like a flat stomach. When you drastically alter your fuel source, your HPT axis notices immediately. It makes adjustments to ensure you survive what it perceives as a famine.
The T3-Carbohydrate Connection and Insulin Signaling
Here is the biochemistry that most standard advice misses. Your thyroid gland produces mostly T4 (thyroxine). T4 is relatively inactive. It is essentially a storage hormone. To feel energetic and burn fat, your body must convert T4 into T3 (triiodothyronine). This is the active hormone. This conversion happens primarily in the liver and kidneys.
This process relies on a specific enzyme called 5’-deiodinase. Research indicates that this enzyme is highly sensitive to insulin and glucose availability. When you restrict carbohydrates severely, insulin levels drop significantly. This happens on a standard keto diet. While low insulin is the goal for reversing type 2 diabetes, chronically low insulin signals the liver that food is scarce.
Consequently, the activity of the 5’-deiodinase enzyme downregulates. Your body tries to protect you from starvation. It slows down the production of T3. Without adequate T3, your metabolic rate plummets. You might be eating very few calories, but your body is burning even fewer.
The Rise of Reverse T3 (rT3) in Ketosis
When the body decides to conserve energy, it doesn’t just stop making T3. It actively puts the brakes on your metabolism. It diverts the T4 hormone down a different pathway to create Reverse T3 (rT3). Think of Free T3 as the gas pedal. Think of Reverse T3 as the parking brake.
Reverse T3 looks just like T3. It fits into the same receptors on your cells. However, it does not activate them. It blocks them. It is like putting the wrong key in a lock. The key goes in, but the door doesn’t open. Meanwhile, the correct key (Free T3) cannot get in.
In a strict Keto Diet for Hypothyroidism context, rT3 levels often rise. This happens if calories or carbohydrates drop too low for too long. This creates a state where your labs might look “normal” because TSH and T4 are fine. Yet you feel terrible. This is often the real cause of the “Keto Flu” that lasts for months. Symptoms include cold hands and feet, brain fog, and a complete stall in weight loss. It is your body’s intelligent response to perceived famine.
“Euthyroid Sick Syndrome” vs. True Hypothyroidism
Clinicians often refer to this phenomenon as “Low T3 Syndrome” or “Euthyroid Sick Syndrome.” It is critical to distinguish this from a damaged thyroid gland. In this case, the gland is working fine. But the peripheral conversion is being blocked by the environment you have created. Studies on starvation models show that T3 can drop by up to 50% during prolonged fasting or severe carb restriction.
This is a survival mechanism. It is not a disease. But it is exactly what we want to avoid when trying to heal. We want to signal safety to the body. We want high metabolic output. We do not want metabolic hibernation.
Key Statistics: Thyroid & Metabolism
- 90% of adult hypothyroidism cases in the USA are caused by Hashimoto’s Autoimmune Thyroiditis.
- 60% of the conversion from T4 to T3 happens in the liver, making liver health crucial for thyroid patients.
- 50-100g of carbohydrates is the estimated “sweet spot” for maintaining T3 conversion while managing weight.
- 1 in 8 women will develop a thyroid disorder during her lifetime (American Thyroid Association).
- 30% reduction in T3 levels can occur within just 4 days of extreme caloric or carbohydrate restriction.
- 20% of thyroid function depends on healthy gut bacteria, which can change drastically on a keto diet.
The Benefits: Why Keto Can Help (Specifically for Hashimoto’s)
If low carb can slow down conversion, why do so many people with thyroid issues swear by it? The answer lies in the immune system. Since the vast majority of hypothyroid cases are autoimmune (Hashimoto’s), managing the immune attack is often more important than managing the hormone levels directly.
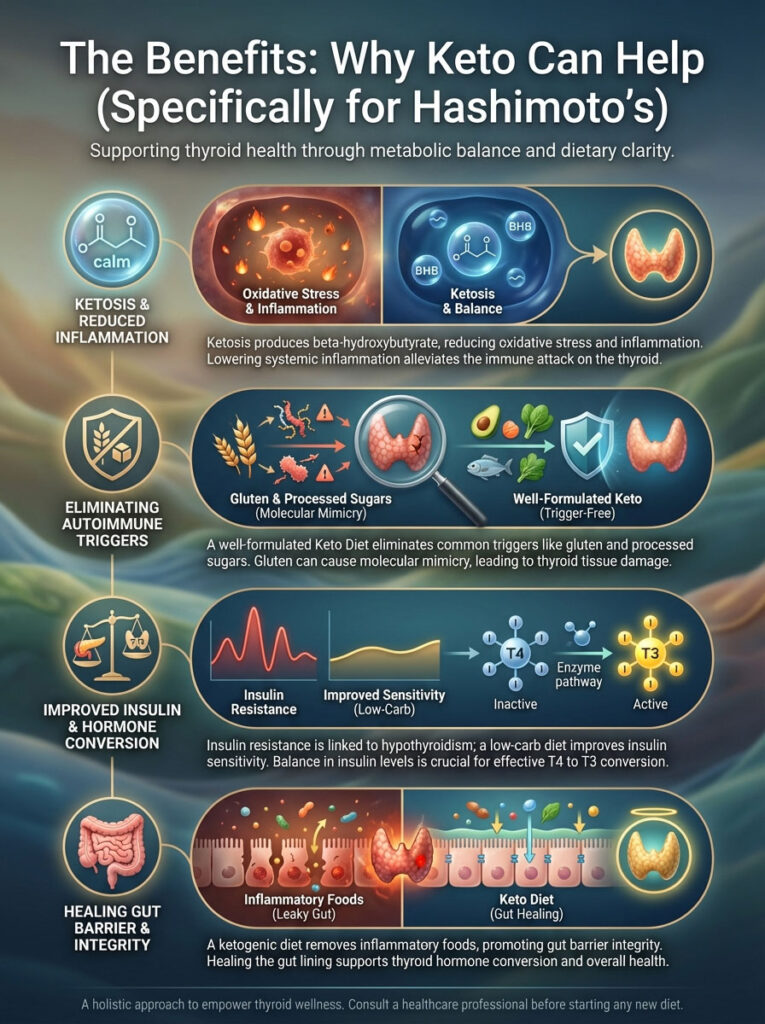
Reducing Inflammation and Antibody Levels
Ketosis produces beta-hydroxybutyrate. This is a ketone body that acts as a powerful signaling molecule. It helps reduce oxidative stress and systemic inflammation. For a patient with Hashimoto’s, the thyroid is under constant assault from antibodies. By lowering systemic inflammation, you lower the assault.
Furthermore, a well-formulated Keto Diet for Hypothyroidism naturally eliminates the most common triggers for autoimmunity. These include gluten, grains, and processed sugars. Gluten is particularly problematic. It has a molecular structure similar to thyroid tissue. When you eat gluten, the body attacks the gluten. But it often attacks the thyroid gland by mistake. This process is known as molecular mimicry. Removing these triggers often leads to a drastic reduction in TPO antibodies.
Addressing Insulin Resistance and Leptin Resistance
There is a strong correlation between hypothyroidism and insulin resistance. When cells become resistant to insulin, it creates a vicious cycle. This leads to more inflammation and weight gain. By using a low-carb approach to restore insulin sensitivity, you eventually help the thyroid receptors work better. The key is balance. We need enough insulin to convert T4 to T3. But we do not want so much that we remain insulin resistant. This is where the nuance of a modified diet comes into play.
Healing the Gut Lining
The gut is often called the “second brain,” but for thyroid patients, it is the second thyroid. Roughly 20% of T4 to T3 conversion happens in the gut. This requires a healthy microbiome and sulfatase enzyme activity. Standard American diets promote intestinal permeability, or “leaky gut.” This allows toxins to enter the bloodstream.
A ketogenic diet removes inflammatory grains and legumes. These foods contain lectins and phytates that can damage the gut lining. By removing these irritants, the gut barrier can heal. A sealed gut prevents the immune system from overreacting. This calms the autoimmune flare-ups associated with Hashimoto’s.
The Risks: When Keto Hurts Thyroid Function
While the anti-inflammatory benefits are clear, the hormonal costs can be steep if the diet is executed without care. We must look at the adrenal connection.

The Adrenal-Thyroid Crosstalk (Cortisol vs. DHEA)
The transition into ketosis is a stressor on the body. It forces the body to manufacture glucose from protein and fat via gluconeogenesis. This process is driven by cortisol, the stress hormone. The HPA (Hypothalamic-Pituitary-Adrenal) axis and the thyroid axis are intimately connected.
When cortisol remains chemically elevated due to strict dieting, fasting, or life stress, it causes problems. It directly inhibits the conversion of T4 to T3. It also increases the production of Reverse T3. Patients who already suffer from “Adrenal Fatigue” (HPA axis dysfunction) are generally the worst candidates for a strict, long-term ketogenic approach. Their bodies cannot handle the additional stressor of carbohydrate deprivation.
Nutrient Depletion and Electrolyte Imbalances
The ketogenic diet is a natural diuretic. As you lose glycogen (stored sugar), you lose water. With that water, you flush out essential electrolytes. These include Sodium, Magnesium, and Potassium. Magnesium is a critical cofactor for thyroid function. If you become deficient, you may experience heart palpitations and muscle cramps. These are often mistaken for thyroid symptoms.
Additionally, there is the Iodine Conundrum. Many people on keto switch to fancy pink Himalayan salt or sea salt. These are typically not iodized. We do not want to overload a Hashimoto’s patient with iodine. However, a complete lack of iodine can lead to goiter and reduced hormone output. It is a delicate balance that requires monitoring.
Mitochondrial Slowdown
Your thyroid hormones control the speed of your mitochondria. These are the power plants inside your cells. When T3 is low, mitochondria produce less ATP (energy). If you are on a strict keto diet and your T3 drops, you might feel “heavy” fatigue. This is cellular fatigue. Your cells literally do not have the spark plugs to burn the fat you are eating. This leads to high circulating triglycerides and stalled weight loss.
Strategic Implementation: The Modified Keto-Thyroid Protocol
So, how do we harness the anti-inflammatory power of keto without tanking our T3 levels? We use a strategy often called “Cyclical Ketogenic Diet” (CKD) or “Targeted Ketogenic Diet” (TKD). This is the gold standard for thyroid patients.

Carb Cycling for Thyroid Health
This is the actionable strategy that changes everything. Instead of staying under 20g of net carbs forever, we implement carb cycling for thyroid health. The logic is simple. We provide intermittent carbohydrate consumption. This is often called a “refeed.” It spikes insulin just enough to upregulate the 5’-deiodinase enzyme. It also resets leptin levels.
For most of my female patients, I recommend a daily intake of 50–75g of net carbs. Alternatively, we use a strategy where they eat strict keto (under 30g) for three days. This is followed by one day of moderate carbs (100g). This prevents the body from adapting to a “starvation” state. These carbs should come from cellular, nutrient-dense sources. Think root vegetables and fruits, not bread or pasta.
Timing Your Carbs
When you eat your carbs matters just as much as what you eat. I advise patients to consume their carbohydrate allocation in the evening. This helps lower cortisol levels before bed. High cortisol at night causes insomnia. By eating carbs at dinner, you support serotonin production. This leads to better sleep. Better sleep means better thyroid function the next day.
Nutrient Synergy: Selenium, Zinc, and Iron
You cannot build a house without bricks. The conversion of T4 to T3 requires specific minerals. Selenium and Zinc are the non-negotiable cofactors for the deiodinase enzyme. Fortunately, a meat-heavy keto diet is often rich in Zinc (from red meat) and Selenium (from pork, beef, and Brazil nuts). However, one must also watch Ferritin levels (iron storage).
Iron is required for the thyroid peroxidase enzyme. If your iron is low, your thyroid cannot function. This is common in women of childbearing age. No amount of carb restriction will fix an iron deficiency. You must test and treat this concurrently.
Comparison Table: Standard Keto vs. Thyroid-Optimized Keto
The following table outlines the differences between a standard approach and one tailored for hormonal health.
| Feature | Standard Ketogenic Diet | Thyroid-Optimized Modified Keto |
|---|---|---|
| Carbohydrate Limit | Strict <20g Net Carbs daily | 30–75g Net Carbs (varied daily) |
| Carb Sources | Mostly fiber/vegetables | Root vegetables, berries, resistant starch |
| Intermittent Fasting | Aggressive (16:8 or OMAD) | Moderate (12:12 or 14:10 max) |
| Protein Intake | Moderate | Moderate-High (to support liver detox) |
| Primary Goal | Deep Ketosis / Ketone production | Metabolic Flexibility / Hormone Balance |
| Refeed Days | Rarely included | Weekly or bi-weekly “Carb Ups” |
| Dairy Consumption | Often high (cheese/cream) | Limited/A2 Dairy (to lower inflammation) |
Analyzing Your Labs: What to Monitor
If you are attempting the Keto Diet for Hypothyroidism, you cannot fly blind. The standard TSH test is insufficient for keto dieters. TSH is a pituitary hormone. It is not a thyroid hormone. It tells us what the brain is asking for. It does not tell us what the tissues are receiving.
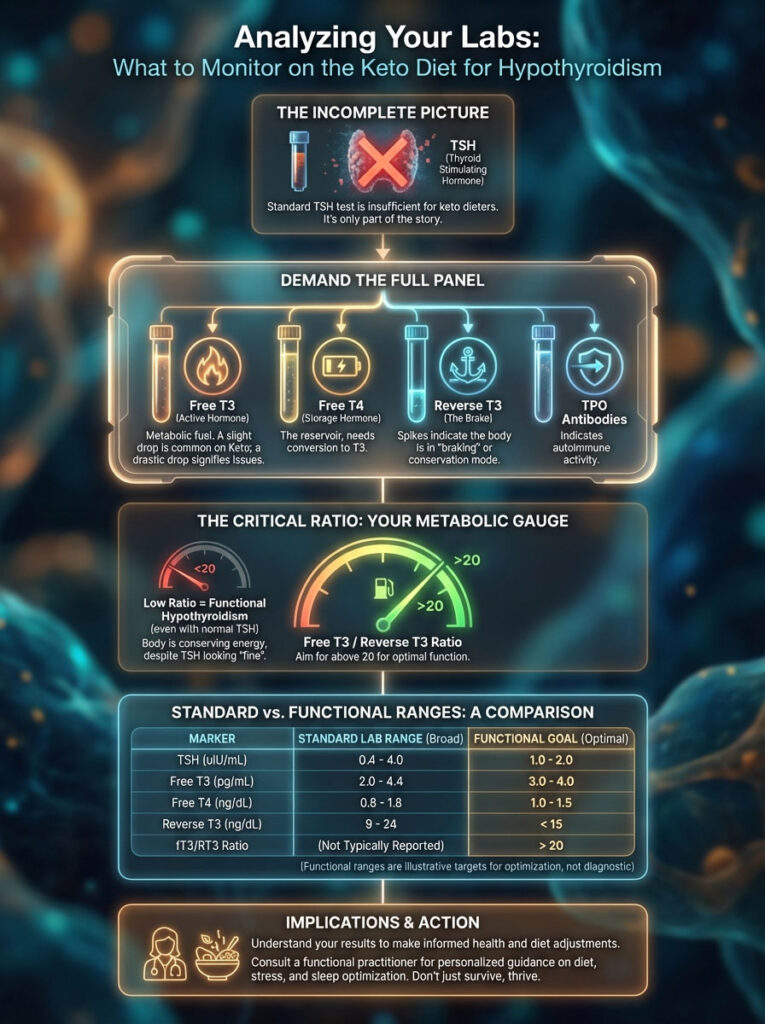
Beyond TSH: The Full Thyroid Panel
To see the full picture, you must demand a full thyroid panel. This includes Free T3, Free T4, Reverse T3, and TPO Antibodies. When adopting a low carb lifestyle, it is common to see Free T3 drop slightly. However, a drastic drop accompanied by a return of symptoms indicates you have pushed the carb restriction too far. If Reverse T3 spikes, it is a clear sign your body is in “braking” mode and needs more fuel.
The Importance of Free T3/Reverse T3 Ratio
Advanced practitioners look at the ratio between Free T3 and Reverse T3. This ratio is the truest indicator of cellular hypothyroidism. You want a ratio greater than 20. If your ratio drops below 20, even if your TSH is normal, you are functionally hypothyroid. This often happens on strict keto when calories are too low. It is a sign to increase carbohydrates immediately.
Comparison Table: Optimal Functional Ranges vs. Standard Lab Ranges
Standard lab ranges are based on a bell curve of the sick population. Functional ranges aim for optimal health.
| Lab Marker | Standard Reference Range | Functional/Optimal Range | What It Indicates on Keto |
|---|---|---|---|
| TSH | 0.5 – 4.5 mIU/L | 1.0 – 2.0 mIU/L | Pituitary signaling |
| Free T3 | 2.0 – 4.4 pg/mL | 3.2 – 4.0 pg/mL | Active hormone status (often drops on keto) |
| Free T4 | 0.8 – 1.8 ng/dL | 1.1 – 1.5 ng/dL | Storage hormone status |
| Reverse T3 | 8 – 25 ng/dL | < 15 ng/dL | Metabolic braking/Starvation mode |
| TPO Antibodies | < 9 IU/mL | 0 IU/mL (Remission) | Autoimmune activity |
Foods to Eat and Avoid for Thyroid Health on Keto
Dietary choices on a Keto Diet for Hypothyroidism must go beyond macros. You can be in ketosis eating processed salami and diet soda. But that will not heal your thyroid. We have to consider the immunogenic properties of food.

The Goitrogen Debate
There is a pervasive myth that thyroid patients must avoid all cruciferous vegetables. People fear broccoli, kale, and cauliflower because they are “goitrogenic.” This means they can theoretically enlarge the thyroid. Here is the truth. Cooking these vegetables deactivates the vast majority of goitrogenic compounds.
Unless you are juicing raw kale every morning and drinking it by the gallon, the benefits outweigh the risks. These veggies contain sulforaphane. This compound aids liver detoxification. Since the liver is where T4 converts to T3, we want to support it. Steaming or roasting these vegetables makes them perfectly safe. However, if you have a confirmed iodine deficiency, you should be more cautious.
Anti-Inflammatory Fats vs. Inflammatory Fats
Not all fats are created equal. To support the cell membranes where thyroid receptors live, focus on anti-inflammatory fats. Coconut oil is exceptional. It contains MCTs (Medium Chain Triglycerides). MCTs bypass the normal digestion process. They provide immediate energy and boost metabolism.
Avocados, olive oil, and grass-fed butter are also staples. Conversely, you must strictly avoid industrial seed oils. Avoid soybean, canola, and corn oil. These are high in Omega-6 fatty acids. Omega-6s drive inflammation and can impair thyroid receptor function. This renders your hormones less effective.
Protein: The Building Block
Thyroid hormones are made from tyrosine. Tyrosine is an amino acid derived from protein. If you do not eat enough protein, you cannot make thyroid hormone. On a modified keto diet, prioritize high-quality protein. Grass-fed beef, wild-caught salmon, and pastured eggs are ideal. Aim for at least 0.8 grams of protein per pound of lean body mass. This also supports the liver, which requires amino acids for detoxification pathways.
Expert Insight: The Dairy Factor
Many keto dieters rely heavily on cheese and heavy cream. However, the protein in dairy (casein) can cross-react with gluten antibodies. If you are not seeing results, try removing dairy for 30 days. Many of my patients find that their “weight loss stall” was actually water retention caused by dairy inflammation.
Managing Medication on Keto
A major oversight for many patients is how the diet affects their medication absorption. Whether you take levothyroxine (Synthroid), liothyronine (Cytomel), or desiccated thyroid (Armour), your needs may change.

Absorption Issues
Keto meals are high in fat. Dietary fat does not typically interfere with thyroid medication absorption if separated by time. However, high fiber intake from massive amounts of vegetables can bind to medication. Always take your thyroid medication on an empty stomach. Take it at least one hour before eating or drinking coffee. Coffee increases gut motility and can flush the medication through your system before it is absorbed.
Decreased Dosage Needs
As you lose weight and inflammation drops, your medication needs often decrease. A dose that was perfect when you were 20 pounds heavier may now be too high. Signs of over-medication include anxiety, rapid heart rate, and insomnia. If you experience this on keto, do not assume it is “keto electrolytes.” Check your TSH and Free T4. You may need to lower your dose with your doctor’s supervision.
Lifestyle Factors: Sleep and Stress
You cannot out-diet a stressful lifestyle. The Keto Diet for Hypothyroidism will fail if you do not manage cortisol. High cortisol blunts the thyroid response.
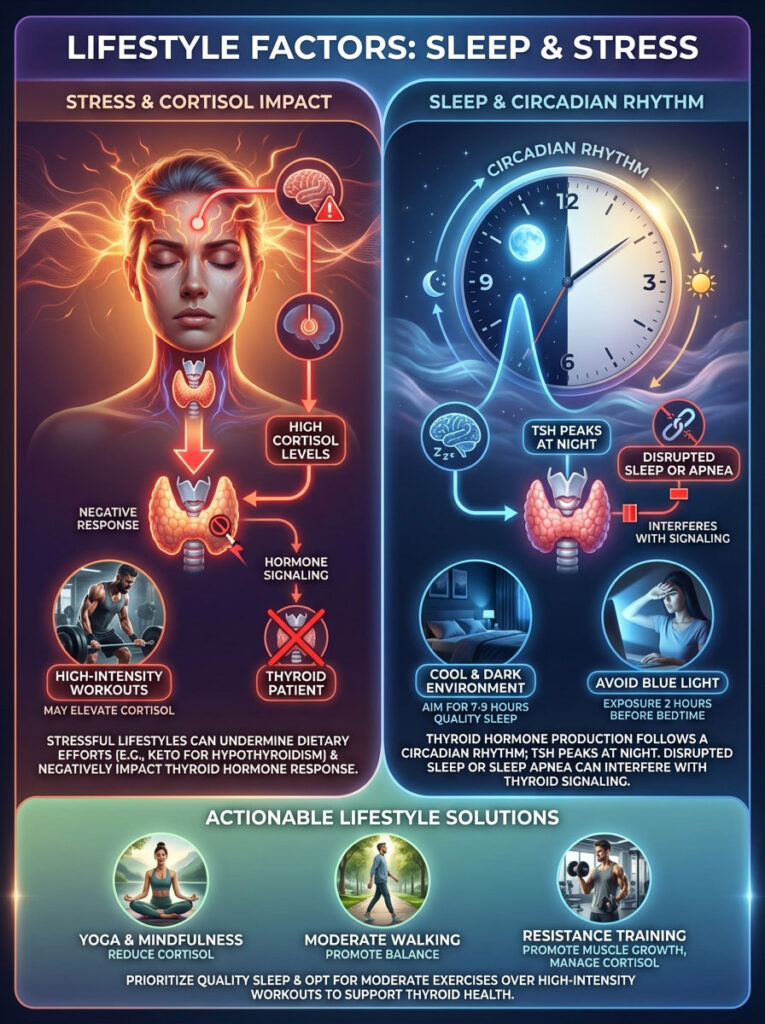
Sleep Hygiene
Thyroid hormone production follows a circadian rhythm. TSH peaks in the middle of the night. If you have disrupted sleep or sleep apnea (common in hypothyroid patients), you disrupt this signal. Prioritize 7-9 hours of sleep. Keep your room cool and dark. Avoid blue light from screens two hours before bed.
Exercise Selection
Many patients try to “burn off” the weight with high-intensity interval training (HIIT) or CrossFit. While these are great for healthy individuals, they can crush a thyroid patient. Intense cardio spikes cortisol. Instead, focus on resistance training. Building muscle increases your basal metabolic rate. It makes you more insulin sensitive without the massive cortisol spike. Walking and yoga are also excellent for lowering stress hormones.
Case Studies and Clinical Observations
Let’s look at how this plays out in the real world. Real scenarios help illustrate the nuance required.

Scenario A: The Stalled Dieter
Consider a 34-year-old woman with Hashimoto’s. She went strict keto and lost 15 pounds of inflammation weight in the first month. But by month three, her hair was thinning. She was exhausted. Her labs showed low Free T3 and high Reverse T3. The solution was not to quit keto. It was to modify it. We added 1/2 cup of sweet potato to her dinner every night. We also supplemented with Selenium. Within weeks, her energy returned. The weight loss resumed because we took her body out of “starvation mode.”
Scenario B: The Stressed Faster
In another case, we had a post-menopausal woman with high cortisol and belly fat. She was doing One Meal A Day (OMAD) and strict keto. Her body was under immense stress from the fasting. We stopped the fasting. We switched her to three high-protein meals a day. We increased her carbs to 75g daily. Her cortisol dropped. Her thyroid function improved. These examples highlight that Hashimoto’s and keto can work together, but only if the approach is tailored to the individual’s stress levels and physiology.
Environmental Toxins and Detoxification
One often overlooked aspect of rapid weight loss on keto is the release of toxins. Persistent Organic Pollutants (POPs) are toxins stored in body fat. When you burn fat rapidly, these toxins are released into the bloodstream. They can disrupt thyroid function.
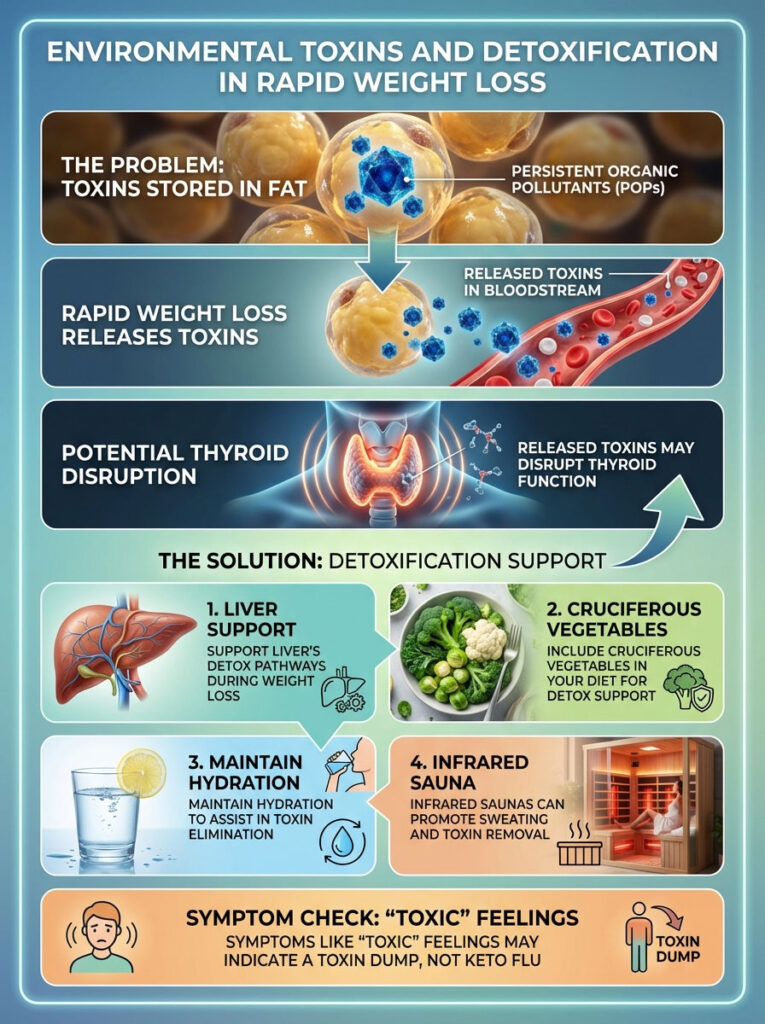
Supporting Detox Pathways
If you are losing weight rapidly, you must support your liver’s detox pathways. This ensures the toxins leave your body rather than recirculating. Cruciferous vegetables help here. Hydration is key. Sweating via infrared saunas can also help eliminate these mobilized toxins. If you feel “toxic” or flu-like during weight loss, it may not be keto flu. It may be a toxin dump. Slow down the weight loss and increase support.
Summary & Key Takeaways
The Keto Diet for Hypothyroidism is a powerful tool. But it is not a religion. It should be used as a therapeutic intervention to lower inflammation and manage insulin. It should not be a dogmatic set of rules that ignores your body’s signals. The evidence is clear. While low carb can help Hashimoto’s by lowering antibodies, strict long-term ketosis can hurt T3 levels if not managed correctly.

The Bottom Line:
- Prioritize nutrient density over strict carb counts.
- Listen to your body. If you are cold, losing hair, or fatigued, you likely need a carb refeed.
- Focus on liver health to support T4 to T3 conversion.
- Use keto to heal the gut and lower inflammation. Then find your personal carb tolerance for long-term maintenance.
- Monitor your labs closely. Look beyond TSH to Free T3 and Reverse T3.
- Manage stress and sleep as aggressively as you manage your macros.
Frequently Asked Questions
Can you follow a ketogenic diet if you have hypothyroidism?
Yes, but it requires a modified approach rather than strict, perpetual ketosis to avoid metabolic slowdown. While the anti-inflammatory nature of keto helps manage Hashimoto’s, long-term carbohydrate restriction can downregulate the HPT axis and inhibit the peripheral conversion of thyroid hormones.
Why does a strict low-carb diet sometimes cause T3 levels to drop?
The enzyme 5’-deiodinase, which converts inactive T4 into active T3, is highly sensitive to insulin and glucose availability. When insulin levels remain chronically low, the liver reduces this conversion to conserve energy, potentially leading to a functional state called Euthyroid Sick Syndrome.
Is the keto diet beneficial for reducing Hashimoto’s antibodies?
The keto diet is excellent for reducing TPO antibodies because it eliminates common autoimmune triggers like gluten and processed sugar. By producing anti-inflammatory ketones like beta-hydroxybutyrate, the diet helps calm the immune system’s attack on the thyroid gland.
What is carb cycling and how does it help thyroid function?
Carb cycling involves strategically increasing carbohydrate intake, often called refeeds, to spike insulin levels and signal metabolic safety to the brain. This practice prevents the body from entering a starvation state and ensures there is enough insulin to facilitate the conversion of T4 to active T3.
Why am I experiencing hair loss and cold hands on keto with hypothyroidism?
These are classic signs of a metabolic brake caused by elevated Reverse T3 (rT3) levels. When the body perceives a famine due to extreme carbohydrate or calorie restriction, it diverts T4 into rT3, which blocks thyroid receptors and slows your basal metabolic rate.
How do I know if I should increase my carbohydrate intake on keto?
If you experience a weight loss plateau, extreme fatigue, or brain fog that persists beyond the initial transition, your body likely needs more glucose. Monitoring your Free T3 to Reverse T3 ratio is the most accurate clinical way to determine if your carb limit is too low for your thyroid health.
Do I need to avoid broccoli and kale on a keto thyroid diet?
No, you do not need to avoid these nutrient-dense vegetables as long as they are cooked. Steaming or roasting cruciferous vegetables deactivates the goitrogens that could theoretically interfere with iodine uptake, allowing you to benefit from their liver-supporting sulforaphane.
Does keto affect the dosage of thyroid medications like Synthroid?
As systemic inflammation decreases and insulin sensitivity improves, many patients find their medication requirements drop. It is crucial to work with your doctor to monitor TSH and Free T4 levels, as over-medication can lead to symptoms like heart palpitations and insomnia.
What are the best carbohydrate sources for a thyroid-optimized keto diet?
Focus on cellular carbohydrates from whole-food sources like sweet potatoes, winter squash, berries, and carrots rather than processed grains. These provide the necessary glucose for T3 conversion while maintaining a lower glycemic load compared to refined sugars or flours.
Can intermittent fasting be combined with keto for hypothyroid patients?
Caution is advised, as aggressive fasting protocols can significantly increase cortisol, which inhibits T4 to T3 conversion. I typically recommend a gentler 12:12 or 14:10 fasting window to support metabolic flexibility without overstressing the HPA axis and thyroid system.
Which minerals are essential for thyroid conversion while in ketosis?
Selenium and Zinc are the primary cofactors required for the deiodinase enzymes to function properly. Additionally, ensuring adequate Ferritin is vital, as the thyroid peroxidase enzyme depends on iron to produce thyroid hormones in the first place.
What thyroid lab markers are most important to track on a low-carb diet?
A standard TSH test is insufficient; you must demand a full panel including Free T3, Free T4, Reverse T3, and TPO antibodies. The ratio between Free T3 and Reverse T3 provides the most accurate picture of how your diet is impacting your cellular metabolism.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Thyroid conditions are complex and highly individual. The physiological impacts of ketogenic dieting can vary significantly between patients. Always consult with a qualified healthcare professional, such as an endocrinologist or functional medicine practitioner, before making significant changes to your diet, lifestyle, or medication regimen.
References
- American Thyroid Association – https://www.thyroid.org – Provides clinical data on Hashimoto’s prevalence and standard diagnostic ranges for TSH and T4.
- The Journal of Clinical Endocrinology & Metabolism – “Effect of Low Carbohydrate Diets on Thyroid Hormones” – Research detailing the sensitivity of the 5’-deiodinase enzyme to glucose.
- Frontiers in Endocrinology – “The HPT Axis and Energy Expenditure” – A study on how the body adjusts metabolic rate based on nutrient availability and insulin signaling.
- National Center for Biotechnology Information (NCBI) – “Autoimmunity and the Gut-Thyroid Axis” – Documentation regarding the 20% of T4 to T3 conversion that occurs in a healthy gut microbiome.
- Institute for Functional Medicine – https://www.ifm.org – Expert insights on the HPA-HPT axis crosstalk and the impact of cortisol on Reverse T3 production.
- Journal of International Medical Research – “Selenium and Zinc in Thyroid Metabolism” – Findings on the essential cofactors required for active thyroid hormone production.








